PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN –POONAM BODRA
In the matter of Sri MOHAN I.P V/s HDFC ERGO GENERAL INSURANCE CO.LTD.,
Complaint No: BNG-H-018-2122-0093
Award No.: IO/(BNG)/A/HI/0075/2021-22
1) The complaint is for the rejection of reinstatement of policy on renewal.
2) The complaint had taken policy since 2017 with the R.I through Canara Bank which was due
for renewal on 15
th
May 2020. He recently came to know that the policy was not renewed for
the period May 2020 to 2021 despite premium was debited from the bank account. He
received SMS message from the bank for the renewal . Based on the same he communicated
to the bank to increase the sum insured and got quote to pay the premium . Accordingly he
agreed to pay and the premium was debited from bank account on 2
nd
May 2020. The Bank
confirmed the acceptance of policy. Later on he realised that policy was not issued instead
premium was refunded to the bank account on 14.05.2020. Neither the Bank nor the insurance
company informed about non issuance of policy. Since the premium was auto debit he was
under the impression that policy was issued. Hence requested the Forum for reinstating the
policy. Once the policy is reinstated he would like to claim the recently incurred medical
expenses.
3) The Forum noted from the documents that Smt.C.R.Nagavika is the Bank account holder
who has taken the policy covering her in-laws Sri.Mohan I.P and Smt.Shalini Mohan .
4) Mr.Vignesh Gowda the spouse Smt.C.R.Nagavika of the Bank account holder and son of
the Complainant I.P.Mohan raised grievance with the Respondent Insurer vide mail
06.03.2021 for reinstating the policy and the R.I replied stating since the tie up with Canara
Bank ended w.e.f 16
th
May 2020 they refunded the premium. Further they stated to approach
Canara Bank for alternate policy with them from other insurer.
5) The Forum asked the complainant vide mail dt. 20.09.2021 to provide correspondence made
by them with the Insurance Company in between the dates of 14.05.2020( date of premium
refund) to 06.03.2021, request for enhancement of sum insured with the Bank ,quote for
premium given by the Bank and his consent . The complainant replied mail dt. 21.09.2021
stating that he did not follow-up with the Insurance Company until he realised non existence
of policy which is on 06.03.2021. The quote was provided by the Bank representative and all
correspondence done orally with the Bank representative hence there is no documents. It has
been a practice in previous years where the policy was made available on App, he assumed
that the policy will be available on the App and did not follow up any further.
6) The R.I submitted that the Tie-up with Canara Bank has ended and intimation for migration
of policy was sent to the Insured Person. He did not opt for migration of policy . The premium
credit made by the Canara Bank was refunded to the account . Hence there is no reason for
raising the complaint.
Forum observed that there is complete lapses on the part of the complainant as admitted by him that
he did not open the App to view the policy in time and by not making immediate follow-up with
the insurance company though the policy was made through the Bank. He made mail correspondence
with the R.I only on 06.03.2021 for reinstatement of policy after the refund of premium on
14.05.2020. He did not act due diligently to protect his policy renewal being the Health Policy holder
since 2017. He did not produce any documentary proof to establish deficiency of services on the
part of the R.I. It is also noted that the tie-up between the Respondent Insurer and the Canara Bank
was ended as on the date of the renewal. The policy holder who has taken the policy on behalf of in-

laws could have approached Canara Bank for alternate policy being the account holder.
In view of above, the Forum did not find any deficiency of services with the R.I. Hence the
complaint does not fall under Rule No. 13 (1) (f)-(policy servicing related grievances against
insurers and their agents and intermediaries) of Insurance Ombudsman Rule,2017 and treated
as NON-ENTERTAINABLE .
Dated at Bangalore on the 24
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL.CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Sri.T.R.ARUNKUMAR V/s STAR HEALTH AND ALLIED INSURANCE
COMPANY LIMITED
Complaint No: BNG-H-044-2122-0215
Award No: IO/BNG/A/HI/0073/2021-22
• The Complaint emanated from partial settlement of Covid-19 claim under policy No.
P/141131/01/2021/00165 Claim No.CIR/2021/141131/0307911 on the ground of makeshift
package . Representation with the RI could not be resolved. Hence the Complainant
approached this Forum for the relief. The complaint was registered.
• After scrutiny of the documents the Forum informed the R.I to relook the claim . The R.I
reviewed the claim and agreed to settle balance claim amount of Rs. 98,934/- as per limits,
terms and conditions of the policy. The complainant agreed and confirmed the settlement
and gave his consent to close the complaint.
The complaint was resolved on compromise basis wherein both have agreed for the same and hence,
the Complaint is treated as Closed and Disposed off accordingly.
Dated at Bangalore on the 24
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN FOR THE
STATE OF KERALA
AND ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Sri.SHARAD V/s STAR HEALTH AND ALLIED INSURANCE COMPANY
LIMITED
Complaint No: BNG-H-044-2122-0220
Award No: IO/BNG/A/HI/0074/2021-22
• The Complaint emanated from rejection of Covid-19 claim under policy No.
P/141111/01/2021/011756 Claim No.CIR/2021/141111/02529406 on the ground of
hospitalization was not required . Representation with the RI could not be resolved. Hence
the Complainant approached this Forum for the relief. The complaint was registered.
• After the registration the R.I reviewed the claim and agreed to settle claim amount of Rs.
2,26,258/- as per limits, terms and conditions of the policy. The complainant agreed and
confirmed the settlement and gave his consent to close the complaint.
The complaint was resolved on compromise basis wherein both have agreed for the same and hence,
the Complaint is treated as Closed and Disposed off accordingly.
Dated at Bangalore on the 24
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN FOR THE
STATE OF KERALA
AND ADDL.CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Sri.T.R.ARUNKUMAR V/s STAR HEALTH AND ALLIED INSURANCE
COMPANY LIMITED
Complaint No: BNG-H-044-2122-0215
Award No: IO/BNG/A/HI/0073/2021-22
• The Complaint emanated from partial settlement of Covid-19 claim under policy No.
P/141131/01/2021/00165 Claim No.CIR/2021/141131/0307911 on the ground of makeshift
package . Representation with the RI could not be resolved. Hence the Complainant
approached this Forum for the relief. The complaint was registered.
• After scrutiny of the documents the Forum informed the R.I to relook the claim . The R.I
reviewed the claim and agreed to settle balance claim amount of Rs. 98,934/- as per limits,
terms and conditions of the policy. The complainant agreed and confirmed the settlement
and gave his consent to close the complaint.
The complaint was resolved on compromise basis wherein both have agreed for the same and hence,
the Complaint is treated as Closed and Disposed off accordingly.
Dated at Bangalore on the 24
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN FOR THE
STATE OF KERALA
AND ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – POONAM BODRA
In the matter of MR. RAVI SHANKAR H Vs MAX BUPA HEALTH INSURANCE CO.
LTD.
Complaint No: BNG-H-031-2122-0318
Award No.: IO/(BNG)/A/HI/071/2021-22
• The Complaint emanated from short settlement of health claims of Rs.3,36,327/- vide claim
number 683134 under the policy no. 30413853202106 (for the policy period: 23.09.2020 to
22.09.2021) issued by the Respondent Insurer (RI).
• The Complainant (Insured Person -IP) was diagnosed with COVID-19 illness – bilateral
pneumonia and he was hospitalised at Brindhavan Areion Hospital, Bangalore from 13.05.2021
to 24.05.2021.
• RI settled the claim for Rs.1,76,169/- as per Covid package rate and disallowed Rs.1,60,158/-.
• The IP approached Grievance cell of RI on 15.07.2021 for the settlement of the balance amount,
but his plea was not considered favourably.
• Thereafter the IP approached this forum for settlement of his claim amount and the complaint is
not yet posted for personal hearing.
• After the intervention of this Forum, RI vide their mail dated 2.09.2021 agreed to settle the
balance claim for Rs.1,58,434/- as per terms and conditions of the policy.
• The IP vide his mail dated 21.09.2021 addressed to this Forum informed that he has agreed to the
settlement offered by the RI.
• Since the complaints were resolved on a compromise basis wherein both parties have agreed for
the same, the complaints are treated as Closed and Disposed of accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
a. The Complainant shall submit all requirements/Documents required for compliance of award
within 15 days of receipt of the award to the Respondent Insurer
b. As per Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with the
award within thirty days of the receipt of the award and intimate compliance of the same to
the Ombudsman
Dated at Bangalore on the 22
nd
day of September, 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
ADDITIONAL CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN –POONAM BODRA
In the matter of Sri AMIYA RAGHAV V/s CARE HEALTH INSURANCE CO.LTD.,
Complaint No: BNG-H-037-2122-0278
Award No.: IO/(BNG)/A/HI/0070 /2021-22
7) The complaint is for the rejection of cashless claim of Rs.1,27,735/- on 25.07.2018 for non
submission of required necessary documents. The complainant approached GRO on
25.07.2018 and the R.I rejected Grievance on 26.07.2018 and requested the complainant to
submit the claim for re-imbursement with all required necessary documents.
8) The complainant did not submit the claim for re-imbursement with the R.I instead he got
claim under corporate policy as per his mail dt. 4/6/2021 addressed to the R.I.
9) The complainant approached the Forum on 25.06.2021 for rejection of cashless claim,
submitted Annexure VIA claiming for Rs.1,27,735/-
10) The Forum noted that the complainant did not approach the Forum with in one year after the
receipt of the GRO reply rejection dt. 26.07.2018.
11) The Forum asked the complainant vide mail dt. 07.09.2021 the reason for his delay approach
and the reason for relief of Rs.1,27,735/- though the claim was reimbursed by the corporate
policy. He replied vide mail dt. 09.09.2021 stating that : ‘he never wanted the settlement from
Religare as it was already settled by corporate insurance but wanted to know why his
insurance claim was rejected even though he declared everything. The Complaint was never
about money. Further since he was not aware of escalation process to the Forum there was
delay’.
12) The R.I filed their objection to dismiss at the very outset as the complaint is not maintainable
under the provision of Insurance Ombudsman Rules,2017 as per Rule 14 Sub-rule 3(b)(ii) and
the claim is already settled by his Corporate Insurer.
Considering the above, the reason for delay approach to the Forum found to be not satisfactory since
under point No.7.19 of policy terms the RI has provided Grievance procedure along the address &
contact details of the Office of the Ombudsman. However the complaint is not for the relief.
The Forum notes that the complainant did not approach the Forum within one year after the receipt
of the GRO reply dt. 26.07.2018 as per Rule No. 14.3(b)(ii) of Insurance Ombudsman Rule,2017
thus found delay of 2 years 11 months .
Hence the complaint is treated as NON-ENTERTAINABLE under Rule No. 14.3(b)(ii) of
Insurance Ombudsman Rule,2017.
Dated at Bangalore on the 17
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Mr. NARASIMHA REDDY Vs RELIANCE GENERAL INSURANCE CO. LTD.
( MUMBAI )
Complaint No: BNG-H-035-2122-0156
Award No: IO/BNG/A/HI/0069/2021-22
b. The Complaint emanated from repudiation of hospitalisation claim under policy
No.- 14152202820002695 and Claim No. 2012100013626 on the ground that non
allopathic treatment is not payable. Representation along with the RI could not be
resolved. Hence the Complainant approached this Forum for relief. The complaint
was registered on 26.06.2021.
c. After scrutiny of the documents, the Forum informed the R.I to relook the claim .
The R.I vide mail dt. 14.09.2021 informed the Forum that they reviewed the claim
and agreed to settle Rs. 10,790/- against claimed amount of Rs.20,200/-. The
Forum sent the mail to the complainant for his consent if agreeable. The
complainant agreed for the settlement and gave his consent to close the complaint.
d. The complaint was resolved on compromise basis wherein both have agreed for
the same and hence, the Complaint is treated as Closed and Disposed off
accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
(a) The Complainant shall submit all requirements/Documents required for settlement of
award within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
Dated at Bangalore on the 16
th
day of September 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL.CHARGE FOR THE STATE OF
KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Mr. NARASIMHA REDDY Vs RELIANCE GENERAL INSURANCE CO. LTD.
( MUMBAI )
Complaint No: BNG-H-035-2122-0156
Award No: IO/BNG/A/HI/0069/2021-22
e. The Complaint emanated from repudiation of hospitalisation claim under policy
No.- 14152202820002695 and Claim No. 2012100013626 on the ground that non
allopathic treatment is not payable. Representation along with the RI could not be
resolved. Hence the Complainant approached this Forum for relief. The complaint
was registered on 26.06.2021.
f. After scrutiny of the documents, the Forum informed the R.I to relook the claim .
The R.I vide mail dt. 14.09.2021 informed the Forum that they reviewed the claim
and agreed to settle Rs. 10,790/- against claimed amount of Rs.20,200/-. The
Forum sent the mail to the complainant for his consent if agreeable. The
complainant agreed for the settlement and gave his consent to close the complaint.
g. The complaint was resolved on compromise basis wherein both have agreed for
the same and hence, the Complaint is treated as Closed and Disposed off
accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
(b) The Complainant shall submit all requirements/Documents required for settlement of
award within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
Dated at Bangalore on the 16
th
day of September 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL.CHARGE FOR THE STATE OF
KARNATAKA

PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – POONAM BODRA
In the matter of MR. KIRAN KUMAR Vs STAR HEALTH AND ALLIED
INSURANCE CO. LTD.
Complaint No: BNG-H-044-2122-0289
Award No.: IO/(BNG)/A/HI/0068/2021-22
• The Complaint emanated from denial of health claims of Rs.1,42,154/- vide claim number
CIR/2021/111113/2378594 under the policy no. P/111113/01/2021/020245 (for the policy
period: 25.11.2020 to 24.11.2021) issued by the Respondent Insurer (RI).
• The Complainant (Insured Person -IP) was diagnosed with COVID-19 and he was
hospitalised at Ramaiah Medical College Hospital, Bangalore from 20.03.2021 to
29.03.2021.
• The RI repudiated the claim vide letter dated 27.06.2021 stating that the hospitalisation was
not warranted as the IP’s SPO2 level was normal.
• The IP approached Grievance cell of RI on 13.07.2021 for the settlement of the balance
amount, but his plea was not considered favourably.
• Thereafter the IP approached this forum for settlement of his claim amount and the
complaint is not yet posted for personal hearing.
• After the intervention of this Forum, RI vide their mail dated 03.09.2021 agreed to settle the
claim for Rs1,38,216/- as per terms and conditions of the policy.
• The IP vide his mail dated 03.09.2021 addressed to RI informed to settle the offered
amount.
• The IP vide his mail dated 15.09.2021 addressed to this Forum informed that he has agreed
to the settlement offered by the RI.
• Since the complaints were resolved on a compromise basis wherein both parties have agreed
for the same, the complaints are treated as Closed and Disposed of accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
a. The Complainant shall submit all requirements/Documents required for compliance of
award within 15 days of receipt of the award to the Respondent Insurer
b. As per Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with
the award within thirty days of the receipt of the award and intimate compliance of the
same to the Ombudsman
Dated at Bangalore on the 15
th
day of September, 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
ADDITIONAL CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Mr. Loknath R Vs Oriental Insurance Co. Ltd.
Complaint No: BNG-H-050-2122-0282
Award No: IO/BNG/A/HI/0067/2021-22
h. The Complaint emanated from the partial settlement of Covid-19 claim for
Rs. 118337/- against claimed amount of Rs. 210557/- under policy No.-
423000/48/2021/830 and Claim No.-55662122105169. Representation along
with the RI could not be resolved. Hence the Complainant approached this
Forum for relief. The complaint was registered on 10.08.2021.
i. After scrutiny of the documents, the Forum informed the R.I to relook the
claim as the claim was settled in accordance with Covid-19 claim settlement
guidelines of Karnataka Govt. instead of the terms and conditions of the
policy. The R.I vide mail dt. 15.09.2021 informed the Forum that they
reviewed the claim and agreed to settle Rs. 63496/- after deduction of an
amount of Rs. 118337/- already paid to the insured . The Forum sent the mail
to the complainant for his consent if agreeable. The complainant agreed for
the settlement and gave his consent.
j. The complaint was resolved on compromise basis wherein both have agreed
for the same and hence, the Complaint is treated as Closed and Disposed off
accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
(c) The Complainant shall submit all requirements/Documents required for settlement
of award within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate
compliance of the same to the Ombudsman.
Dated at Bangalore on the 15
th
day of September 2021.
( POONAM BODRA )
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL. CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – POONAM BODRA
In the matter of MR. KIRAN KUMAR Vs STAR HEALTH AND ALLIED INSURANCE
CO. LTD.
Complaint No: BNG-H-044-2122-0289
Award No.: IO/(BNG)/A/HI/0068/2021-22
• The Complaint emanated from denial of health claims of Rs.1,42,154/- vide claim number
CIR/2021/111113/2378594 under the policy no. P/111113/01/2021/020245 (for the policy period:
25.11.2020 to 24.11.2021) issued by the Respondent Insurer (RI).
• The Complainant (Insured Person -IP) was diagnosed with COVID-19 and he was hospitalised at
Ramaiah Medical College Hospital, Bangalore from 20.03.2021 to 29.03.2021.
• The RI repudiated the claim vide letter dated 27.06.2021 stating that the hospitalisation was not
warranted as the IP’s SPO2 level was normal.
• The IP approached Grievance cell of RI on 13.07.2021 for the settlement of the balance amount,
but his plea was not considered favourably.
• Thereafter the IP approached this forum for settlement of his claim amount and the complaint is
not yet posted for personal hearing.
• After the intervention of this Forum, RI vide their mail dated 03.09.2021 agreed to settle the
claim for Rs1,38,216/- as per terms and conditions of the policy.
• The IP vide his mail dated 03.09.2021 addressed to RI informed to settle the offered amount.
• The IP vide his mail dated 15.09.2021 addressed to this Forum informed that he has agreed to the
settlement offered by the RI.
• Since the complaints were resolved on a compromise basis wherein both parties have agreed for
the same, the complaints are treated as Closed and Disposed of accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
a. The Complainant shall submit all requirements/Documents required for compliance of award
within 15 days of receipt of the award to the Respondent Insurer
b. As per Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with the
award within thirty days of the receipt of the award and intimate compliance of the same to
the Ombudsman
Dated at Bangalore on the 15
th
day of September, 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
ADDITIONAL CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – POONAM BODRA
In the matter of MR. KIRAN KUMAR Vs STAR HEALTH AND ALLIED INSURANCE
CO. LTD.
Complaint No: BNG-H-044-2122-0289
Award No.: IO/(BNG)/A/HI/0068/2021-22
• The Complaint emanated from denial of health claims of Rs.1,42,154/- vide claim number
CIR/2021/111113/2378594 under the policy no. P/111113/01/2021/020245 (for the policy period:
25.11.2020 to 24.11.2021) issued by the Respondent Insurer (RI).
• The Complainant (Insured Person -IP) was diagnosed with COVID-19 and he was hospitalised at
Ramaiah Medical College Hospital, Bangalore from 20.03.2021 to 29.03.2021.
• The RI repudiated the claim vide letter dated 27.06.2021 stating that the hospitalisation was not
warranted as the IP’s SPO2 level was normal.
• The IP approached Grievance cell of RI on 13.07.2021 for the settlement of the balance amount,
but his plea was not considered favourably.
• Thereafter the IP approached this forum for settlement of his claim amount and the complaint is
not yet posted for personal hearing.
• After the intervention of this Forum, RI vide their mail dated 03.09.2021 agreed to settle the
claim for Rs1,38,216/- as per terms and conditions of the policy.
• The IP vide his mail dated 03.09.2021 addressed to RI informed to settle the offered amount.
• The IP vide his mail dated 15.09.2021 addressed to this Forum informed that he has agreed to the
settlement offered by the RI.
• Since the complaints were resolved on a compromise basis wherein both parties have agreed for
the same, the complaints are treated as Closed and Disposed of accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
c. The Complainant shall submit all requirements/Documents required for compliance of award
within 15 days of receipt of the award to the Respondent Insurer
d. As per Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with the
award within thirty days of the receipt of the award and intimate compliance of the same to
the Ombudsman
Dated at Bangalore on the 15
th
day of September, 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
ADDITIONAL CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Mr. Sunil Ambore Vs United India Insurance Co. Ltd.
Complaint No: BNG-H-051-2122-0179
Award No: IO/BNG/A/HI/0066/2021-22
1. The Complaint emanated from partial settlement of Covid-19 claim under
policy No. 5001002819P111087388 and Claim No.HH872124975 on the
ground of non submission of original money receipt of Rs. 60000/-.
Representation along with the RI could not be resolved. Hence the
Complainant approached this Forum for relief. The complaint was registered
on 02.07.2021.
2. The Forum informed the R.I to relook the claim after the complainant informed
the Forum that he has already submitted the required documents . The R.I vide
mail dt. 15.09.2021 informed the Forum that they reviewed the claim and
settled Rs.60000/- against claimed amount of Rs.60000/- via NEFT( no.-
21223788941) on 24.08.2021. The Forum sent the mail to the complainant for
his consent if agreeable. The complainant has confirmed the receipt of amount
Rs. 60000/- vide his mail dt. 15.09.2021 and gave his consent for closing the
complaint .
3. The complaint was resolved on compromise basis wherein both have agreed
for the same and hence, the Complaint is treated as Closed and Disposed off
accordingly.
Dated at Bangalore on the 15
th
day of September 2021.
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Mr. Manish Bahety V/s HDFC Ergo General Insurance Co. Ltd.
Complaint No: BNG-H-018-2122-0092
Award No: IO/BNG/A/HI/0065/2021-22
4. The Complaint emanated from repudiation of hospitalisation claim under
policy No.-2805203520424501000 and Claim No. - RR-HS20-12335435 on
the ground that the submitted claim is for the illness which has a specific 2
years of waiting period as per the policy. Representation along with the RI
could not be resolved. Hence the Complainant approached this Forum for relief.
The complaint was registered on 22.04.2021.
5. After scrutiny of the documents, the Forum informed the R.I to relook the
claim .The R.I vide mail dt. 14.09.2021 informed the Forum that they reviewed
the claim and agreed to settle Rs. 97971/- against claimed amount of
Rs.98271/- . The Forum sent the mail to the complainant for his consent if
agreeable. The complainant agreed for the settlement and gave his consent.
6. The complaint was resolved on compromise basis wherein both have agreed
for the same and hence, the Complaint is treated as Closed and Disposed off
accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
I.The Complainant shall submit all requirements/Documents required for settlement of award
within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
Dated at Bangalore on the 14
th
day of September 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL.CHARGE FOR THE STATE OF
KARNATAKA

PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – POONAM BODRA
In the matter of: Mrs. Kamal Deep Vs Care Health Insurance Limited
Complaint No: BNG-H-037-2122-0309
Award No.: IO/(BNG)/A/HI/0064/2021-22
• The Complaint emanated from the repudiation of health claim vide claim number
91575144-01 under the policy no. 17642769 issued by Respondent Insurer (RI).
• Complainant’s daughter Ms. Anisha Peter (Insured Person -IP) was admitted at Aster
CMI Hospital on 30.01.2021 wherein she was diagnosed with Postprandial
Hyperglycemia.
• Post the discharge of IP, the complainant filed a reimbursement claim and the RI
repudiated the claim on the ground of non-disclosure of pre-existing disease.
• Complainant approached Grievance cell of RI on 16.07.2021 requested to consider
the claim, but her plea was not considered favourably.
• Thereafter the complainant approached this forum for settlement of her claim and the
complaint is yet to be posted for personal hearing.
• After the intervention of this Forum, RI vide their mail dated 08.09.2021 agreed to
settle the claim for Rs.75,749/- as per term and conditions of the policy.
• Complainant vide her mail dated 13.09.2021 addressed to this Forum informed that
she has agreed to the settlement offer by the RI.
• Since the complaint was resolved on compromise basis wherein both parties have
agreed for the same, the complaint is treated as Closed and Disposed off
accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
c. The Complainant shall submit all requirements/Documents required for compliance of
award within 15 days of receipt of the award to the Respondent Insurer
d. As per Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with
the award within thirty days of the receipt of the award and intimate compliance of the
same to the Ombudsman
Dated at Bangalore on the 14
th
day of September, 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
ADDITIONAL CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Sri. M.VIJAYA V/s Care Health Insurance Ltd.(Gurugram)
Complaint No: BNG-H-037-2122-0311
Award No: IO/BNG/A/HI/0063/2021-22
• The Complaint emanated from rejection of claim under policy No. 11515505 for the
hospitalization of Insured Person Smt.Pushpa Vijay for the period 09.01.2021 to 15.01.2021
on the ground of PED which falls under waiting period. Representation along with the RI
could not be resolved. Hence the Complainant approached this Forum for relief. The
complaint was registered.
• After scrutiny of the documents the Forum informed the R.I to relook the claim. The R.I vide
mail dt. 09.09.2021 informed the Forum that they reviewed the claim and agreed to settle
Rs.3,02,190/- against claimed amount of Rs.3,16,810/- by deducting non-medical expenses
as per terms and conditions of policy. The Forum sent the mail to the complainant for his
consent if agreeable. The complainant agreed for the settlement and gave his consent and
requested the Forum to close the complaint vide mail dt. 13.09.2021.
• The complaint was resolved on compromise basis wherein both have agreed for the same and
hence, the Complaint is treated as Closed and Disposed of accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
• The Complainant shall submit all requirements/Documents required for settlement of award
within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
Dated at Bangalore on the 13
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN FOR THE
STATE OF KETALA &
ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Smt. Vidya V.Kathote V/s STAR HEALTH AND ALLIED INSURANCE
COMPANY LIMITED
Complaint No: BNG-H-044-2122-0205
Award No: IO/BNG/A/HI/0062/2021-22
• The Complaint emanated from partial settlement of Covid-19 claim under policy No.
P/141212/01/2021/000279 Claim No.CIR/2021/141212/02013248 on the ground of
settlement as per GIC circular. Representation with the RI could not be resolved. Hence the
Complainant approached this Forum for the relief. The complaint was registered.
• After scrutiny of the documents the Forum informed the R.I to relook the claim. The R.I
reviewed the claim and agreed to settle Rs.85,671/- as per limits, terms and conditions of
the policy. The complainant agreed for the settlement and gave her consent to close the
complaint.
• The complaint was resolved on compromise basis wherein both have agreed for the same and
hence, the Complaint is treated as Closed and Disposed of accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
• The Complainant shall submit all requirements/Documents required for settlement of award
within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
Dated at Bangalore on the 13
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN FOR THE
STATE OF KERALA
AND ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Ms Mumtaz Habib Lala Vs Star Health And Allied Insurance Co. Ltd.
Complaint No: BNG-H-044-2122-0262
Award No: IO/BNG/A/HI/0060/2021-22
• The Complaint emanated from the partial settlement of Covid-19 claim for Rs. 31069/- against
claimed amount of Rs. 73,322/- under policy No.-P/181314/01/2021/008201 and Claim No.-
CIR/2022/181314/2603394 . Representation along with the RI could not be resolved. Hence the
Complainant approached this Forum for relief. The complaint was registered on 04.08.2021.
• After scrutiny of the documents the Forum informed the R.I to relook the claim. The R.I vide mail
dt. 08.09.2021 informed the Forum that they reviewed the claim and agreed to settle Rs. 14,805/-
after deduction of an amount of Rs. 10,886/- already paid via NEFT ( UTR No.-
N222211596891848 ) dated 10.08.2021 . The Forum sent the mail to the complainant for his
consent if agreeable. The complainant agreed for the settlement and gave his consent.
• The complaint was resolved on compromise basis wherein both have agreed for the same and
hence, the Complaint is treated as Closed and Disposed off accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
a) The Complainant shall submit all requirements/Documents required for settlement of award
within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
Dated at Bangalore on the 13
th
day of September 2021.
( POONAM BODRA )
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL. CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- Smt. POONAM BODRA
In the matter of: MR. RASHMI KUMAR RANADIVE V/s MANIPAL CIGNA HEALTH
INSURANCE CO. LTD.
Complaint No: BNG-H-053-2122-0176
Award No: IO/BNG/A/HI/0059/2021-22
• The Complaint emanated from partial settlement of hospitalisation claim under policy
No.PROHLR111229000 and Claim No.24182169 on the ground of consideration of OT
consumables as non-medical expenses by RI. Representation along with the RI could not be
resolved. Hence the Complainant approached this Forum for relief. The complaint was registered
on 01.07.2021.
• After scrutiny of the documents the Forum informed the R.I to relook the claim. The R.I vide mail
dt. 06.09.2021 informed the Forum that they reviewed the claim and agreed to settle Rs.73060/-
against claimed amount of Rs.73060/-. The Forum sent the mail to the complainant for his consent
if agreeable. The complainant agreed for the settlement and gave his consent.
• The complaint was resolved on compromise basis wherein both have agreed for the same and
hence, the Complaint is treated as Closed and Disposed off accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
b) The Complainant shall submit all requirements/Documents required for settlement of award
within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
Dated at Bangalore on the 9
th
day of September 2021.
(Smt. POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- Smt. POONAM BODRA
In the matter of: Sri.SIDDAPPA GOUDA PATIL. V/s STAR HEALTH AND ALLIED
INSURANCE COMPANY LIMITED
Complaint No: BNG-H-044-2122-0151
Award No: IO/BNG/A/HI/0058/2021-22
• The Complaint emanated from rejection of Covid-19 claim under policy No.
P/141141/01/2021/002453 Claim No.CIR/2021/141141/0369817 on the ground of that based on
the hospital records the Insured Person need only home isolation and hospitalization does not
warrant . Representation with the RI could not be resolved. Hence the Complainant approached
this Forum for the relief. The complaint was registered.
• After scrutiny of the documents the Forum informed the R.I to relook the claim . The R.I vide
mail 06.09.2021 informed the Forum that they reviewed the claim and out of claimed amount of
Rs. 1,61,025/- (including Pre & Post Hospitalization charges) an amount of Rs. 1,06,648/- was
settled to the Insured as per policy terms and conditions vide NEFT transaction
no. N222211597540197 dated 10/08/2021 which was agreed by the complainant. The
complainant agreed for the settlement and informed the Forum vide mail dt.06.09.2021 his
consent to close the complaint.
• The complaint was resolved on compromise basis wherein both have agreed for the same and
hence, the Complaint is treated as Closed and Disposed of accordingly.
Dated at Bangalore on the 6th day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN FOR THE
STATE OF KERALA
AND ADDL.CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORETHE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – POONAM BODRA
In the matter of MR. SUNIL ANANT JINRALKAR Vs STAR HEALTH AND ALLIED
INSURANCE CO. LTD.
Complaint No: BNG-H-044-2021-0804
Award No.: IO/(BNG)/A/HI/0057/2021-22
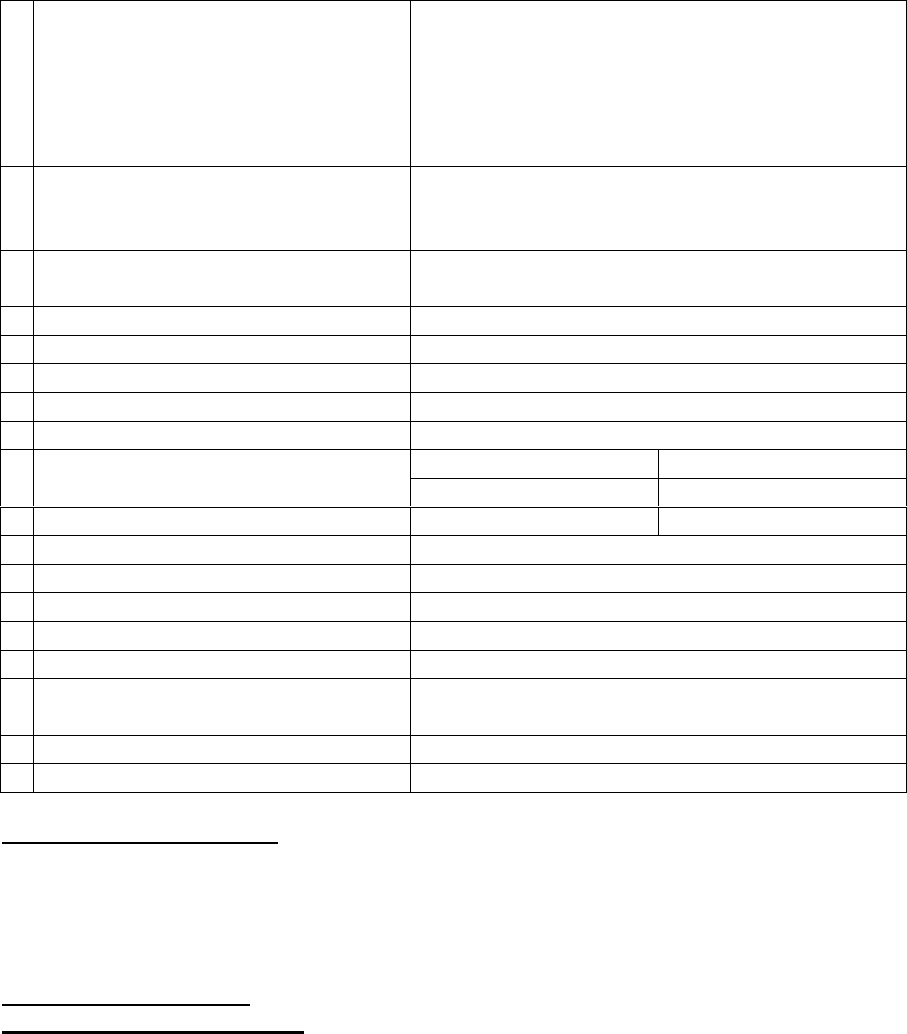
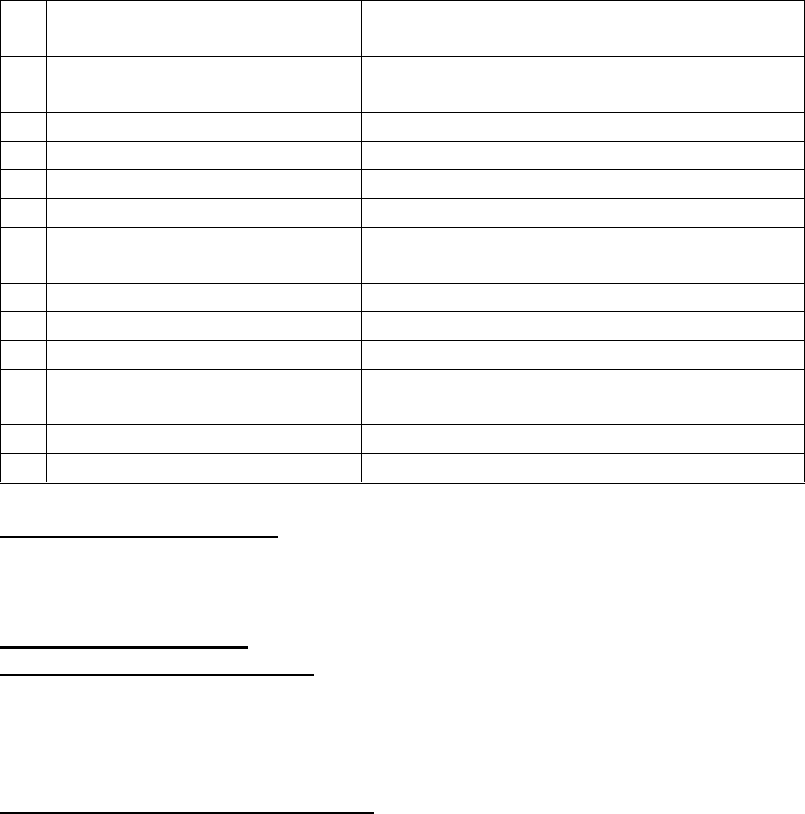
1
Name & Address of the Complainant
Mr. Sunil Anant Jinralkar
Ekdanta Residency, Omkar Wing, Flat No. S1
Raghunath Pet, Angol, Belgaum
Karnataka - 574106
Mobile: 9886484444
Email: [email protected]
2
Policy Number
Type of Policy
Duration of Policy/ Policy Period
P/700002/01/2021/027129
Health (Individual) Corona Kavach Policy
27.07.2020 to 08.05.2021
3
Name of the Policyholder/Proposer
Name of the Insured
Mr. Sunil Anant Jinralkar
Self
4
Name of the Insurer
Star Health and Allied Insurance Co. Ltd.
5
Date of repudiation
NA
6
Reason for repudiation
NA
7
Date of receipt of the Annexure VI A
23.03.2021
8
Nature of complaint
Short Settlement of health claim (COVID-19)
9
Amount of claim
Claim # 0255659
Claim # 0276431
Rs.99,451/-
Rs.6,05,979/-
10
Date of Partial Settlement
28.11.2020
06.01.2021
11
Amount of relief sought
Upto the sum insured limit
12
Complaint registered under Rule no.
13 (1) (b) of Insurance Ombudsman Rules, 2017
13
Date of hearing through Online VC
23.07.2021
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent Insurer
Dr. Umadevi M.B. (Sr. Manager)
Mr. Virupaksha (Legal Dept.)
15
Complaint how disposed
Disallowed
16
Date of Award/Order
02.09.2021
17. Brief Facts of the Case:
The complaint emanated from short settlement of health claims by Respondent Insurer
(hereafter referred to as RI). Complainant represented to Grievance Redressal Officer (GRO)
of RI for reconsideration of his claim. However his plea was not considered favourably. Hence
the complainant approached this Forum for resolution of his grievance.
18. Cause of Complaint:
a) Complainant’s arguments: The Complainant (Insured Person - IP) submitted that he was
covered under Corona Kavach Policy with RI vide policy no. P/700002/01/2021/027129 with
a sum insured of Rs.5,00,000/- for a period from 27.07.2020 to 08.05.2021. IP was diagnosed
with COVID-19 and he was admitted at Venugram Hospital, Belgaum from 22.08.2020 to
26.08.2020. Further IP was admitted at Apoorva Multispeciality Hospital, Belgaum from
28.08.2020 to 11.09.2020. The IP applied reimbursement claims of Rs.99,451/- and
Rs.6,05,979/- whereas the RI settled for Rs.58,377/- and Rs.2,35,000/- for first and second
hospitalisation respectively. The Complainant represented to GRO of the RI for consideration
of his balance claim amount upto the sum insured limit. The Complainant did not get any
favourable reply from the RI. Hence he approached this Forum for help in getting his eligible
claim amount from the RI.
b) Respondent Insurer’s Arguments: The RI in their Self Contained Note (SCN) dated
23.04.2021, whilst admitting issuance of policy submitted that IP was diagnosed with COVID-
19 positive and he was hospitalized at Apoorva Multispeciality Hospital, Karnataka for the
period during 28.08.2020 to 11.09.2020 wherein he was diagnosed with COVID Positive,
ARDS (Acute Respiratory Distress Syndrome) with B/L (Bilateral) Pneumonia. The IP
submitted claim documents for reimbursement of medical expenses of Rs.6,05,979/-. Based on
the available claim documents an amount of Rs. 2,35,000/- was settled to the IP vide NEFT
Transaction No. 101097523304 dated 11.01.2021. An amount of Rs.3,70,979/- was deducted
for the reason as follows:
1.The ICU and ROOM PACKAGE IS INCLUSIVE OF MEDICINES, INVESTIGATION,
O2 and OTHER CHARGES. Hence, Rs.3,70,979/- was deducted.
In view of their submissions, the RI prayed for passing an appropriate order.
19. Reason for Registration of complaint:
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017.
20. The following documents were placed for perusal:
• Complaint along with enclosures,
• Respondent Insurer’s SCN along with enclosures and
• Consent of the Complainant in Annexure VIA & and Respondent Insurer in
VII A
21. Result of personal hearing with both the parties (Observations & Conclusions):
Personal hearing by the way of online Video-conferencing through GoTo Meet was conducted
in the said case. Complainant and Representatives of RI joined using online VC and presented
their case. Confirmation from all the participants about the clarity of audio and video was taken
to which the participants responded positively.
The Complainant strongly argued that the claims should be settled upto the sum insured limit
i.e. Rs.5,00,000/- combining both the claims as per terms and conditions of the policy. The RI
strongly contended that considering the GIC circular they have paid package charges as per
Government of Karnataka notification dated 23.06.2020. The RI further added that the IP was
given injection ACTEMRA 400MG and which is not recommended in case of COVID. They
submitted that there are two different versions of bills and thus there are discrepancies in
hospital billing and suppression of fact by the IP and there could be a fraudulent activity
involved. They also highlighted the exorbitant charges made by the hospitals in both the claims.
Internet studies reveal that ACTEMRA (Tocilizumab) 400 MG INJECTION is a medicine used
alone or with other medications to treat moderate to severe rheumatoid arthritis. The Forum
asked the IP if he was suffered with rheumatoid arthritis and he responded negative.
The Forum directed the RI to investigate for the bills raised and medication/lab-reports given
by the hospitals. They discussed with the hospital’s representative Dr. Shivanand Haligouder
and furnished a report vide their email dated 23.08.2021 which is reproduced as follows:
1. Indication for extended ICU stay - Justified that Mr. Sunil had fluctuating oxygen levels
and severe drop noted, hence admission was extended. Agreed to send complete ICU notes
2. Two different bills- No proper clarification given, said management will be questioned.
3. Administration of multiple antibiotics- No clarification given
4. Unauthenticated lab reports- No pathologist available in Belgaum
5. Chronological order pharmacy bills- No clarification given
6. Indication for Tocilizumab - Not clarified
7. Details about previous admission- He couldn't clarify
Summary of the discussion - The treating doctor couldn't clarify many of the points raised
and repeatedly said admission was made as he had breathlessness, no other issue was
addressed, he also confirmed he will be submitting complete indoor case records, video
recordings and other related papers, but till date it was not provided.
Forum has perused the documentary evidence available on records and the submissions made
by both the parties during the personal hearing pertaining to both the claim numbers. Forum
notes that the complainant filed a single complaint mentioning two claim numbers towards his
hospitalisations. Both the claims were considered under single complaint.
The dispute is whether partial settlement of health claims under the policy is in order or not.
Claim # 0255659 pertaining to 1
st
hospitalisation at Venugram Hospital, Belgaum from
22.08.2020 to 26.08.2020 the IP claimed Rs.99,451/- and RI settled it for Rs.58,377/- by
applying the package charges as per Government of Karnataka notification dated 23.06.2020.
Claim # 0276431 pertaining to 2
nd
hospitalisation at Apoorva Multispeciality Hospital,
Belgaum from 28.08.2020 to 11.09.2020 the IP claimed Rs.6,05,979/- and RI settled it for
Rs.2,35,000/- stating ICU and room package is inclusive of medicines, investigation, O2 and
other charges.
Forum notes from the hospital bills in both hospitalizations that the charges for COVID
isolation ward, Covid private ward and COVID ICU are exorbitantly billed at per day rate of
Rs.15,000/- Rs.18,000/- and Rs.20,000/- respectively. The medical document and the pharmacy
bill reveal that the IP was administered with the injection ACTEMRA 400MG which is not
prescribed for the treatment of COVID patient.
In the absence of proper justification of the exorbitant ward/room/ICU charges and
administration of irrelevant medications/injections by the hospital the Forum concludes that
the instant case is having many inconsistencies. Therefore the claims are fraudulent in nature
and the benefits under the claims cannot be given to the IP.
Forum observes that RI has already settled a total amount of Rs.2,93,377/- (i.e. Rs.58,377/- in
Claim # 0255659 and Rs.2,35,000/- in Claim # 0276431) which could have been denied based
on the discrepancies in claim documents. The Forum notes that having settled an amount
beyond the policy coverage, no recovery of the same can now be made by RI. The Forum
maintains the status quo in regard to claim settlement. The complaint is disallowed.
A W A R D
Taking into account of the facts and circumstances of the case and the submissions made by
both the parties and documents submitted, the Forum maintains the status quo in respect of
claim settlement made by the RI.
The Complaint is DISALLOWED.
Dated at Bangalore on the 02
nd
day of September, 2021.
(POONAM BODRA)
INSURANCE OMBUDSMAN
ADDITIONAL CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Smt.POONAM BODRA
In the matter of Sri MURALI MOHAN PN V/s MANIPAL CIGNA HEALTH
INSURANCE LTD.
Complaint No: BNG-H-053-2021-0823
Award No.: IO/(BNG)/A/HI/0056/2021-22
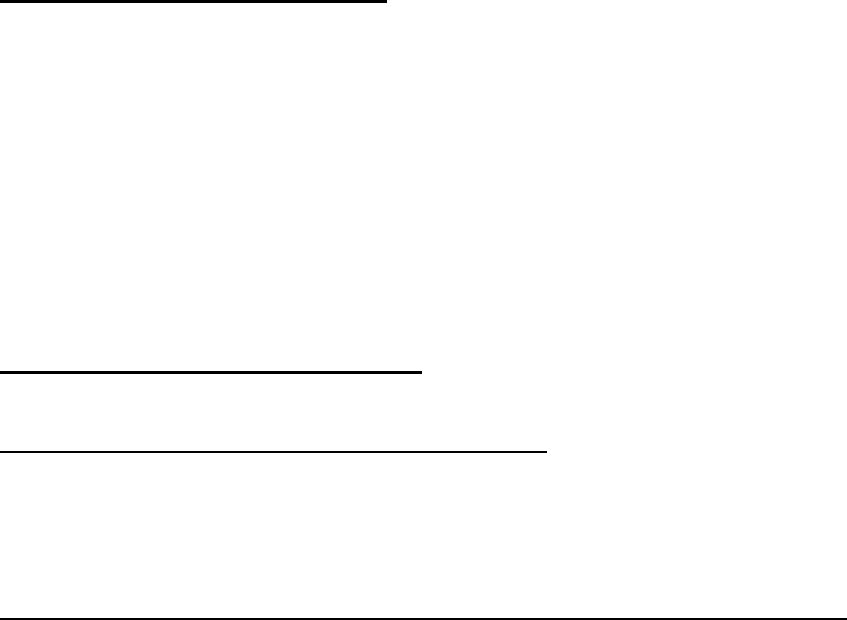
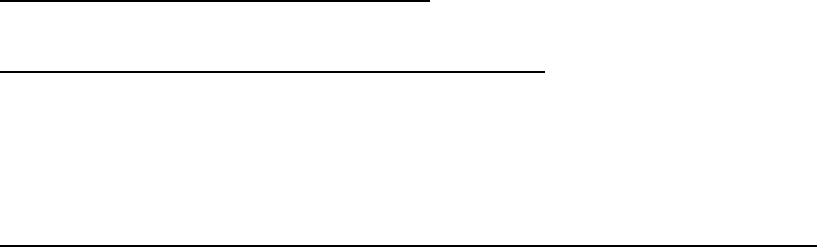
1
Name & Address of the
Complainant
Sri. Murali Mohan P.N
No.94, 2
ND
Main 3rs cross,
Vittal Nagar, ISRO Lay out,
Bangalore
KARNATAKA -560 111
Mob.No. 9972398800
Mail ID :[email protected]
2
Policy No.
Type of Policy
Duration of Policy/ Policy
Period
PROHLR010200106
Pro Health Plus Individual Health Insurance
Policy
26-08-2020 to 25-08-2021
3
Name of the Insured/ Proposer
Name of the policyholder
Sri. Murali Mohan P.N
Self
4
Name of the Respondent
Insurer
Manipal Cigna Health Insurance Company
Limited
5
Date of repudiation
NA
6
Reason for repudiation
Settled as per terms and conditions
7
Date of receipt of Annexure
VI-A
29.03.2021
8
Nature of complaint
Partial settlement of Covid -19 claim
9
Amount of claim
Rs.1,76,891/-
10
Date of Partial Settlement
NA
11
Amount of relief sought
Rs.1,76,891/-
12
Complaint registered under
Rule no:
13(1) (b) Insurance Ombudsman Rules,
2017
13
Date of hearing/place
26.07.2021 / Bengaluru
14
Representation at the hearing
a) For the Complainant
Self
b) For the Respondent Insurer
Smt.Swetha Nair- Legal
15
Complaint how disposed
Dismissed
16
Date of Award/Order
01.09.2021
17. Brief Facts of the Case: It is a case of partial settlement of claim towards hospitalization
for Covid-19.. The Complainant took up the matter with the Grievance Cell of the
Respondent Insurer (RI) and the same was not considered favourably.
18. Cause of Complaint:
a) Complainant’s arguments: The Complainant submitted that he was hospitalized at
Ramakrishna Hospital, Jayanagar for Covid-19 treatment. The Respondent Insurance (RI) did
not consider major medication expenses and settled partial claim.
His representation to GRO along with doctor’s recommendation was not considered favourably.
Hence he approached forum for relief.
b) Respondent Insurer’s Arguments:
RI submitted their Self Contained Note by mail dated 21.04.2021 admitting the issuance of
policy, partial settlement of claim as per terms and conditions of policy.
The Complainant on 28th December 2020 registered a reimbursement claim bearing No.
23583925 (Annexure C) claiming Rs. 5,09,363/-. The reimbursement claim was filed for his
treatment at Ramakrishna Hospital, Bengaluru, Karnataka from 26th October 2020 to 4th
November, 2020 due to Covid Pneumonitis with Covid -19 positive.
After due scrutiny of the claim documents, the Company settled the claim of the Complainant
as per the policy terms and conditions and after making deductions in accordance with the
ceiling provided by GIC circular (Annexure D). It is submitted that in order to allay the fears
of all insurance policyholders and to bring complete clarity and transparency in the treatment
of Covid-19 insurance claims, the General Insurance Council, in discussion with expert
medical professionals employed by member insurance companies, has brought about a
Schedule of rates for Covid-19 claims being filed with its member insurance companies.
Insurance companies shall be guided by the Treatment Protocols prescribed by ICMR. These
rates are broadly based on the schedule of rates suggested for covid-19 treatment by NitiAyog
Panel.
Hence, in accordance with the GIC prescribed rates, the Company settled the claim of the
Complainant for Rs. 2,56,869/- through NEFT no. 021501624GN00009 on 15th February 2021
taking into consideration Category of the Hospital under ‘B’ . For the Complainant’s claim, the
deductions amounting Rs. 2,52,494/- were made being in excess of GIC prescribed rates. The
same was communicated to the Complainant through claim settlement letter dated 16th
February 2021 with detailed reasons for deduction.
It is important to mention herein that as per Annexure D, per day expenses including
Consultation, Nursing Charges, Room Stay & Meals, COVID testing, Monitoring &
Investigations–Biochem & Imaging; Physiotherapy, PPE, Drugs & Medical Consumables,
Biochemical Waste Management & other Protective gear and Bed side procedures like Ryles
tube insertion, urinary tract Catheterization forms part of the per diem cost mentioned in the
above referred table.
The Complainant subsequently approached the grievance cell of the Company for
reconsideration of the deductions.
That as per Annexure D, investigations are also part of the Per Diem cost, however in cases
where diagnostics need to be conducted more frequently, capping has been put for those tests.
Though the investigations form part of Per Diem cost, the Company considered the expenses
for certain investigations, over and above the Per Diem cost for certain investigations namely,
ABG,X-ray, CBC, CT- Chest and D-dimer and paid as the additional amount mentioned against
respective test in below table of Annexure D. Thus, in accordance with the same the Company
paid an additional amount of Rs. 76,103/- to the Complainant towards investigations and the
same was communicated to him vide settlement letter dated 16th March 2021.
In the light of above submissions, it is submitted that the above mentioned claim has already
been settled and the Hon’ble Ombudsman may be pleased to absolve us from the liability.
The claims are paid out of common pool of funds belonging to all the policy holders of the
Company, which makes it obligatory upon the Company to check the genuineness of each claim
before honouring it in the larger interest of all policy holders. They adopt best business and
ethical practices and have dealt with the claims of the complainant with utmost authenticity.
In the light of the above the RI requested the Forum to absolve them from the complaint made.
19. Reason for Registration of complaint:-
The complaint falls within the scope of the Insurance Ombudsman Rules, 2017
20. The following documents were placed for perusal.
(i) Complaint along with enclosures,
(ii) Respondent Insurer’s SCN along with enclosures and
(iii) Consent of the Complainant in Annexure VIA & and Respondent Insurer in VII
A
21. Result of personal hearing with both the parties (Observations & Conclusions):
Personal hearing was conducted through video conference and the participants confirmed the
clarity of audio and video. The complainant submitted that on the day of hearing he received
mail for the balance settlement of Rs.1,26,826/- for which he is not agreeable and argued
that he seek full settlement. Further he contended that as per Doctor’s advice post discharge
he hired oxygen, and commuted by ambulance to his residence hence the same has to be
allowed. The R.I explained in details the non-admissible expenses of Rs. 46,565/- as per
policy terms and conditions. They also submitted that the hospital bills are inflated.
The R.I was asked to submit calculation as per policy terms and conditions reasonable and
customary charges as the Forum noted that the Hospital charged separately for Room Rent,
Nursing Charges, RMO charges Etc.,and for the investigation charges are inflated . As the
complainant strongly contended that there was necessity for oxygen post discharge the RI was
asked to furnish Ct/X-ray results, and the complainant’s SP02 at the time of discharge.
Post hearing the R.I submitted the required details and the Forum has taken the cognizance
of the same while passing this order.
They submitted that bill inflation has been noted in the pathological investigation report,
nursing charges and RMO charges which was billed separately from room charges.
Investigations done are related to the diagnosis, however the charges are inflated. Eg HRCT
billed at 6000.The average cost is 3000-3500/ HRCT. Similarly for Xray the average cost is 500 ,
billed here for 900/xray.ABG test is on an average 400/test, here it has been billed at 900/day
and done daily. D-Dimer done at 1200
Moreover, the HRCT report shows minor covid infection in the chest. While Spo2 levels has
been near normal during hospitalisation, other vitals have remained normal and the
Complainant does not suffer from any co-morbidities. Symptomatically, the Complainant did
not exhibit severe breathing difficulty; nevertheless he has been administered 6 litres of
oxygen which is indicated when oxygen dips below 90%. On the other hand, throughout
admission, the SPO2 levels have remained above 90%.This also indicates inflation. Similarly,
the SPO2 level at discharge was 96%, which does not require oxygen administration at home
for a month. However Oxygen Cylinder to be used outside hospital is a specific non-payable
item under the Non-medical Expenses listed in the policy TnC.
Claim is re-evaluated in the light of reasonable and customary charges as per Clause II.1 of the
policyTnC.
Room rent includes RMO charges and bed charges. These are called out usually by hospitals.
In the policy RMO charges are not payable separately and are to be considered part of room
rent. As per Clause IX(Definitions) Room rent includes associated medical expenses which in
turn includes medical practitioner’s fees. Both definitions under the policy TnC are extracted
below:
“59.Room Rent - Room Rent means the amount charged by a Hospital towards Room and
Boardingexpenses and shall include the associated medical expenses.”
“6.Associated Medical Expenses shall include Room Rent, nursing charges, operation theatre
charges,fees of Medical Practitioner/ surgeon/ anesthetist/ Specialist and diagnostic tests,
excluding cost ofmedicine, conducted within the same Hospital wherethe Insured Person has
been admitted.”
The Nursing charges are usually 500/- day for a shared room, here billed at Rs.3400/- day.
This Forum has perused the documentary evidence available on record and the submissions
made by both the parties during the personal hearing.
The issue to be decided is whether partial settlement of covid-19 claims is in order .
Forum notes that IP was diagnosed with COVID-19 and he was admitted at Ramakrishna
Hospital, Bangalore with the complaint of fever since 1week and cough since 2 days from
26.10.2020 to 04.11.2020 diagnosed with Covid 19 Positive- severe illness with No history of
DM/HTN/Bronchial Asthma/Epilepsy,IHD/ Thyroid Disorder ( No Co morbid) . He was
admitted in Private ward-Unit 1 which is co-sharing ward. IP incurred a total expenses of
Rs.4,71,645/- towards the main hospitalisation bill and filed a reimbursement claim for the
same along with pre and post hospitalization amount of Rs. 13,315/- & 11,343/- respectively,
Health Check up cost of Rs. 11,260/-, Ambulance Rs.1800/- totalling to Rs. 5,09,363/- with
RI. The RI initially settled the claim for an total amount of Rs.2,56,869/- considering the GIC

guidelines and pre post hospitalization amount and further settled Rs.76,103/- towards high
end investigations totalling to Rs.3,32,972/-.
Post hearing the R.I informed the forum that vide transaction No.121102643GN002178 dt.
30.07.2021 they paid balance amount of Rs. 1,26,826/- . Hence found that the R.I settled total
amount of Rs. 4,59,798/-less non payable amount of Rs. 49,565/- .
The Forum has gone through the details of disallowed expenses provided by the R.I and notes
that the expenses towards Oxygen post discharge is an exclusion as per Annexure IV- Under
EXTERNAL DURABLE DEVICES Sl.No136 and the Ambulance charges are payable only
from the residence to the hospital as per II.6 Ambulance cover where as the complainant is
claiming from the hospital to his residence after the discharge. Accordingly he is not entitled
and other disallowed expenses are in order as per terms and conditions of policy.
The Forum observed that the hospital inflated bill by charging under different heads for
Room ,Nursing charges and for the RMO charges beyond the scope of policy coverage as per
the definition No. 59 Room Rent and No.6. Associated Medical Expenses . Accordingly,
the complainant is not entitle for RMO charges . The consultation charges (general Medicines)
are billed for 16 Nos. for the duration of hospitalization period of 10 days found to be inflated
the bill. The R.I Settled the claim beyond the eligible amount even considering towards
nursing charges @Rs.3500/- for 10 days which should have been the part of Room rent.
The Forum also notes that the R.I settled Rs. 1,26,826/- after the hearing on 30.07.2021 which
is before passing order from the Forum found to be not in order when the Forum asked the R.I
to furnish the calculation as per terms and conditions of policy.
The complainant also did not inform the Forum the receipt of Rs.1,26,826/- after the hearing ,
when he sought relief from the Forum for Rs. Rs.1,76,891/- which is not appreciable. In view
of which the Forum considers the disputed amount is Rs.49,565.00 only.
The Forum relies on :
The Hon’ble Supreme Court of India in the case of Suraj Mal Ram Niwas Oil Mills (P) Ltd.
Vs. United India Insurance Co. Ltd. & Anr., interalia held that:
“Before embarking on an examination of the correctness of the grounds of
repudiation of the policy, it would be apposite to examine the nature of a contract
of insurance. It is trite that in a contract of insurance, the rights and obligations
are governed by the terms of the said contract. Therefore, the terms of a contract of
insurance law have to be strictly construed and no exception can be made on the
ground of equity”.
The claims are paid out of common pool of funds belonging to all the policy holders of the
Company , the R.I cannot settle the claim beyond the scope of the policy in the larger interest
of all policy holders. Hence the R.I is strictly advised to adhere the policy terms and conditions
while admitting the claim.
Considering the above the Forum found that the complainant was paid more than the entitled
amount and deduction of Rs. 49,565/- is in order.
Hence, the Complaint is DISMISSED
A W A R D
Taking into account of the facts and circumstances of the case, the documents and
the oral submissions made by both the parties, this Forum found that the
complainant was paid more than the entitled amount beyond the policy terms
and conditions and deduction of Rs. 49,565/- towards disallowed expenses are in
order.
Hence, the Complaint is DISMISSED.
Dated at Bangalore on the 1
st
day SEPTEMBER of 2021.
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA
AND ADDL. CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- Smt. POONAM BODRA
In the matter of: Mr. Santhosh K S Vs Star Health And Allied Insurance Co. Ltd.
Complaint No: BNG-H-044-2122-0137
Award No: IO/BNG/A/HI/0055/2021-22
• The Complaint emanated from repudiation of Covid-19 claim under policy No.-
P/141116/01/2021/007300 and Claim No.-CIR/2022/141116/2405508 on the ground of
unwarranted hospitalisation. Representation along with the RI could not be resolved. Hence
the Complainant approached this Forum for relief. The complaint was registered on
26.05.2021.
• After scrutiny of the documents the Forum informed the R.I to relook the claim. The R.I
vide mail dt. 30.08.2021 informed the complainant that they reviewed the claim and agreed
to settle Rs. 2,50,000/-against claimed amount of Rs.2,50,000/-. The Forum sent the mail
to the complainant for his consent if agreeable. The complainant agreed for the settlement
and gave his consent. The complainant has confirmed the receipt of amount Rs. 2,51,541/-
to the Forum vide his mail dt. 31.08.2021.
• The complaint was resolved on compromise basis wherein both have agreed for the same
and hence, the Complaint is treated as Closed and Disposed off accordingly.
Dated at Bangalore on the 1
st
day of September 2021.
(Smt. POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL. CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF
KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Sri.D.R.MANJUNATH V/s STAR HEALTH AND ALLIED INSURANCE
COMPANY LIMITED
Complaint No: BNG-H-044-2122-0161
Award No: IO/BNG/A/HI/0061/2021-22
• The Complaint emanated from rejection of Covid-19 claim under policy No.
P/141214/01/2020/004750 Claim No.CIR/2021/141214/0355496 on the ground of
discrepancy in the hospital records. Representation with the RI could not be resolved.
Hence the Complainant approached this Forum for the relief. The complaint was registered.
• After scrutiny of the documents the Forum informed the R.I to relook the claim . The R.I
reviewed the claim and agreed to settle Rs.7,07,384/- against claimed amount of
9,66,000/- as per limits, terms and conditions of the policy. The complainant agreed for the
settlement and gave his consent to close the complaint. The R.I confirmed the payment
made through
NEFT –SBI –N247211624855285 dt. 04/09/2021.
The complaint was resolved on compromise basis wherein both have agreed for the same and
hence, the Complaint is treated as Closed and Disposed of accordingly.
Dated at Bangalore on the 13
th
day of SEPTEMBER 2021
(POONAM BODRA)
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA
AND ADDL.CHARGE FOR THE STATE OF KARNATAKA

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, STATE OF KARNATAKA
(UNDER RULE NO: 16/17 of THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN- POONAM BODRA
In the matter of: Ms Mumtaz Habib Lala Vs Star Health And Allied Insurance Co. Ltd.
Complaint No: BNG-H-044-2122-0262
Award No: IO/BNG/A/HI/0060/2021-22
• The Complaint emanated from the partial settlement of Covid-19 claim for Rs. 31069/-
against claimed amount of Rs. 73,322/- under policy No.-P/181314/01/2021/008201 and
Claim No.-CIR/2022/181314/2603394 . Representation along with the RI could not be
resolved. Hence the Complainant approached this Forum for relief. The complaint was
registered on 04.08.2021.
• After scrutiny of the documents the Forum informed the R.I to relook the claim. The R.I
vide mail dt. 08.09.2021 informed the Forum that they reviewed the claim and agreed to
settle Rs. 14,805/- after deduction of an amount of Rs. 10,886/- already paid via NEFT
( UTR No.- N222211596891848 ) dated 10.08.2021 . The Forum sent the mail to the
complainant for his consent if agreeable. The complainant agreed for the settlement and
gave his consent.
• The complaint was resolved on compromise basis wherein both have agreed for the same
and hence, the Complaint is treated as Closed and Disposed off accordingly.
Compliance of Award:
Attention of the Complainant and the Insurer is hereby invited to the following:
c) The Complainant shall submit all requirements/Documents required for settlement of
award within 15 days of receipt of the award to the Respondent Insurer.
b. According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer shall
comply with the award within thirty days of the receipt of the award and intimate
compliance of the same to the Ombudsman.
Dated at Bangalore on the 13
th
day of September 2021.
( POONAM BODRA )
INSURANCE OMBUDSMAN
FOR THE STATE OF KERALA AND
ADDL. CHARGE FOR THE STATE OF KARNATAKA
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, STATE OF M.P. & C.G.
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
OMBUDSMAN – JUSTICE ( RETD.) ANIL KUMAR SRIVASTAVA
Mr Sumeet Bhandawat ..…………………..…………………..……………………………………Complainant
V/S
Manipal Cigna Health Ins Co Ltd………………..……..………..…………………………………Respondent
COMPLAINT NO: BHP-H-053-2122-0019 ORDER NO: IO/BHP/A/HI/ /2021-22
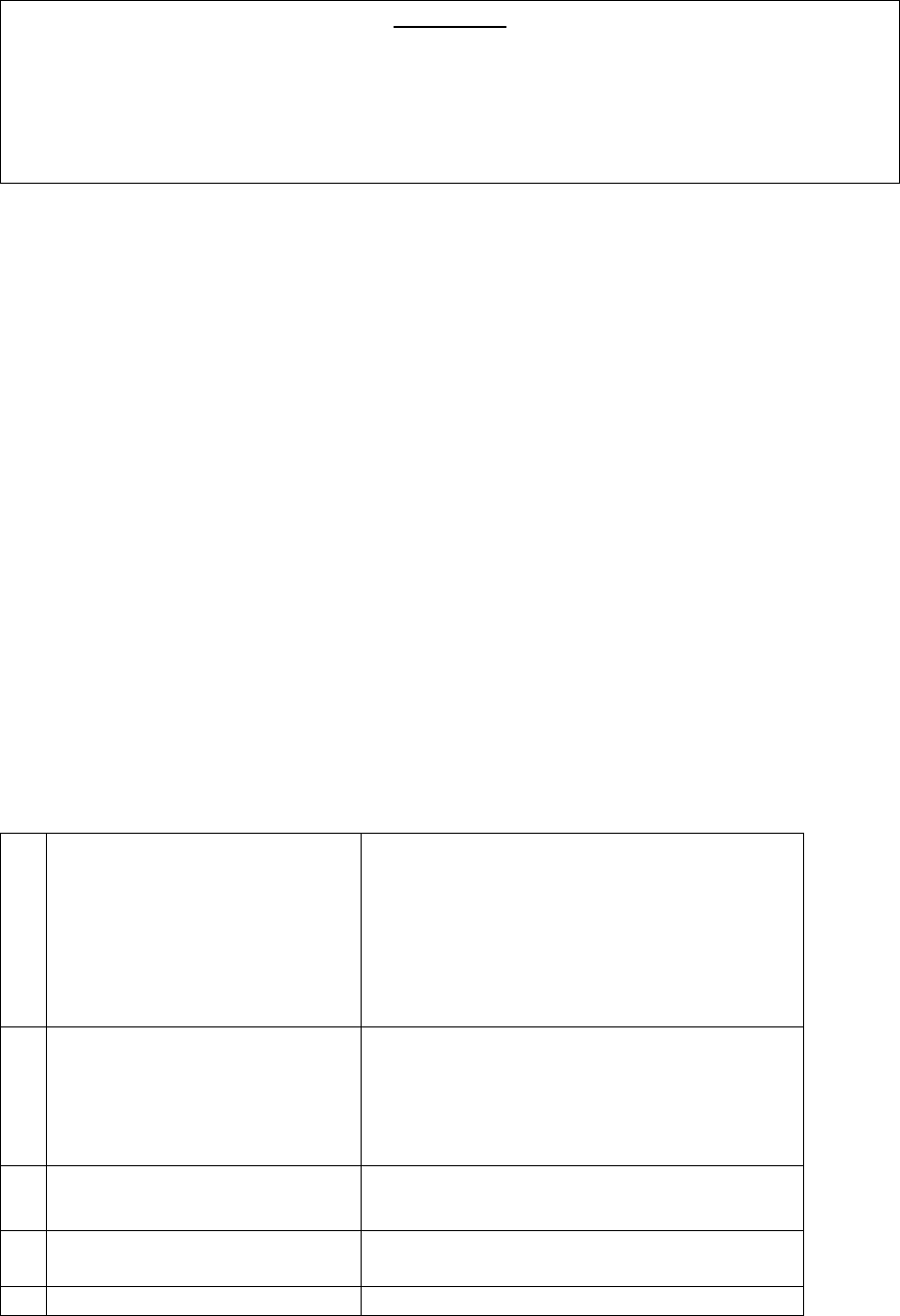
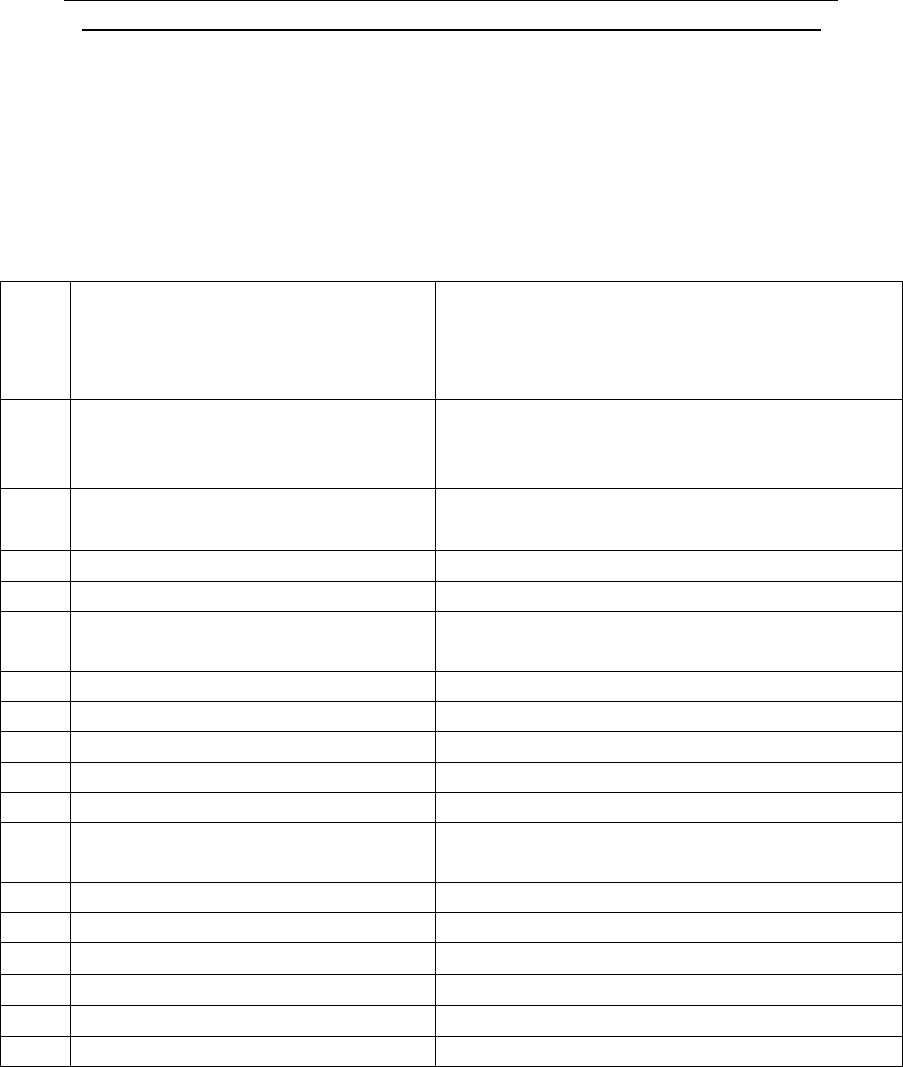
17. Mr. Sumeet Bhandawat (Complainant) has filed a complaint against Manipal Cigna
Health INS Co Ltd (Respondent) alleging rejection of his claim.
18. Brief facts of the Case-
1.
Name & Address of the
Complainant
Mr. Sumeet Bhandawat
H.No-217,W.NO-08, Pachore Road
Shujalpur City Shajapur
Madhya Pradesh 465 333
2.
Policy No:
Type of Policy
Duration of policy/Policy period
PROHLR410021080
Manipal Cigna Pro Health Ins. Policy
20.02.2020 to 19.02.2021
3.
Name of the insured
Name of the policyholder
Mr. Sumeet Bhandawat
As above
4.
Name of the insurer
Manipal Cigna Health Ins Co Ltd
5.
Date of Repudiation/ Rejection
22.01.2021
6.
Reason for Repudiation/
Rejection
Fraudulent Claim
7.
Date of receipt of the Complaint
07.04.2021
8.
Nature of complaint
Non Settlement of Claim
9.
Amount of Claim
Rs.2, 37,690/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.2,37,690/-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule
2017
13.
Date of hearing/place
On 17.09.2021 at OIO, LUCKNOW
14.
Representation at the hearing
• For the Complainant
Mr Sumeet Bhandawat
• For the insurer
Mrs Swetha Nair
15.
Complaint how disposed
Award
16.
Date of Award/Order
17.09.2021

a) Contention of the complainant- The complainant has stated that he has purchased
a Health policy from respondent and have been paying its premium regularly. On
29.10.2020 he was diagnosed covid positive and admitted in the city hospital Shujalpur
M.P. As his condition got deteriorated and as per city scan report his lungs were infected
to the extent 40 to 50 %, he was referred to Sai Hospital Indore and hospitalized from
03.11.2020 to 13.11.2020. On discharge he has incurred the expenses of Rs.2,37,690/-.
The treatment bills was submitted to the respondent. But respondent has rejected the
claim on baseless ground of unjust and highly unfair and stating that claim documents
were found to be manipulated during verification and claim stands repudiated under
clause VIII.19 “ Fraudulent Claim of the policy”.
B) Contention of the respondent - The respondent in their SCN have stated that the
Complainant submitted proposal form on dated 20
th
February, 2017 for purchasing
health insurance policy for his family. Respondent has issued Policy vide
No.PROHLR410021080 w.e.f 20.02.2017 to 19.02.2018 and in continuation till
19.03.2021 to 18.03.2022 for the S.I Rs.4.50 lakhs. The Complainant on 27
th
November,
2020 registered a reimbursement claim for his alleged hospitalization in Sai Hospital,
Indore due to covid-19 infection from 3
rd
November, 2020 to 13
th
November, 2020 for
reimbursement of Rs.2,37,690/- incurred during hospitalization. On scrutiny of the
documents it has been observed that there were multiple discrepancies owing to which
thE claim was found to be not genuine i.e (1) As per initial assessment sheet patient was
admitted with complaints of fever. Vitals show patient to be a febrile (Not having fever).
Billing has been done for O-2 given at 6 times. On admission patient had 92% on RA,
post that stats have been above 95% consistently, yet O-2 has been given. This suggests
bill inflation. (2) Vitals are normal throughout the admission. This shows that
hospitalization was not required. (3) As per hospital documents Pt. age is 43 yrs. but as
per HRCT chest reports & amount paid receipts on 02.11.2020 which is issued from
Sodani diagnostic center, he is 35 years old. (4) For the HRCT there is no referral slip. The
patient has also stated that he has not sought any consultation before admission. (5)
Patient had already tested positive for covid before admission, yet non related tests like
dengue have been advised suggesting inflation of bill. No pre -admission RT-PCR
submitted by the patient. (6) The pharmacy bills are all in series at different time stamps.
The bills have been prepared manipulating the dates. (7) As per assessment sheets the
complaints have been persisting 5-6 days before admission but no pre hospitalization
consultation has been done. (8) Tariff from the hospital shows that the charges for single
private room are Rs.2500/- per day and Rs.3500/- per day for deluxe rooms. However,
billing has been done for Rs.4000/- per day. Room rent should include nursing charges,
the same has been billed separately. (9) Lab registers show only entry for CRP test, no
other test mentioned although receipt and test reports published for other tests as
well. (10) On the blood investigation reports of Agnihotri Path Lab, pathologist name is
Dr.Romsha Sir Kanungo but as per MCI website Dr.Romsha Sirkanungo is not registered
as a pathologist, It’s only plain MBBS. During investigation copy of pathologist
registration was not provided by pathology lab. Therefore, after careful evaluation of
the documents, the respondent rejected the claim under Clause VIII.19 for the multiple
discrepancies observed in the documents through rejection letter dated 22
nd
January,
2021.
19. Complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
20. I have heard both parties at length and perused paper filed on behalf of the complainant
as well as the Insurance Company.
21. Admittedly complainant is the policy holder of the respondent who submitted his for
Covid-19 with the respondent which was repudiated vide letter dated 22.01.2021 on
the following ground :
“On scrutiny of the documents it has been observed that we have received claim
documents claimant Mr. Sumeet Bhandawat admitted at Sai Hosital from 03.11.2020 to
13.11.2020 with complaints of Covid-19 positive. Claimant is covered under Manipal
Cigna Health Insurance Pro Health Insurance Pro Health Group Insurance policy since
20.02.2017. On verification of the case and the hospitalization documents, multiple
discrepancies are noted. The claim documents found to be manipulated during
verification. Hence the claim stands repudiated under Clause VIII.19.We also reserve the
right to repudiate the claim under any other ground/s available to be subsequently.”
At the very outset, it would be relevant to mention that the claim was repudiated on
ground the of multiple discrepancies in the bills and records but nowhere is mentioned

that what were the discrepancies? Even no opportunity of hearing was given to the
insured to explain the same. Without giving any opportunity of hearing, respondents
have repudiated the claim unilaterally which is not permissible under the law.
Respondents should have given an opportunity of hearing to the complainant before
repudiating the claim. Accordingly, complaint is allowed with direction to the
respondents to afford an opportunity of hearing to the insured treat the claim as a fresh
and convey their decision through a reasoned speaking order.
Order :
Complaint is allowed. Respondents are directed to give an opportunity of hearing to
the complainant/insured and decide the claim as a fresh with reasoned speaking order
within a period of 45 days.
22. Let copies of the order be given to both the parties.
Date: 17.09.2021 Justice (Retd.) Anil Kumar
Srivastava
Place: Lucknow (Insurance Ombudsman)
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, STATE OF M.P. & C.G.
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
OMBUDSMAN – JUSTICE ( RETD.) ANIL KUMAR SRIVASTAVA
Mr Sumeet Bhandawat ..…………………..…………………..……………………………………Complainant
V/S
Manipal Cigna Health Ins Co Ltd………………..……..………..…………………………………Respondent
COMPLAINT NO: BHP-H-053-2122-0019
Heard the complainant as well as representative of the respondent.
During the course of hearing, respondent’s representative pointed the discrepancies
in tbe bills of purchase of medicines. She also pointed out that pathological reports
are not annexed, only bills are annexed. Even reports are not verified by the
concerned treating doctor.
In such circumstances, complainant is required to get the bills and reports verified
from the treating doctor and also to explain as to how there is discrepancy in the serial
number of the bills of purchase of medicines.
List on 6th September 2021.
Date: 06.08.2021 Justice (Retd.) Anil Kumar Srivastava
Place: Lucknow (Insurance Ombudsman)
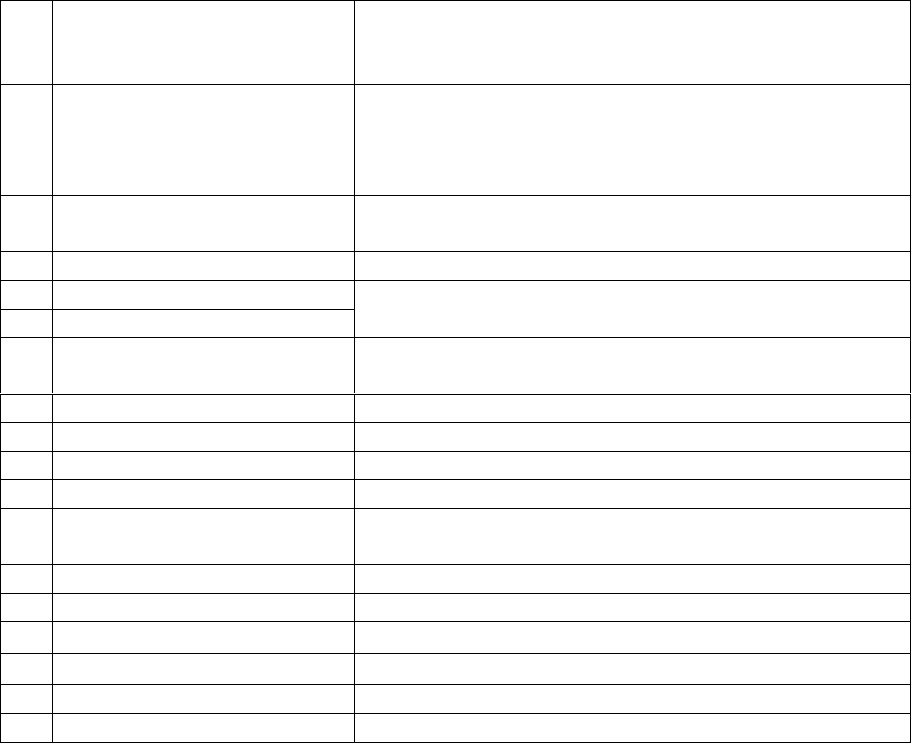
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Jeetendra Kumar Behera Vrs. Future Generali India Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-016-2122-0044
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Jeetendra Kumar Behera,
Near Debalok Lodge,
Madhupatna, Cuttack-753010. Mob-6371993696
2
Policy No:
Type of Policy
Duration of policy/Policy
period
CRP-94-20-7000714-00-000. Corona Rakshak Policy
15/07/2020 to 25/04/2021
Date of admission 07/11/2020 D.O.D 17/11/2020
3.
Name of the insured
Name of the policyholder
Mr. Jeetendra Kumar Behera
Mr. Jeetendra Kumar Behera
4.
Name of the insurer
Future Generali India Insurance Co. Ltd
5.
Date of Repudiation
09/03/2021
Non-disclosure of pre-existing disease.
6.
Reason for repudiation
7.
Dt of receipt of the
Complaint
05/05/2021
8.
Nature of complaint
Requested to advice the Insurer to settle the claim
9.
Amount of Claim
Rs.2,50,000/-
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs. 2,50,000/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
09.09.2021, Bhubaneswar
14.
Representation at the hearing
• For the Complainant
Self through VC
• For the insurer
Dr Akanksha Saxena, Executive through VC
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
09.09.2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Jeetendra Kumar
Behera was covered under policy No. CRP-94-20-7000714-00-000 for the period from
15/07/2020 to 25/04/2021 having sum insured of Rs.2,50,000/-. Being detected Covid positive,
he was admitted in Sadguru Hospital, Jagatpur, on 07/11/2020 and discharged on 17/11/2020.
Then he lodged a claim for settlement, which was repudiated by the Insurer on the ground non-
disclosure of material fact.
b. The insurer in their self-contained note confirmed issuance of the above policy and stated
that the complainant had undergone hospitalisation at Sadguru Hospital for Covid-19, is a
known case of “Type -2 Diabetes Mellitus & Hypertension and the random blood sugar on the
day of admission was 537.0mg/dl.
Complainant’s HBA1C level on 09-Nov-2020 was 9.8. HBA1C is measured primarily to
determine the three-month average bold sugar level which is quite evident that insured is
having this illness prior to policy inception. The complainant also suffering from Hypertension.
They had called for case papers along with other details to find out the duration of Diabetes
and Hypertension, which the complainant is yet not provided which resulted in repudiation of
the claim. The complainant is a known case of Type-2 Diabetes and Hypertension which was
not disclosed in proposal form. The insurer has been misled to issue the policy by suppression
of material facts which are necessary to disclose at the time of taking an insurance policy,
thereby depriving the Insurer of a fair chance to rightly assess the proposal form submitted and
rendering contract void-ab-inito. Therefore, the action under the claim by the insurer is just and
fair and there is no discrepancy at insurer’s end, hence complaint should be dismissed on the
merits.
18. a. Complainant’s Argument; -He has submitted all the required documents, but the insurer
repudiated his claim which is not justified.
b. Insurer’s Argument: The complainant did not disclose the pre-existing disease so they
repudiated the claim.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of medical report
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard both
the parties. The insurer stated that the claim is not payable since the insured was a known a
case of type II diabetes and had not declared the same in the proposal form. The insured
informed that Covid has nothing to do with Diabetes and it is a fixed benefit policy.
22. The attention of the complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rule,2017:
a. According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall
comply with the award within 30 days of the receipt of the award and shall intimate
the compliance of the same to the Ombudsman.
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, it is observed that the complainant was
tested Covid positive and was hospitalised with active line of treatment for more than
72 hours, which are basic requirements for benefits under the policy. It is also
observed that the insurer declined the claim for non-submission of documents, but in
SCN explained about non-disclosure of pre-existing disease. The Forum finds the
treatment falls within the scope of the policy and therefore, the claim is payable.
Accordingly, the insurer is advised to pay the complainant Rs.2,50,000/- (Rs. Two lakh
fifty thousand only) towards full and final settlement of the claim.
The complaint stands allowed.
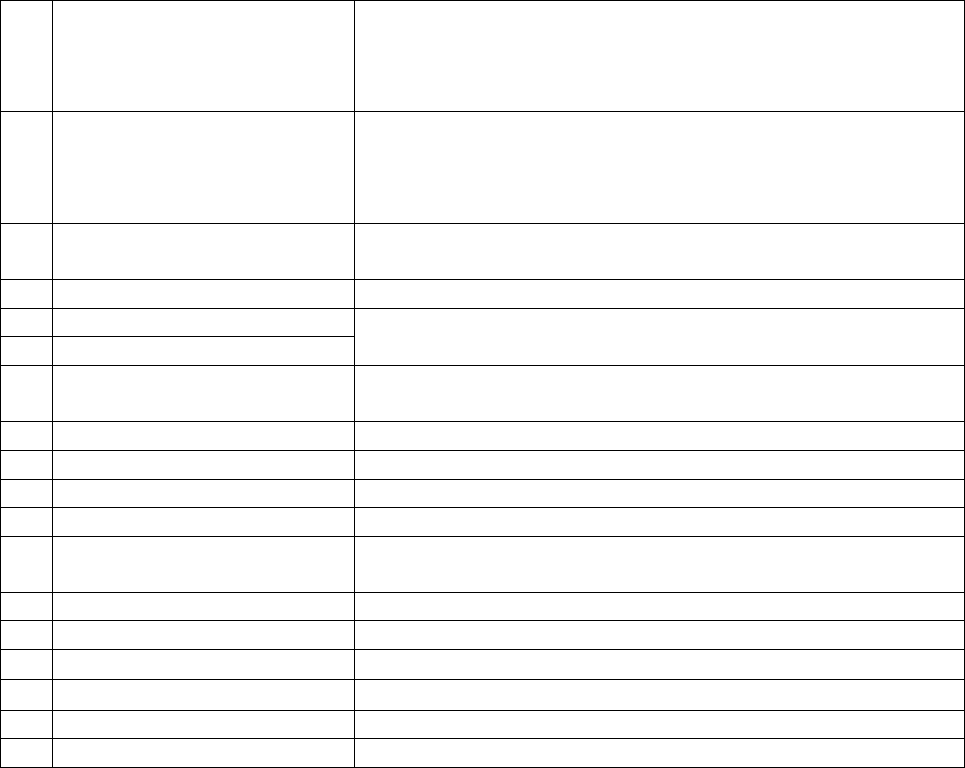
b. As per Rule 17(8) of the said rules, the award of Insurance Ombudsman shall be
binding on the Insurers.
Dated at Bhubaneswar on the 09
th
day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Kali Prasad Jena Vrs. Future Generali India Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-016-2122-0043
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Kali Prasad Jena
Ananta Pur, Bhairpur,
Dist: Cuttack-754200
Mob-9338412999
2
Policy No:
Type of Policy
Duration of policy/Policy
period
CRP-94-20-7506512-00-000
Corona Rakshak Policy
22/07/2020 to 02/05/2021
Date of admission 05/09/2020 D.O.D 11/09/2020
3.
Name of the insured
Name of the policyholder
Mr. Kali Prasad Jena
Mr. Kali Prasad Jena
4.
Name of the insurer
Future Generali India Insurance Co. Ltd
5.
Date of Repudiation
01/02/2021
Non-receipt of required documents.
6.
Reason for repudiation
7.
Date of receipt of the
Complaint
10/05/2021
8.
Nature of complaint
Requested to advice the Insurer to settle the claim
9.
Amount of Claim
Rs.2,50,000/-
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs. 2,50,000/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
09.09.2021, Bhubaneswar
14.
Representation at the hearing
a) For the Complainant
Self through VC
b) For the insurer
Dr. Akanksha Saxena, Executive through VC
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
09.09.2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Kali Prasad Jena
was covered under policy No. CRP-94-20-7506512-00-000 for the period from 22/07/2020 to
02/05/2021 having sum insured of Rs.2,50,000/-. Being detected Covid positive (Antigen Test)
he was admitted in Covid Care Centre, Dreams, Tangi, on 05/09/2020 and discharged on
11/09/2020. Then he lodged a claim for settlement, which was repudiated by the Insurer on the
ground there was no active line of treatment, insured was admitted for
isolation/evaluation/investigation purpose. Being aggrieved with the repudiation, the
complainant made an appeal before this forum for redressal.
b. The insurer in their self-contained note confirmed issuance of the above policy and stated
that the complainant had undergone hospitalization at Covid Care Centre, for “Covid Positive
Pneumonitis. As per discharge summary there were no clinical features (symptoms or signs)
that necessitated hospitalization. Temperature @96.8 F, SPO2@99%.
The policy is designed and developed by IRDAI and IRDAI clearly stated that admission has
to be as per guidelines issued by MOFHW.
OPERATIVE CLAUSE
If during the policy period the insured Person is diagnosed with COVID and hospitalised for
more than seventy-two hours following Medical Advice of a duly qualified Medical
Practitioner as per the norms specified by Ministry of Health and Family Welfare, Government
of India, the Company shall pay the agreed sum insured towards the Coverage mentioned in
the policy schedule
Provided further that, any amount payable under the policy shall be subject to terms of coverage
exclusions, conditions and definitions contained herein. Maximum liability of the Company
under all such claims during the policy period shall be the Sum Insured opted and specified in
the schedule.
The Circular dated 17th March 2020 issued by MOFHW: Guidelines on Clinical Management
of COVID – 19 Government of India Ministry of Health & Family Welfare Directorate
General of Health Services (EMR Division) defines Guidelines on Clinical Management of
COVID – 19.
COVID–19 may present with mild, moderate, or severe illness; the latter includes severe
pneumonia, ARDS, sepsis and septic shock. Early recognition of suspected patients allows for
timely initiation of IPC (see Table 2). Early identification of those with severe manifestations
(see Table 2) allows for immediate optimized supportive care treatments and safe, rapid
admission (or referral) to intensive care unit according to national protocols. For those with
mild illness, hospitalization may not be required unless there is concern for rapid deterioration.
All patients discharged for home should be instructed to return to hospital if they develop any
worsening of illness.
Uncomplicated illness
Patients with uncomplicated upper respiratory tract viral infection, may have non-specific
symptoms such as fever, cough, sore throat, nasal congestion, malaise, headache. The elderly
and immunosuppressed may present with atypical symptoms.
Mild pneumonia
Patient with pneumonia and no signs of severe pneumonia. Child with non-severe pneumonia
has cough or difficulty in breathing/ fast breathing: (fast breathing - in breaths/min): <2 months,
≥60; 2–11 months, ≥50; 1– 5 years, ≥40 and no signs of severe pneumonia
Severe pneumonia
Adolescent or adult: fever or suspected respiratory infection, plus one of the following;
respiratory rate >30 breaths/min, severe respiratory distress, SpO2 <90% on room air Child
with cough or difficulty in breathing, plus at least one of the following: central cyanosis or
SpO2 <90%; severe respiratory distress (e.g. grunting, chest in- drawing); signs of pneumonia
with any of the following danger signs: inability to breastfeed or drink, lethargy or
unconsciousness, or convulsions. Other signs of pneumonia may be present: chest indrawing,
fast breathing (in breaths/min): <2 months ≥60; 2–11 months ≥50; 1–5 years ≥40. The diagnosis
is clinical; chest imaging can exclude complications.
That indeed the guidelines issued by Government of Odisha further clearly states that for mild
/ uncomplicated illness hospitalization is not required. Reference no.8789 / 23-Mar-
20/HFW/SCW/I/EMER/0001/2020. That basically insured was admitted for isolation /
evaluation/ investigation purpose and there was no active line of treatment, so the claim was
repudiated. Below is the supporting policy condition. Clause 6.1. Investigation &
Evaluation (Code- Excl 04)
i. Expenses related to any admission primarily for diagnostics and evaluation purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current diagnosis
and treatment
They also cited and annexed the following recent Insurance Ombudsman Orders on Corona
Rakshak Claim in support of their repudiation
a. Order of Hon’ble Ombudsman (Maharashtra) with respect to Asymptomatic Corona Rakshak
claim in the matter of Star Health & Allied Insurance Company Vs Dr. Mahesh Shinde b. Order
of Hon’ble Ombudsman (Rajasthan) with respect to Asymptomatic corona Rakshak claims in
the matter of Future Generali India Insurance Company Ltd. Vs Sh. Shyam Lal Sharma c. Order
of Hon’ble Ombudsman (Kerala) with respect to Asymptomatic corona Rakshak claims in the
matter of Future Generali India Insurance Company Ltd. Vs Mr.Jaison Jacob
18. a. Complainant’s Argument; -He Stayed 7 days in covid care centre and received active
treatment from the doctors, still the insurer repudiated his claim which is not justified.
b. Insurer’s Argument: The action under the claim by insurer is just and fair and there is no
discrepancy at insurer’s end hence the complaint should be dismissed on the merits.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses and cited Insurance Ombudsman orders.
b. Photo copy of medical report
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard both
the parties. The insured stated that he was admitted in the Covid Care Centre for Covid
treatment. But he does not know what medicines were given. The insurer stated that there
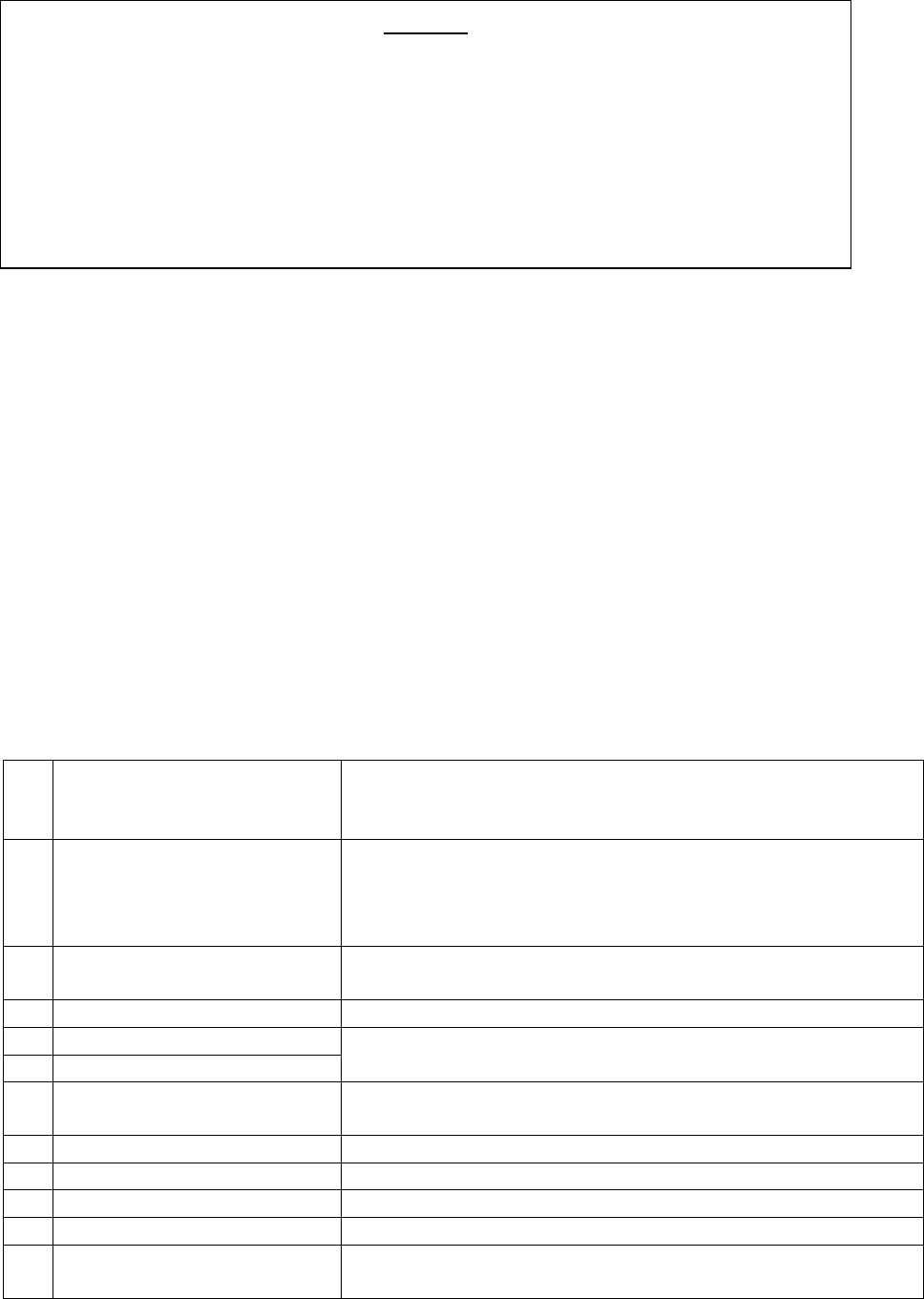
was no active line of treatment and he was kept in isolation, therefore, the claim is not payable.
Dated at Bhubaneswar on the 09th day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF PUSPANJALI PANDA Vrs. TTA AIG GENERAL INSURANCE CO. LTD.
COMPLAINT REF: NO: BHU-G—047-2122-0069
AWARD NO: IO/BHU/A/GI/ /2021-22
1.
Name & Address of the
Complainant
Puspanjali Panda
C/o Late Ashok Mishra, Kazidiha, Madhupatna,
Cuttack, Odisha. Pin-753010. Cell no.-8280500514
2.
Policy No:
Type of Policy
Duration of policy/Policy
period
02352078670100,
Home Guard Plus
3 years-30/09/2019 to 29/09/2022
Date of Death-14/10/2020
3.
Name of the insured
Name of the policyholder
Mr Ashok Mishra
Mr Ashok Mishra
4.
Name of the insurer
Tata AIG General Insurance Company Limited
5.
Date of Repudiation
23/01/2021
Not covered within scope of policy condition
6.
Reason for repudiation
7.
Dt. of receipt of the
Complaint
09/03/2021
8.
Nature of complaint
Non settlement of claim
9.
Amount of Claim
Rs.15,00,000/-
10.
Date of Partial Settlement
Claim repudiated
11.
Amount of relief sought
Rs.15,00,000/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, it is observed that the complainant has
not submitted any document about the type of treatment. Even the Discharge
summary does not contain the details of treatment. In absence of treatment details,
the complainant is not entitled for benefits under the policy.
Accordingly, the complaint stands dismissed.
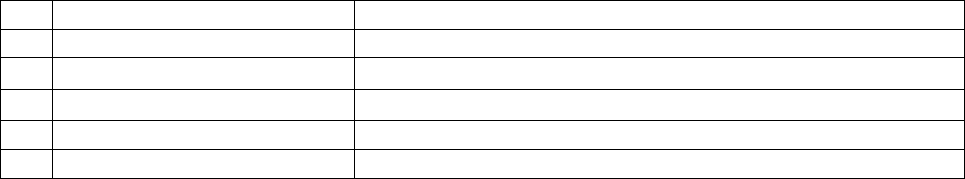
13.
Date of hearing/place
13/09/2021, Bhubaneswar
14.
Representation at the hearing
• For the Complainant
Self through Phone
• For the insurer
Dr. Vishal Sawant through VC
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
13/09/2021
17. a. Brief Facts of the Case/ Cause of Complaint: - The insured had taken a Home Guard
Plus Policy no. 02352078670100 from Tata AIG General Insurance Company Limited for the
period 30/09/2019 to 29/09/2022 for a sum insured of Rs.15,00,000/-. The Insured was referred
by CMC and was admitted at Sun Hospital Privated Limitd, Tulsipur, Cuttack on 03/10/2020
with complainants of breathlessness, loss of appetite, fever, generalised weakness. He was
diagnosed as Covid Pneumonia with Hypertension and expired on 14/10/2020. After his death
his wife cum complainant had lodged claim with Insurer for getting entire sum insured of
Rs.15,00,000/-. The claim was repudiated by the Insurer on the ground that coverage was for
critical illness and the medical condition with which Insured was suffering was not one of them.
Being aggrieved with repudiation complainant has approached this forum for redressal of her
grievance.
b. The insurer, in its self-contained note, has admitted insurance of Insured’s life for a sum
insured of Rs.15,00,000/- under home guard plus policy against critical illness and accidental
death. Critical illness covers Nine diseases such as: - 1-Cancer of specified severity, 2-Kidney
failure requiring regular dialysis, 3-Multiple sclerosis with persisting symptoms, 4-Major
organ/bone marrow transplant, 5-Open heart replacement or repair of heart valves, 6-Open
Chest CABG, 7-Stroke resulting in permanent symptoms, 8-Permanent paralysis of limbs, 9-
Fist heart attack – of specified severity and Accidental death. The insured had complaints of
breathlessness, loss of appetite, fever and generalized weakness and died due to COVIDF
Pneumonia with Hypertension and died while undergoing treatment on 14/10/2021 at Sun
Hospital Pvt Ltd., Cuttack. As same was neither due to sickness of specified disease of critical
illness nor accidental death, they are not liable to admit the claim as per coverage of the policy.
18. a. Complainant’s Argument: - As her husband had taken a Home Guard Plus policy from
insurer, she is entitled to get the claim. She further claimed that as her husband was only earning
member, she is entitled for full sum insured to clear the housing loan availed by her late
husband.
• Insurer’s Argument: - They had rightly repudiated the claim as policy covers death due
to nine types critical illness and accidental death. The insured had died due to COVID
pneumonia with hypertension and same does not fall under the coverage of policy.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017.
20. The following documents are placed in the file.
a. Photocopies of Policy, & policy wordings
b. Photocopies of all hospital records and bills
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents relating the complaint and heard both the parties.
The complainant stated that her husband was under Covid treatment and died due to heart
attack during treatment. The insurer informed that there is no single document suggesting
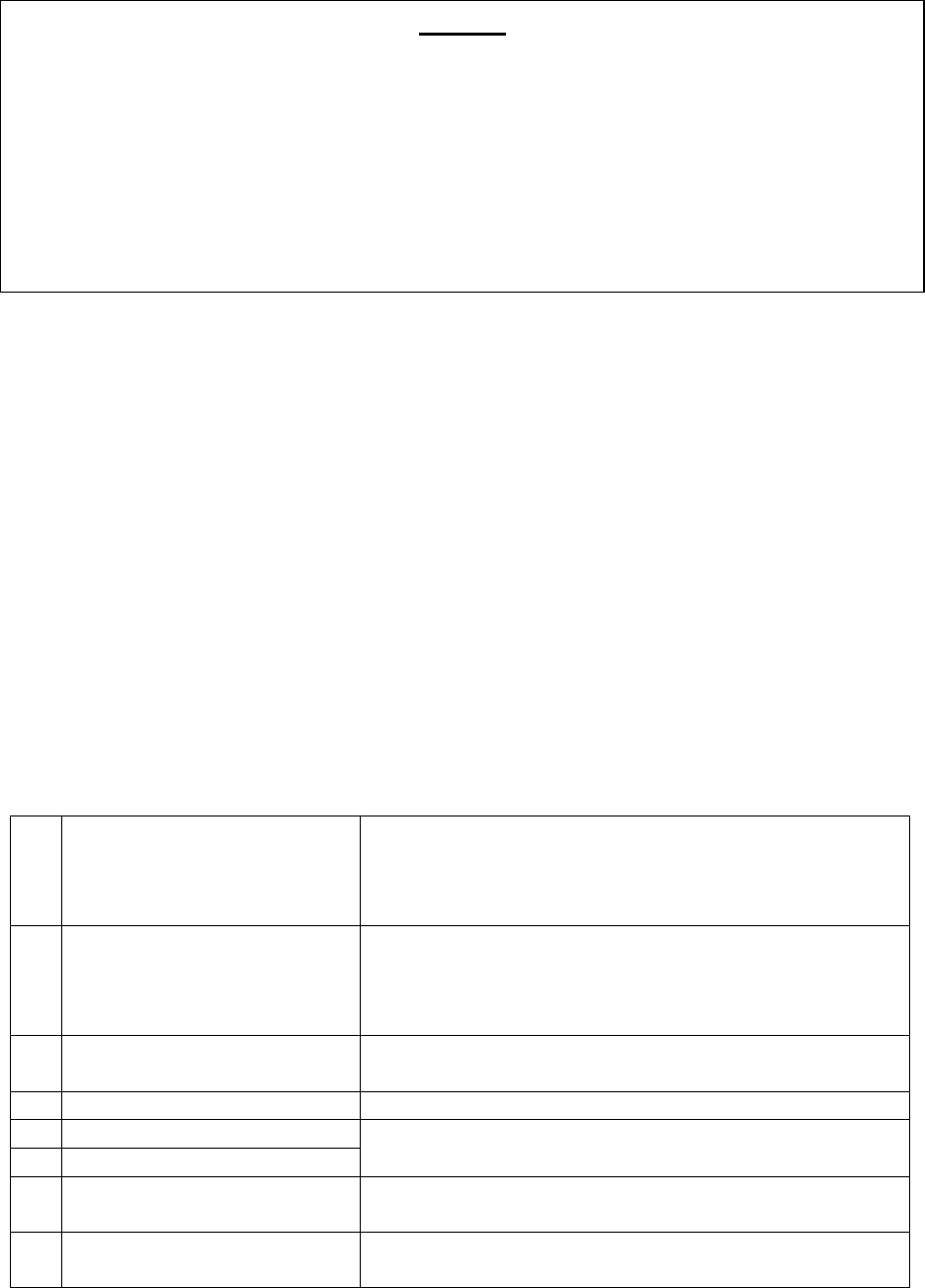
death due to Heart attack. The insurer informed that the patient was under treatment for
Covid and died out of Covid as per all medical reports and the same is not covered under the
policy.
Dated at Bhubaneswar on the 13
th
day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Mahammed Shah Riaz Vrs. Max Bupa Health Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-031-2122-0094
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Mahammed Shah Riaz,
Shah Manzil C/o Hotel Rajdhani,
Chintamaniswar, Cuttack Road, Bhubaneswar-751006
Mob-9437012731
2
Policy No:
Type of Policy
Duration of policy/Policy
period
31694066202100. Health Insurance
30/04/2021 to 29/04/2022
Date of admission Not applicable.
3.
Name of the insured
Name of the policyholder
Mr. Mahammed Shah Riaz
Mr. Mahammed Shah Riaz
4.
Name of the insurer
Max Bupa Health Insurance Co. Ltd
5.
Date of Repudiation
Not applicable. Cancellation of policy on 05/07/2021
Non-disclosure of pre-existing disease.)
6.
Reason for repudiation
7.
Dt of receipt of the
Complaint
02/08/2021
8.
Nature of complaint
Requested to advice the Insurer to re-issue the policy
with all benefits and continuity
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, the Forum examined the policy coverage
and the cause of death and found that the patient died out of Covid 19. The complainant
in her applications to this office has also mentioned the death in Covid. The policy does
not cover benefits for Covid 19 treatment or death due to Covid. Therefore, the
complainant is not entitled for the claimed benefits under the policy.
Accordingly, the complaint stands dismissed.
9.
Amount of Claim
Not applicable
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Not applicable
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
17/09/2021, Bhubaneswar
14.
Representation at the hearing
a) For the Complainant
Self through VC
b) For the insurer
Mr. Bhuvan Bhaskar, Executive through VC
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
17/09/2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Mahammed
Shah Riaz and his spouse are covered under Oriental Insurance Mediclaim policy vide No.
345300/48/2009/481 w.e.f 30/04/2008 to 29/04/2009 and the said policy has been renewed
continuously till 29/04/2021 (for 13 years). In view of upgrading his policy he ported the policy
to Max Bupa Health Insurance Co ltd and paid premium of Rs.34,102/-. Accordingly, Policy
bearing No.31694066202100 was issued effecting from 30/04/2021 to 29/04/2022 having sum
insured of Rs.5,00,000/-. After two days of receiving the policy, the complainant informed the
insurer vide his mail dated 03/05/2021 regarding his medication for diabetes and hypertension
for about one year and requested to make necessary changes in the policy. But the insurer
instead of endorsing the policy, they cancelled it and refunded an amount of Rs.25,576/- to the
complainant. Being aggrieved, the complainant made an appeal before this forum for redressal.
b. The insurer in their self-contained note stated that Mr. Mohammed Shah Riaz shared
information through telephonic conversation with their Health Insurance counsellor- Telesales
for the issuance of a Health Insurance Policy to insure himself and his wife. The complainant
specifically proposed through telephonic conversation to pay an annual premium. The details
of the policy were also explained to him by the insurance agent/sales representative. It is
pertinent to mention herein that the complainant had full knowledge of the terms and conditions
of the policy. The policy was ported from his prior insurance policy with Oriental insurance to
Max Bupa Health Insurance in the month of April,2021.
On the basis of declaration made by the complainant vide his mail dated 18/04/2021, the insurer
has issued a policy bearing No. 31694066202100 commencing from 30/04/2021 to 29/04/2022
in the name of the complainant and his spouse for a sum insured of Rs.5,00,000/-. The company
has sent welcome letter to the complainant which contained customer information sheet,
Insurance certificate, premium receipt, terms and conditions of the policy, product benefit table,
health check-ups along with relevant annexures. The receipt of the aforesaid documents is not
disputed by the complainant which implies that the complainant was in actual knowledge of
the governing terms and conditions of the insurance policy and the same cannot be now refused
at such a later stage.
The policy terms and conditions comprised Free Look Period whereby policy holder if is
dissatisfied with the terms and conditions of the policy, then he/she had the option of cancelling
the policy within 15 days of receipt of the policy. It was only in the month of May,03,2021 that
the complainant sent an e mail stating that “had inadvertently failed to mention that I have been
taking medication for Hypertension and Diabetes for about a year”
Every interested insured person has to make full and frank disclosure of history of illness
suffered by him and by those proposed to be insured in the proposal stage, even during porting

of a policy, as per IRDAI (Health Insurance) Regulation,2016. It is clarified that porting does
not absolve or allow the porting insured from disclosing true and complete facts about his/her
health conditions. Also, the applicable Regulations while granting the right to porting to the
insurers does not take away the right to underwriter the risk from the insurance company.
Clause 12 of the IRDAI (Health Insurance) Regulation,2016 grants unconditional right to
insurance company to fully underwrite the risk and accept/reject accordingly. It is stated that
the post issuance disclosure made by the Complainant regarding HTN and DM, clearly
indicates that the time of porting, the insurance company was not allowed to underwrite the
policy in a just and fair manner. Accordingly, the policy was cancelled by the company.
18 a. Complainants Argument: - He had a continuous health insurance policy for 13 years
without any claim. Now at this state, at the age of 62, rejecting the policy would mean losing
his waiting period too which will highly unjust and unfair to him
b. Insurer’s Argument: - The post issuance disclosure made by the Complainant regarding
HTN and DM, clearly indicates that, the time of porting, the insurance company was not
allowed to underwrite the policy in a just and fair manner. Accordingly, the policy was
cancelled by the company.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of Oriental policy issuance details
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard both
the parties. It is observed that the complainant has been renewing his policy since 2008 with
the Oriental Insurance Co Ltd. In 2021-22 renewal time, he ported the policy to Max-Bupa
Health Insurance Co ltd and admitted that he, due to wrong understanding, did not mention
about his medication for HTN and Diabetes. Therefore, immediately on receipt of the policy
document, he informed the insurer to incorporate these two illnesses as pre-existing. But the
insurer cancelled the policy and refunded the premium. The insurer stated that the
complainant did not disclose his pre-existing conditions at the time of taking the policy, but
informed only after the policy was underwritten. Since this is a case of non-disclosure of facts,
they cancelled the policy and refunded premium as per policy terms and conditions.
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, the forum finds the complainant to be a
senior citizen, who had continuously renewed his policy, without any claim so far, with
another insurer before porting the present insurer. The complainant, during hearing,
admitted that it was his mistake as he thought it was not required to declare pre-existing
medication since he has been renewing the policy for last 13 years and the four-years-
restriction period has already passed for pre-existing disease. Considering the age of
the complainant, the difficulties of not getting any renewal hereafter and possibility of
not getting continuity of renewal benefits, since it is a case of porting, the insurer is
directed to restore the policy from the date of cancellation without any gap, without
changing the terms conditions except endorsing the pre-existing conditions as declared
by the complainant, on collection of refunded premium (without charging any
additional premium). The complainant is advised to pay the insurer the refund amount
early for restoring the policy by the insurer.
Accordingly, the complaint is allowed.
22. The attention of the complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rule,2017:
a. According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall
comply with the award within 30 days of the receipt of the award and shall intimate
the compliance of the same to the Ombudsman.
b. As per Rule 17(8) of the said rules, the award of Insurance Ombudsman shall be
binding on the Insurers.
Dated at Bhubaneswar on the 17th day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Madan Mohan Samantray Vrs. The Oriental Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-050-2122-0080
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Madan Mohan Samantray
Plot No. 25 (A), Patrapada,
PO; Patrapada, Bhubaneswar-751019
Mob-9437696132
2
Policy No:
Type of Policy
Duration of policy/Policy
period
345300/48/2020/2401
OBC-Oriental Mediclaim Policy.
10/03/2020 to 09/03/2021 (inception 10/03/2014)
Date of admission 29/05/2020 D.O.D 29/05/2020
3.
Name of the insured
Name of the policyholder
Mr. Madan Mohan Samantray
Mr. Madan Mohan Samantray
4.
Name of the insurer
The Oriental Insurance Co. Ltd
5.
Date of Repudiation
09/09/2020
There is no active line of treatment.
6.
Reason for repudiation
7.
Dt of receipt of the
Complaint
26/07/2021
8.
Nature of complaint
Requested to advice the Insurer to settle the claim
9.
Amount of Claim
Rs. 51,760/-
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs. 51,760/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
17/09/2021, Bhubaneswar
14.
Representation at the hearing
a) For the Complainant
Self through VC
b) For the insurer
Mr. Amaresh Rout, DM through VC
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
17/09/2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Madan Mohan
Samantray is covered under policy No. 345300/48/2020/2401 for the period from 10/03/2020
to 09/03/2021 having Sum Insured of Rs.5,00,000/-. He was admitted in AMRI Hospital on
29/05 2020 for FLEXIBLE CYSTOSCOPY and discharged on same day i.e. on 29/05/2020.
He lodged a claim for reimbursement of hospital expenses which was repudiated on the ground,
there was no active line of management and patient mainly underwent various investigations.
Being aggrieved with the repudiation, the complainant made an appeal before this forum for
redressal.
b. The insurer in their self-contained note confirmed issuance of the above policy and stated,
on scrutinizing the submitted claim documents, it has been observed, Mr. Madan Mohan
Samantray (67 years Male) was admitted in AMRI hospitals, Bhubaneswar for flexible
Cystoscopy and diagnosis BPH. As per General Exclusion Clause 4.9, expenses incurred at
Hospital or Nursing Home primarily for evaluation/diagnosis purposes which is not followed
by active treatment for ailment during hospitalisation period are excluded from payment of
claim.
Further, as per Clause 3.21 only an Insured person who admitted to Hospital and stays for at
least 24 hours for the sole purpose of receiving the treatment for suffered
ailment/illness/disease/injury/accident is liable for compensation. The complainant got
admitted and discharged from the hospital on the same day as per the In-patient Bill cum
Receipt.
18. a. Complainant’s Argument; - The reason for repudiation made by the Insurer is not
acceptable to him. The reason for various investigations cystoscopy was required for
hospitalisation as per advice of Dr. Manas Ranjan Pradhan.
b. Insurer’s Argument: There was no active line of management & patient mainly underwent
various investigations.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of medical report
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard both
the parties. The complainant stated that he has been renewing the policy since 2012. On this
claim, he wrote many times but the insurer did not respond to any of his letters. But he got a
letter dated 09.09.2020 repudiating his claim on invalid grounds. The insurer informed that
the complainant was admitted in the hospital mainly for investigation purposes and he was
not given any active line of treatment. The insurer further stated that the patient did not stay
for more than 24 hours in the hospital, therefore, the claim is not payable.
Dated at Bhubaneswar on the 17th day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Pradipta Kumar Das Vrs. National Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-048-2122-0081
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Pradipta Kumar Das,
Plot No. 103, Bhudheswari Colony,
Po; Bhudheswari, Bhubaneswar-751006. Mob-9853211334
2
Policy No:
Type of Policy
Duration of policy/Policy
period
16320048208560000028. National Mediclaim Policy
27/08/2020 to 26/08/2021
Date of admission 27/03/2021 D.O.D 27/03/2021
3.
Name of the insured
Name of the policyholder
Mrs. Asita Das
Mr. Pradipta Kumar Das
4.
Name of the insurer
National Insurance Co. Ltd
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, it is observed that the procedure was
carried out under local anaesthesia and the patient was hospitalised for lesser than 24
hours. The policy is examined and found that the procedure also does not fall under the
Day Care category. The Forum finds that the procedure does not fulfil the requirements
of either ‘Hospitalisation’ or ‘Day Care’ treatment under the policy for a claim.
Therefore, the claim is not payable under the policy.
Accordingly, the complaint stands dismissed.
5.
Date of Repudiation
01/06/2021
Cosmetic surgery not covered under the policy.
6.
Reason for repudiation
7.
Dt of receipt of the
Complaint
26/07/2021
8.
Nature of complaint
Requested to advice the Insurer to settle the claim
9.
Amount of Claim
Rs. 10952/-
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs. 10952/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
20/09/2021, Bhubaneswar
14.
Representation at the hearing
1. For the Complainant
Self through Phone
2. For the insurer
Dr. Amit Agarwal through VC
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
20/09/2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Pradipta Kumar
Das and his spouse Mrs. Anita Das are covered under policy No. 16320048208560000028 for
the period from 27/08/2020 to 26/08/2021 having sum Insured of Rs.200,000/-. His wife Mrs.
Anita Das was admitted in L V Prasad Eye Institute, Bhubaneswar on 27/03/2021 for surgery
of LEFT EYE XANTHELASMA and discharged on 27/03/2021. The complainant lodged a
claim for reimbursement of hospital expenses which was repudiated on the ground that
cosmetic surgery is not covered under the policy. Being aggrieved with the repudiation, the
complainant made an appeal before this forum for redressal.
b. The insurer in their self-contained note confirmed issuance of the above policy and stated
that the patient Mrs. Anita Das, wife of Mr. Pradipta Kumar Das, was admitted at L V Prasad
Eye Institute, Bhubaneswar on 27/03/2021 for the surgery of LEFT EYE XANTHELESMA.
The treating doctor furnished a report stating that the patient Anita Das having left eye
Xanthelasma, which is a COSMETIC BLEMISH, considered as Cosmetic Surgery. The patient
Mrs. Anita Das was diagnosed with Xanthelasma in the left Eye. Xanthelasma are yellowish
plaques that occur most commonly near the inner canthus of the eyelid, more often on upper
lid than lower lid (Source-Google). Xanthelasma was removed through Surgery which is
considered a Cosmetic Surgery. Besides the opinion by the Doctor of TPA, they had obtained
a second opinion from an independent Eye Surgeon Dr. Gautam Panda who corroborated that
it was a Cosmetic Surgery. Therefore, the claim has been rejected as per Clause 4.14 of the
policy. Wordings of Clause 4.14: The company shall not be liable to make any payment under
the policy in respect of any expenses incurred in connection with or in respect of following
disease/treatment for Cosmetic or aesthetic treatment of any description, change of life or sex
change operation, hormone replacement therapy. Expenses for plastic surgery other than as
may be necessitated due to illness/disease/injury.
18. a. Complainant’s Argument; - Without proper investigation/examination of medical report
they repudiated the claim which is not justified.
b. Insurer’s Argument: Xanthelasma was removed through Surgery which is considered a
Cosmetic Surgery, not covered under the policy.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses b. Photo copy of medical report
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents relating the complaint and heard both the parties.
The complainant stated that her wife (the patient) got infection in her left eye and got pain
with swelling. He said that his wife did not go for the purpose of cosmetic surgery. But as per
the doctor, cosmetic surgery was necessitated. The Insurer stated it was a case of cosmetic
surgery as per LV Prasad Eye institute certificate dated 21.04.2021 and therefore, the claim is
not payable.
22. The attention of the complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rule,2017:
a. According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall
comply with the award within 30 days of the receipt of the award and shall intimate
the compliance of the same to the Ombudsman. b. As per Rule 17(8) of the said rules,
the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Bhubaneswar on the 20th day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, the Forum has examined the certificates
dated 21.04.2021 and dated 03.06.2021 issued by the same treating hospital. It is found
that the surgery was planned as she had symptoms because of profusion. The excision
biopsy was done for Xanthelasma and epidermal inclusion cyst. From the nature of
illness and the surgery, it is clear that the cosmetic surgery was a necessity and
therefore, the claim is payable under the policy clause No-4.14. The insurer is directed
to pay the complainant Rs.9,641/- (Rs. Nine thousand six hundred and forty-one only,
as per bill copies submitted to this office) towards full and final settlement of the claim.
Accordingly, the complaint is allowed.
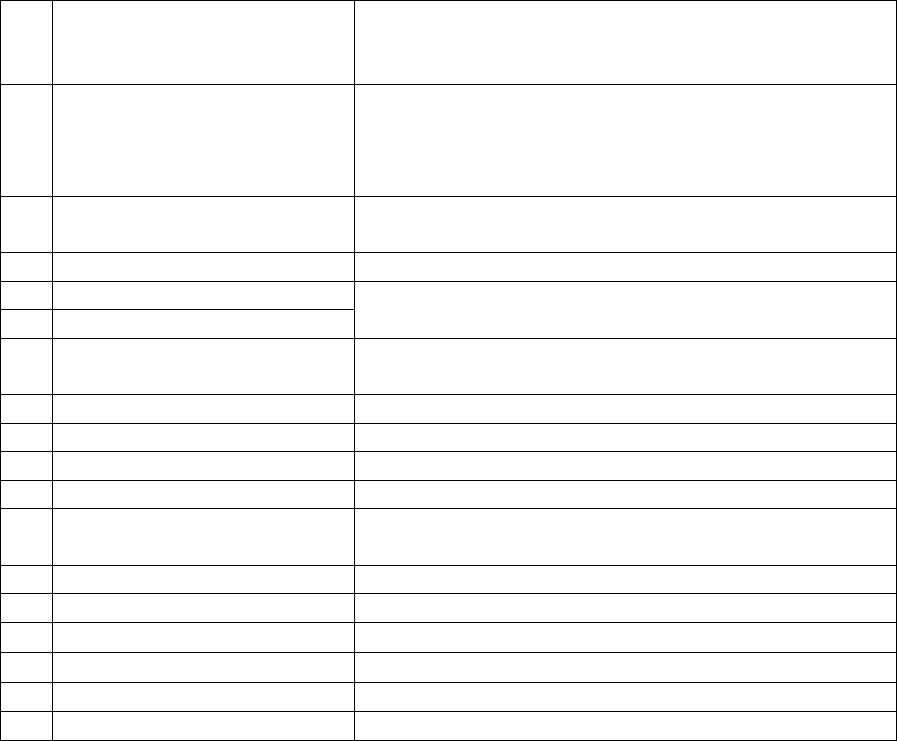
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Radheshyam Agrawal Vrs. Star Health and Allied Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-044-2122-0084
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Radheshyam Agrawal,
Plot No. 1061, Sai Tower, Flat No. C/1,
Nayapalli, Bhubaneswar-751012. Mob-9437019690
2
Policy No:
Type of Policy
Duration of policy/Policy
period
P/191211/01/2021/005366. Carona Kavach Policy
17/07/2020 to 28/04/2021
Date of admission 22/03/2021 D.O.D 28/03/2021
3.
Name of the insured
Name of the policyholder
Mr. Radheshyam Agrawal
Mr. Radheshyam Agrawal
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd
5.
Date of Repudiation
04/05/2021
Patient needs only self-isolation by home quarantine.
6.
Reason for repudiation
7.
Date of receipt of the
Complaint
27/07/2021
8.
Nature of complaint
Requested to advice the Insurer to settle the claim
9.
Amount of Claim
Rs. 78,752
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs. 78,752
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
20/09/2021, Bhubaneswar
14.
Representation at the hearing
➢ For the Complainant
Self through VC
➢ For the insurer
Mr. K B S Das through VC
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
20/09/2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Radheshyam
Agrawal is covered under policy No. P/191211/01/2021/005366 for the period from
17/07/2020 to 28/04/2021
Having Sum Insured of Rs. 5,00,000/-. Being detected covid positive he was admitted in Aditya
Ashwini Hospital, Bhubaneswar on 22/03/2021 and discharged on 28/03/2021. Then he lodged
a claim for reimbursement of hospital expenses which was repudiated by the insurer on the
ground, patient needs only self-isolation by home quarantine instead of hospitalisation. Being
aggrieved with the repudiation, the complainant made an appeal before this forum for redressal.
b. The insurer in their self-contained note confirmed issuance of the above policy and stated
that the complainant made a claim vide Claim No. CIR/2021/191211/2362456 and submitted
a Claim form dated 28/03/2021 lodging a claim for Rs. 78,824/- under the above CORONA
KAVACH POLICY. The complainant Mr. RADHESHYAM AGRAWAL, aged about 52 years
took treatment at ADITYA ASHWINI HOSPITALS, BHUBANESHWAR on 22/03/2021 and
was diagnosed with COVID-19, PNEUMONIA and HTN and was treated by Conservative
Management. The complainant submitted a claim for reimbursement of medical expenses on
30/04/2021 and the same was repudiated vide letter dated 04/05/2021 stating that the insured’s
clinical picture and vital charts indicate that the patient falls under Category A of AIIMS
Protocol. i.e. Mild infection. Therefore, the complainant could have been treated via self-
isolation by home quarantine. Hence, the hospitalization was not warranted. On receipt of the
Notice from Hon’ble Ombudsman, the claim was once again reviewed and considered for
settlement for Rs. 76,971/-. The working sheet is also attached to the SCN.
REASONS FOR DEDUCTIONS: As per Other Excluded Expenses of the policy, the charges
pertaining to BLOOD GROUPING is not payable. Hence, a sum of Rs. 129/- was deducted
from Investigation and Diagnostics. As per Other Excluded Expenses of the policy, the charges
pertaining to NURSING CAPS, GLOVES, HANDRUB, MASK and COTTON are not payable.
Hence, a sum of Rs. 1,674/- was deducted from Medicines within Hospital. As per Other
Excluded Expenses of the policy, the charges pertaining to REGISTRATION FEES is not
payable. Hence, a sum of Rs. 50/- was deducted from Professional Fees under Pre-
Hospitalization Expenses. (Total Claimed Amount Rs. 78,824 Less: Deductions Rs. 1,853/-
Balance Payable Rs. 76,971/-). Hence, the admissible amount is Rs. 76,971/-. Under the above
circumstances, they hereby offer to settle the claim for Rs. 76,971/- in full as per Policy
Conditions.
18. a. Complainant’s Argument; - The Insurance company repudiated the claim by finding
unwanted facts & faults.
b. Insurer’s Argument: He wanted full settlement of the claim for Rs.76,971/-
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of medical reports
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard both
the parties. The insurer stated that they have now agreed to settle the claim for Rs.76,971/-.
The complainant expressed unhappiness about the insurer’s services and requested for
settlement of full amount of Rs.78,752/-.
22. The attention of the complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rule,2017:
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, the Forum finds that the complainant
is eligible to get Rs.77,491/-. Therefore, the insurer is directed to pay the complainant
Rs. 77,491/- (Rs. Seventy-seven thousand four hundred ninety-one only) towards full
and final settlement of the claim.
Accordingly, the complaint is allowed.
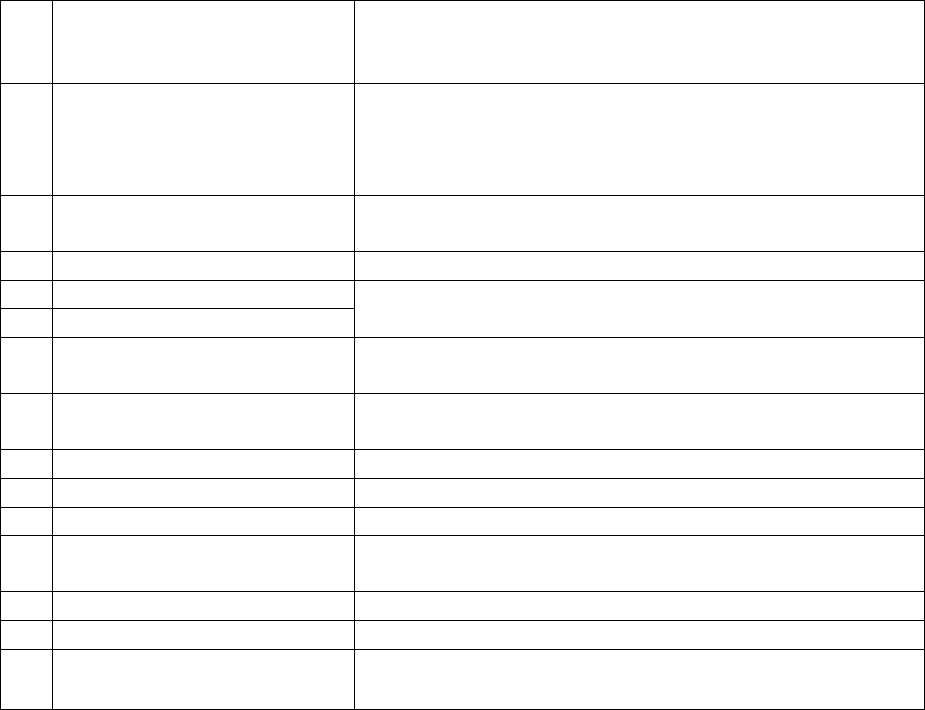
a. According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall comply with
the award within 30 days of the receipt of the award and shall intimate the compliance of the
same to the Ombudsman.
b. As per Rule 17(8) of the said rules, the award of Insurance Ombudsman shall be binding on
the Insurers.
Dated at Bhubaneswar on the 20th day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Rajesh Agrawal Vrs. HDFC Ergo Genera Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-018-2122-0092
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Rajesh Agrawal,
Shiv Kuti, Kacheri Road, Rourkela-769012
Dist: Sundargarh, Odisha. Mob-9437044283
2
Policy No:
Type of Policy
Duration of policy/Policy
period
2805203526018100000
Optima Restore Floater Insurance Policy
28/01/2021 to 27/01/2022 (sum Insured Rs.25,00,000/-)
Date of admission Not applicable
3.
Name of the insured
Name of the policyholder
Mr. Anil Agrawal
Mr. Anil Agrawal
4.
Name of the insurer
HDFC Ergo General Insurance Co ltd
5.
Date of Repudiation
29/03/2021 (Cancellation of policy)
Cancellation of policy due to cheque dishonoured
6.
Reason for repudiation
7.
Dt. of receipt of the
Complaint
30/07/2021
8.
Nature of complaint
Requested to advice the Insurer to renew the policy with
continuity benefit
9.
Amount of Claim
Not Applicable
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Not applicable
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
22/09/2021, Bhubaneswar
14.
Representation at the hearing
• For the Complain-
ant
Not required
• For the insurer
Not required
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
22/09/2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Rajesh Agrawal
and his family were covered under Policy No. 6000075246 of Apollo Munich Insurance Co.
Ltd which was valid till 27/01/2021. In the year 2020 Apollo Munich Health Insurance CO.
Ltd was taken over by HDFC Ergo General Insurance Co. Ltd. In the month of December,2020
the complainant received a renewal notice from HDFC Ergo General Insurance Co. Ltd
(without payment link) that the policy is due for renewal on 27/01/2021. He contacted the
customer care to provide payment link but no response was received. Then he approached local
Branch office of HDFC Ergo General Insurance Co. Ltd, but they refused to accept payment
initially, but after request they agreed and on 27/01/2021 and he paid premium vide cheque No.
5207 and a policy was issued on 28/01/2021.
On 5
th
March,2021 the complainant and his wife were hospitalised for covid treatment and in
the 1
st
week of April,2021 he lodged a claim for reimbursement of hospital expenses. In the
2nd week of April,2021 he received a letter from the Insurer that the payment of premium was
not received and policy shall be treated as void from the inception. In the 3
rd
week of April,
2021 his claim was paid by the Insurer. When he approached local Branch of HDFC Ergo
regarding policy cancellation, they informed that cheque No.5207 paid towards renewal
premium, have returned due to insufficient fund. Then he approached his banker ICICI BANK,
they confirmed vide their letter dated 26/04/2021 that the cheque was not represented to them
for payment. So, he again approached the Insurer with all facts and documents, they informed
cheque was dishonoured on 28/01/2021 for reason “R025-prohibiting alternation/correction on
cheque. He requested to the insurer to return the cheque with proof that it had been presented
for payment. They assured to provide but failed to do so. Being aggrieved with the cancellation
of policy the complainant made an appeal before this forum for redressal.
b. The insurer in their self-contained note stated that the complainant had submitted premium
through cheque No. 005207 drawn on ICICI bank dated 27/01/2021 towards the issuance of
policy No. 2805203526018100000. Based on premium submitted through cheque the afore
mentioned policy was issued. The said cheque was presented to HDFC bank on 28/01/2021
and the same was returned with remarks “prohibiting alternation/correction on cheque under
CTS copy of the bank. Since premium was not received, the policy issued was forwarded for
necessary cancellation and accordingly, a cancellation letter was issued on 28/03/2021.
During the intervening period of time, two claims were registered on account of the
hospitalisation of the complainant and his wife. Since both the claims were registered prior to
policy cancellation, the claims were settled. Now they are willing to reinstate the policy subject
to submission of premium.
18. a. Complainant’s Argument; - Cancellation of policy without giving him an opportunity to
pay the premium is not justified.
b. Insurer’s Argument: They cancelled the policy due to dishonoured of cheque. Now they are
agreed to reinstate the policy subject to submission of premium
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of cheque and bank letter.
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint. It is observed
that the insurer has reinstated the policy before scheduled hearing and the complainant has
no further grievance on the matter. This is confirmed by the complainant vide his mail dated
19.09.2021. Accordingly, no hearing is required.
Dated at Bhubaneswar on the 22nd day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Vikash Agarwal Vrs. United India Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-051-2122-0065
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Vikash Agarwal,
C/o Shyam Sundar Ratan Kumar,
Nandi Sahi, Cuttack-753001. Mob-9937165078
2
Policy No:
Type of Policy
Duration of policy/Policy
period
2603012820P104202047. Carona Kavach Policy
24/07/2020 to 03/02/2021
Date of admission 05/09/2020 D.O.D 18/09/2020
3.
Name of the insured
Name of the policyholder
Mr. Vikash Agarwal
Mr. Vikash Agarwal
4.
Name of the insurer
United India Insurance Co. Ltd
5.
Date of Repudiation
18/02/2021
Non- disclosure of pre-existing disease.
6.
Reason for repudiation
7.
Dt of receipt of the
Complaint
10/05/2021
8.
Nature of complaint
Requested to advice the Insurer to settle the claim
AWARD
Taking into account the facts and circumstances of the case and the fact that the
insurer has renewed/reinstated the policy to the satisfaction of the complainant, the
matter now stands resolved.
Accordingly, the matter stands disposed of.
9.
Amount of Claim
Rs. 2,25,305
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs. 2,25,305/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
22/09/2021, Bhubaneswar
14.
Representation at the hearing
1) For the Complainant
Self through VC and Phone
2) For the insurer
Mr. P K Rout, Manager
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
22/09/2021
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Vikash Agarwal
is covered under policy No. 2603012820P104202047 for the period from 24/07/2020 to
03/02/2021 having sum insured of Rs. 3,00,000/-. He was admitted in CARE Hospital,
Bhubaneswar on 05/09/2020 being detected Covid positive and discharged on 18/09/2020. Out
of his total expenses of Rs.4,70,454/- he got reimbursed Rs.2,45,149/- from Star Health and
Allied Insurance Co. Ltd and for balance amount he lodged a claim with United India Insurance
Co Ltd for reimbursement which was repudiated by United India Incurrence Co. Ltd on the
ground of non- disclosure of pre-existing disease i.e. Bronchial Asthma. The insurer also stated
that the complainant has received the claim in full from another insurer and the amount which
constitute to be non-payable items are claimed with them, which is not payable. But while
submitting documents to this office, it is found that the complainant is silent on the claim
received from the other insurer and has preferred full claim amount of Rs.4,70,454/- without
deducting the amount already received. However, on being aggrieved with the repudiation, the
complainant made an appeal before this forum for redressal.
b. The insurers, in their self-contained note confirmed issuance of the above policy and stated
that the claim pertains to hospitalisation period of 05/09/2020 to 14/09/2020 at Care hospital,
Bhubaneswar for Covid treatment (Date of discharge differs from the, Discharge summary
submitted to Insurer and Discharge summary submitted to Ombudsman office.) On scrutiny
the discharge certificate dated 14/09/2021 of Care Hospital, it is observed that the patient was
a known case of Bronchial Asthma. This aspect was not disclosed in the proposal form while
taking the above policy, which is suppression of fact.
In the medical information clause No. VI of the proposal form it was clearly asked “Are you/the
person proposed for insurance in good health and free from physical and mental disease or
infirmity or medical complaints? To which the proposer answered as Yes. Then again for
question “have any of the persons who are proposed for insurance ever suffered from/are
suffering from any of the following: -respiratory disease, to which the insured ticked as No
(Even though he was having Bronchial Asthma, which is a respiratory disease). As per the
condition No. 3.8 of the policy “the policy shall be void in the event of non-disclosure of any
material fact by the policy holder. In view of the above suppression of fact, the policy becomes
void. Hence the claim is not payable as per condition No. 3.8 of the policy. Moreover, the
insurer has already got his claim settled with another insurer. The other insurer has settled the
claim in line with GI Council rules, which is also applicable to us. So even considering our
policy also this claim does not qualify for any further payment, since maximum claim as per
GI Council rate has been covered at the other insurer. Hence, no further claim i9s payable.
18. a. Complainant’s Argument; - Insurer repudiated to re-imburse basing on false, mischievous,
baseless fabricated and unfounded allegations of Bronchial Asthma, whereas he has never
suffered from this disease at any time till to-day.
b. Insurer’s Argument: Due to non-disclosure of material fact by the policy holder the claim
was repudiated.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of medical report
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard both
the parties. On a query if the complainant has made any claim from any other insurer, the
complainant during hearing stated that his claim is partially settled by Star Health and Allied
Insurance Co ltd and he has submitted all the documents to the present insurer for settlement
of balance claim. He is not aware of any other discharge voucher received by the insurer but
the insurer denied the claim under non-disclosure of pre-exiting illness, which is not correct
as he did not have any such illness prior to admission in hospital. The insurer stated that the
hospital has sent the Discharge Summary (DS) to their TPA but the complainant has submitted
a different Discharge Summary in his petition. Both the documents vary from each other
though it is issued by the same hospital for the same patient. It varies in respect of date of
discharge (in one it is 14.09.2020 and in the other it is 18.09.2020) Similarly, the ward number,
Bed number are different in both documents. Further in the 18.09.2020 Discharge Summary
the comments like ‘Associated Diagnosis (comorbidities): Bronchial Asthma’ and ‘Medical
History: K/C/O Bronchial Asthma are missing’, which are important in the underwriting and
decision making of the claim. The insurer stated that the DS submitted by the hospital directly
to the TPA is authentic and the fact that the complainant suppressed material facts at the time
of proposal and also at the time of claim. The insurer further stated that the other insurer has
settled the claim in full after deducting the non-payable items and said non-payable items are
not payable by any other company under any other policy, which is equally applicable to them.
The complainant has claimed the amounts which are non-payable under any policy. For all the
above reasons, the insurer informed that the claim is not payable.
Dated at Bhubaneswar on the 22nd day of September, 2021
INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, the Forum finds that the complainant has
lodged his claim with two different insurers, where one has settled in part and the present
insurer has denied in toto. The complainant did not disclose to this Forum in his
application on the complaint instead asked for full amount as relief, which lacks full
disclosure to the Forum. It is also found that the hospital has issued two different
Discharge Summaries against the same patient and same illness, not consistent to each
other involving matters which are important for consideration of the claim. The forum
considers non- disclosure of material facts in the proposal to be another important factor.
Further, the forum examined the claim details of the other insurer and found that the
claim amount which is not paid by the other insurer is because of non-payable items
under the policy, which is equally applicable for other policies too. In view of the above,
the forum finds the complaint fails to have merits for consideration and therefore, the
complainant is not entitled for any compensation from the present insurer.
Accordingly, the complaint stands dismissed.
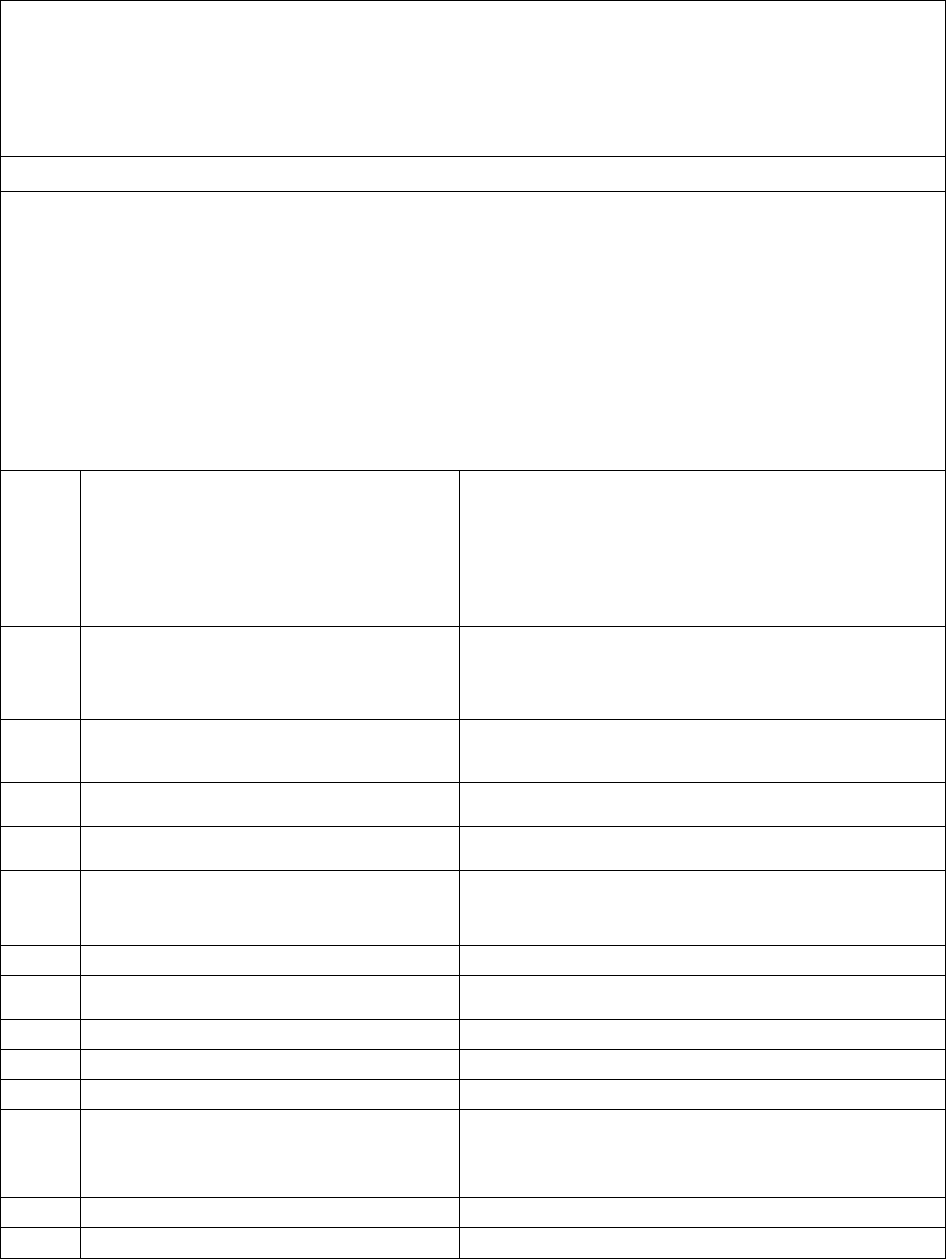
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri Suresh Chandra Panda, IAS
Case between: Mr. CHOLLETI SRINIVAS ………………The Complainant
Vs
M/s CARE Health Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .037.2122.0302
Award No.: I.O.(HYD)/A/HI/ 0048/2021-22
1.
Name & address of the complainant
Mr. Cholleti Srinivas
Flat #104, Shikara Apartments,
Chappal Bazar,Hyderabad
Telengana State- 500 027
(Cell No. 90309-74778)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
13545374
Floater insurance
31.01.2019 to 30.01.2022
3.
Name of the insured
Name of the Policyholder
Mr. Srinivas Cholleti
Mr. Srinivas Cholleti
4.
Name of the insurer
M/s CARE Health Insurance Co. Ltd.
5.
Date of Repudiation
06.12.2020
6.
Reason for repudiation
Query regarding first consultation of diabetes not
replied
7.
Date of receipt of the Complaint
18.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 3,13,764/-
10.
Date of Partial Settlement
------
11.
Amount of Relief sought
Rs. 3,13,764/-
12.
Complaint registered under
Rule No.13 (b) of Ins. Ombudsman
Rules, 2017
Rule 13 (b) – any partial or total repudiation of claims
by the Life insurer, General Insurer or
the Health insurer
13.
Complaint how disposed
Allowed ( Statistical Purpose)
14.
Date of Order/Award
27.09.2021
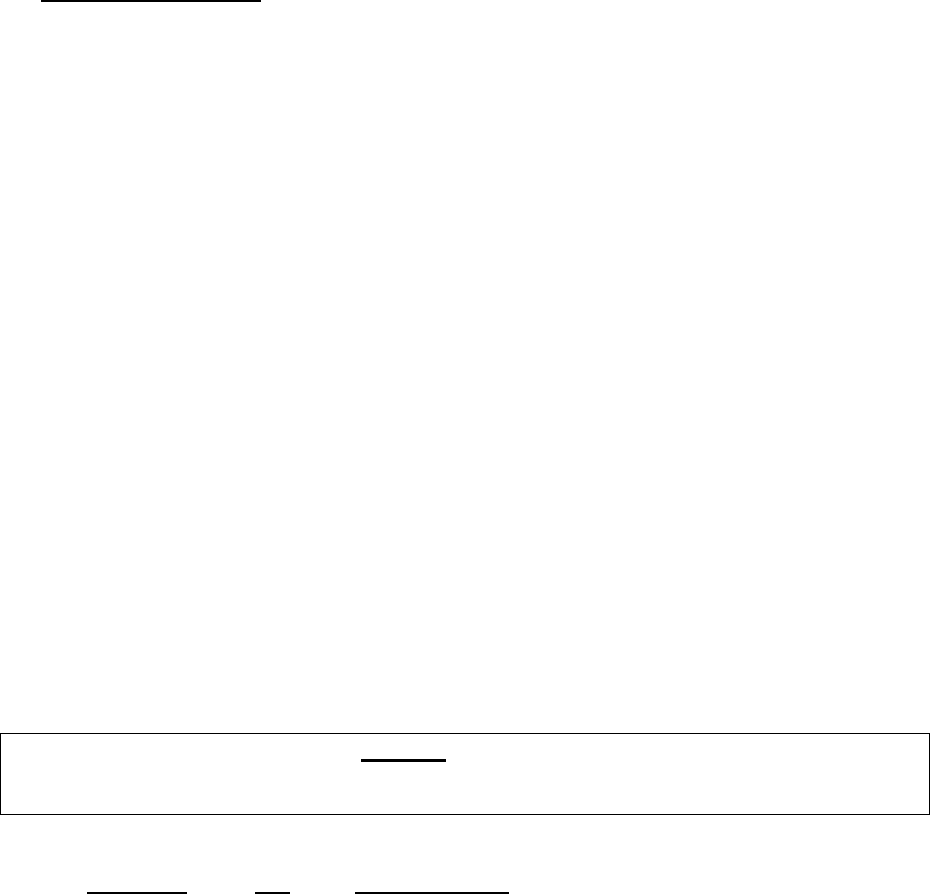
15 )Brief Facts of the Case:
The complainant had purchased a 3 year medical insurance policy from the respondent in which he
had included his spouse, son, daughter and him. During the period of insurance, he was admitted
between 01.10.2020 - 06.10.2020 at Subhiksha Hospitals, Hyderabad to undergo treatment for his
bilateral pneumonia (Corads-4) with Covid-19 (suspect) with which he was diagnosed. Subsequently,
he had lodged a claim under his medical insurance policy with the respondent. The respondent had
raised certain queries related to his medical condition of Diabetes to which he had responded
appropriately. Despite giving his clarifications, the respondent had denied the claim citing deficiency
of the requirements called for. Unhappy with the poor services of respondent who had failed to
respond to his emails and calls properly, he had therefore approached this Forum to seek justice.
16) Cause of Complaint: Rejection of Mediclaim
17) Reason for Registration of Complaint:
The claim preferred by the complainant was non - settlement of Mediclaim by the insurer. As the com-
plaint fell under Rule 13(b) of Insurance Ombudsman Rules, 2017, it was registered.
After registration of complaint by this Forum and before hearing, the insurer further reviewed the claim
and processed it and agreed to settle the claim for Rs.2,98,314/- vide mail dated 20.09.2021. The Com-
plainant accepted the settlement vide his letter addressed to the Insurer giving his unconditional ac-
ceptance for settlement of the claim for Rs.2,98,314/-. The insurer have informed this Forum vide mail
dated 27.09.2021 of having initiated the claim settlement for the said amount. ( Two Lakhs ninety eight
thousand three hundred and fourteen only).
AWARD
The complaint is treated as resolved and closed.
Dated at Hyderabad on the 27
th
day of September,2021.
(Suresh Chandra Panda)
OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
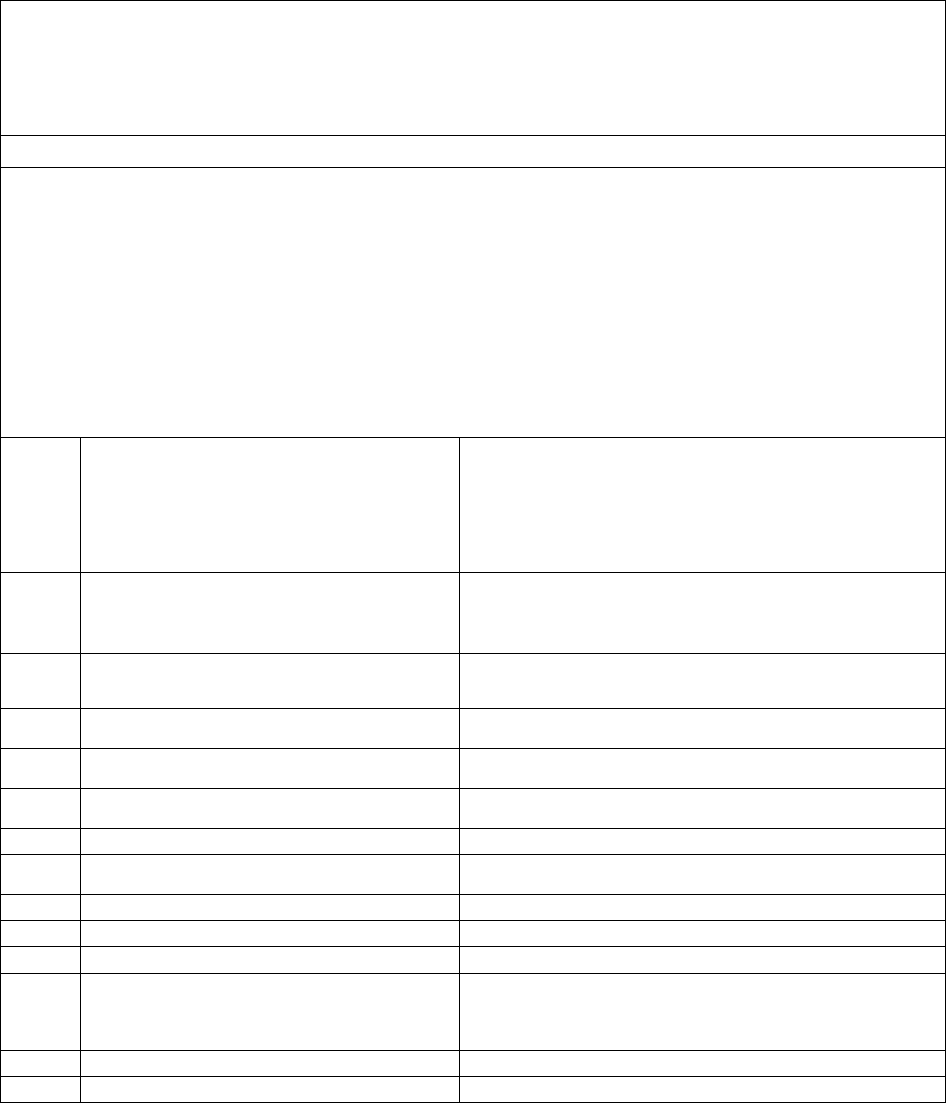
I.O.(HYD)/A/HI/ 0049 /2021-22
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri Suresh Chandra Panda, IAS
Case between: Mr. SREENIVASA PRASAD CHINTAPALLI ………………The Complainant
Vs
M/s Royal Sundaram General Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .038.2122.0319
Award No.: I.O.(HYD)/A/HI/ 0049 /2021-22
1.
Name & address of the complainant
Mr. Sreenivasa Prasad Chintapalli
Chintapalli Heights, III Floor, Plot #24, MIG-1,
D. No. 1-74-29, Sector-3, M V P Colony,
Visakhapatnam,Andhra Pradesh- 530 017
(Cell No. 94401-90960)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
MFG0025850000101
Family health floater policy
16.02.2019 to 15.02.2020
3.
Name of the insured
Name of the Policyholder
Mrs. Ch. Lakshmi
Mrs. Ch. Lakshmi
4.
Name of the insurer
M/s Royal Sundaram General Insurance Co. Ltd.
5.
Date of Repudiation
Not mentioned
6.
Reason for repudiation
Deficiency in submission of claim papers
7.
Date of receipt of the Complaint
02.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 18106/-
10.
Date of Partial Settlement
-----
11.
Amount of Relief sought
Rs.18106/- including post hospitalization expense
12.
Complaint registered under
Rule No.13 (b) of Ins. Ombudsman
Rules, 2017
Rule 13 (b) – any partial or total repudiation of claims
by the Life insurer, General Insurer or
the Health insurer
13.
Complaint how disposed
Allowed
14.
Date of Order/Award
27.09.2021
15 )Brief Facts of the Case:
The complainant’ wife who was covered under the medical insurance policy had incurred
hospitalization expense towards her treatment taken for HTN, CVA with ICH in Pradhama Hospital
where she was admitted from 19.12.19 to 30.12.19. However, on submission of the claim papers, the
respondent had sought certain requirements which the complainant had stated to have submitted.
Despite his correspondences with the respondent by placing a request to reimburse his wife’s claim,
there was no favorable response from them. Annoyed with their poor service, the complainant had
approached this Forum to seek justice.
16) Cause of Complaint: Rejection of Mediclaim
17) Reason for Registration of Complaint:
The claim preferred by the complainant was non - settlement of Mediclaim by the insurer. As the com-
plaint fell under Rule 13(b) of Insurance Ombudsman Rules, 2017, it was registered.
After registration of complaint by this Forum and before hearing on 27.09.2021, the insurer vide their
mail dated 17.09.2021 informed of having reviewed the complaint and settled the claim for an amount
of Rs.16496/- towards hospitalization and Rs.1584/- towards post hospitalization expenses by way of
NEFT on 08/09/2021. The Complainant agreed to the settlement and informed of having received the
NEFT amount and requested this Forum to close his complaint.
AWARD
The complaint is treated as resolved and closed.
Dated at Hyderabad on the 27th day of September, 2021.
(Suresh Chandra Panda)
OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
I.O.(HYD)/A/HI/ 0050 /2021-22
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri Suresh Chandra Panda, IAS
Case between: Mr. R ADINARAYANA ………………The Complainant
Vs
M/s STAR Health & Allied Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .044.2122.0313
Award No.: I.O.(HYD)/A/HI/ 0050 /2021-22
1.
Name & address of the complainant
Mr. Rangisehetty Adinarayana
H. No. 3-11-252, Road #2, Sri Shankar Colony,
L B Nagar, Ranga Reddy,Hyderabad
Telengana State – 500 074
(Cell No. 97005-04116)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
P/131140/01/2021/015888
Young star insurance policy
23.01.2021 to 22.01.2022
3.
Name of the insured
Name of the Policyholder
Rangisetty Adinarayana
Rangisetty Adinarayana
4.
Name of the insurer
M/s STAR Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
04.07.2021
6.
Reason for repudiation
Claim falls under the exclusion Clause No. 11
7.
Date of receipt of the Complaint
17.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 2,52,826/-
10.
Date of Partial Settlement
-------
11.
Amount of Relief sought
Rs. 2,52,826/-
12.
Complaint registered under
Rule No.13 (b) of Ins. Ombudsman
Rules, 2017
Rule 13 (b) – any partial or total repudiation of claims
by the Life insurer, General Insurer or
the Health insurer
13.
Complaint how disposed
Allowed
14.
Date of Order/Award
27.09.2021
15 )Brief Facts of the Case:
The complainant had purchased an annual medical insurance policy from the respondent wherein he
had included his spouse, two dependent children, and him for a basic floater sum insured of Rs. 5
Lakhs. He was hospitalized in Sai Teja Hospital, Hyderabad between 24.04.2021 and 30.04.2021 to
undergo treatment for Viral Pneumonia. Subsequently, he had filed a claim for reimbursement with
the respondent but it was rejected by them on ground that the hospital where he underwent
treatment was blacklisted by the Insurance Company. He had tried in vain to represent to the
respondent to reconsider his claim favorably. Unhappy with the lack of response, the complainant had
therefore approached this Forum to seek justice.
16) Cause of Complaint: Non settlement of Mediclaim.
17) Reason for Registration of Complaint:
The claim preferred by the complainant was non - settlement of Mediclaim by the insurer. As the com-
plaint fell under Rule 13(b) of Insurance Ombudsman Rules, 2017, it was registered.
After registration of complaint by this Forum and before hearing, the insurer further reviewed the claim
, processed it and agreed to settle the claim for Rs.2,39,535/- . The Complainant accepted the settlement
vide mail dated 21.09.2021 for Rs.2,39,535/-. Hence, this Forum directs the respondent insurer to accept
and settle the claim for Rs.239535/- as agreed and inform the NEFT details .
AWARD
Taking into account the facts & circumstances of the case and the information/documents
placed on record, the insurer is directed to settle the claim for Rs.2,39,535/- .
The complaint is Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:
1) According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
2) According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 27th day of September ,2021.
(SURESH CHANDRA PANDA)
OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS
Case between: Mr. DASARI MURALIDHAR ………………The Complainant
Vs
M/s The Oriental Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .050.2122.0312
Award No.: I.O.(HYD)/A/HI/ 0051 /2021-22
1.
Name & address of the complainant
Mr. Dasari Muralidhar
201, S V Enclave, Pragathi Enclave,
Neelima Greens Colony, Miyapur,
Hyderabad,Telengana State- 500 049
(Cell No. 62811-24293)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
431500/48/2021/4176
Corona Kavach Policy
06.08.2020 to 17.05.2021
3.
Name of the insured
Name of the Policyholder
Mr. Dasari Muralidhar
Mr. Dasari Muralidhar
4.
Name of the insurer
M/s The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
26.06.2021
6.
Reason for repudiation
RT- PCR test which is mandatory was not done
7.
Date of receipt of the Complaint
30.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 3,30,000/-
10.
Date of Partial Settlement
------
11.
Amount of Relief sought
Rs. 3,30,000/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
27.09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.C.Shankaraiah, SDM
15.
Complaint how disposed
Allowed
16.
Date of Order/Award
27.09.2021

17) Brief Facts of the Case:
The complainant had purchased a short term Corona Kavach medical policy from the respondent to
include his spouse, two dependent children and him. During the policy period, he was admitted to Sia
Life Hospital between 01.05.2021 -07.05.2021 to undergo treatment for the medical diagnosis of
Covid-19 Viral Pneumonia. Subsequently, he had filed a reimbursement claim against the policy with
the respondent. The respondent however had denied his claim citing non compliance of the specific
policy clause embedded in the policy. Unhappy with the reasons given for the rejection of his claim,
the complainant had therefore approached this Forum to seek justice.
18) Cause of Complaint: Repudiation of claim made against the medical Insurance policy.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that he had mild fever with cough
from 15.04.2021 and had therefore got his RT PCR test done as abundant caution at Health Valley
Hospital on 18.04.2021 but whose test report was negative for Covid. However, his temperature had
soared up to 104 degrees F by the same evening and continued for the next three days. There upon,
he had consulted a pulmonologist Dr Swetha Kasturi, MD and upon her advice had got his CT scan
done at Tenet Diagnostics for Covid-19 on 27.04.2021. The impression drawn from this test was Covid-
19 affecting his lungs with CORADS-5 ratings, and was concluded as typical of Covid19. The pul-
monologist had changed the prescription of medicines to Covid medication. Despite the same, his
health had deteriorated and was advised to undergo tests such as Ferritin serum, CPB, CRP, LDH which
he had underwent on 01.05.2021 at Tenet Diagnostics. Since he had started to develop breathless-
ness, he was advised to admit himself in a Covid specialty hospital immediately. He could ultimately
get admit in Sai Life hospital after he had to encounter a lot of difficulty in getting a vacant bed. The
test reports received on the subsequent day revealed high, abnormal and disturbing levels of Ferritin,
WBC, Absolute Neutrophil count, Neutrophil Lymphocyte ratio, CRP, LDH thus apparently pointing out
that he had contracted the dreaded Covid-19 virus. He was put under medication and oxygen supple-
mentation to maintain his SPO2 level at 97% as he had become severely hypoxemic, along with sup-
portive round the clock critical care up to 07.05.2021. He had renewed the policy as he felt it necessary
after his discharge from hospital.
The denial of claim by respondent was not agreeable to him because a false negative outcome in RT
PCR test was not uncommon and the studies indicate that 33% of the patients affected with Covid-19
had false negative results initially despite the presence of virus. The reasons for the same were due to
irregularities in sampling techniques, delayed analysis, ineffective sample storage and also due to var-
iable gene targets in RT PCR investigation or if the test was done when there was an absence of viral
throat carriage or if it was below the threshold for the virus to be detected. Thus in the view of com-
plainant, RT PCR test was by no means conclusive. The very source of his illness and hospitalization
being Covid -19, repudiation of his claim by respondent on grounds of a false negative RT PCR test
result was incorrect despite undeniable evidence. When he questioned the respondent, the complain-
ant was asked to submit his representations along with the relevant documents. Upon furnishing the
same to respondent on 30
th
June in support of his claim, he did not get any positive response despite
his repeated requests to reconsider the same but only to be turned away with an advice to approach
this Forum.
As a post doctoral scholar in microbiology and a sole bread winner for his family, he was currently
unemployed due to pandemic and the promise made by respondent through their announcement to
come to rescue of their policy holder made him to procure the same but such denial of the claim by a

nationalized company had amounted to their dishonest and deceitful conduct. He had therefore
pleaded before this Forum to look in to the documents which support his claim and to direct the re-
spondent to settle the claim in full and at the earliest time.
b) Insurer’s argument:
Self contained note was submitted by the respondent. They had issued a Corona Kavach policy from
web portal of their company on 06/08/2020 for a sum insured of Rs.5 Lakhs, policy commencing from
06/08/2020 to 17/05/2021. The insured Mr.D.Muralidhar got admitted to SIA life hospital, Kondapur,
Hyderabad on 01/05/2021 and discharged on 07/05/2021. He got admitted with complaints of cough,
generalized weakness, mild SOB, Fever spikes since 6 days, dryness of mouth since 5 days. Before his
admission to Sia hospital, he underwent RT-PCR test at Health valley hospital on 18/04/2021 and the
result showed Covid19 negative. This report was not submitted to them until much later. He consulted
Dr.Sweta Kumari , Pulmonologist who advised him to undergo CT scan of Thorax on 27/04/2021 when
his fever did not subside. At Tenet Diagnostics, Banjara Hills, Hyderabad he underwent scanning with
a report showing a score of 8/25, which was observed to be a reading of Mild covid. His report from
consulting radiologist Dr.V.Sudheer Reddy showed mild interstitial thickening in both lungs and he
opined as indicating Viral Pneumonia. The diagnostic tests pertaining to LDH serum & Ferratin were
showing abnormal readings however the discharge summary did not mention the same. No antigen
test was done. No RTPCR from government authorized diagnostic center, Corad-5 score indicated
likely chances of covid-19 and not a definite indicator of covid-19. Hence they had dismissed the claim.
19) Reason for Registration of Complaint:
The insurer rejected the claim preferred by the complainant. As the complaint falls under Rule 13.1(b)
of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a) Policy with terms and conditions.
b) Correspondence with insurer
c) Rejection letter, discharge summary, reports, consolidated bill etc.,
d) Self Contained Note with its enclosures.
21) Result of hearing with both parties:
Pursuant to the notices given by this Forum, both the parties attended the personal hearing on 27.09.2021
at Hyderabad. Both the parties reiterated their arguments for and against the complaint.
The Forum has observed that the CT scan was taken from Tenet diagnostics, an NABL accredited diagnostic
center. The CT scan score of 8/25 shows he is infected with Covid. The Ferratin, CRP, D-Dimer and IL(6)
readings clearly show he was a covid patient. The contention of the Insurer for rejection of the claim that
there was no confirmatory diagnosis of Covid by a government authorized diagnostic center is not ac-
cepted because Tenet diagnostics is a NABL accredited diagnostic center and the result of diagnostic re-
ports shows positive covid-19 infection Corad-5. The Forum observes from the submissions made by the
complainant that Doctor advised him to get admitted to a hospital and that his condition at the hospital
was serious, having been on oxygen support and having had to be in a prone position due to acute respir-
atory distress. The Forum observes from the medical records are good enough to suggest that complainant
is infected with Covid-19. Hence this Forum directs the respondent insurer to admit and settle the claim
in respect of the eligible component of the Corona treatment underwent, in full.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the par-
ties during the course of the personal hearing and the information/documents placed on record, the
insurer is directed to settle the claim for the eligible component of corona treatment in full.
The complaint is Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance Ombudsman
Rules, 2017:
a) According to Rule 17(6) the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
b) According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as spec-
ified in the regulations, framed under the Insurance Regulatory & Development Authority of India Act from
the date the claim ought to have been settled under the Regulations till the date of payment of the amount
awarded by the Ombudsman.
c) According to Rule 17 (8) the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 27
TH
day of September, 2021.
(SURESH CHANDRA PANDA)
INSURANCE OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
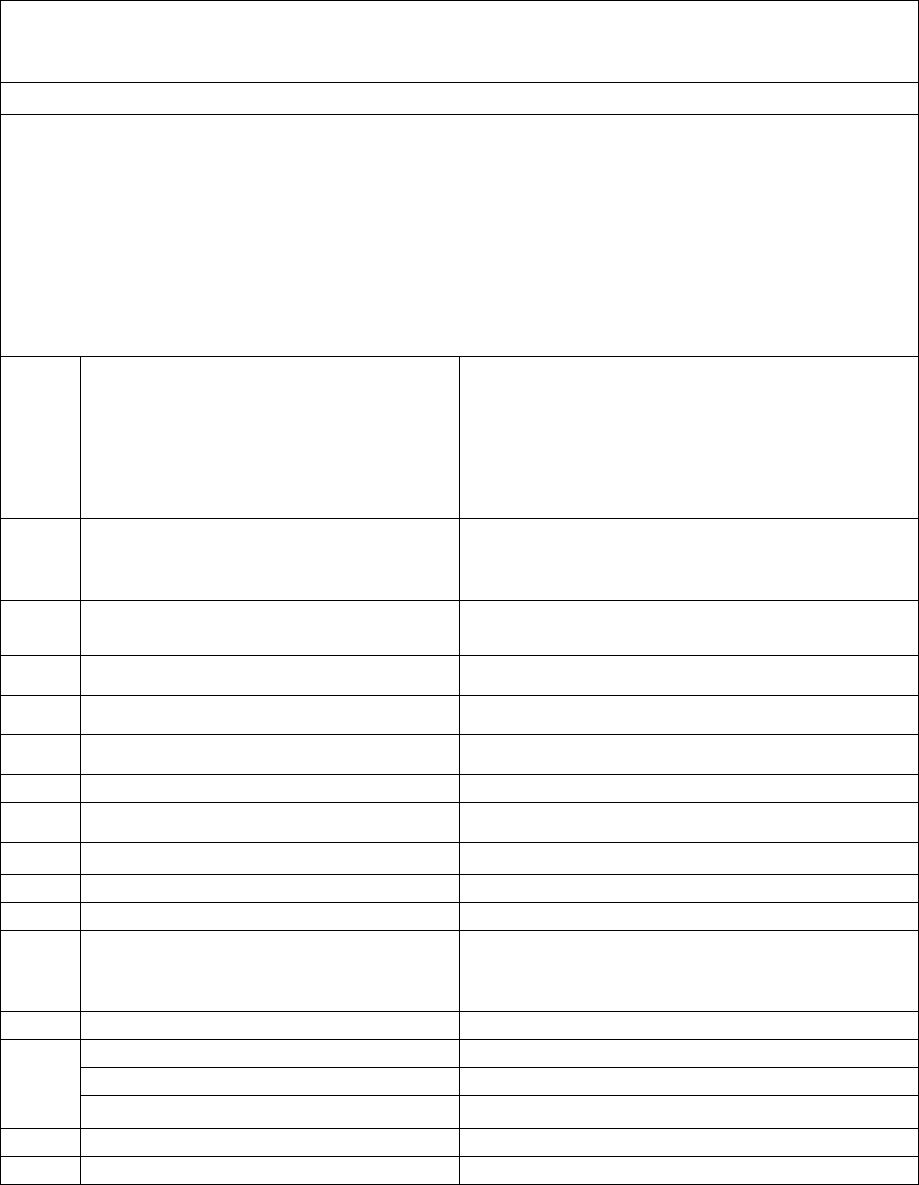
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS
Case between: Mr. CHINNAM POORNA CHANDRA RAO ………………The Complainant
Vs
M/s STAR Health & Allied Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .044.2122.0317
Award No.: I.O.(HYD)/A/HI/ 0052 /2021-22
1.
Name & address of the complainant
Mr. Chinnam Poorna Chandra Rao
Flat #101, TVS Mahathi Apartments,
Lanco Hills Road, Manikonda,
Behind SR Digi school,Hyderabad
Telengana State- 500 089
(Cell No. 95430-07007)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
P/111100/01/2020/007078
Star Group Health insurance- Revised
04.10.2019 to 03.10.2020
3.
Name of the insured
Name of the Policyholder
Mr. Chinnam Poorna Chandra Rao
Mr.Chinnam Poorna Chandra Rao
4.
Name of the insurer
M/s STAR Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
21.06.2021
6.
Reason for repudiation
Treatment does not require hospitalization
7.
Date of receipt of the Complaint
04.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 1,54,942/-
10.
Date of Partial Settlement
06.07.2021
11.
Amount of Relief sought
Rs. 79,614/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
27.09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.M.Ravi Kumar, AGM, Legal
15.
Complaint how disposed
Allowed partially
16.
Date of Order/Award
28.09.2021
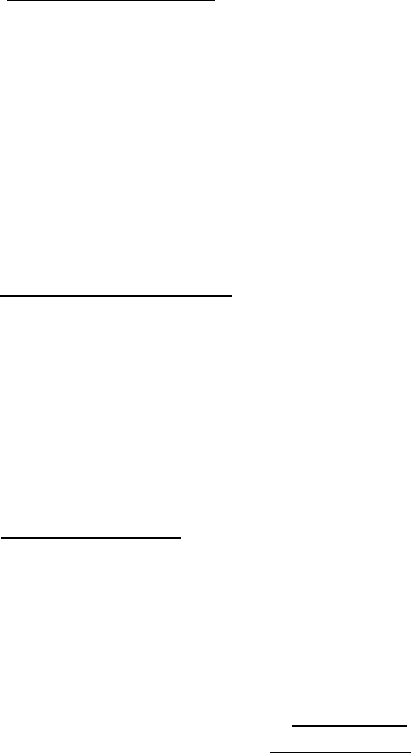
17) Brief Facts of the Case:
The complainant had filed a claim towards his in-hospitalization treatment taken for Covid at sunshine
hospitals, against the medical insurance policy which he had purchased from the respondent. However,
the respondent who had initially declined to admit his claim had settled the same for a partial amount
of Rs. 75,328/- after he had approached the Grievance department with his representation to
reconsider his claim. Unhappy with the partial settlement of his claim, the complainant had therefore
approached this Forum to seek justice.
18) Cause of Complaint: Partial payment of claim made against the medical Insurance policy.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that when he had received an
amount of Rs. 75,328/- after his representation to the respondent’s Grievance department, he had
sent emails on three occasions to seek the details with a request to them to settle his balance claim
amount. As a senior citizen who was diagnosed with Covid positive and got admitted only at the advice
of his doctor, the reasons given by respondent initially to reject his claim was not justified and there-
after the partial settlement of his claim without sharing the details with him was unacceptable.
b) Insurer’s argument:
Self contained note was submitted by the respondent over mail. They had once again reviewed and con-
sidered for payment of Rs. 11,424/- in addition to their earlier settlement. The details are as follows:
Claim Amount Rs. 1,55,442-00
Payables Rs. 86,752-00
Less paid Rs. 75,328-00
Balance Payable on review Rs. 11,424-00
Details of deductions: Total Rs 68,690-00 were not allowed as under:
Rs 22,680 - Bedsheet, cap, gown kit, face shield, Handrub, Gloves, Masks are not payable.
Rs 43,750 - Medical record, Sanitization, Risk Allowance Charges, cross referral charges are
not payable.
Rs 2,260 - Bill No. 7300 No patient name hence disallowed, PPE charge, Covid Profile No Break
Up. Hence 80% allowed.
They requested the Hon'ble Ombudsman office to verify the same and on acceptance, the additional
amount shall be arranged for payment.
19) Reason for Registration of Complaint:
The insurer partially settled the claim preferred by the complainant. As the complaint falls under Rule
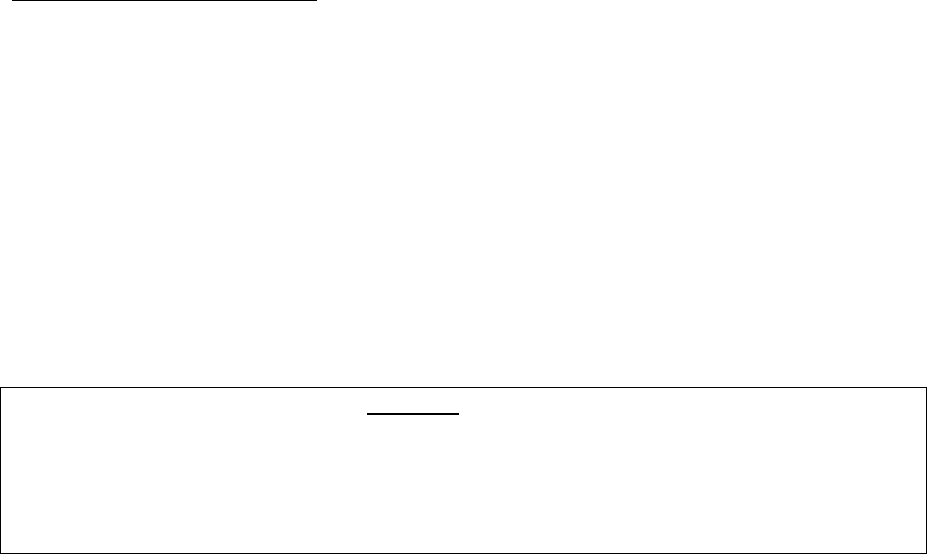
13.1(b) of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy
b. Discharge summary
c. claim assessment sheet
d. Correspondence with insurer
e. Self contained note.
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum both parties attended the online hearing at Hyderabad on
27.09.2021.
The Respondent insurer had agreed to pay Rs.11,424/- in addition to the earlier settlement made. The
Forum has sought for a detailed analysis for the disallowed amount of Rs. 68,690/- out of which as per
policy condition the cost towards the following disallowed items amounting to Rs.37,130/-are allowed.
Hence, the Forum directs the respondent insurer to admit and settle the claim for Rs. 48,554/-.
ITEM Cost in Rs.
Cap
30
Gown kit
18000
Face shield
300
Hand rub
750
Gloves
900
Mask
1900
Sanitation charges
7500
Cross referral charges
7750
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the par-
ties during the course of the personal hearing and the information/documents placed on record, the
insurer is directed to settle the claim for 48,554/-(Rs.11,424+Rs.37,130) .
The complaint is Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:
3) According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
4) According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as
specified in the regulations, framed under the Insurance Regulatory & Development Authority of
India Act from the date the claim ought to have been settled under the Regulations till the date of
payment of the amount awarded by the Ombudsman.
5) According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.

Dated at Hyderabad on the 28th day of September , 2021.
( SURESH CHANDRA PANDA )
OMBUDSMAN FOR
THE STATES OF A.P.,
TELANGANA AND YANAM CITY
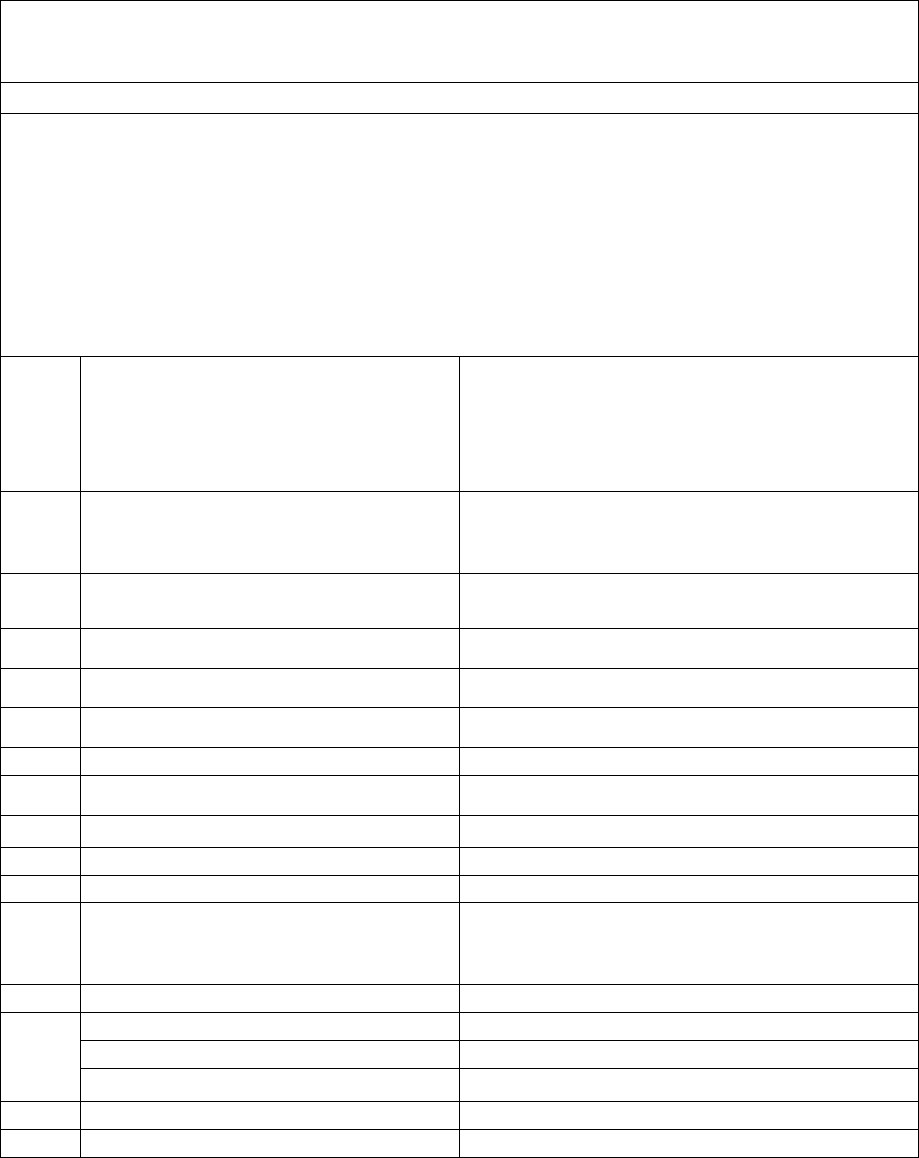
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri Suresh Chandra Panda, IAS
Case between: Mr. BALANTHRAPU SUDHAKAR ……………The Complainant
Vs
M/s STAR HEALTH AND ALLIED INSURANCE CO.LTD…….…………The Respondent
Complaint Ref. No. I.O.(HYD).H .044.2122.0316
Award No.: I.O.(HYD)/A/HI/ 0053 /2021-22
1.
Name & address of the complainant
Mr. BALANTHRAPU SUDHAKAR
H.NO.11-9/3/A, Ground Floor,
GADDIANNARAM,DILSUKHNAGAR,
HYDERABAD. TELANGANA-500060.
MOBILE NO.81422 22710
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
P/131141/01/2021/000822
CORONA KAVACH POLICY
19.08.2020 TO 31.05.2021
3.
Name of the insured
Name of the Policyholder
Mr.B.Sudhakar
Mr.B.Sudhakar
4.
Name of the insurer
M/s.Star Health & Allied Insurance Co.Ltd.,
5.
Date of Repudiation
24.07.2021
6.
Reason for repudiation
Covid +ve Test Report not submitted
7.
Date of receipt of the Complaint
09.08.2021
8.
Nature of complaint
Complaint on repudiation of claim
9.
Amount of Claim
Rs. 2,35,000/-
10.
Date of Partial Settlement
NA
11.
Amount of Relief sought
Rs.2,35,000/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
27.09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.M.Ravi Kumar, AGM, Legal
15.
Complaint how disposed
Dismissed
16.
Date of Order/Award
28.09.2021
17) Brief Facts of the Case:
The Complainant had taken the Corona Kavach policy for Rs.5,00,000/- for the period from 19/08/2020 to
31.05.2021 from the Respondent Insurer. During the policy period the complainant had suffered with fever
and coughs and underwent CT SCAN OF CHEST (HRCT) in a private Diagnostic Centre, on his own. The Test
Results confirmed ViraL Pnemonia(CO-RADS-5) with severity Score of 16/25. Since the Test Results had con-
firmed the positive existence of Covid-19 he had joined in the Hospital on 13/05/2021 for treatment and
discharged on 18.05.2021. The complainant had lodged the claim with the RI for reimbursement of expenses
incurred during the hospitalization. However his claim was rejected by the RI on the grounds that the Covid-
19 Test Report was not obtained from a government authorized diagnostic centre which is a pre-condition
for admitting the claim as per the Policy condition No.4.1.
18) Cause of Complaint: Delay in settlement of Claim by the Respondent Insurer under the Medical
Insurance policy.
a) Complainant’s argument:
The complainant had objected to reject the claim revoking the policy condition No.4.1 which was not
issued to him. He had received a single page policy without any policy wording and he was kept in
dark on the terms and conditions of the policy by the RI. He had not approached the Covid Lab recog-
nized by the Govt. due to long queues for the covid test to avoid further exposure. However he had
undergone HRCT of Chest which confirmed Viral Pneumonia (CO-RADS-5) WITH SEVERITY SCORE OF
16/25. Based on the positive existence of Covid and severity levels he had joined in the hospital and
got treatment for Covid. Since the CT Scan and Hospital treatment confirms the diagnosis of COVID
the complainant pleaded for settlement of his claim based on the documentary evidence instead of
relying on technical grounds.
b) Insurer’s argument:
The RI had submitted the SCN on 21.09.2021. As per the SCN the RI had confirmed the receipt of claim
from the insured under the Corana Kavach Policy issued by them. On scrutiny of the claim documents
the RI had observed that the insured was diagnosed with Viral Pneumonia-19 and the insured patient
had not done covid test at ICMR approved Centre. The RI had stated that as per the policy Base Cover
4.1 the company shall indemnify medical expenses incurred for Hospitalization of the insured person
during the policy period for the treatment of Covid on Positive Diagnosis of Covid in a government
authorized diagnostic centre. However, the insured patient had not done covid Test at an ICMR ap-
proved centre. Since the Corona Kavach policy was specific to cover only Covid ailment subject to
positive diagnosis in a government authorized centre the RI was unable to settle the claim. Hence the
claim was repudiated and communicated to the insured. The RI had justified the rejection of the claim
based on the terms and conditions of the policy and on the settled Law that term of the policy shall
govern the contract between the parties.
19) Reason for Registration of Complaint:
The insurer rejected the claim preferred by the complainant. As the complaint falls under Rule 13.1(b)
of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy with terms and conditions
b. Discharge summary/Medical Reports
c. Correspondence with the Insurer
d. Self contained note with annexures
21) Result of the personal hearing with both the parties:
Both the parties attended the online hearing held on 27.09.2021 and made their submissions on the
complaint.
The Forum observed that the complainant had not undergone Covid Test in any Government author-
ized diagnostic centre and has therefore not complied with the policy condition No.4.1 of Corona Ka-
vach policy. Further as per the medical records from ARK health care multispecialty hospital, his vital
medical parameters were within normal limits. The case is found to be devoid of any merit, and hence
is dismissed.
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the par-
ties during the course of the Online Hearing and the information/documents placed on record, the
Forum upholds the repudiation of the claim by the respondent insurer.
The complaint is DISMISSED.
Dated at Hyderabad on the 28
th
day of SEPTEMBER, 2021.
( SURESH CHANDRA PANDA )
OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
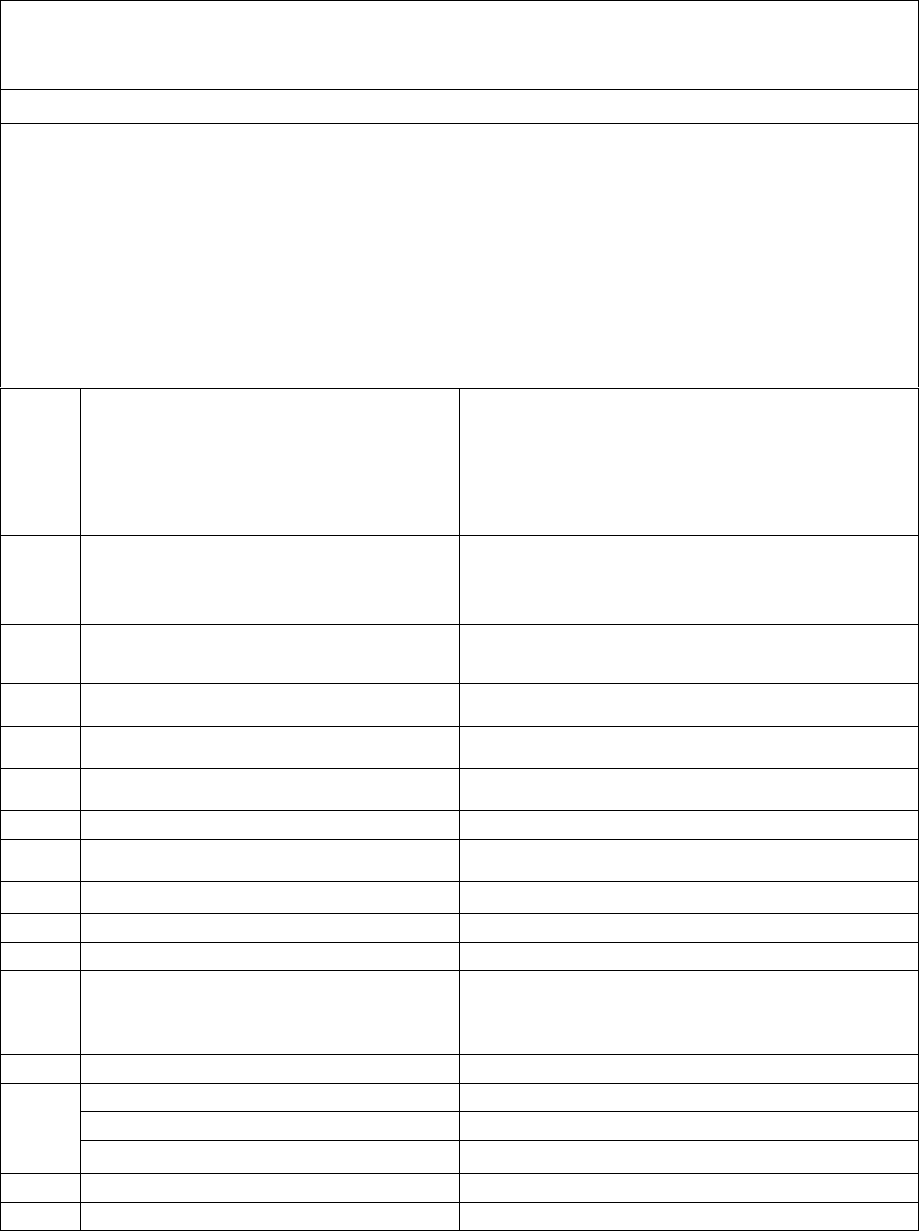
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS
Case between: Mr. D. LAXMI NARAYANA REDDY ………………The Complainant
Vs
M/s HDFC ERGO General Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .018.2122.0315
Award No.: I.O.(HYD)/A/HI/ 0055 /2021-22
1.
Name & address of the complainant
Mr. D. Laxmi Narayana Reddy
H. No. 37-72/7/4, J J Nagar,
Neredmet X Road,Secunderabad
Telangana- 500 094
(Cell No. 92461-04008)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
2805203623296401000
Medical insurance policy
24.02.2021 to 23.02.2022
3.
Name of the insured
Name of the Policyholder
Mrs. D Shobha Reddy
Mr. D Laxminarayana Reddy
4.
Name of the insurer
M/s HDFC ERGO General Insurance Co. Ltd.
5.
Date of Repudiation
27.07.2021
6.
Reason for repudiation
Claim documents are not genuine
7.
Date of receipt of the Complaint
26.08.2021
8.
Nature of complaint
Rejection of covid-19 mediclaim
9.
Amount of Claim
Rs. 2,54,700/-
10.
Date of Partial Settlement
------
11.
Amount of Relief sought
Rs. 2,54,700/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation
of claims by the Life insurer, General Insurer or
the Health insurer
13.
Date of hearing/place
29.09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.Aneesh Bhaskaran, Sr.Mngr Legal
15.
Complaint how disposed
Allowed
16.
Date of Order/Award
29.09.2021
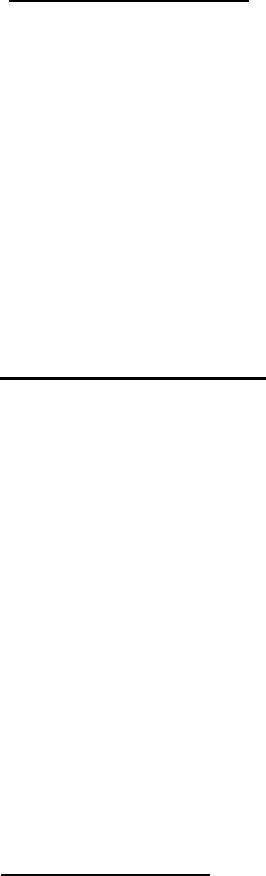
17) Brief Facts of the Case:
The complainant had purchased an annual medical insurance policy from the respondent
company and as per the documents submitted; his wife was admitted to Ramya hospital on
14.05.2021 to undergo treatment for the medical diagnosis of Covid with bilateral pneumonia.
She was discharged from the hospital on 23.05.202. Subsequently, she had filed a claim with
the respondent only to be denied by them on grounds of the documents having been forged.
Despite the clarification given to respondent by the complainant, the claim of his wife was not
considered favorably by the respondent. Displeased with the rejection of his wife’s
hospitalization claim, the complainant had therefore approached this forum to seek justice.
18) Cause of Complaint: Repudiation of claim made against the medical Insurance policy.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that he had been associated
with the respondent for a long time and that he had claimed only once in the previous year
when his wife was hospitalized for Dengue fever. The current claim fell within the present
policy period. His submission was that his wife was unable to breathe and her SPO2 levels had
dropped due to which he had tried to contact all the net work hospitals that could provide him
cashless facility. However, none of these hospitals had vacant beds available due to high num-
ber of admission of cases in Hyderabad at that point of time and she could get admission in
Ramya Hospital, Secunderabad where there was no cashless facility. He had clarified that the
entire amount was paid to hospital after she was discharged from there and thereafter had sub-
mitted all the original documents as shared to him by the hospital, with the respondent. He had
pleaded that if there were any discrepancies noted in those documents by respondent, the hos-
pital ought to be made responsible for the same and not he who was the respondent’s genuine
customer. He had therefore requested the Forum to conduct thorough investigation and to en-
able him to get the claim amount from the respondent and also to direct them to restore his
policy.
b) Insurer’s argument:
Self contained note was submitted by the respondent. They had issued Optima restore floater
policy, period commencing from 24/02/2021 to 23/02/2022 for a total sum insured of Rs.25
Lakhs covering the insured and his family. On discreet investigation they found spouse of the
insured Sm D.Shoba reddy had all the classic symptoms of covid-19 since 09/05/2021, got
herself tested on 10/05/2021, test result showed her covid-19 positive on 11/05/2021. She con-
sulted Dr.Nithya who advised her general medication. On doctors advice she underwent CTSS
scan and upon doctors advice got herself admitted to Ramya Hospital on 14/05/2021. During
her stay she was shifted to covid isolation ward and later to ICU on 18/05/2021. Patient was
discharged on 23/04/2021 as per the discharge report. From the doctors notes it was found that
she was on ventilator from 18/05/2021 to 20/05/2021 but there was no justification provided.
Also on 21/05/2021 her SPO2 levels were maintained with oxygen support and were dis-
charged on 23.05.2021. As per the treating doctors statement he mentioned that patient had
recovered by 20/05/2021 but on the request of the patient, her stay in hospital was extended.
She has also requested to reduce 3 days O2 charges from the main bill. Doctor has explained
that patient was discharged on 20/05/2021 but on patient’s request they had charged for extra
3 days and obtained written statement from Dr.Mahesh Swamy. Post discussion with the treat-
ing doctor, they found insured’s mobile timeline was matching with admission upto 20/05/2021
at ramya hospital and after that date it was showing somewhere else. Print shot of timeline
discrepancy was submitted. The insured hid the fact that on request they got prepared for extra
3 days hospitalization bill while she was actually discharged on 20/05/21 and not 23/05/21, it
amounted to misrepresentation of facts. Post receiving repudiation letter they obtained a med-
ical certificate dated 27.07.2021 from the hospital confirming discharge date to be 23/05/2021
as an afterthought to vindicate their discrepancy. Since they were not genuine, the claim was
repudiated as per the policy clause dealing with fraud, misrepresentation, non disclosure of
material facts. The policy of the complainant was cancelled with effect from 24.02.2021 as per
another letter dated 12.08.2021 issued to the complainant.
19) Reason for Registration of Complaint:
The insurer rejected the claim preferred by the complainant. As the complaint falls under Rule
13.1(b) of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy
b. Rejection letter
c. Correspondence with insurer
d. Self contained note with enclosures.
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum both parties attended the online hearing at Hyder-
abad on 29.09.2021 .Both the parties reiterated their stand for and against the complaint.
The complainant stated that his wife Smt D.Shobha Reddy was admitted from 14.05.2021 to
23.05.2021 at Ramya Hospital for covid-19 treatment. She was kept in the ICU for 9 days and
3 days in a general award. His claim was rejected and his policy was cancelled stating the
documents submitted by him were forged. He reiterated that he was eligible for the reimburse-
ment claim and restoration of cancelled Policy.
The Respondent insurer informed that on further investigation of the claim, it was found that
as per the treating doctor’s statement the patient had recovered by 20.05.2021 but on the request
of the patient her discharge from the hospital was extended by three more days ie., upto
23.05.2021. Since this amounted to misrepresentation of facts, the claim was denied and the
policy was cancelled.
The Forum observed hospitalization of Smt D.Shobha Reddy with Covid-19 is not disputed by
the respondent insurer. She has been discharged from the hospital on 20.05.2021 and the re-
spondent insurer has produced the treating doctor’s certificate of the same hospital that they
stayed till 23
rd
on their own request to be kept under observation. At the best the insurer may
not pay the hospital bills pertaining to hospitalization from 21.05.2021 to 23.05.2021 because
it was on their own request. However, it is incumbent upon the respondent insurer to clear the
entire admissible hospital bills for the period of hospitalization from 14.05.2021 to 20.05.2021
as per the terms and conditions of the Policy. Again it is found that the respondent insurer have
cancelled the policy on the grounds of forgery. It may be said that, staying in the hospital for 2
or 3 more days on their own request is not a matter of forgery or fraud. Rather the cancellation
of the policy by the respondent insurer is too harsh a measure. Therefore, policy should also be
restored with continuity benefits.
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both
the parties during the course of the personal hearing and the information/documents placed on
record, the insurer is directed to pay claim for hospitalization from 14.05.2021 to 20.05.2021
and restore the policy protecting all the continuity benefits.
The complaint is Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:
• According to Rule 17(6), the insurer shall comply with the award within 30 days of the re-
ceipt of the award and intimate compliance to the same to the Ombudsman.
• According to Rule 17(7), the complainant shall be entitled to such interest at a rate per
annum as specified in the regulations, framed under the Insurance Regulatory & Develop-
ment Authority of India Act from the date the claim ought to have been settled under the
Regulations till the date of payment of the amount awarded by the Ombudsman.
• According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the In-
surers.
Dated at Hyderabad on the 29th day of September , 2021.
( SURESH CHANDRA PANDA )
INSURANCE OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
Award no:Hyd:IO:A:HI:0056:21-22
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS (Retd)
Case between: Mr. Madhusudhana Rao Kasina ………………The Complainant
Vs
M/s HDFC ERGO General Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .018.2122.0304 &305
Award No.: I.O.(HYD)/A/HI/ 0056 /2021-22
1.
Name & address of the complainant
Mr. Madhusudhana Rao Kasina
Plot #119 120 C, Flat #301, Sai Krishna
Apartment,Raghavendra Colony,Behind Sia Life
Hospital,Rangareddy District,
Telengana State- 500 084
(Cell No. 77024-46888)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
2861 1010 3219 2000 000
Corona Kavach Policy
13.04.2021 to 22.01.2022
3.
Name of the insured
Name of the Policyholder
Mr. Kasina Abhishek & Mrs K.Swarajya lakshmi
Mr. Madhusudhana Rao Kasina
4.
Name of the insurer
M/s HDFC Ergo General Insurance company
5.
Date of Repudiation
23.07.2021
6.
Reason for repudiation
Claim does not fall within the scope of home
care expense
7.
Date of receipt of the Complaint
20.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 16,296/- and Rs.18,974/-
10.
Date of Partial Settlement
-----
11.
Amount of Relief sought
Rs. 16,296/- and Rs.18,974/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
29.09.2021, online Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.Aneesh Bhaskaran
15.
Complaint how disposed
Allowed
16.
Date of Order/Award
29.09.2021
17) Brief Facts of the Case:
The complainant had purchased a corona kavach medical insurance policy from the respondent valid
for 285 days in which he had included his son, spouse and him. His son and wife were diagnosed with
COVID positive on 10.05.2021 and were advised by the treating doctor to quarantine themselves at
home for 14 days besides advising them to undergo treatment for the disease. Thereafter, he had filed
the reimbursement claim under the medical insurance policy with the respondent. The respondent
had stated that the claim was not within the scope of the policy. Unhappy with the rejection of the
claims, the complainant has approached this Forum to seek justice.
18) Cause of Complaint: Repudiation of claims made against the medical Insurance policy.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that the insurance policy he had
purchased from the respondent was exclusively a COVID policy. His entire family covered under the
policy had the symptoms of the disease on 10.05.2021 and had therefore approached a doctor at AIG
hospitals, Hyderabad. On the basis of this doctor’s advice, they had quarantined themselves at home for
the entire treatment period besides giving their blood samples for testing and monitoring their SPO2
levels, PR & temperature. These readings were noted in a note book maintained by them and was shown
to the treating doctor. The matter regarding home treatments taken by them was informed to the re-
spondent company on 16.05.2021. Luckily all the three could recover and avoid being admitted in hos-
pital. The reimbursement claim filed by him on 11.05.2021 was settled by the respondent. However,
the same was denied in respect of his son’s and wife’s treatment when he had filed their claim on
25.06.2021.
He has pleaded that the reimbursement claims pertaining to his son and wife ought to be allowed by
respondent as per the clause 1.2 of the policy. In this regard, he had submitted that all the sub clauses
were complied by her such as the medical practitioner’s advice to undergo treatment at home, continu-
ous active line of treatment which were monitored by him and the health status such as SPO2 levels,
PR, Temperature readings which was updated to the doctor for the entire period of home care treatment.
b) Insurer’s argument:
Self contained note was submitted by the respondent. They had issued a Corona Kavach Policy to
Mr.Kasina Madhusudhan Rao and his family (2 adults and 1 child), policy commencing from
13.04.2021 to 22.01.2022. The insured persons were diagnosed with Covid-19 and underwent home
quarantine. On perusal of the claim documents they observed that since they had no co morbidities,
were advised Home quarantine for 14 days and home rest. They had sent two query letters dated
03/07/2021 and 17/07/2021 seeking complete treatment records, vital, monitory charts, SPO2 levels but
they did not receive any response from the insured. Hence they sent a repudiation letter dated
23.07.2021 repudiating the claim. The insured persons were not hospitalized for Covid-19 and had un-
dergone only home quarantine which was not payable as per policy terms and conditions.
Award no:Hyd:IO:A:HI:0056:21-22
19) Reason for Registration of Complaint:
The insurer rejected the claims preferred by the complainant. As the complaint falls under Rule 13.1(b)
of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy
b. Rejection letter
c. Correspondence with insurer
d. Self contained note with enclosures.
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum both parties attended the online hearing at Hyderabad on
29.09.2021 .Both the parties reiterated their stand for and against the complaint.
The complainant stated that himself, his wife and his son were covered under one Corona Kavach Pol-
icy. All three of them were infected with Covid-19, and as per treating doctor’s advice they were treated
under Home quarantine. While his claim was settled by the insurance company, the claims pertaining
to that of his wife and son were rejected.
The respondent insurer have sent a mail on 29.09.2021 at 11.38 am, informing the Forum of having
reviewed the claims and agreed to settle as per the previous claim settled by them in respect of the
insured Mr.K.Madhusudhana Rao. Therefore, this Forum directs the respondent insurer to admit and
pay the claims as agreed in respect of Mr. Abhishek (son) for Rs.16,296/- and Mrs .K.Swarajya Lak-
shmi (spouse) for Rs. 18,974/- subject to the terms and conditions of the Policy .
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the parties
during the course of the personal hearing and the information/documents placed on record, the insurer
is directed to accept and settle the claims for Rs.16,296/- to Mr.Abhishek and Rs.18,974/- to
Mrs.K.Swarajya Lakshmi subject to terms and conditions of the policy.
The complaint is Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:
• According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
• According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as
specified in the regulations, framed under the Insurance Regulatory & Development Authority of
India Act from the date the claim ought to have been settled under the Regulations till the date of
payment of the amount awarded by the Ombudsman.
• According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 29th day of September , 2021.
(SURESH CHANDRA PANDA )
INSURANCE OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
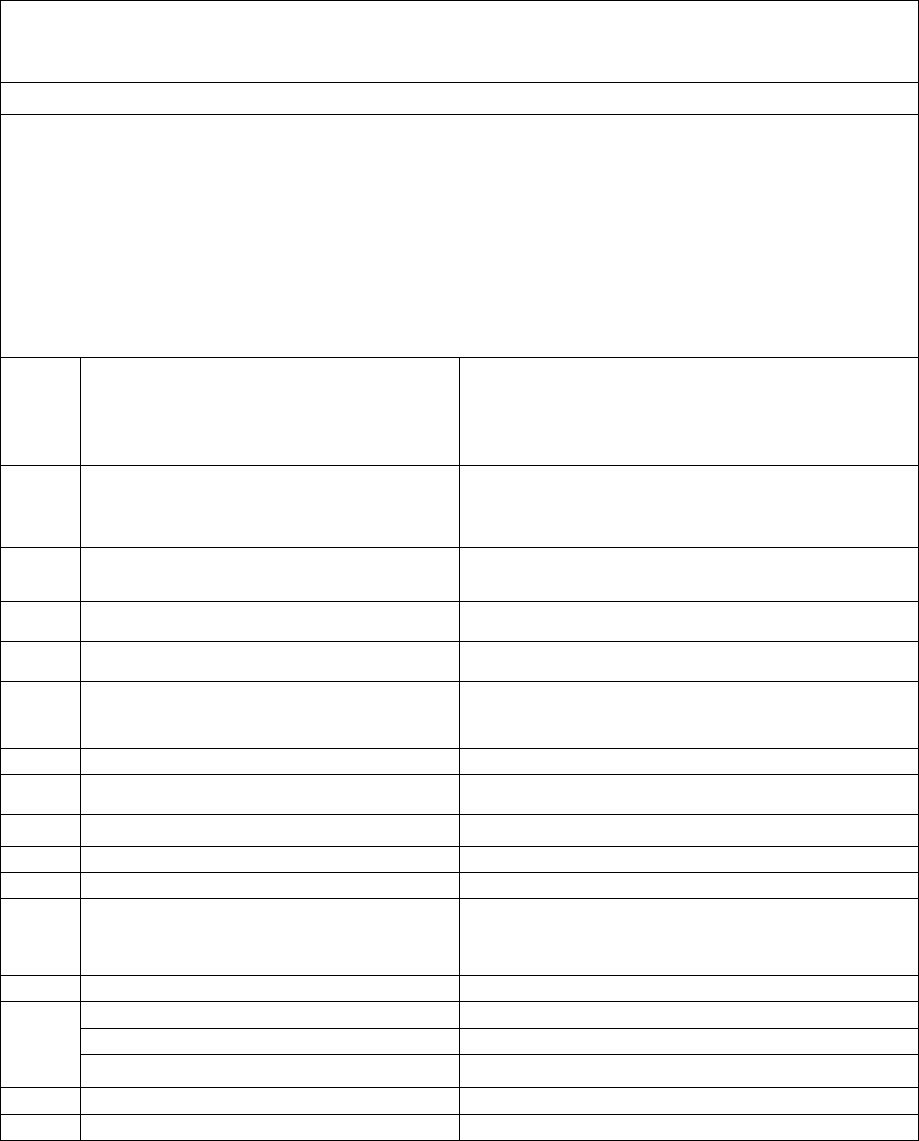
Award no:IO/Hyd/A/HI/21-
22/0057
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS
Case between: Mr. SAMUEL J PRASANNA KUMAR………………The Complainant
Vs
M/s HDFC ERGO General Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .018.2122.0307
Award No.: I.O.(HYD)/A/HI/ 0057 /2021-22
1.
Name & address of the complainant
Mr. S J Prasanna Kumar
Hazel H Sam C/o Mrs. Caroline,
K Rupert, P O Box 41,
Hyderabad,Telengana State- 500 004
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
130100/11051/AAO1339122
Easy health floater standard
12.03.2020 to 11.03.2021
3.
Name of the insured
Name of the Policyholder
Mr. Sammuel J Prasanna Kumar
Mrs. Hazel H Sam
4.
Name of the insurer
M/s HDFC ERGO Health Insurance Co. Ltd.
5.
Date of Repudiation
-----
6.
Reason for repudiation
Duration of pre-existing medical condition not
provided
7.
Date of receipt of the Complaint
06.09.2021
8.
Nature of complaint
Rejection of mediclaim
9.
Amount of Claim
Rs.10,30,099/-
10.
Date of Partial Settlement
----
11.
Amount of Relief sought
Rs.5 Lakhs being the Sum insured
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
29.09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.Aneesh Bhaskaran
15.
Complaint how disposed
Allowed
16.
Date of Order/Award
29.09.2021
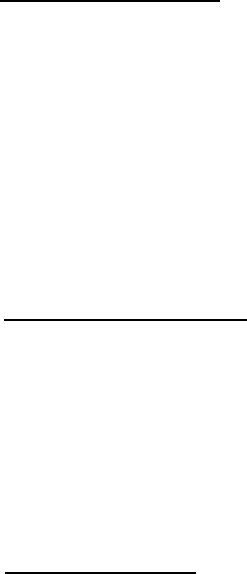
17) Brief Facts of the Case:
The complainant’s wife had renewed the annual medical insurance policy from the respondent and
during the policy renewal period, the complainant had been hospitalized in Apollo Hospitals to
undergo treatment for his E Coli infection of the spine. He had sought reimbursement of his
hospitalization cost for the treatment taken between 29.06.2020 -12.07.2020 at Apollo hospitals from
the respondent but the same was denied citing deficiency of requirements. Unhappy with the
pendency of his claim even after having made several correspondences with the respondent, the
complainant had therefore approached this Forum to seek justice.
18) Cause of Complaint: Denial of the claim made against the medical Insurance policy.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that he was covered under the
medical insurance policy purchased from the erstwhile Apollo Munich which was later taken over by
the respondent company. Prior to the existing policy, he had insured his health with M/s CIGNA TTK
Pro health insurer from 2016. In respect of the rejection of his claim, the complainant had stated that
the documents pertaining to the duration of his diabetes and Koch’s along with post consultation and
treatment records were submitted to the respondent’s office nearly on 3 occasions. However no action
was initiated by respondent.
b) Insurer’s argument:
The insurer sent a mail dated 24/09/2021 informing admissibility of the claim on further scrutiny of
the documents submitted. First policy inception date was 29.02.2016. The insured was detected with
DM in 2019 and since the diagnosis of the ailment falls under the policy period, they have considered
admitting the claim.
19) Reason for Registration of Complaint:
The insurer rejected the claim preferred by the complainant. As the complaint falls under Rule 13.1(b)
of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy
b. Rejection letter
c. Correspondence with insurer
d. consent mail dated 24.09.2021
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum both parties attended the online hearing at Hyderabad on
29.09.2021.
The complainant stated having been insured with Cigna TTK for 4 years commencing from 2016. He
had ported his policy with Apollo Munich from 2020-21 which is now called HDFC Ergo. His claim
for E Coli infection of the spine and hospitalization expenses of Rs.10,30,099/- billed by Apollo Hos-
pital, Hyderabad was denied on grounds of non-disclosure of pre-existing disease of Diabetes Mellitus.
The respondent insurer informed of having reviewed his claim and found that he was insured with them
since 2016 and since he was diagnosed with DM in 2019 which falls within the policy period, the claim
was admissible. As the hospital bill of Rs.10,30,099/- exceeds the sum insured under the policy , the
respondent insurer is directed to admit the claim upto the available sum insured under Easy Health
Floater standard Policy.
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the parties
during the course of the personal hearing and the information/documents placed on record, the insurer
is directed to pay upto the available sum insured under the policy.
The complaint is Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:
• According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
• According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as
specified in the regulations, framed under the Insurance Regulatory & Development Authority of
India Act from the date the claim ought to have been settled under the Regulations till the date of
payment of the amount awarded by the Ombudsman.
• According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 29
th
day of September , 2021.
(SURESH CHANDRA PANDA)
OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
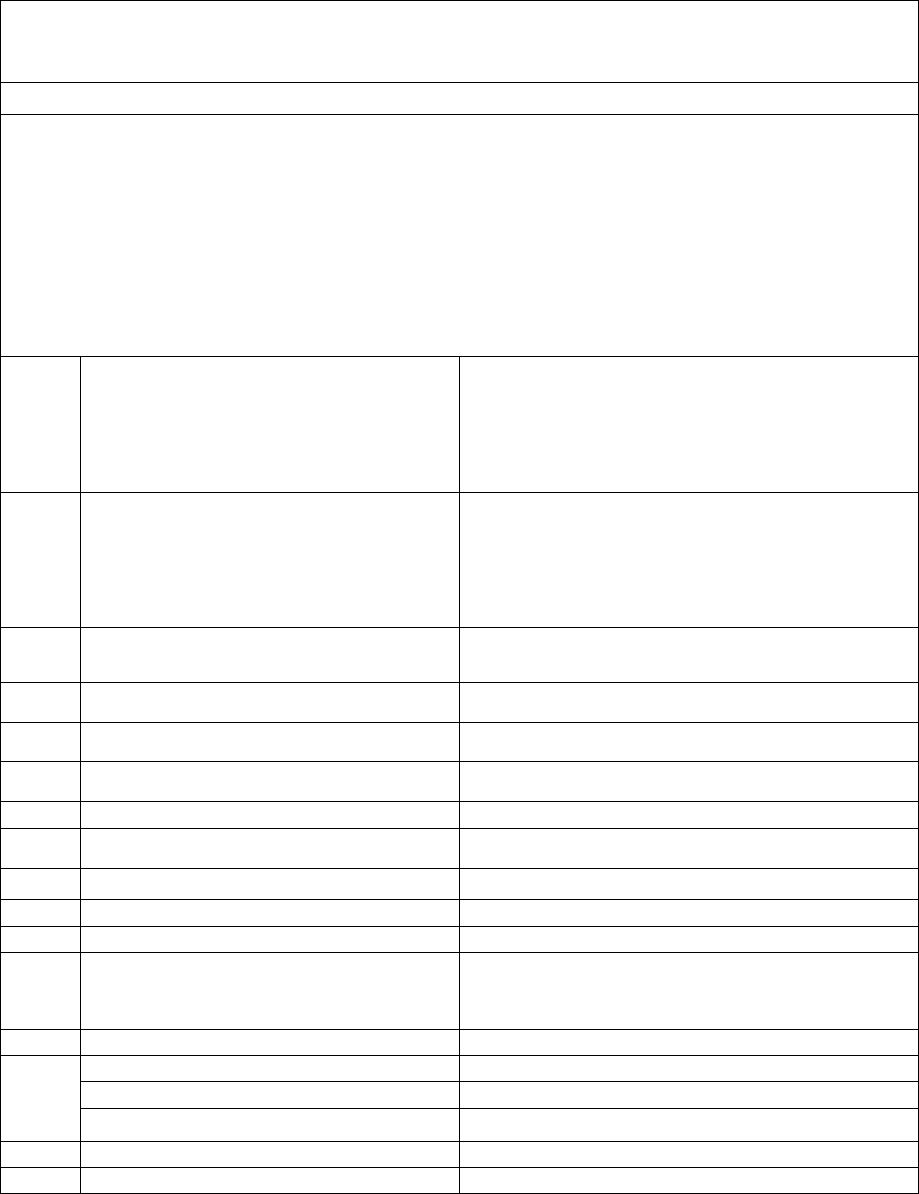
Award no:IO/Hyd/A/HI/21-
22/0058
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS
Case between: Mr. JITENDRA KUMAR VARMA ………………The Complainant
Vs
M/s HDFC ERGO General Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .018.2122.0306
Award No.: I.O.(HYD)/A/HI/ 0058 /2021-22
1.
Name & address of the complainant
Mr. Jitendra Kumar Varma
6-144, Sri Laxmi Homes, Laxmipur Village,
Malkapur Road,Karimnagar
Telangana- 505 451
(Cell No. 99853-84225)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
2825 2025 5233 5401 000
2866 1009 8273 4000 000
Health Suraksha Silver, Super top up
04.01.2021 to 03.01.2022
02.02.2021 to 01.02.2022.
3.
Name of the insured
Name of the Policyholder
Mr. Jitendra Kumar Varma
Mr. Jitendra Kumar Varma
4.
Name of the insurer
M/s HDFC ERGO General Insurance Co. Ltd.
5.
Date of Repudiation
22.02.2021
6.
Reason for repudiation
Claim falls outside the scope of policy
7.
Date of receipt of the Complaint
01.09.2021
8.
Nature of complaint
Denial of balance claim under super top up
9.
Amount of Claim
Rs. 11,32,442/-
10.
Date of Partial Settlement
28.03.2021, Rs.2,36,506/- paid
11.
Amount of Relief sought
Rs. 7,92,442/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
29.09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.Aneesh Bhaskaran
15.
Complaint how disposed
Dismissed
16.
Date of Order/Award
29.09.2021

17) Brief Facts of the Case:
The complainant had renewed his annual health Suraksha policy which was in the fourth year of the
policy period. He was hospitalized on 08.01.2021 due to epigastric abdominal pain. His claim was paid
under that policy. However, he was readmitted in the same hospital on two more occasions pertaining
to the same medical illness and the claim bills pertaining to the later two hospitalizations was denied
by the respondent citing policy exclusion clause sec E II ix of the policy. Aggrieved with the decision by
respondent which went against him, the complainant had therefore approached this Forum to seek
Justice.
18) Cause of Complaint: Repudiation of subsequent claims made against the medical Insurance policy.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that since he had never claimed
previously under the Health Suraksha policy, the respondent had given a cumulative bonus of Rs.
60,000/- under the policy. The claim that he had lodged was during its 3
rd
annual renewal. He was
admitted for the first time on 29.12.2020 at Kanpur medical college and after his discharge from the
hospital he had to admit himself in AIG Hospitals, Hyderabad as his medical condition persisted result-
ing in nausea and vomit associated with fever for the past 15 days. The hospitalization treatment cost
incurred during the period of his admission between 08.01.2021-20.01.2021 for an amount of
Rs. 3,40,000/- was approved by respondent for Rs. 2,36,506/-. Thereafter his health had deteriorated
and he was readmitted in AIG Hospitals, Hyderabad from 01.02.2021 to 04.02.2021 and from
04.02.2021 to 22.02.2021 wherein the hospital had charged him an amount of Rs. 3,68,624/- and
Rs. 4,23,818/- respectively for his treatment. Since the treatment costs soared high and as he was not
having the wherewithal to pay his hospital bills, the respondent was contacted by his brother to permit
refill of the entire sum insured along with cumulative bonus since the policy had such provision once
the sum insured got exhausted. He was initially given a cashless approval for Rs. 2,90,000/- as per the
refill sum insured but thereafter the same was withdrawn and his claim was repudiated on grounds of
his ailment falling outside the scope of insurance policy on the basis of the entire claim file that was
sought from him.
The complainant had contended that denial of his latter claim by respondent was unethical because the
treatment which he underwent was same and in continuation to the previous treatment underwent by
him on 29.12.2020 for which the respondent had approved and paid that claim. He had therefore ques-
tioned the respondent as to how they could adapt different grounds for settlement of his previous claim
and repudiation of his current claim. He had pleaded that he had ran into debts because of the respondent
who if they had denied his first claim, he would not have taken treatment in such corporate hospital and
incur huge debts. This act of respondent had not only put his family into debts but had also caused
mental and emotional trauma. He had also requested the forum that his brother be permitted to attend
the hearing since he was undergoing treatment in Govt. Civil hospital, Karimnagar and requested to
view his case sympathetically.
b) Insurer’s argument:
Self contained note was submitted by the respondent. They had issued Health suraksha family policy
on 14.12.2018 and renewed thereafter. The current policy commencing from 04.04.2021 to 03.01.2022
had a sum insured of Rs.5 Lakhs. The insured got hospitalized at Asian Institute of Gastroenterology
from 08/01/2021 to 20/01/2021 for Acute Pancreatitis with infected necrosis (unspecified). They had
settled the claim for Rs.2, 55,682/- against claimed amount of Rs.2, 69,212/- by way of NEFT on
28/03/2021. The insured got further admitted from 04/02/2021 to16/02/2021 at the same hospital and
for the same ailment. They observed from the ICP records dated 08/02/2021 that he was diagnosed with
Acute on chronic pancreatic (ethanol induced). The first cashless claim was paid as the company was
not aware of the Alcoholic pancreatitis. However, later when the medical documents during the second
admission clearly read out that it was alcoholic pancreatitis; it was evident that due to alcoholic lifestyle
he was getting admitted. Any treatment or admission due to alcoholism falls under exclusion of the
policy hence the claim was denied rightfully. With the above submission, they pleased for dismissal of
the complaint.
19) Reason for Registration of Complaint:
The insurer rejected the claim preferred by the complainant. As the complaint falls under Rule 13.1(b)
of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy
b. Rejection letter
c. Correspondence with insurer
d. Self contained note with enclosures.
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum both parties attended the online hearing at Hyderabad on
29.09.2021. Both the parties reiterated their stand for and against the complaint.
The complainant stated his first hospitalization at Kanpur Medical Collage for the same ailment was
settled by the insurance company while his second claim of hospitalization at AIG Hospital, Hyderabad
for relapse of the same ailment was denied.
The respondent insurer made their submission that cashless claim was approved by them for admission
at Kanpur medical collage based on the Discharge summary that diagnosed him with Acute pancreatitis
with infected necrosis( unspecified) . However during the current hospitalization the discharge sum-
mary showed he suffered from Acute on chronic pancreatic (ethanol induced). Since the policy perma-
nent exclusion under Section E (II) ( ix),excludes treatment of addictive conditions like alcoholism,
drug or substance abuse and consequences thereof , the claim was not payable.
Award no:IO/Hyd/A/HI/21-
22/0058
The Forum perused all the documents submitted and find that the complainant’s treatment for Acute
Chronic Pancreatitis was a consequence of alcohol intake and which falls under Permanent exclusion
Section E (II) ( ix) of the Policy . Hence this Forum does not see any need to interfere with the decision
of the respondent insuer.
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the parties
during the course of the personal hearing and the information/documents placed on record, the com-
plaint devoid of any merit is dismissed without costs.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:

• According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
• According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as
specified in the regulations, framed under the Insurance Regulatory & Development Authority of
India Act from the date the claim ought to have been settled under the Regulations till the date of
payment of the amount awarded by the Ombudsman.
• According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 29
th
day of September , 2021.
(SURESH CHANDRA PANDA)
OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
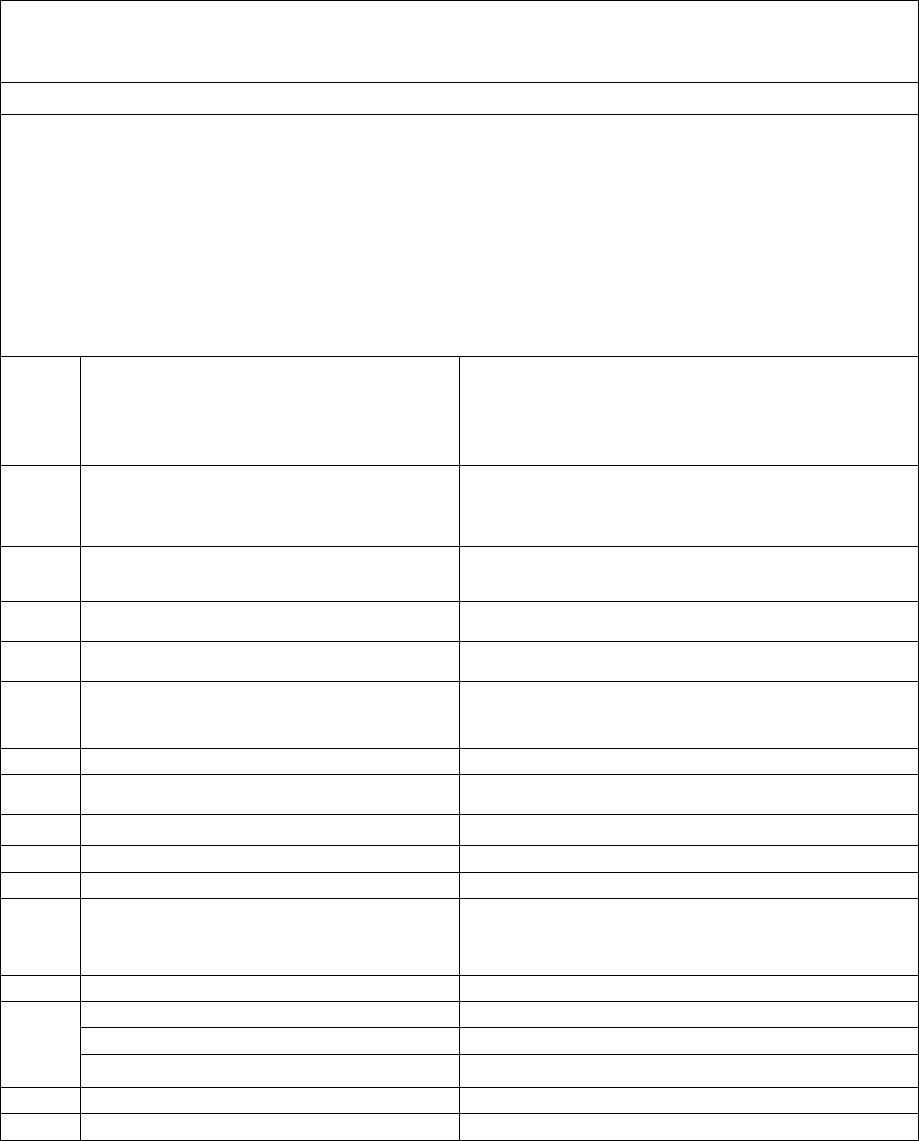
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS
Case between: Mr. Rajesh Doma ………………The Complainant
Vs
M/s MAX BUPA Health Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .031.2122.0314
Award No.: I.O.(HYD)/A/HI/ 0059 /2021-22
1.
Name & address of the complainant
Mr. Rajesh Doma
D. No. 16/136-A, Machavaram, Machilipatnam,
Krishna District,Andhra Prdesh- 521 002
(Cell No. 63048-41304)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
31214327202000
Health companion variant 2
09.06.2020 to 08.06.2021
3.
Name of the insured
Name of the Policyholder
Mr. Rajesh Doma
Mr. Rajesh Doma
4.
Name of the insurer
M/s MAX BUPA Health Insurance Co. Ltd.
5.
Date of Repudiation
-----
6.
Reason for repudiation
Claim paid partially as per the policy terms and
conditions
7.
Date of receipt of the Complaint
31.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 3,07,695/-
10.
Date of Partial Settlement
30.06.2021
11.
Amount of Relief sought
Rs. 78,145/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
29 .09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.Bhuwan Bhaskar
15.
Complaint how disposed
Allowed partially
16.
Date of Order/Award
29.09.2021
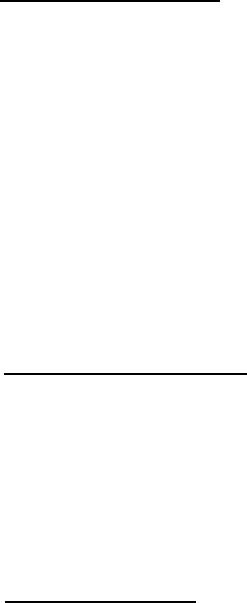
17) Brief Facts of the Case:
The complainant had purchased an annual medical insurance policy from the respondent company
wherein he had included his spouse, his daughter and him for a base sum insured of Rs. 5 Lakhs. On
18.05.2021, he was admitted to Niruja Rehabilitation and Nursing home to undergo treatment for his
final medical diagnosis of Viral Pneumonia which was secondary to SARS Cov-2. He was discharged
from the hospital on 23.05.2021. Subsequently, an amount of Rs. 3, 07,695/- was sought by him
towards the hospital expense he had incurred to which the respondent had processed his claim and
settled it for an amount of Rs. 78,145/-. Not happy with the reason given by respondent and their
Grievance team regarding the major portion of his claim having been disallowed, the complainant had
therefore approached this Forum to seek justice.
18) Cause of Complaint: Partial settlement of Mediclaim.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that he had applied for reimburse-
ment of his hospitalization expense on 26.05.2021 only after paying the same to hospital towards his
treatment for COVID-19. However, the respondent had settled his claim a month later for an amount of
Rs. 78,145/- as against the claim amount of Rs. 3,07,695/-. The reason given by the respondent towards
the disallowance of his balance claimed amount did not figure anywhere in the policy terms and condi-
tions as contended by the complainant.
b) Insurer’s argument:
Self contained note was submitted by the respondent. They received an online application form propos-
ing for health insurance policy from the insured. On the basis of declarations made they had issued
Health companion variant 2 policy commencing from 09.06.2020 to 08.06.2021 for a sum insured of
Rs.5 Lakhs. They had received a claim no bearing 673823 about hospitalization of the insured from
18.08.2021 to 23.05.2021 at Niruja Rehabilitation and nursing home where he was diagnosed with Viral
Pneumonia secondary to SARS COV-2. The claim was processed as per applicable ceiling rate for an
amount of Rs.78,145/- . With the above submission, they have requested for dismissal of the complaint.
19) Reason for Registration of Complaint:
The claim preferred by the complainant was rejected by the insurer. As the complaint falls under Rule
13(b) of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy with terms and conditions
b. Discharge summary
c. Correspondence with insurer
d. Self contained note with enclosures.
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum, both the parties attended the online hearing at Hyderabad
on 29.09.2021.
The complainant informed that out of the total hospitalization expenses of Rs.3,06,945/- , he received
only Rs.78,145/- . He is at a loss to understand why Telangana State Government ceiling rates are
applicable to his policy.
The respondent insurer informed that they had followed Telangana State Government ceiling rates for
covid patients and paid Rs.12,000/- per day for 6 days i.e, Rs.72,000/- and Rs.6145/- was paid towards
HRCT scan and remdesivir injection.
The Forum opined that as per IRDAI Covid-19 guidelines, State government ceiling rates for treatment
and cost incurred during hospitalization does not apply for insurance policies, where sum insured should
be taken as the ceiling limit. Therefore, the respondent insurer was asked to provide list of disallowed
items and it was provided over mail on 29.09.2021 at 12.30 PM, as follows:-
Total expenses incurred: Rs.3,06,945/-
Partial amount paid: Rs. 78,145/-
Amount reviewed for payment: Rs.1,65,882/-
Amount disallowed: Rs. 62,918/-
The Forum orders payment of an additional amount of Rs.28,178/- with respect to the following disal-
lowed in addition to the amount of Rs.1,65,882/ as agreed by the insurer over mail :
17. DMO charges: Rs.15000
18. Monitor charges: Rs.3000
19. Pulse oxymeter: Rs.5000
20. Safety consumable charges Rs.3000
21. Masks, cap, gloves: Rs. 2178
Total Rs.28,178/-
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the parties
during the course of the personal hearing and the information/documents placed on record, the insurer
is directed to pay an additional amount of Rs.1,94,060/- ( Rs.1,65,882+28,178), in settlement of the
claim.
The complaint is Partially Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:
• According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
• According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as
specified in the regulations, framed under the Insurance Regulatory & Development Authority of
India Act from the date the claim ought to have been settled under the Regulations till the date of
payment of the amount awarded by the Ombudsman.
• According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 29th day of September, 2021.
(SURESH CHANDRA PANDA)
INSURANCE OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Ombudsman - Shri. Suresh Chandra Panda, IAS
Case between: Mr. ARGAL MANMOHAN SINGH ………………The Complainant
Vs
M/s MAX BUPA Health Insurance Co. Ltd…………The Respondent
Complaint Ref. No. I.O.(HYD).H .031.2122.0303
Award No.: I.O.(HYD)/A/HI/ 0060 /2021-22
1.
Name & address of the complainant
Mr. Argal Manmohan Singh
H. No. 2-1-PC/108, Plot #10,
Panchami Colony,Sri Maremma Nagar, Yellamma
Bandla,Kukatpally,Hyderabad
Telengana State- 500 072
(Cell No. 79753-21693)
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
31403340202000
Family Floater
14.10.2020 to 13.10.2021
3.
Name of the insured
Name of the Policyholder
Mr. Argal Manmohan Singh
Mr. Argal Manmohan Singh
4.
Name of the insurer
M/s MAX Bupa Health Insurance Co. Ltd.
5.
Date of Repudiation
------
6.
Reason for repudiation
Partial settlement of Covid claim
7.
Date of receipt of the Complaint
23.08.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 3,20,475/-
10.
Date of Partial Settlement
03.07.2021
11.
Amount of Relief sought
Rs. 2,30,305/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation of
claims by the Life insurer, General Insurer or the
Health insurer
13.
Date of hearing/place
29.09.2021, online, Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr. Bhuwan Bhaskar
15.
Complaint how disposed
Allowed partially
16.
Date of Order/Award
29.09.2021
17) Brief Facts of the Case:
The complainant had purchased a medical insurance policy from respondent and had filed a
reimbursement claim towards the treatment taken by him for COVID in Ravi Hospitals. The respondent
had reimbursed only a fraction of his claim amount to him. Despite his request to respondent to settle
the balance claim amount, they had not responded to him in the affirmative. Disappointed with the
partial settlement of his claim, he had therefore approached this Forum to seek justice.
18) Cause of Complaint: Partial reimbursement of claim made against the medical Insurance policy.
a) Complainant’s argument:
In his letter addressed to this Forum, the complainant had submitted that although he was tested negative
for COVID-19 on 03.05.2021, he could not walk due to weakness and thereafter he was admitted in
Ravi Hospital, Hyderabad to undergo treatment after his HRCT test report confirmed positive for
COVID, and also because he had developed fever, head ache, cough and breathing problem. However
on submission of his claim bills, he was shocked to know that the respondent had settled his claim
amount for Rs. 90,170/- as against Rs. 320,475/- incurred by him towards his treatment. Despite his
correspondence to the respondent requesting them to reimburse his balance amount, they had not cred-
ited the same to his account.
b) Insurer’s argument:
Self contained note was submitted by the respondent. They received an online application form propos-
ing for health insurance policy from the insured. On the basis of declarations made they had issued
Family Floater health policy commencing from 14.10.2020 to 13.10.2021 for a sum insured of Rs.10
Lakhs. They had received a claim no bearing 678630 about hospitalization of the insured from
13.05.2021 to 18.05.2021 at Ravi Hospital, Hyderabad where he was diagnosed with Covid-19. Out of
the total claim amount of Rs.3,20,475/- they had approved an amount of Rs.90,170/- . The insured filed
a claim for disallowed amount .They had deducted Rs. 17,500/- towards room charges and paid
Rs.4000/- per day, Rs. 5,000/- towards nursing charges, Rs. 7,500/- towards duty doctor charges, Rs.
4,505/- out of Rs. 6,500/- towards HRCT charges, Rs. 37,500/- towards service charges, Rs. 1,24,300/-
towards hospitality services, Rs. 30,000/- ( Rs.18000+12000) towards doctors’ fees. Since the disal-
lowed items are not payable, they pleaded for dismissal of the complaint.
19) Reason for Registration of Complaint:
The claim preferred by the complainant was rejected by the insurer. As the complaint falls under Rule
13(b) of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy with terms and conditions
b. Discharge summary
c. Correspondence with insurer
d. Self contained note with enclosures.
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum, both the parties attended the online hearing at Hyderabad
on 29.09.2021.
The complainant informed that out of the total hospitalization expenses of Rs.3,20,475/- , he received
only Rs.90170/- . He is at a loss to understand why Telangana State Government ceiling rates are ap-
plicable to his policy.
The respondent insurer informed that they had followed Telangana State Government ceiling rates for
covid patients.
The Forum opined that as per IRDAI Covid-19 guidelines, State government ceiling rates for treatment
and cost incurred during hospitalization does not apply for insurance policies, where sum insured should
be taken as the ceiling limit. Therefore, the respondent insurer was asked to provide list of disallowed
items and it was provided over mail on 29.09.2021 at 12.30 PM, as follows:-
Total expenses incurred: Rs.3,20,475/-
Partial amount paid: Rs. 90,170/-
Amount reviewed for payment: Rs.1,86,965/-
Amount disallowed: Rs. 43,340/-
The Forum orders payment of an additional amount of Rs.26,240/- with respect to the following disal-
lowed in addition to the amount of Rs.1,86,965/ as agreed by the insurer over mail :
22. Masks, cap, gloves: Rs. 1240
23. Isolation charges Rs.15000
24. Fumigation charges Rs.10000
Total Rs.26240/-
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the parties
during the course of the personal hearing and the information/documents placed on record, the insurer
is directed to pay claim an additional amount of Rs.2,13,205/- ( Rs.1,86,965+26,240), in settlement of
the claim.
The complaint is Partially Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rules, 2017:
• According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
• According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as
specified in the regulations, framed under the Insurance Regulatory & Development Authority of
India Act from the date the claim ought to have been settled under the Regulations till the date of
payment of the amount awarded by the Ombudsman.
• According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 29th day of September, 2021.
(SURESH CHANDRA PANDA)
INSURANCE OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Amir Chand V/S The Oriental Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-050-2021-0744
1.
Name & Address of the Complainant
Shri Amir Chand
1879/7, Urban Estate, Karnal, Haryana-
132001
Mobile No.- 8708921600
2.
Policy No:
Type of Policy
Duration of policy/Policy period
261301/48/2021/695
PNB-Oriental Mediclaim Policy
08-02-2021 To 07-02-2022
3.
Name of the insured
Name of the policyholder
Amir Chand
Amir Chand
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
N.A
6.
Reason for repudiation
N.A
7.
Date of receipt of the Complaint
22-03-2021
8.
Nature of complaint
Enhancement of premium amount
9.
Amount of Claim
N.A
10.
Date of Partial Settlement
N.A
11.
Amount of relief sought
To set aside decision of enhancement of
premium amount.
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(c) – any dispute in regard to
premium paid or payable in terms of the
policy.
13.
Date of hearing/place
10.09.2021/Online hearing
14.
Representation at the hearing
For the Complainant
Shri Amir Chand, the complainant
For the insurer
Shri Sanjiv Kumar Madan, Sr. DM, DO,
Karnal
15.
Complaint how disposed
Award under Rule 17
16.
Date of Award/Order
10.09.2021
17) Brief Facts of the Case: Shri Amir Chand (hereinafter, the complainant) has filed this
complaint against The Oriental Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect
enhancement of premium.
21. Cause of Complaint:
a)Complainant’s argument: He purchased a mediclaim policy of the Oriental Insurance
Company Ltd. for Rs. 5,00,000/- in February 2017 considering it a good policy as the premium
of the policy was about Rs. 7,000 only. In February 2018 at the time of renewing this policy,
he paid a little more amount due to enforcement of GST. The insurance company renewed the
policy of the complainant with the premium amount of Rs.19587/-in February 2020, but this
year in 2021, the insurance company again enhanced the premium amount from Rs.19587/-

to Rs. 20567/- arbitrarily. He made so many requests verbally, on telephone and through mails
to different authorities of the insurance company to withdraw the decision of enhancing the
premium amount, but they told him that the company enhanced the premium amount under
the guidelines of IRDA, keeping into consideration of the cost of insurance products. The
company has not informed him that which clause of guidelines of IRDA and the cost of which
insurance products the company has taken into consideration at the time of increasing the
premium amount.
b) Insurers’ argument: As per SCN, the rates of premium, coverage etc. is fixed by the company
as per guidelines of IRDA and approval also obtained wherever required statutory. Premium
is based on cost factors of all type and the same are reviewed by appropriate competent
authorities from time to time and necessary modification in coverage and premium rates and
terms and conditions are made so as to keep the product viable for public as well as for the
company, which is PSU of Govt. of India. Sharp increase in Medical Cost, which resulted in high
ICR has led to increase in premium. The premium rates of Health Insurance products are
revised from time to time by the insurer in view of the support of experience data to back up
its future estimates. The factors involved in re-pricing of these products are morbidity, risk
margin, inflation, expenses etc. It is mandatory to maintain a solvency margin of 150% for
every insurer, irrespective of the amount of risks that the promoting entities of insurer carry
or the extent of liabilities that arise from the pricing of the insurance policies. Therefore, the
periodic review of the product pricing is necessary.
19. Reason for Registration of Complaint: Incorrect enhancement of premium.
20. The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant has filed complaint before this forum when his premium was enhanced from
Rs. 19587/- (2020-21) to Rs. 20567/- (2021-22) stating that the Insurers have enhanced the
premium without explaining to him the reasons for the same. However, ahead of the renewal
for 2021-22, he had lodged his protest with the Insurers, but still chose to pay the enhanced
premium to get his policy renewed. The Insurers had replied to him on 24.02.2021 by way of
email, explaining the reasons for enhancement of the premium.
In these circumstances, the Insurers cannot be faulted and the complaint shall deserve to be
rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules,2017)
Insurance Ombudsman - Shri Sudhir Krishna
Case of Tejinder Kaur V/S The Oriental Insurance Co. Ltd.
Complaint Ref. NO: CHD-H-050-2021-0761
1.
Name & Address of the Complainant
Smt. Tejinder Kaur W/o Shri Devinder Singh,
R/o H. No.- 1860, Sector-49 B, Nirwana
Society,
Chandigarh-160047
Mobile No.- 8847370136
2.
Policy No:
Type of Policy
Duration of policy/Policy period
231494/48/2020/122
Happy Family Floater
09-07-2019 To 08-07-2020
3.
Name of the insured
Name of the policyholder
Devinder Singh
Tejinder Kaur
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
06.12.2020
6.
Reason for repudiation
Not payable as per policy condition 4.8
7.
Date of receipt of the Complaint
26-03-2021
8.
Nature of complaint
Incorrect denial of mediclaim
9.
Amount of Claim
Rs.5,00,000/-
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
Rs.5,00,000/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total
repudiation of claims by an insurer
13.
Date of hearing/place
10.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Smt. Tejinder Kaur, the complainant
For the insurer
Shri Varun Goyal, Asst. Manager I/c, BC,
Suhana
15
Complaint how disposed
Award under Rule 17
16
Date of Award/Order
10.09.2021
17. Brief Facts of the Case: Smt. Tejinder Kaur (hereinafter, the complainant) has filed this
complaint against The Oriental Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect
denial of claim.
18. Cause of Complaint:
a) Complainant’s argument: Her husband Devinder Singh felt sick and was hospitalized on
20.05.2020. Complete history of the patient was mentioned in pre authorization form by
treating doctor and initial amount of Rs.153000/- was authorized by the TPA to the hospital
after complete scrutiny of documents and said history of the patient. On 06.06.2020 the
patient died and the hospital sent final bill for Rs.832882/-to TPA for approval before discharge
of the patient/body of the patient. Claim was denied along with already authorized amount
of Rs.153000/- causing complainant harassment at that time. The complainant submitted all
documents for reimbursement of claim to TPA for which they did not send any response. In
the first week of December, 2020, the complainant asked TPA about the status of the claim
and was shocked to know that claim had been rejected. The complainant lodged grievance
with the insurer and received reply wherein it was mentioned that the claim was repudiated
as per clause 4.8 of policy. There is nothing as such in the claim as per hospital record or death
summary given by the hospital that could attract clause 4.8 of the policy.
b) Insurers’ argument: As per SCN, the Patient late Sh. Davinder Singh 69 Y/M was admitted
at Max. Superspeciality Hospital, Mohali on 20.05.2020 with complaints of loose stools,
decreased urine output where he was diagnosed as a case of Septic shock with multiple organ
failure, GI bleed, Chronic liver disease, Enceplopathy -Hepatic /Metabolic/Septic and Urinary
tract infection. He had a history of CKD (3Yrs.)/CLD/HTN (15Yrs). Patient was on treatment for
CKD last two years with Dr. Manish Kumar Singla. Cashless facility was requested which was
processed as per policy terms and conditions. From the submitted documents, TPA had raised
query to hospital. As satisfactory reply is not received cashless facility was not processed and
insured is advised to come under reimbursement. Later on, insured had lodged
reimbursement claim for an amount of Rs.832881/- which was processed as per policy terms
and conditions and found to be non- admissible. As per received documents patient got
admitted in hospital with complaints of liver cirrhosis and ckd nephrotic Syndrome with past
treatment record h/o alcohol taken which is confirmed by health clinic hence case is not
admissible, as per clause 4.8 of the Policy. In view of the above, insurer issued repudiation
letter to insured vide letter dated 06.12.2020.
19) Reason for Registration of Complaint: Incorrect denial of claim
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
1. Result of Personal hearing with both parties(Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The deceased life assured (DLA) was hospitalized on 20.05.2020 and the Insurers (TPA) had
issued pre-authorization for an initial amount of Rs.153000 to the hospital. While continuing
with the treatment in the hospital, the DLA expired on 06.06.2020 and the hospital sent final
bill for Rs.832882 to the TPA for approval. The TPA raised query to hospital and upon not
getting satisfactory reply, withdrew the cashless facility and advised the Complainant to come
under reimbursement. Subsequently, the Complainant lodged reimbursement claim for an
amount of Rs.832881, which the Insurers repudiated citing Clause 4.8 of the Policy, which
excludes diseases due and/or use, misuse or abuse of drugs/alcohol.
The Indoor Case Paper on the date of admission to the hospital records the past history of the
DLA as HTN (15 years) and CKD (3 years) and was diagnosed for CKD/CLD/HTN. The
Death/Discharge Summary of the Hospital notes the cause of death as ‘Septic shock with
Multiple Organ Failure, GI Bleed, CLD, UTI, Acute on CKD”. The entire set of the hospital
records do not indicate that the DLA had any history of alcohol use, misuse or abuse or that
any of his ailments were owing to use, misuse or abuse of alcohol. Therefore, the repudiation
of the claim on the grounds of Clause 4.8 was not justified. Pursuantly, the Complaint deserves
to be allowed.
Award
The complaint is allowed and the Insurers are directed to admit and settle the claim
as per the terms and conditions of the policy within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Chetan Raina V/S The United India Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-051-2021-0734
1.
Name & Address of the Complainant
Shri Chetan Raina
405, Carnation Tower, Omaxe Green Valley,
Sector-41-42, Faridabad, Haryana- 121003
Mobile No.- 9891160674
2.
Policy No:
Type of Policy
Duration of policy/Policy period
0427002819P110691125
Individual Health Policy
27-11-2019 To 26-11-2020
3.
Name of the insured
Name of the policyholder
Chetan Raina
Chetan Raina
4.
Name of the insurer
The United India Insurance Co. Ltd.
5.
Date of Repudiation
20.03.2020
6.
Reason for repudiation
Dental treatment not covered
7.
Date of receipt of the Complaint
17-03-2021
8.
Nature of complaint
Repudiation of health claim
9.
Amount of Claim
Rs. 48613/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Actual expenses with interest
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claim by an insurer
13.
Date of hearing/place
17.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
1. Shri Chetan Raina, the complainant
2. Dr. Ramesh Raina, F/o the complainant
For the insurer
Dr. Rakesh Kapurapu, Admin. Officer, Delhi RO-1
15
Complaint how disposed
Recommendation under Rule 16
16
Date of Award/Order
17.09.2021
17. Brief Facts of the Case: Shri Chetan Raina (hereinafter, the Complainant), has filed this complaint
against the United India Insurance Co. Ltd. (hereinafter, the Insurers) for non-settlement of his health
claim.
18. Cause of Complaint:
a) Complainants argument: He had a mediclaim policy from United India Insurance Co. for more
than a decade. Because of severe bacterial infection of the throat, he had to be hospitalized in
QRG Hospital Faridabad in March 2020. Hospital raised a bill of Rs. 48613/- and it being a cashless
policy, all the relevant documents in original were submitted to the insurance company for
reimbursement to the hospital. The same however was denied to him without assigning a valid
reason. The case was submitted for reimbursement and after repeated reminders he was
informed that the claim could not be settled on the pretext of the infection being related to dental
treatment and its complication. He produced the letter of his treating hospital doctor saying that
the Bacterial infection of throat was neither related to dental extraction nor its complication. But
he failed to get the positive response from the company, so filed this complaint.
b) Insurers’ argument: As per SCN submitted by insurance company, a claim was reported to the
Heritage Health Insurance TPA Pvt. Ltd on 06.03.20, which was denied by TPA on 20.03.2020 due
to the reason, “Insured submitted claim of expenses incurred on the complications of tooth
extraction done on 29.02.2020. As per policy clause 4.9, dental treatment and its complication
are not covered in the policy.” Also the discharge summary of the hospital (QRG Medicare Ltd.)
dt. 09.03.2020 mention ‘presenting complaints : The Patient presented with complaints of pain
and swelling left side of Jaw for one week ad odynophagia with h/o tooth extraction on
29.02.2020’.
19. Reason for Registration of Complaint: Non-settlement of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion)
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers inform that the Complainant has approached this forum without
approaching their Grievance Portal and has also not submitted some of the documents to them
that he has submitted to this forum. Having said that, the Insurers offer to review the claim, if the
Complainant submits all the relevant documents to them on their Grievance Portal. The
Complainant accepts this offer. Thus an agreement of conciliation could be arrived at between
the Complainant and the Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Complainant shall submit all the relevant documents
to the Insurers on their Grievance Portal and the Insurers shall review the claim as per the terms and
conditions of the policy.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 17, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Harpreet Singh Kapoor V/S HDFC ERGO General Insurance Co. Ltd
Complaint Ref. No.: CHD-H-018-2021-0743
1.
Name & Address of the Complainant
Shri Harpreet Singh Kapoor
# 8, Corner View Colony, Near Walia Hospital,
G.D.N.S. Road, Patiala, Punjab- 147001
Mobile No.- 9815985957
2.
Policy No:
Type of Policy
Duration of policy/Policy period
160100/11228/AX00068549-03
Health Individual
09-08-2020 To 08-08-2021
3.
Name of the insured
Name of the policyholder
Harpreet Singh Kapoor
Harpreet Singh Kapoor
4.
Name of the insurer
HDFC ERGO General Insurance Co. Ltd.
5.
Date of Repudiation
18.02.2021
6.
Reason for repudiation
Due to non-disclosure and concealment of facts
7.
Date of receipt of the Complaint
22-03-2021
8.
Nature of complaint
Incorrect denial of claim
9.
Amount of Claim
Rs. 373383/- + Rs.63698/- = Rs. 437081/-
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
Rs. 373383/- + Rs.63698/- = Rs. 437081/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of claims
by an insurer
13.
Date of hearing/place
17.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Harpreet Singh Kapoor, the complainant
For the insurer
Shri Manoj Prajapati, Manager (Corporate Legal)
15
Complaint how disposed
Award under Rule 17
16
Date of Award/Order
17.09.2021
17. Brief Facts of the Case: Shri Harpreet Singh Kapoor (hereinafter, the complainant) has filed this
complaint against HDFC ERGO General Insurance Co. Ltd. (hereinafter, the insurers) alleging
incorrect denial of claim.
18. Cause of Complaint:
a) Complainant’s argument: He was admitted for his Left Leg- DVT in Fortis Hospital Mohali and
prior to his operation, pre-authorization cashless claim was denied by the insurance company.
He filed a reimbursement claim on 9
th
&10
th
January, 2021. He kept on providing the documents
and fulfilled all their formalities continuously even in his unwell physical condition in the hope
of claim reimbursement. But regretfully after getting all the hospital record and personal details,
they rejected both the health claims on the same ground as they rejected his pre auth cashless
claim. After completing 36 months of this health policy, they rejected claim at the time of
emergency need. The complainant is seeking the intervention of this forum as the grievance cell
of the company also repudiated this claim .
b) Insurers’ argument: As per SCN, insurers received a re-imbursement claim for admission of the
Policyholder/Insured, to Fortis Hospital with the date of admission being 19.12.2020 and date
of discharge 23.12.2020 with claim amount of Rs. 3,73,383/- for the diagnosis of Left Leg DVT
and Left Leg Mechanical Thrombectomy-Venous Done on 19.12.2020. After reviewing the
submitted documents it was noted that Complainant had history of DVT since 2009, which was
not disclosed by him in Proposal form. In view of the non-disclosure of the said grave material
fact by the Policyholder in the proposal form, the claim was rejected vide repudiation letter
dated 18.02.2021. The Complainant had also submitted his pre & post claim of Rs. 63,698/-,
which was also rejected by the respondent company for the same reason.
19. Reason for Registration of Complaint: Denial of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant accepts that he had the PED of deep vein thrombosis (DVT) while taking the
subject policy and states that he had disclosed it to the Axis Bank staff, who had sold the policy
to him, and they ought to have recorded the same in the Policy suitably. He also states that such
PEDs are to be excluded only for up to 4 years. The Insurers state that exclusion becomes
operative only if the PED is disclosed, else, non-disclosure clause would apply.
It is a settled principle that the person buying a policy has to ensure that all details about her/him
are duly reflected in the Policy and upon receipt of the policy, s/he should locate errors and
omissions, if any, and either ask for corrections or seek cancellation of the policy within the free-
look period, if s/he is dissatisfied about any terms or details of the policy.
In these circumstances, it is concluded that the Complainant had not disclosed the material
information of his past medical history while seeking to buy the subject policy. Therefore, the
Insurers were justified in repudiating the claim. Pursuantly, the complaint would deserve to be
rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 17, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Shri Rambir Singh V/S Star Health and Allied Insurance Co. Ltd.
Complaint Ref No.: CHD-H-044-2021-0696
1.
Name & Address of the Complainant
Shri Rambir Singh
House No. 224, Lane-9, Shiv Enclave Part -I Ismailpur,
Faridabad ,Haryana-121003;
Mob. 9650343S03, 9871203746, 9654321046,
8384069796
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/161121/01/2021/013627
Family Health Optima Insurance Plan
13-10-2020 to 12-10-2021
3.
Name of the insured
Name of the policyholder
Rambir Singh
Rambir Singh
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
11-02-2021
6.
Reason for repudiation
Non- disclosure of PED
7.
Date of receipt of the Complaint
08-03-2021
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs 1,70,000/- as per complaint
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs 1,70,000/- as per complaint
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of claims
by an insurer
13.
Date of hearing/place
17.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Rambir Singh, Complainant
For the insurer
Smt Mamta Gupta, Chief Manager (Claims)
15
Complaint how disposed
Award under Rule 17
16
Date of Award/Order
19.09.2021
17. Brief Facts of the Case: Shri Rambir Singh (hereinafter, the Complainant) has filed this complaint
against Star Health and Allied Insurance Co. Ltd. (hereinafter, the Insurers) for wrongly repudiating
his health claim.
18. Cause of Complaint:
1. Complainant’s argument: He is a poor person aged 60 years retired as a Bus Driver from DTC in
December 2020. He had a health insurance with United India, which was ported to Star Health
in October 2020. He felt some health problem in 07
th
January 2021 and got admitted to Metro
Hospital, Faridabad. As advised by the health experts, treatment was done and it was informed
by Metro Hospital to Star Health and accordingly one TPA visited the hospital and took note of
the patient and also from Hospital. On 9th January 202l, when Hospital asked Star Health to
reimburse the payment, Star Health insurance denied to make the payment and Hospital was
not able to discharge him without payment and also threatened to cancel the policy if any pay-
ment is demanded. In such pathetic condition his family with great difficulty managed to arrange
payment around Rs. 170000/- to hospital. He also pointed that he has have not taken any pre-
vious claims from his previous Insurance company and just after switching to Star Health Policy.
Seeing his health and financial condition, he has requested this forum to kindly instruct Star
Health insurance to reimburse his claim with interest and penalty applicable for denial mode of
payment.
2. Insurers’ argument: The Insurers have stated that the Complainant took the subject policy for
the period 13/10/2020 to 12/10/2021 by way of porting from The United India Insurance Co.
Ltd. He reported the claim of Rs. 1,70,000 in the 1st year after porting the Policy. As per com-
plaint, he was admitted on 07/01/2021 at Metro Heart Institute- Faridabad and discharged on
09/01/2021. As per Discharge Summary from the treating hospital, the insured was diagnosed
with Acute Coronary Syndrome, Coronary Artery (Significant Single Vessel) Disease, LV Dysfunc-
tion (LVEF=45%) and Hypertension. The Insured raised pre-authorization request to avail cash-
less facility and the same was rejected vide letter dated 09/01/2021. On scrutiny of claim docu-
ments, it was observed from the Inpatient History & Physical Examination Record that the com-
plainant was a known case of Coronary Artery Disease for the past 5 years and undergone PTCA
(Percutaneous Transluminal Coronary Angioplasty) procedure 5 years ago. This pre-existing dis-
ease was not disclosed in the proposal for porting by the insured. Hence, the right of the Insurer

to evaluate the risk prior to accepting the proposal was deprived, consequently, the cashless
request was rejected vide letter dated 09/01/2021. Since, the insured has not disclosed the
above mentioned pre-existing disease / condition in the proposal form at the time of inception
of the policy; Treatment of diseases related to Cardio Vascular System is incorporated in the
Insured’s policy as pre existing disease/condition by passing endorsement on 11/01/2021. As
per Condition No. 6 of the policy, “Disclosure to information norms: The policy shall become
void and all premiums paid thereon shall be forfeited to the Company, in the event of mis-rep-
resentation, mis description or non-disclosure of any material fact by the policy holder.” Hence,
the claim was repudiated and communicated to the insured vide letter dated 11/02/2021.
19. Reason for Registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The subject Policy was ported to the Insurers on 13.10.2020. The Complainant filed the subject
claim within the first year of the ported policy. Upon investigation into the Claim, the Insurers
discovered documents that indicated that the Complainant was a known case of Coronary Artery
Disease for the past 5 years and had undergone PTCA (Percutaneous Transluminal Coronary
Angioplasty) procedure 5 years ago, which he had not disclosed in the proposal for porting. The
Complainant states that he had signed on blank proposal form. It is, however, a settled principle
that the person signing a proposal form is responsible for all the entries made for him. Therefore,
it is concluded that the Complainant had not disclosed the material information relating to his
past medical history in the proposal form for porting the policy. Pursuantly, the Insurers were
justified in repudiating the claim and the complaint would deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 19, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Sansar Singh Sirohi V/S The Oriental Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-050-2021-0739
1.
Name & Address of the Complainant
Shri Sansar Singh Sirohi
# 199-A, Sector-4, Mansa Devi Complex,
Panchkula, Haryana-0
Mobile No.- 8288024126
2.
Policy No:
Type of Policy
Duration of policy/Policy period
231102/48/2020/792
Mediclaim Policy
16-03-2020 To 15-03-2021
3.
Name of the insured
Name of the policyholder
Sansar Singh Sirohi
Sansar Singh Sirohi
4.
Name of the insurer
The Oriental General Insurance Co. Ltd.
5.
Date of Repudiation
N. A
6.
Reason for repudiation
N. A
7.
Date of receipt of the Complaint
18-03-2021
8.
Nature of complaint
Settlement of claim for an inadequate amount.
9.
Amount of Claim
Rs. 130156/-
10.
Date of Partial Settlement
-
11.
Amount of relief sought
Rs. 61000/- plus interest @5%
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claims by an insurer
13.
Date of hearing/place
17.09.2021/Online hearing
14.
Representation at the hearing
For the Complainant
Shri Sansar Singh Sirohi, the complainant
For the insurer
Shri Jaspal Rai, Manager, DO-1, Chandigarh
15
Complaint how disposed
Award under Rule 17
16
Date of Award/Order
17.09.2021
17. Brief Facts of the Case:
Shri Sansar Singh Sirohi (hereinafter, the complainant) has filed this complaint against The
Oriental Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect settlement of claim.
18. Cause of Complaint:
a) Complainant’s argument: His hospitalization expenses bills including Pre & Post hospitalization
amounting to Rs.1,30,156/- was settled by insurers for Rs.55635/- after deducting Rs. 61917/-
from the claimed amount, wherein the following deductions are quite unjustified:
Expense Head Deducted Amt. Remarks
1. Surgeon Fee 20,600/- Room Rent capping, Reasonable & Custom-
ary
2. Surgery Charges 14,800/- -do-
3. Bed Charges 8,000/- Not Justified
4. OT Charges 15,600/- Non payable
5. RMO Charges 2000/- -do-
b) Insurers’ argument: As per SCN, complainant submitted two medical bills of Rs.127604/- &
Rs.10800/- for treatment of complex anal fistula with Hemorrhoids for admission from
16.05.2020 to 19.05.2020 and dressing for the period 20.05.2020 to 06.06.2020 @300/- per
dressing. Accordingly, Raksha Health Insurance TPA Pvt. Ltd. settled both the bills for amount
Rs.57993/-. The details of payments as per claim settlement vouchers are as under:
Claim No. Claimed Amount Deductions Paid Amount
55652021029956 Rs. 127,604/- Rs.69611/- Rs.57993/-
55652021172223 Rs. 10800/- Rs.6900/- Rs.3900/-
Claim no.55652021029956 was paid for Rs.57993/-. In case where the treatment or the
surgery is in non PPN Hospitals & non-PPN city, the amount is restricted in accordance to
customary and reasonable expenses in that particular city. The procedure charges of
Rs.115000/- are too much in excess of the reasonable and customary expenses for
Fissurectomy. It is more than twice of package of hospitals like Amcare. Claims were paid as
per rates of Amcare hospital, Zirakpur according to clause 2.37 of the policy terms & conditions
related with Reasonable and Customary charges. Any expenses other than the above have to
be borne by the insured himself. The amount of treatment in other hospitals is also same
against the surgery of Fissurectomy . Further claim no.55652021172223 was paid for Rs.3900/-
after deduction of Rs.6900/- from dressing charges, as only one dressing is done in a day. The
deductions have been made as per clause 2.37 of the policy terms and conditions.
19. Reason for Registration of Complaint: Incorrect settlement of claim
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion)
Case called. Parties are present and recall their arguments as noted in Para 18 above. The
Complainant had undertaken treatment in a Non-network Hospital. The Complainant states
that he had adopted this hospital as the treating doctor in the hospital was the best known in
his field of specialization. The Insurers state that that they have settled the claim as per the
“Reasonable & Customary charges”, for which purpose, they examined the rates approved for
4 network hospitals in the vicinity and adopted the PPN rates for Amcare Hospital, Zirakpur,
for which the rate was the highest of all the 4 hospitals, and Amcare being a 110-bed hospital,
was bigger than the hospital where the Complainant had taken the treatment. Upon
examination of the arguments and the evidence submitted by both the parties, it is concluded
that the Insurers were justified in adopting the rates applicable for Amcare Hospital as
mentioned above, according to clause 2.37 of the policy terms & conditions relating to
Reasonable and Customary charges. Pursuantly, the complaint would deserve to be rejected.

Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 17, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Aman Goel V/S HDFC ERGO General Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-018-2021-0718
1.
Name & Address of the Complainant
Shri Aman Goel
C/o Main Bazar, Charkhi Dadri, Haryana-127306
Mobile No.- 9991465321
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2828100842204100000
Health Policy
24-08-2020 To 23-08-2021
3.
Name of the insured
Name of the policyholder
Aman Goel
Aman Goel
4.
Name of the insurer
HDFC ERGO General Insurance Co. Ltd.
5.
Date of Repudiation
31.01.2021
6.
Reason for repudiation
Misrepresentation
7.
Date of receipt of the Complaint
16-03-2021
8.
Nature of complaint
Rejection of mediclaim
9.
Amount of Claim
Rs.90536/-
10.
Date of Partial Settlement
N.A
11.
Amount of relief sought
Claim amount
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claims by an insurer
13.
Date of hearing/place
24.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Aman Goel, the complainant
For the insurer
Ms Shweta Pokhriyal, Manager (Legal)
15.
Complaint how disposed
Award under Rule 17
16.
Date of Award/Order
24.09.2021
17. Brief Facts of the Case: Shri Aman Goel (hereinafter, the complainant) has filed this complaint
against HDFC ERGO General Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect denial
of claim.
18. Cause of Complaint:
a) Complainant’s argument: The information and documents submitted by him are correct and no
fact has been concealed. The insurance company’s allegation of some misstatement in the claim
is incorrect. He is not aware about the facts placed before the insurer by their investigator. But
he has not concealed any fact in the information provided to the investigator. The denial of his
claim and suspension of policy is totally wrong.
b) Insurers’ argument: As per SCN, the insured was admitted in Life Care Multispecialty Hospital
from 24.12.2020 to 29.12.2020 and was diagnosed with AFI with UTI with Severe Dehydration.
After receiving the claim, an independent investigator was appointed in order to verify the
genuineness and veracity of the facts. During the investigation, the following observations were
made:
1. As per the discharge summary, insured was presented with complainant of high-grade fever
with chills and rigor, repeated vomiting, not accepting orally, pain in abdomen, burning mictu-
rition, increased frequency of urine since 2 days. However, as per statement of the complain-
ant, he had gone to Dadri to attend a function where he felt unwell and was admitted in the
hospital. This shows that there is manipulation of the history of the insured. Treating Doctor,
Dr.Bajrang is a 76 years old person and is never found inside hospital while the investigator has
visited this hospital many times in last 2 years, hence treating doctor confirmation could not
be collected.
2. The entire treatment record of the complainant comprising initial assessment sheet, daily pro-
gress notes and the vital and treatment chart is recorded in one handwriting irrespective of
the time of entry, which means that the person recoding is on duty 24 hours in the hospital,
which is highly unlikely.
3. Further, 2 different signatures have been observed in vital and medication chart but against
the same handwriting, which means that there is an attempt to misrepresent the facts.
4. Till 4 days continuously 12 injections PCM along with Piprat was given but in vital chart fever
is persistent above the 101*F, it means 12 injections are ineffective and PCM was not working,
which is not possible as doctor is prescribing this in acute febrile illness.
It is clear from the above submissions that complainant misrepresented the material facts to
insurers in order to extract money and therefore his claim was repudiated vide letter dated
31.01.2021.
19. Reason for Registration of Complaint: Incorrect denial of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
I have examined the arguments and the evidence submitted by the Complainant and the Insurers.
In view of the multiple discrepancies observed in the claim documents as narrated in Para 18b
above, the Insurers were justified in repudiating the claim. Pursuantly, the complaint shall deserve
to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 24, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Bhupender Singh V/S Manipal Cigna Health Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-053-2021-0738
1.
Name & Address of the
Complainant
Shri Bhupender Singh
S/o Shri Virender Singh, V.P.O.- Budha Khera, Teh.-
Safidon, Distt.- Jind, Haryana- 126113
Mobile No.- 9813855985
2.
Policy No:
Type of Policy
Duration of policy/Policy period
PROHLN200032455
Health Policy
19-03-2020 To 18-03-2021
3.
Name of the insured
Name of the policyholder
Virender Singh
Virender Singh
4.
Name of the insurer
Manipal Cigna Health Insurance Co. Ltd.
5.
Date of Repudiation
14.01.2021
6.
Reason for repudiation
Non-submission of requirements
7.
Date of receipt of the Complaint
18-03-2021
8.
Nature of complaint
Rejection of mediclaim
9.
Amount of Claim
Rs. 22305/-
10.
Date of Partial Settlement
N. A
11.
Amount of relief sought
Claim amount
12.
Complaint registered under Rule
no.: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation of
claims by an insurer
13.
Date of hearing/place
24.09.2021/Online hearing
14.
Representation at the hearing
For the Complainant
1. Shri Bhupinder Singh, the Complainant
2. Shri Virender Singh, F/o the Complainant &
Policyholder
For the insurer
Ms Shweta Nair, Deputy Manager (Legal)
15
Complaint how disposed
Recommendation under Rule 16
16
Date of Award/Order
24.09.2021
17. Brief Facts of the Case: Shri Bhupender Singh (hereinafter, the complainant) has filed this complaint

against Manipal Cigna Health Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect
rejection of claim of his father Shri Virender Singh.
18. Cause of Complaint:
a) Complainant’s argument: His father while getting down from the stairs got slipped on the morning
of 05.11.2020 which caused injury to his left hand. Thereafter, the patient was taken to hospital and
doctor on seeing X-ray talked about the bone fracture and operated in emergency. After getting
discharged from the hospital on 09.11.2020, complainant submitted all papers and bills through
post on 19.11.2020 and remaining papers on 14.12.2020 as demanded by company. On 18.12.2020,
the complainant received a phone call from Manipal Cigna Insurance Company and was asked to
file written report of accident on what’s app and its hardcopy would be collected later on. He also
informed that investigation would also be conducted in the hospital. But thereafter, he neither made
any phone-call nor collected the papers. Thereafter, the company demanded the papers time and
again and all the papers have been submitted to the company. After this he lodged complainant
with IRDAI. But even after that the insurance company cancelled the claim due to non-completion
of documents. The complainant is seeking intervention of this forum for payment of their claim.
b) Insurers’ argument: As per SCN, the reimbursement claim was rejected vide letter dated 14
th
January, 2021 as they did not receive the additional information from complainant sought through
letters dated 30 Nov2020, 11 Dec 2020, 22 Dec 2020 & 02 Jan 2021, hence the decision on
admissibility of claim could not be taken. As per policy definition no VII.6 b if the deficiency in the
necessary claim documents is not met or are partially met in 10 working days of the first intimation,
we shall remind you of the same and every 10 days thereafter. We will send a maximum of three
reminders. This claim stands repudiated and the same was intimated to the complainant. The
complainant approached the grievance cell requesting reconsideration of the company’s decision
as regards the claim. After due evaluation of the request, the company again through the email
dated 11
th
January 2021, 31
st
January 2021 and 10
th
March 2021 stated that claim was rejected for
non-submission of documents and further requested the complainant to submit the said documents
for reconsideration of the claim. However, the complainant chose not to submit the said documents.
19. Reason for Registration of Complaint: Incorrect settlement of claim
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage the Insurers offer to review the claim after examining the documents, within 30 days.
The Complainant accepts this offer. Thus an agreement of conciliation could be arrived at between
the Complainant and the insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the insurers. Accordingly, the Insurers shall review the claim after examining the
documents, within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 24, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Ritu Sharma V/S The United India Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-051-2122-0001
1.
Name & Address of the Complainant
Smt. Ritu Sharma
68-B, Sant Sunder Singh Nagar,
Dubri- Dhandra Road, Ludhiana, Punjab-141116
Mobile No.- 9877430154
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2007002818P102104980 &
2007002819P101838492
Medicare policy
05-05-2019 To 04-05-2020
3.
Name of the insured
Name of the policyholder
Ritu Sharma
Ritu Sharma
4.
Name of the insurer
The United India Insurance Co. Ltd.
5.
Date of Repudiation
22.10.20
6.
Reason for repudiation
Hospitalization less then 24 hrs.
7.
Date of receipt of the Complaint
31-03-2021
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.214229/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs. 214229/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation
of claim by an insurer
13.
Date of hearing/place
24.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Smt. Ritu Sharma, the complainant
For the insurer
Shri Jugesh Sikka, Sr. Assistant (Legal)
15.
Complaint how disposed
Award under Rule 17
16.
Date of Award/Order
24.09.2021
17. Brief Facts of the case: Smt. Ritu Sharma (hereinafter, the Complainant), has filed this
complaint against the United India Insurance Co. Ltd. (hereinafter, the insurers) for non-
settlement of her health claim.
18. Cause of Complaint:
a) Complainant’s argument: She has purchased policy no. 2007002818P102104980 and
2007002819P101838492 from United India Insurance Co. Ltd. Under these policies, she claimed
for her cancer treatment. Few of these claims are still pending. Her claims for reimbursement
were rejected by TPA on the basis of flimsy ground. She requested for relief in the matter.
b) Insurers’ argument: As per SCN submitted by insurance company, the insured Smt. Ritu
Sharma had lodged the claim in policy no. 2007002819P101838492. The TPA duly registered,
entertained, and processed the claim as per the terms and conditions of the policy. The
insured was called upon to submit the documents and after receipt of the documents, the TPA
recommended to repudiate the claim on the ground: Claim reported for CA breast (LT)
PT1NOM0, Inj. Herceptin Given. This injection is an adjuvant Biological/Immunological
therapy and does not fall under the scope of the policy. Patient had taken treatment on OPD
basis, whereas minimum 24 hours hospitalization is required. Hence claim recommended for
repudiation under 3.14." After receipt of the claim file, the competent authority of the
company duly scrutinized file in terms of the policy and found that claim is not payable and
accordingly claim of the insured was repudiated as per clause 3.15 (Hospitalization), 2.1B
(requirement of 24 hrs hospitalization) and 4.15 (related with experimental/unproven
treatment) of the policy.
19. Reason for Registration of Complaint: Repudiation of health claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of hearing with the parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The claim relates to the administration of Inj. Herceptin to the Complainant on Day care basis.
The Insurers had repudiated the claim citing the provisions of the policy relating to Hospitalization,
Requirement of 24 hrs hospitalization, and Experimental/unproven treatment. In the instant case,
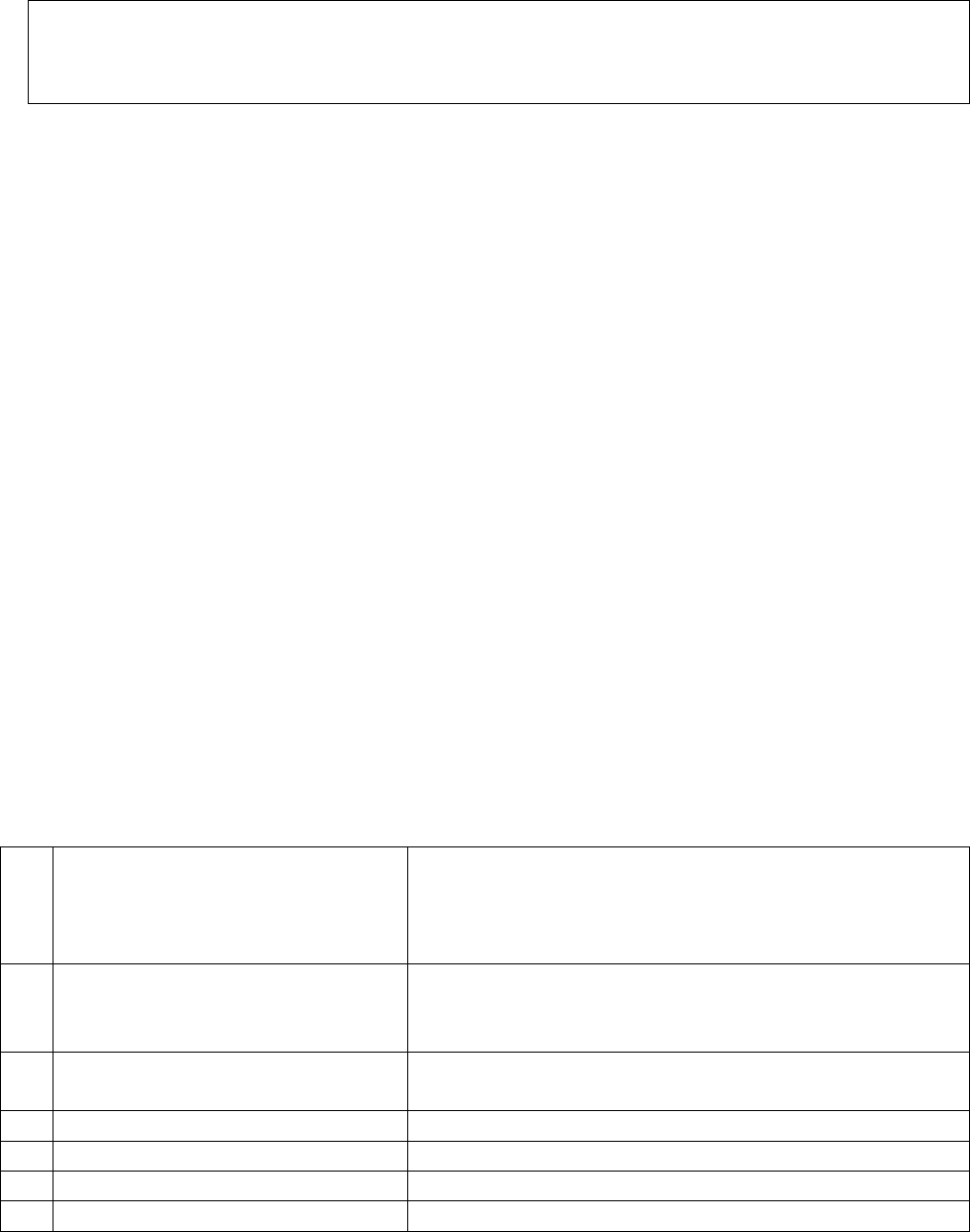
there was no hospitalization over 24 hours and this day care treatment is not included in the list
of day care treatments admissible for claim under the subject policy. Therefore, the Insurers were
justified in repudiating the claim and, pursuantly, the complaint shall deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 24, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Sanjay Gupta v/s Bajaj Allianz General Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-005-2021-0754
1.
Name & Address of the
Complainant
Shri Sanjay Gupta
# 46/D, New Kitchlu Nagar, Opp. Stan Auto Lane,
Hambra Road, Ludhiana, Punjab-141008
Mobile No. 9356771421
2.
Policy No:
Type of Policy
Duration of policy/Policy period
OG-20-3016-8430-00000046
Health Guard Policy
14-03-2020 to 13-03-2021
3.
Name of the insured
Name of the policyholder
Sanjay Gupta
Sanjay Gupta
4.
Name of the insurer
Bajaj Allianz General Insurance Co. Ltd.
5.
Date of Repudiation
10-12-2020
6.
Reason for repudiation
Non-disclosure of PED
7.
Date of receipt of the Complaint
30-03-2021
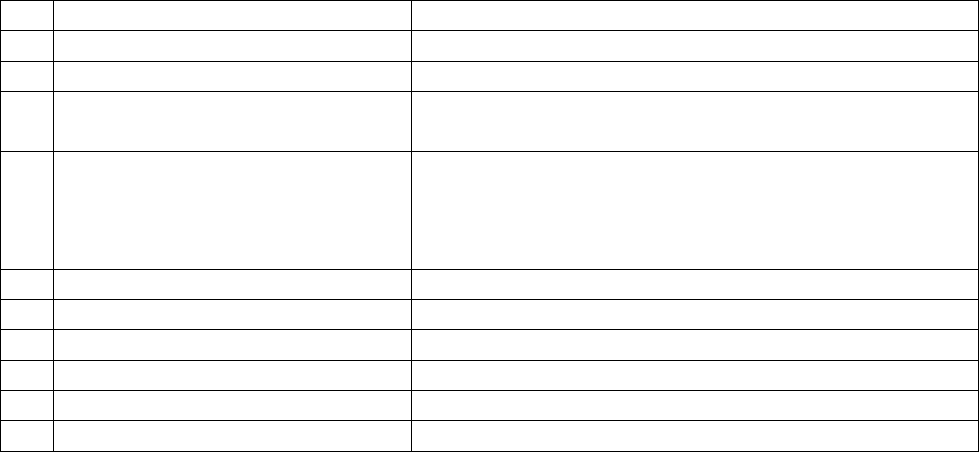
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs 51,036 /-
10.
Date of Partial Settlement
Not Applicable
11.
Amount of relief sought
Rs 51,036 /- plus 18% as harassment and mentally
torture charges.
12.
Complaint registered under Rule
No.:
Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation of
claims by an insurer
13.
Date of hearing/place
24.09.2021 / Online hearing
14.
Representation at the hearing
For the Complainant
Shri Sanjay Gupta, Complainant
For the insurer
Dr. Ravindra Shingate, Deputy Manager (Health Admin.)
15.
Complaint how disposed
Award under Rule 17
16.
Date of Award/Order
24.09.2021
17. Brief Facts of the Case: Shri Sanjay Gupta (hereinafter, the Complainant) has filed this
complaint against Bajaj Allianz General Insurance Co. Ltd (hereinafter, the Insurers), for
wrongly repudiating his claim.
1. Cause of Complaint:
1. Complainant’s argument: He is a regular mediclaim policyholder since 14/03/2011
without any break. During March 2019, he received a call from Bajaj Allianz claiming
that their company is better than National Insurance Co. and he must port his policy
with all benefits. He told them that he has BP problem (that is also mentioned in his
Discharge card of DMC Hospital when he was admitted due to UT) and his wife's uterus
had been removed in 2007. He submitted them all his policies since 2011 with all med-
ical records and made the required payment. They ported his policy. During September
2020 he felt chest pain and had to take admission in DMC hospital. The Insurers repu-
diated his claim with the remarks that he is suffering from BP for the past 6 years and
company does not pay for any pre-existing disease. However, PED is the disease, which
existed before the start of policy. But he is having mediclaim policy since 14/03/2011
and BP is already mentioned in DMC Hospital record of 2014. He also emphasized that
he is holding the mediclaim policy of same sum insured from National Insurance Co.
as in Bajaj. Then how insurance company can treat it as PED? So he requested this
forum to direct the Insurers to pay the remaining claim amount.
2. Insurers’ argument: The Insurers have stated that the complainant had taken this Pol-
icy which was valid from 14
th
March 2020 to 13
th
March 2021 He had intimated a claim
on 26th Sep 2020 for Hypertension (HTN) with Bicuspid Aortic Valve - Moderate Aortic
Regurgitation, Coronary Artery Disease from Dayanand Medical College and Hospital
– Ludhiana with Date of Admission 26-09-2020 and Date of Discharge 27-09-2020.
They registered cashless claim vide claim No OC-21-1002-8430-00010743, but, after
scrutinizing the documents, found that complainant was having history of HTN since 6

years, which was not disclosed on proposal form while opting for policy from Bajaj.
Hence, the insurance company has repudiated the claim, as the policy does not extend
coverage for any expenses incurred on the treatment of illness, which is pre-existing
to the policy and is not disclosed on the proposal form. From the indoor cases papers
and the questionnaire submitted by insured during investigation where he specifically
stated that he was suffering from HTN from 6 years and his treating doctor is Dr
Sandeep Puri. Furthermore, the complainant is on medication and taking Telma-20 for
HTN, which was never disclosed in proposal form. Therefore, insurance company has
rightly repudiated the claim of complainant on the ground of non-disclosure of mate-
rial facts. Hence, the complaint of complainant is liable to be dismissed. The said policy
issued with portability from National Insurance Company with Special Condition as - It
is hereby agreed and understood that the Health Guard (Revision) policy is issued with
portability benefit from Mediclaim policy of National Insurance Co. Ltd. & continuity is
extended from 14-03-2015. Further, in case insured is opting portability with higher
sum insured, he shall disclose his medical illness in proposal form and portability form
to ascertain his to decide accept the proposal or reject the proposal, In this case Shri
Sanjay Gupta was covered for Rs. 4 lakh Sum Insured (SI) and opted for SI of Rs. 5 lakh
in the policy with Bajaj without disclosing his actual existing ailments which he was
aware of. So there is breach of basic Principle of insurance “Utmost good faith”. There-
fore, this case may kindly be dismissed.
19. Reason for Registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
1. Result of Video Conferencing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant had ported the subject Policy to the present Insurers on 1.03.0219 for one
year and renewed it subsequently. He submitted the subject claim for his hospitalization in
September 2020 for treatment of Hypertension (HTN) with Bicuspid Aortic Valve - Moderate
Aortic Regurgitation, Coronary Artery Disease. While examining the case, the Insurers found
that HTN was noted as his pre-existing ailment for past 3 years in the indoor case papers,
whereas in the Policy Porting Proposal Form, he had declared no ailments. In this background,
the Insurers were justified in repudiating the claim on the ground of non-disclosure of material
information and, pursuantly, the complaint shall deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 24,
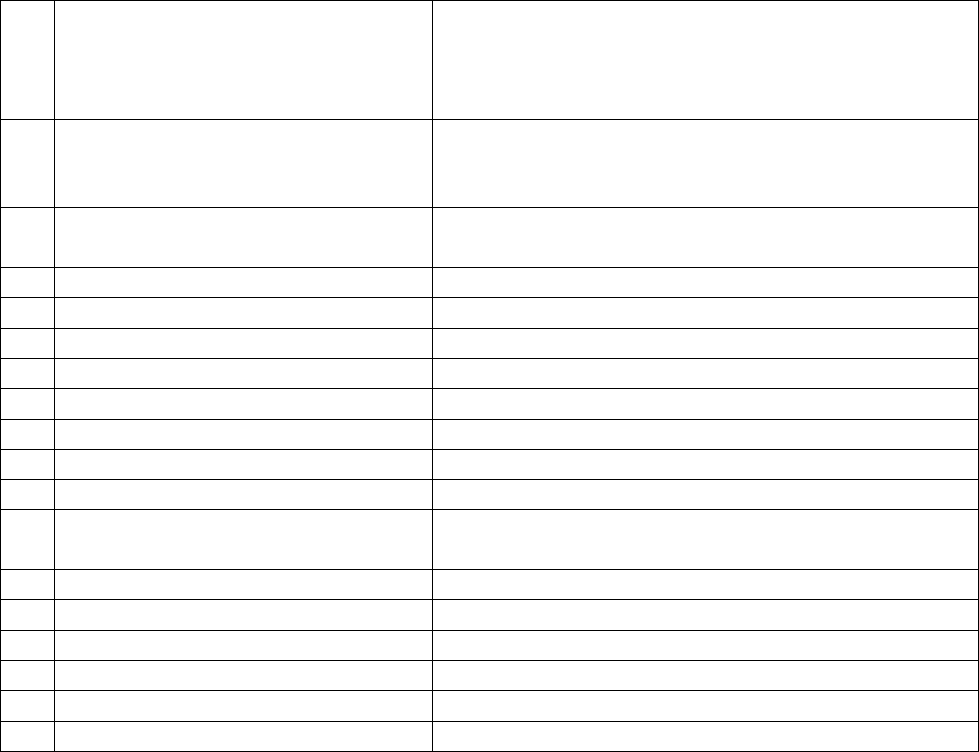
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Varinder Pal Singh V/S The United India Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-051-2122-0003
1.
Name & Address of the Complainant
Shri Varinder Pal Singh
88, Street No. 3/A, Janta Colony, Nr. Chowk Basti
Jodhewal, Ludhiana, Punjab- 141007
Mobile No.- 9855700101
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2008002819P101405123
Family Medicare Policy
06-05-2019 To 05-05-2020
3.
Name of the insured
Name of the policyholder
Varinder Pal Singh & Ramandeep Kaur
Varinder Pal Singh
4.
Name of the insurer
The United India Insurance Co. Ltd.
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the Complaint
31-03-2021
8.
Nature of complaint
Deduction in claim
9.
Amount of Claim
Rs. 118832/-(Out of this 90,000/- paid by Co.)
10.
Date of Partial Settlement
Not provided
11.
Amount of relief sought
Rs. 28832/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claim by an insurer
13.
Date of hearing/place
24.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Varinder Pal Singh, the complainant
For the insurer
Shri Sanjeev Kumar, Sr. Divl. Manager, DO-2, Ludhiana
15
Complaint how disposed
Award under Rule 17
16
Date of Award/Order
24.09.2021
17. Brief Facts of the case: Shri Varinder Pal Singh (hereinafter, the Complainant), has filed this
complaint against the United India Insurance Co. Ltd. (hereinafter, the insurers) for alleged undue
deduction in health claim.
18. Cause of Complaint:
a) Complainant’s argument: In July 2019, on doctor’s advice, Lap Hysterectomy surgery of his wife
was performed and treatment was taken from Iqbal Nursing Home, Ludhiana. Against hospital
bill of surgery for Rs. 104720/-, company deducted Rs. 30746/- at the time of reimbursement.
After surgery treatment amount of bill is Rs. 11748/- . But at the time of reimbursement,
company deducted Rs. 2364/- (Total deduction is 30746 + 2364 = 33110). After his request
company credited Rs. 4278/-. He has requested for the balance amount (33110-4278=28232).
b) Insurers’ argument: As per SCN submitted by insurance company, patient Smt. Ramandeep Kaur
had undergone Lap. Hysterectomy in Iqbal Nursing Home & Hospital and hospitalized from
25.07.2019 to 29.07.2019. Hospitalization expenses claimed is Rs. 86236/-, pre and post
expenses Rs. 32596/- (18484+14112), i.e. total claimed amount by insured is Rs. 118832/-. The
payable amount as per policy is 20% of sum insured of Rs. 3 lakh, as per policy clause 1.2 F, which
is Rs. 60,000/- plus pre and post expenses limit of 10% of sum insured as per policy clause 1.2 G,
which is Rs. 30,000/-, so total payable amount is Rs. 90,000/- in this claim. TPA has approved and
paid Rs. 73974+11748+4278 = 90,000/-, against the claimed amount Rs. 118832/-, which is
correctly paid and no scope of more balance payment is left as per policy terms and conditions.
19. Reason for Registration of Complaint: Deduction in health claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
I have examined the arguments and the evidence submitted by both the parties. The Insurers had
correctly determined the total admissible amount of the claim as Rs. 60,000 for the main
hospitalisation and Rs. 30,000 for the post- hospitalisation expenses, as described in Para 18b
above. However, a part of this total amount of Rs. 90,000, that is Rs. 4278, was paid on 08.07.2020,
which is several months after the submission of the required documents by the Complainant.
Therefore, the Insurers will need to pay interest on this amount in terms of the provisions of the
IRDAI (PPHI) Regulations 2017. The complaint deserves to be allowed to this extent only.
Award
The complaint is allowed partially and the Insurers are directed to pay interest on the delayed
payment of the balance admissible claim of Rs. 4278, which was paid to the Complainant on
08.07.2020, in terms of the provisions of the IRDAI (Protection of Policyholders’ Interests)
Regulations 2017, within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 24, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Rajinder Sharma V/S Cholamandalam Ms Gen. Insurance Co.
Ltd.
Complaint Ref. No. : CHD-H-012-2122-0002
1. On 31.03.2021, Shri Rajinder Sharma had filed a complaint in this office against Chol-
amandalam Ms Gen. Insurance Co. Ltd. for non settlement of health claim of his father
under policy no. 2876/00057345/000062/000/02.
2. This office pursued the case with the insurance company to re-examine the com-
plaint and they agreed to reconsider the claim.
1. Insurance Company informed vide letter dated 17.09.2021 that claim of complainant
has been processed and amount of Rs.62450/- has been paid to the complainant on
06.09.2021.
2. Shri Rajinder Sharma, complainant also vide e-mail dt. 20.09.2021 has confirmed that
he received the disputed compensation from the company and has given consent to
close his complaint.
3. In view of the above, no further action is required to be taken by this office and the
complaint is closed accordingly.
Dated : 24.09.2021 Insurance Ombudsman
Place : Chandigarh

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman Sh. Sudhir Krishna
Case of Akhil Gandhi v/s Star Health and Allied Insurance Co.
Ltd.
Complaint Ref No: CHD-H-044-2122-0038
1. On 08.04.2021, Shri Akhil Gandhi had filed a complaint in this office against Star
Health and Allied Insurance Co. Ltd for repudiation of his father health claim. The
required documents were submitted to the insurance company but the insurance
company did not settle his claim under policy no. P/211114/01/2020/015001.
2. This office pursued the case with the insurance company to re-examine the com-
plaint. Insurance company vide their email dated 01-09-2021 informed that they
have decided to consider the claim for settlement as per terms and condition of the
policy for Rs 2,73,880/-.
3. Shri Akhil Gandhi confirmed vide email 01-09-2021 that he agrees to the offer of the
insurance company and he wants to withdraw his case from this forum.
4. Now, Insurance company vide email dated 28.09.2021 confirmed that they have re-
leased claim amount of Rs 2,73,880/- under the claim no CIR/2021/211114/
2246340 (Rs 2,71,724 + 2,156/- ) through NEFT transaction no- 109160366401 on
16.09.2021.
5. In view of the above, no further action is required to be taken by this office and the
complaint is closed accordingly.
Dated: 28.09.2021 Insurance Ombudsman

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman Sh. Sudhir Krishna
Case of Tripti Jain v/s Star Health and Allied Insurance Co.
Ltd.
Complaint Ref No: CHD-H-044-2122-0034
1. On 07.04.2021, Smt Tripti Jain had filed a complaint in this office against Star Health
and Allied Insurance Co. Ltd for cancellation of her family policy number
P/211119/01/2020/005860. The required clarifications were submitted to the in-
surance company but the insurance company did not reinstate her policy no.
P/211119/01/2020/005860.
2. This office pursued the case with the insurance company to re-examine the complaint
and they agreed to reinstate the cancelled policy vide email dated 31.08.2021.
3. Smt Tripti Jain confirmed vide email 02-09-2021 that insurance company has agreed
to her request and she wants to withdraw her case from this forum.
4. Now the insurance company has confirmed vide email dated 17.09.2021 that the pol-
icy has been restored.
5. In view of the above, no further action is required to be taken by this office and the
complaint is closed.
Dated: 28.09.2021 Insurance Ombudsman

PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman Sh. Sudhir Krishna
Case of Kanwaldeep Singh v/s Star Health and Allied Insurance Co.
Ltd.
Complaint Ref No: CHD-H-044-2122-0223
1. On 23.06.2021, Shri Kanwaldeep Singh had filed a complaint in this office against Star
Health and Allied Insurance Co. Ltd for deduction of his health claim. The required
documents were submitted to the insurance company but the insurance company did
not settle his claim under policy no. P/161130/01/2021/028059.
2. This office pursued the case with the insurance company to re-examine the com-
plaint. Insurance company vide their email dated 27-08-2021 informed that they
have decided to consider the claim for settlement as per terms and condition of the
policy for Rs 22,620/-.
3. Shri Kanwaldeep Singh confirmed vide email 31-08-2021 that insurance company has
agreed to pay his claim for Rs 22,620/- and he wants to withdraw his case from this
forum.
4. Now, Insurance company vide email dated 17.09.2021 confirmed that they have re-
leased claim amount of Rs 22,620/- under the claim no CIR/2022/161130/2573764
through NEFT transaction no- 109160366417 on 16.09.2021.
5. In view of the above, no further action is required to be taken by this office and the
complaint is closed.
Dated: 28.09.2021 Insurance Ombudsman
AWARD NO.IO/KOC/A/HI/0249/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-035-2122-0445
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 09.09.2021
1.
Name and Address of the
complainant
:
Mr. Santhana Kumar S
Csb Ulloor Cheruvikkal Trivandrum
69501
2.
Policy Number
:
920292028521000794
3.
Name of the Insured
:
Mr. Santhana Kumar S
4.
Name of the Insurer
:
Reliance General Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
29.06.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Absent
2. For the Insurer
:
Mr. Sujith

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Santhana Kumar S is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he has applied for claim under Reliance General Covid-19 Total
protection policy number 220392028521000794 covering both diagnosis and
quarantine cover. As per the benefit policy of reliance general insurance, the company is liable
to pay 50% of the sum insured if the insured person is quarantined for covid-19 for at least 14
days. He has been issued a certificate from the Government of Kerala of completing 14 days
of quarantine at SEKT 19 KURUPS LANE SASTHAMANGALAM ( his rented house address) and
was released on 2nd November 2020, 14 days after getting admitted. He requests the
Ombudsman to get his genuine hospitalization claim of Rs 25,000/- paid.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the Compliant / Insured understood the features of the policy and thereafter filled and
submitted the proposal form. It is submitted that upon receipt of the Proposal Form, the
Company has issued RELIANCE COVID-19 PROTECTION INSURANCE- Policy bearing no.
220392028521000794 to Ms Santhana Kumar S and the risk was covered from 20-Jun-2020
to 19-Jun-2021 for Sum Insured of Rs. 50,000/-, subject to Policy Terms and Conditions.
It is clearly mentioned in the Policy terms and conditions:
Quarantine means isolation of an individual either due to Diagnosis or suspected infection of
COVID-19. For the purpose of this Policy, Quarantine shall mean isolation which is prescribed
by either the Union Health Ministry approved testing centre, or the Central or the State
Government; and in a place arranged and approved as a Quarantine center by the Central
or State Government. Self-isolation is not Quarantine.
Section 4: Specific Exclusions related to Section-3 vii which speaks that Self Quarantine: Self
Quarantine is not covered.
The relevant portion of the Policy terms and conditions is mentioned below:
Under section 4 Specific Exclusions related to Section-3 : vii. Self-Quarantine: Self-Quarantine
is not covered and xliii. Quarantine means isolation of an individual either due to Diagnosis or
suspected infection of COVID-19. For the purpose of this Policy, Quarantine shall mean
isolation which is prescribed by either the Union Health Ministry approved testing centre, or
the Central or the State Government; and in a place arranged and approved as a Quarantine
center by the Central or State Government. Self-isolation is not Quarantine. On the basis of
details and documents provided by the complainant and on discussion held with the

claimant/insured it was revealed that he was only home quarantined and diagnosed Covid
Negative. The copy of Covid Negative Certificate and Home Quarantine notice published in
front of the building where the claimant residing by District Administration
Thiruvananthapuram are available.
The complaint went under Quarantine on 20/10/2020 . Complainant got his Covid negative
Report on 23/10/2020 . Since complainant was not infected, there was no requirement for
the complainant to spend the remaining period under quarantine . Under Policy the
quarantine coverage is applicable only if person is covid positive or under suspicion of covid
for 14 days suspension ended when complainant report came negative The
Complainant/Insured was Home Quarantined from 20-October-2020 to 02-November-2020
as per the direction of Kerala State Government. The Health Department of Kerala
Government has issued Quarantine Certificate dated 02-Nov-2020. However, since the
claim was repudiated on 24-Aug-2021 under section 4 Specific Exclusions related to Section-
3 : vii. Self-Quarantine: Self-Quarantine is not covered and xliii. Quarantine means isolation of
an individual either due to Diagnosis or suspected infection of COVID-19. For the purpose of
this Policy, Quarantine shall mean isolation which is prescribed by either the Union Health
Ministry approved testing centre, or the Central or the State Government; and in a place
arranged and approved as a Quarantine center by the Central or State Government and in a
place arranged and approved as Quarantined Centre by the Central and state Government .
Self- isolation is not Quarantine.
It is submitted that the Complainant’s claim has been rightly repudiated as per policy terms
and conditions as the Complainant has not undergone Quarantine in a place arranged and
approved as a Quarantine center by the Central or State Government. Home Quarantine is
not covered under the policy. The present complaint lacks merits, there is no cause of action
in the matter, the complaint is not maintainable and deserves to be dismissed. It is therefore
humbly prayed that the Hon’ble forum may graciously be pleased to dismiss the present
complaint in the interest of justice.
3. I heard the Respondent Insurer. The Complainant was absent. On 11/8/2021 a letter was
dispatched to him intimating the Date and Time of Hearing. Subsequently , prior to the
Hearing, he was informed on his mobile no. 8220513231 about the same. On the day of
Hearing, he did not respond to 8 calls or more made to his two mobile nos. available in the
records with this Forum or to the email that was sent to him on the email id with which
correspondence has been made earlier.
The Respondent Insurer submitted that the complainant was in self isolation . The
complainant was quarantined on 20/10/2020 and tested negative after 3 days. He
quarantined himself solely for availing benefit under the policy. The policy provides for benefit
only when quarantined in a place arranged and approved as a Quarantine center by the
Central or State Government and Self-isolation is not Quarantine.
4. I have gone through the documents submitted by both the sides and heard the Respondent
Insurer. The complainant has claimed 50% of the Sum Insured under Quarantine Cover stating
that he is entitled to it as he was quarantined for 14 days due to covid-19 . He has submitted

a Covid negative Lab Test Report of 23/10/2020 but has not submitted Covid positive Lab Test
Report ( from a Govt. approved Testing centre). The Quarantine Certificate dt. 2/11/2020
issued by the Medical Officer , Thiruvananthapuram, Govt. of Kerala, states that he has
completed 14 days of home/ instituitional Quarantine for 14 days and released on 2/11/2020 ,
while the Home under Quarantine Notice of the District Administration, Thiruvanathapuram
establishes that the complainant was under Home Quarantine only. It is also stated by the
complainant himself that he was under quarantine in his rented house.
According to Sec 2 xliii , Quarantine means isolation of an individual either due to Diagnosis
or suspected infection of Covid 19 and Quarantine shall mean isolation in a place arranged
and approved as a Quarantine center by the Central or State Government. Self-isolation is not
Quarantine.
In view of the above, the claim is not tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 9
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0250/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-050-2122-0342
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.

AWARD PASSED ON 09.09.2021
1.
Name and Address of the
complainant
:
Mr. Thampi Jacob
Thekkekkara House, Thirumaradi P
O, Ernakulam-686662
2.
Policy Number
:
441700/48/2019/491
3.
Name of the Insured
:
Ms. Shiji Thampi
4.
Name of the Insurer
:
The Oriental Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
01.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
9.
Parties present at the hearing
1. For the Complainant
:
Settled before hearing
2. For the Insurer
:
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Thampi Jacob is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he has policy for himself and his family and that previously he
has got his claim settled for Ayurvedic treatment but the present claim of 26/7/2020 for his
wife’s treatment was not settled stating that it is Ayurvedic treatment. Vempilly Ayurveda
Hospital is approved by the TPA. He had spent an amount of Rs. 30,111/- There is no response
to his Griev. letter. He requests the Ombudsman to get his claim settled.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that they have settled the claim for Rs. 27,261/-
3. The Respondent Insurer has settled the claim for Rs. 27,261/- and the complainant has
confirmed having received the amount from the Respondent Insurer through NEFT transfer to
his bank account and the complainant has withdrawn the complaint.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 9
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0251/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0353
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 10.09.2021
1.
Name and Address of the
complainant
:
Mr. C R Gopesh
Naamam GP-06 Green Park Thiruvambadi
P O Thrissur 680022
2.
Policy Number
:
P/181216/01/2021/002568
3.
Name of the Insured
:
Mr. C R Gopesh
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
05.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. C R Gopesh (Online)
2. For the Insurer
:
Mr. Manu Mohan (Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. C R Gopesh is the policyholder.
1. Averments in the complaint are as follows:
The complainant stated that the claim was raised on 17.4.21 for his son, 5years old who
underwent Circumcision on a very emergency basis at Thangam Hospital, Palakkad, following
a sudden urine blockage . The claim was rejected quoting it as an `exclusion under the policy`.
His son had become part of the family medical insurance plan with Apollo Munich insurance
since his birth in Feb. 2016, till he switched to the respondent insurance company last year.
The complainant prayed for the settlement of he claim. The quantum of relief sought is
Rs.14,413/-.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the Complainant had taken Star Comprehensive Health Insurance policy commences
from 12/07/2020 to 11/07/2021 for the Sum Insured of Rs.7,50,000/- vide policy No:
P/181216/01/2021/002568. The policy covers hospitalization expenses incurred in India as an
inpatient subject to the definitions, conditions and exclusions, set there in. It is submitted
that the complainant `s son ( Krishsaketh G.S) was admitted at Thangam Hospital, Palakkad
for the treatment of Balanoposthitis , Tight Foreskin, Retention of Urine and underwent
Circumcision. The Discharge summary issued by the Thangam Hospital, Palakkad indicated
that that the complainant`s son had undergone Circumcision. As per the policy claue -
Exclusion No.4 (1) , the Company shall not be liable to make any payments under this policy
in respect of any expenses what so ever incurred by the insured person in connection with or
in respect of Circumcision, Preputioplasty, Frenuloplasty, Preputial Dilatation and Removal of
SMEGMA. Hence the insurer had repudiated the claim and the same was informed to the
complainant on 03/05/2021. Further on escalation to grievance department another expert
team reviewed and rejection justified .
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
son, 5years old who underwent Circumcision on a very emergency basis at Thangam Hospital,
Palakkad, following a sudden urine blockage . The claim was rejected quoting exclusion of
the procedure in the policy. The Respondent Insurer submitted that the discharge summary
issued by the Thangam Hospital, Palakkad, indicated that the complainant`s son underwent
Circumcision. As per Exclusion No.4 (1) of the policy: The Company shall not be liable to make
any payments under this policy in respect of any expenses what so ever incurred by the
insured person in connection with or in respect of Circumcision, Preputioplasty, Frenuloplasty,
Preputial Dilatation and Removal of SMEGMA. Hence the insurer had repudiated the claim.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this case the claim for the complainant`s 5 years old son who
underwent Circumcision following a sudden urine blockage was denied.
The arguments put forth by the respondent insurer were that the discharge summary issued
by the Thangam Hospital, Palakkad , indicated that the complainant`s son underwent
Circumcision. As per Exclusion No.4 (1) of the policy, the Company shall not be liable to make
any payments under this policy in respect of any expenses what so ever incurred by the
insured person in connection with or in respect of Circumcision, Preputioplasty, Frenuloplasty,
Preputial Dilatation and Removal of SMEGMA. I therefore do not want to interfere in the
decision of the respondent insurer in rejecting the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 10
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0252/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0345
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 10.09.2021
1.
Name and Address of the
complainant
:
Mr. Joji James
Parathumpara House, Kura P
O ,Chengamanadu Kottarakara Kollam
691557
2.
Policy Number
:
P/181112/01/2021/011004
3.
Name of the Insured
:
Mr. Joji James
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
30.06.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Joji James (Online)
4. For the Insurer
:
Mr. Manu Mohan (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Joji James is the policyholder.
1. Averments in the complaint are as follows:
The complainant working as a Forest Range Officer in the Kerala Forest & Wildlife Dept., stated
that on 21.12.20, while returning home after work in the evening met with a bike accident at
6.45PM near Kottarakara, , injuring his right leg and hands. He was taken to the Vijaya Hospital,
Kottarakara from where he was shifted to the SP Fort Hospital, Trivandrum, since the injury
was serious. On the right leg , it was a Comminuted Bicondylar Fracture Right Fibia whereas
on his left hand, it was a Comminuted Fracture Distal Radius & for the Right hand , Volar
Barton Fracture right Wrist . On 22.12.20, surgery was performed for his right leg and left
hand and then his left hand. Plates and screws were fixed. He underwent two major surgeries
and was discharged on 28.12.20. The respondent insurer was also informed. The hospital bill
at the SP Fort Hospital, Trivandrum was Rs.5,53,466/-. The claim was rejected stating non-
disclosure of material facts. He had fluctuations in the Creatinine level and had consulted
doctor. It was never been a serious issue. This was revealed to the Casualty Doctor at the time
of the hospitalization at the Vijaya Hospital, Kottarakara . The respondent insurance company
advocated this as CKD and the claim was denied and later the policy was also cancelled. The
matter was taken up with Grievance Cell of the respondent insurer but was in vain. The
complainant prayed for the settlement of the claim.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant had taken a Family Health Optima Insurance Policy for the period
19/10/2020 to 18/10/2021 vide Policy No. P/181112/01/2021/011004 for the sum insured of
Rs.4,00,000/-. The policy covers hospitalization expenses incurred in India as an inpatient
subject to the definitions, conditions and exclusions, set there in. The company issued the
policy to the complainant based on the proposal form submitted by the insured. The proposal
form is the basis and integral part of the contract, on the basis of which the policy is issued.
The policy is issued strictly according to the terms and conditions only and it is a settled law
that the parties to the insurance contract are bound by the terms and conditions of the policy
issued. The acceptance of the proposal was based on the information/details given by the
proposer. Acceptance of risk is to be decided by the insurance company. If the health status
of the proposer is found satisfactory based on the facts in the proposal, the insurer would
accept the risk and issue policy. If a proposer submits wrong information in the proposal to
mislead the insurer to issue a policy, it is fraud . The respondent insurer had received a request
for the cashless treatment from SP Fort Hospital, Thiruvananthapuram stating that the
complainant was admitted at this hospital on 22/12/2020, for the treatment for Comminuted
Bicondylar Fracture Right Tibia, Comminuted Fracture distal radius (LT), Volar Barton fracture
right wrist.. The letter dated 21/12/2020 issued by Vijaya Hospital, Kottarakkara clearly reveals
that the patient is a known case of Diabetic Mellitus, Hypertension and CKD( Chronic Kidney
Disease) and discharged against medical advice. After receiving claim documents , the
respondent insurer had send a query letter dated 23/12/2020, to the hospital authority and
requested to forward the following details:-
1. As per the records patient is a known case of CKD - kindly clarify its dura-
tion and provide prior consultations
2. Circumstances of injury along with date and time
3. X ray images
Based on the query letter, the hospital authority had forwarded the copies of lab reports &
hospital records . It is submitted that the Lab Investigation report dated 10/09/2020 shows :-
1. Creatinine Test : 3.2 mg/dl ( Normal Range : 0.5 – 1.5 mg/dl )
The letter dated 26/12/2020 issued by Vijaya Hospital, Kottarakkara clearly stated that the
complainant was on regular check up under the Nephrology Department in the hospital since
13/08/2020. He is a known case of CKD( Chronic Kidney Disease) & on regular
treatment .Based on the available medical records, it is clearly evident that the patient had
history of Kidney Disease and on regular treatment before the inception of policy and it was
not revealed in the proposal form at the time of the inception of the policy. As the complainant
had willfully suppressed the pre-existing disease in the proposal form, which is the basis of
contract at the time of taking the policy, it amounts to suppression of material facts. The
respondent insurer repudiated the cashless claim based on the grounds suppression of material
facts as per terms and conditions of the policy and the same was informed to the complainant
and hospital authorities on 28.12.20.
On discharge from the hospital, the complainant had submitted the completed claim form along
with lab reports & bills for Rs. 5,53,466/- . The discharge summary dated 28/12/2020 issued
by the SP fort Hospital, Thiruvananthapuram clearly revealed that the complainant had a past
history of Renal Disease and Hypertension . Based on the available medical records, the
respondent insurer repudiated the claim on grounds of suppression of material facts as per terms
and conditions of the policy . This was informed to the complainant on 04/06/2021. It is
submitted that as per conditions No: 5(10) of the policy, the company may cancel the policy on
grounds of misrepresentation, Fraud, Moral hazard, Non disclosure of material fact as declared
in the proposal form. On that basis the respondent insurer had cancelled the policy in the name
of the complainant and the same was informed to his last known address on 31/12/2020 .The
allegations raised by the complainant in the complaint are not fully correct and are denied. It is
submitted that if there is a suppression/Non disclosure/ Misrepresentation of material facts in
proposal form – in a contract of insurance, any fact which would influence the mind of a
prudent insurer in deciding whether to accept and not to accept the risk is a material fact-
(Regulatory and Development Authority (Protection of Policy holders Interests) Regulations,
2002. Regulation 2 (1) (d)) if the proposer has knowledge of such fact, he is obliged to disclose
it to the insurer, particularly the answer to said questions will entitle the insurer to repudiate
its liability under the policy.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that on
he was involved in a bike accident while he was returning from work at around 6.45PM on
21.12.20 . He was taken to the Vijaya Hospital, Kottarakara and then shifted to the SP Fort

Hospital, Trivandrum, as the injury was serious. He had fractures on his right leg and hands.
He underwent two major surgeries and was discharged on 28.12.20. His claim was rejected
stating non-disclosure of material facts. As there were fluctuations in Creatinine levels which
was not serious, he had consulted doctor, the respondent insurance company considered it
as CKD and the claim was denied. The Respondent Insurer submitted that the discharge
summary dated 28/12/2020 issued by the SP fort Hospital, Thiruvananthapuram clearly
indicates that the complainant had past history of Renal Disease and Hypertension . The claim
was repudiated on the grounds suppression of material facts and the policy was cancelled, as
per terms and conditions of the policy.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this case the claim for the surgery of the complainant`s fractured hands
and right leg following an accident involving bike, was denied, the arguments put forth by the
respondent insurer were:: 1. As per medical records the complainant had a past history of
Renal Disease and Hypertension which were not disclosed while taking the policy. 2. This
tantamount to suppression of material facts. 3. The claim was rejected on account of non
disclosure of material facts and the policy was cancelled; are all tenable. I therefore do not
want to interfere in the decision of the respondent insurer in rejecting the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 10
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0253/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0325
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 10.09.2021
1.
Name and Address of the
complainant
:
Mr. Harikrishnan V
Jayavilasm Parakode Pathanamthitta
691554
2.
Policy Number
:
P/181134/01/2021/001011
3.
Name of the Insured
:
Mr. Harikrishnan V
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
28.06.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Harikrishnan V (Online)
2. For the Insurer
:
Mr. Manu Mohan (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Harikrishnan V is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he was insured against Covid 19 vide policy
no.P/181134/01/2021/001011 dated 18.8.20. He was infected with Covid 19 on 27.1.21 and
underwent home quarantine. Due to its severity, he was admitted at the Believer`s Church
Medical College Hospital, Thiruvalla, for treatment after 5days of the infection. He was
discharged on testing Covid negative. On claiming after the treatment, his claim was rejected
on flimsy grounds. The Complainant prayed for the settlement of the claim. The quantum of
relief sought is Rs.2.5lacs.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant had taken a Corona Rakshak policy for the period 15/8/20 to 27/5/21
for a sum insured of Rs.2,50,000/-, vide policy no. P/181134/01/2021/001011. The
complainant was admitted at the Believers Church Medical Hospital, Thiruvalla, on 1/2/21 for
the treatment of Covid 19 infection Category A, Mild and after treatment was discharged on
5/2/21. As per the discharge summary from the hospital his vitals were normal and no active
line of treatment was given but only vitamin tablets prescribed. There were no symptoms
requiring an inpatient care/an admission in a hospital. As per the available medical records it
was clear that the patient stayed at the hospital for the observation/monitoring i.e. under the
institutional quarantine and hospitalization was not warranted.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that
whilst engaged in Police duties at Sabarimala, he got infected with Covid 19. He was tested
Covid 19 positive on 27.1.21 and underwent home quarantine. Since it became severe, he
was hospitalised. His claim for Covid 19 (Category A) treatment at the Believers Church
Medical Hospital, Thiruvalla, for the period 1.2.21 to 5.2.21, was denied. The complainant
pleaded for the claim settlement. The Respondent Insurer submitted that that the
complainant had taken a Corona Rakshak policy for the period 15/8/20 to 27/5/21 for a sum
insured of Rs.2,50,000/-. He was admitted at the Believers Church Medical Hospital,
Thiruvalla, on 1/2/21 for the treatment of Covid 19 infection Category A, Mild and after
treatment was discharged on 5/2/21. The discharge summary from the hospital indicates that
his vitals were normal and no active line of treatment was given. Only vitamin tablets were
prescribed. As per the available medical records it was clear that the patient stayed at the
hospital for the observation/monitoring i.e. under the institutional quarantine and
hospitalization was not warranted.
4. I heard the Complainant and the Respondent Insurer and had gone through the records
submitted.
I have analysed the following to arrive at a just and fair decision:
1. As per the Complainant`s argument, he got infected with Covid 19 on 27.1.21 whilst
engaged in duty as a Police Official at Sabarimala. The Doctors Progress Notes dated 1.2.21,
from the Believers Church Medical College Hospital, Thiruvalla, where he was hospitalized
from 1.2.21 to 5.2.21., for Covid 19 treatment confirmed that the Complainant had a “History
of working in Sabarimala as Police, 2weeks back”. Around 20 policemen were found Covid 19
positive.
2. Being a Police official, he is a frontline worker.
On analyzing the above, I find that the claim is payable. The respondent insurer therefore has
to pay the sum insured amount of Rs.2,50,000/-, to the Complainant.
In the result, an award is passed, directing the Respondent Insurer to pay an amount of
Rs.2,50,000/-, subject to submission of all records, within the period mentioned hereunder.
No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 10
th
day of September 2021.
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0256/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-031-2122-0329
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 13.09.2021
1.
Name and Address of the
complainant
:
Mr. Muhammed Salih P
Palmalayil House Perumpillichira P
O Thodupuzha Idukki 685605
2.
Policy Number
:
31319155202000
3.
Name of the Insured
:
Mr. Muhammed Salih P
4.
Name of the Insurer
:
MAX BUPA HEALTH INSURANCE
CO.LTD
5.
Date of receipt of Complaint
:
26.05.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
1. For the Com-
plainant
:
Mr. Muhammed Salih P (Online)
2. For the Insurer
:
Ms. Shital Patwa (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Muhammed Salih P is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had claimed for claim reimbursement for Lower Back Pain. On
16.2.21, he slip and fall and was admitted at the Ayur Bethaniya Ayurveda Hospital for 21days
treatment and physiotherapy. The medical expenses were Rs.1,54,436/-, which he had
remitted. All documents were submitted, including Medical certificate, but the claim was
rejected stating treatment under taken by him in 2018, for lower back pain, which he had not
claimed .
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that
the complainant submitted a Proposal Form proposing the issuance of a Health
Insurance Policy to Niva Bupa Health Insurance Co. Ltd.( Formerly known as Max Bupa
Health Insurance Co. Ltd.)to insure himself and his family.
On the basis of the
Declaration made therein under, the Company has issued a Health Companion
Variant 2 policy bearing No. 3 1319155202000 commencing from 10.08.2020
to 09.08.2021 in the name of complainant for a base sum insured of Rs.5, 00, 000/
-. A claim was filed by the complainant for the settlement of expenses of Rs.
1,54,436/ -, incurred during his hospitalization at Ayur Bethaniaya Ayurvedic
Hospital from
24.02.2021 to 17.03.2021, wherein the patient was treated for Low
Back Pain. On receipt of the claim for reimbursement, the respondent company as
per the guidelines forms by IRDAI and to know the veracity of the claim appointed
an investigator to investigate the claim. During the investigation, an old treatment
record of 05. 10.2018 had been discovered wherein symptoms of lower back ache
was mentioned . As per the received medical documents and the investigation done,
it was revealed that the complainant had been suffering from low back ache since
2018 and hypothyroidism since 20 years which is a pre existing condition and as such
the claim was denied as per clause 5.1.
5.1 Pre-existing Diseases:-
All Pre-existing Diseases shall not be covered until 48 months of continuous coverage have elapsed
since the inception of the First Policy with Us for Insured Persons to whom Variant 1 Plan is applicable
as specified
in the Product Benefits Table and until 36 months of Continuous
coverage
have elapsed
since the inception of the First Policy with us for Insured
Persons to whom Variant 2, Variant S Plans
and Family First Policy
are applicable as specified in the Product Benefits Table.
It is pertinent to state that as per the emergency notes from triage sheet dated 5.10.18, it
was apparent that the complainant had back problem ache since the said date. Accordingly
the claim was denied under the pre existing clause wherein the disease is covered only after
serving a waiting period of 36months.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
underwent 21days
from
24.02.2021 to 17.03.2021
at the A yur Bethaniaya
Ayurvedic Hospital
, for
treatment and physiotherapy for Lower Back Pain following a slip
and fall. His claim was rejected claim was rejected stating the treatment taken by him in 2018,
for lower back pain, for which he had not claimed . He prayed for the settlement of medical
expenses of Rs.1,54,436/-, incurred. The Respondent Insurer submitted that
the
complainant had submitted a claim for reimbursement of Rs. 1,54,436/ -, incurred
during his hospitalization
for Low Back Pain
at A yur Bethaniaya Ayurvedic
Hospital from
24.02.2021 to 17.03.2021. On receipt of the claim related papers from
the complainant, During the investigation, an old treatment record of 05. 10.2018
had been discovered wherein symptoms of lower back ache was mentioned . As per
the received medical documents and the investigation, it was made known that the
complainant was suffering from low back ache since 2018 and hypothyroidism since
20 years which is a pre existing condition and as such the claim was denied as per
clause 5.1.
Accordingly the claim was denied under the pre existing clause wherein the
disease is covered only after serving a waiting period of 36months.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this case where the complainants claim for the Lower Back pain
following a slip and fall was denied, the respondent insurer argued that as per the medical
records and
investigation, it was made known that the complainant was suffering from
low back ache since 2018 and hypothyroidism since 20 years which is a pre existing
condition as per clause 5.1.
Accordingly the claim was denied under the pre existing clause
wherein the disease is covered only after serving a waiting period of 36months, are tenable .I
therefore do not want to interfere in the decision of the respondent insurer in denying the
claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 13
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0257/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0364
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 13.09.2021
1.
Name and Address of the
complainant
:
Mr. Prasanth P
Kadayil Puthen Veedu, Pullamalaputhur,
Kollam - 69150
2.
Policy Number
:
P/181134/01/2021/000802
3.
Name of the Insured
:
Mr. Prasanth P
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
12.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Prasanth P (online)
4. For the Insurer
:
Mr. Manu Mohan (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Prasanth P is the policyholder.
1. Averments in the complaint are as follows:
The complainant stated that his claim under the Corona Rakshak policy was repudiated on the
ground that “As per the terms and conditions of the policy issued, Lump Sum Benefits shall
be payable on positive diagnosis of Covid , requiring hospitalization and not for the
institutional quarantine. The reason is baseless and unjustified. He was hospitalised in a
hospital set up by the Health Dept. of the State of Kerala. It was a fully fledged hospital run by
the Health Dept. of the Ministry of Health. The complainant was tested Covid19 positive and
underwent treatment as an Inpatient for 11days from 10.12.20 to 20.12.20. The case sheets
clearly mention the name of the hospital as CFLTC Valakom, Kollam. CFLTC and Covid second
line treatment centers are hospitals set up by the Health Dept., Government of Kerala with
treatment facilities when Covid was at its peak. They are not institutional quarantine centers
as made out by the respondent insurer. As per the salient features of the policy in Malayalam,
handed over to him, it was clearly mentioned that if you undergo treatment for Covid 19 for
over 72 hours in a Government or Government recognized hospital he will be getting the full
amount. In this case the insured amount is Rs.1.5lacs.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the Complainant had taken a Corona Rakshak Policy for the period from 30/07/2020 to
11/05/2021 for a Sum Insured of Rs. 1,50,000/- vide policy No P/181134/01/2021/000802.
The insured patient was admitted at the COVID 19 First Line Treatment Centre (CFLTC)- Kollam
on 10/12/2020 for the treatment of COVID 19 and after the treatment was discharged on
20/12/2020. It is submitted that in the discharge card issued by CFLT Centre- Kollam reveals
that the patient`s SPO2 value is 99% ( Normal Range : 94 – 100% ). The condition of the patient
i.e. , whether symptomatic or asymptomatic & the category of the condition ( A,B,& C), was
silent in the discharge card. As per the terms and conditions of the policy it is clearly men-
tioned that “the claim shall be payable on positive diagnosis of Covid 19 requiring hospitali-
zation for a minimum period of 72 hours”. Here Covid positive was diagnosed but hospitali-
zation was not warranted and hence admitted in the CFLTC for observation. No specific treat-
ment was given to the patient and no documents submitted other than discharge summary.
As per terms and condition of the policy, Lump sum benefit equal to 100% of the Sum Insured
shall be payable on positive diagnosis of COVID, requiring hospitalization for a minimum con-
tinuous period of 72 hours. The positive diagnosis of COVID shall be from a government au-
thorized diagnostic centre. The policy is designed to mitigate the huge expenses incurred for
the prolonged treatment. As per the definition clause (3.7) of the policy hospitalization means
admission in a hospital designated for Covid 19 treatment by the government for a minimum
period of 72 consecutive in-patient care hours.

As per the definition clause (3.8) of the policy stated In – patient care means treatment for
which the insured person has to stay in a hospital continuously for more than 72 hours for
the treatment of COVID. In the instant case, no treatment was provided to the patient. Hence
stay in the hospital was not at all essential.
Based on the above mentioned definitions, it was clear that the claim was payable only if the
insured person had stayed / admitted in a hospital for the treatment of COVID and required
hospitalization. In this case, the insured patient was admitted at COVID 19 First Line Treatment
Centre (CFLTC) and it was only an institutional quarantine facility and not a hospital. Hence
CFLTC doesn’t come under the definition of Hospital as per policy norms. CFLTCs provide
institutionalised care and treatment to mild or asymptomatic COVID positive patients. This
level provides essential COVID care as well as specialised care via telemedicine facility linked
to the COVID Hospital.
The patient stayed at the CFLT centre i.e. under institutional quarantine for observation. Since
CFLTC is not a hospital and lack the infrastructure of a hospital as per policy clause, the insurer
had rightly repudiated the claim. As per the policy, a Hospital is defined as:-
Hospital means any institution established for the in-patient care and day care treatment of
disease/injuries and which has been registered as hospital with the local authorities under
the Clinical Establishments (Registration and Regulation) Act, 2010 or under the enactments
specified under Schedule of Section 56 (1) of the said Act, OR complies with all minimum cri-
teria as under:
1. Has qualified nursing staff under its employment
2. Has at least ten inpatient beds, in these towns having a population of
less than ten lakhs and fifteen inpatient beds in all other places.
3. Has qualified medical practitioner (s) in charge round the clock.
4. Has a fully equipped operation theatre of its own where surgical proce-
dures are carried out.
5. Maintains daily records of patients and shall maje these accessible to
the Company’s authorized personnel
6. For the purpose of this policy any other set-up designated by the gov-
ernment as hospital for the treatment of COVID-19 shall also be consid-
ered as hospital.
The guidelines for Covid-19 defines Quarantine. “Quarantine means the separation and re-
striction of movement or activities of persons who are not ill but who are believed to have
been exposed to infection, for the purpose of preventing transmission of diseases”. The pur-
pose of Quarantine during the current outbreak is to reduce transmission by:
1. Separating contacts of COVID -19 patients from community
2. Monitoring contacts for development of sign and symptoms of COVID -19, and

3. Segregation of COVID -19 suspects, as early as possible from among other quarantined
persons.
4.
The Guidelines with regard to CFLTC clause 3( pre requisite for CFLTC) only mentions that
CFLTCs provide institutionalised care and treatment to mild or asymptomatic COVID positive
patients. This level provides essential COVID care as well as specialised care via telemedicine
facility linked to the COVID Hospital. The requisites essential for CFLTC already mentioned in
it. None of the requisites does n`t comes under the definition of hospital as per policy condi-
tion. Asymptomatic patients doesn`t need hospitalisation. If there is severe symptoms of
Covid, then such patients are to be referred to Covid hospital for inpatient care. That means
such symptomatic patients will never treated under CFLTC. The insurer had repudiated the
claim and the same was informed to the insured on 10/03/2021. Further on escalation to
grievance department another expert team reviewed and rejection justified.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that on
testing Covid19 positive, he underwent treatment as an Inpatient for 11days from 10.12.20
to 20.12.20. The case sheets clearly mention the name of the hospital as CFLTC Valakom,
Kollam. CFLTC and Covid second line treatment centers are hospitals set up by the Health Dept.,
Government of Kerala with treatment facilities when Covid was at its peak. They are not
institutional quarantine centers as made out by the respondent insurer. As per the salient
features of the policy in Malayalam, handed over to him, it was clearly mentioned that
treatment undergone for Covid 19 for over 72 hours in a Government or Government
recognized hospital will be getting the full amount. The complainant prayed for the settlement
of the claim. The Respondent Insurer submitted that the insured patient was admitted at
COVID 19 First Line Treatment Centre (CFLTC)- Kollam on 10/12/2020 for the treatment of
COVID 19 and after the treatment he was discharged on 20/12/2020. The condition of the
patient ie, whether symptomatic or asymptomatic & category of the condition ( A,B,& C) was
silent in the discharge card. As per the terms and conditions of the policy it is clearly
mentioned that “the claim shall be payable on positive diagnosis of covid 19 requiring
hospitalization for a minimum period of 72 hours”. Here Covid positive has been diagnosed
but hospitalization was not warranted and admitted in CFLTC for observation. No specific
treatment was given to the patient and no documents submitted other than discharge
summary.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted. In this case where the complainant`s Covid 19 claim was denied, the arguments
put forth by the respondent insurer were ::-1. The insured patient was admitted at the COVID
19 First Line Treatment Centre (CFLTC). 2. The condition of the patient ie, whether
symptomatic or asymptomatic & category of the condition ( A,B,& C) was silent in the
discharge card.3. No specific treatment was given to the patient and no documents were
submitted other than discharge summary. 4. The patient stayed at CFLT centre i.e. under
institutional quarantine for observation. Since CFLTC is not a hospital and lack the
infrastructure of a hospital as per policy clause, the claim was repudiated; are all tenable. I
therefore do not want to interfere in the decision of the respondent insurer in denying the
claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 13
th
day of September 2021.
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0258/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0375
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 13.09.2021
1.
Name and Address of the
complainant
:
Mrs. Preetha C
W/o Mr.Dinesh Kumar K E Nair, C/o
YOJAKA, 2nd Floor, ABCO Trade Centre,
NH-66, Kottara Chowki, Mangalore,
Dakshina Kannada, Karnataka - 575006
2.
Policy Number
:
P/181313/2021/004453

3.
Name of the Insured
:
Mrs. Preetha C
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
12.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
5. For the Complainant
:
Mrs. Preetha C (Online)
6. For the Insurer
:
Mr. Manu Mohan (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mrs. Preetha C is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that at the time of taking policy, it was informed by the concerned
person from the respondent insurer that the policy will be active immediately after
completion of 3months from the date of issue of the policy and the complainant will be
entitled for the policy benefits including OP charges immediately on activation. But on
submission of the claims they had rejected the same for reasons well known to them. The
quantum of relief sought is 80% to 90% of the claim amount.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant had taken a Star comprehensive Individual Health Insurance policy from
the insurer for the period from 08/09/2020 to 07/09/2021, for a Sum Insured of Rs. 5,00,000/-
vide policy No: P/181313/01/2021/004453, covering the complainant. The policy covers
hospitalization expenses incurred in India as an inpatient subject to the definitions, conditions
and exclusions, set there in. The Insured had registered 2 claims during the first year of the
policy.
It is submitted that in first claim No: CIR/2021/181313/2251823, the complainant was
admitted at Mangala Hospital & Mangala Kindey foundation, Mangalore on 14/02/2021 for
the treatment for Dysfunctional Uterine bleeding with anemia and D & C done on 14/02/2021
under GA and after the treatment she was discharged on the same day. After the treatments
were over, the complainant had submitted a completed claim form with medical certificate,
discharge summary, lab reports & bills for Rs. 22,041/- . The Ultra Sound scan of the abdomen
dated 14/01/2021 shows as below mentioned findings:-
1. Bulky Retroverted uterus
2. Endometrial thickness of 10-12 mms
3. Left ovarian simple cyst of 30 mms
4. Chronic calculus Cholecystitis
It is submitted that As per Waiting period 3(II)( H)of the policy: - “The company is not liable to
make any payment under this policy if the hospitalization is directly or indirectly for all
treatments (conservative. Interventional, laparoscopic and open) related to all diseases of
Cervix, Uterus, Fallopian tubes, Ovaries, Uterine Bleeding, Pelvic Inflammatory diseases
during the first two years of continuous operation of the insurance cover.” Based on the
available records, it was confirmed that the insured patient had underwent D& C for Uterine
bleeding and the same are excluded for a period of two years as per Waiting period 3(II)( H)
of the policy - “The company is not liable to make any payment under this policy if the
hospitalization is directly or indirectly for all treatments (conservative. Interventional,
laparoscopic and open) related to all diseases of Cervix, Uterus, Fallopian tubes, Ovaries,
Uterine Bleeding, Pelvic Inflammatory diseases during the first two years of continuous
operation of the insurance cover.” Since the present illness falls within the Waiting period
3(II)( H) of the policy, the insurer was not liable to consider the claim as per terms and
conditions of the policy. Hence the insurer had repudiated the claim and the same was
informed to the complainant on 10/03/2021. In second claim No: CIR/2022/181313/2531949,
the complainant was admitted at Justice K.S.Hegde Charitable Hospital, Mangalore on
27/04/2021, for the treatment for Cholelithiasis, Grade II hiatus Hernia, Acne Grade III, Fissure
in ano and underwent Laparoscopic Cholecystectomy & UGI Scopy done and after the
treatment, she was discharged on 03/05/2021. After the treatments were over, the
complainant had submitted completed claim form with medical certificate, discharge
summary, lab reports & bills of Rs.53,055/- . The discharge summary issued by Justice
K.S.Hegde Charitable Hospital, Mangalore clearly reveals that the patient had complaints of
Abdominal pain since 2 years . Moreover it was also noted that the patient had visited a local
hospital 2 years back where a scan was done and was told she had gallbladder stone. The
patient had underwent Hemorrhoidectomy twice – 10 years and 8 years back and surgery for
Fistula in ano 5 years back. As per Waiting period 3(II)( E),(F) & (J)of the policy: - “The company
is not liable to make any payment under this policy if the hospitalization is directly or indirectly
for all treatments (conservative, interventional, laparoscopic and open) related to Hepato-
pancreato-biliary diseases including Gall bladder and Pancreatic calculi, all types of
management for Kidney and Genitourinary tract calculi, all types of Hernia, Fistula, Fissure in
Ano, Hemorrhoids, Pilonidal Sinus and Fistula, Rectal Prolapse, Stress Incontinence during the
first two years of continuous operation of the insurance cover.” Based on the available records,
it was confirmed that the insured patient had underwent Laparoscopic Cholecystectomy for
Cholelithiasis, Grade II hiatus Hernia, Acne Grade III, Fissure in ano and the same is excluded
for a period of two years as per Waiting period 3(II)( E) ,(F) & (J )of the policy. Hence the insurer
had repudiated the claim and the same was informed to the complainant on 27/05/2021.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that while
taking the policy it was informed to her that on completion of 3-months from the date of
issuance of the policy, the complainant will be entitled for the policy benefits including OP
charges also. But when claims were submitted, they were denied. The complainant prayed for
settling claims. The Respondent Insurer submitted that the insured had registered 2 claims
during the first year of the policy. The first claim was for the treatment for Dysfunctional
Uterine bleeding with anemia and D & C done at Mangala Hospital & Mangala Kindey
foundation, Mangalore under GA, on 14/02/2021 and discharged the same day. It was
confirmed that the insured patient underwent D& C for Uterine bleeding and the same is
excluded for a period of two years as per Waiting period 3(II)( H of the policy. The second claim
was for the treatment for Cholelithiasis, Grade II hiatus Hernia, Acne Grade III, Fissure in ano
and underwent Laparoscopic Cholecystectomy & UGI Scopy done, at the Justice K.S.Hegde
Charitable Hospital, Mangalore on 27/04/2021 to 03/05/2021. The policy period was from
08/09/2020 to 07/09/2021. Based on the available records, it was confirmed that the insured
patient had underwent Laparoscopic Cholecystectomy for Cholelithiasis, Grade II Hiatus
Hernia, Acne Grade III, Fissure in ano and the same is excluded for a period of two years as
per Waiting period 3(II)( E) ,(F) & (J )of the policy. Hence the insurer had repudiated these
claims.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this case where the complainant`s claims were denied, the arguments
put forth by the respondent insurer were:-The complainant had two claims. The first one was
for the treatment for Dysfunctional Uterine bleeding with anemia and D & C done on
14/02/2021 under GA and discharged the same day at the Mangala Hospital & Mangala
Kindey foundation, Mangalore and the second one for the treatment for Cholelithiasis, Grade
II hiatus Hernia, Acne Grade III, Fissure in ano and underwent Laparoscopic Cholecystectomy
& UGI Scopy done from 27/04/2021 to 03/05/21, at the Justice K.S.Hegde Charitable Hospital,
Mangalore. The policy period was from 08/09/2020 to 07/09/2021. These two claims were
denied as the same were excluded for a period of two years as per Waiting period 3(II)( E) ,(F)
& (J )of the policy; are all tenable.
I therefore do not want to interfere in the decision of the respondent insurer in rejecting these
claims.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 13
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0260/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-048-2122-0362
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 15.09.2021
1.
Name and Address of the
complainant
:
Mrs. Bincy George,
Mayamparambil Thalappara
Thalayolapatambu P O Kottayam
686605
2.
Policy Number
:
57170502010000757
3.
Name of the Insured
:
Mrs. Bincy George
4.
Name of the Insurer
:
The National Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
05.07.2021
6.
Nature of complaint
:
Partial rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
10.09.2021
9.
Parties present at the hearing
1. For the Com-
plainant
:
Mrs. Bincy George (Online)
2. For the Insurer
:
Mr. Rajesh Srinivasan

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding partial rejection of mediclaim. The
complainant, Mrs. Bincy George is the policyholder.
1. Averments in the complaint are as follows:
The Complainant submitted that she was holding a health insurance policy of the respondent
insurer bearing policy No. 57170502010000757. On 10.03.2021, the complainant nsent a
request for approval for a Hysterectomy surgery to the insurer. As per their approval of
Rs.50,000/- , she got admitted in the hospital on 17.03.2021 and the surgery was done on
18.03.2021. She got discharged on 19.03.2021. The discharge bill for Rs.1,41,929/- was
submitted for approval by 10.30 to the company. But waiting during the whole day the
company allowed only Rs.46,800/- by evening at 7.00 pm. When enquired about the reason
for reduction of the amount, it was known that she was cheated.
The complainant had taken a policy during 2009 for a sum insured of Rs.50,000/-. During 2017
it was enhanced to RS.3,00,000/-. It was informed by the respondent insurer that for claiming
the enhanced amount of 3 lakh , she had to wait for 48 months. When she approached for
the approval, the company concealed this information and told her that she can claim for 3
lakhs. Only believing them, she had undergone the surgery.
The date on which the surgery was done ie on 18.03.2021, there was only 3 months left to
complete the 48 months duration. If it was informed to her earlier, she wouldn’t have gone
for the surgery. She could have waited for three months. It is submitted that the complainant
is holding the policy for the past 13 years and the respondent insurer has made huge financial
liabilty. Henc eshe requests this forum to intervene and find a proper solution to her issue.
2. The Respondent Insurer entered appearance and filed a self-contained note. It is submitted
that this is a grievance in respect of short-payment of claim made under National Medicalim
policy. They have issued the policy bearing No. 57170502010000757 for the period
15.06.2020 to 14.06.2021 to Mr. George Mathew covering the following members.
Name Age Sum Insured
1. Mr George Mathew 55 yrs Rs.3,00,000/-
2. Mrs. Bincy George 49 yrs Rs.3,00,000/-
3. Ms. Sneha Mariya George 22 yrs Rs.1,00,000/-
Mrs Bincy George was admitted in VPS Lakeshore hospital on 17.03.2021 for bleding PV for
past 25 days-AUB. It is observed form the medical records that she was treated for ‘Thickened
Endometrium” during the hospitalization. Also the attending Doctor has confirmed that
Mirena Insertion was previously done to her in October 2014 for treating heavy bleeding. The
insured was having National Medicalim policy with the insurer from 2009 for a sum insured of
Rs.50,000/- each till 2016.The the sum insured was increased to Rs.3,00,000/- for the
complainant and for his spouse and Rs.1,00,000/- for his daughter with effect from 2017.
As per the policy condition No.5.17 –Enhancement of Sum insured- Sum insured under the
policy can be enhanced only at the time of renewal. Sum insured can be enhance up to
Rs.5,00,000/- subject to discretion of the company. The waiting period and conditions as
mentioned under Exclusions4.1,4.2 and 4.3 will apply to incremental portion of the sum
insured. As per the Exclusion No & 4.1- The Company shall not be liable to make any payment
under the policy in respect of any expenses incurred in connection with or in respect of:
4.1- Pre- existing diseases- All pre-existing diseases until 48 months of continuous coverage
has elapsed. Any complication arising from pre-existing ailment/disease/injuries will be
considered as a part of the pre-existing health condition of disease.
Observation:- The insured has increased the sum insured from Rs.50,000/- to Rs.3,00,000/-
wef 2017. As such the existing policy, in which the claim is made, is 4
th
year policy. Since the
waiting period and the exclusions until 48 months will be applicable to the incremental
portion of the sum insured, the claim was processed and settled for Rs.46,800/- based on the
earlier sum insured of Rs.50,000/- with cumulative bonus. Since the claim was settled on the
basis of the policy condition and there is no short payment of claim.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that she
had taken a policy during 2009 for a sum insured of Rs.50,000/-. During 2017 it was enhanced
to RS.3,00,000/-. It was informed by the respondent insurer that for claiming the enhanced
amount of 3 lakh , she had to wait for 48 months. When she approached for the approval, the
company it was informed that she can claim for 3 lakhs. Only believing them, she had
undergone the surgery. The date on which the surgery was done ie on 18.03.2021, there was
only 3 months left to complete the 48 months duration. If it was informed to her earlier, she
wouldn’t have gone for the surgery. She could have waited for three months. It is submitted
that the complainant is holding the policy for the past 13 years and the respondent insurer
has made huge financial liabilty. The Respondent Insurer submitted that there is a waiting
period of 48 months for the enhanced sum insured to be eligible for payment for certain
ailments. The complainant had undergone hysterectomy surgery and the same comes under
the ailments which need to complete 48 months to become admissible. The sum insured was
enhanced during 2017 and hence she was eligible for earlier sum insured of Rs.50,000/- and
the claim was settled for Rs. 46,800/-. Hence the respondent insurer has settled the claim as
per terms and conditions of the policy.
4. On hearing both the parties and on scrutiny of the documents, it is found that the
respondent insurer has settled the claim rightly as per terms and conditions of the policy. The
complainant was having a sum insured of Rs.50,000/- since 2009. The sum insured was
enhanced to RS.3,00,000/- during 2017. She had undergone hysterectomy surgery during
18.03.2021. As per policy terms and conditions this surgery has a waiting period of 48 months.
There was three months more to complete 48 months. The enhance sum insured will become
payable only after completing the waiting period and hence the claim was settled for
Rs.46,800/- based on the previous sum insured. As per the policy terms and conditions there
are certain ailments which need 24/36/48 months waiting period. It was informed that a claim
was settled for Hernia operation within the enhanced sum insured which needed only
completion of 24 months. The policy is clear about the details and the decision of the
respondent insurer to settle the claim based on the previous sum insured is justifiable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 15
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0261/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(c) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-048-2122-0350
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 15.09.2021
1.
Name and Address of the
complainant
:
Mr. S Vijayakumar,
Vrindavan TC-15/1680 Lekshmi

Nagar B 8/5 Kesavadasapuram
Thiruvananthapuram 695004
2.
Policy Number
:
570201502010001595
3.
Name of the Insured
:
Mr. S Vijayakumar
4.
Name of the Insurer
:
The National Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
05.07.2021
6.
Nature of complaint
:
Renewal of policy
7.
Amount of relief sought
:
--
8.
Date of hearing
:
10.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Consent Given
2. For the Insurer
:
Mr. Sooraj V (Online)
AWARD
This is a complaint filed under Rule 13 1(c) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding renewal of policy. The complainant, Mr.
S Vijayakumar is the policyholder.
1. Averments in the complaint are as follows:
The Complainant submitted that he was holding National Parivar policy bearing No.
570201502010001595. He is a retired principal, Senior citizen. The policy was renewed
without his eligible 5% no claim discount. The case regarding the renewal of his policy was
taken up as early as 19.01.2021 with the Senior citizen desk of the company and a reminder
was sent on 30.01.2021. There was no response and he represented his case to the consumer
support wing, with a copy to Senior citizen desk of the company on 05.02.2021 followed by
sending another reminder on 09.02.2021. Inorder to have continuous coverage, he renewed
the policy online on 11.02.2021, with only his digital discount. He represented the case with
the local Manager of the company on 18.02.2021 requesting him to refund the excess
premium collected, deny his eligible discount.
The late reply received from the Manger on 15.03.2021 did ot provide a convincing reply to
his grievance and was forced to regiser his case with the Grievance cell of the Company on
21.03.2021. Cosequently, the Manager sent a mail on 21.03.2021. Consequently, the Manager
sent a mail on 31.03.2021stating his eligibility of a new type of discount of 3% arising out of
deletion of maternity/infertility cover amounting to Rs.1176/- and repeating the argument
that his no claim discount has already been adjusted.
However as requested in the mail, he furnished his bank details for the refund of the new
found eligible discount and stated that his grievance still stands and cannot be considered as
closed.Till date the new found discount has neitherbeen credited in his account nor have
received any mail from the company after 31.03.2021. He again approached the IRDAI on
05.05.2021 with no favourable response till date. He received a message from the Grievance
cell on 28.05.2021 stating thathis grievance is closed.
The complainant stongly believe that his eligible discount of 5% of the premium, being the no
claim bonus is denied to him. The authorities of the company have not evaluated his policy
properly, even though he had taken up the case much earlier.The finding of the new additional
3% discount was known to him only because he reaised a complaint. This forum can imagine
the condition of lakhs of policy holders like him who are denied with their eligible discount
form a Government company.
The complainant’s contention is that all his eligible discounts were not considered while
renewing the policy. Any adjustment made , as claimed by the company, must be reflected in
the policy. His policy shows only the digital discount. The eligible discounts denied to him with
cgst/sgst/cess has to be refunded. It is also submitted that all the deduction/addition to the
premium should be shown in the polciy. By going through the documents, the complainant
hope that this forum can understand the stress and strain a senior citizen like him must go
through to forcefully avail eligible discounts from Government Company. The complainanat
request this forum to consider his grievance.
2. The Respondent Insurer entered appearance and filed a self-contained note. It is submitted
that the Insured renewed his Policy online vide National Parivar Mediclaim Policy No
570201502010001595 for the period 11/02/2021 to 10/02/2022. He remitted a Total
Premium of Rs.39, 908/-
Premium was revised upwards by the Company under the National Parivar Mediclaim Policy
with effect from October 1st 2020 . Accordingly, premium payable under the aforesaid Policy
net of all eligible discounts is Rs.38742/- (Rs. 32557 Plus GST and Kerala flood cess).
The following are the discounts available under the National Parivar Mediclaim Policy:
“Rest of India” Zone Discount@20% in Premium. This has already been availed by the Insured
during online renewal
No Claim Discount@5% in Premium. The Insured has already availed the same during online
renewal
Online Renewal Discoun[email protected]% in Premium. The Insured has already availed the same
Discount@3% on individual premium in lieu of no Maternity/Infertility cover for Insured and
spouse over forty five years of age. However, this discount amounting to Rs.1176/- could not
be given due to a system error
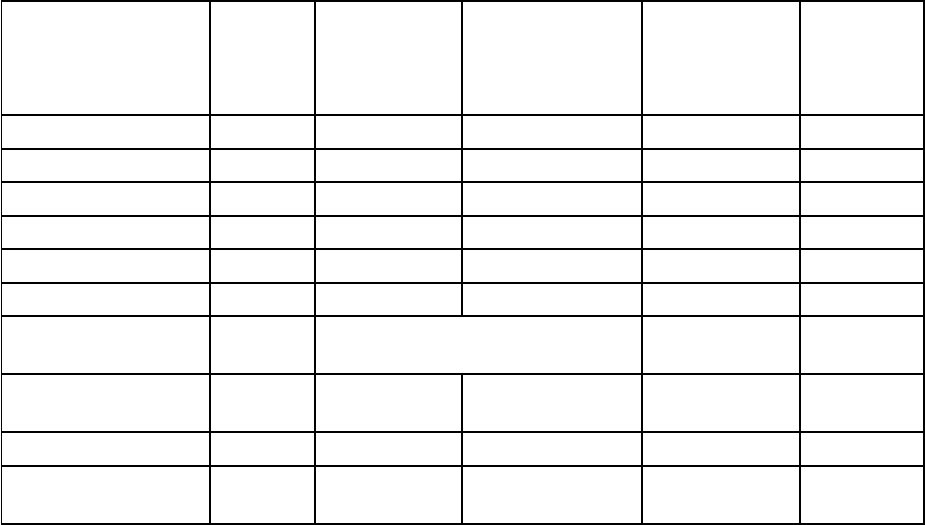
Long Term Discount on Total Premium (for policy period of two /three years). The subject
Policy being valid for a duration of one year only, this discount is not applicable under the
same
Given below is the calculation for arriving at the final premium under the Policy
NAME
AGE
PREMIUM
AS PER THE
CHART
LESS ZONE
DISCOUNT 20 %
LESS NO
CLAIM
DISCOUNT
5%
Less
maternity
discount
S VIJAYAKUMAR
67
35002
28001
26601
25802
SMT MANJU
57
8670
6936
6589
6391
M AARATHY
31
1576
1261
1198
1198
TOTAL
33391
LESS 2.5% DIGITAL DISCOUNT
Rs 834/-
32557
18%GST+1%
FLOOD CESS
6185
TOTAL
PREMIUM
38742
We have already addressed the Insured’s complaint vide our e mails dated 15/03/2021 &
31/03/2021. As is evident from the foregoing computation, we have already given the Insured
No Claim Discount of 5%. Hence, there is no substance to the Insured’s complaint that No
Claim Discount was not availed by him.
However, the Insured and his spouse are entitled to Discount in Premium@3% on individual
premium in lieu of no Maternity/Infertility cover, net of which premium that ought to been
charged is Rs.38742/- . Hence, we are prepared to refund the difference of Rs.1166/- to the
Insured.
Submitted for the kind consideration of Hon’ble Insurance Ombudsman .
3. I heard the Respondent Insurer. The Complainant was not able to attend the hearing due to
ill health and gave consent to this forum to consider his case on its merits. The Respondent
Insurer submitted the details of premium computation and accepted that there was a system
error due to which a discount in Premium@3% on individual premium in lieu of no
Maternity/Infertility cover, was not given. They are now ready to allow the same.
4. On hearing the respondent insurer and on scrutiny of the detailed computation, it is found
that the premium calculation is correct as per the chart given in the self-contained note, which
is self-explanatory, except for Discount in Premium@3% on individual premium in lieu of no
Maternity/Infertility cover. Now the respondent insurer is ready to refund the difference in
premium collected to the complainant.
In the result, an award is passed, directing the Respondent Insurer to pay an amount of
Rs.1166/-, within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 15
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0262/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-018-2122-0348
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 15.09.2021
1.
Name and Address of the
complainant
:
Mr. James Jose
Kattakayam 39/5966 14th cross road
extn Panampilly Nagar Ernakulam
682036
2.
Policy Number
:
2861100878845200000
3.
Name of the Insured
:
Ms. Rose James
4.
Name of the Insurer
:
HDFC ERGO General Insurance
Company Ltd.

5.
Date of receipt of Complaint
:
02.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
10.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. James Jose (Online)
4. For the Insurer
:
Mr. Aneesh Bhaskaran (Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. James Jose is the policyholder.
1. Averments in the complaint are as follows:
The Complainant submitted that he had taken a Covid Kavach insurance policy for his
daughter Rose James from the respondent insurer for an amount of Rs.3,00,000/-, under
policy No. 2861100878845200000. When his daughter was tested covid positive, she was
asymptomatic and hence not admitted to hospital for treatmenr. However after covid
infection, while she was working in her office, she developed breathing problems and other
illnesses and hence was admitted to an ayurvedic hospital for treatment of post covid illnesses.
Before admitting to the hospital, they informed the respondent insurerand took their
permission so as t o get reimbursement of treatment expenses. However after treatment ,
they submitted bills for Rs.97238/- for reimbursement, the respondent isurer rejected the
claim and refused to make any payment which he feel is unfair and not justifiable. Hence he
has approached this forum for directing the insurer to reimburse the expensesof Rs.97238/-
incurred towards treatment of covid.
2. The Respondent Insurer entered appearance and filed a self-contained note. It is submitted
that at the Outset, we are agreeable to submit to the mediation of the Hon’ble Insurance
Ombudsman in the instant complaint and for him to give his recommendation for the
resolution of the Complaint.
With reference to the Complaint we submit as follows:
Insured had taken a Corona Kavach Policy vide Policy No 2861 1008 7884 5200 000 for the
period from 01/10/2020 To 12/07/2021, waiting period 01/10/2020 To 15/10/2020, Policy
Period from 16/10/2020 To 12/07/2021. Policy was taken in favour of Ms. Rose James. For SI
5 lac., with no PED.
That, Insured 26 yr., had made a Reimbursement claim on 28/Apr/2021 which was registered
vide Claim No.R-HS21-12404770. As per the Discharge Summary, Insured was admitted from
03/Mar/2021 to 21/Mar/2021 with C/o of Pain in neck region and difficulty in breathing at
Narayanalyam, Ayurvedic Chikithsa Kendra, Thiruvengappura.
It is the Complainant version that, they had made a representation to the Insurer stating;
Insured had tested Positive in the first week of February/2021, as she developed breathing
difficulty she got admitted at an Ayurvedic hospital for treatment which the complainant
confirmed to have informed on 25/Feb/21 and taken the consent of this Insurer and later she
got admitted. The averment of the Insured is only a self-serving version. The policy of
Insurance is a contract between the Insured and the Insurer. Insured being a prudent person
would have read and construed the policy terms and conditions and no were in the policy
terms it reads about any provision for the insured to make a representation to the insurer
and considering it as a self-approval for making a claim. Further, the Insurer has not given any
consent to the alleged representation made by the complainant.
That the Policy terms clearly reads the requirement to be met while notifying a claim, mere
sending a letter to the Insurer will not meet the need as per the policy terms and conditions.
As policy is a contract the Insured is bound to adhere to the terms and conditions.
That after proper deliberation and careful perusal of the claim documents, we had denied the
claim on the ground that insured is claiming for Ayurveda expenses post COVID with complains
of Neck pain, LBA and Breathing problems. The treatment underwent is not related to Covid
as per policy T&C. Hence, claim was denied.
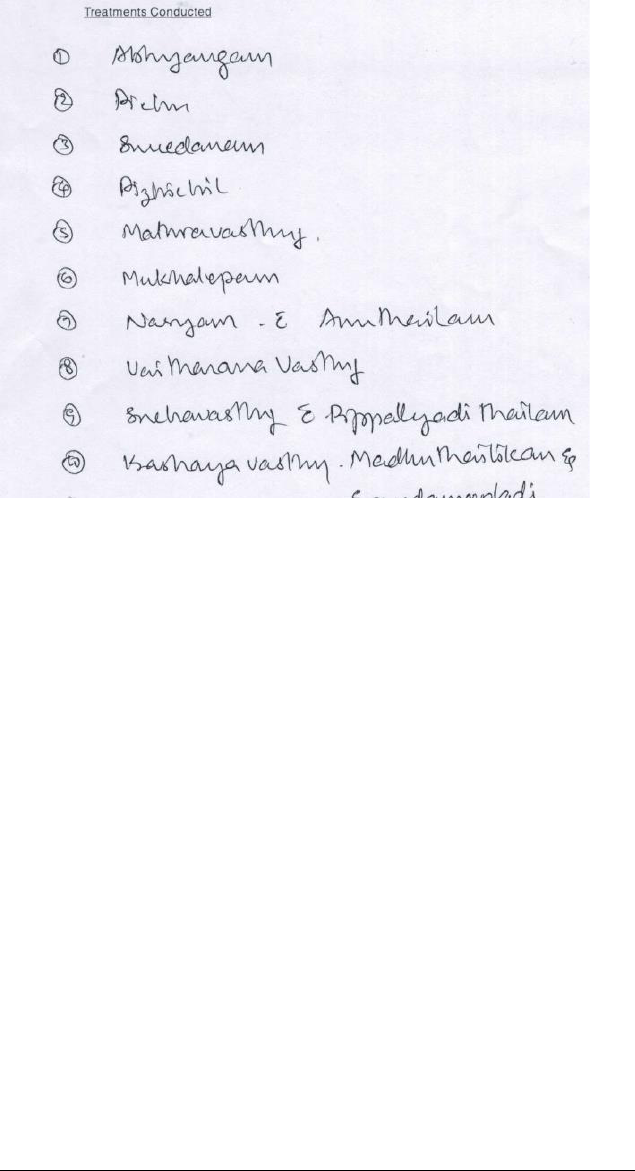
It is evident from the Discharge Summary :
1. Abhyanga : is a massage that's done with warm oil. The oil is applied on the entire body,
from the scalp to the soles of your feet
2. Mukhalepam is a kind of skin care therapy where, different types of herbs, medicated
plants, oils, ghee, juices of plants, fruits are used for skin protection.
3. Nasyam : purifying the head region and nasal passages thereby eliminating Headaches,
Migraine and Sinus related disorders.
4. Anutailam : It is used in the treatment of headache, hair fall, premature greying of hair,
migraines and diseases related to the five sense organs. It is also helpful in balancing the
hormone producing glands in the head and neck area. Avoids greying and falling of hair.
5. Vaitarana Vasti: is a form of Niruha Vasti i.e. decoction enema. In any decoction enema,
rock salt, honey, oil / ghee, paste of medicines,
6. Sneha Vasti is one of the body de-toxification treatments in Ayurveda under Panch-
karma. ( Insured was administered , Pippalyadi Thailam which is an Ayurvedic oil used
externally to treat Piles, Gout, Back ache, Spondylosis, Lower Back and Limbs)
7. Kashaya Vasti is used to treat constipation, neurological ailments, paralysis, flatulence,
lower backache, gout and rheumatism
From the treatment it is evident; Insured had not undergone any specific treatment for COVID.
Further, Insured had to take the treatment at a Government authorized diagnostic center.
NARAYANALAYAM AYU RVEDA CH IKITSAKENDRAM ASOKALAYA, is a government accredited
centre, the Insured is subject to proof of the same.
The policy terms read:
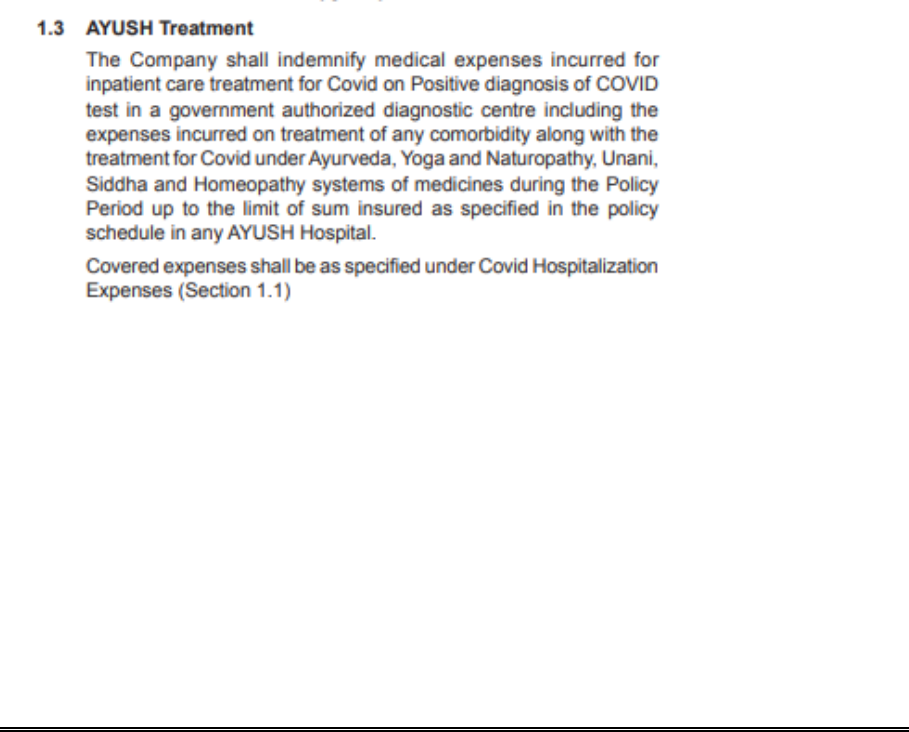
Hence, it is evident the treatment was not for COIVD related treatment. Hence, we had denied
the claim as the condition did not meet the requirement as per the policy terms and
conditions. Seems, the treatment was more related to Migraine and related ailments.
That, the claim was rightly denied on the ground that, as per submitted documents it is
evident, the treatment underwent is not related to COVID, Hence, the claim was denied.
The Claim was denied as per the policy terms and conditions. All other averments made by
the Insured are herewith denied.
The respondent further submits that the Complainant has approached this Hon’ble
Ombudsman to make illegal enrichment from this respondent. There is no deliberate attempt
on the part of this respondent to arbitrarily deny the claim of the Insured.
The Company reserves its right to adduce additional evidence as and when required.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
daughter was tested covid positive and as she was asymptomatic and hence she was not
admitted to hospital for treatmenr. After covid infection, she developed breathing problems
and other illnesses and hence was admitted to an ayurvedic hospital for treatment of post
covid illnesses. The claim for reimbursement was rejected by the insurer. The Respondent
Insurer submitted that the insured suffered from covid during the first week of February and
she developed breathing difficulty and she got admitted at Narayanalyam, Ayurvedic Chikithsa
Kendra, Thiruvengappura for treatment. From the treatment taken at the Ayurveda centre, it
is evident that the Insured had not undergone any specific treatment for Covid. The policy
issued is Corona Kavach policy, which is meant for treatment of covid. Hence the claim was
repudiated.
3. On hearing the complainant and the respondent insurer and on scrutiny of the
documents, it is clear that the treatment taken at the ayurvedic centre was not for
covid. When the insured was diagnosed covid positive, as she was asymptomatic, she
didn’t get admitted to any hospital. Later she had sought treatment for breathing
difficulty in the Ayurvedic centre. The policy is Corona Kavach policy, for treatment of
Covid.
4. There is no pre or post hospitalization expenses offered under this policy. As such the
claim was repudiated by the respondent insurer. The decision is justifiable and hence
I do not want to interfere in to their decision.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 15
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0263/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0367
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 15.09.2021
1.
Name and Address of the
complainant
:
Mr. Shovin Vincent
Irumban House, Panimkulangara
Lane, Ayyanthole P O, Thrissur -
680003
2.
Policy Number
:
CRP-61-20-7010802-00-000
3.
Name of the Insured
:
Mr. Shovin Vincent
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
12.07.2021

6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
9.
Parties present at the hearing
1. For the Complainant
:
Settled before hearing
2. For the Insurer
:
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Shovin Vincent is the policyholder.
1. Averments in the complaint are as follows:
The Complainant submitted that he was holding a Corona Rakshak policy with the respondent
insurer bearing policy No. CRP-61-20-7010802-00-000. He was diagnsed covid positive nad
was hospitalised in Aswini Hospital, Trichur.He had submitted the documents to the insurer
for reimbursement. But they required some more documents and those were submitted.
Later as there was no reply he approahed the Grievance cell and they informed that it will be
settled within 10days. Even after the period, the claim was not settled. Hence he has
approached this forum for getting the claim settled.
2. The Respondent Insurer entered appearance and filed a self-contained note. It is submitted
that the company had issued Corona Rakshak Policy-CRP-61-20-7010802-00-000 for the
period from 24/07/2020 to 05/05/2021 in the favour of Mr. SHOVIN. That the total claimed
amount was INR 250000. That the claim was closed by us due want of additional claim
documents. That we have received all the requisite documents which has fulfilled our
requirement therefore we have proceeded ahead to settle the claim.
The details of the payment is as follows –
Payee Name : Mr. Shovin
Payment Date : 28th July 2021
Payee Bank Name : Canara Bank
NEFT Payment Reference No. : 107285146749
Amount : INR 2,50,000/-
That the letter was sent to insured on confirmation of the claim payment processed to his
bank account through NEFT.
3. As the respondent insurer informed this forum before the Hearing date that they have
settled the claim, no hearing was conducted. The complainant also confirmed that he has
received the claim amount of Rs.2,50,000/-.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 15
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0264/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0366
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 15.09.2021
1.
Name and Address of the
complainant
:
Mr. Senthil Kumar
Chandramukham, Poovanvila
Paloorkonam, Nemom P O,
Thiruvananthapuram - 695020
2.
Policy Number
:
CRP-10-20-7027204-00-000
3.
Name of the Insured
:
Mr. Senthil Kumar
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
12.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
10.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Senthil Kumar (Online)
2. For the Insurer
:
Ms. Akamsha Saxena(online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Senthil Kumar is the policyholder.
1. Averments in the complaint are as follows:
The Complainant submitted that he was holding Corona Rakshak policy of the respondent
insurer bearing policy No.CRP-10-20-7027204-00-000. He was admitted in the covid care
Hospital from 01-05-2021 to 07-05-2021. He had submitted the Covid positive report, Original
Discharge summary and indoor records of the Hospital for consideration of reimbursement.
The respondent insurer rejected the claims arbitrarily and without following the guidelines of
Insurance Regulator IRDAI with regard to the claim settlement.
Due to sudden surge of Corona Virus infection IRDAI had also issued Guidelines vide Circular
No. IRDAI/HLT/MISC/CIR/190/07/2020 dated 16.07.2020 that a makeshift or temporary
Hospital set up any of the centre and the state Government- “a makeshift or temporary
Hospital shall be regarded as a Hospital or network provider Hospital under the definition of
terms and policy of Health policy. In view of the guidelines of the insurance regulator, the
complainant was admitted in the permitted Covid care centre and also qualify all other terms
and conditions of the policy.
It is prayed that this forum may mediate and give instruction to the respondent insurer to
consider and settle the claim reported under the policy.
2. The Respondent Insurer entered appearance and filed a self-contained note. It is submitted
that the respondent company had issued Corona Rakshak Policy bearing Policy No- CRP-10-
20-7027204-00-000 for the period from 15-Aug-20 to 26-May-21. That the total claimed
amount was INR 250000. That patient was diagnosed with Covid-19 on 26-Apr-20, patient was
transferred to CFLTC for further treatment. That the insured had undergone hospitalization at
Directorate of Medical Education, for “Covid-19 positive Category B. That as per discharge
summary there were no clinical features (symptoms or signs) that necessitated hospitalization.
Patient was admitted on 05th day at CFLTC. The patient presented to the hospital with fever,
cough and headache. At hospitalization, the patient’s vital parameters were all within normal
limits.
That, as per Operative Clause of the policy, the admission has to be as per guidelines
specified by MOHFW.
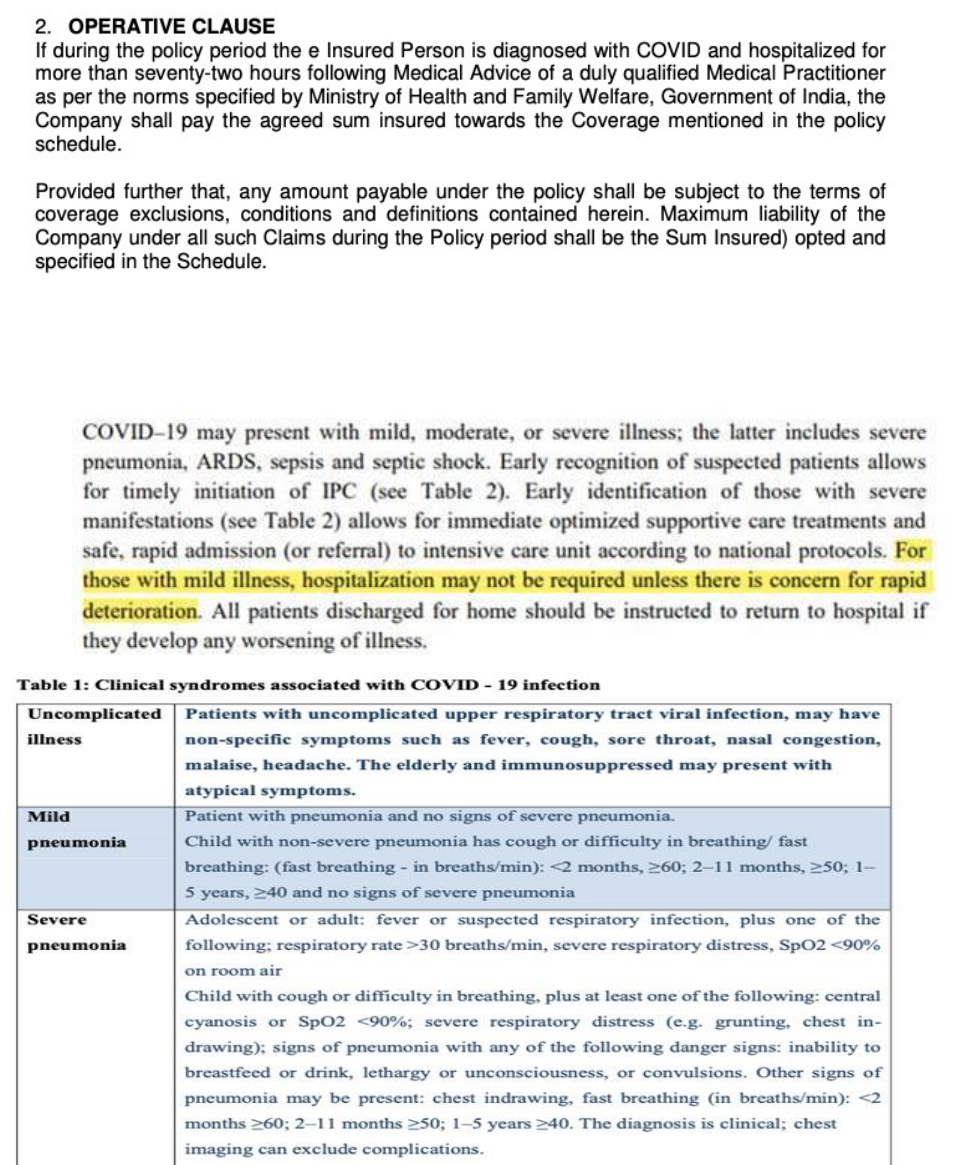
That, as per Circular issued by Government MOHFW dated 17th-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1].
Thus, taking cognizance of all the above factors and govt. guidelines, the claim was repudiated.
Other supporting policy clause is mentioned below:
6.1. Investigation & Evaluation (Code- Excl04)
i. Expenses related to any admission primarily for diagnostics and evaluation purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current
diagnosis and treatment.
The Discharge summary reveals that the complainant was suffering from Renal calculi and he
was shifted from FLTC for consulting the Urologist. This condition was not disclosed while
taking the policy. The claim was repudiated based on non-disclosure of a material fac as Non-
disclosure of material fact makes the policy null and void.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
was diagnosed covid positive and was admitted in First Line treatment Centre for 5 days and
as he had severe body pain and other complications, he was shifted to the Medical college
Hospital ( Directorate of Medical Education). Even though he had submitted all relevant
documents his claim for reimbursement was repudiated by the insurer. The Respondent
Insurer submitted that the complainant was admitted to hospital on diagnosing covid positive.
His vitals were normal. He could have treated at home quarantine and there was no need for
hospitalization. Moreover, he was suffering from renal calculi and he was referred to the
Urologist and was treated for the same. The reason for repudiation of the claim is that the
complainant had concealed the fact of suffering from renal calculi. Hence the claim is not
admissible.
4. I heard both parties and scrutinized the documents. As per the discharge summary, the
patient was asymptomatic for 5 days and hence discharged to home for completion of
quarantine. His vitals were normal and he had not undergone any active line of treatment.
There was no need for hospitalization. He could have home quarantined. As per circulars
issued from time to time by the Central / State governments, patients with mild symptoms
are to be home quarantined. The complainant alleged that he was having severe pain and
that’s why he was shifted from FLTC. The discharge summary states that the complainant was
suffering from renal calculi and he was referred to Urologist. It is clear that he had severe pain
due to this condition and hence he was referred to the specialist. On discharge he was advised
to consult the Urologist after one week. The complainant while taking the policy concealed
the fact of renal calculi. The contract of insurance is contract of utmost good faith. The
complainant should have disclosed to the respondent insurer about the same. The insurer
should have either accepted his risk with certain endorsements/waiting period and with
loaded premium or wouldn’t have accepted the risk. Believing that the insured has declared
his good health condition, the policy was issued. Once, when the respondent insurer found
that the insured has concealed a material fact, the claim was repudiated for non-disclosure.
The decision of the respondent insurer to repudiate policy is based on policy terms and
conditions and justifiable. Hence, I do not want to interfere in to their decision.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 15
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0266/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1 (b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0197
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 16.09.2021
1.
Name and Address of the
complainant
:
Mr. Bibin Mathew Babu
131, Ramalingam Colony, Near
Avinashilingam College, Coimbatore -
641043
2.
Policy Number
:
P/181216/01/2021/007991
3.
Name of the Insured
:
Mr. Bibin Mathew Babu
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
26.05.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
05.08.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Bibin Mathew Babu (Online)
4. For the Insurer
:
Mr. Manu Mohan (Online)

AWARD
This is a complaint filed under Rule 13 1 (b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Bibin Mathew Babu is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he took Corona Kavach Policy from Star health insurance for the
total amount of insurance for 5 laks. He was diagnosed with Covid on 06/02/2021. He was
requested by the health authorities to visit any hospital for consultation.
When he visited the hospital on 07/02/2021 for consultation he was requested to get himself
admitted in the hospital immediately by the doctor at the hospital for further treatment.
He was treated in the hospital for the next 5 days. And after that home quarantine of 14 days
was advised from the date of discharge from the hospital.
His insurance policy was specifically for Corona cover. He had even opted for extra optional
cover by paying an extra amount for the policy. His claim was however rejected by the Ins. Co.
He is not a qualified medical professional to judge or go against the recommendation of a
qualified doctor. He was admitted to hospital based on doctor’s advice. All he did was to heed
to doctor’s advice and admit himself to the hospital.
He believes any common man like him would have done the same in similar scenario and
followed doctor advice.
Hence he requests the Ombudsman to intervene in this issue and help him to get his claim of
Rupees 85,000/-
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that Mr. Bibin Mathew Babu had taken Corona Kavach policy for the period from 29/10/2020
to 10/08/2021 for a Sum Insured of Rs 5,00,000/- vide policy No: P/181216/01/2021/007991.
It is submitted that in claim No: CIR/2021/181216/2238608, the complainant was admitted at
KMCH Institute of Health Sciences and Research, Coimbatore on 07/02/2021 for the
treatment for Covid 19 – Category mild and after treatment he was discharged on 11/02/2021.
After the treatment was over, the complainant has submitted completed claim form,
Discharge summary, Bills of Rs. 83,892/- and Lab reports.
It is submitted that the discharge summary issued by the KMCH Institute of Health Sciences
and Research, Coimbatore clearly reveals the Clinical findings that:-
1. Afebrile (98.4F)
2. Pulse rate:90/Mt (Normal Range: 60 -100 beats per minute).
3. BP( Blood Pressure):120/90 mm of HG
4. SPO2 :- 98% ( Normal Range: 94% to 100%)
5. CVS: S1S2(+)
Moreover in the discharge summary it is clearly noted status as “Category Mild” and vitals are
stable.
It is submitted that the patient status as “Category Mild” and vitals are stable & no active line
of treatment was given but only vitamins tablets prescribed. Here Covid positive has been
diagnosed but the patient vitals are stable, Respiration rates, SPO2, Pulse rate, Temperature
seems normal , hospitalization was not warranted and he was under observation. There were
no symptoms requiring inpatient care/ admission in a hospital. Corona Symptoms like fever,
Sore throat, Headache ,Chills Loss of smell or taste, Congestion or runny nose, Nausea or
vomiting, Diarrhea or breathing difficulty were absent and hence it doesn’t require admission
in a hospital. No specific treatment given to the patient. In a Covid case, the primary
symptoms are fever, Sore throat, Headache, Chills Loss of smell or taste, Congestion or runny
nose, Nausea or vomiting, Diarrhea and low level of SPO2. SPO2 is oxygen saturation, is a
measure of the amount of oxygen-carrying hemoglobin in the blood relative to the amount of
hemoglobin not carrying oxygen. The body needs certain level of oxygen in the blood or it will
not function as efficiently. In fact, very low levels of SpO2 can result in very serious respiratory
symptoms. The normal oxygen level which is measured by a pulse oximeter usually
range from 95% to 100%. The Blood oxygen levels below 90% are considered low (hypoxemia)
and hence oxygen support is mandatory in such cases. But in this case the insured person’s
SPO2 recorded value is 98% i.e., well within normal range only.
Based on the available medical records it is clear that the patient`s vitals are stable and stayed
at hospital only for observation/ Monitoring i.e. under isolation and it doesn’t require
admission in a hospital. Hence the insurer had repudiated the claim and the same was
informed to the insured on 20/03/2021.
Further on escalation to grievance department another expert team reviewed and rejection
justified.
In short, the Company has rightly repudiated the claim after application of its mind to all
material facts, evidences and circumstances affecting the claim.
Hence, pray that may be totally exonerated from any liability under the claim.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
was admitted in the hospital on Doctor’s advice and he wishes to know as to why his claim
was rejected. He also wanted to know if he would be entitled to any penalty for non-payment
of his claim. . The Respondent Insurer submitted that the complainant’s SpO2 was normal ,
so also other vitals and chest was clear. He was treated only on oral medicines and Vitamins.
4. I have heard both the sides and perused the documents. The complainant was admitted
with c/o nasal block, post nasal drip 1 week, loss of smell 1 day. There was no h/o fever, sore
throat, cough, breathlessness or burning abdominal pain, vomiting, loose stools , loss of taste.
On admission his SpO2 was 98% and Vitals were noted as normal. He was diagnosed as Covid
Cat Mild. The claim was repudiated by the respondent since the complainant could have been
home quarantined as per Govt. guidelines on Covid Protocol.. However, I am of the opinion
that the claim is tenable as he incurred expenses for the investigations and treatment at the
hospital for his Covid symptoms amidst the pandemic situation.
The complainant is not entitled to any penalty from the respondent insurer for non-settlement
of his claim.
The admissible claim amount is Rs.75,964/- after deduction of non-medicals and non-payables.
In the result, an award is passed, directing the Respondent Insurer to pay an amount of Rs.
75,964/- , within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 16
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
Copies to:
Mr. Bibin Mathew Babu,
131, Ramalingam Colony, Near
Avinashilingam College,
Coimbatore - 641043.
The Manager,
Star Health & Allied Insurance Co.Ltd.,
Zonal Office,
4
th
Floor, Carmel Towers,
Cotton Hill P.O.
Vazhuthacaud,
Thiruvananthapuram 695 014.
AWARD NO.IO/KOC/A/HI/0267/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-055-2122-0386
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 16.09.2021
1.
Name and Address of the
complainant
:
Mr. Bobin Chandra B
House No 54 A TC 3/2376 3 Near Siso
Books Balasubramanian Lane Pattom
Thiruvananthapuram Kerala 695004
2.
Policy Number
:
13-20-0155627-00
3.
Name of the Insured
:
Mr. Bobin Chandra B
4.
Name of the Insurer
:
Aditya Birla Health Insurance Company
Limited
5.
Date of receipt of Complaint
:
09.06.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
9.
Parties present at the hearing
1. For the Complainant
:
Settled before hearing
2. For the Insurer
:
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim (Covid). The
complainant, Mr. Bobin Chandra B is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he held an active policy 13-20-0155627-00 under Aditya Birla
Insurance from 30/09/2020 . He was admitted in Hospital due to severe Covid19 on 22 Jan
2021. He was hospitalised for 10 days due to covid. The insurance had cashless facility with
hospital and when he enquired they said the facility is not available now even though the
hospital is listed under cashless facility. He has submitted all the hospital bills in the first week
of February itself. The insurance authorities have asked for further hospital documents and I
have submitted twice. Later he came to know that his insurance claim was rejected for no
reason. He is an ordinary citizen and the insurance company is purposely denying insurance
claims citing technical reasons which he is unaware as a customer.
When he took the policy , he underwent a complete medical test under the clinic mentioned
by Aditya Birla Insurance company which checks BP, cholesterol etc and he has taken the same
under their instruction and he was healthy . He did not receive any calls from insurance
company after the initial checkup.
He used to visit a family doctor in the past as part of periodic visit and his cholesterol level
was in the border line and doctor advised not to take any medication for the same and doctor
mentioned exercise and diet since his BMI is perfect and the doctor advised not to take any
medicines. Everything was normal and he never had any hospital admission in the past.
When he was admitted to the hospital due to covid ,the doctor asked about any health issues
in the past. He told that he had no health issues or hospital admission in the past and he had
mentioned borderline cholesterol in the past and it became normal after exercise.
He was normal when he took the insurance. He got admitted due to covid only .
The company rejected the claim citing a note by the doctor in the hospital admission. He had
written to the grievance cell of the company and they have rejected his claim request.
He had submitted all the documents and had not hidden any medical conditions at the time
of taking the insurance. He was admitted to the hospital which has a cashless facility and
everything was denied by the insurance side. He took this insurance in the hope to safeguard
his hospital emergencies and he feels the insurance company is trying to deny insurance by
citing reasons . He has been waiting for the last 5 months for the claim settlement. He
requests processing his claim for a speedy settlement of the same.
He had to spend close to 1.25 lakhs for hospital expenses and had insurance coverage of 5
lakhs. He request Ombudsman’s intervention in this claim and to favour verdict for a normal
customer who suffered due to corona disease. He stated that the Ins. Co. is finding loopholes
and rejecting customer claims.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the Insured Mr. Bobin Chandra is covered under Activ Assure – Diamond Policy having
Policy No. 13-20-0155627-00 from 30/09/2020 to 29/09/2021. 4. That we received a claim
from the insured for reimbursement of hospitalisation expenses incurred for his treatment at
SUT Hospital, Thiruvananthpuram from 22/01/2021 to 01/02/2021 for the treatment of
COVID 19. The said claim was registered as Claim no. 1122010049022 for an amount of Rs.
125147.46/-. However, the said claim was repudiated as the indoor case papers showed that
the complainant has been suffering from dyslipidemia since September 2020 and he did not
disclose the same in the proposal form. 5. That on receipt of the complaint in grievance cell
and on the basis of the doctor’s statement submitted by the complainant, the case was re-
evaluated and the claim was approved on 17/08/2021 itself. An amount of Rs. 1,12,561.46
was paid to the complainant after deducting the deductibles in accordance with policy terms
& conditions.
3. The Respondent Insurer has settled the claim for Rs.1,12,561.46 and the Complainant
stated that his claim is settled and withdrew the complaint.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 16
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0268/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0365
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Mr. Chanchal De
E-2, Service Officers Flats, DRDO Residential
Complex, Lucknow Road, Timarpur, Delhi -
110054
2.
Policy Number
:
1002042820P111315816

3.
Name of the Insured
:
Mr. Chanchal De
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
12.07.2021
6.
Nature of complaint
:
Partial rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Chanchal De (Online)
4. For the Insurer
:
Ms. Sabeena C M (Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding partial rejection of mediclaim. The
complainant, Mr. Chanchal De is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that the sum insured of his present policy bearing
no.1002042820P111315816 is Rs.2 Lakhs but the respondent insurance company and TPA
calculated his reimbursement claim based on a lower sum insured of Rs.1.25 Lakhs. The sum
insured of his previous policy for 2020-21 was also Rs.2 Lakhs and his sum insured for the year
2019-20 was Rs.1.5 Lakhs and 2018-19 was Rs.1.25 Lakhs. All the four year policy copies are
attached along with the complaint. Also the TPA has not paid the PPE charges, which are
charged compulsorily by the hospital during this COVID time. Further, the pre-anasthesia
checkup (PAC) charges are also not paid.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that Mrs.Champa De ( Mother of Mr.Chanchal De) was hospitalized on 11/03/2021 with
complaints of some protruding through vagina & difficulty in passing urine. Initial
consultation was on 04/02/2021 during which she was diagnosed with III/IV Uterovaginal
Prolapse. Doctor has mentioned in initial consultation that the issue has aggrevated since 2
months. Vaginal hysterectomy with pelvic floor repair was done under spinal anaesthesia on
12/03/2021.
Sum Insured under the Policy was increased to Rs.2lakhs during renewal on 08/01/2020.
Previous policy sum insured are as below.
1. 1002042819P111877383- Rs.200000/-
2. 1002042818P112854400- Rs.150000/-
3. 1002042817P114245799- Rs.125000/-
As per the Policy condition: 5- Permanent Exclusions & Waiting period
5.2 Specific Disease/ Procedure Waiting Period (Code- Excl02):
i. Expenses related to the treatment of the listed Conditions, surgeries/treatments
-Treatment for Menorrhagia/ Fibromyoma, Myoma and Prolapse of Uterus , shall
be excluded until the expiry of 24 months of continuous coverage after the date
of inception of the first policy with us.
ii. In case of enhancement of sum insured the exclusion shall apply afresh to the
extent of sum insured increase.
Sum Insured considered for the present claim is Rs.150000/- for which 24 months of
continuous cover has elapsed.
Maximum limit per surgery for Hysterectomy is restricted to 25% of SI (Rs.37500.00)
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that the
sum insured of his current policy is Rs.2 lakhs, but the respondent insurance company
approved his mothers claim based on a lower sum insured of Rs.1.25 Lakhs only. Also the PPE
charges and pre-anasthesia checkup charges are also not paid. The Respondent Insurer
submitted that the patient was hospitalized on 11/03/2021 for vaginal hysterectomy with
pelvic floor repair. As per policy condition, waiting period for hysterectomy is 2 years and in
case of enhancement of sum insured, the exclusion shall apply afresh to the extent of sum
insured increase. Sum insured considered for the subject claim is Rs.1.5 Lakhs for which
continuous cover has elapsed and not 1.25 Lakhs as alleged by the complainant.
4. After hearing the Complainant and the Respondent Insurer and perusing the exhibits
produced before the forum, I find that the Respondent Insurer has settled the claim well in
compliance with the terms and conditions of the policy and paid the complainant the amount
he is rightly entitled to receive. Hence I find no reason to interfere in the decision of the Insurer.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0271/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0316
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Mr. R Govindan
Ramangalath House Mekkad Kariyad 683589
2.
Policy Number
:
1009012819P110489915
3.
Name of the Insured
:
Mr. R Govindan
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
28.06.2021
6.
Nature of complaint
:
Partial rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. R Govindan (Online)
2. For the Insurer
:
Mr. Renju R Krishnan (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding partial rejection of mediclaim. The
complainant, Mr. R Govindan is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had taken health insurance policy bearing
no.1009012819P110489915 with respondent insurance company Angamaly branch. On
22/09/2020, for the treatment of cataract eyes, he was admitted and treated at Little Flower
hospital Angamaly. The claim submitted is settled partially and approved Rs.11,165/- only out
of Rs.17445/- incurred.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant Mr.R Govindan had taken a Health Insurance policy in 2005 covering
himself also with family members, and is continuously renewed with the company without
any break in policy periods. There was a claim reported for the proposer himself in 2019-20
policy-1009012819P110489915. The insured was admitted at Little Flower Hospital, Angamaly
on 21/09/2020 for the treatment of Right Eye Senile Immature Cataract. Right eye
Phacoemulsification+intraocular lens implantation procedure was therefore done on
21/09/2020. Following surgery procedure, he was admitted there one day for further
observations.
The policy inception is 05/03/2005 and is renewing continuously since then. In 2017-18 policy
the sum insured was enhanced to 100,000/- from 75000/-.The sum insured opted in the
mentioned policy is Rs.100,000/- only. He was admitted for one day and the room/nursing
charges incurred was Rs.2500/-.Since the eligible room /nursing charge is only Rs.1000/-.The
proportionate clause must be applicable in this claim. Treatment /investigation charges as per
the bill was Rs.17445/-and applying the proportionate clause, the expense assessed as
Rs.6978/- only. Mask /PPE kit and such costs assessed as Rs.378/-(50% of 755).Medicine
charges calculated as Rs.1243/-.Pre hospitalization investigation charge for Rs.1566/-is also
incurred .Sum up of whole the above there assessed the amount as Rs.11165/-
only.(1000+8544+1243+378).
On scrutiny of medical documents from the hospital, it is clear that -the admission is only for
a day care procedure and the proportionate clause applied due to the room/nursing charges
exceeding its limit of Rs.1000/-. According to the policy clauses/conditions,the final payable
amount assessed as above.
As mentioned by the insured, policy clause 1.2.1 says for cataract surgery-”Actual expenses
incurred or 25% of the sum insured whichever is less, subject to a maximum of Rs.40000/- per
eye”. Here the actual expense incurred is Rs.11165/-, is less than 25% of the SI 100000/-
ie.Rs.25000/-.Hence, claim was settled for Rs.11165/-.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
Cataract operation was done at Little Flower hospital. His claim for getting the reimbursement
was partly settled by the insurance company. They settled only 11,165/- against the claimed
amount of Rs.17,445/-. The Respondent Insurer submitted that policy clause 1.2.1 says for
cataract surgery-”Actual expenses incurred or 25% of the sum insured whichever is less,
subject to a maximum of Rs.40000/- per eye”. Here the actual expense incurred is Rs.11165/-,
is less than 25% of the SI 100000/- ie.Rs.25000/-.Hence, claim was settled for Rs.11165/-.
4. After hearing the Respondent Insurer and complainant insured and perusing the the
exhibits produced before the forum, I find that the insured had not produced any bills or
medical records in support of his claim and the applicable policy clause for Gold & Senior
Citizen Plan of the insurance policy issued by the respondent insurer is : Hospitalisation
benefits : 1 – Cataract – Actual Expenses incurred or 25% of the sum insured whichever is less,
subject to a maximum of Rs.40,000/- per eye. Hence I find no reason to interfere with the
decision of the insurer in repudiating the claim by the respondent insurance company.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0272/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0346
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Mr. E K Ramesh Kartha
Veena Eradi House Vinayaka Nagar
Edappally 682024
2.
Policy Number
:
HHS80700578673
3.
Name of the Insured
:
Mrs.Kiran M S
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
29.06.2021
6.
Nature of complaint
:
Partial rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Kiran M S (Online)
2. For the Insurer
:
Mr. Pushkaraj S Bandal (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding partial rejection of mediclaim. The
complainant, Mr. E K Ramesh Kartha is the husband of the insured.
1. Averments in the complaint are as follows:
The Complainant stated that his wife Smt.MS Kiran was undergone CATARACT surgery on
11/05/2020 at Giridhar Eye Institute, Kdavanthra and he submitted the bills amounting to
Rs.59,024/- for reimbursement to the respondent insurance company. They sanctioned an
amount of Rs.36,717/- against the claim of Rs.59,024/-. He made a complaint against this to
the grievance cell, it was also rejected by the company. Now he submitting this appeal against
the partial rejection of his insurance claim of his spouse.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that The patient Ms. Kiran M S, W/O Mr. E K Ramesh Kartha got admitted on 11/05/2020 and
discharged on 12/05/2020 from Giridhar Eye Institute and treatment done for left eye
cataract . Thereafter, insured submitted treatment documents along with completed claim
form seeking reimbursement for the same hospitalization and accordingly bill entered as
reimbursement claim for Rs. 59023 /- as per submitted bills and documents received by
insured, under her policy and the same was received by Heritage Health Insurance TPA
on 02/06/2020 for necessary action (HH872103716) . After scrutinizing the claim papers
query letter had been issued to insured on 19/06/2020 as under :
a. Provide the original Dr.advice for pre &post hospitalization period against investigation&
medicine bill.
b. Provide, the Claim Intimation Copy duly received by us , If the same not yet reported,
Kindly Clarify the Reason. (Intimation must be submitted within 48 Hrs. from Admission
Date as per terms & condition of the Policy.
On receipt of query reply from insured the claim had been settled for Rs. 36717/- against the
claim amount and paid vide cheque number 20111618664 on 09/08/2020 and the
deductions were as follows:
Rs. 9000.00 on Bill No V dated 12/05/2020 (Surgeon Fees) - MAXIMUM AMOUNT PAID
AS PER REASONABLE & CUSTOMARY CLAUSE 2.44.
Rs. 537.60 on Bill No 6 dated 13/05/2020 (Medicines by Shop) - AS PER CLAUSE
NO:4.10 NON MEDICAL EXPENSE IS NOT PAYABLE.
Rs. 3750.00 on Bill No 0002 dated 12/05/2020 (Procedures) - MAXIMUM AMOUNT
PAID AS PER REASONABLE & CUSTOMARY CLAUSE 2.44.
Rs. 400.00 on Bill No 2 dated 05/05/2020 (Pathology) - NO DETAILS ENCLOSED.
Rs. 250.00 on Bill No 7 dated 09/05/2020 (X-ray (Radiography)) - ORIGINAL X-RAY
REPORT NOT ENCLOSED CLAUSE NO:5.D.1(ix).
Rs. 5250.00 on Bill No 0002 dated 12/05/2020 (OT Charges) - MAXIMUM AMOUNT
PAID AS PER REASONABLE & CUSTOMARY CLAUSE 2.44.
Rs. 10.00 on Bill No 0002 dated 12/05/2020 (Medicines by Hospital) - AS PER CLAUSE
NO:4.10 NON MEDICAL EXPENSE IS NOT PAYABLE.
Rs. 179.00 on Bill No 8 dated 18/05/2020 (Medicines by Shop) - AS PER CLAUSE
NO:4.10 NON MEDICAL EXPENSE IS NOT PAYABLE.
Rs. 95.00 on Bill No 5 dated 11/05/2020 (Medicines by Shop) - AS PER CLAUSE NO:4.10
NON MEDICAL EXPENSE IS NOT PAYABLE.
Rs. 2835.00 on Bill No 0002 dated 12/05/2020 (Consumables) - MAXIMUM AMOUNT
PAID AS PER REASONABLE & CUSTOMARY CLAUSE 2.44.
Accordingly the claim has been processed and settled . The claim has been processed
considering the reasonable and customary clause. The rates of MICS in other hospitals with
same infrastructure and within same geographic location are as under :
Vasan Eye Care Hospital Pvt. Ltd Rs.39000/-
Ahalia Foundation Eye Hospital Rs.35000/-
Precise Eye Care Pvt. Ltd Rs.37000/-
The claim has been processed as per policy terms and conditions. Clause 2.44 of the policy
reads as under :
REASONABLE AND CUSTOMARY CHARGES
Reasonable and Customary charges mean the charges for services or supplies, which are
the standard charges for the specific provider and consistent with the prevailing charges
in the geographical area for identical or similar services, taking into account the nature
of illness/injury involved.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
wife underwent Cataract surgery(LE) at Giridhar Eye Institute, the claim submitted to the TPA
(Heritage Health Insurance TPA) was settled partially only. An amount of Rs.36,717/- was
settled against the claimed amount of Rs.59,023/-, spent for the surgery at the hospital. Her
Right Eye surgery for Cataract was done at the same hospital was settled fully as Cashless by
the then TPA of the respondent insurance company, Family Health Plant TPA. The Respondent
Insurer submitted that the reimbursement claim submitted by the complainant insured in
connection with the Cataract Eye surgery for the Left Eye was settled by Heritage Health
Insurance TPA, the same was processed as per the terms and conditions of the policy. The
same patient’s Right Eye Cataract surgery was done at the same hospital in 2019 and the claim
was settled by the then TPA, Family Health Plan limited by cashless arrangement. Earlier, this
hospital was in the Network hospital(PPN) list, so the previous claim for the right eye surgery
was settled in cashless. Both these claims were settled as per Policy Clause 2.44 of the Group
Health Insurance Policy about the reasonable and customary charges taking into account the
nature of procedures done. For the Right Eye surgery also the amount settled is Rs.36,000/-,
which is the rate prevailed in other hospitals with similar infrastructure for MICS surgeries.
4. After hearing the Complainant and the observations and clarifications given by the
respondent insurer, I find that the settlement done in the subject claim is justifiable and
reasonable and well in compliance with the terms and conditions of the policy and paid the
complainant insured, the amount he is rightly entitled to receive. Hence I do not find anything
which warrants further payment.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0273/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-052-2122-0368
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Mr. Sujendra Bose V J
Vettukattil House, Shoranur
Palakkad - 679123

2.
Policy Number
:
2856/61645360/00/000230352
3.
Name of the Insured
:
Mr. Sujendra Bose V J
4.
Name of the Insurer
:
Universal Sompo Gen. Insu. Co. Ltd.
5.
Date of receipt of Complaint
:
12.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Sujendra Bose V J (Online)
4. For the Insurer
:
Dr. Ahamed (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Sujendra Bose V J is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had availed a Corona Rakshak policy from respondent insurer
Universal Sompo General Insurance company through the Intermediary bank ‘Indian Overseas
Bank’. The cover was for 9 months and 15 days starting from 24/07/2020 to 05/05/2021.
During this period he was infected by the pandemic Covid-19 and treated in Baby Memorial
Hospital from 05/11/2020 to 09/11/2020. A total of Rs.29,706/- was spent in the hospital
with all the necessary documents and records. He approached the respondent insurance
company for the reimbursement of the treatment expenses, which they rejected saying
different reasons and excuses.
Later his wife and her parents also infected by Covid-19 and treated. His wife and there
parents were also covered by the policies issued by the respondent insurer bearing policy nos.
2856/61643117/00/000228358 – Reshma KP, 2856/61843238/00/000230250 –
Muraleedharan KP, 2856/61643240/00/000230360-Puzhpa KP. Hence these cases also to be
considered along with his complaint for resolution.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that the
Complainant Insured obtained Online “Corona Rakshak Policy” for Reshma K P, Muraleedharan K P,
Pushpa K P. The policy wordings along with the applicable terms and conditions were sent to the
Insured.
It is humbly stated that Mr.Reshma K P was hospitalized for the period from 21/10/2021 to
28/10/2021 at Baby Memorial Hospital with ailment of Covid 19 infection.
It is stated that as per provided document Insured presented with history of fever, shivering, headache,
bodyache since20.10.20, loss of taste since 21.10.20, on admission temperature was 98.6 degrees,
spO2 98%, other vitals were also within normal limits, on systemic examination no abnormality
detected, (respiratory system examination - no breathing difficulty), patient was managed with
multivitamins and other supportive measure, there was no hypoxia or oxygen requirement during stay.
The patient was diagnosed as covid positive with mild symptoms. Based on these findings it appears
that the patient could have been managed on OPD basis and hospitalization was primarily for
observation, monitoring purpose.
It is humbly stated that MrsPushpa K P was hospitalized for the period from 22/10/2021 to
02/11/2020 at Baby Memorial Hospital with ailment of Covid 19 infection. As per provided
documents, it has been observed that insured is a K/C/O HTN and the same was not disclosed
to us at the time of policy inception. Copy of the proposal form and medical documents are
annexed and marked as (“Annexure 5”)
It is humbly stated that MrMURALIDHARAN.K.P was hospitalized for the period from
23/10/2021 to 02/11/2020 at Baby Memorial Hospital with ailment of Covid 19 infection. As
per provided documents it has been observed that patient was incidentally found to have
Covid test positive, there was history of contact with covid 19 positive patient. He was found
to have asymptomatic covid infection, systemic examination was normal, vitals were within
normal limits. There was nohypoxia or oxygen requirement during stay. Based on these facts
the admission was primarily for observation/monitoring purpose and patient could have been
managed on OPD / home isolation basis. Based on these facts claim stands repudiated hypoxia
or oxygen requirement during stay. Based on these facts the admission was primarily for
observation/monitoring purpose and patient could have been managed on OPD / home
isolation basis.
The claim of the insured was repudiated vide our letters dated 21/12/202022/12/2020,29/01/2021 .
The Operative Clause in the terms and conditions of Corona Rakshak Policy succinctly states that “ If
during the policy period the Insured is diagnosed with Covid and hospitalized for more than seventy-
two hours following Medical Advice of a duly qualified Medical Practitioner as per the norms specified
by Ministry of Health and Family Welfare, Government of India, the company shall pay the agreed sum
insured towards the Coverage mentioned in the policy schedule.
Provided further that, any amount payable under the policy shall be subject to the terms of coverage
exclusions, conditions and definition contained herein. Maximum liability of the Company under all
such claims during the Policy period shall be the Sum Insured opted and specified in the Schedule.
It is further submitted on perusal of treatment papers the vitals of the insured at all times which does
not warrant hospitalization.
In this regard we would also like to emphasize on CLINICAL GUIDANCE FOR MANAGEMENT OF ADULT
COVID-19 PATIENTS dated April 22, 2021 issued by AIIMS/ICMR-COVID 19 National TASK FORCE/JOINT
Monitoring Group (Dte. GHS) Ministry of Health & Family Welfare, Government of India, which lays
down the protocol for Mild Disease, Moderate Disease and Sever Disease. It is further submitted that
for Mild Symptom the Home Isolation & Care has been prescribed. The government of India, Ministry
of Health & Family Welfare has been issuing guidelines time and again for Home Isolation of
mild/asymptomatic COVOD-19 cases. As per the revised guidelines dated April 28, 2021 the Ministry
of Health & Welfare has yet again reiterated that the patients who are clinically assigned to be
mild/asymptomatic are recommended for Home Isolation.
Copy of CLINICAL GUIDANCE FOR MANAGEMENT OF ADULT COVID-19 PATIENTS dated April 22, 2021
issued by AIIMS/ICMR-COVID 19 National TASK FORCE/JOINT Monitoring Group (Dte. GHS) Ministry of
Health & Family Welfare, Government of India and Revised guidelines for Home Isolation of
mild/asymptomatic COVID cases dated April 28, 2021 is annexed and marked as (“Annexure 7”Colly).
That the clause in Revised guidelines for Home Isolation of mild/asymptomatic COVID cases dated April
28, 2021 which states that:
7. When to seek medical attention
Patient/Care giver will keep monitoring their health. Immediate medical attention must be sought if
serious signs of symptoms develop. These could include-
1. Difficulty in breathing
2. Dip in Oxygen saturation (SpO2 <94% on room air)
3. Persistent pain/pressure in the chest
4. Mental confusion or inability to arouse.
Therefore it is humbly stated that the claim has been rightly rejected as per the policy terms &
conditions. In view of the above, it is humbly submitted by this respondent that this Hon’ble
Ombudsman may kindly dismiss the present complaint and oblige.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
availed a Corona Rakshak policy from Universal Sompo General Insurance company for himself
and wife through the intermediary, Indian Overseas Bank. The Sum Insured opted was
Rs.2,50,000/-. He was Covid positive and treated at Baby Memorial hospital from 05/11/2020
to 09/11/2020. A total amount of Rs.29,706/- was spent there. His wife and her parents were
also infected with the corona virus in the meanwhile. His parents-in-law were also taken
Corona Rakshak policy from the respondent insurance company. After the treatment, his wife
and her parents were also applied for getting the compensation benefit from the respondent
insurer. The respondent insurer rejected all the claims without stating any valid reasons. The
Respondent Insurer submitted that the complainant insured has taken the Corona Rakshak
policy for himself, his wife and her parents from their company through online mode. The
policy conditions along with the applicable terms were sent to the insured. The complainant
insured and his wife were admitted at the hospital with vitals (temperature – 98.6 degrees,
SPO2 – 98%) within normal limit. The patients were diagnosed as covid positive with mild
symptoms. Hence the hospitalization was primarily for observation and monitoring purpose
only, hence repudiated the claims. The patient Muralidharan with co morbidities of
hypothyroidism and diabetes and patient Pushpa was having co morbidities of hypertension.
Both these insured were not disclosed these pre-existing history of hypothyroidism and
hypertension at the time of taking the insurance. Also during investigation the respondent
insurer came to understand that the expenses incurred at the hospitals were reimbursed by a
Nationalised insurance company. The respondent insurer repudiated the claims of
Muralidharan and Pushapa for the reason of non disclosure of pre-existing diseases.
4. After hearing the insured and the respondent Insurer and perusing the documents
produced before the forum, I find that the operative clause of the policy states that if during
the policy period, the insured person is diagnosed with COVID and hospitalized for more than
seventy-two hours following Medical Advice of a duly qualified Medical Practitioner as per the
norms specified by Ministry of Health and Family Welfare, Government of India, the company
shall pay the agreed sum insured towards the Coverage mentioned in the policy schedule. As
per the documentary evidences available, this forum find that the patients were apparently
hospitalized for isolation / observation purpose only and the vitals were normal during the
hospitalization. And the hospital expenses incurred were settled by another insurance
company by an indemnity policy. Hence I find that the respondent insurance company is
justified in repudiating the claims and I feel there is no need to interfere with the decision of
the insurer.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0274/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0397
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Mr. Anish Jain
Kollappillil House Esi Road
Ernakulam North Ernakulam 682018
2.
Policy Number
:
CRP10-20-7023031-00-000
3.
Name of the Insured
:
Mr. Anish Jain
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
07.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
15.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Anish Jain (Online)
2. For the Insurer
:
Dr Akamsha Saxena(Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Anish Jain is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he is an Advocate by profession, presently the Central
Government Standing Counsel, High Court of Kerala. His Corona Rakshak policy number is
CRP-10-20-7023031-00-000 and Claim Number 10-CRP-20-3-897885-01. He was admitted in
Sunrise Hospital on 02/10/2020 at 11 am as he was tested COVID 19 positive on 01/10/2020.
He was tested due to severe fever and headache and the same was not subsiding with
medicine, his physician advised to take an Antigen Test. He along with his wife and younger
son Philip K Jain who was below 1 year and was breast feeding got hospitalized as they also
turned Covid positive.
He got admitted in Sunrise Hospital, Kakkanad on 02/10/2020, he was treated as an inpatient
till 05/10/2020. As requested by him, the doctor discharged him and advised him to continue
medication and undergo home quarantine. Then he started processing his insurance claim.
His claim was rejected on 28/10/2020 alleging “insured didn’t need hospitalization and was
kept for observation purpose and insured would have been treated on OPD basis.” Even
though, it is a qualified physician who had admitted him for treatment, in a well reputed
Hospital and he was administered with medicines and injections at the Hospital. Later he
approached the Grievance Redressal Cell on 02/03/2021, again the respondent insurance
company rejected his claim for the same reason ‘hospitalisation is not justified’.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that company had issued Corona Rakshak Policy, Policy no- CRP-10-20-7023031-00-000 for
the period from 06-Aug-20 to 18-May-21. That the total claimed amount was INR 250000.
That the insured had undergone hospitalization at Sunrise Hospital, for “Covid-19 Antigen
Positive. That as per discharge summary there were no clinical features (symptoms or signs)
that necessitated hospitalization. The patient was otherwise asymptomatic and admitted only
basis his Covid positive status and complain of headache. Patient’s vital parameters not
captured at admission and/ or discharge.
1. That, as per Operative Clause of the policy, the admission has to be as per guidelines
specified by MOHFW.
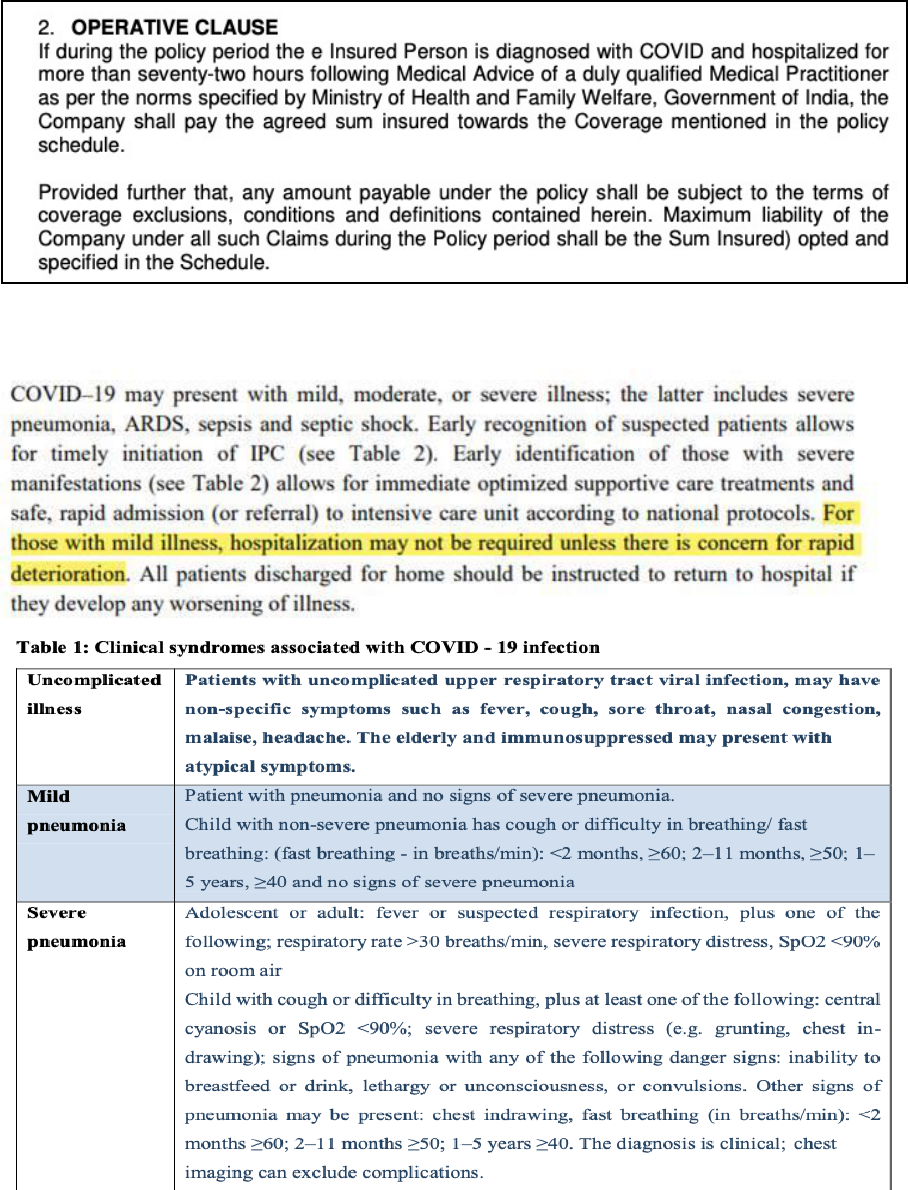
2. That, as per Circular issued by Government MOHFW dated 17
th
-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1].
3. That, furthermore to have an unbiased decision on the claim, an opinion of Independent
Forensic Expert was sought, as per forensic expert- Mr. Anish Jain was hospitalized mainly
for isolation/ observation investigation /evaluation purposes only. His isolation/
observation investigation /evaluation and treatment for symptoms faced, could easily have
been managed on domiciliary basis.
4. Thus, since basically insured was admitted for isolation / evaluation/ investigation
purpose and there was no active line of treatment, the claim was repudiated.
6.1. Investigation & Evaluation (Code- Excl04)
i. Expenses related to any admission primarily for diagnostics and evaluation purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current
diagnosis and treatment
It is therefore prayed to Hon’ble Ombudsman that the action under the claim by insurer is just
and fair and there is no discrepancy at insurer’s end hence the complaint should be dismissed
on the merits. The documents in support of contentions of the insurance company are enclosed
herewith and further the insurance company reserves its right to submit other relevant
documents if required.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
was admitted in Sunrise Hospital, Kakkanad on 02/10/2020, when he was tested positive on
01/10/2020. He taken Antigen test due to severe fever and headache and the same was not
subsiding with usual medicines. Along with him, his wife and their breast feeding child also
got admitted at the hospital as they also turned covid positive. They underwent treatment at
the hospital upto 05/10/2020. As per their request the doctor discharged them and advised
them to continue medication and undergo home quarantine. When he started processing his
insurance claim with the respondent insurance company, they rejected the claims of himself
and his wife stating the reason that the hospitalization was not necessary. The Respondent
Insurer submitted that as per the discharge summary, there was no clinical features
(symptoms or signs), that necessitated hospitalization. The patients were otherwise
asymptomatic and the admission was only on the basis of Covid positive status. Hence the
claims were rejected as per operative clause of the policy.
4. After hearing the insured and the respondent Insurer and perusing the documents
produced before the forum, I find that the operative clause of the policy states that if during
the policy period, the insured person is diagnosed with COVID 19 and hospitalized for more
than seventy-two hours following Medical Advice of a duly qualified Medical Practitioner as
per the norms specified by Ministry of Health and Family Welfare, Government of India, the
company shall pay the agreed sum insured towards the Coverage mentioned in the policy
schedule. As per the documentary evidences available, this forum find that the patient was
asymptomatic and apparently hospitalized for monitoring/observation/isolation purpose only.
Hence I find no reason to interfere in the decision of the insurer in repudiating the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0275/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0399
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Mr. Anish Jain
Kollappillil House Esi Road
Ernakulam North Ernakulam 682018
2.
Policy Number
:
CRP10-20-7023031-00-000
3.
Name of the Insured
:
Mr. Anish Jain
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
07.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
15.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Anish Jain (Online)
2. For the Insurer
:
Dr Akamsha Saxena(Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Anish Jain is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he is an Advocate by profession, presently the Central
Government Standing Counsel, High Court of Kerala. His Corona Rakshak policy number is
CRP-10-20-7023031-00-000 and Claim Number 10-CRP-20-3-897885-01. It is submitted that
his wife Adv.Sebi Bridgit PF admitted in Sunrise Hospital on 02/10/2020 at 11 am as she was
tested COVID 19 positive on 01/01/2020. She was tested due to severe fever and headache
and the same was not subsiding with medicines, her physician advised to take an Antigen Test.
She is a person with nasal allergies and random attack of breathing issues. He along with his
wife and her younger son Philip K Jain who was below 1 year and was breast feeding got
hospitalized as they also turned Covid positive.
She got admitted in Sunrise Hospital, Kakkanad on 02/10/2020, she was treated as an
inpatient till 05/10/2020. As requested by the complainant, the doctor discharged her and
advised her to continue medication and undergo home quarantine. Then the complainant
insured started processing his insurance claim. His claim was rejected on 28/10/2020 alleging
“insured didn’t need hospitalization and was kept for observation purpose and insured would
have been treated on OPD basis.” Even though, it is a qualified physician who had admitted
him for treatment, in a well reputed Hospital and he was administered with medicines and
injections at the Hospital. Later he approached the Grievance Redressal Cell on 02/03/2021,
again the respondent insurance company rejected his claim for the same reason
‘hospitalisation is not justified’. The claim was solely repudiated stating the reason that the
executive had already taken the medication given during the hospitalization with TPR, BP, Drug
administration chart was not provided. It is highly misappropriate to repudiate the claim, with
the lame reasons.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the company had issued Corona Rakshak Policy, Policy no- CRP-10-20-7023031-00-000
for the period from 06-Aug-20 to 18-May-21. That the total claimed amount was INR 250000.
That the insured had undergone hospitalization at Sunrise Hospital, for “Covid-19 Antigen
Positive on 01-Oct-20. That as per discharge summary there were no clinical features
(symptoms or signs) that necessitated hospitalization. The patient presented to the hospital with
headache & cough. Patient had SpO2-98% at admission.
That, as per Circular issued by Government MOHFW dated 17th-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1].
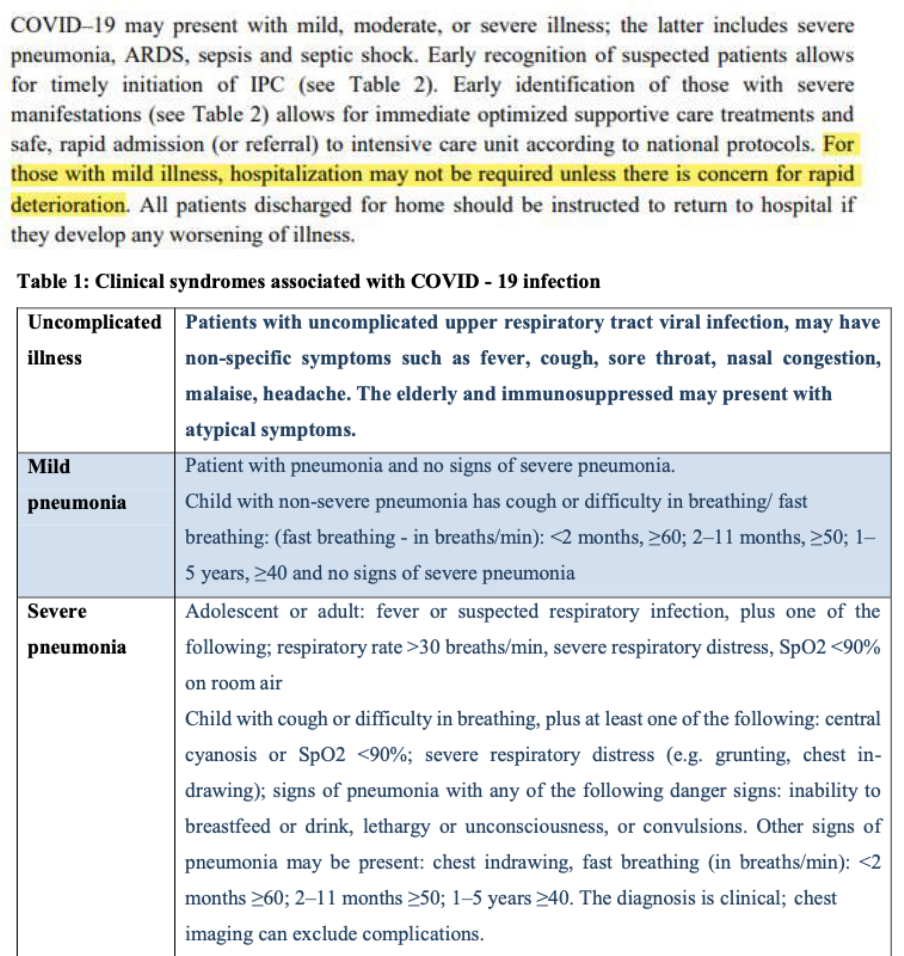
That, as per Operative Clause of the policy, the admission has to be as per guidelines specified
by MOHFW.
That, furthermore to have an unbiased decision on the claim, an opinion of Independent
Forensic Expert was sought, as per forensic expert- Ms. SebiBridgit was hospitalized mainly
for isolation/ observation/ investigation /evaluation purposes only. Her isolation/ observation/
investigation /evaluation and treatment for symptoms faced, could easily have been managed
on domiciliary basis. The hospital has also allowed her to take discharge on request without
any indemnity certificate implying that there was no risk in sending her home.
Thus, since basically insured was admitted for isolation / evaluation/ investigation purpose
and there was no active line of treatment, the claim was repudiated.
6.1. Investigation & Evaluation (Code- Excl 04)
i. Expenses related to any admission primarily for diagnostics and evaluation
purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current
diagnosis and treatment
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
wife was admitted in Sunrise Hospital, Kakkanad on 02/10/2020, when he was tested positive
on 01/10/2020. She had taken Antigen test due to severe fever and headache and the same
was not subsiding with usual medicines. Along with her, he and their breast feeding child also
got admitted at the hospital as they also turned covid positive. They underwent treatment at
the hospital upto 05/10/2020. As per their request the doctor discharged them and advised
them to continue medication and undergo home quarantine. When he started processing
their insurance claim with the respondent insurance company, they rejected the claims of
himself and his wife stating the reason that the hospitalization was not necessary. The
Respondent Insurer submitted that as per the discharge summary, there was no clinical
features (symptoms or signs), that necessitated hospitalization. The patients were otherwise
asymptomatic and the admission was only on the basis of Covid positive status. Hence the
claims were rejected as per operative clause of the policy.
4. After hearing the insured and the respondent Insurer and perusing the documents
produced before the forum, I find that the operative clause of the policy states that if during
the policy period, the insured person is diagnosed with COVID 19 and hospitalized for more
than seventy-two hours following Medical Advice of a duly qualified Medical Practitioner as
per the norms specified by Ministry of Health and Family Welfare, Government of India, the
company shall pay the agreed sum insured towards the Coverage mentioned in the policy
schedule. As per the documentary evidences available, this forum find that the patient was
asymptomatic and apparently hospitalized for monitoring/observation/isolation purpose only.
Hence I find no reason to interfere in the decision of the insurer in repudiating the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0276/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0421
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Ms. Sheela Gopalan
9/1151A, Gopal Nivas, Ajantha
Road, Mattancherry, Kerala - 682002

2.
Policy Number
:
FHR-39-20-7357010-00-000
3.
Name of the Insured
:
Ms. Sheela Gopalan
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
14.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
15.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Ms. Sheela Gopalan (Online)
2. For the Insurer
:
Dr Akamsha Saxena(Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Ms. Sheela Gopalan is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that she is the complainant and insured under the Future Health
Suraksha Individual Policy No.FHR-39-20-7357010-00-000. Her earlier policy was from
26/09/2017 to 25/09/2018 for 5 Lakhs sum insured, 31/10/2018 to 30/10/2019 for Rs.3 lakhs
- sum insured, and 31/10/2019 to 30/01/2020 for Rs.5 lakhs - sum insured, from Religare
Health Insurance company. Hence the first inception date is 26/09/2017 and the present
policy starts from 31/10/2020 to 30/10/2021, which is continuation of prior policy issued by
Religare Health Insurance company. She had complaints of swelling and pain over left limb
due to the history of travel in car for 2-3 hours 7 days back. Hence on 22/01/2021, he
approached a physician at Sangeeth Hospital and treated there for cellulitis(l) leg. She was
diagnosed diabetes for the first time on 29/01/2021 and treated there upto 04/02/2021 as
outpatient. The doctor advised antibiotic medicines and dressing there. For better treatment,
he went to Medical Trust Hospital on 04/02/2021 and got admitted there for a month from
04/02/2021 to 03/03/2021 for left leg cellulitis. He was also undergone surgery on her left
lower limb and had a skin grafting too. The total bill including the hospital expenses came to
Rs.2,34,244.35.
Her claim was rejected on 06/02/2021 stating that the insurance company cannot give
approval for cashless facility, since she was suffering from Diabetes Mellitus since 1 year, and
the same was not disclosed at the time of taking the policy. Actually she was diagnosed with
diabetes mellitus first time from Sangeetha Hospital at the time of consultation for swelling
of left leg. On 03/03/2021, she was discharged from the hospital and applied for
reimbursement claim. On 18/03/2021, she received a notice of cancellation of policy on the
ground that, she had made non disclosure of material facts, i.e. the patient had history of
diabetes since 1 year which is prior to policy inception. On 19/03/2021, she went to
respondent insurers office and submitted clarification received from the Medical Trust
hospital stating that she was diagnosed with diabetes 2 months back and in the claim form
previously filled is erroneously written as 1 year by clerical mistake. The company accepted
her clarification and gave her a letter stating the policy made active and also the company is
satisfied with the clarification letter from the hospital.
Meanwhile on 27/03/2021, the company’s investigator made investigation of her claim and
visited both her house and the hospital and submitted a report that she had past history of
Ayurvedic Medication of T2DM alleged to have gathered from indoor case sheets from
Medical Trust hospital. Then she sent a letter stating that she had no past history of Ayurvedic
medication of T2DM, and it was an inadvertent mistake crept in the indoor case sheet of
Medical Trust Hospital at the time of admission. On 26/05/2021, she received the claim
repudiation letter from the company stating that her claim does not fall under the purview of
the policy and the company will not pay the claim as the patient had the history of diabetes
since 1 year, which was not disclosed in the proposal form.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the company had issued Health Suraksha Policy, Policy no- FHR-39-20-7357010-00-000
for the period from 31-Oct-20 to 30-Oct-21 Policy schedule and policy wordings are annexed
hereto. That the total claimed amount was INR 234244. That the insured had undergone
hospitalization at Medical Trust Hospital, for “Left Lower Cellulitis, Type II Diabetes Mellitus”
for the period 04-Feb-21 to 03-Mar-21. That insured was suffering from Diabetes Mellitus
since 01 year which was prior to policy inception and was not disclosed in proposal form. That
patient’s HBA1C levels were on 04-Feb-21 “9.8” which further confirms that patient is a
having chronic diabetes. That the Company has been misled to issue the policy by suppression
of material facts which are necessary to disclose at the time of taking an insurance policy,
thereby depriving the company of a fair chance to rightly assess the proposal form submitted
and rendering contract void-ab-inito.
Insured’s Obligations: The Insured Person must disclose all Pre-Existing Disease/s, injury/
disability before taking the Policy. Non-disclosure may result in claim not being paid. The
Insured Person must disclose any material information during the Policy Period.
Disclosure to information norm: The policy shall be void and all premium paid thereon
shall be forfeited to the Insurer in the event of misrepresentation, mis-description or non-
disclosure of any material fact.
That complainant has signed the proposal form which clearly states that she has no pre-existing
diseases. It is therefore prayed to Hon’ble Ombudsman that the action under the claim by
insurer is just and fair and there is no discrepancy at insurer’s end hence the complaint should
be dismissed on the merits. The documents in support of contentions of the insurance company
are enclosed herewith and further the insurance company reserves its right to submit other
relevant documents if required.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that her
previous health insurance policy was with Religare Health Insurance company from
26/09/2017 to 30/10/2020. Now the present policy with the respondent insurer started from
31/10/2021. Hence the first inception date of her health insurance policy was w.e.f 26/09/2017.
Her claim was rejected stating that she was suffering from DM since 1 year. Actually she was
diagnosed with diabetes only 2 months back and the Type 2 DM mentioned in the Discharge
summary of Medical Trust hospital is an error. She submitted a clarification from the hospital
stating that they have mentioned history of DM by clerical mistake only. The Respondent
Insurer submitted that in the proposal form submitted along with the portability form, the
complainant insured not disclosed any existence of illness like diabetes. The Insured Person
must disclose all Pre-Existing Disease/s, injury/ disability before taking the Policy. Non-
disclosure may result in policy gets void and claim not being paid. The Insured Person must
disclose any material information during the Policy Period. Hence the action taken by the
insurance company under the claim is just and fair and no discrepancy from the part of the
respondent insurer.
4. After hearing the Respondent Insurer, complainant and perusing the complaint and the
exhibits produced before the forum, I find that the insured patient had a history of T2DM,
SYSTEMIC HTN and Dyslipidemia even before taking the insurance portability, which are not
disclosed in the proposal form and/or portability form and therefore I do not find any reason
to interfere with the decision of the insurer in repudiating the claim for non disclosure and
pre-existing condition which is the cardinal rule governing any insurance contract.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0277/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0398
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the
complainant
:
Mr. Genci George
Naduvathezhuth House
Ayyapankavu Ernakulam North
Ernakulam 682018
2.
Policy Number
:
CRP-39-207530147-00-000
3.
Name of the Insured
:
Mr. Genci George
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
07.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
15.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Genci George (Online)
2. For the Insurer
:
Dr Akamsha Saxena(Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim (Covid). The
complainant, Mr. Genci George is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had taken Corona Rakshak policy from the respondent
insurance company for himself and wife Smt.Binu Genci bearing policy no.CRP-39-207530147-
00-000 on 21/08/2020. His wife got infected with Corona Virus and tested COVID 19 positive
on 01/01/2020. She got admitted in Sunrise Hospital, Kakkanad on 01/10/2020. She was an
inpatient till 07/10/2020. Since there was no cashless claim in the insurance policy and the
bill was mounting, she consulted her doctor and asked for a compulsory discharge, when
symptoms started subsiding. The doctor discharged her and advised to continue medication
and undergo home quarantine. Then he started processing for the insurance claim and send
all documents to the respondent insurance company on 04/10/2020. The claim was rejected
by the insurance company on 24/12/2020, then he approached the Grievance Cell, but again
the claim was repudiated. She was Covid positive undisputedly and was hospitalized from
02/10/2020 to 07/10/2020 as per company’s condition of 72 hours hospitalization as an
inpatient in a hospital designated for Covid 19 treatment by the Government. As the
beginning of Covid pandemic situation in Kerala, hospitalization was compulsory.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the company had issued Corona Rakshak Policy, Policy no- CRP-39-20-7530647-00-000
for the period from 25-Jul-20 to 05-May-21. That the total claimed amount was INR 250000.
That the insured had undergone hospitalization at Sunrise Hospital, for “Covid-19 Antigen
Positive on 01-Oct-20. That as per discharge summary there were no clinical features
(symptoms or signs) that necessitated hospitalization. The patient presented to the hospital with
high grade fever. Vital parameters (especially SpO2 on RA) not captured either in first
consultation of discharge summary.
That, furthermore as per Operative Clause of the policy, the admission has to be as per
guidelines specified by MOHFW.
That, as per Circular issued by Government MOHFW dated 17th-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1].
That, furthermore to have an unbiased decision on the claim, an opinion of Independent
Forensic Expert was sought, as per forensic expert- Ms. Binu Genci, was hospitalized mainly
for isolation/ observation/ investigation /evaluation purposes only. Her isolation/ observation/
investigation /evaluation and treatment for symptoms faced, could easily have been managed
on domiciliary basis.
Thus, since basically insured was admitted for isolation / evaluation/ investigation purpose
and there was no active line of treatment, the claim was repudiated.
6.1. Investigation & Evaluation (Code- Excl04)
i. Expenses related to any admission primarily for diagnostics and evaluation
purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current
diagnosis and treatment.
It is therefore prayed to Hon’ble Ombudsman that the action under the claim by insurer is just
and fair and there is no discrepancy at insurer’s end hence the complaint should be dismissed
on the merits. The documents in support of contentions of the insurance company are
enclosed herewith and further the insurance company reserves its right to submit other
relevant documents if required.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
had taken Corona Rakshak policy for himself and wife from the respondent insurer. His wife
got infected with corona virus and got admitted in Sunrise hospital, Kakkanad. She was an
inpatient from 01/10/2020 to 07/10/2020. When symptoms started subsiding, he asked for
a compulsory discharge and the doctor discharged her and advised to continue medication
and undergo home quarantine. The claim submitted to the respondent insurance company
was rejected stating the reason that there were no symptoms or signs that necessitated
hospitalisation. The Respondent Insurer submitted that as per discharge summary, there
were no symptoms or signs which necessitated a hospitalization. The patient presented to
the hospital with fever, her vital parameters especially SpO2 On RA not captured either in first
consultation of discharge summary. Furthermore as per the Operative clause of the policy,
the admission has to be as per guidelines specified by MOHFW.
4. After hearing the insured and the respondent Insurer and perusing the documents
produced before the forum, I find that the operative clause of the policy states that if during
the policy period, the insured person is diagnosed with COVID 19 and hospitalized for more
than seventy-two hours following Medical Advice of a duly qualified Medical Practitioner as
per the norms specified by Ministry of Health and Family Welfare, Government of India, the
company shall pay the agreed sum insured towards the Coverage mentioned in the policy
schedule. As per the documentary evidences available, this forum find that the patient was
asymptomatic and apparently hospitalized for monitoring/observation/isolation and
investigation purpose only. Hence I find no reason to interfere in the decision of the insurer in
repudiating the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0278/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1 (b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0191
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Rajesh K R
Nochikkadi House, Chevarambalam P O,
Kozhikode - 673017
2.
Policy Number
:
P/181311/01/2021/002065
3.
Name of the Insured
:
Mr. Rajesh K R

4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
30.04.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
05.08.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Rajesh K R (Online)
4. For the Insurer
:
Mr. Manu Mohan (Online)
AWARD
This is a complaint filed under Rule 13 1 (b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Rajesh K R is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had taken Corona Rakshak Policy (No
P/181311/01/2021/002065) by paying Rs.6,178.00 towards premium covering period from
30.07.2020 to 11.05.2021. The complainant states that his claim falls well within the
conditions specified in the Corona Rakshak Policy, which are elaborated below :-
Surprisingly the Ins. Co. has come up with a new reason that "Insured patient's vitals are
stable throughout admission, investigations are within normal limit and could have been
managed under home isolation" for vaguely repudiating his legally valid claim !!!. Repudiation
of his claim is a willful one, conveniently forgetting that his claim falls well within all the
conditions mentioned in the Policy and is a perfect example of breach of contract. He requests
the ombudsman to kindly consider his plea and sanction the claim at the earliest possible.
2. The Respondent Insurer entered appearance and filed a self contained note. It
is submitted that Mr. K R RAJESH had taken Corona Rakshak policy for the period from
30/07/2020 to 11/05/2021 for a Sum Insured of Rs 2,50,000/- vide policy No:
P/181311/01/2021/002065
It is submitted that the complainant was admitted at Kozhikode District Co-operative Hospital
on 07/01/2021 for the treatment for Covid 19 – Category A and after treatment he was
discharged on 14/01/2021.
After the treatments were over, the complainant has submitted completed claim form,
Discharge summary, Bills of Rs.40,029/- and Lab reports.
It is submitted that the OP case sheet dated 07/01/2021 issued by the Kozhikode District Co-
operative Hospital clearly reveals that Covid 19 Catergory A has been diagnosed and also
noted that the insured had past history of Chronic urticaria & Known case of Dyslipedemia
( DLP- Border line – not on medication) .
It is submitted that Chronic urticaria (CU) is a disturbing allergic condition of the skin.
Although frequently benign, it may sometimes be a red flag sign of a serious internal disease.
Moreover in the discharge summary it is clearly noted status as “Category A” and vitals are
stable. Only vitamin and oral medicines given to the patient.
It is submitted that the patient`s status as “Category A” and vitals are stable & no active line
of treatment was given but only vitamins tablets prescribed. Here Covid positive has been
diagnosed but the patient vitals were stable, Respiration rates, SPO2, Pulse rate, Temperature
seems normal , hospitalization was not warranted and he was under observation. There were
no symptoms requiring inpatient care/ admission in a hospital. Corona Symptoms like fever,
Sore throat, Headache ,Chills Loss of smell or taste, Congestion or runny nose, Nausea or
vomiting, Diarrhea or breathing difficulty were absent and hence it doesn’t require admission
in a hospital. No specific treatment given to the patient. In a Covid case, the primary
symptoms are fever, Sore throat, Headache, Chills Loss of smell or taste, Congestion or runny
nose, Nausea or vomiting, Diarrhea and low level of SPO2. SPO2 is oxygen saturation, is a
measure of the amount of oxygen-carrying hemoglobin in the blood relative to the amount of
hemoglobin not carrying oxygen. The body needs certain level of oxygen in the blood or it will
not function as efficiently. In fact, very low levels of SpO2 can result in very serious respiratory
symptoms. The normal oxygen level which is measured by a pulse oximeter usually
range from 95% to 100%. The Blood oxygen levels below 90% are considered low (hypoxemia)
and hence oxygen support is mandatory in such cases. But in this case the value of the SPO2
was not mentioned.
Based on the available medical records it is clear that the patient`s vitals are stable and stayed
at hospital only for observation/ Monitoring i.e. under isolation and it doesn’t require
admission in a hospital. Hence the insurer had repudiated the claim and the same was
informed to the insured on 30/03/2021.

Further on escalation to grievance department another expert team reviewed and rejection
justified.
In short, the Company has rightly repudiated the claim after application of its mind to all
material facts, evidences and circumstances affecting the claim.
Hence, we pray that we may be totally exonerated from any liability under the claim.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
tested Covid +ve and was admitted to Co-operative Hospital. He had suffered body pain ,
diarrhea, shivering and fever. Within 3 days he tested Covid -ve. Doctor had told to test after
11 days . He was given 5 injections due to D Dimer variation as there was blood clotting. The
Respondent Insurer submitted that his vitals were normal . He is a k/c/o DLP and since D
Dimer is based on DLP, the complainant was given anti coagulant injection.
4. I have heard both the sides and perused the documents. I have also gone through the X-ray
report of 14/1/2021. The Discharge Card of the complainant states diagnosis as Cat A Covid19,
implying mild symptoms. The OP Case sheet and Admission Record of 7/1/2021 mention severe
myalgia and headache but No fever or cough and the latter also mentions ‘ No dyspnea’ . Symp-
toms of diarrhea, shivering and fever mentioned by the complainant during the Hearing, do not
appear therein. On the other hand, the Discharge Card states, ‘ no h/o sore throat, difficulty in
breathing, bowel or bladder complaints.’ The Doctor’s Report of 8/1/2021 states ‘Vitals stable,
Saturation Maintained.’
The X-ray report of 14/1/2021 states ‘ Mild parenchymal opacity with air bronchogram in right
lower lobe , Likely pneumonia,’ . however , it is noticed that no specific treatment was given fol-
lowing the X-ray findings. Moreover, the complainant got discharged on request the same day .
Although the complainant stated that he was Covid negative within 3 days, it is observed that
from the Discharge Card that the complainant was still Covid positive when he was discharged .
The symptoms at admission in any case, did not warrant hospitalization. During the
hospitalization, the complainant was treated only on oral medicines for Covid symptoms. The
Clexane injections were administered due to his pre-existing Dyslipidemia conditions. The
Discharge Summary states that the complainant was a k/c/o DLP (borderline) not on
medication and has h/o Chronic Urticaria. It is observed that these conditions were not
disclosed at the time of taking policy on 30/7/2020. According to General Condition 8.1
Disclosure of Information , the Policy becomes void on account of Non-disclosure of material
fact by the policy holder.
In view of the foregoing reasons, the claim is not tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0279/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0333
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Sunil K D
Kovath House Cheruval Pazhayi P O
Nenmenikkara Pudukkad Thrissur 680301
2.
Policy Number
:
P/181213/01/2021/014782
3.
Name of the Insured
:
Mr. Sunil K D
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
30.06.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Sunil K D (Online)
4. For the Insurer
:
Mr. Manu Mohan (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Sunil K D is the policyholder.
1. Averments in the complaint are as follows:
The complainant stated that he was admitted at the Amala Institute of Medical Sciences ,
Thrissur on 11/01/ 2021 , with severe chest pain . Preliminary investigations done at the
Cardiology department revealed an Acute Coronary syndrome – Inferior Wall Infarction. On
the same day Coronary Angiogram was performed and was diagnosed to have Double Vessel
Disease. Coronary Artery Bypass Graft was advised and the same was performed on 15.1.21.
After the procedure, he continued in the hospital and was discharged on 22.1.21. The claim
was rejected stating that the medical procedure underwent was for a pre existing clinical
condition. As per the case notes and remarks of the Cardiologist had clearly stated that the
Complainant do not have any pre existing Cardiac illness. The CAG and CABG were
necessitated following an acute Cardiac event and therefore cannot be considered as a pre
existing medical condition. The quantum of relief sought is the claimed amount.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant had taken a Medi classic Individual Health Insurance Policy for the pe-
riod commencing from 11/12/2019 to 10/12/2020 and the same has been renewed up to
10/12/2021 for a sum insured of Rs.2 lakhs vide Policy No. : P/181213/01/2021/014782. The
policy covers hospitalization expenses incurred in India as an inpatient subject to the defini-
tions, conditions and exclusions, set there in. The respondent insurer issued the policy to the
complainant based on the proposal form submitted by him. The proposal form is the basis
and the integral part of the contract, on the basis of which the policy is issued. The insured
patient was admitted at the Amala Institute of medical sciences , Thrissur on 11/01/ 2021
for the treatment of Coronary Artery Disease- Double vessel disease, Diabetic mellitus and
underwent Coronary Artery Bypass Grafting X 03 Graft and after the treatment he was dis-
charged on 22/01/2021 . After the discharge from hospital, the complainant submitted claim
form with discharge summary, bills of Rs. 2,04,760/-and reports. The discharge summary is-
sued by the Amala Institute of Medical Sciences , Thrissur , revealed that the complainant
had a history of Diabetics Mellitus. The Coronary Angiogram Report dated 11/01/2021 clearly
shows :
1. LMCA : Is normal,; trifurcates into LAD, LCx and Ramus.
2. LAD : Type IV and diffusely diseased. Ostioproximal LAD shows diffuse lesion
causing 90% stenosis. Mid LAD shows subtotal occlusion with faint antegrade flow
and retrograde filling from heterocollaterals via RCA. Di(2mm) diffusely diseased
and shows 90% stenosis in ostioproximal segment with slow flow distally. Other
diagonals and septals are of small calibre.
3. Ramus: (2mm) shows subtotal occlusion in ostioproximal segment with faint ante-
grade flow.
4. LX : Non dominant and small system and shows mild diffuse disease.

5. RCA : Dominant. Proximal to mid RCA shows multiple non critical plaques. Precrux
RCA shows normal and divides into RPDA and RPLV. RPDA(1.75mm) is normal.
On perusal of the medical treatment records, the Respondent Insurer collected an
Independent expert medical opinion which confirmed that there was no evidence of an acute
coronary syndrome and it was chronic in nature. This means that the patient was suffering
from this ailment before the inception of the policy. Based on the available records, it was
confirmed that the ailment for which the complainant had undergone treatment was pre-
existing. Since the ailment was pre existing, the respondent insurer repudiated the claim
based on waiting period No:IV(1)(A) of the policy i.e., pre existing disease. As per the policy,
Pre-existing disease is under waiting period No:3(iii) of the policy which states that “Pre-
Existing Disease as defined in the policy, until 48 months of continuance coverage have
elapsed, since inception of the first policy with any Indian Insurance company”. Moreover it
is elaborately explained in the Definition clause of the policy that Pre- Existing Disease/
conditions means any ailments or injury or related condition(s) for which the insured person
had signs or symptoms and /or was diagnosed and /or received medical advice/ treatment
within 48 months prior to insured person’s first policy with the Company. The insurer had
informed the repudiation to the complainant on 05/04/2021.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that on
11/01/ 2021, due to severe chest pain he was taken to the Amala Institute of Medical Sciences ,
Thrissur . This condition occurred suddenly and can`t be presumed. Only the investigation
revealed that he had an Acute Coronary syndrome – Inferior Wall Infarction following which
Coronary Angiogram was performed and diagnosed to have Double Vessel Disease. Coronary
Artery Bypass Graft was carried out on 15.1.21. The treatment was given only after the patient
was diagnosed. The claim was rejected stating that the medical procedure underwent was for
a pre existing clinical condition. From the case notes and remarks of the Cardiologist it was
clear that he do not have any pre existing Cardiac illness. The Respondent Insurer submitted
that the discharge summary from the Amala Institute of Medical Sciences , Thrissur , revealed
that the patient had a history of Diabetics Mellitus. The treatment records as well as the
Independent expert medical opinion confirmed that there were no evidence of the acute
coronary syndrome and it was chronic in nature. This means that the patient was suffering
from this ailment before the inception of the policy on 11/12/2019. Based on the available
records, it was confirmed that the ailment for which the complainant had undergone
treatment was pre-existing. Since the ailment was pre existing, the respondent insurer
repudiated the claim based on waiting period.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted. In this case where the complainant`s claim for the Coronary Artery Bypass Graft
was denied, the arguments put forth by the respondent insurer were :-
1). The complainant was admitted for the treatment of Coronary Artery Disease- Double ves-
sel disease, Diabetic mellitus and underwent Coronary Artery Bypass Grafting X 03 Graft
.2).The discharge summary issued by the Amala Institute of Medical Sciences , Thrissur , re-
vealed that the complainant had a history of Diabetics Mellitus. 3). There were no evidence
of an acute coronary syndrome. On scrutinising the medical treatment records and as per
the Independent expert medical opinion, It was chronic in nature. These indicated that the
patient was suffering from the ailment prior to the policy inception. 4. As per the policy, Pre-
existing disease is under waiting period No: iii of the policy which states that “Pre- Existing
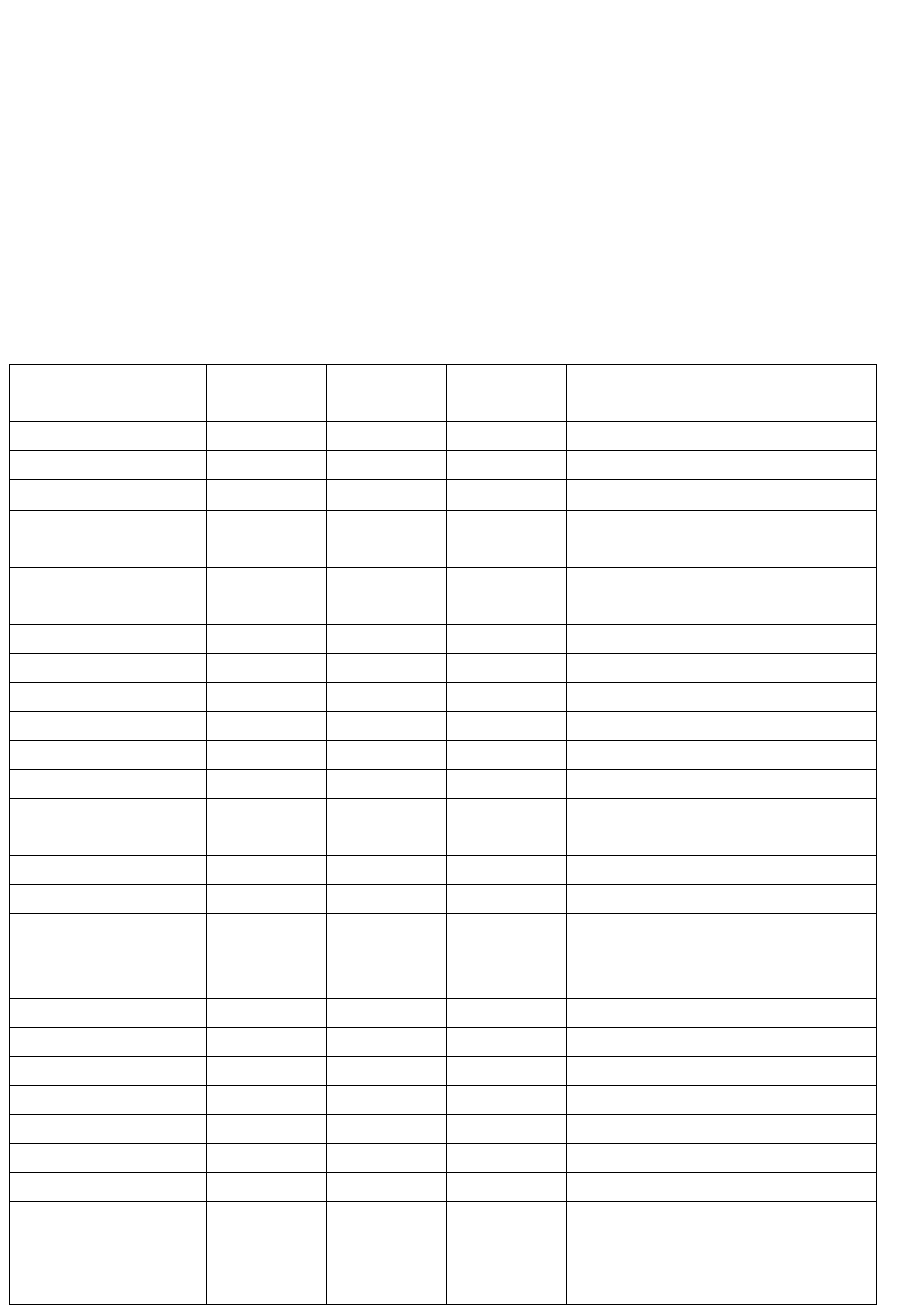
Disease as defined in the policy, until 48 months of continuance coverage have elapsed, since
inception of the first policy with any Indian Insurance company”. Hence the claim was denied.
The complainant argued that:- 1. The causative factor for the severe chest pain suffered by
the complainant was identified only after his hospitalisation .2. The Initial Patient Assessment
Form dated 11/01/ 2021 from the hospital, Amala Institute of Medical Sciences , Thrissur ,
submitted indicated `no history of CAD/CAG`. 3. In the Patient Assessment Form from the
hospital, Amala Institute of Medical Sciences , Thrissur, the duration of DM & Dyslipidemia
were shown as 4months.
On hearing both sides I find that the arguments put forth by them are not convincing. A pre
policy medical check up could have been insisted by the respondent insurer which would have
revealed the health of the condition of the Complainant. Here the benefit of doubt must go
in favour of the Complainant. Therefore the Respondent Insurer was directed to submit the
admissible amount. The admissible amount submitted is shown below:-
CLAIMED
AMT Rs.
DEDUCTION
Rs.
ADMISSIBLE
AMT Rs.
REASON
BIOCHEMISTRY
17203
17203
0
LAB REPORT NOT ENCLOSED
CARDIAC
PROCEDURE
5726
285
5441
PREPARATION NOT PAYABLE
CLINICAL
PATHOLOGY
4394
4394
0
LAB REPORT NOT ENCLOSED
DENTAL
860
860
ECG & ECHO
3376
3376
MONITORING
250
250
MICROBIOLOGY
3306
3306
0
LAB REPORT NOT ENCLOSED
MRD
475
475
0
ADMISSION NOT PAYABLE
RADIOLOGY
2108
2108
REGISTARTION &
CONSULTAT
1390
1390
MEDICAL PROCEDRE
8977
320
8657
PULSE OXYMETRE NOT PAYABLE
USS
9740
9740
WARD PROCEDURE
1994
679
1315
PRINITING STATIONERY,SPONGE
BATH,DIET COUNSELLING NOT
PAYABLE
ICU ROOM
6210
6210
ROOM
4966
4966
PROFESSIONAL
5970
5970
BLOOD BANK
5022
5022
SURGERY
55620
55620
PHYSIOTHERAPY
2889
2889
0
MEDICINE
61121
5804
55317
MASK,GLOVES,LANCET,STRIP,SWAB,
GAUZE,EASY
BATH,PAD,UNDERPAD,HANDRUB,
SHEET,DRAPE AND NON PAYABLE
REG &
CONSULTATION
300
50
250
REGISTRATION NOT PAYABLE
CREDIT
2563
38
2525
MUG NOT PAYABLE
LAB
300
300
RETURN
0
0
204760
32554
172206
CLAIMED AMOUNT
204760/-
ADMISSIBLE
AMOUNT
Rs.189409/-
Rs.17203/- PAYABLE SUBJECT TO
THE SUBMISSION OF
BIOCHEMISTRY ORIGINAL LAB
REPORT.
In the result, an award is passed, directing the Respondent Insurer to pay an amount of Rs.
1,89,409/- (out of which Rs.17,203/- is payable subject to submission of Biochemistry
Original Lab Reports), within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 29
th
day of September 2021.
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0280/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0385
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mrs. Susan John jacob
Manicheril MRA 121A Sree Lane Muttada
Trivandrum 695025
2.
Policy Number
:
P/181120/01/2021/005210
3.
Name of the Insured
:
Mrs. Susan John jacob
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
08.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
16.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mrs. Susan John jacob (Online)
2. For the Insurer
:
Mr. Manu Mohan (Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mrs. Susan John jacob is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that she was admitted KIMS Medical Hospital on testing Covid
Pneumonia from 14.2.21 to 24.2.21. She had undergone Nephrectomy 30 years ago, which
was requested by the respondent insurer but not shared, as it was neither Covid related nor
a pre existing disease. During 2013, she suffered Choriditis which was cured and the Steroid
medication was stopped in 2014. Her claim was rejected stating that she was under Steroid
which was not disclosed when she took the policy . The complainant prayed for the
reimbursement of the claim.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant had taken a Family Health Optima policy no. P/181120/01/2021/005210,
for the period 9.12.20 to 8.12.21, for a Sum Insured of Rs.5,00,000/-. The proposal form is
the basis and the integral part of the contract, on the basis of which the policy is issued. The
complainant was admitted at the KIMS Hospital, Trivandrum on 14.2.21 for the treatment of
Covid 19 Category C, Steroid induced Hyperglycemia, Hypothyroidism, Dyslipidemia, S/P
Nephrectomy and after the treatment was discharged on 23.2.21. After treatment the
Complainant submitted the claim form, discharge summary, lab reports and bill for
Rs.1,83,240/-. The discharge summary dated 23.2.21 issued by the said hospital revealed that
the patient had a past history of (S/p) Surgical Procedure of Nephrectomy. The abdomen
sonogram report dated 23.2.21 showed the following findings:-
Tiny GB Calculus
Right kidney not Visualized – post Nephrectiomy status
Left kidney appears bulky – suggestive of compensatory hypertrophy
An investigation was arranged and Medical Reports were collected from the hospital which
revealed that the complainant had a history of Right Nephrectomy 35 years back and
recurrent chest infection – left in 2008,2009 & 2010. As per the reports dated 9.4.21 from the
said hospital, the complainant had a history of Blurring of Vision – Had retinal issues –
Degeneration treatment at the Shankar Neythralayaueitis and treatment Choroiditis was on
steroids for 1 ½ years. The records of 14/2/21 from the KIMS hospital Trivandrum, revealed
that the complainant had a past history of admission for Pneumonia in 2008, 2009,2010 and
was admitted in Abu Dhabi for left sided Pneumonia which was prior to the inception of the
policy, not revealed in the proposal form. The claim was denied and the policy was terminated
and this was informed to the complainant.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that on
testing Covid positive, she was admitted at the KIMS Medical Hospital, from 14.2.21 to 24.2.21.
Her claim was denied stating non disclosure. She underwent Nephrectomy 30 years ago,
which was not shared with the respondent insurer as it had no connection with Covid. Also
she had Choriditis which was cured in 2014 and the Steroid medication was stopped . The
complainant prayed for the settlement of the claim. The Respondent Insurer submitted that
the complainant underwent treatment for Covid 19 Category C, Steroid induced
Hyperglycemia, Hypothyroidism, Dyslipidemia, S/P Nephrectomy from 14.2.21 and was
discharged on 23.2.21 after the treatment. As per the discharge summary and investigation,
the insured had a past history of (S/p) Surgical Procedure of Nephrectomy 35 years back and
recurrent chest infection – left in 2008,2009 & 2010 , which was prior to the inception of the
policy, not disclosed . The claim was rejected and the policy was terminated.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this case where the complainant`s Covid 19 –Category C treatment
claim was denied, the arguments put forth by the respondent insurer were that the discharge
summary and the investigation indicated that,the complainant had a history of Right
Nephrectomy 30 years back and recurrent chest infection – left in 2008,2009 & 2010 and
Choriditis in 2013, were not disclosed in the proposal and hence the claim was denied and
the policy was terminated ; are all tenable. I therefore do not want to interfere in the decision
of the respondent insurer in rejecting the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0281/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0400
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Prasad T P
Thayyilparambil S L Puram P O Alappuzha
688523
2.
Policy Number
:
P/181222/01/2021/004201
3.
Name of the Insured
:
Mr. Prasad T P
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
06.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
16.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Prasad T P (Online)
2. For the Insurer
:
Mr. Manu Mohan (Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim (Covid). The
complainant, Mr. Prasad T P is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he is the holder of the respondent insurer`s . He was admitted
due to Corona Virus disease at the Camelot Covid 19 CFLTC – Level2(under the Health Service
Dept.), Govt. of Kerala. The terms and conditions of the policy is that Rs.1000/- per day is
payable , maximum 60 days, for hospital admission. His claim was rejected. The complainant
prayed for taking suitable action.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that te complainant had taken a Star Hospital Cash Policy for the period 20.11.19 to 19.11.20
and the same was renewed up to 19.11.21, for the hospital cash amount of Rs.1000/- per day
vide policy no.P/181222/01/2021/04201. The complainant was admitted at the CFLTC –
Pathirappally, Allapuzha on 26.11.20 on testing Covid positive and was discharged on 6.12 20.
As per coverage clause no. 6A (Sickness Hospital Cash) of the policy, “During the period stated
in the schedule, if the insured person shall contract any disease or suffer from any illness and
if such disease/illness shall, upon the advice of a duly qualified Medical Practitioner, require
admission of the insured patient as an inpatient in any hospital in India for the purpose of
medical / surgical treatment, then the company will pay the insured person, hospital cash
amount mentioned in the schedule for every 24 hours of hospitalization subject to the
maximum number of days stated in the schedule”. The complainant was admitted in the CFLTC
and it was only an institutional quarantine facility and not a hospital. CFLTC doesn`t come
under the definition of hospital as per policy norms. CFLTCs provide institutionalized care and
treatment to mild or asymptomatic Covid positive patients. Since CFLTC is not a hospital and
lack the infrastructure of a hospital a per policy clause, the insurer had repudiated the claim.
On escalation to the grievance dept., another expert team reviewed and the rejection was
justified.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
was hospitalised at the Camelot Covid 19 CFLTC – Level2(under the Health Service Dept.),
Govt. of Kerala for treating Covid 19. The terms and conditions of the policy were that @
Rs.1000/- per day is payable , for a maximum of 60 days, for hospital admission. The claim was
rejected.. The Respondent Insurer submitted that the complainant was admitted in the CFLTC
and it was only an institutional quarantine facility and not a hospital. CFLTC doesn`t come
under the definition of hospital as per policy norms. CFLTCs provide institutionalized care and
treatment to mild or asymptomatic Covid positive patients. Since CFLTC is not a hospital and
lack the infrastructure of a hospital a per policy clause, the insurer had repudiated the claim.

4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this complaint on rejection of the complainant`s claim under the Star
Hospital Cash Policy for Covid 19 treatment at the Covid 19 CFLTC – Level 2(under the Health
Service Dept.), Govt. of Kerala, Allapuzha; on analysing the medical records and arguments,
I find that his admission at the Covid 19 CFLTC – Level 2(under the Health Service Dept.), Govt.
of Kerala, Allapuzha, was for the treatment of Covid 19(Categry B). Therefore, in this case the
admission is justified. The respondent insurer has to pay the admissible amount as per the
policy terms and conditions for the period of admission i.e from 26.11.20 to 6.12.20(10days)
calculated as follows:-
Admission Period : 26.11.20 to 6.12.20 = 10days @ Rs.1000/-(as per policy terms & conditions)
=Rs.10,000/-.
In the result, an award is passed, directing the Respondent Insurer to pay an amount of Rs.
10,000/-, within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 29th day of September 2021.
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN

AWARD NO.IO/KOC/A/HI/0282/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0405
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Monykuttan P K
Palliparambil Kizhakkethil, Angadical
South P O, Chengannur - 689122
2.
Policy Number
:
P/181212/01/2017/001431
3.
Name of the Insured
:
Mr. Monykuttan P K
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
13.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
16.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Monykuttan P K (Online)
2. For the Insurer
:
Mr. Manu Mohan (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The

complainant, Mr. Monykuttan P K is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he took a policy from the respondent insurer on 15.7.16 to 14.7.17,
covering him and his family, vide policy no. P/181212/01/2017/001431, paying a premium of
Rs.24,737/-. The policy was renewed up to 14.7.21. The complainant was admitted at the
Amrita Hospital Ernakulam, on 23.11.20 till 28.12.20 for the treatment of Cerebro Vascular
Accident and submitted a claim on 30.12.20. The respondent insurer on 25.1.21 sought for
additional documents which the complainant had send on 15.2.21. The claim was rejected vide
letter dated 6.3.21 on grounds of suppression of material facts and intended to cancel the policy
coverage of the complainant stating policy condition no.5(5),14 & 9. Earlier the complainant
was hospitalized in the year 2013. He further states that he had no disease before 2013 and after
2013 till 2021 and even thereafter. Therefore the findings of the respondent insurer that the
complainant had suppressed material facts are not correct.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant had taken Star Comprehensive Health Insurance Policy for the period
from 15/07/2016 to 14/07/2017 and the same has been renewed up to 14/07/2021 vide
Policy No. P/181223/01/2021/000853 for the sum insured of Rs.10,00,000/- . The policy
covers hospitalization expenses incurred in India as an inpatient subject to the definitions,
conditions and exclusions, set there in. The company issued the policy to the complainant
based on the proposal form submitted by the insured. The proposal form is the basis and
integral part of the contract, on the basis of which the policy is issued. The complainant was
admitted at Amrita Institute of Medical Sciences - Ernakulam on 23/11/2020 for the treatment
for CVA- Subacute infarct in right occipital lobe S/p 4 Vessel DSA- Extracranial carotids are
tortous and slightly ectatic. Hence, possibility of connective tissue disorders (FMD/Co1 4A1
mutation) cannot be ruled out (26/11/2020). Mechanism- ? vasculopathy secondary to
COL4A1 mutation/Fibromuscular dysplasia and after the treatment he was discharged on
28/11/2020. After discharge, the insured had submitted the claim form, Discharge summary,
Lab reports and previous records and Bills of Rs. 76,496/- .
It is submitted that the column of clinical information of MRI report dated 24/11/2020
shows the complainant had “recurrent history of CVA. On receiving the above mentioned
documents, the insurer had forwarded a query dated 27/01/2021 to the insured and
requested to forward the following documents:-.
Treating doctor’s letter stating exact onset, duration and cause for CVA
(Cerebrovascular accident)
First and all consultation papers and investigation reports
Complete sets of Inpatient case sheet records
Based on the query letter, the complainant had forwarded the previous treatment details. It
is submitted that the discharge summary dated 22/11/2013 , issued by Amrita Institute of
Medical Sciences – Ernakulam revealed that the complainant was treated for Acute Infarct
Right Cerebellum & Right anterior inferior cerebellar artery thrombosis. Moreover it was also
noted that the complainant had history of venous thrombosis in right lower limb one year
back. The Doppler Study of Right Lower Limb Veins dated 20/06/2012 issued by Amrita
Institute of Medical Sciences – Ernakulam shows Deep venous system incompetence with an
incompetent perforatoe along great saphenous vein as described . The MRI of Brain( Contrast)

dated 15.11.2013 issued by Amrita Institute of Medical Sciences – Ernakulam shows Acute
Infarct involving the right cerebellum . It is submitted that the complainant had admitted in
his original complaint under Ground No: D the following : “Earlier the complainant was
hospitalized in the year 2013”. These details were intentionally suppressed by the complainant
at the time of inception of the policy. The available medical records, clearly stated that the
patient had history of Acute Infarct Right Cerebellum ( Stroke )prior to the inception of policy
which was not revealed in the proposal form at the time of inception of policy. As the
petitioner has willfully suppressed the Stroke in the proposal form, which is the basis of
contract at the time of taking the policy. Hence the insurer had repudiated the claim based on
suppression of material facts as per terms and conditions of the policy . As per condition No:
18 of the policy, the company may cancel the policy on grounds of misrepresentation, Fraud,
Moral hazard, Non disclosure of material fact as declared in the proposal form. On that basis
the insurer had cancelled the policy in the name of the complainant and the same was
informed to the complainant .
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
underwent treatment for Cerebra Vascular Accident, at the Amrita Hospital, Kochi, from
23.11.20 to 28.12.20. On submitting the claim form, discharge summary, medical records and
bills etc., the claim was rejected on grounds of suppression of material facts and intended to
cancel the policy. He was earlier hospitalized in the year 2013 and had no disease before 2013
and after 2013 till 2021 and . The findings of the respondent insurer that he had suppressed
material facts are incorrect. The Respondent Insurer submitted that the complainant underwent
treatment for CVA from 23/11/2020 to 28/12/20 . On scurinizing the claims documents, the
MRI report dated 24/11/2020 shows the complainant had “recurrent history of CVA. The
previous treatment details forwarded by the complainant, on querying, revealed that the
complainant was treated for Acute Infarct Right Cerebellum & Right anterior inferior cerebellar
artery thrombosis , as per the discharge summary dated 22/11/2013 , issued by Amrita Institute
of Medical Sciences – Ernakulam. Moreover it was also noted that the complainant had history
of venous thrombosis in right lower limb one year back. The Doppler Study of Right Lower
Limb Veins dated 20/06/2012 issued by Amrita Institute of Medical Sciences – Ernakulam
shows Deep venous system incompetence with an incompetent perforatoe along great
saphenous vein as described . The MRI of Brain( Contrast) dated 15.11.2013 issued by Amrita
Institute of Medical Sciences – Ernakulam shows Acute Infarct involving the right cerebellum .
The complainant had admitted in his original complaint under Ground No: D ,the following :
“Earlier the complainant was hospitalized in the year 2013”. These details were intentionally
suppressed by the complainant at the time of inception of the policy. Therefore based on the
medical records the claim was denied and the policy was terminated.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this claim wherein the complainant`s treatment for CVA was denied on
ground of suppression of material facts , the arguments put forth by the respondent insurer
were that:-
1.On scrutinizing the claims documents, the MRI report dated 24/11/2020 shows that the
complainant had “recurrent history of CVA”. 2. The previous treatment details forwarded by
the complainant, on querying, revealed that the complainant was treated for Acute Infarct
Right Cerebellum & Right anterior inferior cerebellar artery thrombosis , as per the discharge
summary dated 22/11/2013 , issued by Amrita Institute of Medical Sciences – Ernakulam. 3.
It was noted that the complainant had history of venous thrombosis in right lower limb one
year back. 4.The Doppler Study of Right Lower Limb Veins dated 20/06/2012 issued by Amrita
Institute of Medical Sciences – Ernakulam shows Deep venous system incompetence with an
incompetent perforatoe along great saphenous vein as described . 5. The complainant had
admitted in his original complaint under Ground No: D ,that r he was hospitalized in the year
2013.
The details therefore were intentionally suppressed by the complainant at the time of
inception of the policy. Hence based on the medical records the claim was denied and the
policy was terminated, stands admissible. I therefore do not want to interfere in the decision
of the respondent insurer in rejecting the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29
th
day of September 2021.
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0283/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0410
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Akbershan M
Charuvila Puthenveedu, Thrikkovil Vattom,
Kannanalloor P O, Kollam - 691576
2.
Policy Number
:
P/181131/01/2021/003694
3.
Name of the Insured
:
Mr. Akbershan M
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
14.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)

7.
Amount of relief sought
:
--
8.
Date of hearing
:
16.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Ms Jesna H(Online)
2. For the Insurer
:
Mr. Manu Mohan (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Akbershan M is the policyholder.
1. Averments in the complaint are as follows:
The Complainant and his spouse holding a Corona Rakshak policy of the respondent insurer
were admitted at the Taluk Fort Hospital on testing Covid positive. Their claims were rejected
stating they were under institutional quarantine. Taluk hospital comes under the local self
government. The complainant prayed for the settlement of their claims.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant and spouse had taken a Corona Rakshak policy for the period 10.10.20
to 23.1.21, for a sum insured if Rs.2.5lacs each vide policy no. P/181131/01/2021/003694. The
insured registered two claims during this period. The complainant and spouse on testing Covid
19 positive- Category A, were admitted at the Taluk Hospital, Thiruvananthapuram , on
31.10.20 and after treatment were discharged on 10.11.20. The discharge summary issued by
the hospital was silent about the patient clinical parameters like temperature, pulse, SPO2
levels etc. The patients vitals were stable and no active line of treatment were given to them.
Only vitamin tablets were prescribed. From the medical records it was clear that the patients
were asymptomatic and vitals stable and stayed in the hospital only for observation i.e. under
institutional quarantine. Hence the claims were repudiated. Further on escalation to the
grievance department another expert team reviewed and the rejection was justified.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that The
Complainant and his spouse holding a Corona Rakshak policy of the respondent insurer were
admitted at the Taluk Fort Hospital on testing Covid positive. Their claims were rejected stating
they were under institutional quarantine. Taluk hospital comes under the local self
government. The Respondent Insurer submitted that the complainant and spouse on testing
Covid 19 positive- Category A, were admitted at the Taluk Hospital, Thiruvananthapuram , on
31.10.20 and after treatment were discharged on 10.11.20. The discharge summary issued by
the hospital was silent about the patient clinical parameters like temperature, pulse, SPO2
levels etc. The patients vitals were stable and no active line of treatment were given to them.
Only vitamin tablets were prescribed. From the medical records it was clear that the patients
were asymptomatic and vitals stable and stayed in the hospital only for observation i.e. under
institutional quarantine. Hence the claims were repudiated.
4. I heard the complainant and the respondent insurance and had gone through then records
submitted. In this complaint where the Covid claim of the complainant and his spouse for their
admission at the Fort Hospital, Trivandrum,was denied stating that they were under
institutional quarantine, the arguments piut forth by the respondent insurer were the
complainant and spouse on testing Covid 19 positive- Category A, were admitted at the Taluk
Hospital, Thiruvananthapuram , on 31.10.20 and after treatment were discharged on 10.11.20.
The discharge summary issued by the hospital was silent about the patient clinical parameters
like temperature, pulse, SPO2 levels etc. The patients vitals were stable and no active line of
treatment were given to them. Only vitamin tablets were prescribed. From the medical
records it was clear that the patients were asymptomatic and vitals stable and stayed in the
hospital only for observation i.e. under institutional quarantine and hence claims were
repudiated, are all tenable. I therefore do not want to interfere in the decision of the
respondent insurer in rejecting the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0285/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0439
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Hasanul Banna K N
5/1089 C DV Junction Mattancherry
Kochi 682002
2.
Policy Number
:
CRP-39-20-7530665-00-000
3.
Name of the Insured
:
Mr. Hasanul Banna K N
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
23.07.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid
7.
Amount of relief sought
:
--
8.
Date of hearing
:
23.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Hasanul Banna K N (Online)
2. For the Insurer
:
Dr. Akamsha Saxena (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Hasanul Banna K N is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he was diagnosed Covid Positive on 10/10/2020 and was
admitted to Govt. CFLTC, Mattancherry on 11/10/2020 and discharged on 22/10/2020. He
had lodged claim on 30/10/2020 and was informed that the claim was repudiated stating that
patient is known case of seizure disorder which was not disclosed at the time of taking the
policy. The complainant stated that he had only one episode of seizure at the age of 10 and
no symptoms thereafter. During Covid he had symptoms of loss of smell and taste. He
requests the Ombudsman to provide relief by ordering settlement of his claim.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the company had issued Corona Rakshak Policy, Policy no- CRP-39-20-7530665-00-000
for the period from 24-Jul-20 to 05-May-21. That the total claimed amount was INR 100000.
That the insured had undergone hospitalization at Covid First Line Treatment Centre, for
“Covid-19 Antigen Test Negative”.
That policy covers Covid-19 positive diagnosis , below is the supporting policy condition:
COVID Cover: Lump sum benefit equal to 100% of the Sum Insured shall be payable on
positive diagnosis of COVID, requiring hospitalization for a minimum continuous period of 72
hours. The positive diagnosis of COVID shall be from a government authorized diagnostic
centre.
That as per discharge summary there were no clinical features (asymptomatic) at
hospitalization. The patient presented to the hospital with h/o seizure disorder (10 years
back). At hospitalization, the patient’s vital parameters were all within normal limits:
That, as per Circular issued by Government MOHFW dated 17th-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1].
That, furthermore as per Operative Clause of the policy, the admission has to be as per
guidelines specified by MOHFW.
That on scrutiny of claim documents it is observed that insured submitted a Discharge
Summary for admission on 11-Oct-20 and discharged on 22-Oct-20 for Covid 19 Antigen Test
Negative.
Circular issued by Government of Kerala vide no. 31/F2/2020/Health date 28th March 2020
defines first line treatment centre
Definition: The centre identified as Covid Health care Centre should treat all mild and moderate
symptomatic persons under surveillance and should be utilized for treating positive cases,
when need arise
They are primary level health care centers for providing care to less serious cases and referral
of serious cases to the Covid Hospitals to avoid crowding directly in the Covid Hospital and
wastage of resources.
That to have an unbiased opinion on the case, an opinion from external specialist was sought,
as per forensic expert- Mr. Hasanul Banna was hospitalized mainly for isolation/ observation
/evaluation purposes only. His isolation/ observation /evaluation and oral, supportive
treatment for symptoms faced, could easily have been managed on domiciliary basis.
That, there was non-disclosure of material facts (Seizure Disorder),the patient was Covid-19
Negative , lastly there was no active line of treatment as patient was admitted for isolation
/evaluation / investigation. Thus, the claim was repudiated.
COVID Cover: Lump sum benefit equal to 100% of the Sum Insured shall be payable on
positive diagnosis of COVID, requiring hospitalization for a minimum continuous period of
72 hours. The positive diagnosis of COVID shall be from a government authorized diagnostic
centre
6.1. Investigation & Evaluation (Code- Excl04) i. Expenses related to any admission primarily
for diagnostics and evaluation purposes. ii. Any diagnostic expenses which are not related or
not incidental to the current diagnosis and treatment.
3.5. Disclosure to information norm: The policy shall be void and all premium paid thereon
shall be forfeited to the Company in the event of misrepresentation, misdescription or non-
disclosure of any material fact by the policy holder.
It is therefore prayed to Hon’ble Ombudsman that the action under the claim by insurer is just
and fair and there is no discrepancy at insurer’s end hence the complaint should be dismissed
on the merits.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
claim was rejected stating that he had seizure . He stated that he was not under medication
for seizure complaints. Also, since the policy is a Benefit Policy, PED should not be taken into
consideration. The Respondent Insurer submitted that there was no active line of treatment.
His vitals, temperature, RR, SpO2 were normal. He was given only oral medicines. The
Discharge Summary mentions about Pre Existing Disease of Seizure which is a major ailment,
but the same was not disclosed by the complainant at the time of taking the policy.
4. I have heard both the sides and perused the documents. The complainant stated in his
complaint that he had symptoms of loss of smell and taste. The Discharge Summary mentions
symptomatic without specifying symptoms. However, it is observed in the Admission Record
that the complainants SpO2 was 99 % and his temperature was Normal. The complainant
had history of seizure 10 yrs back but it was not disclosed in proposal form while taking the
policy. Disclosure is a must even while taking a Benefit Policy . As per General Terms and
Condition 8.1. of the policy: Disclosure of Information -The Policy shall be void and all
premium paid thereon shall be forfeited to the Company in the event of misrepresentation,
mis-description or non-disclosure of any material fact by the policyholder.
The claim is therefore, not tenable, in view of the foregoing reasons.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0286/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0455
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Balu Abraham Varughese
VH335 TC4/2372, Vikramapuram
Hills, Kuravankonam, Kowdiar,
Thiruvananthapuram - 695003
2.
Policy Number
:
CRP-10-20-7547346-00-000
3.
Name of the Insured
:
Mr. Balu Abraham Varughese
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
27.07.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid
7.
Amount of relief sought
:
--
8.
Date of hearing
:
23.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Balu Abraham Varughese
(Online)
4. For the Insurer
:
Dr. Akamsha Saxena (Online)

AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Balu Abraham Varughese is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his wife and two children were quarantined from 14/1/2021 to
21/1/2021 tested Covid positive on 21/1/2021. Although his family Floater Policy and his
Company policy allow him to get admitted in hospital, they were advised by Kerala Govt.
Medical Officer and Health officials to go for Home Isolation as 4 of them from the same family
were detected with covid . All the documents were submitted for claim. They had to opt for
make shift isolation being asymptomatic, considering hospital beds to be available for critical
patients. IRDA has issued advisory to Ins. Cos. to process claims for all make shift hospitals or
temporary hospitals . Despite the advisory, the Ins. Co. denied the claims.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the company had issued Corona Rakshak Policy, Policy no- CRP-10-20-7547346-00-000
for the period –15-Oct-20 to 26-Jul-21.
Three claims have been registered . That the claimed amount was INR 250000 for each
insured.
That the insureds were under Home Isolation monitored by Arya Vilasam Kodukulanji, for
Covid-19.
That as per insured’s mail dated 10-Feb-21, at 17:45, he has clearly stated that insureds
were under Home Quarantine.
That policy covers minimum continuous 72 hours of hospitalization ; below are the
supporting policy clauses :
1. 4.1. COVID Cover Lump sum benefit equal to 100% of the Sum Insured shall be payable on
positive diagnosis of COVID, requiring hospitalization for a minimum continuous period of
72 hours. The positive diagnosis of COVID shall be from a government authorized diagnostic
centre.
2. 3.7. Hospitalisation means admission in a hospital designated for COVID-19 treatment by
Government, for a minimum period of seventy-two (72) consecutive ‘In-patient care’ hours.
3. 3.8. In-Patient Care means treatment for which the insured person has to stay in a hospital
continuously for more than 72 hours for treatment of COVID.
4. 3.6. Hospital means any institution established for in-patient care and day care treatment of
disease/ injuries and which has been registered as a hospital with the local authorities under
the Clinical Establishments (Registration and Regulation) Act, 2010 or under the enactments
specified under Schedule of Section 56(1) of the said Act, OR complies with all minimum
criteria as under: i. has qualified nursing staff under its employment round the clock; ii. has at
least ten inpatient beds, in those towns having a population of less than ten lakhs and fifteen
inpatient beds in all other places; iii. has qualified medical practitioner (s) in charge round the
clock; iv. has a fully equipped operation theatre of its own where surgical procedures are
carried out v. maintains daily records of patients and shall make these accessible to the
Company’s authorized personnel. vi. For the purpose of this policy any other set-up
designated by the government as hospital for the treatment of Covid-19 shall also be
considered as hospital.
That, since patient was under Home Isolation and there was no hospitalization, claim was
repudiated.
It is therefore prayed to Hon’ble Ombudsman that the action under the claim by insurer is just
and fair and there is no discrepancy at insurer’s end hence the complaint should be dismissed
on the merits.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
wife and children tested Covid positive and were advised Home quarantine by the Public
Health department. He had wanted them to be hospitalized but as law abiding citizen, his wife
and children took Home Isolation , according to the Guidelines notified by the Central and
Kerala State Govts. that patients with mild symptoms need not be hospitalized. Since they
were Covid Positive and were under Home Isolation for more than 72 hours as evident from
the Discharge Certificate, he is entitled to the Benefit under the Policy. IRDA has issued
advisory to Ins. Cos. to process claims for all make shift hospitals or temporary hospitals. He
had incurred expenditure for travelling from Kochi to Thiruvananthapuram to take care of his
family during their home isolation. The Respondent Insurer submitted that the complainant’s
wife and children were under Home Isolation. Invariably, patients under Home Isolation are
either under the supervision of a Doctor who is a Private practitioner or a Doctor in a Hospital
and for every Home Isolation, a Certificate is issued. There is no mention of monitoring of
vitals nor is there a medicine chart along with the Discharge Certificate, which has been
issued to the complainant’s wife and children and it only specifies that it is Home Isolation.
4. I have heard both the sides and perused the documents. It is evident from the Discharge
Certificates issued to the complainant’s wife and children that they were only under Home
Isolation and that they were not hospitalized. The policy provides for payment of Lump sum
Benefit equal to 100% of the Sum Insured, on positive diagnosis of COVID, requiring
hospitalization for a minimum continuous period of 72 hours following Medical Advice as per
the norms specified by Ministry of Health and Family Welfare, Govt. of India. This condition
stated in the Operative Clause of the Policy is not fulfilled. The claim is therefore, not tenable.
As regards the IRDA advisory referred to by the complainant, it pertains to ‘costs of treatment
of COVID – 19’ in a make-shift or temporary hospital permitted by Central / State government
and states that , ‘ Where a policyholder who is diagnosed as Covid-19 positive is admitted into
any such make-shift or temporary hospital on the advice of a medical practitioner or
appropriate Government authorities, notwithstanding the definition of hospital specified in

the terms and conditions of policy contract, the treatment costs shall be settled by insurers.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0287/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0472
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Nissamudeen A B
Arackaparambu Kummanam P O
Chengalam South Kottayam 686022
2.
Policy Number
:
CRP-39-20-7012240-00-000
3.
Name of the Insured
:
Mr. Nissamudeen A B
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.

5.
Date of receipt of Complaint
:
02.08.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid
7.
Amount of relief sought
:
--
8.
Date of hearing
:
23.09.2021
9.
Parties present at the hearing
5. For the Complainant
:
Mr. Nissamudeen A B (Online)
6. For the Insurer
:
Dr. Akamsha Saxena (Online)
AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Nissamudeen A B is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he became Covid positive on 21/8/2020 and got admitted to
CFLTC , Ettumanoor as per directions of Kottayam Medical College Health Centre on 22/8/2020.
He lodged claim with necessary documents. Repudiation of the claim has thoroughly pained
him and caused much mental agony beyond description. He is entitled to the claim as per
policy terms. He requests the Ombudsman to direct the Ins. Co. to settle the claim for Rs.
2,50,000/- , cost of Rs. 25,000/- and any such relief found just and equitable.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the company had issued Corona Rakshak Policy, Policy no- CRP-39-20-7012240-00-000
for the period from 24-Jul-20 to 05-May-21. That the total claimed amount was INR 250000.
That the insured had undergone hospitalization at CFLTC Hospital, for “Covid-19
That as per discharge summary there were no clinical features (symptoms or signs) that
necessitated hospitalization. The patient presented to the hospital with cough & fever. At
hospitalization, the patient’s vital parameters were all within normal limits.
That, as per Operative Clause of the policy, the admission has to be as per guidelines
specified by MOHFW.
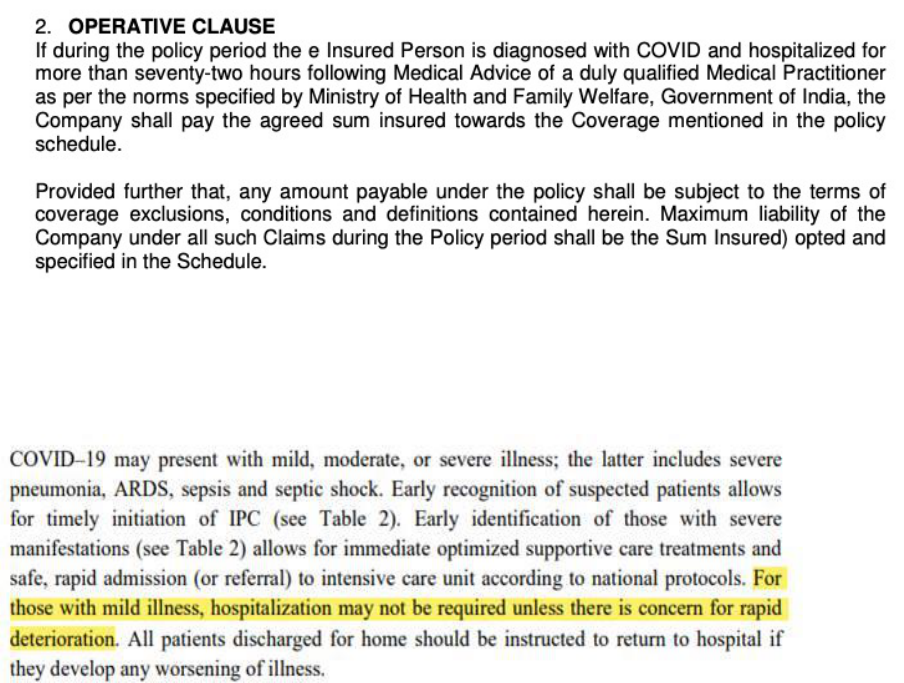
That, as per Circular issued by Government MOHFW dated 17th-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1]. Copy of Circular is annexed hereto to and is marked as Annexure “D”.
That on scrutiny of claim documents it is observed that insured submitted a Discharge
Summary for admission on 22-Aug-20 and discharged on 30-Aug-20 for Covid 19.
Circular issued by Government of Kerala vide no. 31/F2/2020/Health date 28th March 2020
defines first line treatment centre
Definition: The centre identified as Covid Health care Centre should treat all mild and
moderate symptomatic persons under surveillance and should be utilized for treating
positive cases, when need arise
They are primary level health care centers for providing care to less serious cases and
referral of serious cases to the Covid Hospitals to avoid crowding directly in the Covid
Hospital and wastage of resources.
That, furthermore to have an unbiased decision on the claim, an opinion of Independent
Forensic Expert was sought, as per forensic expert- Mr. Nissamudeen AB was hospitalized
mainly for isolation/ observation/ evaluation purposes only. His isolation/ observation/
evaluation and treatment for symptoms faced, could easily have been managed on
domiciliary basis.
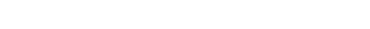
That, basically insured was admitted for isolation / evaluation/ investigation purpose and
there was no active line of treatment. Thus, we had asked for Indoor case papers and details
of treatment given during hospitalization. Insured has yet not submitted the details which
resulted in repudiation of claim.
Below are the supporting clause:
6.1. Investigation & Evaluation (Code- Excl04)
i. Expenses related to any admission primarily for diagnostics and evaluation purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current diagnosis
and treatment.
It is therefore prayed to Hon’ble Ombudsman that the action under the claim by insurer is just
and fair and there is no discrepancy at insurer’s end hence the complaint should be dismissed
on the merits.
3.I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
signature and the signature of his brother, Mr Nissar M B in complainant no. KOC-H-016-2122-
0473, are similar except for the very last part of the signature. The Respondent Insurer
submitted that mismatch in signature is a legal issue.
4. It is a known legal fact that signature authenticates a document. It is observed that the
signature of the complainant is different in the Complaint, the Annexure VI A form supplied
by Ombudsman Office and the Annexure VIA typed and submitted to this Forum by the
complainant and is identical with the different signatures in the documents filed in respect of
complaint no. KOC-H-016-2122-0473 lodged by Mr. Nissar M B and any dissimilarity stated to
be in the very last part of the signature is also not evident. The identity of the complainant
is not established.
Further, it is observed from the Progress Note issued by the CFLTC that the complainant’s
vitals were normal, he was afebrile, his temperature being 96 and 97 degrees during the
period in the CFLTC and SpO2 98 and 99%. He was stable and asymptomatic. There was
therefore, no necessity to get hospitalized in terms of the Govt. guidelines for Covid positive
patients. He was in the CFLTC only for isolation.
It is also observed that the complainant had a h/o Allergic Rhinitis , which is not disclosed
while taking the policy . As per General Terms and Condition 8.1. of the policy: Disclosure of
Information -The Policy shall be void and all premium paid thereon shall be forfeited to the
Company in the event of misrepresentation, mis-description or non-disclosure of any material
fact by the policyholder.
In view of all the above, the claim is not tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the f 29
TH
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0288/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0473
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Nissar M B
Arackaparambu Kummanam P O
Chengalam South Kottayam 686022
2.
Policy Number
:
CRP-39-20-7006024-00-000
3.
Name of the Insured
:
Mr. Nissar M B
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.
5.
Date of receipt of Complaint
:
02.08.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid

7.
Amount of relief sought
:
--
8.
Date of hearing
:
23.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Nissar M B (Online)
2. For the Insurer
:
Dr. Akamsha Saxena (Online)
AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Nissar M B is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he became Covid positive on 22/8/2020 and was admitted to
CFLTC , Ettumanoor as per directions of Kottayam Medical College Health Centre on 23/8/2020.
He lodged claim with necessary documents. Repudiation of the claim has thoroughly pained
him and caused much mental agony beyond description. He is entitled to the claim as per
policy terms. He requests the Ombudsman to direct the Ins. Co. to settle the claim for Rs.
2,50,000/- , cost of Rs. 25,000/- and any such relief found just and equitable.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that
The company had issued Corona Rakshak Policy, Policy no- CRP-39-20-7006024-00-000 for
the period from 23-Jul-20 to 04-May-21.
That the total claimed amount was INR 250000. That the insured had undergone
hospitalization at CFLTC Hospital, for “Covid-19
That as per discharge summary the patient at admission was asymptomatic; i.e. There were
no clinical features (symptoms or signs). At hospitalization, the patient’s vital parameters
were all within normal limits:.
That, as per Operative Clause of the policy, the admission has to be as per guidelines
specified by MOHFW.
That, as per Circular issued by Government MOHFW dated 17th-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1].

That on scrutiny of claim documents it is observed that insured submitted a Discharge
Summary for admission on 23-Aug-21 and discharged on 02-Sep-21 for Covid 19.
Circular issued by Government of Kerala vide no. 31/F2/2020/Health date 28th March 2020
defines first line treatment centre
Definition: The centre identified as Covid Health care Centre should treat all mild and
moderate symptomatic persons under surveillance and should be utilized for treating
positive cases, when need arise.
They are primary level health care centers for providing care to less serious cases and
referral of serious cases to the Covid Hospitals to avoid crowding directly in the Covid
Hospital and wastage of resources.
That, furthermore to have an unbiased decision on the claim, an opinion of Independent
Forensic Expert was sought, As per forensic expert- Mr. Nissar MB was hospitalized mainly
for isolation/ observation purposes only as he was asymptomatic. His isolation/ observation
and management of asymptomatic Covid, could easily have been managed on domiciliary
basis.
Thus, taking cognizance of all the above factors and govt. guidelines, the claim was
repudiated.
That, basically insured was admitted for isolation / evaluation/ investigation purpose and
there was no active line of treatment. Thus, the claim was repudiated.
Below are the supporting clause:
6.1. Investigation & Evaluation (Code- Excl04)
i. Expenses related to any admission primarily for diagnostics and evaluation purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current diagnosis
and treatment
It is therefore prayed to Hon’ble Ombudsman that the action under the claim by insurer is just
and fair and there is no discrepancy at insurer’s end hence the complaint should be dismissed
on the merits.
3.I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
signature and the signature of his brother, Mr. Nissamudeen A B in complainant no. KOC-H-
016-2122-0472, are similar except for the very last part of the signature. The Respondent
Insurer submitted that any mismatch in signature is a legal issue.
4. It is a known legal fact that signature authenticates a document. It is observed that the
signature of the complainant is different in the Complaint, the Annexure VI A form supplied
by Ombudsman Office and the Annexure VIA typed and submitted to this Forum by the
complainant and is identical with the different signatures in the documents filed in respect of
complaint no. KOC-H-016-2122-0472 lodged by Mr. Nissamudeen A B and any dissimilarity
stated to be in the very last part of the signature is also not evident. The identity of the
complainant is not established.
Further, it is observed from the Progress Note issued by the CFLTC that except for cough on
two days, the complainant was asymptomatic for the other four days ,with vitals being normal
and temperature being 98.6 degrees during the period in the CFLTC and SpO2 98 and 99%.
He had no co-morbidities and no Red Flag signs. There was therefore, no necessity to get
hospitalized in terms of the Govt. guidelines for Covid positive patients. He was in the CFLTC
only for isolation.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29th day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0289/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-016-2122-0480
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mr. Thomas C V
Chittilapilly House Annammanada
Thrissur 680741
2.
Policy Number
:
CRP3920701261000000,
CRP3920100759500000,
CRP3920701286000000
3.
Name of the Insured
:
Mr. Thomas C V
4.
Name of the Insurer
:
Future Generali India Insurance Co.
Ltd.

5.
Date of receipt of Complaint
:
06.08.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid
7.
Amount of relief sought
:
--
8.
Date of hearing
:
23.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Thomas C V (Online)
2. For the Insurer
:
Dr. Akamsha Saxena (Online)
AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is Rejection of mediclaim - Covid. The complainant,
Mr. Thomas C V is the policyholder.
1. Averments in the complaint are as follows: The Complainant stated that at the time of taking
policy they told him that if the family members who have taken the policy are positive in a
covid test , they will get 2.5 lakhs for each person if they are admitted in the hospital for 72
hrs. He and his family were positive in corona test in Nov. 2020 and were admitted in the
hospital for 5 days (120 hrs.). All the documents are submitted to the Ins. Co. They are asking
for documents which were not mentioned at the time of taking the policy. This is against the
terms and conditions of insurance . He requests the Ombudsman to do the necessary .
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the company had issued Corona Rakshak Policy, Policy no- CRP-39-20-7012610-00-000
for the period –08-Aug-20 to 05-May-21
That the total claimed amount was INR 250000.
That the insured had undergone hospitalization at CFLTC Taluk Head Quarters Hospital, for
“Covid-19”.
That as per discharge summary at admission patient had no clinical features (symptoms or
signs) that necessitated hospitalization. As per discharge summary his general condition was
good. Patient was admitted only with Covid positive status.
That, as per Operative Clause of the policy, the admission has to be as per guidelines
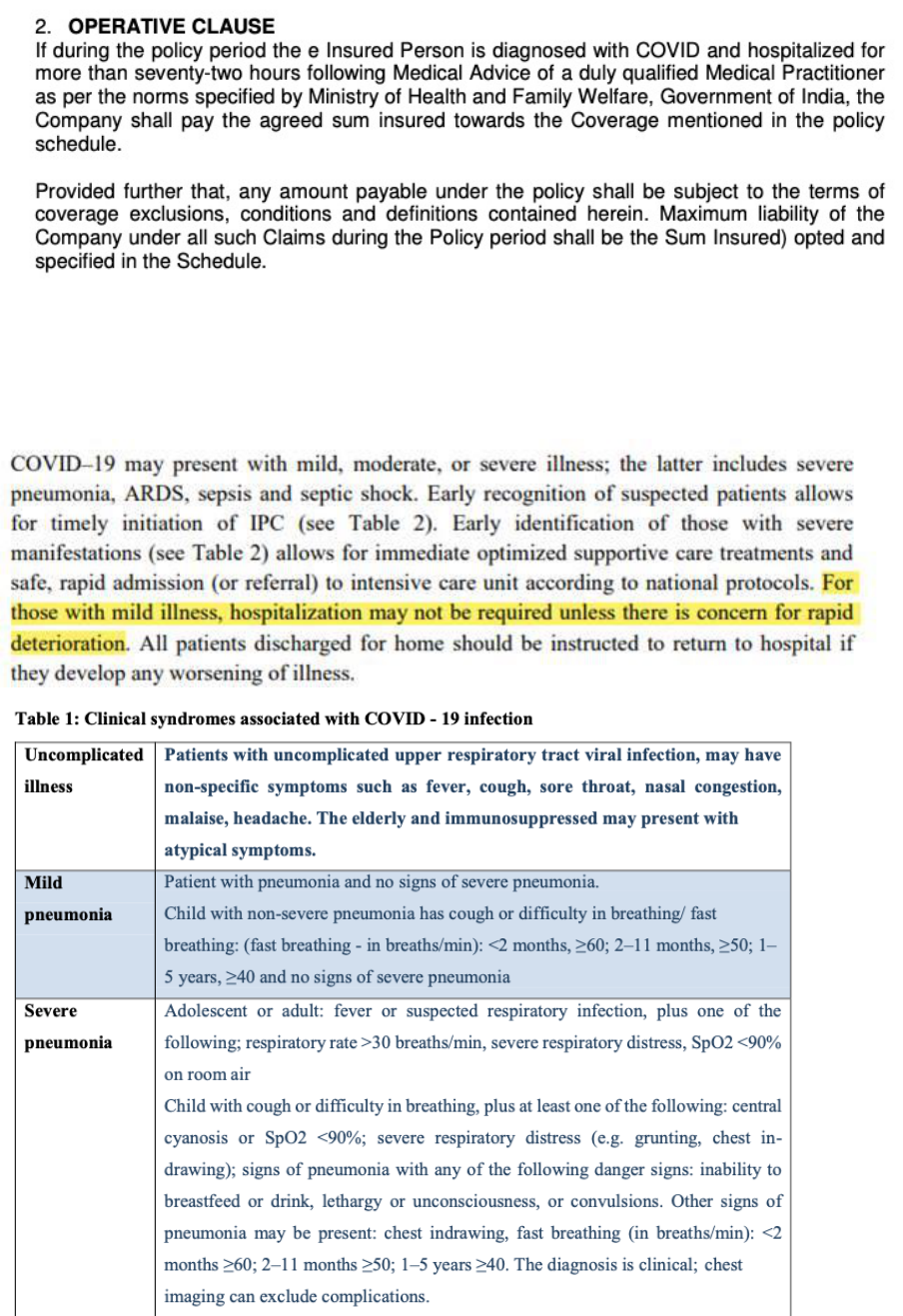
specified by MOHFW.
That, as per Circular issued by Government MOHFW dated 17th-Mar-20, Mild Symptoms
does not require hospitalization. [Table 2, clinical syndromes associated with Covid-19
infection.1].
That on scrutiny of claim documents it is observed that insured submitted a Discharge
Summary for admission on 22-Nov-20 and discharged on 01-Dec-20 for Covid 19.
Circular issued by Government of Kerala vide no. 31/F2/2020/Health date 28th March 2020
defines first line treatment centre
Definition: The centre identified as Covid Health care Centre should treat all mild and
moderate symptomatic persons under surveillance and should be utilized for treating
positive cases, when need arise
They are primary level health care centers for providing care to less serious cases and
referral of serious cases to the Covid Hospitals to avoid crowding directly in the Covid
Hospital and wastage of resources.
That, furthermore to have an unbiased decision on the claim, an opinion of Independent
Forensic Expert was sought, As per forensic expert- Mr. Thomas was hospitalized mainly for
isolation/ observation and evaluation purposes only. His isolation/ observation and evaluation
could easily have been managed on domiciliary basis.
That, basically insured was admitted for isolation / evaluation/ investigation purpose and
there was no active line of treatment. Thus, we had asked for Indoor case papers and details
of treatment given during hospitalization. Insured has yet not submitted the details which
resulted in repudiation of claim.
Below are the supporting clause:
6.1. Investigation & Evaluation (Code- Excl04)
i. Expenses related to any admission primarily for diagnostics and evaluation purposes.
ii. Any diagnostic expenses which are not related or not incidental to the current diagnosis
and treatment
It is therefore prayed to Hon’ble Ombudsman that the action under the claim by insurer is just
and fair and there is no discrepancy at insurer’s end hence the complaint should be dismissed
on the merits.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that at
the time of taking policy they told him that if tested covid positive , claim will be paid if they
are admitted in the hospital for 72 hrs. He and his family were positive in corona test in Nov.
2020 and were admitted in the hospital for 5 days. The Ins. Co. is asking for documents which
were not mentioned at the time of taking the policy. The Respondent Insurer submitted that
they had no symptoms that necessitated hospitalization. They come under Home quarantine
purview.
4 . I have heard both the sides and perused the documents. Corona Lab Test reports are not
submitted by the complainant. The Discharge Card of the complainant and his wife, treatment
and investigations are left blank and that of the daughter investigations are blank and
treatment given is only oral medicines. Lump sum benefit equal to 100% of the Sum Insured
shall be payable only when required to be hospitalized for more than seventy-two hours
following Medical Advice of a duly qualified Medical Practitioner as per the norms specified
by Ministry of Health and Family Welfare, Government of India. I am of the opinion that there
was no necessity for their hospitalization and that they were admitted to the CFLTC only for
isolation.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29th day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0291/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-012-2122-0453
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Darwin Antony
Earavelil House, Karingamthuruthu,
Kongorpilly P O, Ernakulam - 683518
2.
Policy Number
:
2894/00032573/000/00
3.
Name of the Insured
:
Mr. Darwin Antony
4.
Name of the Insurer
:
Cholamandalam MS Gen. Insu.Co.
Ltd
5.
Date of receipt of Complaint
:
27.07.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid
7.
Amount of relief sought
:
--
8.
Date of hearing
:
23.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Darwin Antony (Online)
2. For the Insurer
:
Dr Sudipta (Online)

AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Darwin Antony is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he is a driver and that at the time of taking policy he was told
that on becoming Covid positive and with 72 hours hospitalization , he would be entitled to
Rs. 50,000/- Unfortunately on 11/12/2020 , he tested Corona positive and got admitted in the
CFLTC of North Paravur Taluk Hospital. Due to this illness, he had much body pain and he was
not able to go for work. He has an unwell mother and wife and children and they are
dependent on him alone. After getting discharged he lodged claim with the Ins. Co. along with
documents but they rejected his claim. Though he paid premium he had no benefit out of it .
The Ins. Co. cheated him. He requests the Ombudsman to take necessary measures on his
complaint.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the subject mentioned policy is a Corona Rakshak Policy issued in the name of
complainant Mr Darwin Antony for the period effective from 06/09/2020 to 04/03/2021 for
sum insured of Rs 50000 / which is subject to terms , conditions and exclusions of the policy.
On Scrutiny of the claims documents submitted, we observe that the claim is not admissible
for the following reasons:
On perusal of the claim documents, it is observed that the treatment given during the
hospitalization period doesn’t warrant inpatient admission; only oral medications were
administered and Insured medical condition was within normal limits and not requiring
hospitalization as per Ministry of Health Guidelines
The vitals were stable and admission not required hence the claim is inadmissible
The complainant was admitted in CFLTC North Parur for Covid 19- positive and the discharge
summary shows no active line of treatment .On perusal of, medical records, It is understood
that inpatient hospitalisation is not justified as vitals were stable .The discharge summary as
well as the progress note and out-patient record dated 11/12/20 from Taluk Hospital will
prove that no active line of treatment was given to the complainant , hence the claim is
inadmissible.
This respondent have rightly repudiated the claim vide letter dated 23/02/2021 which is
reproduced herewith. “On perusal of the document it is observed that the treatment given
during hospitalisation period does not warrant inpatient admission; only oral medications
were administered and insured medical condition was with in normal limits and not requiring
hospitalisation as per Ministry of Health Guidelines ‘’
As per the Clinical Management Protocol issued by Ministry of Health , Government Of India,
clause 7 states as to Clinical severity and assessment parameters where in it is explained the
case of mild case of clinical severity where in certain symptoms are mentioned therein and
mentioned with management at Home or covid centre . In the present case , as per the
discharge summary itself , the complainant had no such symptoms and could have managed
at home quarantine. The claim form which was duly filled by the treated doctor will also prove
that there was no active line of treatment.
It is further submitted that Clause 10 (1) of Clinical Management Protocol issued by Ministry
of Health , Government Of India the states about management of mild cases . Patients with
mild disease may present to primary care /outpatient department, or detected during
community outreach activities, such as home visits or by telemedicine. The complainant had
no symptoms or had no history of co-morbidities. Even he had no symptoms of complications
that would prompt urgent care. Thus this respondent had rightly repudiated the claim and
hence for the above mentioned reasons, the complaint is to be dismissed
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
is a driver by occupation and that at the time of taking policy he was told that on becoming
Covid positive and with 72 hours hospitalization, claim would be paid. The Respondent
Insurer submitted that in the Discharge Summary, no symptoms were noted. The vitals of the
patient, BP, RR, SpO2 and temperature were normal and hospitalization was not required as
per mandatory guidelines issued by Govt. no medication except oral antibiotics were
administered
4. I have heard both the sides and perused the documents. The Discharge Card states,
temperature normal, SpO2 normal, no murmurs. The Progress Record mentions Admitted
with Complaints of fever, fatigue , next day myalgia, but only oral medicines were
administered. Premium payment does not automatically guarantee payment of Benefit under
the policy. The policy is subject to certain terms and conditions. Lump sum benefit equal to
100% of the Sum Insured shall be payable only when required to be hospitalized for more than
seventy-two hours following Medical Advice of a duly qualified Medical Practitioner as per the
norms specified by Ministry of Health and Family Welfare, Government of India. I am of the
opinion that there was no necessity for the hospitalization and that the complainant was
admitted to the CFLTC only for isolation.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0292/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-012-2122-0425
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Babu Paily
Maliyekkal House, NSS Road,
Chalakkudy, Thrissur-680307
2.
Policy Number
:
2894/00032583/000/00
3.
Name of the Insured
:
Mr. Babu Paily
4.
Name of the Insurer
:
Cholamandalam MS Gen. Insu.Co.
Ltd
5.
Date of receipt of Complaint
:
19.07.2021

6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
14.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Babu Paily (Online)
2. For the Insurer
:
Dr Sudipta(Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Babu Paily is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he tested Covid positive on 6/10/2020 and was admitted to
CFLTC, St James Academy, Chalakudy from 8/10/2020 to 16/10/2020. His claim was rejected
stating he was asymptomatic and there were no specific complaints for admission. The Ins.
Co. has not responded to the issue registered in the IGMS portal of IRDA quoting the fact that
Corona Rakshak policy pays Lump sum benefit to take care of hospitalization expenses and
loss of income due to covid hospitalization. There is no mention by insurers or media about
symptomatic or asymptomatic covid and active line of treatment in the policy wordings. The
Ins. Co. has ignored IGMS and this shows its arrogance to customers and regulatory framework.
The complainant requests the Ombudsman to order settlement of his claim for Rs. 50,000/- ,
besides Rs. 50,000/- for mental agony and stress and 12% interest on claim amount till date
of settlement.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the subject mentioned policy is a Corona Rakshak Policy issued in the name of
complainant Mr Babu M P for the period effective from 06/09/2020 to 02/06/2021 for sum
insured of Rs 50000 / which is subject to terms , conditions and exclusions of the policy.
On Scrutiny of the claims documents submitted, we observe that the claim is not admissible
for the following reasons:
On perusal of the claim documents, it is observed that the treatment given during the
hospitalization period doesn’t warrant inpatient admission; only oral medications were
administered and Insured medical condition was within normal limits and not requiring
hospitalization as per Ministry of Health Guidelines
The vitals were stable and admission not required hence the claim is inadmissible
The complainant was admitted in CFLTC , St James Academy , Chlakkudy for Covid 19- positive
and the discharge summary shows no active line of treatment .On perusal of, medical records,
It is understood that inpatient hospitalisation is not justified as vitals were stable .The
discharge summary as well as the treatment certificate will prove that there was no active
line of treatment was given to the complainant , hence the claim is inadmissible.
This respondent have rightly repudiated the claim vide letter dated 09/12/20 which is
reproduced herewith. “On perusal of the document it is observed that the treatment given
during hospitalisation period does not warrant inpatient admission; only oral medications
were administered and insured medical condition was with in normal limits and not requiring
hospitalisation as per Ministry of Health Guidelines ‘’
As per the Clinical Management Protocol issued by Ministry of Health , Government Of India,
clause 7 states as to Clinical severity and assessment parameters where in it is explained the
case of mild case of clinical severity where in certain symptoms are mentioned therein and
mentioned with management at Home or covid centre . In the present case , as per the
discharge summary itself , the complainant had no such symptoms and could have managed
at home quarantine. The claim form which was duly filled by the treated doctor will also prove
that there was no active line of treatment.
It is further submitted that Clause 10 (1) of Clinical Management Protocol issued by Ministry
of Health , Government Of India the states about management of mild cases . Patients with
mild disease may present to primary care /outpatient department, or detected during
community outreach activities, such as home visits or by telemedicine. The complainant had
no symptoms or had no history of co-morbidities. Even he had no symptoms of complications
that would prompt urgent care. Thus this respondent had rightly repudiated the claim and
hence for the above mentioned reasons, the complaint is to be dismissed
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
is an auto rickshaw driver and that he was affected by Covid and he had fever, body pain and
cough but his claim was denied. He could not go for work for those 14 days. It is 1 year now.
The Respondent Insurer submitted that the complainant was asymptomatic and his General
condition was good. He was admitted in CFLTC only for isolation. No treatment was given.
4. I have heard both the sides and perused the documents. The Discharge Summary states
diagnosis as Covid 19 and that the complainant was Asymptomatic and that his General
condition was good. Investigations and Treatment rows are left blank, implying that no
treatment was given. It is therefore evident that he was admitted only for isolation. There was
no requirement of hospitalization as per Govt. Guidelines in this regard and the claim is not
tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0293/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-012-2122-0352
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Ummer Kunhali
Pattathoduvil House Perimbalam P
O Malappuram Kerala 676509
2.
Policy Number
:
2876/00096987/000/00
3.
Name of the Insured
:
Mrs. Khadeeja
4.
Name of the Insurer
:
Cholamandalam MS Gen. Insu.Co.
Ltd
5.
Date of receipt of Complaint
:
02.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Numeer k m (Online)
2. For the Insurer
:
Dr. Prabhu (Online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Ummer Kunhali is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his wife was admitted for Covid , from 16/12/2020 to 22/12/2020.
However the claim was rejected and the Health Insurance policy covering himself and his wife
was cancelled. The claim was rejected stating that his wife had Diabetes. He confirmed to
them that she has Diabetes since 4 yrs. The Ins. Co. stated that they were not informed. The
policy was taken through their Bank and they were not aware that they had to disclose Pre
existing diseases. He has returned from the Gulf and living by means of farming. He has
incurred loss due to claim rejection and requests the ombudsman to intervene and take a
decision.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the subject mentioned policy is a group health policy issued in the name of complainant
Mr Ummer Kunhali for the period effective from 05/11/2020 to 04/11/2021 for sum insured
of Rs 3,00,000/- which is subject to terms , conditions and exclusions of the policy.
The claimant’s wife Mrs Kadeeja Ummer was admitted to KIMS Alshifa Super Speciality
Hospital from 16/12/2020 to 22/12/2020 for Covid -19.
It was mentioned in the discharge summary that she had past history of systemic
hypertension, type diabetes mellitus, paroxysmal AF, bronchial asthma. Hence this
respondent had sent query letters dated 19/01/2021, reminder letters dated 04/02/2021 ,
requesting the complainant to specify when the patient first complained of and sought
medical attention with regard to DM/ HTN/ CAD/COPD/BA (Condition ) with consultation
papers , to furnish the onset , duration , progress of ailments and further treatment taken ,
with letter from the treating doctor mentioning the onset , etiology , duration of illness
along with first and previous consultation papers pertaining to present illness
The complainant upon receipt of the query letter submitted, the medical report from Dr
Kuttys’ Clinic , Tirur Road , Malappuram , certifying that complainant’s wife was under
treatment for Type 2 Diabetes and hypertension for the last 4 years and on medication for
the last 4 years
Hence this respondent had repudiated the claim vide its letter dated 12/03/2021 on the
following grounds which is re-iterated here under-
On perusal of the claims documents, the insured is suffering from diabetic since 4 years as
per the history recorded in the submitted documents, this information is not disclosed in the
proposal form while proposing for insurance. In view of this non-disclosure of material
information, the contract of insurance becomes void and no claim is payable under this
policy
Hence for the above mentioned reasons, this respondent is not in a position to honour the
claims. Hence the claims of the petitioner was repudiated on just and reasonable grounds of
the policy wordings
For the above mentioned reasons, the complaint is to be dismissed
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
wife was admitted for Covid on 16/12/2020 . Claim was rejected and the Health Insurance
policy covering himself and his wife was cancelled. The claim was rejected stating that his
wife had Diabetes. He confirmed to them that she has Diabetes since 4 yrs. The Ins. Co.
stated that they were not informed. The policy was taken through their Bank and they were
not aware that they had to disclose Pre existing diseases . The Respondent Insurer submitted
that the policy is in force from 2019 and the complainant’s wife was under treatment for
Type 2 Diabetes and hypertension for the last 4 years and on medication for the last 4 years
4. I have heard both the sides and perused the documents. The complainant’s wife is a known
case of Systemic HTN, T2DM, paroxysmal AF and bronchial asthma. These Pre-existing
diseases were not disclosed in the Enrolment Form at the time of taking the policy. According
to the General Condition 4.16 the Policy shall be void and all premium paid thereon shall be
forfeited , in the event of misrepresentation, mis-description or non-disclosure of any
material fact by the insured person(s). The claim is therefore, not tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0294/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-012-2122-0379
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Manikandan C
Chodath House Irimbiliyam
Malappuram Edayur North 676552
2.
Policy Number
:
2894/00032150/000/00
3.
Name of the Insured
:
Mr. Manikandan C
4.
Name of the Insurer
:
Cholamandalam MS Gen. Insu.Co.
Ltd
5.
Date of receipt of Complaint
:
05.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Manikandan C (Online)
2. For the Insurer
:
Dr Sudipta(Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Manikandan C is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he was diagnosed Covid Positive based on test on 3/10/2020
and was admitted to CFLTC, Pattambi the same day. He was discharged on 13/10/2020 on
being Covid negative. His claim was however repudiated stating that hospitalization was not
warranted, only oral medicines were given and medical condition was within normal limits.
He lodged grievance also. The Discharge Card states that he was symptomatic and that he
had cough and nasal discharge. Admission was decided by the Govt. Health officials and
treating Doctor. The claim denial conditions are not stated in the policy. He requests the
Ombudsman to pass an Order for Rs. 1 lakh.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the subject mentioned policy is a Corona Rakshak Policy issued in the name of
complainant Mr Manikandan C for the period effective from 05/09/2020 to 01/06/2021 for
sum insured of Rs ,100,000 / which is subject to terms , conditions and exclusions of the
policy.
On Scrutiny of the claims documents submitted, it is observed that the claim is not
admissible for the following reasons:
The treatment given during the hospitalization period doesn’t warrant inpatient admission;
only oral medications were administered and Insured medical condition was within normal
limits and not requiring hospitalization as per Ministry of Health Guidelines
The vitals were stable and admission not required hence the claim is inadmissible
The complainant was admitted in CFLTC , Pattambi, for Covid 19- positive and the discharge
summary shows no active line of treatment .On perusal of, medical records, It is understood
that inpatient hospitalisation is not justified as vitals were stable .The discharge summary as
well as the treatment certificate will prove that there was no active line of treatment was
given to the complainant , hence the claim is inadmissible.
This respondent have rightly repudiated the claim vide letter dated 03/02/21 which is
reproduced herewith. “On perusal of the document it is observed that the treatment given
during hospitalisation period does not warrant inpatient admission; only oral medications
were administered and insured medical condition was with in normal limits and not requiring
hospitalisation as per Ministry of Health Guidelines ‘’
As per the Clinical Management Protocol issued by Ministry of Health , Government Of India,
clause 7 states as to Clinical severity and assessment parameters where in it is explained the
case of mild case of clinical severity where in certain symptoms are mentioned therein and
mentioned with management at Home or covid centre . In the present case , as per the
discharge summary itself , the complainant had no such symptoms and could have managed
at home quarantine. The claim form which was duly filled by the treated doctor will also prove
that there was no active line of treatment.
It is further submitted that Clause 10 (1) of Clinical Management Protocol issued by Ministry
of Health , Government Of India the states about management of mild cases . Patients with
mild disease may present to primary care /outpatient department, or detected during
community outreach activities, such as home visits or by telemedicine. The complainant had
no symptoms or had no history of co-morbidities. Even he had no symptoms of complications
that would prompt urgent care. Thus this respondent had rightly repudiated the claim and
hence for the above mentioned reasons, the complaint is to be dismissed
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
claim is not settled for a year. He had taken the policy along with others working in the
supermarket with him . he had high fever, throat pain and loss of smell and taste for 3 to 4
days. The Respondent Insurer submitted that the admission is not justified since the
complainant’s vitals were normal . He was given only supportive treatment. Admission was
not necessary.
4. I have heard both the sides and perused the documents. The complainant is 18 yr. old and
was diagnosed with Covid 19 Category A as per the Discharge Summary , however the Physical
findings are mentioned as Vitals stable. The Case Record mentions complaints of cough, nasal
discharge 1 day, cough 1 day more, rest of the days normal, with SpO2 97 to 99% ,
Temperature normal and below normal, during the period in the CFLTC. He was treated only
on oral medicines. He was in the CFLTC only for isolation and no hospitalization was
warranted as per Govt. Guidelines in this regard. The claim is not tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0295/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-050-2122-0371
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Sajith K N
Shyameyam, Kanakappilly House,
Chettarickal, Koratty South P O,
Chalakkudy, Thrissur - 680308
2.
Policy Number
:
443500/48/2019/1129
3.
Name of the Insured
:
Mrs. Ammu G Kaimal
4.
Name of the Insurer
:
The Oriental Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
12.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Sajith K N (Online)
2. For the Insurer
:
Ms. indira T M (Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Sajith K N is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his wife had taken a Happy family Policy for Rs. 3 lakhs. The
complainant stated that his father was admitted in hospital from 12/7/2019 to 27/7/2019
and claim was submitted in Aug. , 2019. Subsequently documents that were called for were
submitted. However the claim has not been settled despite phone calls and visits to the Ins.
Co. and TPA’s offices. In Aug. 2020 he was told that the claim was not settled because the
hospital did not provide some information to the TPA. He then obtained the hospital’s letter
and submitted to the TPA. His Griev. Letter did not receive any response. He requests the
Ombudsman to get his claim settled.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that a Happy Family policy No.443500/48/2019/1129 for the period 19/01/2019 to
18/01/2020 covering Narayanan Kutty and 4 others with a floater Sum Insured of
Rs.3,00,000/- was issued.
Mr. Narayan Kutty was admitted in the Hospital on 12.07.2019 for ACUTE EXCERBATION of
COPD Grade 1, enlarged prostate and Hypertension & Diabetics. He was discharged on
27.07.2019. MD-INDIA has rejected the claim based on the patient is a smoker and current
illness is a complication of that.
Thereafter patient had produced letter issued by treating Doctor of St. James Hospital,
Chalakudy, wherein it is mentioned that present illness is not due to smoking. Based on this
letter, MD-INDIA , claim settling authority, has been advised to settle the claim based on
hospital bills and provide UTR NUMBER for producing before Hon'ble OMBUDSMAN.
3.I heard the Complainant and the Respondent Insurer. The Complainant submitted that policy
is in force since 2011. His father was admitted in hospital and claim was submitted in Aug.,
2019. All documents were submitted. However the claim has not been settled for 25 months.
The Respondent Insurer submitted they had rejected the claim based on the noting that
patient is a smoker and his illness is therefore a complication of that. They subsequently
received a Medical certificate from the hospital that the illness is not due to smoking.
4. I have heard both the sides and perused the documents. The complainant was diagnosed
with Acute Exacerbation of COPD, Grade I Enlarged Prostate, Hypertension, Diabetes Mellitus
and CLD. The complainant mentioned during the Hearing that his father had lost his right hand
long back. No Pre-existing disease or Condition is specified or detailed in the Proposal Form
although the question in the Personal History as to good health and being free from physical/
mental disease, infirmity, major complaints has been answered in the negative.
The complainant has admitted that his father was in the habit of smoking and that he quit
smoking 20 yrs. ago. COPD is known to be an after-effect of smoking and the same was not
declared while taking the policy. According to the terms and conditions of the policy,
DISCLOSURE TO INFORMATION NORM, the Policy shall be void, in the event of
misrepresentation, mis-description or non-disclosure of any material fact. The claim is
therefore, not tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0296/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-050-2122-0426
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. P D Martin
Puthussery House Ayyampuzha
Potta Ernakulam 683581
2.
Policy Number
:
441502/48/2021/8070

3.
Name of the Insured
:
Mr. P D Martin
4.
Name of the Insurer
:
The Oriental Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
20.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
14.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. P D Martin (Online)
2. For the Insurer
:
Mr. Binod Kumar(Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. P D Martin is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his mother suffered back pain and was admitted from 10/3/2021
to 11/3/2021 in Aster Medicity 50 kms away from his residence . The Ins. Co. denied his claim
stating that there was no need for hospitalization. He feels this is injustice. Therefore , he
requests the Ombudsman to get his claim settled by the Ins. Co.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the proposal form for Happy Family Floater Insurance Policy through his insurance agent
on 19.11.2009, the insured proposed insurance coverages for himself and his dependent
parents for a Total sum of Rs.1,00,000.00. On scrutiny of the proposal form and also the self
declaration form submitted by the insured, the proposal had been accepted on receipt of
premium and the policy schedule alongwith the Terms and Conditions of the Policy had also
been issued to him vide policy number 441502/48/2010/3301.
The insured subsequently renewed his policy and the policy coverage particulars of the
insured person, are as follows:-
Sl.
No.
Policy
Type
Policy Number
Period of Insurance
Sum
Insured
Remarks
From
To
1
HFF Policy
441502/48/2010/330
19.11.2009
18.11.2010
100000
SI on Floater Basis

1
2
HFF Policy
441502/48/2011/335
0
19.11.2010
18.11.2011
100000
SI on Floater Basis
3
HFF Policy
441502/48/2012/351
1
19.11.2011
18.11.2012
100000
SI on Floater Basis
4
HFF Policy
441502/48/2013/342
8
19.11.2012
18.11.2013
100000
SI on Floater Basis
5
HFF Policy
441502/48/2014/350
8
19.11.2013
18.11.2014
100000
SI on Floater Basis
6
HFF Policy
441502/48/2015/323
5
19.11.2014
18.11.2015
100000
SI on Floater Basis
7
HFF Policy
441502/48/2016/329
2
19.11.2015
18.11.2016
100000
SI on Floater Basis
8
HFF Policy
441502/48/2017/294
4
19.11.2016
18.11.2017
200000
SI on Floater Basis
9
HFF Policy
441502/48/2018/315
5
19.11.2017
18.11.2018
200000
SI on Floater Basis
10
HFF Policy
441502/48/2019/319
1
19.11.2018
18.11.2019
200000
SI on Floater Basis
11
HFF Policy
441502/48/2020/315
7
19.11.2019
18.11.2020
200000
SI on Floater Basis
12
HFF Policy
441502/48/2021/807
0
19.11.2020
18.11.2021
200000
SI on Floater Basis
During the currency of the policy, policy number 441502/48/2021/8070, the insured,
Mr. P.D. Martin, had lodged a claim through M/s. M D India Healthcare Services TPA Pvt. Ltd.,
for the treatment undertaken for his dependent mother, insured person, Mrs. Mary
Devassykutty. She had been hospitalised at Aster DM Healthcare Pvt. Ltd., Kochi for a period
from 10.03.2021 to 11.03.2021 for the diagnosis of Spinal Canal Stenosis DM Lumbar Disc
Dissorder. The claim had been denied as per the terms and conditions of the policy.
As per the Discharge Summary for the subject hospitalisation, the insured person had
presented with the complaints of lower back pain since 2013. She was diagnosed with Left
Sacro lliac joint related pain, Lumbar Degenrative Disc Disorder, Facet Joint Arthropathy, Spinal
Canal Stenosis, Diabetes Mellitus, Bilateral Chronic Suppurative Otitis Media Right Side Active
Left Side Dry.
Patient was treated with Left side Sacro lliac Joint Intra Articular Steroid Injection under C-
ARM.
The treatment given to patient can be administered as Out patient.
TPA repudiated the claim on the basis that the treatment given to the patient does not support
the need for hospitalization , (as per clause 3.11 of the policy). Clause No.3.11 read as “DAY
CARE TREATMENT: refers to medical treatment, and/or surgical procedure which is: a)
undertaken under General or Local Anaesthesia in a Hospital/day care centre in less than
24 hrs because of technological advancement, and b) which would have otherwise required
a Hospitalisation of more than 24 hours. Treatment normally taken on an out-patient basis
is not included in the scope of this definition. ”.
In this claim, the applicable sum insured was taken as Rs.1,00,000.00. The insured person,
Mrs. Mary Devassykutty has continuously been covered under the policy since 19.11.2009.
The Total Claim on the above mentioned policy has been Rs.14,464/- and the TPA has denied
the same, which the Insured is claiming now.
Now the insured lodged a complaint with Insurance Ombudsman for non-payment of Claim.
it has been observed that the denial of the claim by the TPA is in order as per the terms and
conditions of the policy and intimated the insured accordingly.
On the basis of the documents submitted by the insured, the benefits payable as per the Terms
and conditions of the Policy is therefore annexed below:-
It is a fact that the Claim was repudiated by the Grievance Cell, RO Kochi also.
The complaint is not maintainable as per the terms and conditions of the policy. Hence
respectfully submit that no additional benefits would become payable under the policy to the
insured in this claim. In view of the above, pray that the Honorable Ombudsman may be
pleased to accept our submissions and the complaint may be dismissed.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
mother, 70 yrs.of age, suffered back pain and was admitted on 10/3/2021 on the advice of
Doctor as it is not ordinary injection. The injection was administered in the Operation Theatre.
Initially the hospital stated that Rs,10,000/- was approved by the Ins. Co. but after two days
the hospital asked him to pay as the Ins. Co. denied. The Respondent Insurer submitted that
the complainant’s mother was diagnosed with Left Sacro lliac joint related pain, and was
treated with Left side Sacro lliac Joint Intra Articular Steroid Injection under anesthesia but
the treatment given to patient can be administered as out-patient.
4. I have heard both the sides and perused the documents. The complainant’s mother was
administered Left side Sacro lliac Joint Intra Articular Steroid Injection under C-ARM. I am of
the opinion that her admission in the hospital was necessary considering her age and possible
side effects of steroids. The Admissible Claim amount is Rs.12,380/- as arrived under:
Sub_category
Bill_Amt
Approvel
amount
deduction
s
reason
OTHER EXPENSES/
Admission charges
200
200
0
PROFESSIONAL
FEES
400
400
0
ROOM
500
500
0
INVESTIGATIONS
2990
2990
0
OTHER EXPENSES
360
0
360
Food and other
beverages charges are
not payable.
NURSING
CHARGES
250
250
0
MEDICAL
CONSUMABLES
1000
0
1000
Protection charges
Charges are not payable
OTHER EXPENSES
500
0
500
Insurance Processing
Charges Are Not Payable
INVESTIGATIONS
120
120
0
MEDICAL
CONSUMABLES
387
387
0
CONSERVATIVE
6500
6500
0
OPERATION
THEATRE BILLING
1307
0
1307
Non-medical expenses
are not payable. - GAUZE
/ Examination Gloves /
DIGITAL THORMOETR /
FACE MASK / bactorub
OPERATION
THEATRE BILLING
151
68
83
Non-medical expenses
are not payable. - BLOOD
GLUCO STRIP
PROFESSIONAL
FEES
400
400
0
MEDICAL
CONSUMABLES
618
618
0
MEDICAL
CONSUMABLES
1323
1323
0
Copay
1376
Total
payable
amount
12,380
In the result, an award is passed, directing the Respondent Insurer to pay an amount of Rs.
12,380/- subject to submission of Original Bills by the Complainant to the Respondent Insurer ,
within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0297/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-050-2122-0354
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Noble Pappachan
Palliyan House, Karukutty P O,
Ernakulam - 683576
2.
Policy Number
:
441502/48/21/05713
3.
Name of the Insured
:
Mr. Noble Pappachan
4.
Name of the Insurer
:
The Oriental Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
09.07.2021
6.
Nature of complaint
:
Partial rejection of mediclaim
(Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Noble Pappachan (Online)
4. For the Insurer
:
Mr. Binod Kumar(Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding partial rejection of mediclaim. The
complainant, Mr. Noble Pappachan is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he was admitted for Corona treatment. Initially he consulted
doctor for high fever and since his condition did not improve, doctor suggested emergency
admission the next day and there he underwent Covid test on 4/3/2021. He tested positive
and his condition got worse. The hospital contacted the Ins. Co. and they approved his claim
but they paid only Rs. 25,138/- against the total amount of Rs. 71,820/- His letters to Ins. Co.
and TPA have yielded no result. His family had arranged the amount from friends and
neighbors. He requests the Ombudsman to get the balance claim settled .
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the insured proposed insurance coverages for himself only for a sum insured of
Rs.3,00,000/-. The proposal had been accepted on receipt of premium and the policy
schedule alongwith the Terms and Conditions of the Policy had also been issued to him vide
policy number 441502/48/2021/5713.
During the currency of the policy, the insured, Mr. Noble Pappachan, had lodged a claim
through M/s.MD India Healthcare Services TPA Pvt. Ltd., for the treatment undertaken for self.
He had been hospitalised at MAGJ Hospital, Mookkanoor for a period from 04.03.2021 to
15.03.2021 for the diagnosis of Corona Positive. The claim had been admitted and the amount
paid to the hospital through cashless mode for Rs.25,138.00. As per revised calculation (the
claim as per the SOC of room rent charges) the Total payable claim amount works out to
Rs.48,015/- Hence a balance of Rs.22,877 /- is also approved for payment to the Insured.
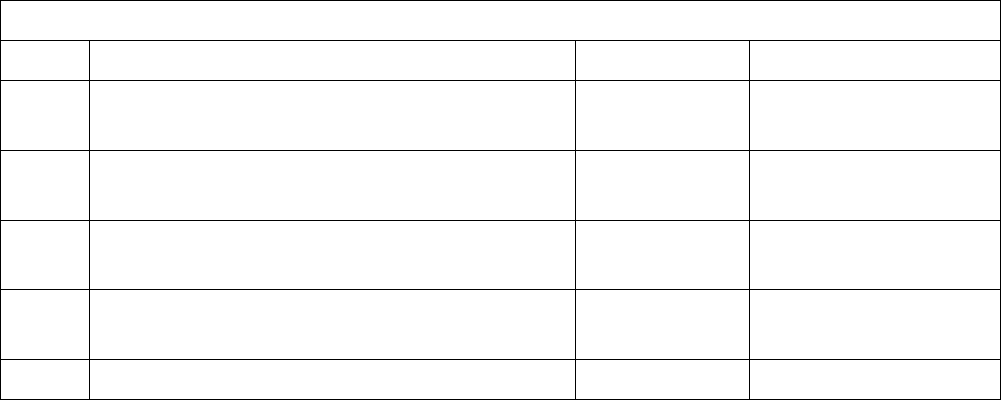
As per the Discharge Summary for the subject hospitalisation, the insured person had
presented with the complaints of Headache, Body pain. He was diagnosed with Covid-19
positive and underwent treatment for the same during the hospitalisation.
It may also be noted that the room rent and consultation charges were paid as per SOC
package only as per IRDA guidelinses and PPE Kit deducted as per usual and customary charge
basis.
On the basis of the documents submitted by the insured, the benefits already paid and
payable as per the terms and conditions of the policy is as below:-
Summary of Claim Amount Paid and Payable
Sl. No.
Particulars
Amount
Remarks
1
Claim Amount Payable as per the bills submitted
by the Insured / Hospital.
71820
Not fully Payable
2
Claim Amount already paid through Cashless
mode to the Hospital
25138
Paid – Cashless
3
Claim Amount already paid through Cashless
mode to the Insured
22847+30
Will be paid on
confirming NEFT
4
Non-Medical expenses not payable
(Sl. No.2, 5 & 8 of the above list)
6535
Not Payable
(**) Sum Insured - 3,00,000.00
Max. amount can be claimed - Sum Insured
Less:-Claim already paid +balance approved 48,015/-
Balance payable, if awarded 17,270/-(non medical)
[ 71820-(25138+30+22847)-6535=17270/-]
In addition Daily Cash Benefit of Rs.16,500/- was paid to the insured on 21.04.2021 under the
same policy
In view of the above, pray that the Honourable Ombudsman may be pleased to accept the
submissions and the complaint may be dismissed.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
was admitted for Covid treatment for 11 days from 4/3/2021. He spent Rs. 71,820/- but the
Ins. Co. paid only Rs. 25,138/- to the hospital and he had to pay the balance himself. The
Respondent Insurer submitted that Rs. 25,138/- was paid to the hospital as cashless claim but

there was an error in the calculation. A further amount of Rs. 22,877/- is payable.
The hospital has not adhered to the Schedule of Charges( SOC) agreed upon between the
Hospital and the TPA and has charged the complainant a higher rate, which cannot be
entertained.
4. I have heard both the sides and perused the documents. I am of the opinion that the TPA
should have monitored the rate being charged by the hospital. The complainant cannot be
deprived of the entitled amount under the policy on account of the hospital not adhering to
the Agreement laid down between the TPA and the Hospital. The Admissible Claim amount
inclusive of Admission Fees is therefore, as under:
Total Claimed amount :Rs.7,1820/-
Non payable :Rs.6,470/-
Total admissible amount :Rs. 65,350/-
as per policy terms & conditions
Already settled to hospital : Rs.25,168/-
Settled to patient : Rs. 22,847/-
Remaining Admissible Amount : Rs. 17,335 /-
In the result, an award is passed, directing the Respondent Insurer to pay an amount of Rs.
17,335 /- , within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 30
TH
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0299/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-055-2122-0315
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mrs. Sabira Sageer
Kaliparambil House SRM Road Kochi
682018
2.
Policy Number
:
GHI-BF_19-IN4833829
3.
Name of the Insured
:
Mr. K S Sageer
4.
Name of the Insurer
:
Aditya Birla Health Insurance Company
Limited
5.
Date of receipt of Complaint
:
09.07.2021
6.
Nature of complaint
:
Rejecton of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Ms. Sabira Sageer (Online)
2. For the Insurer
:
Ms. Manali Shukla(online)

AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejecton of mediclaim. The complainant,
Mrs. Sabira Sageer is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that she and her family are insured for the past 3 yrs. with Bajaj
Insurance . In 2019-2020, her husband crossed 60 yrs. of age and Bajaj Insurance themselves
got them insured with Aditya Birla Health Insurance. The 3
rd
year policy was taken as a
continuation of the earlier 2 years. On 1/2/2021, her husband underwent colloid cyst surgery
on throat . The claim was however, rejected . Her attempts at visiting the offices of both Bajaj
insurance and Aditya Birla Insurance have been in vain.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that they are settling the claim
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that the
Ins. Co. did not pay the claim for eight months. . The Respondent Insurer submitted that they
had rejected the claim since there is a Waiting Period of 2 years. However, now they have
granted Continuity benefits and are ready to settle the claim for Rs. 78,315/- They will also be
sending the link to the complainant for renewing the policy. If the complainant is interested ,
she may use the link to pay the renewal premium within two days .
4. I have heard both the sides and perused the documents. The Complainant has not
submitted any claim documents to this Forum. The respondent Insurer has agreed to settle
the claim for Rs. 78,315/- and the complainant has agreed to the amount in settlement of the
claim. The respondent Insurer has also offered to send a link to the complainant for renewing
the policy and the complainant stated that she would take a decision whether to renew or not.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0300/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-023-2122-0450
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Ms. Anu James
Edamana House Edanad P O Pala
686574
2.
Policy Number
:
H0582800
3.
Name of the Insured
:
Ms. Anu James

4.
Name of the Insurer
:
IFFCO-TOKIO Genl. Insc. Co. Ltd.
5.
Date of receipt of Complaint
:
03.08.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid
7.
Amount of relief sought
:
--
8.
Date of hearing
:
23.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Ms. Anu James (Online)
4. For the Insurer
:
Dr Balasubramanian (Online)
AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Ms. Anu James is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that she was infected with Covid 19 on 21/4/2021 and was admitted
in hospital with c/o fever, cough, sore throat and breathing difficulty. She submitted all the
claim documents on 5/6/2021.. They called for Indoor Case Papers, which also she submitted.
But they closed the claim stating insufficiency of documents. She once again submitted the
documents but she did not get any response although she wrote to the griev. Dept. also. She
is a nurse by profession. She requests the Ombudsman to provider her the eligible amount.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the respondent Insurance Company (hereinafter referred to as “Iffco Tokio General
Insurance Co Ltd”) had issued a Corona Rakshak Benefit policy, with the Sum Insured of INR
2,50,000, for the period from 30/12/2020 to 10/10/2021, strictly subject to terms and conditions
of the policy,
That it is pertinent to mention that the Policy terms and conditions specifically mentions as policy
clause 4.1 “Covid Cover”, 3.7 Hospitalization, 3.6 Hospital, as stated under:-
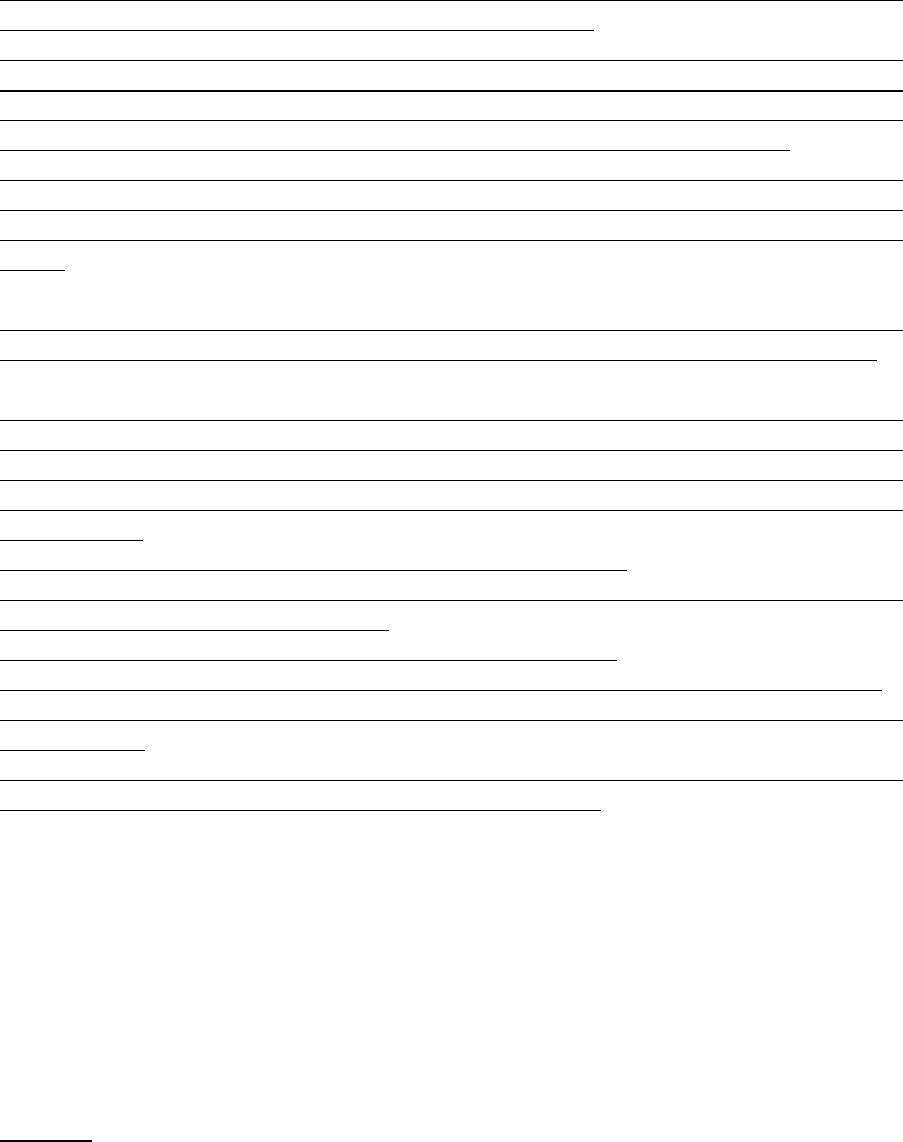
1. 2. OPERATIVE CLAUSE:- If during the policy period the Insured Person is diagnosed with
COVID and hospitalized for more than seventy-two hours …..
following Medical Advice of a duly qualified Medical Practitioner as per the norms specified
by Ministry of Health and Family Welfare, Government of India, the Company shall pay the
agreed sum insured towards the Coverage mentioned in the policy schedule, the copy of
guidelines issued by Ministry of Health and Family Welfare, Government of India,
2. 4.1 - COVID Cover :- Lump sum benefit equal to 100% of the Sum Insured shall be payable on
positive diagnosis of COVID, requiring hospitalization for a minimum continuous period of
72 hours. The positive diagnosis of COVID shall be from a government authorized diagnostic
centre.
3. 3.7 - Hospitalisation means admission in a hospital designated for COVID-19 treatment by
Government, for a minimum period of seventy-two (72) consecutive ‘In-patient care’ hours.
4. 3.6. Hospital means any institution established for in-patient care and day care treatment of
disease/ injuries and which has been registered as a hospital with the local authorities under
the Clinical Establishments (Registration and Regulation) Act, 2010 or under the enactments
specified under Schedule of Section 56(1) of the said Act, OR complies with all minimum cri-
teria as under:
1. has qualified nursing staff under its employment round the clock;
2. has at least ten inpatient beds, in those towns having a population of less than ten lakhs and
fifteen inpatient beds in all other places;
3. has qualified medical practitioner (s) in charge round the clock;
4. has a fully equipped operation theatre of its own where surgical procedures are carried out.
5. maintains daily records of patients and shall make these accessible to the Company’s author-
ized personnel.
6. For the purpose of this policy any other set-up designated by the government as hospital for
the treatment of Covid-19 shall also be considered as hospital.
That the client had submitted a claim, where the patient was found COVID positive with fever,
cough, sore throat, on 21/04/2020 and was treated in Nirmala Medical Center, Kerala from
21/04/2021 to 24/04/2021.
On scrutiny of submitted medical documents, it was concluded that patient had a history of
fever, cough, sore throat . Query was raised for indoor case paper with treatment chart, to the
insured dated on 13/05/2021. As per the received indoor case paper, temperature, pulse rate,
respiratory rate are within normal limits, insured vitals were stable. Insured admitted for the
purpose of isolation to prevent infection. Hence, the claim was repudiated on 04/08/2021 due
to hospitalization not justified,
PLEA: -
In the light of above submission, it is clear that there was no deficiency on the part of insurer,
as the claim was legally & justifiably repudiated considering the terms and conditions of the
insurance policy and accordingly the claim is not tenable and earnestly plead for the dismissal
of the complaint filed by the complainant and further pass such other order which Hon’ble
Ombudsman would deem fit.
3.I heard the Complainant and the Respondent Insurer. The Complainant submitted that she
had submitted all the claim documents to the Ins. Co. and also approached their Griev. Dept.
but there was no update from them. They had misplaced her Indoor Case papers also. Later,
when she filed Complaint with this Forum, then they sent a rejection letter stating that her
symptoms were mild. She had got admitted to the hospital out of panic as she was working as
trainee nurse in Covid ward during April and May 2021. She had low BP and fainting, severe
cough and headache besides chest infection and severe chest pain . She took discharge
because she was not able to bear the hospital expenses. After discharge when she joined for
duty, she was put again in Covid ward and so she had to quit her job .
The Respondent Insurer submitted that as per the indoor case paper, temperature was 98
degrees, pulse rate 80,82, respiratory rate 20 , SpO2 all within normal limits, insured vitals
were stable. Insured admitted for the purpose of isolation.
4. I have heard both the sides and perused the documents. The complainant repeatedly stated
that she was a trainee nurse in Carmel Hospital, however no Nursing Certificate or Trainee
Nurse Certificate/ Employment Certificate was submitted to this Forum. The complainant, 24
yrs. of age , was in the hospital from 21/4/2021 06:29 to 24/4/2021 06:42 , 72 hrs. She
wanted to go home and got discharged just after 72 hrs . She had not tested Covid negative by
then . Hospital asked her to Repeat Antigen Test on 30/4/2021 only.
Lump sum benefit equal to 100% of the Sum Insured shall be payableonly when required to be
hospitalized for more than seventy-two hours following Medical Advice of a duly qualified
Medical Practitioner as per the norms specified by Ministry of Health and Family Welfare,
Government of India. The complainant’s vitals were normal with SpO2 98 and 99 % and her
temperature was 98.6 all the days. She was treated only on oral medicines. Although she stated
that she had chest infection and severe chest pain , no tests were conducted .Her statement of
her condition of low BP and fainting, headache besides chest infection and severe chest pain
are not reflected in the Discharge Summary. I am of the opinion that she got herself admitted
in the hospital for 72 hrs. solely with the intention of deriving Benefit under the policy. I opine
that her condition did not warrant hospitalization.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0302/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-012-2122-0384
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Saju K J
Kachappilly House, Vettukadavu
Road, Chalakudy P O, Thrissur -
680307
2.
Policy Number
:
2894/00030870/000/00
3.
Name of the Insured
:
Mr. Saju K J
4.
Name of the Insurer
:
Cholamandalam MS Gen. Insu.Co.
Ltd
5.
Date of receipt of Complaint
:
19.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
14.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Saju K J (Online)
2. For the Insurer
:
Dr Sudipta(Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Saju K J is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he, his wife and son were diagnosed covid positive and were
admitted to Govt. CFLTC, St James Medical Academy during Nov, 2020. His claim was rejected
stating that Query response was not received. The indoor case papers were provided. It shows
that he was suffering from severe headache for two consecutive days during the admission.
He was administered medicines. His wife had body pain and cough and has not recovered still
and was admitted to Apollo Adlux Hospital for post covid sequlae. The repudiation of the claim
caused severe mental agony as he had already been under severe financial distress due to
unemployment during the admission and quarantine period. He requests the Ombudsman to
provide relief by ordering settlement of full claim amount of Rs. 2 lakhs.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the subject mentioned policies are Corona Rakshak Policy issued in the name of
complainant Mr Saju K J for the effective period from 03/09/2020 to 30/05/2021 for sum
insured of Rs 100000 in the name of his wife Mrs Shiny for the effective period from
03/09/2020 to 30/05/2021 for sum insured of Rs 50000 , and in the name of his son ,Mr
Sharon Saju for the effective period from 03/09/2020 to 30/05/2021 for sum insured of Rs
50000 and the same is subject to terms , conditions and exclusions of the policy.
On Scrutiny of the claims documents submitted, we observe that the claims are not admissible
for the following reasons:
On perusal of the claim documents, it is observed that the treatment given during the
hospitalization period doesn’t warrant inpatient admission; only oral medications were
administered and Insured medical condition was within normal limits and not requiring
hospitalization as per Ministry of Health Guidelines
The vitals were stable and admission not required hence the claims are inadmissible
The complainant, his wife and son were admitted in CFLTC , St James Academy , Chlakkudy for
Covid 19- positive
In the claim of Mr Sharon Saju , the discharge summary shows no active line of treatment .On
perusal of, medical records, It is understood that inpatient hospitalisation is not justified as
vitals were stable hence the claim is inadmissible.
In the claims of complainant Mr Saju K J and Mrs Shiny , query request were made for
submission of indoor case papers and vital charts . The indoor case papers and vital charts
were not submitted by the complainant even after the query request. Thus the available
medical documents such as the discharge summary and medical certificate, shows no active
line of treatment. On perusal of, medical records, It is understood that inpatient
hospitalisation is not justified as vitals were stable .The discharge summary as well as the
treatment certificate will prove that no active line of treatment was given to the complainant
and his son , hence the claims are inadmissible.
This respondent have rightly repudiated the claim of Mr Sharon Saju which is reproduced
herewith. “On perusal of the document it is observed that the treatment given during
hospitalisation period does not warrant inpatient admission; only oral medications were
administered and insured medical condition was with in normal limits and not requiring
hospitalisation as per Ministry of Health Guidelines ‘’
As per the Clinical Management Protocol issued by Ministry of Health , Government Of India,
clause 7 states as to Clinical severity and assessment parameters where in it is explained the
case of mild case of clinical severity where in certain symptoms are mentioned therein and
mentioned with management at Home or covid centre . In the present case , as per the
discharge summary itself , the complainant had no such symptoms and could have managed
at home quarantine. The claim form which was duly filled by the treated doctor will also prove
that there was no active line of treatment.
It is further submitted that Clause 10 (1) of Clinical Management Protocol issued by Ministry
of Health , Government Of India the states about management of mild cases . Patients with
mild disease may present to primary care /outpatient department, or detected during
community outreach activities, such as home visits or by telemedicine. The complainant had
no symptoms or had no history of co-morbidities. Even he had no symptoms of complications
that would prompt urgent care. Thus this respondent had rightly repudiated the claim and
hence for the above mentioned reasons, the complaint is to be dismissed
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
had Corona and had fever and headache and was in Govt. Hospital for 13 days, his wife had
breathing difficulty , body pain, chest pain and heart rate of 112 and fibrosis in lungs and son
was also diagnosed Covid positive and all were taken by ambulance and admitted to Govt.
CFLTC. His wife was admitted to Apollo Adlux Hospital for post covid problems. He is loading-
worker in FCI and could not go for his work . The Respondent Insurer submitted that no
investigations or treatment was given during hospitalization and they initially repudiated as
Query letters were not responded to. As regards post covid problems of his wife alleged by
the complainant , there is no published medical report on GB Calculus being a post covid
condition .
4. I have heard both the sides and perused the documents. The complainant and his wife and
son were admitted to CFLTC only for isolation. CFLTC does not fall in the definition of hospital.
The following facts are observed from the Discharge Summary / Case Records:
Complainant : treatment given - nil , Case record 10 days: temp below 98.5 all days and
respiration ( SpO2) on 9 days 97, 98% except 7th day 95%. Progress note of 11 days: 2
days headache paracetemol 1-0-1 , all other days G C good
Compalinant’s wife: Case record - temp below 98.5 all days and respiration (SpO2) 99% on
admission, other days 98% TO CHECK
1
st
day body pain / tab diclophenac
4th Day one day cough / syrup expectorant , c mox 1-1-1, T CPM 0-0-1
Compalinant’s son: treatment written and struck. Oral tablets: Azithromycin , cetirizine, c-
omez
During the Hearing, the complainant was asked to submit the Case Record of his son was
within a week of the Hearing but it is not received till date.
The above facts establish that their Vitals were normal , there was no active line of treatment,
only oral medicines given to wife and there was no necessity for hospitalization for them as
per Covid management guidelines from the Govt. The claims are therefore not tenable.
Further, the subsequent consultation taken by the complainant’s wife at Apollo Adlux
Hospital reveal that she had h/o hepatomegaly Gr II and there was No GB calculi, Mild gall
bladder wall edema?/ doubtful, Reactive, due to liver , disease, bilateral ovarian cysts benign
characteristics, which are not related to post Covid medical issues but pre-existing ailments .
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0303/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-012-2122-0383
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Soj Joseph
Chelekattuparambil House,
Govt Hospital Road, Chalakudy P O,
Thrissur - 680307
2.
Policy Number
:
2894/00051038/000/00|2894/00011971|
2894/00051035/000/00
3.
Name of the Insured
:
Mr. Soj Joseph
4.
Name of the Insurer
:
Cholamandalam MS Gen. Insu.Co. Ltd
5.
Date of receipt of Complaint
:
19.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
14.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Soj Joseph (Online)
2. For the Insurer
:
Dr Sudipta(Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Soj Joseph is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he, his wife and son tested Covid positive and were admitted to
CFLTC, St James Medical Academy, Chalakudy during Oct./Nov. 2020. He had registered the
claim on 30/11/2020 and even after providing vital charts and indoor case papers, the Ins. Co.
is delaying his claim settlement. The claims of his wife and son were repudiated. He had severe
cough during the entire duration of admission, his wife had Covid symptoms like loss of smell
etc. and son had loss of smell and taste. Although his son’s claim was registered on 4/12/2020,
query for Discharge Summary, treatment and Vital chart was raised only on 22/2/2021, after
80 days , although Ins. Co, has to settle or reject within 30 days from dt. of receipt of last
necessary documents .
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the subject mentioned policies are Corona Rakshak Policy issued in the name of
complainant Mr Soj Joseph for the effective period from 13/10/2020 to 10/04/2021 for sum
insured of Rs 1,00,000, in the name of his wife Mrs Sheeja for the effective period from
13/08/2020 to 08/02/2021, for sum insured of Rs 50,000 , and in the name of his son ,Mr
Sanjay Soj for the effective period from 13/10/2020 to 10/04/2021 for sum insured of Rs
50,000 and the same is subject to terms , conditions and exclusions of the policy.
On Scrutiny of the claims documents submitted, we observe that the claims are not
admissible for the following reasons:
On perusal of the claim documents, it is observed that the treatment given during the
hospitalization period doesn’t warrant inpatient admission; only oral medications were
administered and Insured medical condition was within normal limits and not requiring
hospitalization as per Ministry of Health Guidelines
The vitals were stable and admission not required hence the claims are inadmissible
The complainant, his wife and son were admitted in CFLTC , St James Academy , Chlakkudy for
Covid 19- positive
In the claim of the wife of the complainant- Mrs Sheeja , the discharge summary , Treatment
certificate and the case records with nurses note and progress note issued from the CFLTC
shows no active line of treatment .On perusal of, medical records, It is understood that
inpatient hospitalisation is not justified as vitals were stable .The discharge summary , case
records, treatment certificate will prove that no active line of treatment was given to the
complainant , hence the claim is inadmissible.
In the claims of complainant Mr Soj Joseph and his son Mr Sanjay Soj , query request were
made for submission of indoor case papers and vital charts as the complainant had
submitted only the discharge summary and medical certificate in both the claims . The indoor
case papers and vital charts were not submitted by the complainant even after the query
request. Thus relying on the available medical documents such as the discharge summary and
medical certificate, shows no active line of treatment. On perusal of, medical records, It is
understood that inpatient hospitalisation is not justified as vitals were stable . The discharge
summary as well as the treatment certificate will prove that no active line of treatment was
given to the complainant and his son , hence the claims are inadmissible.
This respondent have rightly repudiated the claim of Mrs Sheeja which is reproduced herewith.
“On perusal of the document it is observed that the treatment given during hospitalisation
period does not warrant inpatient admission; only oral medications were administered and
insured medical condition was with in normal limits and not requiring hospitalisation as per
Ministry of Health Guidelines ‘’
The claim of Soj Joseph and his son Mr Sanjay Soj are liable to be repudiated on the ground
that “On perusal of the document it is observed that the treatment given during
hospitalisation period does not warrant inpatient admission; only oral medications were
administered and insured medical condition was with in normal limits and not requiring
hospitalisation as per Ministry of Health Guidelines ‘’
As per the Clinical Management Protocol issued by Ministry of Health , Government Of India,
clause 7 states as to Clinical severity and assessment parameters where in it is explained the
case of mild case of clinical severity where in certain symptoms are mentioned therein and
mentioned with management at Home or covid centre . In the present case , as per the
discharge summary itself , the complainant had no such symptoms and could have managed
at home quarantine. The claim form which was duly filled by the treated doctor will also
prove that there was no active line of treatment.
It is further submitted that Clause 10 (1) of Clinical Management Protocol issued by Ministry
of Health , Government Of India the states about management of mild cases . Patients with
mild disease may present to primary care /outpatient department, or detected during
community outreach activities, such as home visits or by telemedicine. The complainant
had no symptoms or had no history of co-morbidities. Even he had no symptoms of
complications that would prompt urgent care. Thus this respondent had rightly repudiated
the claim and hence for the above mentioned reasons, the complaint is to be dismissed
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he,
his wife and son tested Covid positive and were admitted to CFLTC. He had registered the claim
on 30/11/2020 and even after providing vital charts and indoor case papers, the Ins. Co.
delayed claim settlement. He had severe cough, his wife had breathing difficulty and son also
was admitted though he had no problems . The Respondent Insurer reiterated the facts in
their self contained note that the discharge summary and medical certificate, shows no active
line of treatment. Inpatient hospitalisation is not justified as vitals were stable .
4. I have heard both the sides and perused the documents. The following is observed from
the case records:
Complainant- temp: below 98.5 all days , Respiration( SpO2) : 98 or 99 % all days , cough-
treated with syrup expectorant
Complainant’s wife- receive patient to CFLTC , no special complaints ,
temp: below 98.5 all days, Respiration ( SpO2): 98 or 99 % all days
Complainant’s son - received patient to CFLTC , no special complaints ,
temp: below 98.5 all days, Respiration ( SpO2): 98 or 99 % all days
Foremost of all , CFLTC does not fall in the definition of hospital as stated in the policy.
Admission to CFLTC was only for isolation. It is observed that Vitals were normal and there
was no active line of treatment . The treatment if any could have been taken at home. On his
own admission, the complainant and his wife and son had no significant symptoms or none.
I am therefore of the opinion that there was no hospitalization and also that there was no
necessity for hospitalization as per Covid management guidelines issued by the Govt.. The
claims are therefore not tenable.
It is also a fact that most offices in the State ,so also Ins. Cos. , were either closed for varying
durations during the pandemic on account of lockdown or were functioning alternate days ,
so I cannot find fault with any delay whatsoever on the part of the Respondent Insurer.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30th day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0305/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-050-2122-0417
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Dr.Ajin Sunny
Alappadan House, Kalyanamandam
Road, Nadathara P O, Thrissur -
680751
2.
Policy Number
:
443500/48/2021/890
3.
Name of the Insured
:
Mr. Dr.Ajin Sunny
4.
Name of the Insurer
:
The Oriental Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
14.07.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
14.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Dr.Ajin Sunny (Online)
2. For the Insurer
:
Ms.Umavathy C S (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Dr.Ajin Sunny is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had submitted reasons for the delay in claim intimation. As
he met with an accident while travelling with family on 27/2/2021 and had to take rest for a
week. In-between his father tested covid positive and entire family had top quarantine again.
Even though he is busy with Covid duties at Daya Hospital, he had given clarifications to the
Ins. Co.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the office has issued a Corona Rakshak policy No.443500/48/2021/890 for the period
23/09/2020 to 04/07/2021 covering Complainant, Dr. Ajin Sunny with Sum Insured of
Rs.2,50,000/-.
Dr. Ajin Sunny was admitted in Daya General Hospital Ltd., Trichur on 08/02/2021 following
positive diagnosis of covid 19 and discharged on 13/02/2021. But the Insured had submitted
the claim documents to MD India Health Insurance TPA only on 26/03/2021; hence there is
13 days delay in submission of documents by the Insured, which is against clause 7.2 of our
policy. As per clause 7.2, the time limit prescribed for submission of necessary documents by
the Insured person to TPA/Company is within 30 days of date of discharge from the hospital
following positive diagnosis for COVID. This condition was not complied with by the Insured
in this case.
The admissibility of the claim is subject to clauses, exclusions, coverage, terms, conditions
and definitions of the policy. General Condition No.8.2 – Condition to Precedent to
Admission of Liability reads as the terms and conditions of the policy must be fulfilled by the
Insured person for the Company to make any payment for claims arising under the policy.
In view of the above, the claim is not admissible under clause 7.2 and supporting General
Condition 8.2 of our policy and hence, we humbly pray that the Hon'ble Ombudsman may
be pleased to exonerate us from the above liability and dismiss the case accordingly.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that the
delay in intimation was due his parents also contracting Covid seven days after his discharge
and also an accident he met with . The Respondent Insurer submitted that there was delayed
submission of documents and the delay could not be condoned.
4. I have heard both the sides and perused the documents. The Discharge summary states
complaint of fever, mild breathing difficulty, DOE (dyspnea on exertion ) and cough . The
complainant is a Doctor, Health Care Worker at the same hospital and would have
contracted Covid by contact . I am of the opinion that the delay in submission of documents
has to be condoned and that the claim has to be paid. The Sum Insured Rs. 2,50,000/- is the
amount payable.
In the result, an award is passed, directing the Respondent Insurer to pay an amount of
Rs.2,50,000/- , within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0306/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-050-2122-0370
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. A R Balasubramanian
Apartment 61, Juhu Ajanta CHSL,
JVPD Scheme, Gulmohar Road,Vile
Parle West, Mumbai 400049
2.
Policy Number
:
440100/48/2022/430
3.
Name of the Insured
:
Mr. A R Balasubramanian
4.
Name of the Insurer
:
The Oriental Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
30.06.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. A R Balasubramanian (Online)
2. For the Insurer
:
Ms.Maya satish(Online)
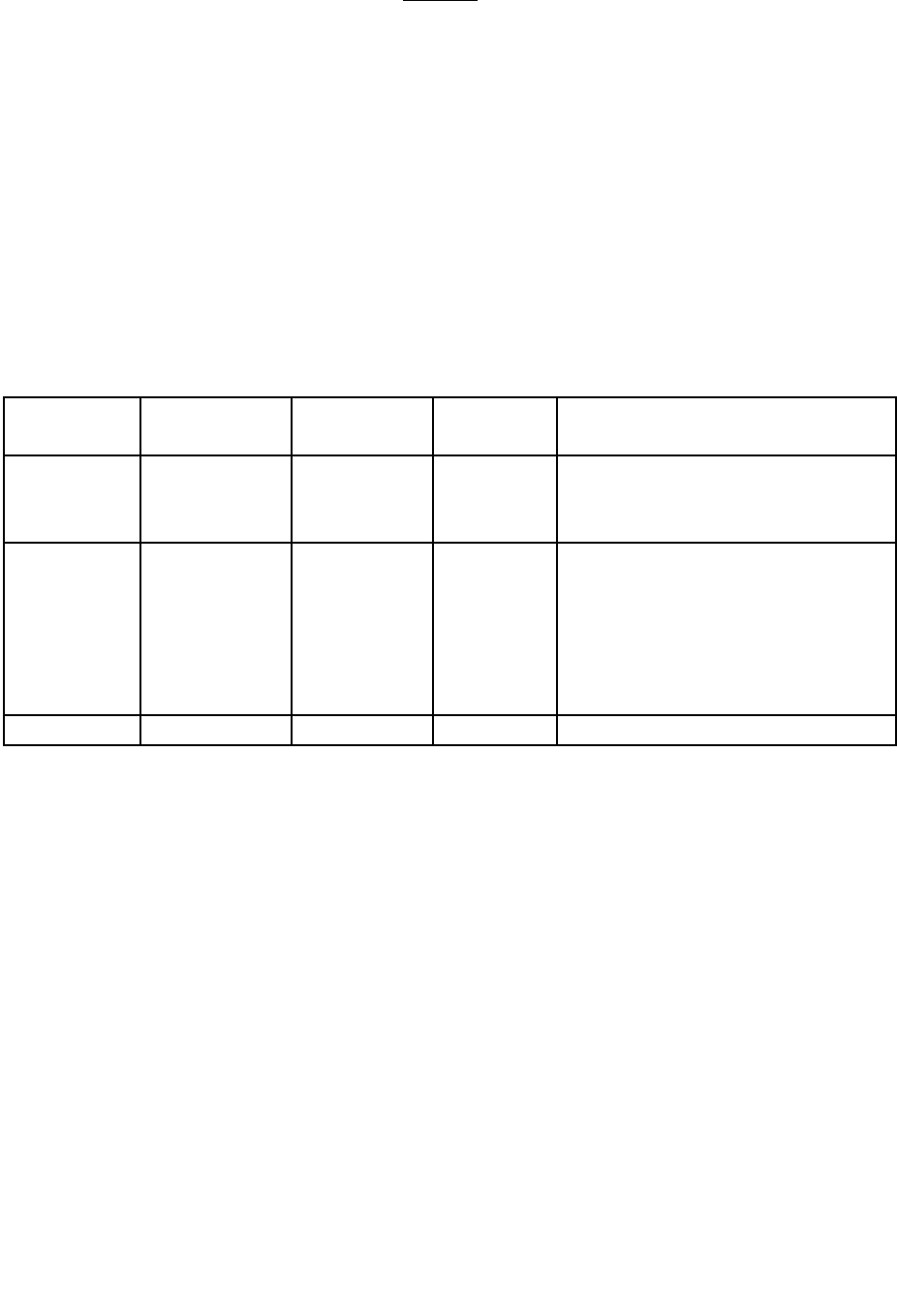
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is Rejection of mediclaim. The complainant, Mr. A
R Balasubramanian is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he has an insurance policy with Oriental insurance for the last
18 years. He had to get both his eyes operated for cataract in November 2020. Details of the
claim are :
Claim no.
Claimed
Amount
Approved
Amount
Rejected
Amount
Rejected A/c head
KOC-1120-
CL-0003064
93,000
35,500
57,500
Anaesthesia charges, surgeon
charges, SPE procurement
charges
KOC-1120-
CL-0003160
95,869
35,500
60,369
Laboratory investigation,
ECG, Anaesthesia charges,
surgeon charges, medicines,
nursing charges (allowed as per
the previous claim), medicines,
OT charges
Total
1,88,869
71,000
117,869
The insurance company has informed e that a large portion of his claim has been rejected as
per clause 1.1, which allows for reasonable and customary charges. He wishes to present his
current situation.
He is a 76-year-old retired citizen. He currently gets a PF pension of Rs. 913 per month, which
is insufficient to meet needs of a decent living by any standards. He moved to live with his son
in Mumbai and has been in Mumbai through the pandemic.
During his stay in Mumbai, his eye sight went from bad to worse and he struggled to even
read regular news, hence he had no option but to see an eye doctor who advised cataract
surgery for both eyes.
Mumbai has been one of the worst affected cities during the pandemic and most hospitals
have been overflowing with covid cases. He has diabetes and blood pressure. With these
comorbidities and age not being on his side, he feared for life, hence he decided to consult at
an specialty eye clinic that does not handle Covid cases.

He is 76 year old and his son has asthma, hence they were not in a position to venture out to
look for alternatives.
Due to these reasons he decided to go ahead with the eye clinic for surgery. Prior to the
surgery, he had inquired with the third party (Vidal Health) and also with the branch offices
(Ravipuram and Layam Road, Ernakulam, Kerala) on whether a maximum cap exists for
cataract surgery. He was informed by them that there are no such monetary caps and the
amount will be reimbursed based on submission of documents per process. Basis this
assurance, he went ahead with the surgery.
What was considered reasonable and customary has undergone a significant change during
the pandemic. This clause also needs to be applied in the context of the profile of the patient,
financial situation and circumstances and not a blind reading of the English mentioned in the
clause.
Hence, he humbly requests the Ombudsman to consider his request and direct the insurer to
pay the claim amount in full.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that Mr. A.R. Balasubramanian who is covered under the MC Policy No.440100/48/2022/430
, had lodged a claim with M/s Vidal Health TPA Pvt. Ltd under the above policy for the
treatment of Cataract surgery for both eyes at Shroff Eye Hospital Mumbai 16.11.2020 and
20.11.2020.
As per the documents submitted he had incurred an amount of Rs.93,000/- and Rs.95,869/-
, towards Cataract Surgery at Shroff Eye Hospital Mumbai.
As per Policy Clause 1.1 of the policy , it is a condition precedent that the expenses incurred
in respect of medically necessary treatment, are reasonable and customary. Therefore, as per
clause1.1 only reasonable and customary charges are payable towards the claim.
The claim was settled on the basis of reasonable and customary taking into consideration the
cost of the same surgery/treatment in a similar hospital in the same locality. The expenses
incurred over and beyond the reasonable and customary charges are to be borne by the
insured. Hence no additional amount is found payable.
It is prayed, that the Hon. Ombudsman may uphold the decision of the company and dismiss
the complaint.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
had undergone cataract surgeries in both eyes and did not receive the full claim payment. .
The Respondent Insurer submitted that Reasonable and Customary charges were paid
according to the policy , by considering charges in similar hospital and locality.
4. I have heard both the sides and perused the documents. The complainant has undergone
Phacoemulsification Cataract surgery with Monofocal MINI WELL IOL for his eyes. The
treatment undertaken by the complainant, 76 yrs. of age, is at a high-end hospital supported
by latest technology. The complainant has taken Family Floater Policy with Sum Insured of
Rs.4 lakhs and he is entitled to claim accordingly for his surgery and hospitalization expenses
incurred at that hospital including charges for Digital Imaging System Assistance. The
Admissible Claim amounts are :
Sl.
No.
Date of
hospitalisation
Amount
Billed
Rs.
Amount
Payable
Less 10% Co-
Pay
Rs.
Amount
Already
Paid Rs.
Balance
admissible
amount Rs.
i
20/11/2020
93,000
83700
31,950
51,750
ii
06/11/2020
95,868
86,281
31,950
54,331
TOTAL
→
1,06,081
In the result, an award is passed, directing the Respondent Insurer to pay an amount of Rs.
1,06,081 , within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0307/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)bREAD WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0475
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Cheriyan P Mathew
Plathodathil House Thelliyoor P O Thiruvalla
Pathanamthitta 689544
2.
Policy Number
:
1005062820P103606688
3.
Name of the Insured
:
Mrs. Jiby Mathew
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
06.08.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
27.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Cheriyan P Mathew (Online)
2. For the Insurer
:
Ms. Dhanya (Online)

AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. Cheriyan P Mathew is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his spouse aged 34 years was admitted at the Kottayam
Thellakam Carithas Hospital on 23.11.20 , with breathlessness and was unable to walk. She
was discharged on 26.4.21. Various tests were taken – Asthma, GERD, Anxiety, Heart-Echo,
Cardiography, CT Pulmonary Antiogram, Neurology, X –Ray etc. The total expenses were
Rs.34,000/-( Hospital Bill- Rs. 23,419 /--). The claim was rejected. The policy inception date
was 21.7.17. The complainant prayed for the settlement of the claim.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the respondent had issued a Family Medicare Insurance Policy, vide Policy
No.1005062820P103606688 to the Complainant for covering himself, spouse, daughter& son
from 21/07/2020 to 20/07/2021. The total Sum Insured was Rs.2,00,000/- and they had
continuous coverage since 21/07/2017.M/s Health India Insurance TPA Services Private
Limited is the Servicing TPA for this Policy. The wife of the Complainant was hospitalized for
a period of 3 days from 23/04/2021 to 26/04/2021 at CARITAS HOSPITAL, Thellakom, Kottayam,
as she was suffering from breathing problems, for diagnostic purposes. This was clear from
the complaint letter and from the documents submitted and also bills.The complainant`s claim
for an amount of Rs.36,244/-, was repudiated by the TPA based on the policy terms and
conditions(Policy Exclusion No 4.11), “Charges incurred at Hospital or Nursing Home primarily
for diagnosis, x-ray or laboratory examinations or other diagnostic studies not consistent with
or incidental to the diagnosis and treatment of positive existence or presence of any ailment,
sickness or injury, for which confinement is required at a Hospital/ Nursing home”. Hence, as
per the policy terms and conditions, the claim is not payable.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
wife was admitted at the Carithas Hospital, Kottayam, on 23.4.21, as she suddenly felt
breathlessness and was unable to walk. After the treatment, she was discharged on 26.4.21.
The claim was denied. The Respondent Insurer submitted that as per the Complainant`s letter
and the documents submitted, it was clear that the patient was admitted for diagnostic
purposes. The claim was therefore denied under policy exclusion -4.11.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted. In this case where the Insured`s claim for her hospitalization for breathlessness
and unable to walk was denied, the arguments put forth by the respondent insurer are:-
1. On scrutiny of the Complainant`s letter and documents submitted, it was clear that the
patient was admitted for diagnosis purposes.
2. The claim was therefore denied under policy exclusion clause -4.11 - “Charges incurred at
Hospital or Nursing Home primarily for diagnosis, x-ray or laboratory examinations or other
diagnostic studies not consistent with or incidental to the diagnosis and treatment of positive
existence or presence of any ailment, sickness or injury, for which confinement is required at
a Hospital/ Nursing home”.
On analyzing the hearing and records, I find that the arguments put forth by the respondent
insurer are tenable. I therefore do not want to interfere in the decision of the respondent
insurer in denying the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0308/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)bREAD WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0376
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.

AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. Raju K K
Kanjiramthadathil House Thiruvaniyoor P O
Puthencruz 682308 Thiruvaniyoor
2.
Policy Number
:
1013012820P109298318
3.
Name of the Insured
:
Mr. Raju K K
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
05.07.2021
6.
Nature of complaint
:
Partial payment of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
3. For the Complainant
:
Mr. Raju K K (Online)
4. For the Insurer
:
Mr. Kiran Mohan and Mr.
Ajithkumar(Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding partial payment of mediclaim. The
complainant, Mr. Raju K K is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he is having a health insurance policy with the respondent
insurer for a sum insured of Rs.2 Lakhs for the last 5 years. He was admitted at Medical Trust
Hospital on 08/01/2021 due to Acute Coronary Syndrome and discharged on 11/01/2021. The
total hospital bill of Rs.1,48,818/- expenditure incurred but the Insurance company approved
an amount of Rs.80,724/- only. The post hospitalization bills claimed for Rs.16.246/- out of
which an amount of Rs.13,682/- was also approved by the insurance company. The
deductions of Rs.68,095/- and Rs.2564/- were made by the insurance company without any
valid reasons.
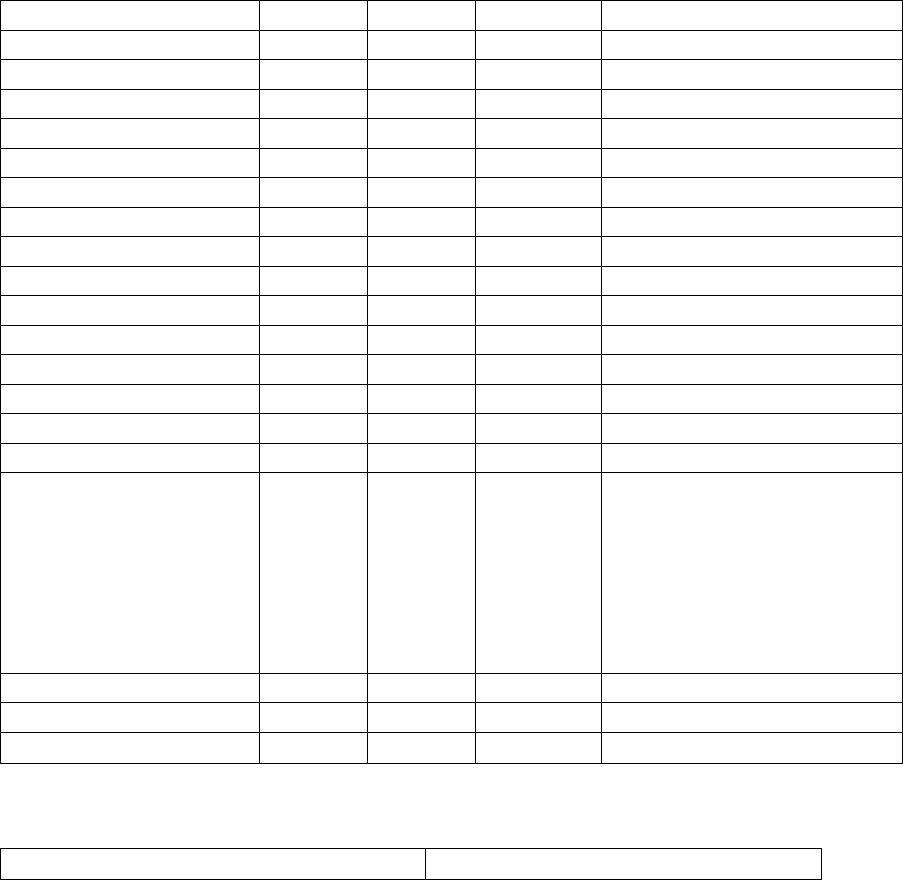
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the Family health insurance policy bearing no.1013012820P109298318 was issued to
Mr.Raju and his family for a floater sum insured of Rs.2,00,000/-. The complainant insured
was admitted in Medical Trust Hospital, Kochi for Acute Coronary Syndrome for the period
from 08/01/2021 to 11/01/2021. The total Bills submitted for this hospital admission was
Rs.1,48,819/-, out of which an amount of Rs.80,724/- was settled. The deduction of
Rs.68,095/- was done for non medical items, food charges, misc charges which are not payable
as per the policy terms and conditions.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
policy is having a sum insured of Rs.2,00,000/-. While settling his reimbursement claim, the
respondent insurance company settled the claim after deducting an amount of Rs.68,095/-
without stating any valid reasons. The Respondent Insurer submitted that the claim was
settled by the company’s TPA. The deductions made by the TPA while settling the claim was
for non payable items like non medical items, food charges and misc charges. The respondent
insurance company reviewed the settlement made by TPA and submitted a detailed
calculation in tabular form as detailed below.
Item
Amount
Payable
Deducted
Reason
Consumables
2000
0
2000
NME
Medicines
13778
13778
0
Misc
96
0
96
NME
Surgical
80688
70545
10143
Consumables
Medical Gas
1500
1500
0
Lab
7760
7760
0
Radiology
300
300
0
Other Investigations
2200
2200
0
Professional/procedures
650
0
650
stab,syringe
Other charges
1300
0
1300
NME
Theatre/Care charges
5600
5600
0
ICU
3250
3250
0
CCU(nursing charges)
750
0
Cath lab
11050
11050
0
professional services
13700
13700
0
Nursing
3297
1200
2097
-750
----------
1347
injection charges , dressing
charges not payable. out of
3297; 750 is nursing
charges in CCU and hence
allowed under ICU
Room rent
1200
1200
0
diet and canteen
450
0
450
NME
148819
132833
15986
So the company is ready to pay an amount of Rs.52,109/- as detailed below
CLAIMED
148819
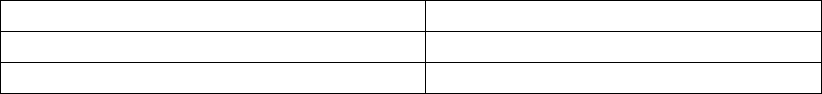
Payable
132833
Already PAID
80724
Balance payable
52109
4. After hearing the complainant and the respondent insurer and perusing the exhibits
produced before the forum, I find that out of the items shown as non payable in the SCN
should be reviewed as per the available sum insured. Therefore in the interest of justice I find
it appropriate to direct the Insurer to pay Rs.52109/- in addition to the amount already paid
under the claim.
In the result, an award is passed, directing the Respondent Insurer to pay an amount of
Rs.52109/-, within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0309/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0442
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mr. K R Prasad
Puthenpurayil House, Pandappilly P O,
Thottakara, Arakkuzha, Muvattupuzha -
686672
2.
Policy Number
:
P/181215/01/2021/003014

3.
Name of the Insured
:
Mr. K R Prasad
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
26.07.2021
6.
Nature of complaint
:
Rejection of mediclaim - Covid
7.
Amount of relief sought
:
--
8.
Date of hearing
:
27.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. K R Prasad (Online)
2. For the Insurer
:
Mr. Manu Mohan (Online)
AWARD
This is a complaint filed under Rule 13 (1)b read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding rejection of mediclaim. The
complainant, Mr. K R Prasad is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he holds a Corona Rakshak policy of the respondent insurer for
the period 30.7.20 to 11.5.21, vide policy no. P/181215/01/2021/003014. The complainant
on testing Covid 19 positive was admitted in the Nirmala Medical Centre, Muvattupuzha on
17.1.21 and was discharged on 21.1.21. On raising a claim with the respondent insurer by
submitting all relevant documents, after much delay, the insurer on 12.3.21, requested for
additional documents. The insurers stated that as per the documents submitted, the
complainant was a k/c/o Bronchial Asthma for one year and required documents to be
produced. It was replied that prior to the instant claim, he was not diagnosed with Bronchial
Asthma. His claim was repudiated vide the insurer`s letter dated 13.4.21. As per the policy,
the only requirement for the claim was that the person should have contracted Covid 19 and
be hospitalized 72 hours during the policy duration. The complainant prayed for a favorable
order. The quantum of relief sought is Rs.1lac.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that in this complaint, the discharge summary issued by the Nirmala Medical Centre ,
Muvattupuzha clearly reveals that the complainant had a history of Bronchial Asthma. The
cashless request dated 17.1.21, from the hospital indicates that the complainant had a past
history of Hypertension since 2years & Asthma since 1 year. The hospital records dated 17.1.21
also reveals that the complainant is a known case of Bronchial Asthma on Foracort 100 Inhaler.
The respondent insurer queried vide letter dated 12.3.21, to the complainant for first and all
consultation papers, investigating reports and treatment details pertaining to Bronchial
Asthma & complete set of Inpatient Case Sheet records, Vital Charts. The complainant
submitted only a letter dated 20.3.21 stating that he was not diagnosed with Bronchial Asthma
and had not treated for the same. As per policy condition no.8.4, the insured person should
provide all additional information and assistance as the company may require in dealing with
the claim.
Moreover the clinical parameters were silent in the discharge card. Based on the available
medical records it was clear that the patient`s vitals were stable and stayed at the hospital
only for observation/monitoring i.e. under institutional quarantine and hospitalization was
not warranted.
In this case as per records, it was clear that the past history of Hypertension since 2years and
Asthma for 1year before the inception of the policy was not revealed in the proposal form at
the time of the inception of the policy, by the Complainant. It amounts to suppression of
material facts. The claim was therefore repudiated which was informed to the complainant on
13.4.21.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he
was covered under the Corona Rakshak policy of the respondent insurer for the period 30.7.20
to 11.5.21. The complainant on testing Covid 19 positive was hospitalized at the Nirmala
Medical Centre, Muvattupuzha, for the period 17.1.21 to 21.1.21. His claim was rejected. The
Respondent Insurer submitted that as per the discharge summary the complainant had a
history of Bronchial Asthma. The cashless request from the hospital indicates that the
complainant had a past history of Hypertension since 2years & Asthma since 1 year. The
hospital records revealed that the complainant was a known case of Bronchial Asthma on
Foracort 100 Inhaler.
For the query to the complainant for submitting the first and all consultation papers,
investigating reports and treatment details pertaining to Bronchial Asthma & complete set of
Inpatient Case Sheet records, Vital Charts, the complainant submitted only a letter stating that
he was not diagnosed with Bronchial Asthma or had not treated for the same. As per policy
condition no. 8.4, the insured person should provide all the additional information and
assistance as the company may require in dealing with the claim. As per the discharge card,
the clinical parameters of the patient were silent. It was clear from the available medical
records that the patient`s vitals were stable and stayed at the hospital only for
observation/monitoring i.e. under institutional quarantine and hospitalization was not
warranted. The claim was therefore denied.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this complaint where the complainant`s Covid 19, claim under the
Corona Rakshak Policy was denied, the arguments put forth by the respondent insurer are:-
1. As per the discharge summary the complainant had a history of Bronchial Asthma.
2. The cashless request from the hospital indicates that the complainant had a past history of
Hypertension since 2years & Asthma since 1 year before the inception of the policy not
revealed in the proposal form at the time of the inception of the policy.
3. As per the medical records, the complainant was a known case of Bronchial Asthma on
Foracort 100 Inhaler.
4. As per the discharge card, the clinical parameters of the patient were silent.
5. From the available medical records it was noted that the patient`s vitals were stable and
stayed at the hospital only for observation/monitoring i.e. under institutional quarantine and
hospitalization was not warranted .
On analyzing the hearing and records, I find that the arguments put forth by the respondent
insurer are tenable. I therefore do not want to interfere in the decision of the respondent
insurer in denying the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0310/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 (1)i READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-048-2122-0457
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the
complainant
:
Mrs. sajeena sherafudeen,
Darul Aman Thirumullavaram P O
Kollam 691012
2.
Policy Number
:
570504501910000932
3.
Name of the Insured
:
Mrs. sajeena sherafudeen
4.
Name of the Insurer
:
The National Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
26.07.2021
6.
Nature of complaint
:
Non renewal of policy
7.
Amount of relief sought
:
--
8.
Date of hearing
:
27.09.2021
9.
Parties present at the hearing
1. For the Complainant
:
Mr. Sherafudeen (Online)
2. For the Insurer
:
Ms. Geetha Nair (Online)

AWARD
This is a complaint filed under Rule 13 (1)i read along with Rule 14 of the Insurance
Ombudsman Rules, 2017. The complaint is regarding non renewal of policy. The complainant,
Mrs. sajeena sherafudeen is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that she was holding a health policy of the respondent since
11.2.2015 till 10.2.21. Due to the Pandemic and financial crisis, she could remit the premium
only on the 47 th day from the renewal due date i.e. on 29.3.21. The insurer declined to renew
the policy and requested to take a fresh policy. The complainant prayed for directing the
insurers to renew the policy with continuity benefits.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted
that the complainant had approached the branch office of the respondent insurer for renewal
of her policy with continuity benefits on after a period of 47days break in insurance from the
date of expiry (10.2.21). All Mediclaim policies are subject to renewal with continuity of
benefits after condonation of delay for a maximum period of 30days from the date of expiry,
provided no claims during the break period will be entertained.
The condition no.5.16 reads as thus:
“ Renewal 5.16
The policy may be renewed by mutual consent. The company is not bound to give notice that
it is due for renewal. Renewal of the policy cannot be denied other than on grounds of fraud,
moral hazard, misrepresentation or non co-operation. In the event of break in the policy a
grace period of 30 (thirty) days is allowed. Coverage is not available during the grace period.
“
An amount of Rs.28,970/- (Rupees Twenty Eight Thousand Nine Hundred and Seventy Only)
was collected from Insured as deposit premium informing her that the same will be treated
as renewal premium, if at all the Competent Authority entertains her request for renewal with
continuity benefits and if the request is not entertained, the amount will be refunded which
was agreed by the Insured.
After several requests for providing the Bank account details to initiate the refund, she had
evaded the reminders and approached this Honourable forum.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that she
was holding the health policy since 11.2.2015 till 10.2.21 . Due to the pandemic situation and
financial crisis, the premium was remitted by her only on 29.3.21 i.e. on the 47 th day from
the renewal due date. The Respondent Insurer didn`t renew the policy and requested to take
a fresh policy. The Respondent Insurer submitted that the Complainant had approached the
branch office of the respondent insurer on 29.3.21 for renewing her policy with continuity
benefits after a period of 47days break in insurance, from the date of expiry of the policy( i.e.
10.2.21). All Mediclaim policies are subject to renewal with continuity of benefits after
condonation of delay for a maximum period of 30days from the date of expiry, provided no
claims during the break period will be entertained.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted. In this complaint where the complainant`s Parivar Mediclaim policy was not
renewed, the arguments put forth by the respondent insurers were:-
1. The complainant approached the respondent insurer for renewing her health policy , after
47 days of the expiry of the policy.
2. The previous policy expired on 10.2.21 and the complainant approached the respondent
insurer for renewing the policy on 29.3.21, i.e. after a gap of 47days.
3. All Mediclaim policies are subject to renewal with continuity of benefits after condonation
of delay for a maximum period of 30days from the date of expiry, provided no claims during
the break period will be entertained. Hence the renewal was denied.
In Consideration of the tenable arguments put forth by the respondent insurer, I do not want
to interfere in the decision of the respondent insurer in denying the renewal of the policy.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
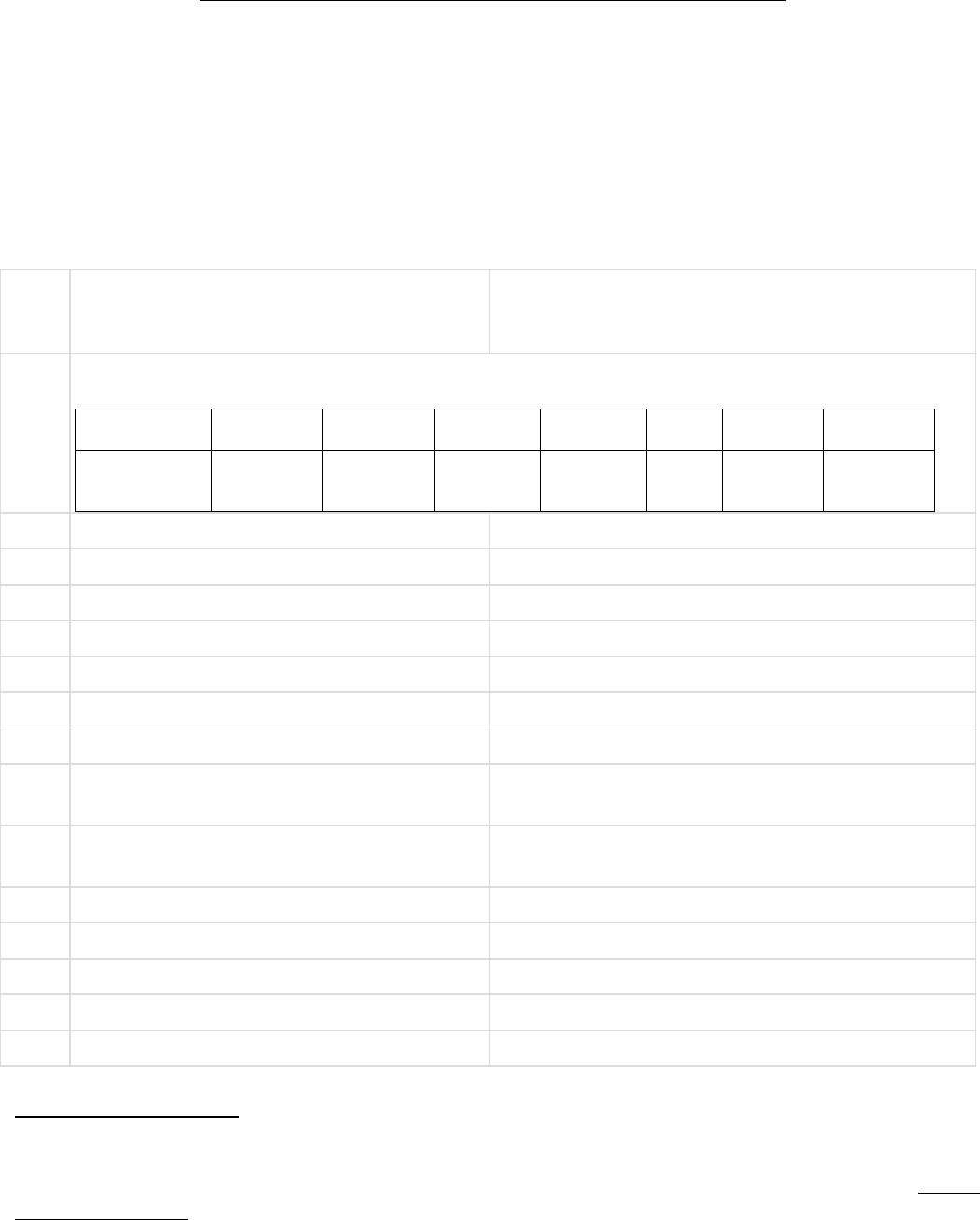
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P. K. RATH
CASE OF COMPLAINANT – Sri Arup Chakra
borty
VS
RESPONDENT: -- Care health Insurance Co. Ltd
COMPLAINANT REF: NO: KOL-H-037-
2122-0272
AWARD NO:
IO/KOL/A/HI/0235/2021-2022
1.
Name &Address OfThe Complainant
Sri Arup Chakra borty
CK_ 12, Sector- 2, Salt city.
Kolkata- 700091, West Bengal.
2.
Type Of Policy: Health
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
30711894
3 lakh
20.03.2021
19.03.2022
03.04.2021
38055
Mediclaim
Annual
3.
Name of insured
Sri Panchanan Chakra borty
4.
Name of the insurer
Care health Insurance Co. Ltd
5.
Date of receipt of the Complaint
24.08.2021
6.
Nature of Complaint
Repudiation of claim
7.
Amount of Claim
1.78 lakh
8.
Date of Partial Settlement
NA
9.
Amount of relief sought
1.78 lakh
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1) (b).
11.
Date of hearing
Place of hearing
27.09.2021
Kolkata
12.
Representation at the hearing
--
a)For the Complainant
Sri Arup Chakraborty
b)For the Insurer
Dr. Nisha Sharma
13.
Complaint how disposed
Through on line hearing.
14.
Date of Award
29.09.2021
Brief Facts of the Case: --
Insured, Late Sri Panchanan Chakraborty initially had a fall 4 days back. He admitted to Divine Nursing
home with a complaint of pain around right hip joint. Diagnosed in Nursing home as Intertrochanteric
Fracture, right femur. Date of admission was 03.04.2021, Date of discharge- 10.04.2021. However, Patient
died on 10.04.2021. Cause is shown as pneumonia type 2 respiratory failures & post operative case of right
fracture.
From treatment progress report it is observed that insured was a known case of COPD for last 5 years & was
under medication. He had pneumonia 3 years back. COPD with medication & HTN were not disclosed while
taking policy.
(Refer treatment sheet).
However, initially claim was rejected on 06.04 2021 by Insurer as per clause 7.1 (waiting period- 30 days).
Later on insurer further informed the insured on 19.07.2021 that the cause of rejection is for non disclosure
of material fact. Here the Complainant is nephew of the Insured who provided an affidavit stating him as
the legal heir of the victim.
Contention of the complainant:-
The Complainant, through on line phone call attended the meeting & urged that whatever the Insurer stated
about past suffering of the Insurer is not correct & with malafied intention. Insured had no past ailment &
even if it stated in medical documents, it is not correct. Hence claim should be considered.
Contention of the Respondent:
The contributory cause of death of the Insured (about 70 yrs old) as reflected in medical report is from
pneumonia Type II & respiratory failure. Treatment sheet reveals that Insured was a COPD patient, had
obstructive airways disease & was on MDI (mechanically ventilated). He had pneumonia 3 years back. But
while taking the said policy, it was not disclosed in proposal form. Concealment of material fact prejudices
the right of recovery of the complainant from the scope of cover as per clause 7.1 of policy terms & condi-
tions.
Observation and conclusions:
1) The statement of the Insurer is supported by medical documents of the concern Hospital where the
patient undertook treatment.
2) No documentary evidences been provided by claimant other than oral denial of the suffering during the
course of hearing.
AWARD
Taking into account the facts & circumstances of the case & the submissions made by both the parties in
hearing, also on going through the submitted documents, it is observed that the decision of the Insurer
towards rejection of claim is based on documents as provided by the Complainant. It is therefore decided
not to entertain the claim as is concluded by Insurance Company. The Complaint is therefore, closed without
any relief to the Complainant & treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the provisions of Insurance
Ombudsman Rule 2017.
SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – Sri Buddhadeb Nandi
VS
RESPONDENT: -- Care Health Insurance Co. Ltd
COMPLAINANT REF: NO: KOL-H-037-
2122-0278
AWARD NO: IO/KOL/A/HI/0236/2021-2022
1.
Name &Address OfThe Complainant
Sri Buddhadeb Nandi
Vill- Chouberia, P.O- Panchra,
P. S Jamalpur, Dist- Burdwan- 713401 West
Bengal.
2.
Type Of Policy: Health
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
17901045
40 lakh
07.08.2020
06.08.2021
04.08.2021
63196/-
Mediclaim
Annual
3.
Name of insured
Sri Buddhadeb Nandi
4.
Name of the insurer
Care Health Insurance Co. Ltd
5.
Date of receipt of the Complaint
02.09.2021
6.
Nature of Complaint
Non refund of premium.
7.
Amount of Claim
74572/- including tax.
8.
Date of Partial Settlement
NA
9.
Amount of relief sought
74572/-
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1) (b).
11.
Date of hearing
Place of hearing
27.09.2021
Kolkata
12.
Representation at the hearing
--
a)For the Complainant
Sri Buddhadev Nandi
b)For the Insurer
Dr Nisha Sharma.
13.
Complaint how disposed
Through on line hearing.
14.
Date of Award
29.09.2021
Brief Facts of the Case: --
This is floater family health policy of Sri Buddhadeb Nandi as against Sum insured of 40 lakh for the policy
period – 07.08.2020 to 06.08.2021. Policy purchased on line. Mediator was through broker M/S Spash IMF
Private Ltd. Premium paid through SBI debit card on 06.08.2020. As there was several mistakes in policy
(proposal not signed by him), rectification endorsement done on 28.01.2021 by the Insurer as per request of the
Insured. Insured had one claim for treatment of Thyroid operation at Bangalore & he submitted all the
documents in original to the Broker. But neither claim settled nor documents refunded by the Broker. So,
assuming the policy, sold as fraudulent by the broker, Complainant requested to Insurer for refund of policy
premium on 04.08.2021 as against cancellation of policy. As cancellation request given just prior two days from
the date of policy expiry no refund given. The alleged claim is for the complaint OF NON REFUND OF
PREMIUM.
Contention of the complainant:-
Basically the Broker is responsible for the mis- selling of the Policy. He submitted all claim documents to the
Broker, not the Insurance Company. But broker is not supporting his in any way. Not returning the claim
documents to him. . So he requested for refund of the premium as he could not avail the benefit of the policy he
had with the present Insurer.
Contention of the Respondent:
Request letter for refund of Premium received just two days before the expiry of the policy. Hence No refund
stands as payable as per policy terms & conditions.
Observation and conclusions:
1) Complainant had communication earlier towards rectification of the Policy in respect of mis spelling in name
& other particulars which had been rectified by Insurer accordingly through endorsement on dated 28.01.2021.
2) Policy refund amount stands as nil beyond 6 months of expiry of policy as per policy provision 7.11(b) of the
stipulated policy.
3) No claim papers been submitted to the Insurer as is revealed from the statements of the Complainants &
from the documents as submitted by him. Insurer also confirmed the same in hearing.
AWARD
Taking into account the facts & circumstances of the case & the submissions made by both the parties in
hearing, also from the submitted documents it is observed that the refundable amount after expiry of ( six)
6 months from the date of inception of policy towards cancellation is Nil as per policy provision. Therefore,
the decision of Insurer towards non refund of premium stands valid as per policy terms & conditions. Ac-
cordingly, following policy provision, the Complaint of the Complainant is closed & disposed of without any
relief to the Complainant.
The attention of the Complainant and the Insurer is hereby invited to the provisions of Insurance Ombudsman
Rule 2017.
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K. RATH
CASE OF COMPLAINANT– SHRI SUBRATA PODDER
VS
RESPONDENT: SBI GENERAL INSURANCE CO. LTD.
COMPLAINT REF: NO: KOL-H-040-2122-0256
AWARD NO: IO/KOL/A/HI/0247/2021-2022
1.
Name &Address OfThe Complainant
Shri Subrata Podder
49/G, Kalpataru Apartment
Sarat Bose Road, Siliguri – 734 001.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
4101200100
000052-01
-
16-01-2020
15-01-2021
3.
Name of insured
Shri Subrata Podder
4.
Name of the insurer
SBI General Insurance Company Limited
5.
Date of receipt of the Complaint
31-Jul-2021
6.
Nature of Complaint
Partial settlement of claim
7.
Amount of Claim
2,03,997.00
8.
Date of Partial Settlement
9.
Amount of relief sought
56,400.00
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claim by the insurer
11.
Date of hearing
Place
of hearing
27-Sep-2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Shri Subrata Podder
b)For the Insurer
Ms. Chynikca Modie
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
30-Sep-2021
Brief Facts of the Case:
The complainant-cum-insured, Shri Subrata Podder is covered under SBI Retiree Health Assist Insurance Policy
issued by SBI General Insurance Company. The insured was admitted in the hospital on 12-04-2021 for
treatment of Covid-19 Pneumonia, Diabetes Mellitus and discharged on 24-04-2021. After discharge from the
hospital, the insured lodged claim for Rs.2,03,997/- for reimbursement of treatment expenses but the Insurance
Company settled the claim for Rs.1,38,293/-. The Insurance Company deducted the balance amount as follows :
Rs.40,800/- - For expenses paid extra to the nursing staff, ward boy, ward lady, housekeeping (male and female)
for their isolation duty;
Rs.8,400/- - Nursing charges and practitioner charges which shall be included in Room Rent (made separate
bill);
Rs.7,200/- - Isolation RMO Charges ( made separate bill)
The Insurance Company has stated in their self-contained note that the insured, Shri Subrata Podder was
admitted in the hospital for the period from 12-04-2021 to 24-04-2021 for treatment of Covid-19 Pneumonia,
Diabetes Mellitus. The total claim was for Rs.2,03,997/- and the Insurance Company settled for Rs.1,38,293/-.
Further, on receipt of Ombudsman complaint, the claim was reviewed and made payment of Rs.8,400/-. The
details of final deductions in reimbursement claim is as follows :
Rs.40,800.00 - Covid Care Charges - The charges contain expenses aid extra to nursing staff, ward boy etc.
for their isolation ward duty, which is not payable;
Rs.8,604.00 - Pharmacy Charges - Non-medical expenses, consumables are not covered in the policy;
Rs.7,200.00 - Doctor Charges - Associated medical expenses shall include Room Rent, Fees of Medical
Practitioner/Surgeon/Anaesthetist/Specialist conducted within the same hospital where the insured patient has
been admitted.
Contention of the complainant:
The complainant has stated in the hearing that the insured lodged claim for Rs.2,03,997/- but the Insurance
Company settled the claim for Rs.1,38,293/-. The Insurance Company deducted an amount of Rs.65,704/-
towards mainly the bill for nursing staff, ward boy for isolation ward duty, RMO/Medical Practioner/Sur-
geon/Anaesthetist/Specialist due to non-inclusion in the Room rent Charges. The Hospital billed separately
for isolation general ward charges @ Rs.2,500/- per day, Nursing Charges @ Rs.700/- per day and isolation
RMO Charges @ Rs.600/- per day though the allowable room rent is Rs.5,000/-.
Contention of the Respondent:
The complainant has stated in the hearing that the insured was admitted in the hospital for treatment of Covid-
19 Pneumonia, Diabetes Mellitus for the period from 12-04-2021 to 24-04-2021. The insured lodged claim for
Rs.2,03,997/- and the Insurance Company settled the claim for Rs.1,38,293/-. As per Policy terms and condi-
tions, the room rent means the amount charged by the Hospital towards room and boarding expenses and
shall include the associatd medical expenses. Associated Medical Expenses shall include room rent, nursing
charges, operation theatre charges fees for Medical Practitioner/Surgeon/Anaesthetist/Specialist. The Hospi-
tal has separately charged RMO fees, Covid Care Charges, Nursing Charges which is not payable as per policy
terms and conditions.
Observation and conclusions:
It is observed that the complainant as well as the representative of the Insurance Company both have attended
the hearing online. The complainant has stated in the hearing what he already stated in his written complaint
submitted to this office. The representative of the Insurance Company has stated in the hearing that the claim
has been settled as per Policy terms and conditions.
It is found from the submitted documents and submissions made by both the parties during the course of
hearing that the insured lodged claim for Rs.2,03,997/- but the Insurance Company settled Rs.1,38,293/- and
later settled for Rs.8,400/-. It is observed that as per policy terms and conditions, the RMO charges, fees for
Medical Practioner, RMO fees, Nursing Charges etc. are payable. The Insurance Company has deducted the
above charges as the Hospital Authority have made the bills separately instead of in the Room Rent Charges.
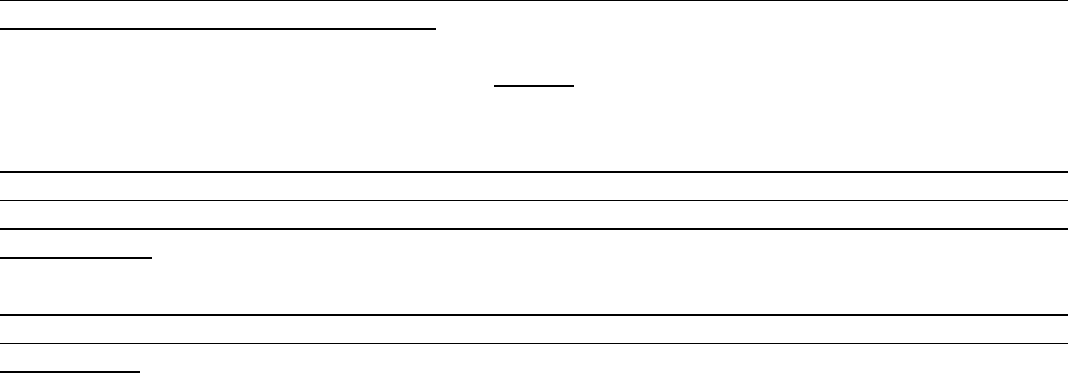
It is also observed that as per policy sum insured, the entitlement of room rent is Rs.5,000/- and the charge for
General Isolation Ward is Rs.2,500/- per day.
AWARD
Taking into account the facts and circumstances of the cases and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the Insurance
Company did not allow the Doctor Charges, Covid Care Charges, RMO Fees as the Hospital Authority has made
Bills separately.
In view of the above and the documents submitted by both the parties, the Insurance Company is directed to
club the room charges and nursing charges and RMO fees to gather as bed charges and pay if any as per room
rent eligibility.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day of 30
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
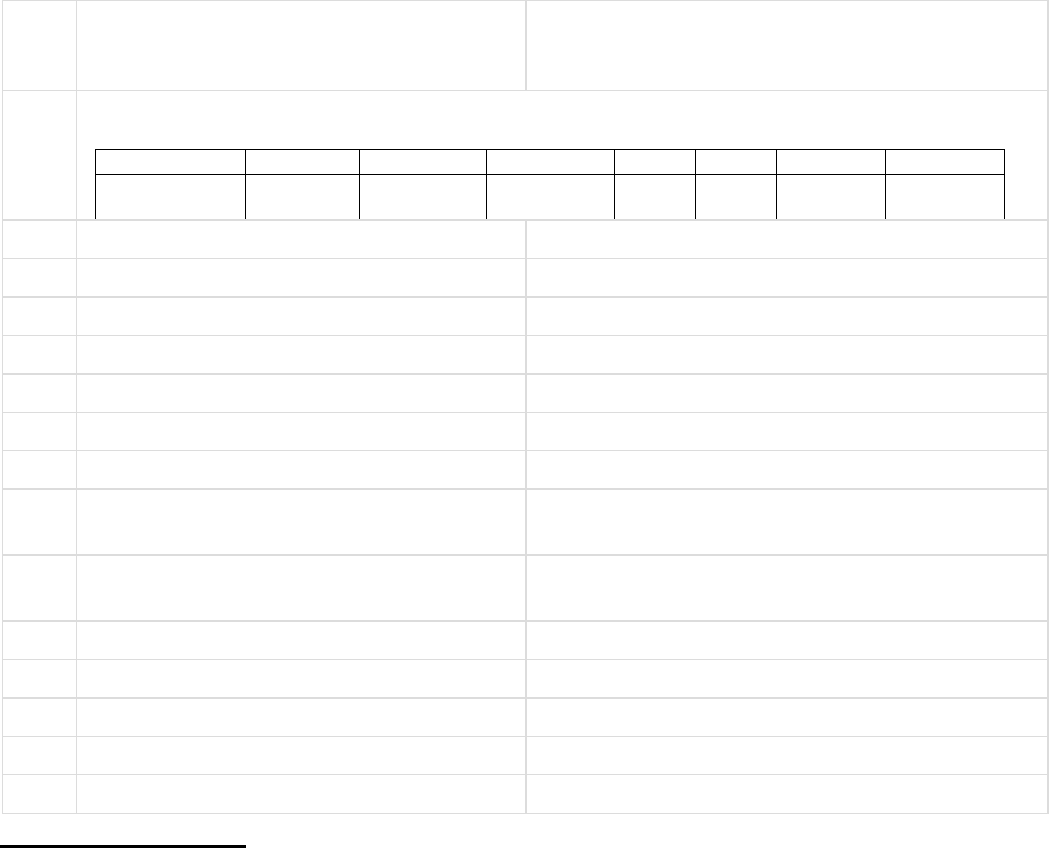
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASEOFCOMPLAINANT– SHRI BHASKAR DEY
VS
RESPONDENT: STAR HEALTH & ALLIED INS. CO. LTD.
COMPLAINT REF: NO: KOL-H-044-2122-0187
AWARD NO:IO/KOL/A/HI/0212/2021-2022
1.
Name &Address OfThe Complainant
Shri Bhaskar De
Vill : Roy Para, P.O : Guptipara
P.S : Balagar, Dist : Hooghly – 712 512.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/191142/01/
2021/003563
300000
19-12-2020
18-12-2021
10059
One year
single
3.
Name of insured
Mrs. Rimpa De
4.
Name of the insurer
Star Health & Allied Insurance Co. Ltd.
5.
Date of receipt of the Complaint
19-Jul-2021
6.
Nature of Complaint
Repudiation of claim
7.
Amount of Claim
87,000.00
8.
Date of Partial Settlement
9.
Amount of relief sought
87,000.00
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claims by the insurer
11.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Shri Bhaskar De
b)For the Insurer
Ms. Sudeshna Bhattacharjee
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
13-Sep-2021
Brief Facts of the Case :
The complainant-cum-insured has stated in his written complaint that the insured ported his 10 years old
Mediclaim Policy from New India Assurance Company to Star Health & Allied Insurance Company on 19-12-
2020 covering himself and his wife, Mrs. Rimpa De. His wife, Mrs Rimpa De was admitted in the hospital on
17-06-2021 with a complaint of back pain and discharged on 22-06-2021. The final diagnosis was Acute Low
Back Pain. During the hospitalization period, the Insurance Company disallowed the cashless facility for non-
disclosure of previous medical history i.e. Polycystic Kidney since 2014.
Mrs. Rimpa De had Polycystic Kidneys since 2014 and no medicine was prescribed for the same. She did not
require any treatment except specific diet. The treating doctor of the hospital has issued a certificate stating that
there is no relation with the Policystic Kidney and there was no renal dysfunction associated with her clinical
presentation. The Insurance Company has repudiated the claim and terminated the policy. Being aggrieved, the
insured lodged complaint to this office for redressal his grievances.
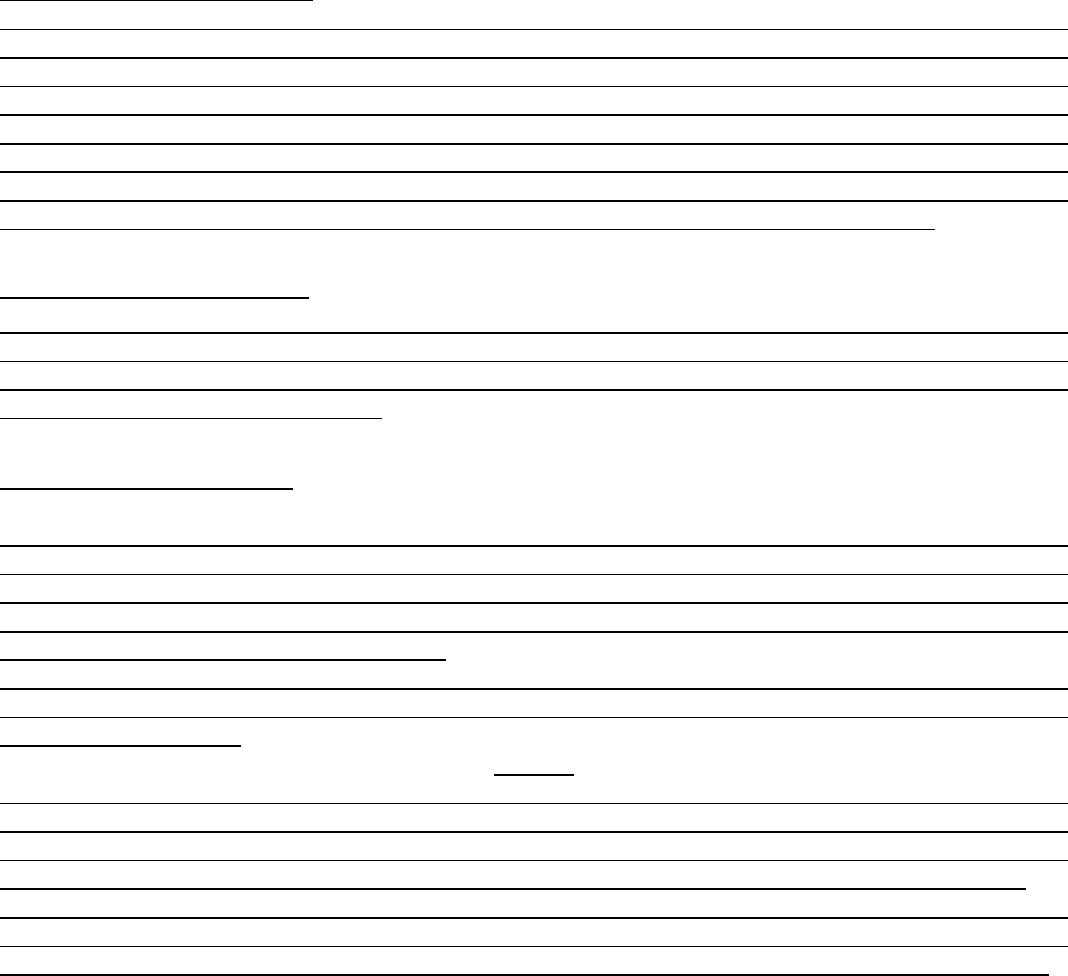
The Insurance Company has stated in their self-contained note that the insured ported the policy from New India
Assurance Company on 19-12-2020. The insured was admitted in the hospital for treatment of Urinary
Retention/Lower Back Pain and the Insurance Company disallowed cashless facility for previous treatment
records for Polycystic Kidney disease.
The Insurance Company repudiated the reimbursement claim as the patient was suffering from Polycystic
Kidney diseases since 2014 and the same was not disclosed at the time of porting the policy.
Contention of the complainant:
The complainant-cum-insured has stated in the hearing that the insured ported his 10 years old policy fro New
India Assurance Company to Star Health & Allied Insurance Company in the year 2020 and Mrs. Rimpa De was
admitted in the hospital on 17-06-2021 with a complaint of acute low back pain. The Insurance Company did
not allow the cashless facility during the hospitalization period. The insured lodged claim for reimbursement
of treatment expenses but the Insurance Company repudiated the claim and cancelled the policy showing the
reason for non-disclosure of previous disease i.e. Polycystic Kidney. The doctor did not prescribe medicines for
the said disease except specific diet. The present treating doctor has also issued a certificate stating that the
sequence of events is not related to Polycystic Kidneys which she has been having for long time.
Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured is suffering from Pol-
ycystic Kidney since 2014 but the same is not disclosed in the proposal form and other portability form at the
time of porting the policy. Hence, the claim is repudiated as per policy terms and conditions. The notice for
cancellation of the policy is also issued.
Observation and conclusions:
It is observed that the complainant has attended the hearing physically at this office premises whereas the
representative of the Insurance Company has attended the hearing online. The complainant has stated in the
hearing what he already stated in his written complaint submitted to this office. The representative of the
Insurance Company has stated in the hearing that the claim has been repudiated due to non-disclosure of the
material fact at the time of porting the policy.
It is found from the submitted documents as well as submissions made by both the parties during the course
of hearing that the insured was diagnosed Polycystic Kidneys in 2014 and the same was not disclosed at the
time of porting of policy.
AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is found that the insured patient is
suffering Polycystic Kidneys disease and the same is not disclosed at the time of porting the policy. Hence, the
Insurance Company has cancelled the policy and repudiated the claim as per policy terms and conditions.
In view of the above, the decision of repudiation and cancellation of the policy made by the Insurance Company
is correct and justified. As such, the Insurance Company is not liable to make any payment towards reimburse-
ment of claim to the complainant. Hence, the complaint is dismissed without any relief to the complainant.
If the decision is not acceptable to the complainant to the complaint, she/he is at liberty to approach any
other Forum/Court as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on Day of 13
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
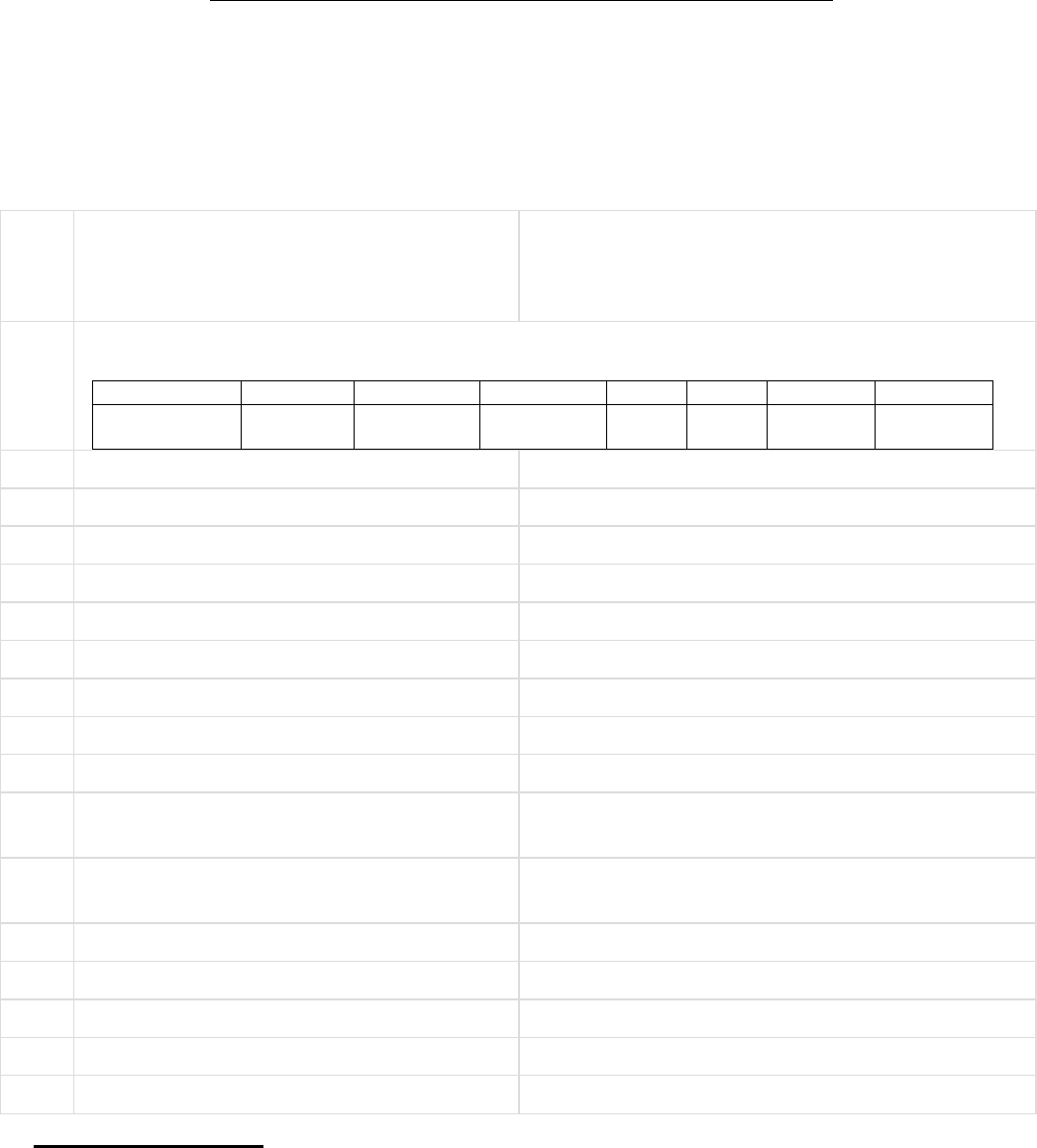
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K. RATH
CASEOFCOMPLAINANT– SHRI BHIMSEN AGARWALA
VS
RESPONDENT: STAR HEALTH & ALLIED INS. CO. LTD.
COMPLAINT REF: NO: KOL-H-044-2122-0200
AWARD NO:IO/KOL/A/HI/0215/2021-2022
1.
Name &Address OfThe Complainant
Shri Bhimsen Agarwala
Manorama Building, 4
th
floor
P-495, Dumdum Park
Kolkata – 700 055.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/191113/01/
2020/006899
1000000
10-12-2019
09-12-2020
28019
One year
single
3.
Name of insured
Shri Bhimsen Agarwala
4.
Name of the insurer
Star Health & Allied Insurance Company Limited
5.
Date of Repudiation
6.
Reason for Repudiation
7.
Date of receipt of the Complaint
20-Jul-2021
8.
Nature of Complaint
Partial settlement of claim
9.
Amount of Claim
3,14,820.00
10.
Date of Partial Settlement
11.
Amount of relief sought
1,38,109.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
the claim by the insurer
13.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Shri Bhimsen Agarwala
b)For the Insurer
Ms. Sudeshna Bhattacharjee
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
13-Sep-2021
17. Brief Facts of the Case:
The complainant-cum-insured has stated in his complaint that the insured had taken a Family Health Optima
Policy from Star Health & Allied Insurance Co. Ltd. with sum insured of Rs.10,00,000.00. The insured was
admitted in the hospital on 09-08-2020 for treatment of Covid-19 positive, T2 DM, Dyslipidemia and
discharged on 18-08-2020. The insured lodged claim for Rs.3,14,820.00 for reimbursement of treatment
expenses but the Insurance Company settled the claim for Rs.1,76,711.00. Being aggrieved, the insured lodged
complaint to this office for redressal of his grievances.
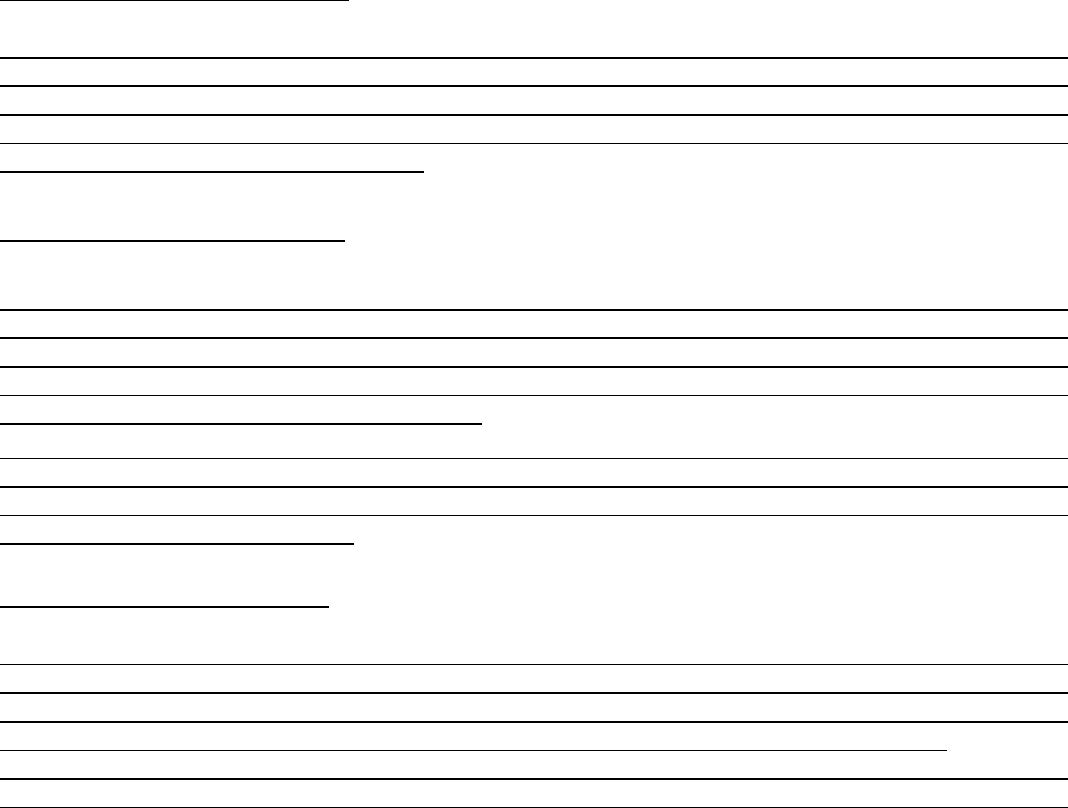
The Insurance Company has stated in their self-contained note that the insured submitted a request for
reimbursement of treatment expenses of Rs.3,14,820.00 but the Insurance Company settled the claim for
Rs.1,69,741.00.
The insured was admitted in the hospital on 05-08-2020 for treatment Covid and discharged on 08-08-2020.
During the hospitalization period, the insured availed cashless facility. On 08-08-2020, the insured was issued
a Transfer Certificate mentioning that the insured is being transferred to higher centre where Covid facility is
available.
During the hospitalization period from 05-08-2020 to 08-08-2020, the Isolation Single Cabin Charge was
Rs.5,500.00 but in reimbursement claim, it was charged for Rs.12,000.00. The Insurance Company settled the
same for Rs.10,000/- per day as standard rate of Single Standard A.C. Room.
The Hospital Authority charged for Oxygen for Rs.2,500/- every day but in ICP, all the SpO2 noted are in room
air does not follow below 94%. The amount of oxygen advised or administered is no where recorded in ICP
but Oxygen is charged in Final Bill.
The Hospital Authority charged Rs.84,986/- as Equipment Hire Charges for Pulse Oxymeter (which is not
payable) but there is no charge for Pulse Oxymeter in the previous cashless claim.
The Physiotherapy and dietician charges for Rs.9,000/- and Rs.300/- for documentation charges are not payable.
18. Contention of the complainant:
The complainant-cum-insured, Shri Bhimsen Agarwala has stated in the hearing that the insured was admitted
in the hospital for treatment of Covid positive and after discharge from the hospital, the insured lodged claim
for Rs.3,14,820/- for reimbursement of treatment expenses. But the Insurance Company has settled the claim
for Rs.1,76,711/- after deduction of Rs.1,38,109/-. Inspite of several request, the Insurance Company did not
settle the balance claimed amount till date.
19. Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured patient was admitted
in the hospital twice and in first hospitalization, the insured has availed cashless facility whereas the second
claim was for reimbursement claim. On 08-08-2020, the insured was issued a Transfer Certificate mentioning
that the insured is being transferred to higher centre where Covid facility is available but the insured patient
has readmitted in the same hospital on next day.
In first claim, the bed charge was Rs.5,500/- per day for Isolation Single Cabin whereas in second claim, the
same was for Rs.12,000/- per day and the Insurance Company has settled for Rs.10,000/- per day considering
the gravity of the case. The Hospital Authority has charged Equipment Hire charge, Physiotherapy and Dieti-
cian charges, which are not payable.
20. Observation and conclusions:
It is observed that the complainant has attended the hearing physically at this office premises whereas the
representative of the Insurance Company has attended the hearing online. The complainant has stated what
he already stated in his written complaint submitted to this office. The representative of the Insurance Com-
pany has stated in the hearing that the claim has been settled as per policy terms and conditions.
It is observed from the submitted documents as well as submissions made by both the parties during the course
of hearing that the Insurance Company has allowed Rs.10,000/- towards room rent instead of Rs.12,000/- per
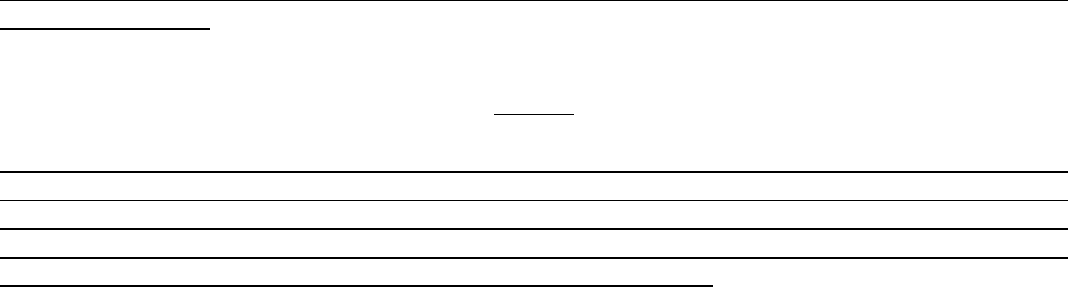
day. The Insurance Company could not provide any documentary evidence for justification but all other de-
ductions are in order.
AWARD
Taking into account the facts and circumstances of the cases and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the Insurance
Company has deducted the room rent Rs.2000/- and could not provide the proper reason for the same. The
other deductions are in order. Hence, the Insurance Company is directed to make payment the deducted
amount in respect of room rent. The complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day of 13
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
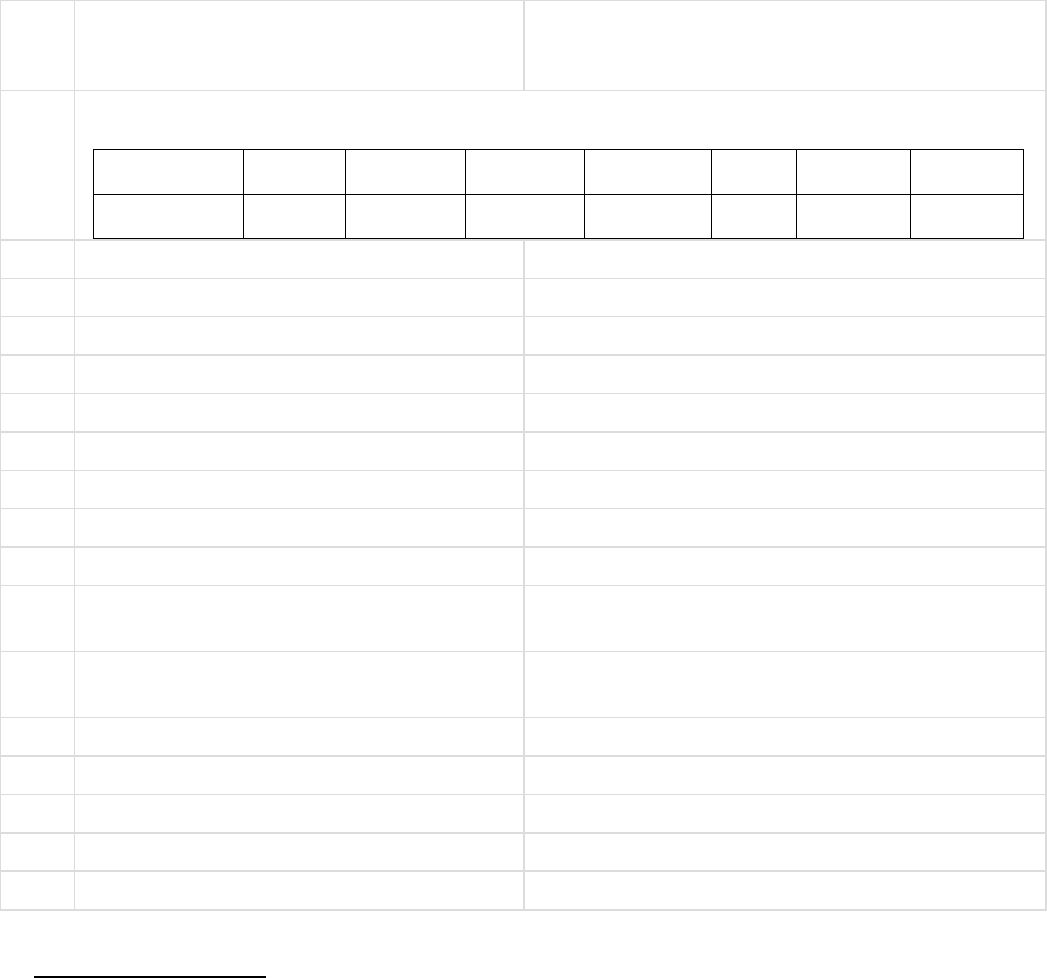
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT– SHRI ASOK KR CHAKRABORTI
VS
RESPONDENT: STAR HEALTH & ALLIED INSURANCE CO.
COMPLAINT REF: NO: KOL-H-044-2122-0217
AWARD NO:IO/KOL/A/HI/0231/2021-2022
1.
Name & Address Of the Complainant
Shri Asok Kumar Chakraborti
9B/2A, Gobindapur Road
Lake Gardens, Kolkata-700 045.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/191116/01/
2020/003320
1000000
02-07-2020
01-07-2021
02-07-2016
53100
One year
single
3.
Name of insured
Mrs. Manasi Chakraborty
4.
Name of the insurer
Star Health & Allied Insurance Co. Ltd.
5.
Date of Repudiation
6.
Reason for Repudiation
7.
Date of receipt of the Complaint
22-Jul-2021
8.
Nature of Complaint
Partial settlement of claim
9.
Amount of Claim
6,80,387.00
10.
Date of Partial Settlement
3,12,403.00
11.
Amount of relief sought
3,67,984.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claim by the insurer
13.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Shri Ashok Kumar Chakraborti
b)For the Insurer
Ms. Sudeshna Bhattacharjee
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
16-Sep-2021
17. Brief Facts of the Case:
The complainant has stated in the complaint that the insured, Mrs. Manasi Chakraborty was admitted in Cure
Centre Nursing Home on 18-09-2020 and expired on 08-10-2020. The cause of death was sudden Cardiac Arrest
and Respiratory failure. The complainant lodged claim for Rs.6,80,387.00 for reimbursement of treatment
expenses incurred during the hospitalization period and pre and post- hospitalization period but the Insurance
Company settled the claim for Rs.3,12,403.00. Being aggrieved, the complainant lodged complaint to this office
for redressal of his grievances.
The Insurance Company has stated in their self-contained note that the insured was admitted in the hospital
for the period from 18-09-2020 to 08-10-2020 for treatment of Subdural Hematoma, Alzeimers disease, HTN.
The insured lodged claim for Rs.6,80,574/- earlier it was Rs.6,25,086/-. The Insurance Company settled the
claim for Rs.3,12,603/-. The Insurance Company reviewed the claim and came to a conclusion to further offer
an amount of Rs.43,042/- towards full and final settlement of the claim. The details of deductions are as follows :
Rs.11,000.00 - Room Rent - excess as per policy terms and conditions;
Rs.300.00 - Delivery Charges - not payable;
Rs.4,600.00 - Glucometer & Blood grouping charges not payable;
Rs.20,280.00 - Non-medical items - not payable;
Rs.1,33,759.00 - Medicines - Gloves, Mask, Urobag, Cap, Apron, Molisheet, Hand Care, Gown, Molicare,
Micropore, 3 Way, Tegaderm, Stocking, Electrodes, Cotton, Johnson Power, Thermometer, AB Gel, Betadine,
Easyfix etc. - non payable;
18. Contention of the complainant:
The complainant-cum-insured has stated in the hearing that the insured Mrs. Manasi Chakraborty was admit-
ted in Cure Centre Nursing Home on 18-09-2020 and expired on 08-10-2020. The cause of death was sudden
Cardiac Arrest and Respiratory failure. The insured lodged the total claim for Rs.6,80,574/- alongwith all the
required documents but the Insurance Company settled the claim for Rs.3,12,403/-.
19. Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured was admitted in the
hospital on 18-09-2020 and expired on 08-10-2020. After discharge from the hospital, the insured lodged claim
for Rs.6,80,574/- earlier it was Rs.6,25,086/-. The Insurance Company settled the claim for Rs.3,12,603/-. On
receipt of the Ombudsman complaint, the Insurance Company reviewed the claim and decided to offer to pay
Rs.43,042/- further towards full and final settlement of the claim. The Insurance Company settled the claim as
per policy terms and conditions.
20. Observation and conclusions:
It is observed that the complainant has attended the hearing physically at this office premises whereas the
representative of the Insurance Company has attended the hearing online. The complainant has stated in the
hearing what he already stated in his written complaint submitted to this office. The representative of the
Insurance Company has stated in the hearing that the claim has been settled as per policy terms and conditions.
It is observed from the submitted documents as well as submissions made by both the parties during the course
of hearing that the deductions made by the Insurance Company is as per policy terms and conditions.
AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the Insurance
Company has reviewed the claim and came to a conclusion to further pay an amount of Rs.43,042/-. It is also
found from the submitted documents that the deductions made by the Insurance Company is in order. As
such, the Insurance Company is not liable to make any payment further except Rs.43,042/-. The Insurance
Company is directed to settle the amount of Rs.43,042/- towards full and final settlement of the claim. Hence,
the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day of 16
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
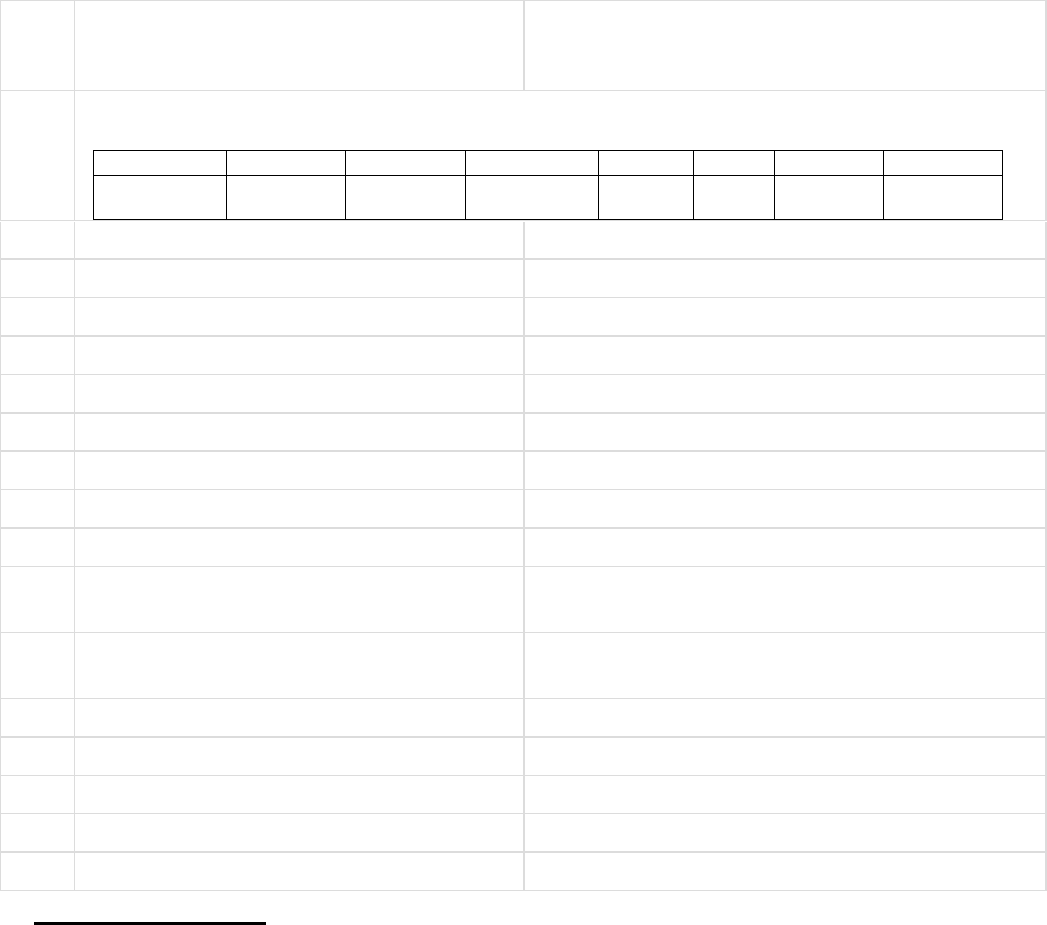
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT– SHRI BIJAY KUMAR AGARWAL
VS
RESPONDENT: STAR HEALTH & ALLIED INS. CO. LTD.
COMPLAINT REF: NO: KOL-H-044-2122-0220
AWARD NO:IO/KOL/A/H/0211/2021-2022
1.
Name &Address OfThe Complainant
Shri Bijay Kumar Agarwal
47/1, B. T. Road, Belghoria
Kolkata – 700 056.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/111101/22
1/11254
500000
10-11-2020
10-10-2021
20077
One year
single
3.
Name of insured
Shri Bijay Kumar Agarwal
4.
Name of the insurer
Star Health & Allied Insurance Company Limitd
5.
Date of Repudiation
6.
Reason for Repudiation
7.
Date of receipt of the Complaint
20-Jul-2021
8.
Nature of Complaint
Partial settlement of claim
9.
Amount of Claim
1,49,805.00
10.
Date of Partial Settlement
11.
Amount of relief sought
42,512.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claim by the insurer
13.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Shri Wansh Agarwal, son of the complainant
b)For the Insurer
Ms. Sudeshna Bhattacharjee
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
13-Sep-2021
17. Brief Facts of the Case:
The complainant-cum-insured has stated in his written complaint that the insured was diagnosed with Covid-19
positive and as per advice of treating doctor, the insured was admitted in the hospital on 31-03-2021 for treatment
of Covid-19 positive and discharged on 06-04-2021. During the hospitalization period, the Insurance Company
approved an amount of Rs.1,07,293.00 as cashless claim. The Insurance Company did not settle the balance
amount of Rs.33,203.00 inspite of several request and reminders.
The Insurance Company has stated in their self-contained note that the insured has availed cashless facility for
Rs.1,07,293/-. On receipt of the complaint from the Office of the Insurance Ombudsman, the Insurance
Company has decided to reconsider the complaint on the merit of the claim. The Insurance Company has decided
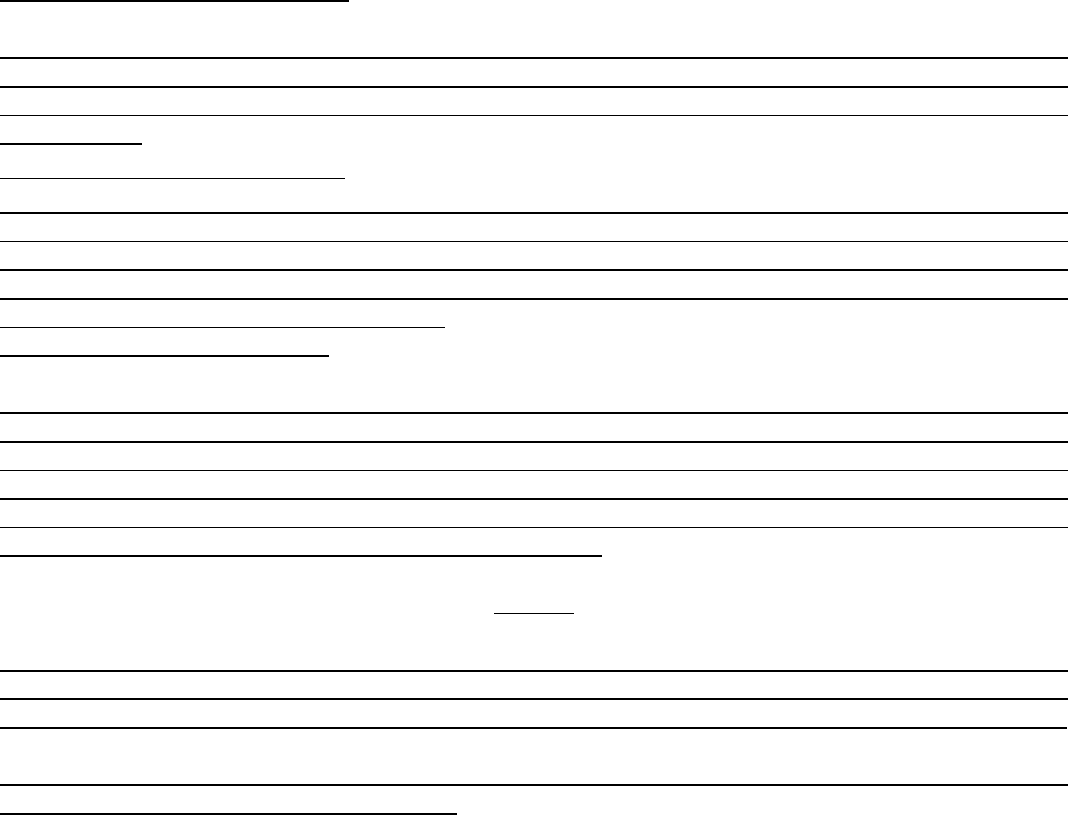
to further remove the restriction on the stay of last two days which was previously disallowed and also reconsider
the usage of Fabiflu. As such, the Insurance Company has decided to pay Rs.17,472/- towards full and final
settlement of the claim.
18. Contention of the complainant:
The complainant has stated in the hearing that the insured was admitted in the hospital for treatment of Covid
and availed cashless facility for Rs.1,07,293/- during hospitalization. The total bill amount was for
Rs.1,49,805/-. In final authorized amount, 2 days stay was restricted along with Fabiflu and other medicines
were not paid.
19. Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the total claimed amount was
Rs.1,49,805/- and approved cashless facility for Rs.1,07,293/-. On receipt of the complaint from the Insurance
Ombudsman Office, the Insurance Company has considered the two days stay in the hospital which was pre-
viously deducted and also reconsidered the usage of Fabiflu. Henceforth, the admissible amount is Rs.17,472/-
towards full and final settlement of the claim.
20. Observation and conclusions:
It is observed that the complainant could not attend the hearing due to poor health. Hence, Shri Wansh
Agarwal has attended the hearing online on behalf of the complainant. The representative of the Insurance
Company has also attended the hearing online. Shri Wansh Agarwal has stated in the hearing what already
stated in the written complaint submitted to this office. The representative of the Insurance Company has
stated in the hearing that the Insurance Company has considered the complaint and decided to settle the claim
for Rs.17,472/- towards full and final settlement of the claim.
AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the Insurance
Company has decided to make payment further for Rs.17,472/- towards full and final settlement of the claim.
In view of the above, the Insurance Company is directed to make payment of Rs.17,472/- to the complainant.
Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day 13
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT– MRS. DOLLY DABRIWAL
VS
RESPONDENT: STAR HEALTH & ALLIED INS. CO. LTD.
COMPLAINT REF: NO: KOL-H-044-2122-0221
AWARD NO:IO/KOL/A/HI/0216/2021-2022
1.
Name &Address OfThe Complainant
Mrs. Dolly Dabriwal
10, Middleton Row
Kolkata - 700 001.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/190000/01/
2021/018875
1500000
05-03-2021
04-03-2022
34916
One year
single
3.
Name of insured
Shri Dhruv Dabriwal
4.
Name of the insurer
Star Health & Allied Insurance Co. Ltd.
5.
Date of Repudiation
6.
Reason for Repudiation
7.
Date of receipt of the Complaint
20-Jul-2021
8.
Nature of Complaint
Partial settlement of claim
9.
Amount of Claim
28,567.00
10.
Date of Partial Settlement
11.
Amount of relief sought
13,567.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total claim repudia-
tion by the insurer
13.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
ABSENT
b)For the Insurer
Ms. Sudeshna Bhattacharjee
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
13-Sep-2021
17. Brief Facts of the Case:
The complainant, Mrs. Dolly Dabriwal has stated in her complaint that the insured, Shri Dhruv Dabriwal is
covered under Star Comprehensive Insurance Policy and in the first week of April, 2021, the insured was
diagnosed with Covid-19 positive. Therefore, the doctor suggested to get him admitted in the hospital so that
necessary care can be taken and proper treatment can be given to him.
Unfortunately, on contacting various hospitals in and around Kolkata, no beds are available in any
hospital/nursing home. Left with no other alternate, the insured patient forced to start treatment at residence in
consultation of doctor. The complainant lodged claim for Rs.28,567.00 to the Insurance Company for
reimbursement of treatment expenses but the Insurance Company settled the claim for Rs.15,000.00 without
arising any reason.
The Insurance Company has stated in their self-contained note that the insured submitted a request for
reimbursement for the expenses borne in Home Quarantine vide Claim Form dated 04-05-2021.
The insured submitted total bill amount to Rs.28,567.00 for reimbursement to which the Insurer settled an
amount of Rs.15,000.00 as per Internal Operative Guidelines extending maximum support towards the
customers at the time of Pandemic.
The Insurance Company has also stated that considering this Pandemic period, the top management of the
Company has issued some Internal Guidelines to consider certain amount based on the Policy sum insured for
treatment of Covid under Home Quarantine to promote treatment at the time of distress in the country and also
to support the people monetarily.
The above benefit is Ex-Gratia and nowhere in the Policy terms and conditions, the above coverage is
mentioned, still considering the period of distress the Insurer has came up with the offer to benefit the
Customer/Insured persons at large at the time of the Pandemic.
Contention of the complainant:
The complainant has confirmed over phone that she is not in a position to attend the hearing.
Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured patient was treated
under doctors at his residence and lodged claim for Rs.28,567/- for reimbursement of treatment expenses.
The Insurance Company has paid an amount of Rs.15,000/- as per Internal Operative Guidelines to consider
certain amount based on policy sum insured for treatment of Covid under Home Quarantine to promote treat-
ment at the time of distress in the country and also support the people monetarily. The above benefit is ex-
gratia and there is no mention in the policy terms and conditions
Observation and conclusions:
It is observed that the complainant could not attend the hearing whereas the representative of the Insurance
Company has attended the hearing online. The representative of the Insurance Company has stated what they
already stated in their self-contained note submitted to this office.
It is found from the submitted documents as well as the submissions made by the representative of the Insur-
ance Company that the Insurance Company has paid an amount of Rs.15,000/- which is an Ex-gratia based on
policy sum insured and not as per policy terms and conditions only to promote treatment as Home Quarantine
at the time of distress in the country and also support the people monetarily.
AWARD
Taking into account the facts and circumstances of the cases and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the insured has
lodged claim for the expenses incurred in Home Quarantine. The Insurance Company has paid an amount of
Rs.15,000/- as per Internal Operative Guidelines to consider certain amount based on policy sum insured for
treatment of Covid under Home Quarantine to promote treatment at the time of distress in the country and
also support the people monetarily. The above benefit is ex-gratia and there is no mention in the policy terms
and conditions. Hence, the Insurance Company is not liable to make any payment further. The complaint is
dismissed without any relief to the complainant.
If the decision is not acceptable to the complainant, She/He is at liberty to apaproach any other Forum/Court
as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on Day of 13
th
Sept, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
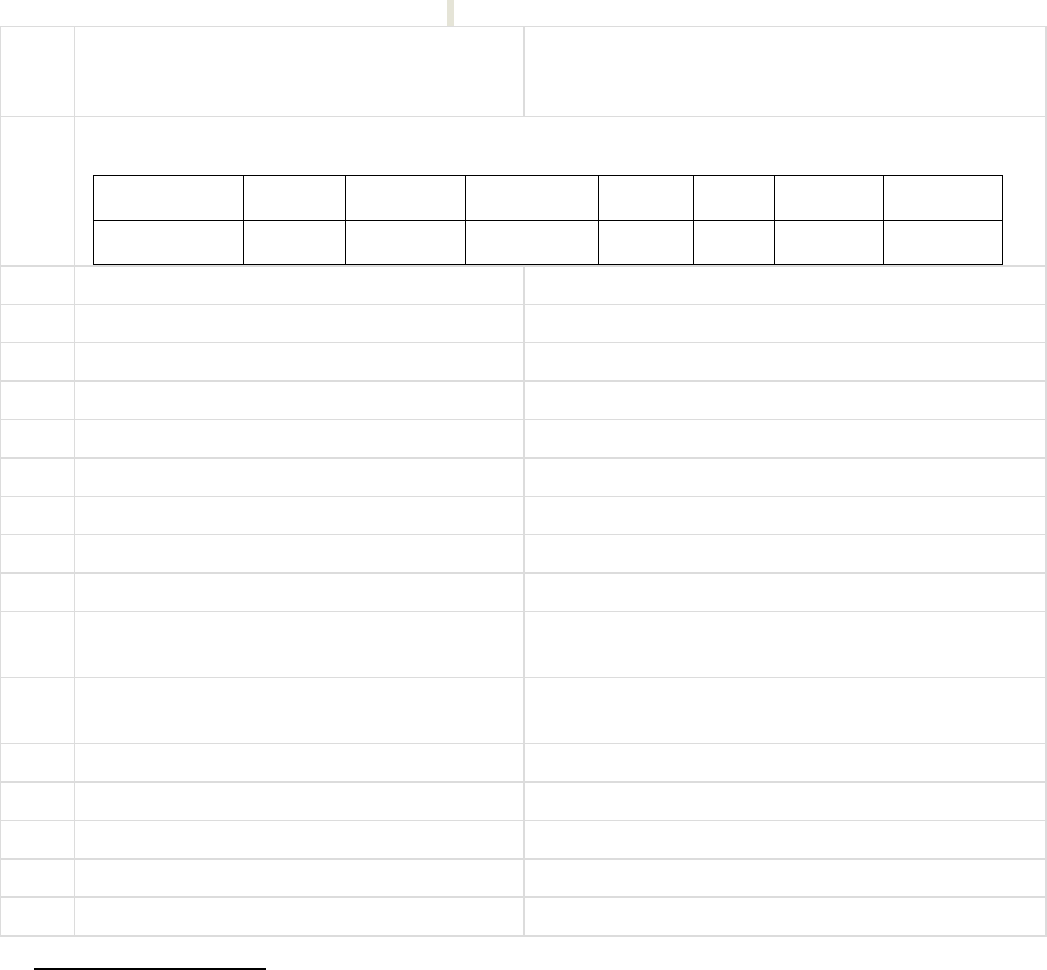
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name:P.K.RATH
CASE OF COMPLAINANT– SHRI SUDIPTO CHAUDHURI
VS
RESPONDENT: STAR HEALTH & ALLIED INS. CO. LTD.
COMPLAINT REF: NO: KOL-H-044-2122-0225
AWARD NO: IO/KOL/A/HI/0248/2021-2022
1.
Name &Address OfThe Complainant
Shri Sudipto Chaudhuri
HB-230, Salt Lake, Sector-3
Bidhannagar, Kolkata – 700 106.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/191111/01/
2020/013415
500000
12-12-2020
11-12-2021
13057
One year
single
3.
Name of insured
Shri Sudipto Chaudhuri
4.
Name of the insurer
Star Health & Allied Insurance Co. Ltd.
5.
Date of Repudiation
6.
Reason for Repudiation
7.
Date of receipt of the Complaint
29-Jul-2021
8.
Nature of Complaint
Partial settlement of Claim
9.
Amount of Claim
42,385.00
10.
Date of Partial Settlement
11.
Amount of relief sought
42,385.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claim by the insurer
13.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Shri Sudipto Chaudhuri
b)For the Insurer
Ms. Sudeshna Bhattacharjee
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
30-Sep-2021
17. Brief Facts of the Case:
The complainant-cum-insured has stated in his written complaint that the insured is covered under Family
Health Optima Insurance Plan with Star Health & Allied Insurance Company Limited. The insured was admitted
in the hospital on 12-01-2021 for treatment of severe compound fracture in right hand resulting from sudden
fall from staircase and discharged on 17-01-2021. The Insurance Company settled the pre-hospitalisation and
hospitalization claim. But the Insurance Company did not settle the post-hospitalisation claim amounting to
Rs.42,385.00. The post-hospitalisation claim documents were submitted to the Insurance Company only after
five days of expiry of 90 days from the date of discharge (date of submission of post-hospitalisation claim is 22-
04-2021)..
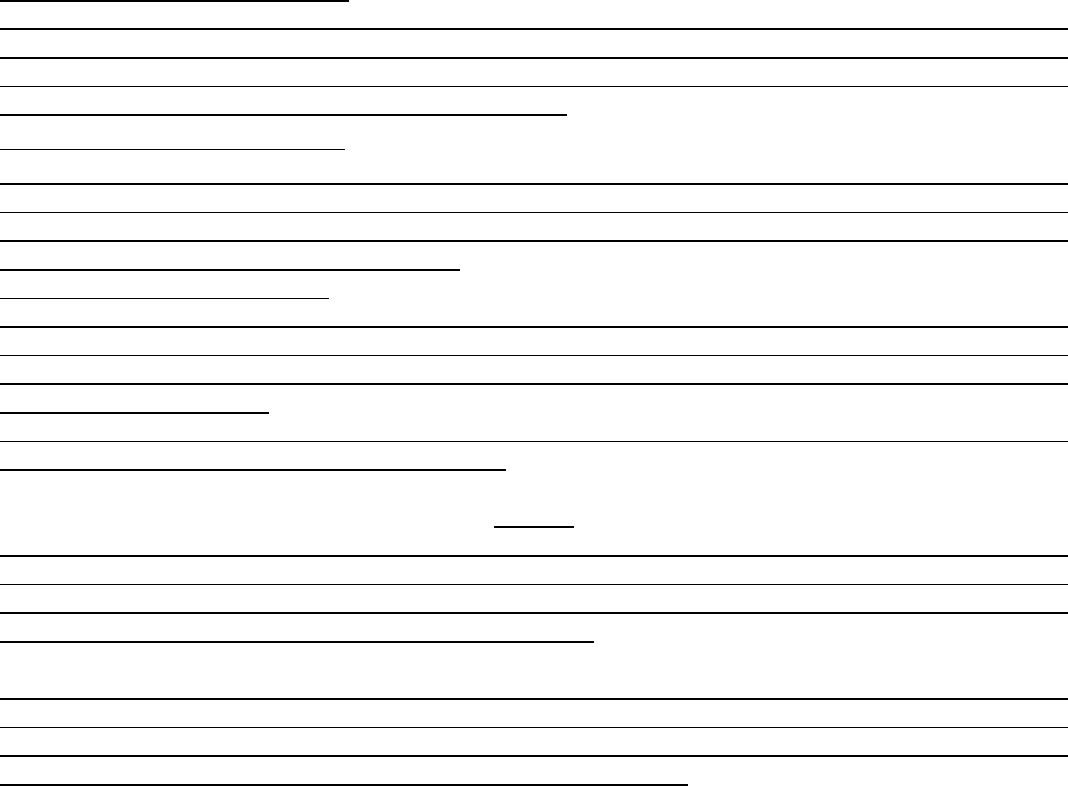
The Insurance Company did not submit the self-contained note that the insured was admitted in the hospital for
treatment of Intra Articular Fracture Distal Radius for the period from 12-01-2021 to 17-01-2021. The insured
availed cashless facility for Rs.2,89,158/- during the hospitalization period. Further the Insurance Company has
paid claim totaling an amount of Rs.32,284/-. The Insurance Company has further offered to pay Rs.28,800/-
which was deducted towards physiotherapy charges in post-hospitalisation claim.
18. Contention of the complainant:
The complainant-cum-insured has stated in the hearing that the Insurance Company did not settle the post
hospitalization claim. The Insurance Company has stated that the maximum claim amount already settled.
The claim documents were submitted to the Insurance Company only after five days of expiry of 90 days from
the date of discharge but there is a grace period of 7 days.
19. Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured availed cashless facil-
ity for Rs.2,89,158/-. The Insurance Company already settled claim totaling an amount of Rs.3,18,758/-. Fur-
ther, the Insurance Company has offered to pay an amount of Rs.28,800/- which was deducted towards phys-
iotherapy charges in post-hospitalisation claim.
20. Observation and conclusions:
It is observed that the complainant and the representative of the Insurance Company both have attended the
hearing online. The complainant has stated in the hearing what he already stated in his complaint submitted
to this office. The representative of the Insurance Company has stated that the claim has been settled as per
policy terms and conditions
It is observed that the Insurance Company has further offered to pay an amount of Rs.28,800/- deducted from
physiotherapy charges in post-hospitalisation claim.
AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the Insurance
Company already settled the claim for Rs.3,18,758/-. Further, the Insurance Company has also offered to pay
an amount of Rs.28,800/- against the physiotherapy charges.
It is found from the submitted documents as well as submissions made by both the parties during the course
of hearing that the decision of settlement of claim made by the Insurance Company is in order. Therefore, the
Insurance Company is directed to pay the amount of Rs.28,800/- further to the complainant within the stipu-
lated time as specified below. The complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day of 30
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN

PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name:P.K.RATH
CASE OF COMPLAINANT– MS. SHARMISTHA KAR
VS
RESPONDENT: NATIONAL INSURANCE COMPANY LTD.
COMPLAINT REF: NO: KOL-H-048-2122-0305
AWARD NO: IO/KOL/A/HI/0250/2021-2022
1.
Name &Address OfThe Complainant
Ms. Sharmistha Kar
Bima Abasan, Flat-E1/3
594/1, Dakshindari Road
Kolkata - 700 048.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum As-
sured
From
Date
To Date
DOC
Premium
Policy
Term
Paying
Term
101900502010001775
600000
21-06-
2020
20-06-2021
28147
One
year
One time
3.
Name of insured
Ms. Sharmistha Kar
4.
Name of the insurer
National Insurance Company Limited
5.
Date of receipt of the Complaint
21-Aug-2021
6.
Nature of Complaint
7.
Amount of Claim
2,30,000.00
8.
Date of Partial Settlement
9.
Amount of relief sought
1,03,716.00
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claim by the insurer
11.
Date of hearing
Place
of hearing
27-Sep-2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Shri Manas Kar, husband of the complainant
b)For the Insurer
Shri Samir Saha
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
30-Sep-2021
Brief Facts of the Case:
The complainant-cum-insured has stated in her complaint that the insured is covered under National Parivar
Mediclaim Policy with National Insurance Company. As per treating doctor’s advice, the insured was admitted
in the hospital on 02-03-2021 with a complaint of bleeding PV and discharged on 06-03-2021. The final
diagnosis was P1+1 with abnormal uterine bleeding. The insured was admitted in a Non-PPN Hospital. After
discharge from the hospital, the insured lodged claim for Rs.2,30,000/- for reimbursement of treatment expenses
but the Insurance Company settled the claim for Rs.1,26,000/-. Being aggrieved, the insured has lodged
complaint to this office for redressal of her grievances.
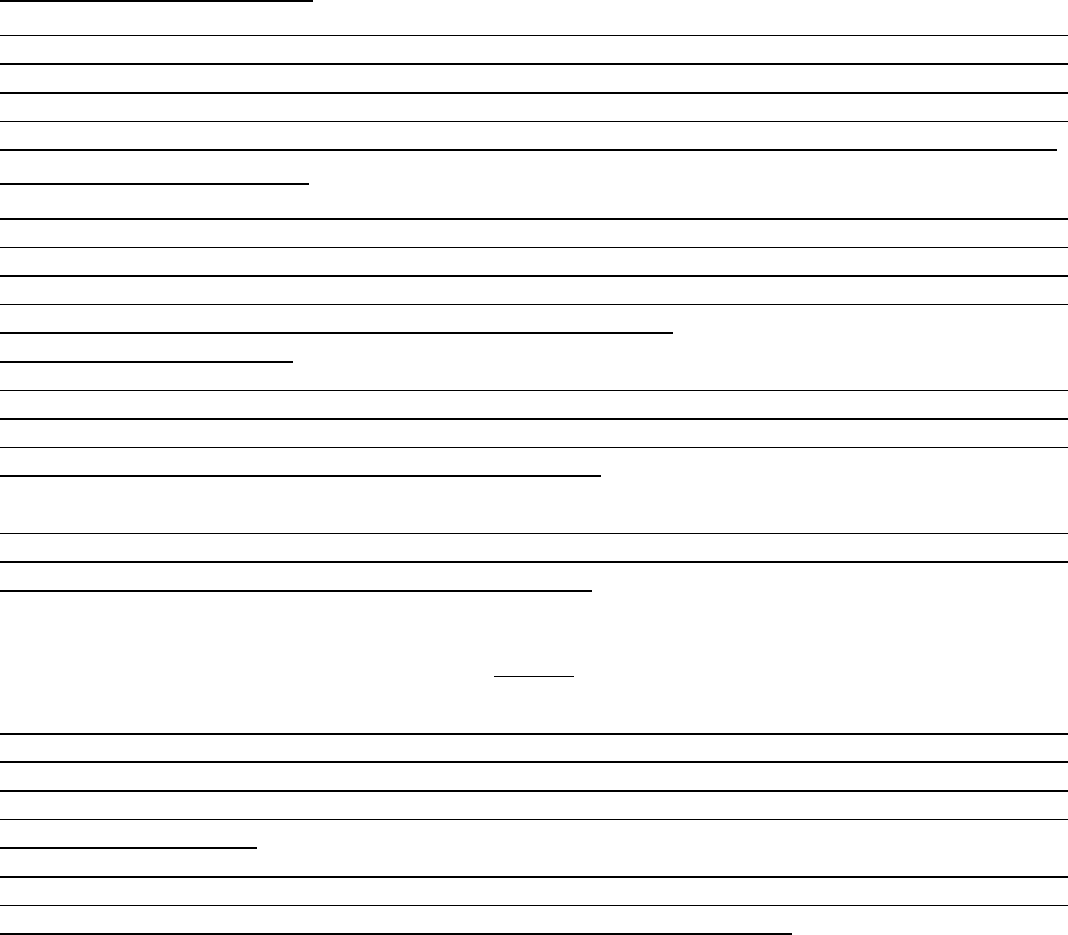
The Insurance Company has stated in their self-contained note that the insured was covered under Parivar
Mediclaim Policy for the period from 21-06-2020 to 20-06-2021 with sum insured of Rs.6,00,000/-. The insured
was admitted in the hospital for the period from 02-03-2021 to 06-03-2021 for the treatment of Abdominal
Hysterectomy. The insured lodged claim for Rs.2,30,058/- against hospitalization expenses. The Insurance
Company has paid an amount of Rs.1,26,342/- as hospitalization procedure charge as per Operative Clause of
the Policy which says that in case of hospitalization, charges reasonably, customarily and necessarily incurred
shall be paid to the insured. Reasonable and Customary Charges have been defined in Clause No.6.42 of National
Parivar Mediclaim Policy.
Contention of the complainant:
Shri Manas Kar, husband of the complainant, has stated in the hearing that the insured was admitted in the
hospital for treatment of Abdominal Hysterectomy and after discharge from the hospital, the insured lodged
claim for reimbursement of treatment expenses but the Insurance Company settled the claim partially. The
Insurance Company has settled the claim as per PPN rate and as per Reasonable and Customary Charges
Clause. The total claim was for Rs.2,30,058/- but the Insurance Company settled the claim for Rs.1,26,342/-.
Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured was admitted in the
hospital for treatment of Abdominal Hysterectomy. The hospital was not under PPN. The Insurance Company
has paid the maximum amount based on highest PPN Package of the same category hospital. The insured did
not avail the PPN Hospital inspite of having knowledge of the same. The Insurance Company has settled the
claim as per Reasonable and Customary Charges Clause of the policy.
Observation and conclusions:
It is observed that the complainant and the representative of the Insurance Company both have attended the
hearing physically at this office premises. The complainant has stated in the hearing what already stated in
the written complaint submitted to this office. The representative of the Insurance Company has stated that
the claim has been settled as per policy terms and conditions.
It is found from the submitted documents as well as submissions made by both the parties during the course
of hearing that the insured is well known about the PPN Package and inspite of it, the insured was admitted in
the non-PPN hospital where cashless facility is not available.
AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the insured was
admitted in the Non-PPN Hospital where cashless facility is not available. The Insurance Company has settled
the claim based on Reasonable and Customary Charges Clause of the Policy and paid the highest package rate
which is standard charges.
It is found from the submitted documents and submissions made by both the parties in the hearing that the
decision of Insurance Company is in order. As such, the Insurance Company is not liable to make any payment
further. Hence, the complaint is dismissed without any relief to the complainant.
If the decision is not acceptable to the complainant, he/she is at liberty to approach any other
Forum/Court as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on Day of 30
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
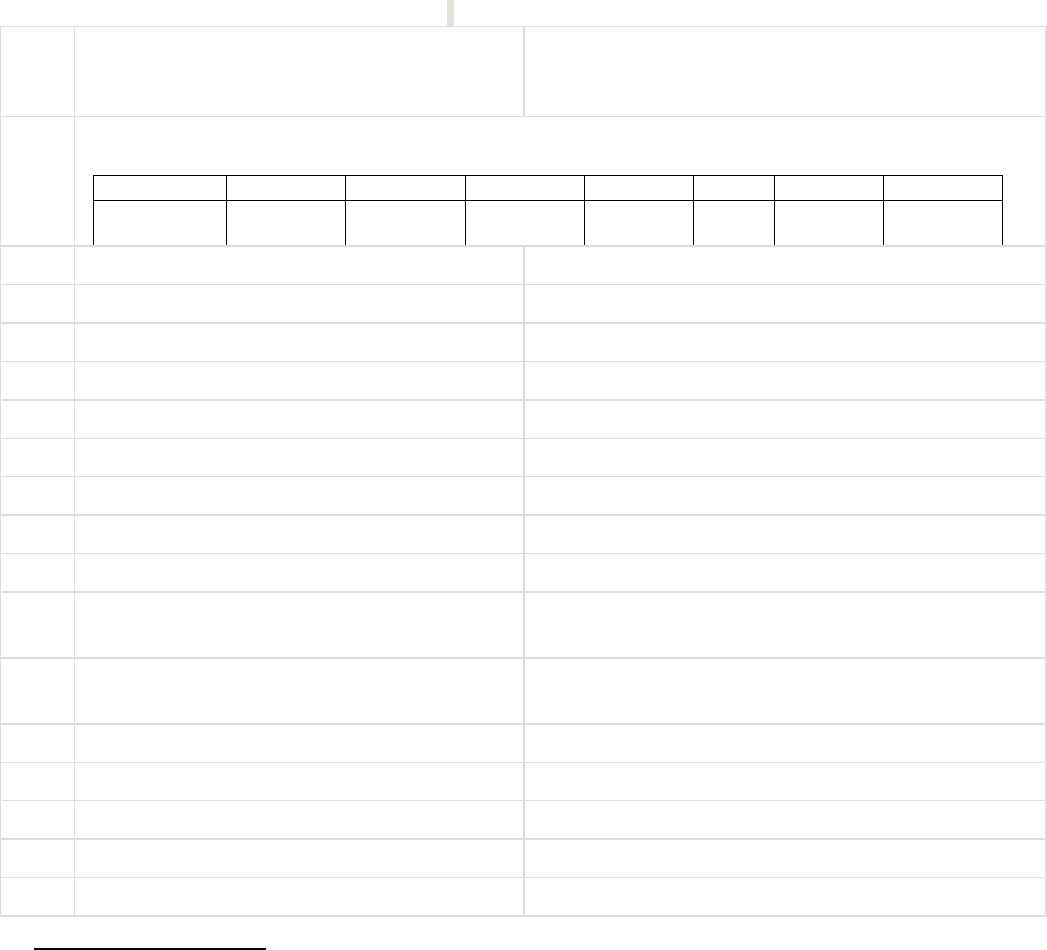
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT– SHRI ARUP MITRA
VS
RESPONDENT: THE NEW INDIA ASSURANCE CO. LTD.
COMPLAINT REF: NO: KOL-H-049-2122-0292
AWARD NO: IO/KOL/A/HI/0249/2021-2022
1.
Name &Address OfThe Complainant
Shri Arup Mitra
27C, K P Roy Lane, 2
nd
floor
Dhakuria, Kolkata – 700 078.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
5109003416
2500003701
200000
16-03-2017
15-03-2018
One year
single
3.
Name of insured
Shri Arup Mitra
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
22-03-2018 and 27-03-2018
6.
Reason for Repudiation
As per Exclusion Clause of the policy
7.
Date of receipt of the Complaint
05-Jul-2021
8.
Nature of Complaint
9.
Amount of Claim
57,341.00
10.
Date of Partial Settlement
11.
Amount of relief sought
57,341.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claim by the insurer
13.
Date of hearing
Place of hearing
27-Sep-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Shri Arup Mitra
b)For the Insurer
Shri Joyjit Sen
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
30-Sep-2021
17. Brief Facts of the Case:
The complainant-cum-insured is covered under New Mediclaim 2012 Policy with the New India Assurance
Company Ltd. The complainant was admitted in the hospital on 20-12-2017 and 31-01-2018 respectively and
discharged on the same day for administering Intra vitreal injection, Lucentis (Ranibizumab). The complainant
submitted claims for Rs.57,341/- (Rs,29,303 + Rs.28,038/-) for reimbursement of treatment expenses but the
Insurance Company did not settle the claims till date. Being aggrieved, the complainant has lodged complaint
to this office for redressal of his grievances.
The Insurance Company has stated in their self-contained note that the insured was admitted in the hospital on
20-12-2017 and 31-01-2018 for administering intra vitreal injection, Lucentis (Ranibizumab) and discharged on
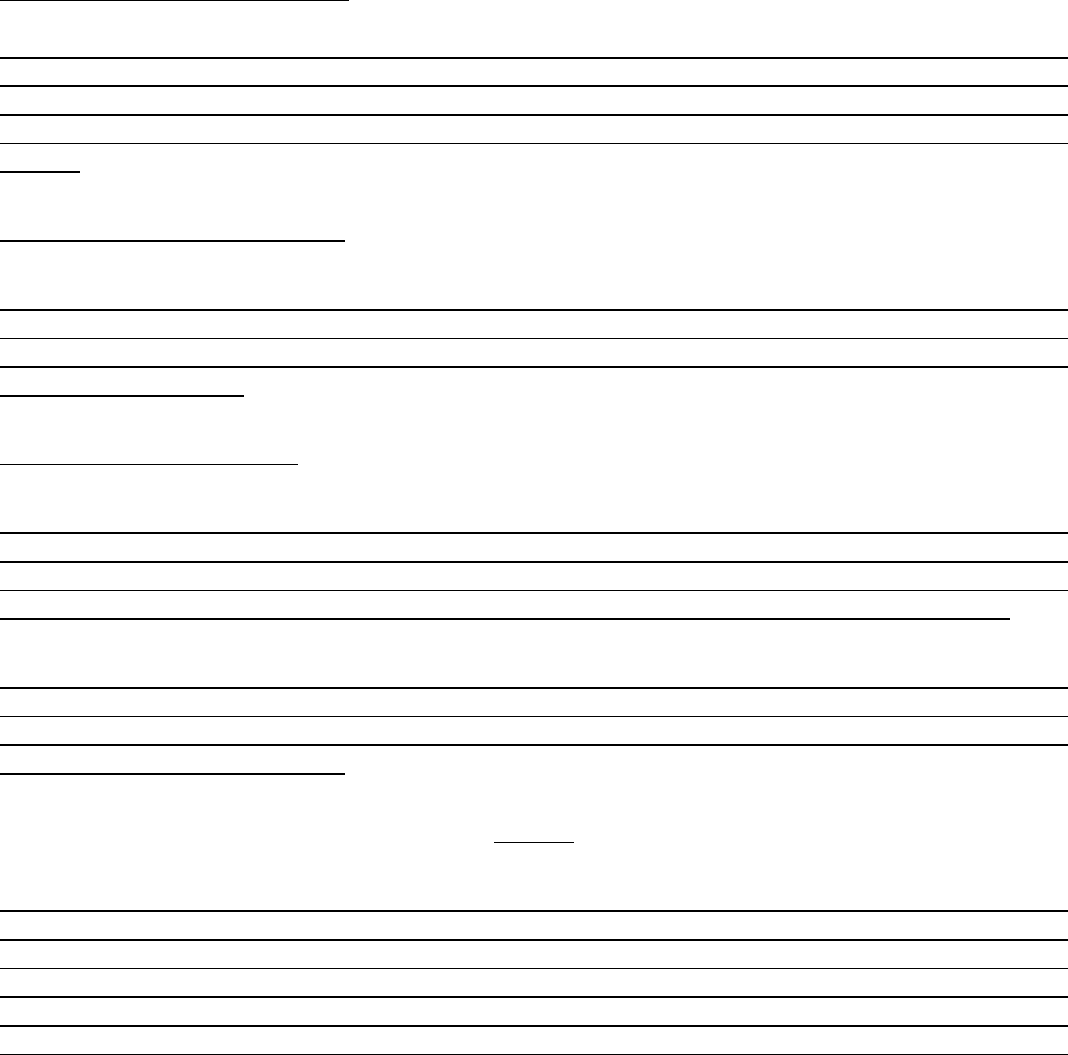
the same day. The insured lodged claims for reimbursement of treatment expenses. The Insurance Company
repudiated claims are not payable as per Day Care Procedure under Policy Exclusion Clauses No.2.11 and
4.4.22.
Exclusion Clause No.2.11 - Day Care treatment refers to medical treatment and/or surgery which are undertaken
under general anesthesia in a hospital/day care centre in less than twenty four hours because of technological
advancement or which would have otherwise required hospitalization more than 24 hours.
Exclusion Clause No.4.4.22 - Treatment for Age Related Macular Degeneration (ARMD) treatments such as
Rotation Field Quantum Magnetic Reasonance (RFQMR), External Counter Pulsation 9ECP), Enhanced
External Counter Pulsation (EECP), Hyperbaric Oxygen Therapy.
18. Contention of the complainant:
The complainant has stated in the hearing that as per advice of the treating doctor, the insured was admitted
in the hospital on 20-12-2017 and 31-01-2018 and discharged on the same day for taking intravetreal injection
and after discharge from the hospital, the insured lodged claims for reimbursement of treatment expenses but
the Insurance Company repudiated the claims. But the Insurance Company settled claims earlier for the same
ailment.
19. Contention of the Respondent:
The representative of the Insurance Company has stated that the claim has been repudiated as per Policy
Clause No.2.11 and 4.4.22 respectively. The insured patient was admitted in the hospital for administering
intra vitreal injection in Day Care basis which is not payable as per policy terms and condition under Clause
2.11 of Mediclaim Policy.
Observation and conclusions :
It is observed that the complainant has attended the hearing physically at this office premises whereas the
representative of the Insurance Company has attended the hearing online. The complainant has stated what
he already stated in his written complaint submitted to this office. The representative of the Insurance Com-
pany has stated in the hearing that the claims have been repudiated as per policy terms and conditions.
It is found from the submitted documents as well as submissions made by both the parties during the course
of hearing that the insured patient was admitted in the hospital as per advice of treating doctor as an inpatient.
Besides, it is for the treating doctor to decide the line of treatment and the type of procedure to be adopted
which is best suited for the patient.
AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the Insurance
Company has repudiated the claims as per policy terms and conditions. The insured patient was admitted in
the hospital as per advice of treating doctor. Besides, it is for the treating doctor to decide the line of treat-
ment and type of procedure to be adopted which is best suited for the patient. As such, the decision of repu-
diation is set aside and the Insurance Company is directed to admit the claims and arrange for payment subject

to applicable deductions in respect of exclusions/non-payables/ceilings/limitatio9ns as specified under the pol-
icy terms and conditions.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day of 30
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name:P.K.RATH
CASE OF COMPLAINANT– SHRI PARTHA MITRA
VS
RESPONDENT: THE ORIENTAL INSURANCE CO. LTD.
COMPLAINT REF: NO: KOL-H-050-2122-0211
AWARD NO:IO/KOL/A/HI/0213/2021-2022
1.
Name &Address OfThe Complainant
Shri Partha Mitra
38/1B, P G H Shah Road
Jadavpur, Kolkata – 700 032.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
311604/48/2
021/4028
100000
25-01-2021
24-01-2022
6284
One year
Single
3.
Name of insured
Shri Partha Mitra
4.
Name of the insurer
The Oriental Insurance Company Limited
5.
Date of receipt of the Complaint
22-Jul-2021
6.
Nature of Complaint
Repudiation of claim
7.
Amount of Claim
9,506.00
8.
Date of Partial Settlement
9.
Amount of relief sought
9,506.00
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) - any partial or total repudiation of
claims by the insurer
11.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Shri Partha Mitra
b)For the Insurer
Shri K Chandrasekhar
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
13-Sep-2021
Brief Facts of the Case:
The complainant-cum-insured has stated in his complaint that the insured was covered under Mediclaim
Insurance Policy with the Oriental Insurance Company. The insured is suffering from Carcinoma of Urothelial
Papillary Trans Cell and admitted for treatment of the same. During hospitalization, the insured patient was
treated by Intra-Vesical BCG at Day Care procedure. After discharge from the hospital, the insured lodged claim
for Rs.9,506.00 but the Insurance Company repudiated the claims showing the reason that the Intra-Vesical BCG
is an immunotherapy agent or vaccine which is not payable as per Policy Exclusion Clause No.4.5. The
Insurance Company paid claims earlier for the same treatment. The insured, being aggrieved, lodged complaint
for redressal for his grievances.
The Insurance Company has stated in their self-contained note that the insured, Shri Partha Mitra was admitted
in the hospital for treatment of Carcinoma of Urothelial pa;illary Trans. Cell treated by Intra-vesical BCG which
is an immunotherapy agent or Vaccine. As per Policy exclusion Note no.4.5 and 2.11 of Individual Mediclaim
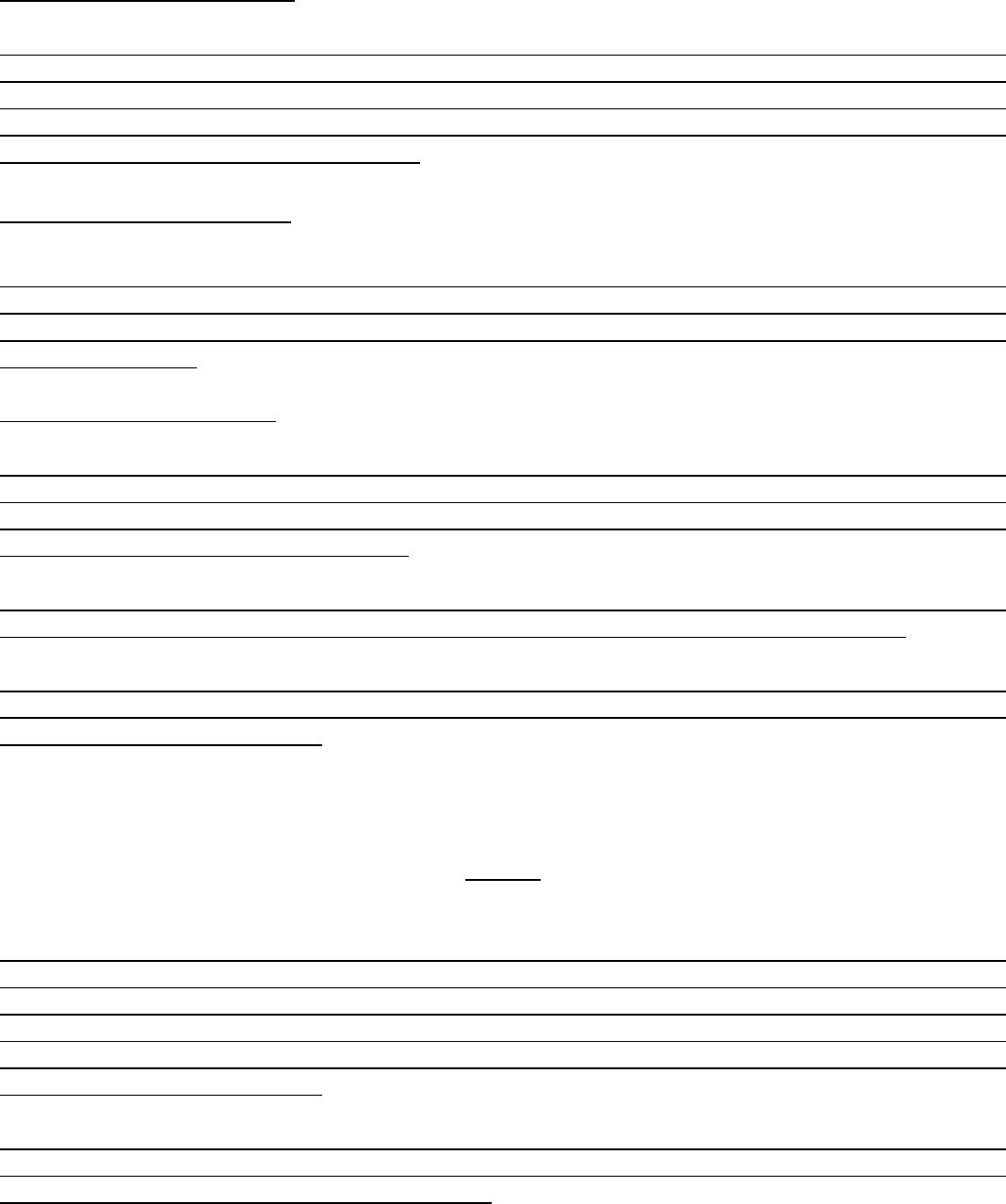
Policy, Vaccine or Immunotherapy is inadmissible. Further, the policy was issued before the new IRDA
Regulations w.e.f. 1
st
October, 2020.
Contention of the complainant:
The complainant-cum-insured has stated in the hearing that the insured is suffering from Carcinoma of Urothe-
lial Papillary Trans Cell and admitted in the hospital for treatment. During the hospitalization period, the
insured patient was treated by Intra-vesical BCG at Day Care procedure. The Insurance Company did not settle
the claims showing the reason that it is a vaccine and the same is not admissible. But the Insurance Company
paid all claims for the same treatment earlier.
Contention of the Respondent:
The insured is suffering from Cancer and was admitted in the hospital for the said disease. During the hospi-
talization, the insured patient was given Intra-vesical BCG which is an immunotherapy agent or vaccine. As per
Policy Exclusion Clause No.4.5, vaccine or immunotherapy is not payable. Hence, the Insurance Company has
repudiated the claim.
Observation and conclusions:
It is observed that the complainant as well as the representative of the Insurance Company both have attended
the hearing physically at this office premises. The complainant has stated what he already stated in his written
complaint submitted to this office. The representative of the Insurance Company has stated that the claim has
been rejected as per Policy Exclusion Clause.
It is observed from the submitted documents as well as submissions made by both the parties during the course
of hearing that the insured patient is suffering from Cancer and the procedure is given in Day Care.
Prima facie, there seems to be no malafide intention on the part of the insured. Besides, it is for the treating
doctor to decide the line of treatment and the type of procedure to be adopted which is best suited for the
patient and most beneficial to him.
AWARD
Taking into account the facts and circumstances of the cases and submissions made by both the parties during
the course of hearing and after going through the documents on record, it is observed that the insured patient
was admitted in the hospital and as per advice of doctor, the Intra-vesical BCG was administered for treatment
of Carcinoma. There seems to be no malafide intention on the part of the insured. Besides, it is for the treating
doctor to decide the line of treatment and the type of procedure to be adopted which is best suited for the
patient and most beneficial to him.
In view of the above, the Insurance Company is directed to admit the claims subject to applicable deductions,
such as, exclusions/non-payables/ceilings/limitations, if any, as specified under the policy terms and condi-
tions. Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day of 13
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
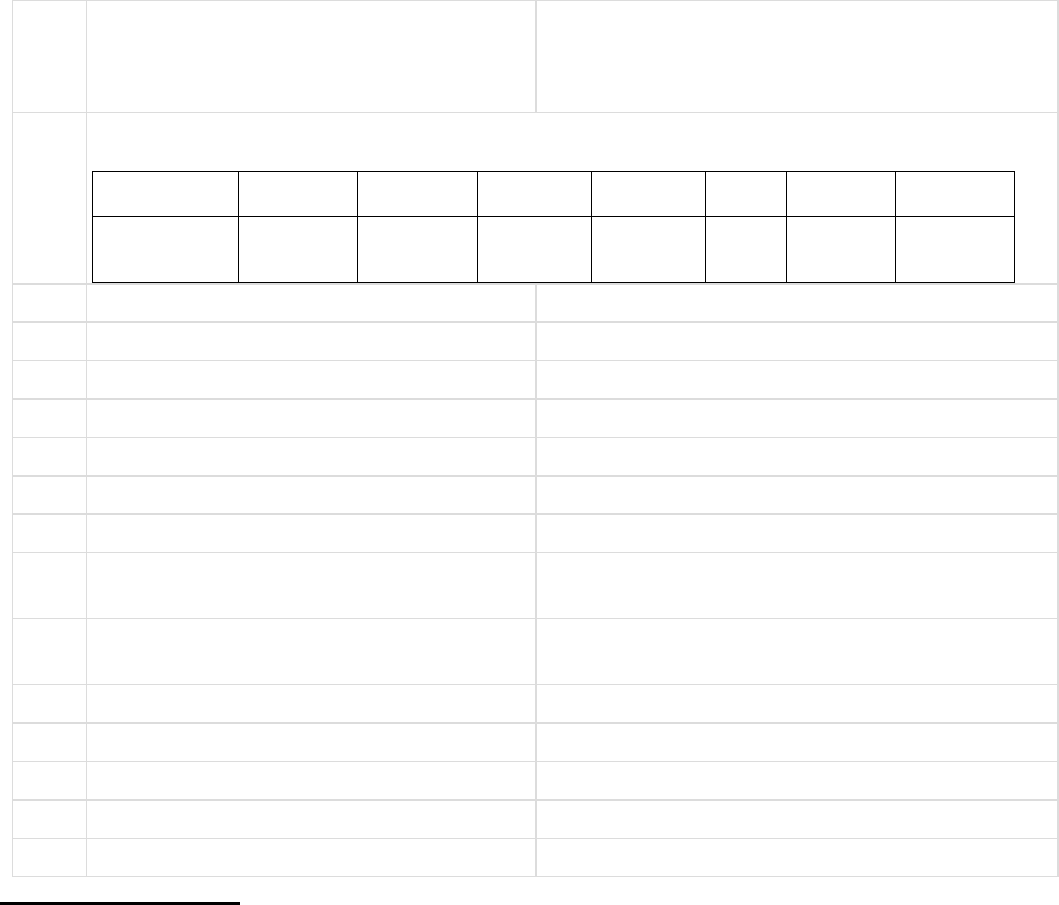
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – Sri Probin Kr. Saha
VS
RESPONDENT: -- National Insurance Co. Ltd
COMPLAINANT REF: NO: KOL-H-048-2122-
0218
AWARD NO: IO/KOL/A/HI/0207/2021-2022
1.
Name &Address OfThe Complainant
Sri Probin Kumar Saha.
58,Ramkrishna Sarani,
Behala, Kolkata- 700060
West Bengal.
2.
Type Of Policy: Health
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
106006/50/20
/10000127
1 lakh
17.04.2020
16.04.2021
22.12.2020
6733/-
Mediclaim
Annual
3.
Name of insured
Sri Probin Kumar Saha
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of receipt of the Complaint
10.08.2021
6.
Nature of Complaint
Rejection of claim.
7.
Amount of Claim
24207/-
8.
Date of Partial Settlement
NA
9.
Amount of relief sought
24207/-
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1) (b).
11.
Date of hearing
Place of hearing
06.09.2021
Kolkata
12.
Representation at the hearing
--
a)For the Complainant
Absent for hospitalization.
b)For the Insurer
Sri Tanmoy Chakraborty
13.
Complaint how disposed
Through on line hearing.
14.
Date of Award
08.09.2021
Brief Facts of the Case: --
Complainant cum patient, after having impairment ( dimness) of vision in right eye since 27.09.2020 & after
having consultation with Doctor on 29.09.2020, admitted to Apollo Hospital on 22.12.2020 at 12.15 PM.
Treatment involve silicon oil removal with 3 part entry & anterior chamber wash in right eye. Released on the
same day at 4.15 PM. Final diagnosis is post operated VR surgery with intraocular emulsified silicon oil in right
eye. Cash less claim denied. Further Reimbursement claim of Rs 24207/- declined by Insurer on 29.10.2020,
applying exclusion clause- 4.8 which states that surgery for correction of eye sight due to refractive error, is
excluded from the scope of cover.
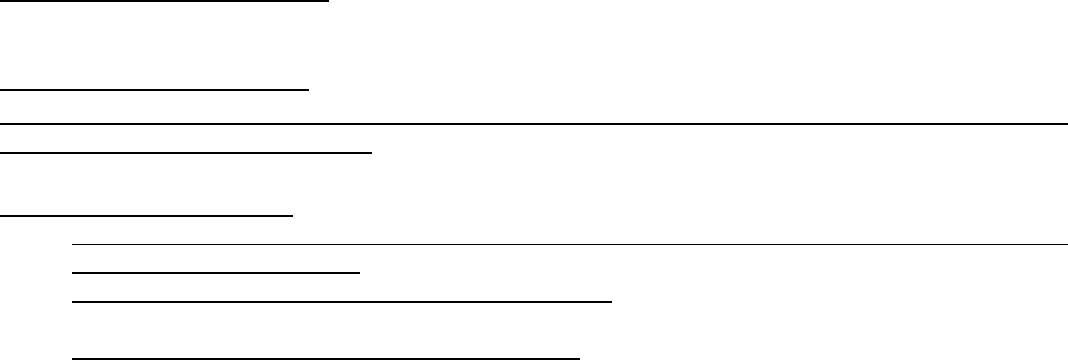
Contention of the complainant:-
Complainant further hospitalized during the time of hearing for other ailment. So requested to consider the claim
in his absence also.
Contention of the Respondent:
Insurer further reviewed the claim based on appeal of the Insured. Now, they have decided to consider the
claim based on submitted documents.
Observation and conclusions:
13) Claim amount is Rs 24207/- for silicon oil removal with 3 parts entry & anterior chamber wash in right
eye at Apollo Medical Centre.
14) Policy cover is against basic sum Insured of Rs one lakh.
AWARD
Taking into account the facts & circumstances of the case & the submissions made by both the parties in
hearing, as also from the submitted documents it is observed that Insurance Company is agreed to
consider the claim upon subsequent review by their claim settling Authority. This is also confirmed
through their self contained note. It is therefore directed to Insurer to settle the claim for an amount of Rs
24207/- subject to verification of bill & cash memos & which is under the ambit of policy coverage. With
this, the Complaint is closed & treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provision of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
Award and shall intimate the compliance to the Ombudsman.
SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – Sri Aloke Das
VS
RESPONDENT: -- Manipal cigna Health Insurance Co. Ltd
COMPLAINANT REF: NO: KOL-H-053-2122-0314
AWARD NO: IO/KOL/A/HI/0234/2021-2022
1.
Name &Address OfThe Complainant
Sri Aloke Das
39, Ashutosh Colony, P.O- Haltu
P.S Garpha, Kolkata-
2.
Type Of Policy: Health
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
PROHLR11124
8881
4.50 LAKH
07.04.2021
06.04.2022
02.07.2021
&
01.05.2021
10987
Mediclaim
Annual
3.
Name of insured
Sri Aloke Das
4.
Name of the insurer
Manipal Cigna Health Insurance Co.
Ltd.
5.
Date of receipt of the Complaint
10.09.2021
6.
Nature of Complaint
Rejection of two Claims under the same policy.
7.
Amount of Claim
126483/- & 36767/-
8.
Date of Partial Settlement
NA
9.
Amount of relief sought
126483/- for the hospitalization period- 01.05.2021
to 06.05.2021 & Rs 36767/- (Hospitalization Period-
02.07.2021 to 04.07.2021).
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1) (b).
11.
Date of hearing
Place of hearing
27.09.2021
Kolkata
12.
Representation at the hearing
--
a)For the Complainant
Sri Aloke Das
b)For the Insurer
Ms Swetha Nair
13.
Complaint how disposed
Through on line hearing.
14.
Date of Award
29.09.2021
Brief Facts of the Case: --
Insured patient cum Complainant Sri Aloke Das complaining for non settlement of two claims under the policy
period-07.04.2021 to 06.04.2022 which is continuing with the present Insurer since 2018. Previously it was
with Religaire Insurance Company. Policy ported on line. There are two claims under the present complaint—
FIRST CLAIM 1) 01.05.2021 to 06.05.2021-at Hope Kolkata Foundation Charitable Hospital. Claim amount—
126483/-, Diagnosis- Fever & LRTI. Pre existing disease- T2DM (as per discharge summary)
2
ND
CLAIM - 2) 02.07.2021 to 04.07.2021 at Aurobindo Seva Sadan, Diagnosis-Acute gastroenteritis, gall
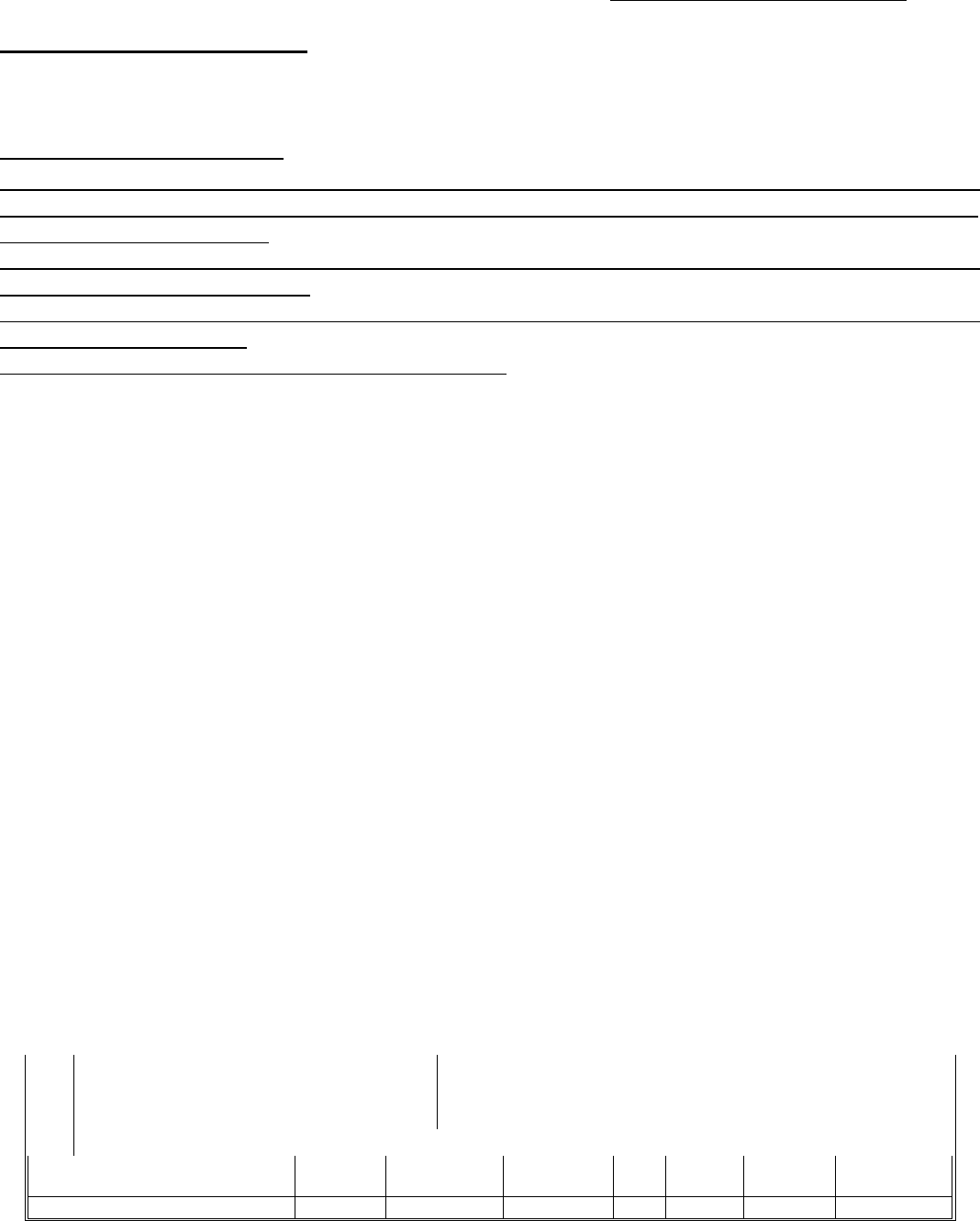
bladder sludge. Claim amount—36767/-. Pre existing disease- T2DM, IBS (irritable bowel syndrome) & Post
Covid status. (As per discharge summary)
Since patient had history of T2DM, IBS before porting the policy & was under treatment 10 years ago, Insurer
declining both the claims as earlier sufferings not disclosed while porting the policy with them.
Contention of the Complainant:-
Complainant in his statement stated that he consulted with Dr Sanjoy Sen about 10 yrs back who stated that
Patient had IBS but he did not undertake any medication on it. So this suffering should not be given any
importance & because of Insistence of Insurer, he confessed the said fact for which he should not be penalized.
Contention of the Respondent:
From the statement of the Insured it is clear that the Insured did not divulge the past suffering of IBS & T2DM
while porting the policy to them which prejudice the right of recovery of the Insured from the scope of cover.
Observation and conclusions:
1)Statement of Insured reflects that about 10 years back he had IBS as per opinion of Dr Sanjoy Sen But he
did not take any medicine for that.
2) From the submitted prescription (OPD) of Sri Aurobindo Seva Kendra, it is observed that Patient had T2DM
& IBS & was on medication.
AWARD
Taking into account the facts & circumstances of the case & the submissions made by both the parties in
hearing, as also from the submitted documents it is observed that the decision of Insurer towards rejection
of claim for non disclosure of past suffering while porting the policy, is supported & substantiated by
documents through prescription (OPD) as well as from the submission of Insured by himself. It is
therefore concluded, not to consider allowance of the said claims, keeping in view the prevailing policy
condition, as well as, in support of Insurer findings & opinion. The Complaint is therefore treated as
closed without any relief to the Complainant & disposed of without further reference.
SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Manas Kumar Bhattachariya
VS
Respondent : Bajaj Allianz General Insc Co. Ltd.
COMPLAINT REF NO: KOL-H-005-2122-0184
AWARD NO:IO/KOL/A /HI/ 0223 / 2021-2022
1.
Name & Address of the Complainant
Mr. Manas Kumar Bhattachariya
Vill. + P.O. Hatiberia, P.S. Haldia, Dist. Purba Medinipur, Pin -
721657.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
OG-21-2410-6021-00000307
10,00,00
14/02/2021
13/02/202
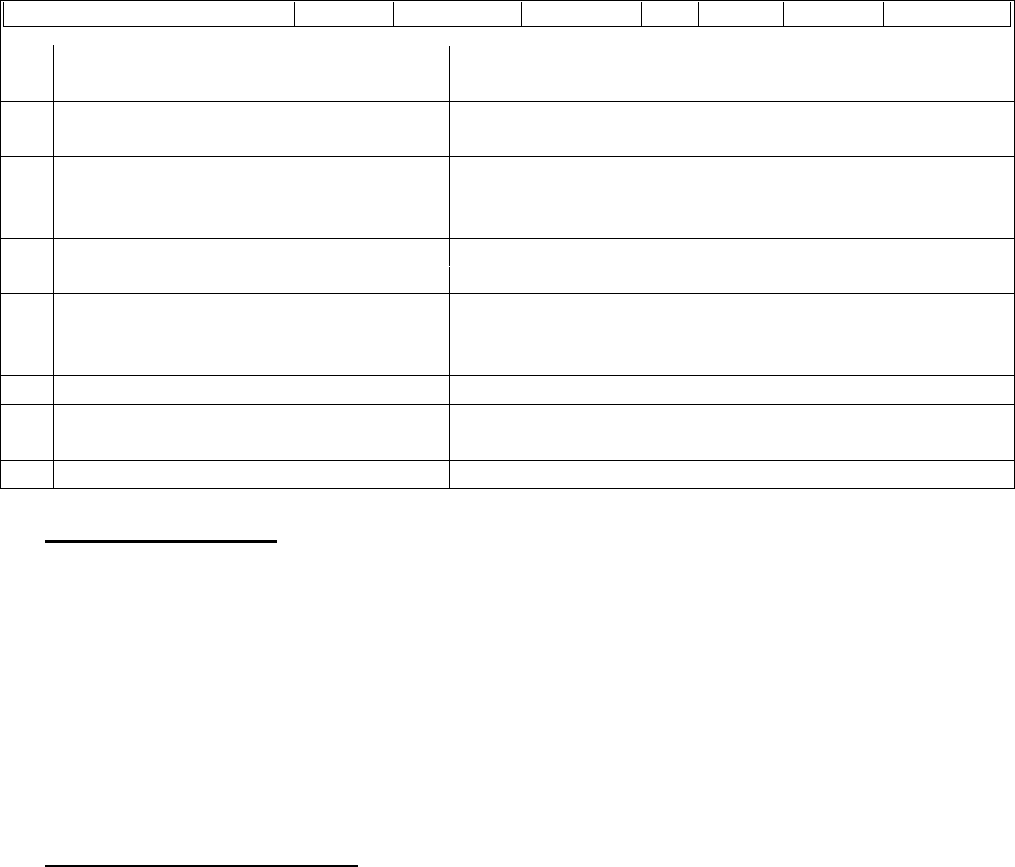
0
2
3.
Name of the insured
Mr. Manas Kumar Bhattachariya
4.
Name of the insurer
Bajaj Allianz General Insc Co. Ltd.
5.
Date of Receipt of the Complaint
15-Jul-2021
6.
Nature of Complaint
Denial of Claim & Cancellation of Policy
7.
Amount of Claim
Treatment Cost = Rs.84,844/- + Premium Rs.16,546/-
Total = Rs.1,01,390/-
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.2,00,000/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Manas Kumar Bhattachariya
• For the insurer
Dr. Ravindra Singate
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021
Brief Facts of the Case:
Policy Name :: Individual Mediclaim
Policy Type :: Health Insurance,
Period of Insurance :: 14/02/2021 to 13/02/2022
Sum Insured :: Rs.10,00,000/-
Hospitalisation date/s:: 15/03/2021 to 17/03/2021
The complainant lodged complaints against the Insurance Company in connection with repudiation of
hospitalisation claim & Cancellation of Policy. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) Claim denied under Non-disclosure of material fact under the policy without considering the fact that
the policy running into 5
TH
year.
(ii) Policy was bought under portability scheme with 4 years continuity benefit which is running into 5
th
year.
(iii) At the time of submission of proposal form, no one from the Company guided the terms and conditions
that apply even after portability with continuous coverage (in this case its 4 years). He thought that as
his policy has already crossed 3 years, most of the surgeries are covered as waiting periods are maximum
of 3 to 4 years.
(iv) He was already covered under previous insurance policy from the New India Assurance when diagnosed
with Gallbladder stone. He could have gone for surgery through cashless facility then also as his policy
had 4 years continuous coverage but decided to try medicines first due to the age being 67 years old and
due to the current pandemic situation. But when the doctor said that there is no other way except surgery,
he decided to go for surgery and at that time he has changed his health insurance from New India to this
Company. To his surprise, they denied the claim and cancelled the policy.

(v) Highlighted (bold) portion on Page 2 & 4 of the policy document where under the terms and conditions
on 4
th
page in Waiting Period Related Clause – Point No.1, it is clearly mentioned:
“Pre-existing health condition or disease or ailment / injuries: Any ailment / injuries: Any ailment
/ disease /injuries /health condition which are pre-existing (treated / untreated, declared / not
declared in the proposal form), in case of any of the insured person of the family, when the cover
incepts for the first time, are excluded for such insured person up to 3 years of this policy being
in force continuously.”
Being aggrieved and dissatisfied with the Non-settlement of claim & Cancellation of Policy by the Insurance
Company, the complainant has approached this office for redressal of his grievance. The complainant has also
given his unconditional and irrevocable consent to the Insurance Ombudsman to act as a mediator between
himself and the insurance company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) dated has stated that:
• That the complainant is a 66years old male patient covered under Punjab National Bank A/C holder and
Mediclaim policy with us since 14th Feb 2021.
• The complainant ported his policy Earlier from Oriental Insurance Company Ltd which was from February
2017 to New India Assurance Company and From New India Assurance Company Ltd to Bajaj Allianz Gen-
eral Insurance Company Ltd (BAGIC) From 14th Feb 2021.
• The proposal form was clean and no any ailment was disclosed, considering no any ailment and no risk
associated we have accepted portability under utmost good faith and is duty of insured to declare all
ailments while filling proposal form to assess the risk correctly. In view of no ailment disclosed they have
given continuity and accepted portability all benefits of waiting periods are passed except for the non-
disclosure as per IRDAI guidelines of portability.
• Cashless request received on 12-Mar-2021 from AMRI HOSPITALS for ailment Flatulence Dyspepsia in the
last 6 months and after evaluation diagnosed as Calculus Cholecystitis and underwent for LAP CHOLE-
CYSTECTOMY Surgery.
• During scrutiny of documents, it was noted that the complainant was having History of Diabetes Mellitus
since 1985, CABG in 2003 & Calculus Cholecystitis in November 2020 which was being never disclosed to
this insurance company while opting portability.
• As per the consultation paper & reply from the complainants it was observed that they never consulted
any Dr. regarding Cholelithiasis.
• First consultation of Dr Debjit Pal is on 9th Nov 2020, where patient is diagnosed as Cholecystitis with
Cholelithiasis and is on treatment for same, insured was aware of the ailments and treatments he is
undergoing before opting portability still the same is not disclosed on proposal form signed by him.
• The duration period of calculus Cholecystitis getting diagnosed was in Nov 2020 and policy incepted with
BAGIC is from 14th Feb 2021, Ailment which is prior to policy with BAGIC & ailment was not disclosed in
proposal form.

• As per the said terms and conditions of impugned insurance contract entered between the Parties, it was
mandatory for the complainant to not to conceal anything. Thereby the declaration given for taking the
present indemnification cover was found to be false. Hence, the policy is cancelled and as he has
breached the principle of utmost good faith and he is not entitled to any benefit under the present In-
surance Cover and non-refund of any pro-rata premium as claim was made on the said policy. In view of
Portability guidelines stated by IRDAI - Ref: IRDAI/HLT/REG/CIR/177/09/2019 Dated-27-Sept 2019.
• Had the ailment was disclosed to them as per the principle of Utmost good faith before portability they
would have not ported the policy with us.
• Hence, along with other non-disclosure (Diabetes Mellitus since 1985, Ischemic Heart Disease -Coronary
Artery Bypass Graft Surgery in 2003) the policy was being cancelled under non-disclosure material fact
under policy clause – B- 13.
• On entire scrutiny of Proposal form, Portability form, nature of non-disclosure, Treatment records the
claim is rejected under –
“The preauthorization request mentions the duration of Calculus Cholecystitis as since 8Nov
2020 which is not being disclosed in the proposal form, hence cashless stands denied under
exclusion clause B 13”
Policy Clause – 13. Disclosure to information norm: The Policy shall be void and all premium paid
hereon shall be forfeited to the Company, in the event of misrepresentation, mis-description or
non-disclosure of any material fact.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A, (d) Self Contained Note
from the insurer, (e) Discharge Summery & (f) Repudiation Letter.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the repudiation is in
consonance with the policy issued to the Complainant.
Hence, the complaint is dismissed without any relief to the complaint.
If the decision is not acceptable to the Complainant, She/He is at liberty to approach any other Forum/Court
as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on the 17
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
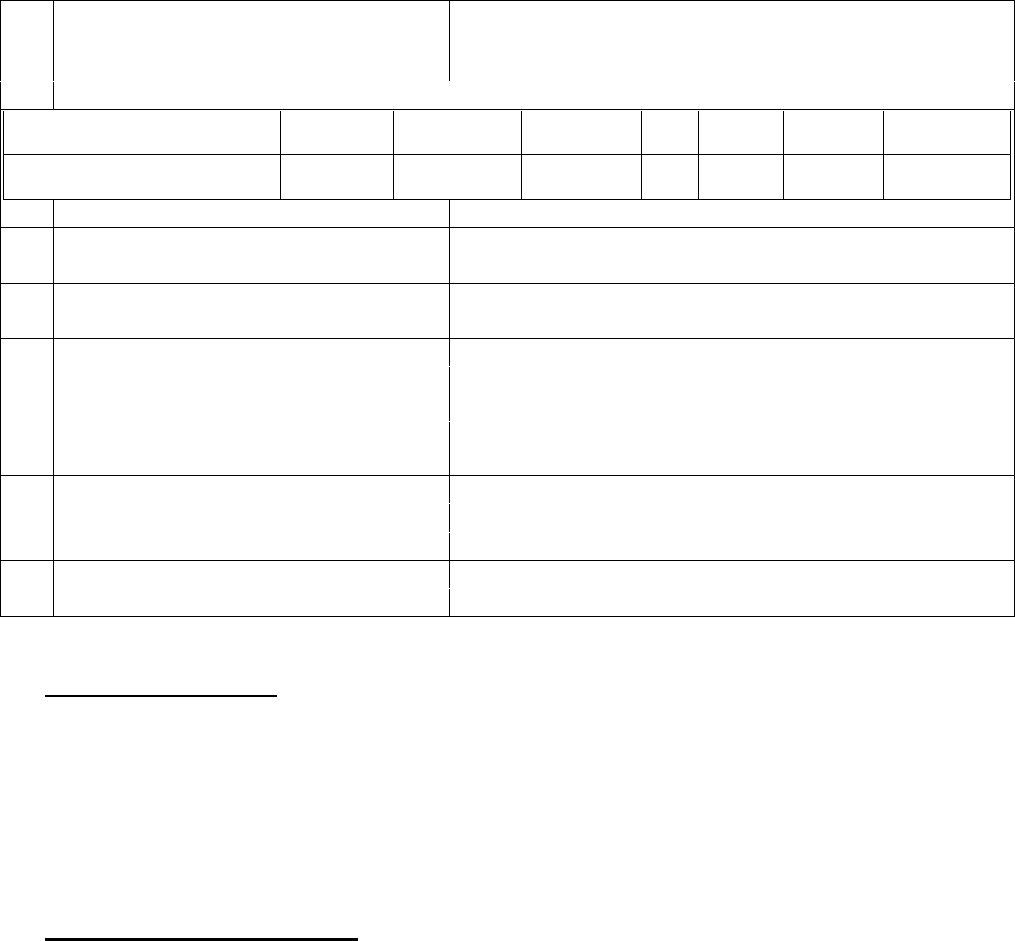
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Sunil Kumar Lakhotia
VS
Respondent : HDFC ERGO General Insurance Company Ltd.
COMPLAINT REF NO: KOL-H-018-2122-0236
AWARD NO:IO/KOL/A /HI/0226 / 2021-2022
1.
Name & Address of the Complainant
Mr. Sunil Kumar Lakhotia
113/4, Bangur Avenue, Block-C, 3rd floor,
Kolkata - 700056.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
150300/11122/AA0014768
7-03
5,00,000
31/10/2019
30/10/202
1
3.
Name of the insured
Mr. Sunil Kumar Lakhotia
4.
Name of the insurer
HDFC ERGO General Insurance Company Ltd.
5.
Date of Receipt of the Complaint
03-Aug-2021
6.
Nature of Complaint
Rejection of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.15,174/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Sunil Kumar Lakhotia
• For the insurer
Ms. Saswata Banerjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021
Brief Facts of the Case:
Policy Name :: Optima Restore Floater Policy,
Policy Type :: Health Insurance,
Period of Insurance :: 31/10/2019 to 30/10/2021
Hospitalisation date/s:: 20/04/2021
The complainant lodged complaints against the Insurance Company in connection with repudiation of his Covid
claim. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:

(i) They have called up HDFC Ergo office to buy Corona Kavach Policy way back in August 2020. However,
their representative suggested that their existing policy covers covid treatment even if it is home care.
Hospitalisation is not mandatory. Call records may be verified as call are recorded.
(ii) So they did not take a separate Corona Kavach Policy as they were paying huge premiums under their
existing family plan.
(iii) They were detected covid positive on 20/04/2020. All documents regarding their claim were duly
submitted. Their claim first rejected on grounds of home care treatment disallowed. When they pursued
them citing IRDA’s guideline in August, 2020 during the 1
st
wave to approve all claims even if under home
isolation and treatment, then they were told that no active line of treatment.
(iv) They were continuously being observed by the doctor online. As they all know, how unpredictable this
disease is: all vital chart were being maintained by them, all bold tests were conducted as per doctor’s
prescription, all protocols were followed so as not to spread the virus further. Hence, they don’t know
what else is the active line of treatment?
(v) Nobody would with the kind of premium which they have been paying would like to not get admitted in
a hospital. It is because of the non-availability and pressure on the health infrastructure, they took the
risk and keeping the interest in front.
Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) On 05/05/2021 they received a claim for reimbursement. It was observed that the insured treated with
oral treatment under home care under home isolation.
(ii) Further, as per symptoms here was no requirement of hospitalisation. Hence, treating doctor had advised
home isolation with oral tablets and no active line of management done.
(iii) Hence, as per above observation claim rejected. Prescription dated 24/04/2021 of and the rejection
letter is attached.
(iv) The Complainant had approached the grievance cell for reconsideration and it was specifically informed
to the complainant that:
k. Active line of treatment is monitoring of the health status by a medical practitioner for each day
through the duration of the home care treatment. Also daily monitoring chart including records of
treatment administered duly signed by the treating doctor is maintained.
l. Hom isolation without any active line of treatment is not covered under your policy or in Corona
Kavach policy as per the policy norms.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the complaint.

Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A & (d) Self Contained Note
from the insurer.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the repudiation is in
consonance with the policy issued to the Complainant.
Hence, the complaint is dismissed without any relief to the complaint.
If the decision is not acceptable to the Complainant, She/He is at liberty to approach any other Forum/Court
as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on the 17
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mrs. Anjali Lakhotia
VS
Respondent : HDFC ERGO General Insurance Company Ltd.
COMPLAINT REF NO: KOL-H-018-2122-0237
AWARD NO:IO/KOL/A /HI/ 0227 / 2021-2022
1.
Name & Address of the Complainant
Mrs. Anjali Lakhotia
113/4, Bangur Avenue, Block-C, 3rd floor,
Kolkata - 700056.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
150300/11122/AA00147687
-03
5,00,000
31/10/2019
30/10/202
1
3.
Name of the insured
Mrs. Anjali Lakhotia
4.
Name of the insurer
HDFC ERGO General Insurance Company Ltd.
5.
Date of Receipt of the Complaint
03-Aug-2021
6.
Nature of Complaint
Rejection of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.14,737/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mrs. Anjali Lakhotia
• For the insurer
Ms. Saswata Banerjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021
Brief Facts of the Case:
Policy Name :: Optima Restore Floater Policy,
Policy Type :: Health Insurance,
Period of Insurance :: 31/10/2019 to 30/10/2021
Hospitalisation date/s:: 20/04/2021
The complainant lodged complaints against the Insurance Company in connection with repudiation of her Covid
claim. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) They have called up HDFC Ergo office to buy Corona Kavach Policy way back in August 2020. However,
their representative suggested that their existing policy covers covid treatment even if it is home care.
Hospitalisation is not mandatory. Call records may be verified as call are recorded.
(ii) So they did not take a separate Corona Kavach Policy as they were paying huge premiums under their
existing family plan.
(iii) They were detected covid positive on 20/04/2020. All documents regarding their claim were duly
submitted. Their claim first rejected on grounds of home care treatment disallowed. When they pursued
them citing IRDA’s guideline in August, 2020 during the 1
st
wave to approve all claims even if under home
isolation and treatment, then they were told that no active line of treatment.
(iv) They were continuously being observed by the doctor online. As they all know, how unpredictable this
disease is: all vital chart were being maintained by them, all bold tests were conducted as per doctor’s
prescription, all protocols were followed so as not to spread the virus further. Hence, they don’t know
what else is the active line of treatment?
(v) Nobody would with the kind of premium which they have been paying would like to not get admitted in
a hospital. It is because of the non-availability and pressure on the health infrastructure, they took the
risk and keeping the interest in front.

Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of her grievance. The complainant has also given her unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) On 05/05/2021 they received a claim for reimbursement. It was observed that the insured treated with
oral treatment under home care under home isolation.
(ii) Further, as per symptoms here was no requirement of hospitalisation. Hence, treating doctor had advised
home isolation with oral tablets and no active line of management done.
(iii) The Complainant had undergone test for COVID 19 on 22/04/2021 and the report was issued on
23/04/2021, the prescription of Dr. Binani mentions Covid Positive case, however the initial prescription
of Dr. Chajer dated 24/04/2021 (copy enclosed) does not mention anything about suffering from Covid
19.
(iv) It is not clear as to the reasons for seeking multiple opinions from doctors for the detailed illness.
(v) The complainant has raised two bills for professional fees of Dr. Chajjer but only one prescription was
submitted by her.
(vi) The complainant has claimed to have been under the treatment of Dr. Chajer but his prescription dated
24/04/2021 does not declare her as Covid 19.
(vii) Hence, as per above observation claim rejected. Prescription dated 24/04/2021 and the rejection letter
is attached.
(viii) The Complainant had approached the grievance cell for reconsideration and it was specifically informed
to the complainant that:
m. Active line of treatment is monitoring of the health status by a medical practitioner for each day
through the duration of the home care treatment. Also daily monitoring chart including records of
treatment administered duly signed by the treating doctor is maintained.
n. Hom isolation without any active line of treatment is not covered under your policy or in Corona
Kavach policy as per the policy norms.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A & (d) Self Contained Note
from the insurer.
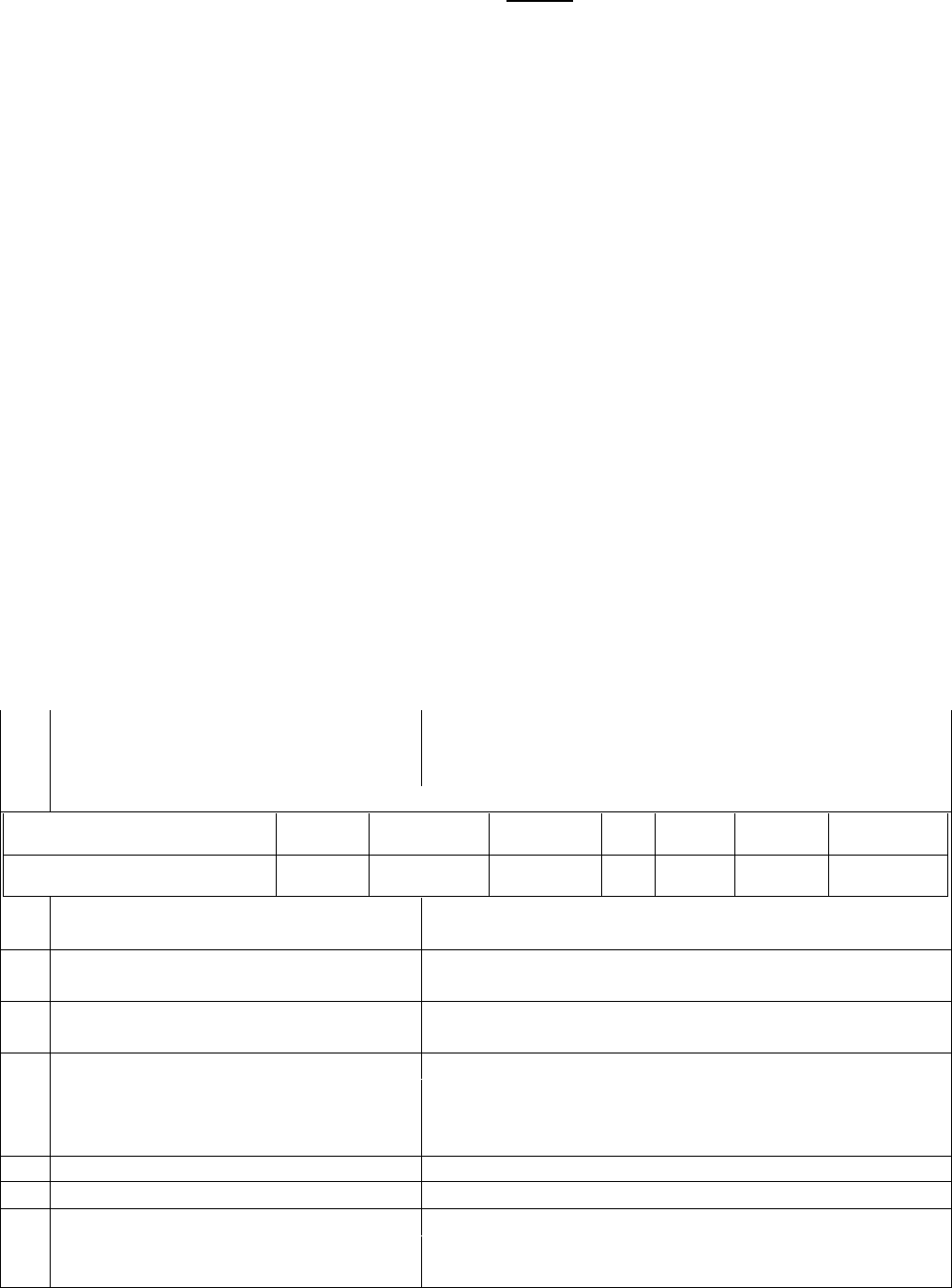
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the repudiation is in
consonance with the policy issued to the Complainant.
Hence, the complaint is dismissed without any relief to the complaint.
If the decision is not acceptable to the Complainant, She/He is at liberty to approach any other Forum/Court
as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on the 17
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Ms. Sangeeta Agarwal
VS
Respondent : IFFCO-TOKIO Genl. Insc. Co. Ltd.
COMPLAINT REF NO: KOL-H-023-2122-0234
AWARD NO:IO/KOL/A /HI/ 0228 / 2021-2022
1.
Name & Address of the Complainant
Ms. Sangeeta Agarwal
Flat-4/1H, Club Town Residency, 57/3, M.M. Feeder Road,
Kolkata - 700056.
2.
Type of Policy: Individual Mediclaim (Corona Kavach Policy)
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
H-0464233
5,00,000
13/10/2020
10/07/202
1
3.
Name of the insured
Ms. Sangeeta Agarwal
4.
Name of the insurer
IFFCO-TOKIO Genl. Insc. Co. Ltd.
5.
Date of Receipt of the Complaint
02-Aug-2021
6.
Nature of Complaint
Repudiation of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.2,15,376/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Ms. Sangeeta Agarwal
• For the insurer
Ms. Neelu Lal
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021

Brief Facts of the Case:
Policy Name :: Corona Kavach Policy,
Policy Type :: Health Insurance,
Period of Insurance :: 13/10/2020 to 10/07/2021,
Sum Insured :: Rs.5,00,000/-,
Hospitalisation date/s:: 19/12/2020 to 31/12/2020.
The complainant lodged complaints against the Insurance Company in connection with repudiation of her
hospitalisation claim. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) Her Covid Claim is repudiated by giving the reason: “Mild Covid”.
(ii) She was admitted in Apollo Gleneagles and was given full course of Remdesivir intravenous injection
which was considered the best god gifted medicine to treat her Covid 19. Hence, her case cannot be
considered as MILD Covid at all.
(iii) Nowhere in their policy, it is mentioned that the policy is not meant for “Mild Covid” case. Neither there
is any mention of its basis of measurement for Mild, Moderate or Severe Cases in the policy. There was
no mention of numerical range for RT-PCR values for various categories of Covid 19 from Mild, Moderate
to Severe. Hence, this is absolutely misleading and fraudulent.
(iv) Another reason given was HTN (Hypertension) which is contrary to my low BP at the time of admission
in the hospital. She is/was never a patient of Hypertension/High BP.
(v) Coming positive Covid Report creates temporary psychological panic for the patient as well as for all
family members / friends and it can temporarily raise or lower the BP of anyone & make her / him
depressed or highly anxious. The same has happened to her. As she became restless due to covid + and
no one in family know what to do next and till a proper arrangement for her hospitalisation is made &
just to make her calm down, she was given some medicines by her relative on emergency basis which
later turnout to be for HTN & anti-anxiety as recorded in hospital records at the time of admission. This
does not be interpreted that she was suffering from HTN or anxiety disease since long period. She is
notan HTN patient which is evident from the hospital record that no medicine for HTN/Anxiety was given
to me during the treatment in the hospital nor prescribed in the discharge certificate as post
hospitalisation prescription. She was only asked to monitor her BP as a precautionary measure for any
side effects of the treatment.
(vi) Not satisfied, the insurer again gave 3
RD
reason given for repudiation was Hypothyroidism not declared
at the time of purchase of policy. No option was available to her or authorised person at the time of filling
the form online for declaring existing diseases – link was not available to declare. Due to glitches and link
failure such things can happen and also the insurer has within their control to amend Policy Terms &
Conditions in online mode without any knowledge to Insured person technically.
Web Content can be changed or updated / manipulated by any host of Web Portal at any point to suit
their interest / display. Surely this has been done after purchase of the policy by her. Even reverification
of data filled in by insured person was not displayed for tick off as OK or a PDF file option for downloading

of the content was not provided so that all relevant information can be rechecked. This is normally done
with all major Bank/ Insurance companies or other similar institutions & instructions.
Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of her grievance. The complainant has also given her unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) dated has stated that:
(i) On scrutiny of the submitted cashless request form along with the supporting documents it was noted
that vitals of the patient were within normal Limits “temp-afebrile, BP 98/68, pulse 98/min, SPO2 98%
CT chest” all of which indicate mild COVID, which could have been managed on home quarantine or
COVID carecentre. The hospitalization was not required.
(ii) It was also noted that the patient is known case of HTN and hypothyroidism and the details of the same
were not disclosed in the proposal form.
(iii) That the patient was admitted in covid care centre for isolation purpose only, as stated in the submitted
claim documents, there was no mention of any symptoms and the hospitalization for such patients are
not required as per guidelines issued by ministry of health welfare for covid 19, attached herewith
(iv) In view of the above points the cashless was denied on 31 st Dec 2020.
(v) In this regard we would like to draw your attention to Clause 2 Operative, 3.7 Hospitalisation, and 3.8 In-
Patient Care of the policy:
“2. OPERATIVE CLAUSE:- If during the policy period the e Insured Person is diagnosed with
COVID and hospitalized for more than seventy-two hours following Medical Advice of a duly
qualified Medical Practitioner as per the norms specified by Ministry of Health and Family
Welfare, Government of India, the Company shall pay the agreed sum insured towards the
Coverage mentioned in the policy schedule, the copy of guidelines issued by Ministry of Health
and Family Welfare, Government of India.
3.7 - Hospitalisation means admission in a hospital designated for COVID-19 treatment by
Government, for a minimum period of seventy-two (72) consecutive ‘In-patient care’ hours.
3.8. In-Patient Care means treatment for which the insured person has to stay in a hospital
continuously for more than 72 hours for treatment of COVID.”
(vi) Further the Company Stated: -
a. The policy clearly states that the claim shall be payable on positive diagnosis of COVID,
requiring hospitalization for a minimum continuous period of 72 hours. In this case the
hospitalization was not required in view of submitted documents.
b. As per guidelines issued by Ministry of Health & Family Welfare, on 07/04/2020, cases
that have been clinically assigned as mild or very mild cases or COVID suspect cases shall be
treated either at isolation centres of with home isolation. The said guidelines further, states that
the Dedicated COVID Health Centre are hospitals that shall offer care for all cases that have been
clinically assigned as moderate only.
c. After denial of the cashless claim the complainant did not submit any claim for reimbursement.
That the cashless claim was denied as per terms and conditions of the policy.

(vii) Hence, the complainant is not entitled to get any relief as the claim of the complainant was repudiated
rightly as per the terms and condition of the insurance policy as stated above.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A, (d) Self Contained Note
from the insurer, (e) Discharge Summery.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the patient the patient
was hospitalised for 13 days and administered with Remdesivir. Hence, denial of claim on the ground of mild
covid is not justified.
In view of the above, the Insurance Company is directed to admit the claim and pay the claim amount of
Rs.2,15,376/- to the Complainant towards full and final settlement of the claim subject to deductions,
limitations, cappings, non-payables, Co-payment (if any) as per Policy Terms & Conditions.
Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of the
Insurance Ombudsman Rules-2017:
(d) As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of
the receipt of the AWARD and shall intimate the compliance to the Ombudsman.
(e) As per the Rule 17(7), the Complainant shall be entitled to such interest at a rate per annum as specified in
the regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date of the claim ought to have been settled under the regulations, till the date of payment of amount
awarded by the Ombudsman.
(f) As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be binding on the Insurers.
Dated at Kolkata on the 17THDay of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
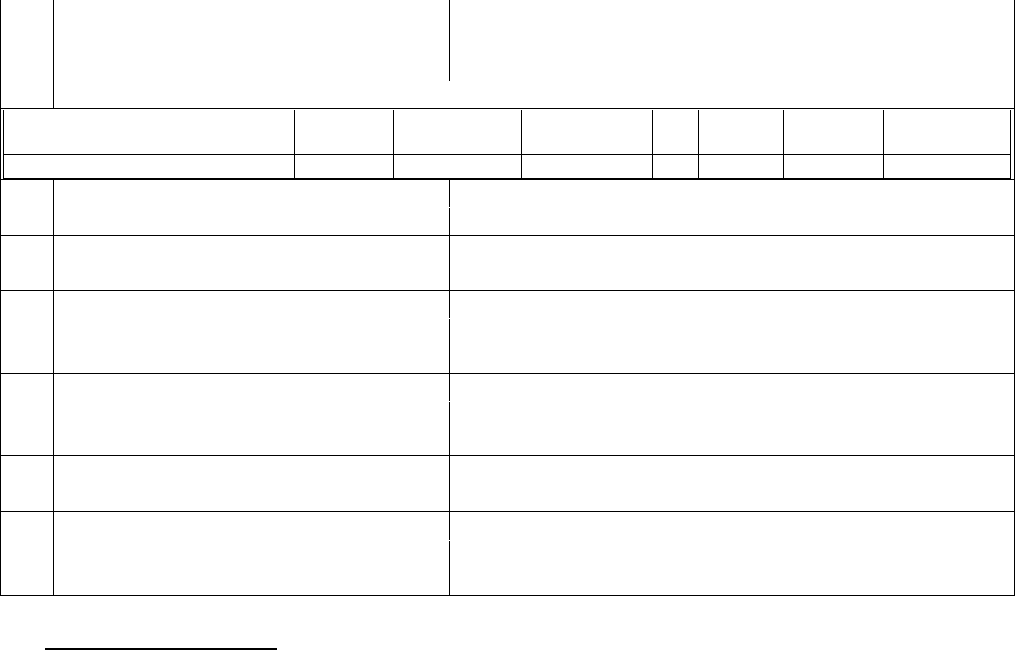
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant: Mr. ABHISHEK CHHAJER
VS
Respondent: The National Insurance Co. Ltd.
COMPLAINT REF NO: KOL-H-048-2122-0258
AWARD NO:IO/KOL/A /HI/ 0224 / 2021-2022
1.
Name & Address of the Complainant
Mr. ABHISHEK CHHAJER
B1/P1/5A2 , PRATHAM , 26 BT ROAD,
Kolkata - 700058.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DO
C
Premium
Policy
Term
Paying Term
101500501910003450
4,00,000
18/09/2019
17/09/2020
3.
Name of the insured
Mr. RATAN LAL CHHAJER
4.
Name of the insurer
The National Insurance Co. Ltd.
5.
Date of Receipt of the Complaint
18-Apr-2021
6.
Nature of Complaint
Repudiation of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.94,686/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. ABHISHEK CHHAJER
• For the insurer
Mr. Subrta Biswas
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021
Brief Facts of the Case:
Policy Name :: National Mediclaim Policy
Policy Type :: Health Insurance,
Period of Insurance :: 18/09/2019 to 17/09/2020
Sum Insured :: Rs.4,00,000/-
Hospitalisation date/s:: 03/10/2019, 03/01/2020, 03/04/2020 & 03/07/2020
(All same day discharges
The complainant lodged complaints against the Insurance Company in connection with repudiation of 4 claims.
Hence, this complaint lodged with this office for settlement of claim.
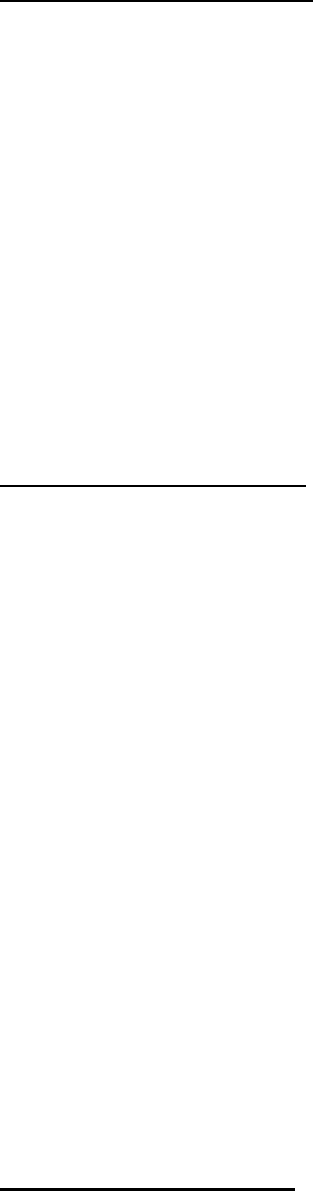
Contention of the complainant:
The complainant stated that:
(i) Based on the award by the Office of Insurance Ombudsman vide Ref. No.KOL-H-048-2021-0178, Award
Ref. No.IO/KOL/A/HI/0478/2020-2021, he expected that these claims will be admissible and requested
to the company for settlement of the claims.
(ii) He is following up regularly for the past several months but not getting any response from the Company.
(iii) The Complainant, during the course of hearing, submitted that his previous as well as the subsequent
similar claims have been settled. But these 3 claims lodged in between are repudiated.
Being aggrieved and dissatisfied with the non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) Mr. Ratan Lal Chajjer, 67 years male admitted in Tata Medical Centre for treatment of Adenocarcinoma
Prostate treated with ELIGARD DEPORT 22.5 MG injection which is also known as leuprolide which is a
manufactured version of a hormone used to treat prostate cancer.
(ii) It is given by injection into a muscle or under the skin. It is not a chemotherapy drug but used as Palliative
treatment to relieve pain or other symptoms Ellegard works by reducing the amount of testosterone in
patient’s blood. This helps to show or stop the growth of cancer cells and helps to relieve symptoms.
(iii) As patient was treated with hormonal therapy and given subcutaneous/intramuscular injection which is
not covered in day care standalone basis.
(iv) Hence, the claim is repudiated: “As per the submitted documents the member was treated for non-
conventional chemotherapy which is not covered as a day care procedure. Hence claim stands rejected
as per Appendix I of NIC – Mediclaim Policy – 2013 conditions”.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A, (d) Self Contained Note
from the insurer.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record and since the treatment is equal with the
chemotherapy and the disease is not excluded under the policy, repudiation of the claims is not justified.
In view of the above, the Insurer’s repudiation is set aside and the Insurance Company is directed to admit the
claims and pay the amount of Rs.94,686/- to the Complainant towards full and final settlement of the claim
subject to deductions, limitations, cappings, non-payables, Co-payment (if any) as per Policy Terms &
Conditions.
Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of the
Insurance Ombudsman Rules-2017:
(g) As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of
the receipt of the AWARD and shall intimate the compliance to the Ombudsman.
(h) As per the Rule 17(7), the Complainant shall be entitled to such interest at a rate per annum as specified in
the regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date of the claim ought to have been settled under the regulations, till the date of payment of amount
awarded by the Ombudsman.
(i) As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be binding on the Insurers.
Dated at Kolkata on the 17
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Dipak Kumar Singh
VS
Respondent : ManipalCigna Health Insurance Company Limited
COMPLAINT REF NO: KOL-H-053-2122-0212
AWARD NO:IO/KOL/A /HI/ 0230 / 2021-2022
1.
Name & Address of the Complainant
Mr. Dipak Kumar Singh
36B, Shakespeare Sarani, 3rd floor, Near Bhartiya Bhasha
Parisad, Kolkata - 700017.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
PROHLR010437288
10,00,00
21/06/2019
20/06/202
0
0
3.
Name of the insured
Mr. Dipak Kumar Singh
4.
Name of the insurer
ManipalCigna Health Insurance Company Limited
5.
Date of Receipt of the Complaint
14-Jul-2021
6.
Nature of Complaint
Repudiation of Claim
7.
Amount of Claim
Rs.4,90,000/-
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.4,90,000/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Dipak Kumar Singh
• For the insurer
Mr.
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021
Brief Facts of the Case:
Policy Name :: Manipal Cigna ProHealth Insurance Policy,
Policy Type :: Health Insurance,
Period of Insurance :: 21/06/2019 to 20/06/2020
Previous Policy :: 21/06/2017 (with this company & with the OIC since 2012),
Sum Insured :: Rs.10,00,000/- + Rs.5,00,000/- (CB),
Hospitalisation date/s::
04/11/2019 to 05/11/2019 Patient Shri Dipak Kumar Singh &
02/11/2019 to 09/11/2019 Patient Ms. Pooja Singh
The complainant lodged complaints against the Insurance Company in connection with repudiation of
hospitalisation claims. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) Claim No.22299022: Dipak Kumar Singh was admitted to Hospital for Chronic Tonsillitis on 04/11/2019.
He is having this policy since 21/06/2017 which was ported from Oriental and there was no waiting
period. But the claim was rejected on the grounds of DM, HTN & DNS and all the necessary documents
were submitted to the Company on time but they keep on asking the same papers again and again. None
of the ailments were there at the time of porting the policy.
(ii) ClaimNo.2299022: Pooja Singh was admitted to hospital for Dengue on 02/11/2019 and discharged on
09/11/2019. He is having this policy since 21/06/2017 which was ported from Oriental and there was no
waiting period. But the claim was rejected on the grounds of
2. “Why the patient couldn’t have been treated on OPD and in discharge summary no active line of
management, managed just with tablets”. His daughter’s condition was not good and Doctor had
strictly advised for hospitalisation and she had dengue so they have admitted her. Her platelets were
also dropping on a regular basis so she was admitted for a week.
3. “Requiring all past treatment details of CKD”
Her daughter was diagnosed with CKD in April 2019 and the ailments were not there at the time of
poting the policy. Doctor’s prescription certifying the same is sent to the company.

(iii) All the necessary documents were submitted to Manipal Cigna on time but they keep on asking the same
papers again and again.
(iv) The Complainant, during the course of hearing, submitted that all the papers have been submitted to
the Company and they have no other papers to submit. The CKD HTN of her daughter Puja Singh 1
st
detected in 2019 only and the certificate from Dr. S. Mukherji has been submitted.
Being aggrieved and dissatisfied with the Non-settlement of claims by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) On 22
nd
June, 2020 Complainant made a reimbursement claim bearing No. 22299022 (Annexure D) for
his hospitalization in Breach Candy Hospital, Mumbai from 04/11/2019 to 05/11/2019 due to Snoring
with Obstructive Sleep apnoea and underwent Uvulopalatoplasty. After due evaluation of the documents,
the Company requested the following documents to be submitted as it was crucial for adjudicating the
claim:
1. Require prenumbered cash paid receipt for the final Hospital bill (Note: Enclosed only receipts
of Rs. 234419/-).
2. Provide 1st & all previous consultation papers related to obstructive sleep disturbance, chronic
tonsillitis, DNS, and maxillary sinusitis.
3. Letter from treating doctor stating duration of Snoring with obstructive sleep disturbance,
chronic tonsillitis.
4. Recent photograph of policy holder.
Despite repeated requests dated 26
th
June, 2020, 7
th
July, 2020 and 21
st
August, 2020 (Annexure
E) the Complainant failed to provide the requested documents.
(ii) Therefore, the claim as per the policy terms and conditions and rejected the claim for non-submission of
required documents vide rejection letter dated 31
st
August, 2020
(iii) Further, on 13
th
June, 2020 the Complainant registered another reimbursement claim for the
hospitalization of his wife Pooja Singh in Woodlands Multispecialty Hospital due to dengue fever. After
due evaluation of the claim documents, the Company requested the Complainant to submit the following
documents which were crucial for adjudicating the claim:
“Require letter from treating doctor stating duration of CKD, HTN with first consultation paper.”
(iv) Despite repeated requests dated 19
th
June, 2020, 1
st
July, 2020,3
rd
August, 2020 the Complainant failed
to submit the required documents. Therefore, the Company was constrained to treat the claim as per
policy terms and conditions. Hence the claim was rejected for non-submission of claim documents
through rejection letter dated 27
th
September, 2020.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.

Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A & (d) Self Contained Note
from the insurer.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that
7. The repudiation of the Claim of Mr. D. K. Singh is in consonance with the policy issued to the
complainant.
Hence, the claim of Mr. D. K. Singh is dismissed without any relief.
8.
If the decision is not acceptable, the complainant is at liberty to approach any other
Forum/Court as per Law of the Land against the Respondent Insurer.
9. The Claim of Ms. Pooja Sing: The inception date of the policy is 26/05/2012 which was with the
Oriental Insurance Company and the policy was ported to Cigna TTK on 21/06/2017. The Cer-
tificate of Dr. S. Mukherjee states that the patient Ms. Pooja Singh, has been suffering from
HTN & CKD since 2019. Since, the Company has not conclusively proved that the HTN and CKD
diseases are existing prior to the inception of the policy, rejection of the claim is not justified.
In view of the above, the Insurer’s repudiation of the Claim of Ms. Pooja is set aside and the Insurance Company
is directed to admit the claim and settle the claim as per terms and conditions of the policy.
Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of the
Insurance Ombudsman Rules-2017:
(j) As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of
the receipt of the AWARD and shall intimate the compliance to the Ombudsman.
(k) As per the Rule 17(7), the Complainant shall be entitled to such interest at a rate per annum as specified in
the regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date of the claim ought to have been settled under the regulations, till the date of payment of amount
awarded by the Ombudsman.
(l) As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be binding on the Insurers.
Dated at Kolkata on the 17
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Anil Kothari
VS
Respondent : STAR HEALTH AND ALLIED INS. CO. LTD. (Kolkata)
COMPLAINT REF NO: KOL-H-044-2021-0581
AWARD NO:IO/KOL/A /HI/0242/ 2021-2022
1.
Name & Address of the Complainant
Mr. Anil Kothari
27/1A, Harish Mukherjee Road, 'Kuber Garden', Flat 5C,
Kolkata - 700025.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
P/191126/01/2020/006140
10,00,00
0
11/03/2020
10/03/202
1
3.
Name of the insured
Mr. Anil Kothari
4.
Name of the insurer
STAR HEALTH AND ALLIED INS. CO. LTD. (Kolkata)
5.
Date of Receipt of the Complaint
16-Mar-2021
6.
Nature of Complaint
Repudiation of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Not Quantified
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
27-September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Anil Kothari
• For the insurer
Ms. Sudeshna Bhattacharjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
30-Seotember-2021
Brief Facts of the Case:
Policy Name :: Senior Citizens Red Carpet Health Insurance Policy,
Policy Type :: Individual Mediclaim,
Period of Insurance :: 11/03/2020 to 10/03/2021,
Previous Insurance :: Since 11/03/2017,
Sum Insured :: Rs.10,00,000/-
Hospitalisation date/s:: 24/10/2020 to 30/10/2020.
The complainant lodged complaints against the Insurance Company in connection with repudiation of his
hospitalisation claim. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:

(i) Last year in the month of October, 2020, he was affected by Covid and was admitted to Samaritan Clinic
Pvt. Ltd, Kolkata.
(ii) He was in best of health and spirit but the pandemic took a heavy toll on his body and subsequently after
getting a blood report, he was affected by this virus and reported positive.
(iii) The company rejected the claim on the ground that he was affected by “COPD”.
(iv) Few years back there was Sleep Apnoea problem but with passage of time the said problem gradually
eradicated.
(v) With no rhyme or reason, they rejected his hospitalised expenses.
Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) The Insured took SENIOR CITIZEN RED CARPET POLICY covering Mr. Anil Kothari (SELF) [with declared
PED- diabetes &HTN and its complications and Mrs. Kashmira Kothari (SPOUSE) for a floater sum Insured
of Rs. 10,00,000/- w.e.f. 11-03-2017
(ii) From the submitted documents it was found that the Insured had past history of COPD. Hence query was
raised vide query letter dated 25-12-2020 requesting submission of the following documents.
II.Letter from the treating doctor stating the exact duration of COPD.
III. Copy of complete set of indoor case papers.
IV.First consultation and Investigation including the same.
(iii) The Insured submitted a letter from the treating doctor Mr. Chetan Gandhi which stated that the duration
of COPD is since last 3
1/2
years. Thus, further query was raised vide letter dated 23-01-2021 requesting
submission of:
I. As per submitted documents, it is mentioned as COPD since 3.5 years. Kindly submit all previous
documents of the same
II. First consultation papers and investigation reports including ECG, ECHO, PFT reports.
III. All previous documents taken before 3 years.
(iv) The Insured again submitted the same set of documents for the fresh query raised for submission of
documents relating to COPD to prudently access the exact duration of ailment for processing the claim,
but the Insured did not submit the required documents requisite by the company for processing the
claim.
(v) Thus, vide letter dated 17-02-2021 the Insured was communicated claim repudiation letter stating that,
“Although the present admission and treatment of the insured patient is for Covid positive, diabetes
mellitus, it is observed from the submitted medical records and the letter dated 04.01.2021 of the
above hospital that the insured patient is a known case of chronic obstructive pulmonary disease
(COPD) since 3 1/2 years. Hence, we requested the insured to furnish the treatment records of chronic
obstructive pulmonary disease. We note that you have not furnished the required documents and
details. In the absence of the above documents/details, we are not able to further process your claim.
As per Condition No. 5 (2) of the above policy, the insured person has to submit all the required
documents and details called for by us.”
(vi) As per condition no. 5(2) of the Policy issued to the Insured, “the Insured person shall obtain and furnish
the company with all original bills, receipts and other documents upon which a claim is based & shall
also give the Company such additional information and assistance as the Company may require in
dealing with the claim”
(vii) Thus, as the Insured have failed to submit the requisitted documents for the proper assessment of the
claim, the Insurer was constrained to repudiate the claim on grounds of non-submission of requested
documents.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A, (d) Self Contained Note
from the insurer, (e) Discharge Summery & (f) Repudiation Letter.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record and since the company has failed to prove
conclusively the pre-existence of the disease COPD at the time of inception of the policy, the Insurer’s
repudiation is set aside and the Insurance Company is directed to admit and settle the claim as per Policy Terms
& Conditions.
Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of the
Insurance Ombudsman Rules-2017:
(m)As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of
the receipt of the AWARD and shall intimate the compliance to the Ombudsman.
(n) As per the Rule 17(7), the Complainant shall be entitled to such interest at a rate per annum as specified in
the regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date of the claim ought to have been settled under the regulations, till the date of payment of amount
awarded by the Ombudsman.
(o) As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be binding on the Insurers.
Dated at Kolkata on the 30
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Anshuman Verma
VS
Respondent : STAR HEALTH AND ALLIED INS. CO. LTD.
COMPLAINT REF NO: KOL-H-044-2122-0273
AWARD NO:IO/KOL/A /HI/0245/ 2021-2022
1.
Name & Address of the Complainant
Mr. Anshuman Verma
Flat No. 103, Anikamal Apartment,, Bidhan Pally, Near
Gitanjali Metro, Kolkata - 700084.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
P/700002/01/2020/042226
5,00,000
06/01/2020
05/01/202
1
3.
Name of the insured
Mr. Anshuman Verma
4.
Name of the insurer
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of Receipt of the Complaint
17-Aug-2021
6.
Nature of Complaint
Repudiation of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Around Rs.41,000/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
27- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Anshuman Verma
• For the insurer
Ms. Sudeshna Bhattacharjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
-September-2021
Brief Facts of the Case:
Policy Name :: Star Comprehensive Insurance 2015,
Policy Type :: Health Insurance,
Period of Insurance :: 06/01/2020 to 05/01/2021
Previous Insurance :: Since 06/01/2019
Sum Insured :: Rs.5,00,000/-
Hospitalisation date/s:: 18/09/2020
The complainant lodged complaints against the Insurance Company in connection with repudiation of
hospitalisation claim of his spouse Mrs. Kahani. Hence, this complaint lodged with this office for settlement of
claim.
Contention of the complainant:
The complainant stated that:

(i) Claim Number.0600022 rejected on ground of policy has only completed 2 months rather than 24 months.
Also neck pain is not considered even if 24 hours hospitalisation get completed before 24 months.
(ii) In this pandemic time, it is hard and critical for arranging all necessary documents and declined his case
on multiple grounds and denied settlement.
(iii) The disease is not a neck pain or cervical, it was due to stiffening of muscle. It has been advised by
treating doctor to have physiotherapy for 30 days to release neck muscle tension.
(iv) Under extreme pain his wife got admitted, however the hospital failed to share all documents in covid
time. Entire set up got reshuffled at hospital. However, the most important part of i.e. the Dorctor’s
Certificate with seal he arranged and submitted
(v) He tried for discharge summary, however the efforts went in vain because of pandemic. Hence, it could
not be provided. Every day he is incurring Rs.700/- expenses due to his wife’s treatment which he is not
claiming. Till now total expenses is more than Rs.78,000/-. However, he has only claimed around
Rs.32,000/-.
(vi) His claim again rejected due the following reasons:
2. Less than 24 hours of hospitalisation happened: he has requested earlier and shared documents of
Doctor’s certificate. Further documents could not be completed.
3. Homeopathic treatment was also entertained: Ayush treatment is being covered under the Star Com-
prehensive Policy.
4. Since policy was under 24 months from the dated inception: Requested if not complete, partial set-
tlement could be initiated.
(vii) He has paid premium of Rs.1,86,213/- in last 3 years. Till now he has asked only asking around Rs.40,000/-.
Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) dated has stated that:
(i) The Insured Mrs. Kahani was treated for cervical Spondylosis at Dr. P. Banerjee’s homeopathic health care
center since 17-09-2020.
(ii) The Insured also went to the Dr. Debasish Adhikary for consulting regarding cervical Spondylosis.
(iii) There is no trace of Insured getting admitted or taking treatment as Outpatient or domiciliary
hospitalization. The Insured only went to the Doctors for consultation.
(iv) The above treatment taken does not at all fall under the coverage purview of the issued policy to the
Insured.
(v) The Insurer further noted that the Insured was having cervical Spondylosis which is not payable before
expiry of two years of continuous coverage.
(vi) Hence, repudiation letter was issued dated 29-03-2021 stating that, “It is observed from the submitted
medical records that the insured patient has undergone treatment for neck pain (cervical Spondylosis)
which is during second year of the policy. As per Exclusion - Specified disease/ procedure waiting
period- Code Excl.02 F of the above policy, expenses incurred by the insured person for treatment of
the above mentioned disease shall be excluded until the expiry of 24 months of continuous coverage
after the date of inception of the first policy with us.”
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A, (d) Self Contained Note
from the insurer & (e) Repudiation Letter.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the repudiation is in
consonance with the policy issued to the complainant.
Hence, the complaint is dismissed without any relief to the complaint.
If the decision is not acceptable to the Complainant, She/He is at liberty to approach any other Forum/Court
as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on the 30
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Subhash Chandra Panja
VS
Respondent : STAR HEALTH AND ALLIED INS. CO. LTD.
COMPLAINT REF NO: KOL-H-044-2122-0283
AWARD NO:IO/KOL/A /HI/0244/ 2021-2022
1.
Name & Address of the Complainant
Mr. Subhash Chandra Panja
S/o Dibakar Panja 6/1, Baghajatin Place, Baghajatin, Kolkata -
700086.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
P/191119/01/2020/008326
10,00,00
0
24/02/2020
23/02/202
1
3.
Name of the insured
Mr. Subhash Chandra Panja
4.
Name of the insurer
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of Receipt of the Complaint
16-Aug-2021
6.
Nature of Complaint
Non-settlement of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.48,855/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
27- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Subhash Chandra Panja
• For the insurer
Ms. Sudeshna Bhattacharjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
30-September-2021
Brief Facts of the Case:
Policy Name :: Family Health Optima Policy,
Policy Type :: Health Insurance,
Period of Insurance :: 24/02/2020 to 23/02/2021,
Previous Insurance :: Since 24/02/2018
Sum Insured :: Rs.10,00,000/-,
Hospitalisation date/s:: 13/10/2020 to 16/10/2020.
The complainant lodged complaints against the Insurance Company in connection with repudiation of
hospitalisation claim of Mrs. Moitree Roy. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) He has submitted all the relevant documents to the insurer for the settlement of claims.
(ii) The insurer responded him and claimed to submit (i) treating doctor letter stating exact duration of
Sequelae of Chronic Duodenal Ulcer, (ii) First and all consultation papers and (iii) complete set of indoor
case papers.
(iii) He submitted the same by taking a specific declaration from Dr. Asim Kumar Pal and other papers as
collected from hospital at the beginning. But the insurer continuously asking for the same.
Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) The Insured Mrs. Moitree Roy, aged 40 years old was admitted at Peerless Hospitex Hospital & research
centre limited from 13/10/2020 to 16/10/2020.
(ii) As per the Discharge Summary of the treating hospital, the insured was diagnosed with DUODENAL SCAR
(Sequelae of Chronic Duodenal Ulcer) and SUBACUTE INTERTEINAL OBSTRUCTION.
(iii) The Insured filed a pre-authorization request to avail cashless treatment vide request letter dated
14/10/2020.

(iv) On receipt of the request query was initiated from the end of the Insurer requesting the following
information:
• Exact diagnosis, Cause and Prior OPD consultation records taken
• Admission case sheet and progress notes
• All positive investigation reports supporting diagnosis. Previous history of hospitalization of similar ill-
ness in this patient. If so, provide its discharge summary.
(v) The Insurer on 15/10/2020 communicated the cashless denial letter stating that as per submitted
documents, the exact diagnosis not yet established and past treatment records related to endometriosis
and tuberculosis not provided, further evaluation required to ascertain exact onset of current ailment.
(vi) Subsequently, the Insured submitted a claim for reimbursement of medical expenses on 23/11/2020 for
a sum of Rs.50,490/-.
(vii) On scrutiny of the documents submitted, the Insurer further raised a query for submission of the
following documents vide Query letter dated 18/12/2020:
d) Kindly provide treating doctor letter stating exact duration of Sequelae of Chronic Duodenal Ulcer,
Endometriosis and cause for Subacute Intestinal Obstruction.
e) First and all consultation papers and investigation reports and treatment details pertaining to it.
f) Complete set of indoor case papers.
(viii) Further reminder letters dated 02/01/2021, 17/01/2021 and 01/02/2021 were sent to the Insured
requesting submission of the above documents required for admissibility of the above claim.
(ix) After several reminders also, the Insured failed to submit the above requested documents. Hence, the
Insurer communicated repudiation letter dated 01/02/2021 stating that despite sending several
reminders the requested documents were not submitted. Thus, they are unable to ascertain the
admissibility of the claim.
As per condition no. 2 of the Policy issued to the Insured, “The Insured person’s shall obtain
and furnish the company with all original bills, receipts and other documents upon which a
claim is based and shall also give the Company such additional information and assistance as
the Company may require in dealing with the claim.”
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A & (d) Self Contained Note
from the insurer.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the repudiation is in
consonance with the policy issued to the complainant.
Hence, the complaint is dismissed without any relief to the complaint.
If the decision is not acceptable to the Complainant, She/He is at liberty to approach any other Forum/Court
as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on the 30
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Subhash Chandra Panja
VS
Respondent : STAR HEALTH AND ALLIED INS. CO. LTD.
COMPLAINT REF NO: KOL-H-044-2122-0284
AWARD NO:IO/KOL/A /HI/0243/ 2021-2022
1.
Name & Address of the Complainant
Mr. Subhash Chandra Panja
S/o Dibakar Panja 6/1, Baghajatin Place, Baghajatin, Kolkata -
700086.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
P/191119/01/2020/008326,
CLI/2
10,00,00
0
24/02/2020
23/10/2021
3.
Name of the insured
Mr. Subhash Chandra Panja
4.
Name of the insurer
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of Receipt of the Complaint
16-Aug-2021
6.
Nature of Complaint
Repudiation of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.56,402/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
27- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Subhash Chandra Panja
• For the insurer
Ms. Sudeshna Bhattacharjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
30-September-2021
Brief Facts of the Case:
Policy Name :: Family Health Optima Policy,
Policy Type :: Health Insurance,
Period of Insurance :: 24/02/2020 to 23/02/2021,
Previous Insurance :: Since 24/02/2018

Sum Insured :: Rs.10,00,000/-,
Hospitalisation date/s:: 28/07/2020.
The complainant lodged complaints against the Insurance Company in connection with repudiation of
hospitalisation claim of Mrs. Moitree Roy. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) He has submitted all the documents for the settlement of claims which was raised for the JAW CYST
operation of his wife Mrs. Moitreye Roy.
(ii) The insurer responded him to submit Histopathological report for the same. He submitted the same by
taking a declaration from the dental surgeon, Dr. Sohel Ali.
(iii) He had talked to the company several time to settle it during COVID situation. But they are continuously
asking for the same.
Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) The Insured Mrs. Moitree Roy was admitted at KD Cure S.C. Das Memorial Medical and Research Centre
- Kolkata from 28/07/2020 to 29/07/2020 for treatment of Jaw cyst.
(ii) The Insured submitted for reimbursement of the medical expenses on 29/09/2020 for a sum of Rs.
56,402/-.
(iii) IOn receipt of all the documents it was noted that, “OPG shows recurrent dental caries in relation to
Upper Right molar teeth No 16 and Cyst is formed in periapical region of that tooth. Cyst in OPG
appears to be Radicular Cyst (Periapical Cyst). Doctor letter also states cystic lining was not conducive
to send for HPE. All these are typical of Radicular Cyst which arises due to cystic transformation of
infected and inflammed periapical tissue secondary to Dental Caries.”
(iv) It is evident from the above facts that the Insured availed treatment which resulted from recurrent dental
carries. Hence, it was treatment received for dental complication which is not payable under the terms
& conditions of the policy unless necessitated by accident as defined under Exclusion no. 32 of the Policy
issued to the Insured.
(v) As per Exclusion no. 32 of the Policy, issued to the Insured states that, “The Company is not liable to
make any payments under this policy in respect of any expenses what so ever incurred by the insured
person in connection with or in respect of Dental treatment or surgery unless necessitated due to
accidental injuries and requiring hospitalization. (Dental implants are not payable).”

(vi) Hence, based on above findings the Insurer conveyed the claim repudiation letter to the Insured dated
12/12/2020 stating that, “As per Exclusion - Code Excl 32 of the above policy, the Company is not liable to
make any payment in respect of any expenses for Dental treatment or surgery unless necessitated due to
accidental injuries and requiring hospitalization. (Dental implants are not payable).We are therefore
unable to settle your claim under the above policy and we hereby repudiate your claim. The above
decision has been taken as per the terms and conditions of the policy and based on the claim
details/documents submitted.”
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the
complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A & (d) Self Contained Note
from the insurer.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the repudiation is in
consonance with the policy issued to the complainant.
Hence, the complaint is dismissed without any relief to the complaint.
If the decision is not acceptable to the Complainant, She/He is at liberty to approach any other Forum/Court
as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on the _Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant : Mr. Susanta Kumar De
VS
Respondent : The Oriental Insurance Co. Ltd. (Kolkata)
COMPLAINT REF NO: KOL-H-050-2122-0291
AWARD NO:IO/KOL/A /HI/0246 / 2021-2022
1.
Name & Address of the Complainant
Mr. Susanta Kumar De,
8/6, North Purbachal, Kalitala Link Road, Kolkata - 700078.
2.
Type of Policy: Individual Mediclaim
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
311400/48/2021/7305
2,00,000
26/09/2020
25/09/202
1
3.
Name of the insured
Mr. Susanta Kumar De
4.
Name of the insurer
The Oriental Insurance Co. Ltd. (Kolkata)
5.
Date of Receipt of the Complaint
24-Aug-2021
6.
Nature of Complaint
Partial Settlement of Claim
7.
Amount of Claim
Rs.97,004/-
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.46,255/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
27- September-2021
Kolkata
12.
Representation at the hearing
• For the Complainant
Mr. Susanta Kumar De
• For the insurer
Mr.
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
30-September-2021
Brief Facts of the Case:
Policy Name :: Happy Family Floater Policy
Policy Type :: Health Insurance,
Period of Insurance :: 26/09/2020 to 25/09/2021
Sum Insured :: Rs.2,00,000/-
Hospitalisation date/s:: 30/04/2021 to 07/05/2021
The complainant lodged complaints against the Insurance Company in connection with partial settlement of his
hospitalisation claim. Hence, this complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) At the time of discharge from hospital, out of total Hospital Expenses of Rs.97,004/- the TPA Medi Assist
approved only Rs.46,706/- and he had to pay the balance amount of Rs.46,255/-
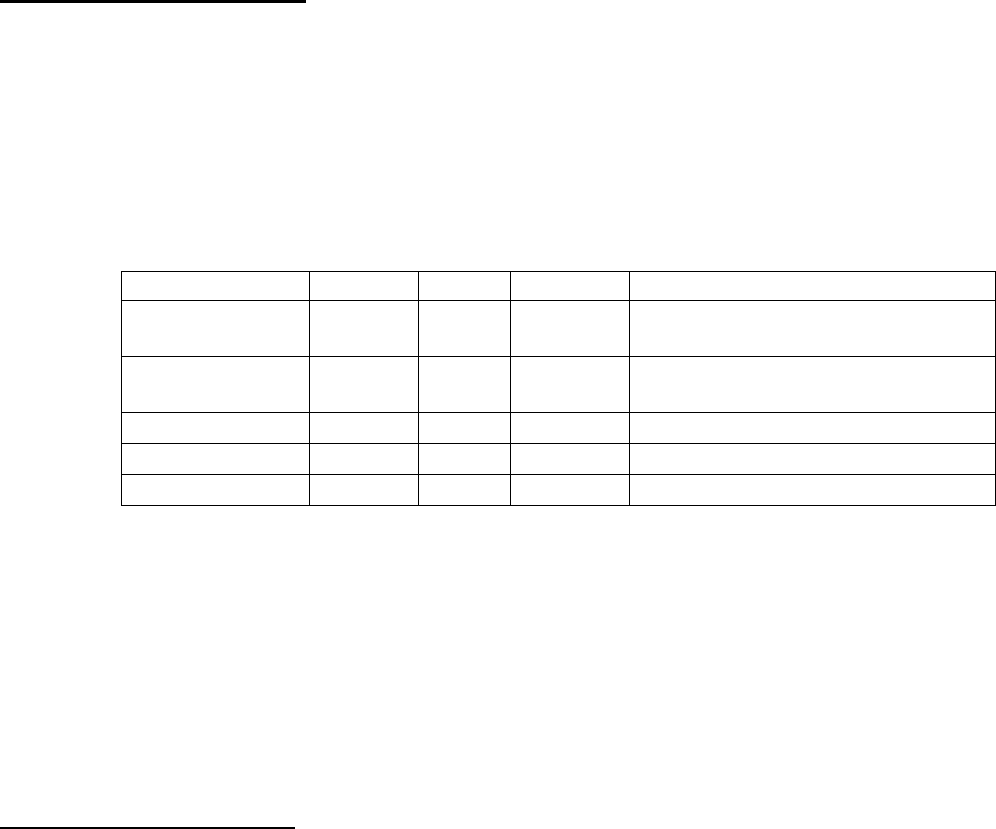
(ii) The TPA informed him that since sum insured of the policy is Rs.2,00,000/- eligible for room rent up to
1% i.e. Rs.2,000/- per day and as he had availed room rent of Rs.4,000/- per day, all other expenses had
been deducted proportionate basis.
(iii) Since his physical condition was serious, doctor advised for immediate hospitalisation. His wife tried to
admit him in Beliaghata ID, Bangur Hospital, Genesis, Desun, Ruby Hospitl but failed due to
nonavailability of bed. Ultimately, they have taken a general bed in Peerless hospital. At the time of
admission in hospital, COVID was so crucial, there was no bed even in government or private hospitals.
Being aggrieved and dissatisfied with the Partial-settlement of claim by the Insurance Company, the complainant
has approached this office for redressal of his grievance. The complainant has also given his unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself and the insurance
company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(iv) As the patient was eligible for 2% of Sum insured as room rent (upto Rs.2,000/- per day as per eligibility),
the patient availed higher (Rs.4,000/-) bed category of room which has resulted in application of Propor-
tionate deduction or Rs.41,066/-: -
Claimed Amount :: Rs.97,004/-
Approved Amount :: Rs.46,706/-
Non-payable Amount :: Rs.41,066/-
Co-Payment 10% :: Rs.5,189/-
Hospital Discount :: Rs.4,063/-
Charges
Claimed
Settled
Deducted
Deduction Reasons
Medicines Drugs
9854
6063
3791
Mask, gloves, gown etc. for
Rs.3,791/-
Consultation/
Visit
6300
3150
3150
Proportionate to HR limit
Miscellaneous
5600
5100
500
Initial assessment charges
Pathology
39250
19625
19625
Proportionate to HR limit
Room Rent
28000
14000
14000
Excess of Room Rent
(ii) The Tariff of Peerless Hospital & B. K. Roy Research Centre has proportionate link t other expenses with
their Room / bed charges and the Bill is charged accordingly.
(v) In view of the above the above proportionate clause was applied and the claim was settled for lesser
amount after adjustment complying with the IRDA Circular IRDA/HLT/REG/CIR/150/07/2016 dated 29
th
July 2016 and IRDAI/HLT/REG/CIR/151/06/2020 dated 11
th
June 2020.
(vi) The representative of the insurance company, during the course of hearing, submitted that the miscella-
neous expenses Rs.500/- deducted is the cost of PPE kit.
The Insurance Company has also given their consent to the Insurance Ombudsman to act as a mediator
between the Complainant and themselves and to give his recommendation for the resolution of the complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A & (d) Self Contained Note
from the insurer.
AWARD
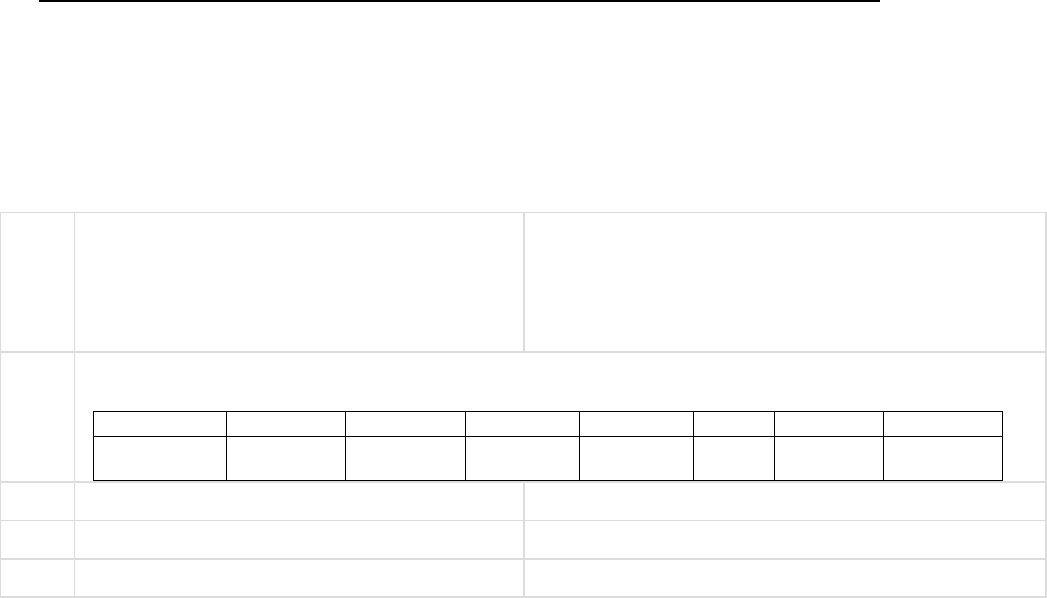
Taking into account the facts & circumstances of the case and the submissions made by both the parties during
the course of hearing & after going through the documents on record it is observed that the settlement of the
claim is in order except the deduction of Rs.500/- towards the cost of PPE Kit.
In view of the above, the Insurance Company is directed to pay an amount of Rs.500/- to the Complainant
towards full and final settlement of the claim.
Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of the
Insurance Ombudsman Rules-2017:
(p) As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of
the receipt of the AWARD and shall intimate the compliance to the Ombudsman.
(q) As per the Rule 17(7), the Complainant shall be entitled to such interest at a rate per annum as specified in
the regulations framed under the Insurance Regulatory and Development Authority of India Act 1999, from
the date of the claim ought to have been settled under the regulations, till the date of payment of amount
awarded by the Ombudsman.
(r) As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be binding on the Insurers.
Dated at Kolkata on the 30
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: Shri P.K. RATH
CASE OF COMPLAINANT – JUGAL KISHOR TAPARIA
VS
RESPONDENT: MANIPAL CIGNA HEALTH INSURANCE CO LTD
COMPLAINT REF: NO: KOL-H-053-2122-0224
AWARD NO: IO/KOL/A/HI/0238/2021-2022
1.
Name & Address of The Complainant
Jugal Kishor Taparia
C/o.Abhishek Kothari
Vandana Apartment Flat 705
22/1 Alipore Road, Kolkata 700027
[9163969999]
2.
Type Of Policy: Life / Health / General
Policy Details: FAMILY FLOATER
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
PROHLR9800
85514
450000
8.6.2020
7.6.2021
8.6.2018
30157
3.
Name of insured
Jugal Kishor Taparia
4.
Name of the insurer
MANIPAL CIGNA HEALTH INSURANCE CO LTD
5.
Date of receipt of the Complaint
29-July-2021
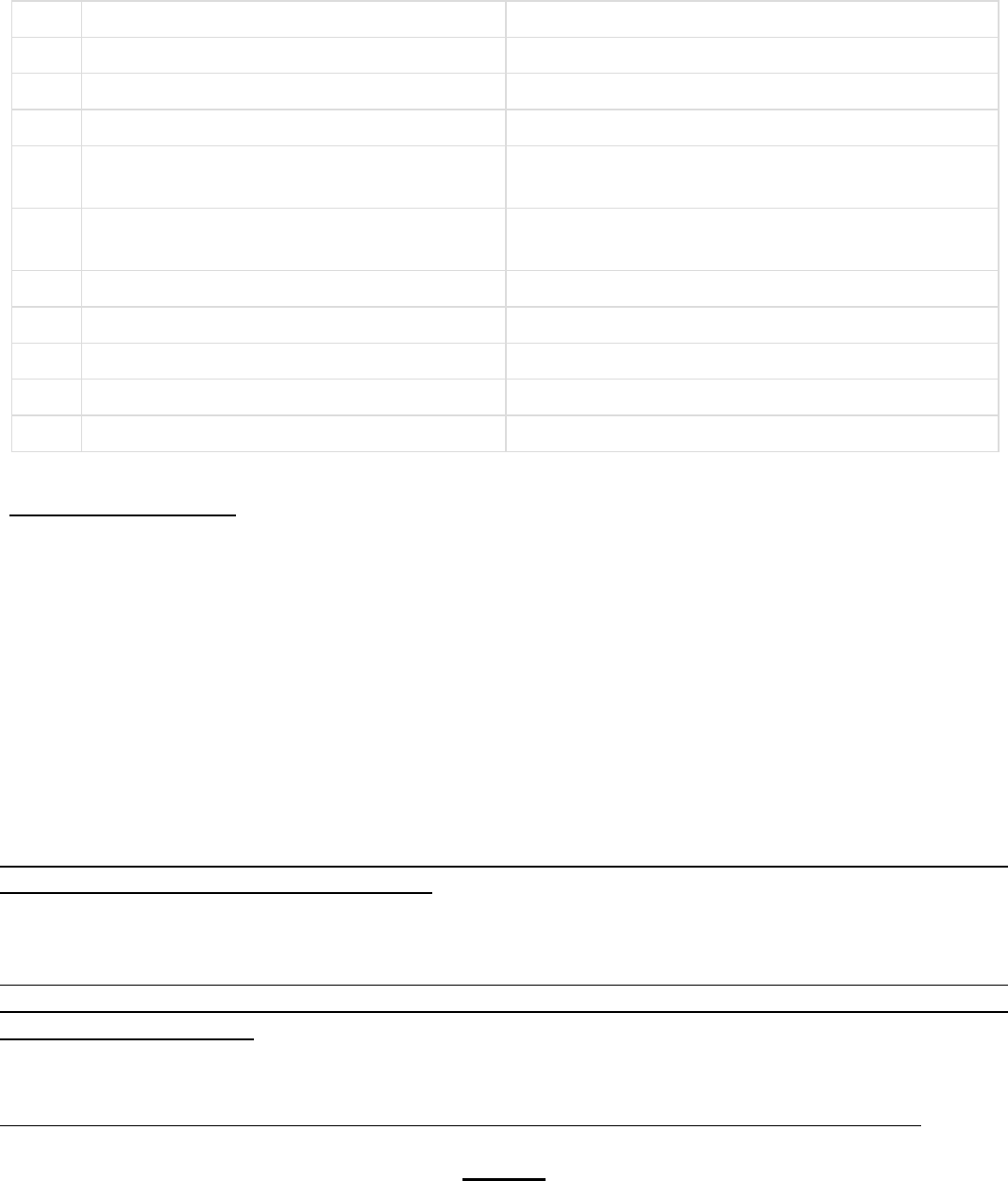
6.
Nature of Complaint
7.
Amount of Claim
52527.00
8.
Date of Partial Settlement
9.
Amount of relief sought
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
13(1)(b)
11.
Date of hearing
Place of hearing
22 September-2021
Kolkata
12.
Representation at the hearing
a) For the Complainant
Jugal KishorTaparia
b) For the Insurer
Swetha Nair
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
28-September-2021
Brief Facts of the Case: Smt Gayatri Taparia, wife of the Complainant was hospitalized at Jeevan Raksha
Hospital at Bikanir, Rajasthan she was hospitalized during 30.10.2020 to 03.11.2020 with the ailment Pneumonia
and submitted bill for hospitalization expense including pre-& post-hospitalisaion which was 52527/-.
Reimbursement of Claim denied by the Insurance Co. considering fraudulent as they have noted multiple
discrepancies on hospitalization documents.
Contention of the complainant: The claim has been repudiated stating Fraudulent but they are not giving any
reply specifying what type of fraudulent it was.
Contention of the Respondent: On verification of the case and hospital documents it is noted by them that
there is multiple discrepancies, therefore, genuinity of the claim not established and as such the claim has been
denied as per Clause VIII.19
Observation and conclusions: It is observed that there is no Discharge Summary from the Hospital.
AWARD
Taking into account the fact & circumstances of the case and the submissions made by both the parties during
the course of hearing and after going through the documents on record it is observed that the claim was
repudiated by the Insurance co. having found multiple discrepancies in submitted documents which was detected
by them as fraudulent in nature. Since the fraud does not come under the purview of the Office of Insurance
Ombudsman, the complaint is treated as closed as this end. However, the Complainant is at liberty to approach
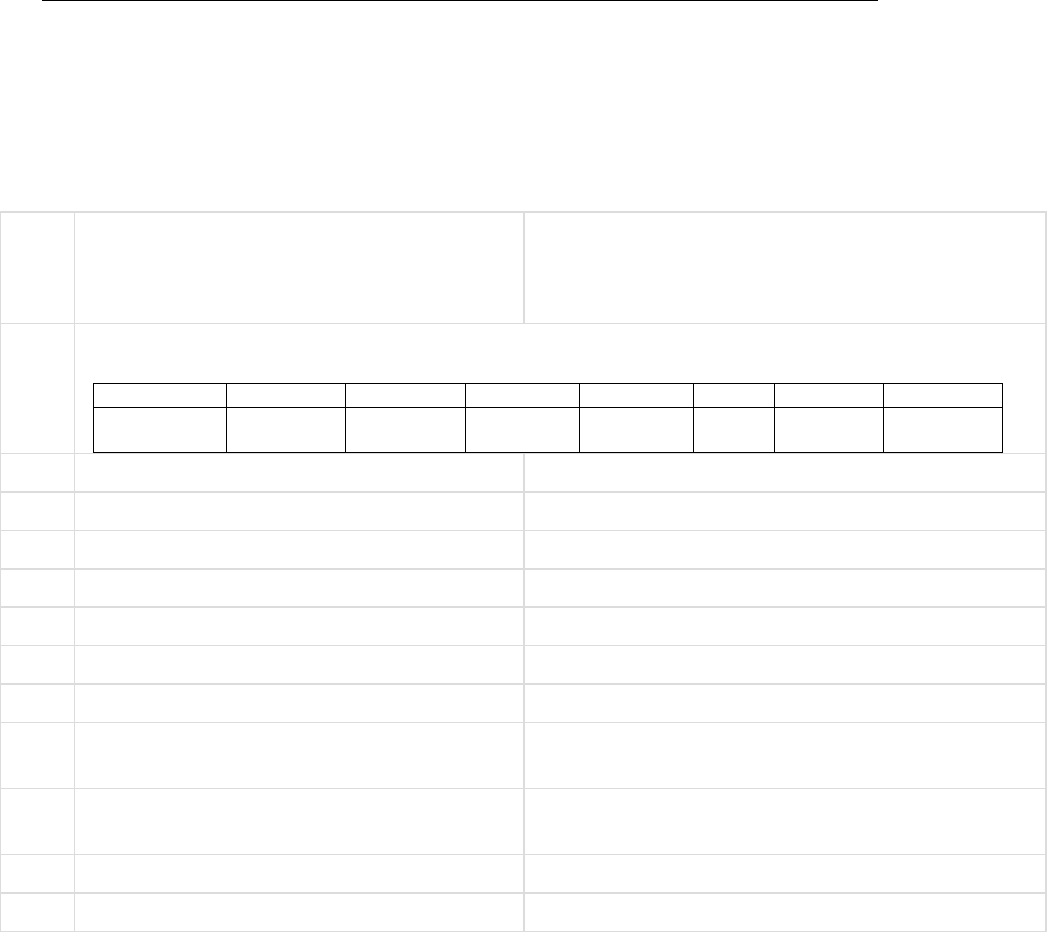
any other Forum/Court as per the Law of the Land.
The subject complaint is therefore dismissed without any relief to the Complainant. The complaint of the
complainant is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017:
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
award and intimate compliance of the same to the Ombudsman.
Dated at Kolkata on 28th Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: Shri P.K. RATH
CASE OF COMPLAINANT – Kishan Lal Agarwal
VS
RESPONDENT: STAR HEALTH & ALLIED INSURANCE
COMPLAINT REF: NO: KOL-H-044-2122-0264
AWARD NO: IO/KOL/A/HI/0237/2021-2022
1.
Name & Address of The Complainant
Kishan Lal Agarwal
36E Charu Avenue
Kokata - 700033
[9831472695]
2.
Type Of Policy: Life / Health / General
Policy Details: SUPER TOP UP POLICY
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/70004/01/
2021/001551
1000000
21.5.2020
20.5.2021
3.
Name of insured
Kishan Lal Agarwal
4.
Name of the insurer
STAR HEALTH & ALLIED INSURANCE & Co. Ltd.
5.
Date of receipt of the Complaint
11-August-2021
6.
Nature of Complaint
Non-settlement of Claim and Exclusion of Name
7.
Amount of Claim
4,11,900-
8.
Date of Partial Settlement
9.
Amount of relief sought
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
13(1)(b)
11.
Date of hearing
Place of hearing
22 September-2021
Kolkata
12.
Representation at the hearing
a) For the Complainant
Kishan Lal Agarwal
b) For the Insurer
Sudeshna Bhattacharyya
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
28-September-2021
Brief Facts of the Case: The Complainant is a patient of CKD. His basic policy is with HDFC. He is having
a Super Top up Policy for Rs. 10 lacs with Star Health and Allied Insurance Co. Ltd. since 21.5.2019. The policy
is renewed continuously but the Complainant’s name has been excluded in the policy commencing from
21.5.2021. His earlier claim was Awarded on 29
th
April 2021 in his favour for a sum of Rs.40,049 utilising his
super top up policy for period FROM 21.5.2020 to 20.5.2021.
A Claim for a sum of Rs.4,11,899.90 is lying pending during the same policy period from 21.5.2020 to
20.5.2021 for Dialysis and Covid 19 and follow up case of Covid 19.
Contention of the complainant: It is not understood why his name has been excluded from the policy at
renewal. A claim is still pending for Rs. 4,11,899/-
Contention of the Respondent: He is a patient of chronic kidney disease since 5.2.2017 when he was admitted
at N G Nursing Home. His basic policy was with HDFC ERGO since long. He has taken the Super Top Up policy
with us for the first time on 21.5.2019 through online. While taking the policy his CKD was pre-existing. Upon
gathering such information his claim was denied for non-disclosure of material fact and his name has been
excluded from the policy at current renewal.
Observation and conclusions: It is observed from the submitted documents [claim process sheet of HDFC
ERGO] that he was suffering from chronic kidney disease with DM since 2017.
AWARD
Taking into account the fact & circumstances of the case and the submissions made by both the parties during
the course of hearing and after going through the documents on record it is revealed that the decision of the
Insurer towards rejection of claim and also exclusion of his name from the policy due to non-disclosure of
material fact seems to be justified based on Policy Terms & Conditions.
The subject complaint is therefore dismissed without any relief to the Complainant. With this the complaint is
closed without further reference. The complaint of the complainant is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017:
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt
of the award and intimate compliance of the same to the Ombudsman.
If the decision is not acceptable to complainant, he is at liberty to approach any other Forum/Court of the
Land against the respondent insurer.
Dated at Kolkata on 28
th
Day of September, 2021 SHRI P K RATH
INSURANCE
OMBUDSMAN
KOLKATA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – AJAY AGARWAL
VS
RESPONDENT: NIVA BUPA HEALTH INS.CO.LTD.
COMPLAINT REF: NO: KOL-H-031-2122-0240
AWARD NO:IO/KOL/A/HI/0218/2021-2022
1.
Name & Address Of The Complainant
Mr.Ajay Agarwal
18, Bedia Danga 1t lane
Tiljala, Kolkata - 700039
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
3129747720
2000
500000
27.07.2020
26.07.2021
14,916/-
Annual
annual
3.
Name of insured
Mr.Ajay Agarwal
4.
Name of the insurer
Niva Bupa Health Insurance Co.Ltd.
5.
Date of Repudiation
12.06.2021
6.
Reason for Repudiation
COVID 19 home quarantine- hospitalization not re-
quired.
7.
Date of receipt of the Complaint
04-Aug-2021
8.
Nature of Complaint
Dissatisfied with Repudiation
9.
Amount of Claim
1,36,094.00
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
1,36,094.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
IOR 13(1)(b) – any partial or total repudiation of
claim by insurer
13.
Date of hearing
Place of hearing
09-Sept-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Mr.Ajay Agarwal
b)For the Insurer
Mr.Bhuwan Bhasker
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
15-September-2021
17. Brief Facts of the Case:
• The complainant had taken a Health Insurance Policy from Niva Bupa Health Ins.Co.Ltd. as per details
above.
• The Insured was suffering from high fever, cough, breathlessness so in consultation with the doctor he
was advised medication. The RT PCR test confirmed COVID positive and Doctors advice was admitted
in Purnam Medicare nursing home on 10.04.2021. He was discharged on 16.04.2021.
• The Insured submitted all the hospital documents for reimbursement of the expenses of Rs.1,36,094/-
to the Insurance Company.
• The Insurance company have repudiated the claim on 12.06.2021 on the grounds that the patients
vitals were stable and investigation reports were within normal limits. Hence as per the guidelines of
AIIMS, New Delhi and Ministry of Health and Family Welfare, Govt. of India, patient with mild sympto-
matic required only self-isolation by home quarantine.
• The Insured being aggrieved with the repudiation has approached The Ombudsman for remuneration.
18. Contention of the complainant: The Complainant having been tested Positive was admitted in hospital
for treatment of COVID-19. The patient was administered with Remdesivir. The Insurer repudiated the claim
on grounds that mild symptomatic patient can be treated by home quarantine and hospitalization not required.
The complainant wants full reimbursement of his hospital bill.
19. Contention of the Respondent: AS per SCN submitted the Respondent states that the hospital documents
and vital stats shows the patient was mild symptomatic with COVID19 having 98% SpO2 saturation in room air
and Temperature was Normal which does not attribute to hospitalization. The treatment administered was
very basic. There was no active line of treatment. The patients does not fall under Category which requires
hospitalization as per AIIMS and Ministry of Health and Family Welfare guidelines. They are of the opinion that
the patient could have home quarantined and the treatment could have been given to him at home. Hospital-
isation was not necessary and hence they have repudiated the claim.
20. Observation and conclusions: The Hearing was scheduled on 09.09.2021 and both the parties were
present for the same. The complainant reiterated that as per Doctor’s advice he was admitted in the hospital
for treatment of Corona. The RT PCR test and the CT Scan confirmed the patient was COVID positive. A total
of 6 nos. Remdesivir injection was also administered to him.
AWARD
Taking into account the facts and circumstances of the case, the submissions made during the hearing and
on perusal of all the documents submitted , it is confirmed that the complainant was suffering from
COVID-19 which is confirmed by the RT PCR Test and CT Scan and was admitted in hospital as per advice
of the doctor. He was treated by administration of Inj.Remdesivir which cannot be given in home
quarantine. The Respondent’s claim that the complainant was given conservative treatment for which
hospitalization not required is not justified. In view of the above, this claim is admitted and the Niva Bupa
Health Insurance Company is directed to settle the claim as per policy terms and conditions alongwith
interest as per Rule 17(7) of Insurance Ombudsman Rule, 2017.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on 15
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – MR.RATHIN DAS
VS
RESPONDENT: STAR HEALTH AND ALLIED INS.CO.LTD.
COMPLAINT REF: NO: KOL-H-044-2122-
0233
AWARD NO:IO/KOL/A/HI/0233/2021-2022
1.
Name & Address Of The Complainant
Mr.Rathin Das
Karbala Road, Vivekananda Pally
|Chinchura, Hooghly - 712103
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
P/191142/01
/2021/00073
7
1000000
08.07.2020
07.07.2021
26001/
-
Annual
Annual
3.
Name of insured
Mr.Rathin Das
4.
Name of the insurer
Star Health and allied Ins.co.ltd.
5.
Date of Repudiation
nm
6.
Reason for Repudiation
Partial payment
7.
Date of receipt of the Complaint
02-Aug-2021
8.
Nature of Complaint
Partial payment
9.
Amount of Claim
213690.00
10.
Date of Partial Settlement
nm
11.
Amount of relief sought
150000.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
IOR 13(1)(b) – any partial or total repudiation of
claim by insurer
13.
Date of hearing
Place of hearing
09-Sept-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Mr.Rathin Das
b)For the Insurer
Ms.Sudeshna Bhattacharjee
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
15-September-2021
17. Brief Facts of the Case:
• The complainant has a health policy for floater 10 lakhs as detailed above
• He was admitted to North City hospital from 18.11.2020 to 27.11.2020 for treatment of COVID 19
• He was misguided by agent and did not avail cashless but submitted documents for reimbursement of
his hospital bill.
• The TPA/Insurance company settled only partial amount against which the insured had represented to
Insurance co. but has received no response from them so he has approached OIO.
18. Contention of the complainant: The complainant is aggrieved for not getting cashless facility. Also the
reimbursed amount is less than half of his total hospital bill. The Insurance co. has not given any clarification
towards the deductions made against his claim.
19. Contention of the Respondent: As per SCN submitted the insurer clarifies that they have settled the
claim for an amount of Rs.1,89,283/- against a total bill of Rs.2,29,046/-. The deductions of Rs.74,760/- are
against reasonable and customy charges, Dengue, IGM, NSI, Covid test, Procalcitonin, Dimer, Ferritin, CRP, IL-
6 and Glocose fasting, Non medical items and Misc expenses(Service charge etc) not payable. The deductions
are as per Covid rates prevailing price fixed by state govt.
20. Observation and conclusions: The complainant and the Respondent were present for the hearing on
09.09.2021. The complainant has confirmed receipt of the balance payment towards his claim and has with-
drawn the claim.
AWARD
The Complainant has confirmed receipt of balance payment from the Insurance Company against his said
claim and has therefore withdrawn his claim. As such , the case is CLOSED.
Dated at Kolkata on 15
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – SMT.ANKANA BAL
VS
RESPONDENT: NATIONAL INSURANCE CO., RANAGHAT
COMPLAINT REF: NO: KOL-H-048-2122-0231
AWARD NO:IO/KOL/A/HI/0219/ 2021-2022
1.
Name & Address Of The Complainant
Ms.Ankana Bal
B-2/54, Kalyani, Dist-Nadia
Pin - 741235
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
154302/50/2
0/10000130
400000
16.05.2020
15.05.2021
8250/-
Annual
Annual
3.
Name of insured
Ms.Ankana Bal
4.
Name of the insurer
National Insurance, Ranaghat
5.
Date of Repudiation
6.
Reason for Repudiation
Partial payment
7.
Date of receipt of the Complaint
30-Jul-2021
8.
Nature of Complaint
Partial payment
9.
Amount of Claim
74757.00
10.
Date of Partial Settlement
20.04.2021
11.
Amount of relief sought
34398.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
IOR- 13(1)(b) – any partial or total repudiation of
claim by insurer
13.
Date of hearing
Place of hearing
09-Sept-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Mr.S. Bal (Father)
b)For the Insurer
Mr.Subhankar Barua
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
15-September-2021
17. Brief Facts of the Case:
• The complainant is holding a Mediclaim policy from National Insurance as detailed above.
• On 15.01.2021 she underwent Myomectomy surgery at Kalyani and was discharged on 18.02.2021.
• She submitted reimbursement claim for Rs.74757/- on 08.02.2021
• The TPA settled the claim for Rs.39965/- on 18.04.2021
• Being aggrieved at the settlement the complainant represented to insurance company but having re-
ceived no reply , she filed complaint with IRDA
• The Insurance co. responded with details of deductions made which is not acceptable by the insured
and hence she filed complaint to Ombudsman.
18. Contention of the complainant: Further to the above, the Insured states that the policy SI is Rs.400000/-
+ CB Rs.20000/- but Insurance company says SI restricted to Rs.300000/- under Clause 4.3 of Mediclaim policy.
She has raised query for the same. Also deduction of Rs.31900/- made for reasonable and customary clause
under 3.29 and Rs.8065/- against Pre and post. Again Rs.700./- disallowed for USG which beyond 30 days of
pre hospitalization. The insured clarifies that the report date is 23.12.2020 and she was admitted on
15.01.2021 which is within 30 days pre hospitalization period, hence should be payable.
19. Contention of the Respondent: As per SCN submitted the Insurance company confirms that they have
already released and amount of Rs.31900/- as per reasonable & customary clause 3.29 and another Rs.8065/-
for pre/post cost.
20. Observation and conclusions: The claimant and the respondent were present for the hearing on
09.09.2021 and they have both placed their contentions before the Honourable Ombudsman. It is observed
that the Insurance company has settled and paid an amount of Rs.39965/- against a total bill of Rs.74757/- as
per Clause 3.29 of the policy.
AWARD
Taking into consideration the facts and circumstances of the case, the contentions made by both the
parties and on perusal of the documents in our record, it is observed that the Complainant had raised a
bill of Rs.74757/- towards here hospitalization for Myomectomy. The Insurance Company has released a
payment of Rs.39,965/- in full and final as Reasonable and Customary charges which is in conjunction
with the policy terms and conditions. As such, the complaint does not merit consideration and the same
is dismissed without any relief to the complainant.
Dated at Kolkata on 15
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – SHARMITA SARKAR
VS
RESPONDENT: NEW INDIA, SARAT BOSE ROAD BRANCH
COMPLAINT REF: NO: KOL-H-049-2122-0199
AWARD NO:IO/KOL/A/HI/0220/2021-2022
1.
Name & Address Of The Complainant
Ms.Sharmita Sarkar
126/F, B.T.Road, Orchard-126
Flat No. 19A,
Kolkata- 700109
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
510601/34/20
/95/00000518
300000
13.09.2020
12.09.2021
5066
Annual
3.
Name of insured
Ms. Sharmita Sarkar
4.
Name of the insurer
The New India Assurance Co.Ltd.
5.
Date of Repudiation
02.02.2021
6.
Reason for Repudiation
Clause No.4.4.6
7.
Date of receipt of the Complaint
20-Jul-2021
8.
Nature of Complaint
Repudiation of claim for hospitalisation
9.
Amount of Claim
148478.00
10.
Date of Partial Settlement
11.
Amount of relief sought
148478.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
IOR 13 (1) (b)- any partial or total repudiation of
claim by insurer
13.
Date of hearing
Place of hearing
09- Sept-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Ms.Sharmita Sarkar
b)For the Insurer
Mr.Deb Kumar Bhattacharya
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
15-Sept-2021
17. Brief Facts of the Case:
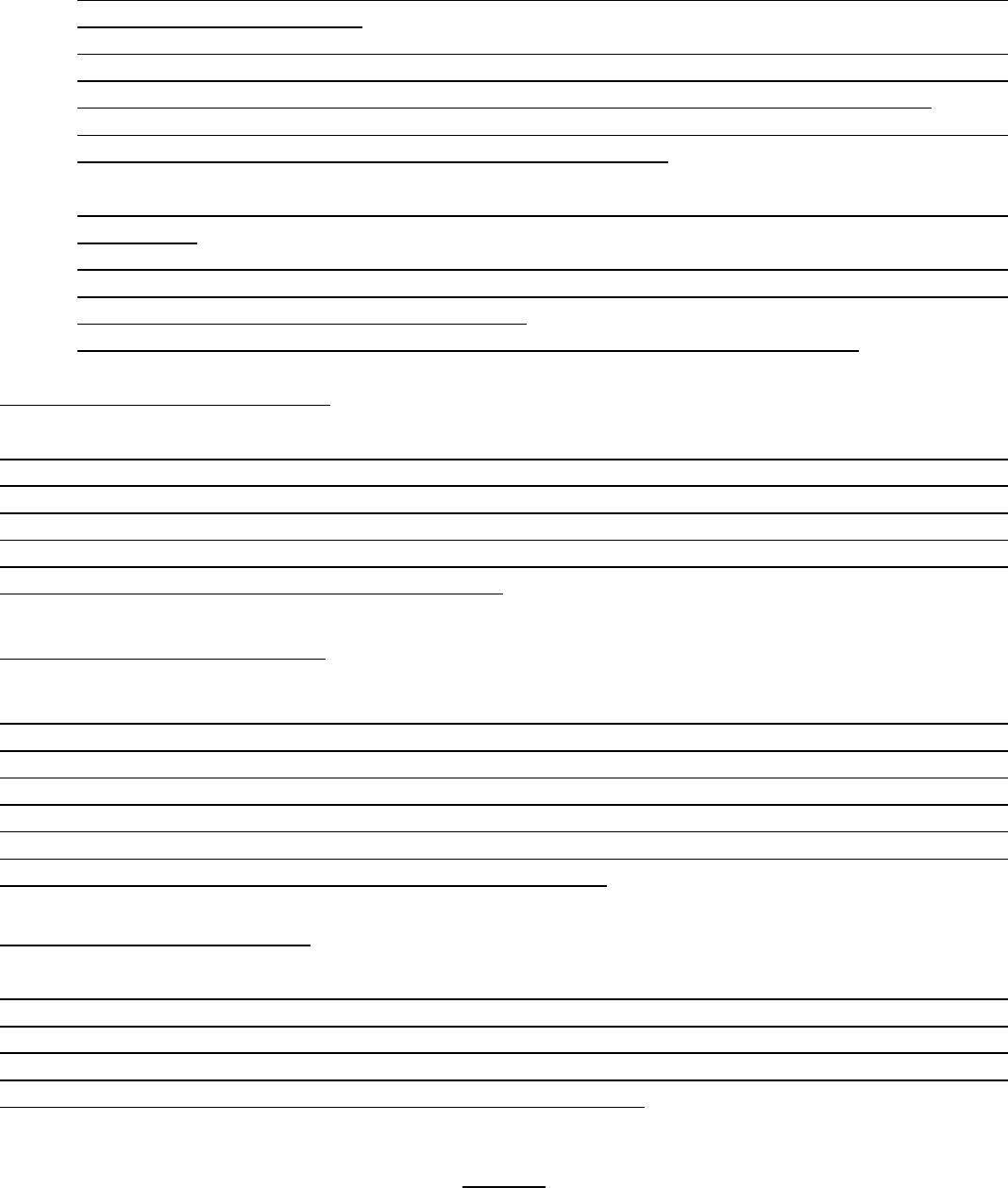
• The Complainant has a Mediclaim policy from New India, Sarat Bose Road Branch, Kolkata as per de-
tails mentioned in table above.
• That on 13.09.2020 the complainant was admitted in RSV Hospital Pvt.Ltd. for treatment of Bilateral
Chocolate Cyst with Bartholin’s cyst(Right) and was treated with Exploratory laparotomy, bilateral
ovarian cystectomy and marsupialization of Bartholin’s gland(right) was done on 14.09.2020.
• After discharge on 19.09.2020 ,the insured submitted all documents to NIA on 24.09.2020 for reim-
bursement of Rs.148478/- as per calculation summary attached.
• On perusal of documents the Insurance Company repudiated the claim under exclusion clause 4.4.6
of the policy.
• The Insured requested to reopen the claim file based on the opinion/clarification by the attending
doctor which states that the subject case was not related to treatment of infertility and hence the
mentioned clause for repudiation is not justified.
• The insured has now approached Insurance Ombudsman for settlement of her claim.
18. Contention of the complainant:
Further to the above the claimant has attached/submitted certificate from the attending doctor Dr.(Col)
J.K.Basu, MD, wherein he confirms that the patient came with history of painful menstruation and pain lower
abdomen for 6 months. She was a suspected case of endometriosis and treated accordingly. She was diag-
nosed with Bilateral Chocolate cyst and advised admission for exploratory laparotomy and has an uneventful
post-operative recovery. The doctor confirms that the patient did not complain of infertility and is nulliparous.
Hence, the claim cannot be rejected on these grounds.
19. Contention of the Respondent:
The Respondent in their SCN have confirmed the mediclaim policy with SI Rs.300000/- and CB Rs.75000/-. They
state that as per claim documents submitted the insured was admitted for primary infertility and the treatment
of infertility and sterility is excluded from the scope of the policy. They have supported their stands with copy
of the doctors prescription dated 08.09.2020. Hence, as per Policy Clause 4.4.6 which states “Convalescence,
general debility, ‘rum down’ condition or rest cure, any treatment relating to Obesity or psychiatric and psy-
chosomatic disorders, infertility, sterility, venereal disease, intentional self-injury and illness of injury caused
by the use of intoxicating drugs/alcohol”, the claim is not payable.
20. Observation and conclusions:
The hearing was scheduled on 09.09.2021 and both the complainant and the respondent were present for the
same. The Complainant was admitted in the hospital for treatment of Bilateral Chocolate Cyst and was given
Exploratory laparotomy, bilateral ovarian cystectomy and marsupialization of Bartholin’s gland(right) was
done. The hospitalization bill was claimed by the insurer for an amount of Rs.1,48,478/-. The Insurance Com-
pany has however, repudiated the claim as per Policy Clause No.4.4.6.
AWARD
Taking into consideration the facts and circumstances of the case, the submissions made during the
hearing and on perusal of the documents submitted on record, it is observed that the complainant
underwent treatment for Bilateral Chocolate Cyst and claimed reimbursement of Rs.1,48,478/-. The
Insurance company has repudiated the claim on grounds of the treatment was for infertility under Policy
Clause 4.4.6 which reads, “Convalescence, general debility, ‘run down’ condition or rest cure, any
treatment relating to Obesity or psychiatric and psychosomatic disorders, infertility, sterility, venereal
disease, intentional self-injury and illness of injury caused by the use of intoxicating drugs/alcohol”. The
Complainant has submitted certificate
by treating doctor who confirms that the treatment was not done for infertility. As such, it is substantiated
that the complainant was admitted for treatment of Bilateral Chocolate cyst which is not related to
infertility. Hence, the repudiation by the insurance company is set aside and The New India Assurance
Co.Ltd. is directed to admit the entire claim for Rs.1,48,478/- in favour of the complainant as per policy
terms and conditions alongwith interest as per Rule 17(7) of Insurance Ombudsman Rules, 2017.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on 15
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
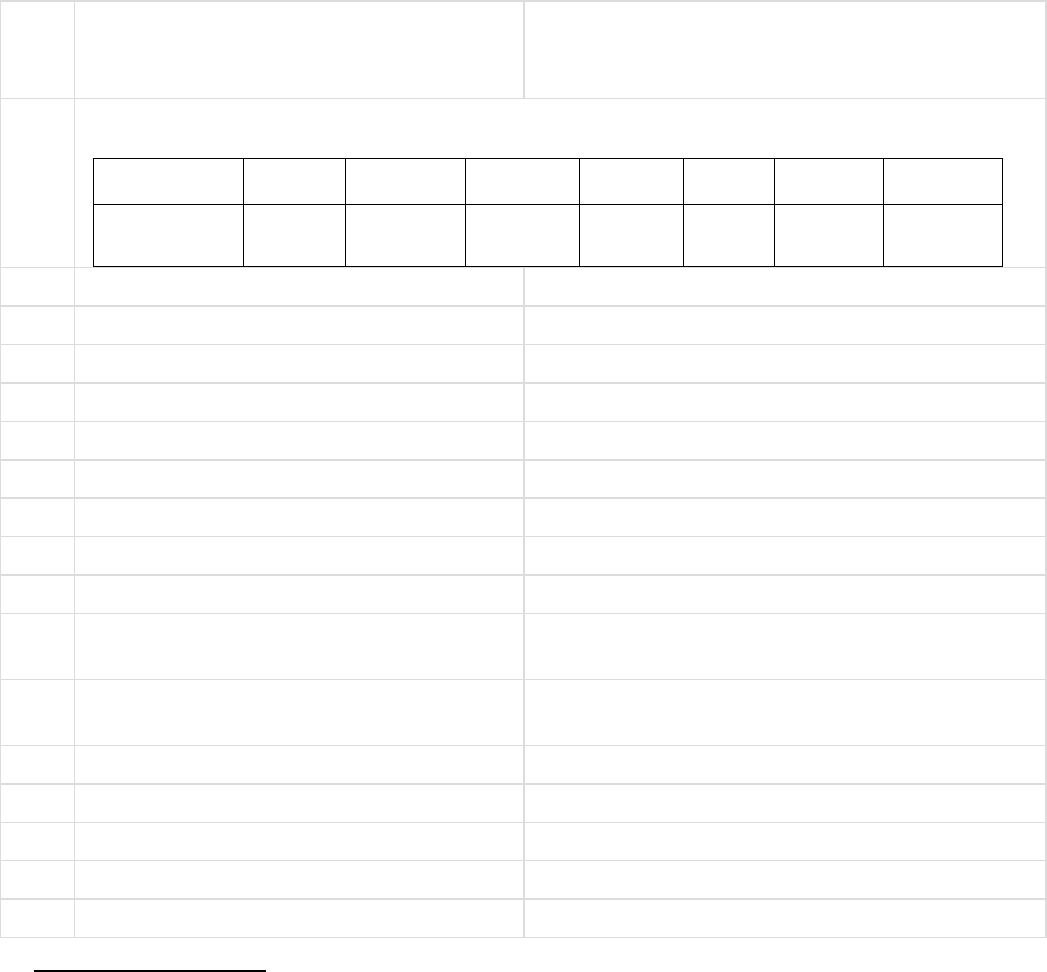
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – ARPAN KUMAR DAS
VS
RESPONDENT: NEW INDIA ASSURANCE CO.LTD.
COMPLAINT REF: NO: KOL-H-049-2122-0246
AWARD NO:IO/KOL/A/HI/0217/2021-2022
1.
Name & Address Of The Complainant
Mr.Arpan Kumar Das
P-1, Roynagar Place, Bansdroni
Kolkata - 700070
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
510100/34/20
/87/00000687
300000
29.07.2020
09.05.2021
7422/-
Annual
annual
3.
Name of insured
Mr.Arpan Kumar Das
4.
Name of the insurer
New India Assurance Co.Ltd.
5.
Date of Repudiation
Partial payment
6.
Reason for Repudiation
Deduction made for non-medical items etc.
7.
Date of receipt of the Complaint
05-Aug-2021
8.
Nature of Complaint
Dissatisfied with partial settlement
9.
Amount of Claim
162300.00
10.
Date of Partial Settlement
09.04.2021
11.
Amount of relief sought
44772.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
IOR 13(1)(b) – any partial or total repudiation of
claim by insurer
13.
Date of hearing
Place of hearing
09-Sept-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Mr.Arpan Kumar Das
b)For the Insurer
Mr.Kumar Kaish
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
15-September-2021
17. Brief Facts of the Case:
• The complainant had taken a Corona Kavachh Policy from New India Assurance as per details above.
• The Insured was diagnosed with COVID-19 and was admitted in hospital from 04.10.2020 to
11.10.2020
• The Insured submitted all the hospital documents for reimbursement of the expenses of Rs.1,62,300/-
to the Insurance Company.
• The Insurance company initially paid Rs.71584/- and then another Rs.48624/- against the total claim
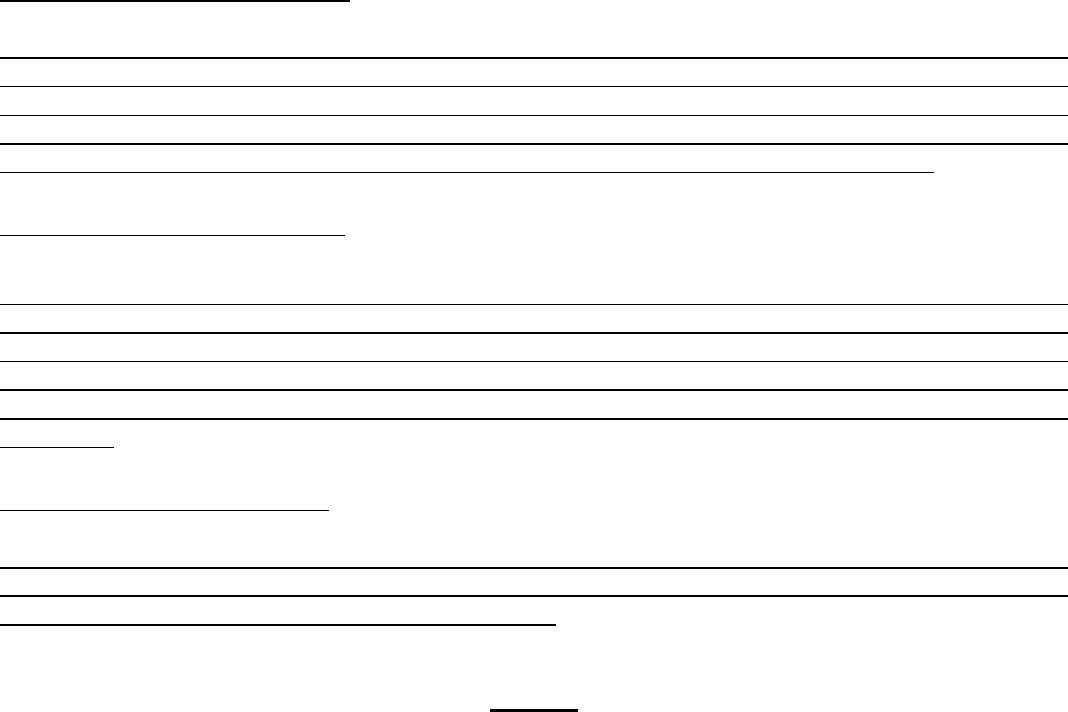
made by the Insured.
•
• The Insured being aggrieved with the partial reimbursement has approached The Ombudsman for re-
muneration.
18. Contention of the complainant:
The Complainant having been tested Positive was admitted in hospital for treatment of COVID-19. The Insurer
made partial payment against total bill of Rs.1.62 lakhs. The insured has raised query that deductions made
against pharmacy charges, medicines which were disallowed in first payment were partially allowed in the 2
nd
payment. Also all deductions made against PPE kit and N95 masks and equipment charges have been disal-
lowed even though raised in the bill by hospital. The insured finds these deductions unjustified.
19. Contention of the Respondent:
As per SCN submitted the Respondent states that the Pharmacy charges were disallowed as per GI circular and
these are included under the daily package rate. They have however paid an amount of Rs.48624/- in order to
close the grievance of the insured keeping in limit of the GI guidelines. Also, the hospital was under PPN and if
the insured had availed cashless then all expenses would have been covered but since the insured sought for
reimbursement the deductions have been made as per GI Council circular. The payment made is fair and
reasonable.
20. Observation and conclusions:
On scrutiny of all the documents it is observed that the Complainant had a Corona Kavachh Policy under which
the Insurance Company has settled and paid the claim for an amount of Rs.71,584/- and Rs.48,624/- , that is,
a total of Rs.1,20,208/- against Total Bill of Rs.1,62,300/-.
AWARD
Taking into account the facts and circumstances of the claim, the submissions made by both parties at the
time of hearing, and on perusal of all documents on record, it is observed that the Insurance Company
has already paid Rs.1,20,208/- to the Insured which is justified as per policy terms and conditions. Hence,
the complaint is dismissed without any relief to the complainant.
Dated at Kolkata on 15
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – DIPAK KR.BHATTACHARYYA
VS
RESPONDENT: NEW INDIA, B.O.510901
COMPLAINT REF: NO: KOL-H-049-2122-0255
AWARD NO:IO/KOL/R/HI/0221/2021-2022
1.
Name & Address Of The Complainant
Mr.Dipak Kr.Bhattacharya
609, Block-O, Godrej Prakriti
187F/1, B.T.Road, Sukchar
Kolkata- 800115
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum As-
sured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
510901/34/20
/16/00000081
1,50,000
08.03.2021
07.03.2022
8795.00
Annual
Annual
P/191135/01/
2021/009719
5,00,000
22.02.2021
21.02.2022
21240.00
Annual
Annual
3.
Name of insured
Dipak Kumar Bhattacharya
4.
Name of the insurer
The New India Assurance Co.Ltd.
5.
Date of Repudiation
6.
Reason for Repudiation
7.
Date of receipt of the Complaint
10-Aug-2021
8.
Nature of Complaint
Delay in claim settlement
9.
Amount of Claim
35100.00
10.
Date of Partial Settlement
11.
Amount of relief sought
13600.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
IOR 13 (1) (a) – delay in settlement of claim be-
yond the time specified in the regulations framed
under the IRDA Act, 1999
13.
Date of hearing
Place of hearing
09- Sept-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Mr.Dipak Kumar Bhattacharya
b)For the Insurer
Mr.Arijit Das
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
15-September-2021
17. Brief Facts of the Case:
• The Claimant has 2 nos. Health policies – one from New India and another from Star Health & Allied
Insurance Co.Ltd. ( details as in table above)
• The claimant underwent LE Cataract Phaco Surgery at Disha Eye Hospital, Barrackpore on 20.03.2021

and was discharged on the same day.
• Star Health settled cashless claim for Rs.21500/- to hospital against a Total Bill of Rs.35100/-.
• The claimant submitted all documents to NIA Dunlop branch on 05.04.2021 for reimbursement of bal-
ance Rs.13600/- but NIA did not respond.
• Again on 12.05.2021 claimant sent a reminder. In response NIA sent email on 13.05.2021 asking for
following documents – Original Final Bill from Hospital , Settlement certificate from Star health ; Rea-
son why Star Health did not pay balance amount of claim ; Provide certificate from TPA confirming no
Pre and post claim raised and confirmation of Sum Insured exhaustion ; provide all original documents
or certified from Star Health.
• New India is awaiting submission of above documents from Claimant.
• The Insured is aggrieved for undue requirement of documents and delay in settlement of claim by NIA
and so he has approached OIO for resolving the issue.
18. Contention of the complainant: The Claimant raises query why the total bill is required if only part
payment has to be made by NIA and original total bill submitted to Star Health. Lens implantation identification
card is not available with the claimant and due to pandemic the claimant cannot go to hospital to collect doc-
ument.
19. Contention of the Respondent: The Respondent in their SCN have confirmed receipt of claim documents
on 08.04.2021 for LE Cataract surgery at Disha Eye Hospital, Barrackpore. After scrutiny of all documents they
have raised query for the following papers from the insured and they are still awaiting reply from the Insured.
• Original Final Bill from Hospital
• Settlement certificate from Star health
• Reason why Star Health did not pay balance amount of claim ;
• Provide certificate from TPA confirming no Pre and post claim raised and confirmation of Sum Insured
exhaustion
• Provide all original documents or certified from Star Health.
20. Observation and conclusions: This is a contribution claim where Star Health & Allied Insurance Co.Ltd.
have settled major portion of the claim and paid Rs.21,500/- to the Insured. The balance of Rs.13,600/- is due
from New India Assurance. The respondent states that the claim may be settled on submission of the docu-
ments as already conveyed to the insured.
AWARD
Taking into account the facts and circumstances of the case, the submissions made by both the parties
and on perusal of the documents on record, it is observed that the claimant has already received Rs.21,500/-
from Star Health & Allied Insurance Co.Ltd. All originals have been submitted to Star Health & Allied
Insurance Co.Ltd. Hence, the complainant is directed to submit copies of Final Bill, and all related
hospitalization documents duly certified by Star Health & Allied Ins.Co.Ltd. alongwith Settlement
Certificate confirming all payments made and Sum Insured exhaustion from Star Health & Allied Ins.
Co.Ltd.
Dated at Kolkata on 15
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
Copy to: 1) Complainant: Mr.Dipak Kumar Bhattacharya
2) Company: The New India Assurance Co.Ltd.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – ARINDAM SEN
VS
RESPONDENT: THE ORIENTAL INSURANCE CO.LTD.
COMPLAINT REF: NO: KOL-H-050-2122-0189
AWARD NO:IO/KOL/A/HI/0222 /2021-2022
1.
Name & Address Of The Complainant
Mr. Arindam Sen
60/143, Haripada Dutta Lane
Golf Gardens, Kolkata - 700033
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
311604/48/2
019/2506
1000000
31.12.2018
30.12.2019
51057/-
Annual
311604/48/2
020/2604
1000000
31.12.2019
30.12.2020
51057/-
annual
3.
Name of insured
Mrs.Jean Sen
4.
Name of the insurer
The Oriental Insurance Co.Ltd.
5.
Date of Repudiation
18.02.2021
6.
Reason for Repudiation
PED – Clause 1.1 & 1.2 and 4.1
7.
Date of receipt of the Complaint
19-Jul-2021
8.
Nature of Complaint
Partial settlement of health claim
9.
Amount of Claim
5,67,344.00
10.
Date of Partial Settlement
11.
Amount of relief sought
4,97,507.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
IOR 13 (1) (b) – any partial or total repudiation of
claim by life insurer, general insurer or health in-
surer
13.
Date of hearing
Place of hearing
09-Sept-2021
Kolkata
14.
Representation at the hearing
a)For the Complainant
Mr.Arindam Sen
b)For the Insurer
Mr.K.Chandra Sekhar
15.
Complaint how disposed
By conducting online hearing
16.
Date of Award
15-September-2021
17. Brief Facts of the Case:
• The Insured was hospitalized on 3 occasions – 13.06.2019 to 27.06.2019 ; 29.12.2019 to 10.01.2020
and 23.02.2020 to 06.03.2020(expired)
• In the 1
st
hospitalization she was diagnosed with Bilateral Organizing Pneumonitis which aggravated to
Interstitial lung disease which led to the 2
nd
& 3
rd
hospitalization.

• The claim for 1
st
hospitalization was paid for Rs.37393/- bye TPA and Rs.49715/- paid by Claimant –
treatment for Bilateral organizing Pneumonitis.
• For the 2
nd
hospitalization at Fortis for treatment of DPLD, the TPA has paid Rs.69837/- against bill of
Rs.298720/-.
• For the 3
rd
claim, OIC repudiated stating that the Sum Insured of Rs.500000/- exhausted in earlier claim
and also 48 months PED exclusion clause 4.1 applicable as policy was migrated to Family Floater in
2017.
• The Insured had 2015-16 policy with 5 lacs sum insured and 1
st
claim triggered. The policy was mi-
grated to Family Floater at the time of renewal with SI Rs.8 Lacs without disclosure of B/L Organised
Pneunomitis. In 2017-18, the Sum Insured was again enhanced to Rs.10 lacs and existing till date.
• Since the insured had not disclosed PED , the enhancement of SI have not been considered and SI has been
taken as Rs.5 lacs only.
18. Contention of the complainant: The Complainant is claiming for balance payment of Rs.497507/- against
the subject 3 claims. The rejection of claim on grounds of PED is not acceptable by him since insured was
diagnosed with BLOP on the 1
st
admission in June 2019 and the discharge summary of Belle View states “No
Symptom related to past history”. Also 1
st
claim was settled by TPA which could not have been done in the
eventuality of PED. The claimant states that the diseases were not pre-existing and were diagnosed and treated
during her 1
st
hospitalization.
19. Contention of the Respondent: The insurer refers to medical certificate of Dr.Ghoshal of Fortis hospital
stating BLOP since 2016. The insured knowingly has enhanced SI to Rs. 10 lacs and migrated to Family floater
policy without disclosing PED, hence policy is Void. They took second opinion of Non TPA doctor who confirms
PED from June 2016. The Insured has manipulated documents of PED certificate violating principle of Utmost
good faith. The SI has also exhausted hence no further payment can be made against the claim. The claim is
not payable as per Operative clause no. 1.1, 1.2 & Exclusion Clause 4.1.
20. Observation and conclusions: The complainant had a health policy from The Oriental Insurance Co.Ltd.
having Sum Insured of Rs.5 lakhs in 2015. The Insured was diagnosed with Bilateral Organised Pneumonia in
June, 2016. The Insured subsequently enhanced Sum Insured under the policy every year to the current Sum
Insured of Rs.10 Lakhs. The insured was admitted in hospital on 3 occasions for DPLD. The Insurance company
has repudiated the claim on grounds of Pre-existing disease not declared under Operative clause 1.1 & 1.2
and Exclusion Clause 4.1.
AWARD
Taking into account the facts and circumstances of the case, the submissions made by the parties at the
Hearing, and on perusal of the documents on record, it is observed that the patient was suffering from
Lung disease since 2016 as has been certified by doctor. The Policy Sum Insured in consideration here
will be Rs.5 Lakhs since as per terms and conditions there is a 4 years waiting period for enhanced sum
insured. The Sum Insured of Rs.5 lakhs is already exhausted due to payment of the claims. Hence, the
complaint is dismissed without any relief to the complainant.
Dated at Kolkata on 15
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: Shri P.K.RATH
CASE OF COMPLAINANT – SANDIP SENGUPTA
VS
RESPONDENT: NATIONAL INSURANCE CO. LTD. DO XVI,
Kolkata
COMPLAINT REF: NO: KOL-H-048-2122-0263
AWARD NO: IO/KOL/A/HI/0240/2021-2022
1.
Name & Address of The Complainant
SANDIP SENGUPTA
67/A/2 Kendua Main Road
Kolkata 700084
[9830165694]
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
101900/50/2
0/10000046
250000 +
CB 75000
11.4.2020
10.4.2021
11.4.2005
38043/
-
Yly
3.
Name of insured
KASTURI SENGUPTA [55]
4.
Name of the insurer
National Insurance Co. Ltd
5.
Date of receipt of the Complaint
11 August-2021
6.
Nature of Complaint
Claim settled at a lesser amount
7.
Amount of Claim
124000.00
8.
Date of Partial Settlement
9.
Amount of relief sought
124000
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
13(1)(b)
11.
Date of hearing
Place of hearing
22 September-2021
Kolkata
12.
Representation at the hearing
a) For the Complainant
Sandip Sengupta
b) For the Insurer
Samir Saha
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
28-September-2021
Brief Facts of the Case: Smt Kasturi Sengupta, Wife of the Complainant had undergone surgery for Calculous
Cholecystitis SLE with APLA at Sri Arabinda Seva Kendra, a Non-PPN hospital and hospitalized during 6
th
December to 16
th
December 2020. Claimed for Rs.2,05,560/- including Pre- and Post-hospitalisation expenses
and settled by the Insurance Co. for Rs. 75991/- as per Operative Clause of the policy No. 3.29 - Reasonably
and Customary charges, hence this complaint. Policy is continuing since 11.4.2005.
Contention of the complainant: The way the TPA has settled the claim is a matter of concern. The said
hospital does not have any agreed rate for any listed procedure and charged the tariff rate of their own. Such
type of reimbursement causes huge financial loss and injustice to proper claim settlement.
Contention of the Respondent: As per SCN the claim was reimbursed as per PPN tariff for Cholecystectomy
surgery as per policy terms and condition under Clause No. 3.29 which is Reasonable and Customary charges
applied for a non-PPN hospital. Accordingly, the highest available rate of PPN tariff was paid in addition to pre-
& post-Hospitalisation expenses.
Observation and conclusions: It is observed that the said hospital is a non-PPN hospital. The following docu-
ments are available in the file a) Complaint letter with Annexure VI-A, b) Discharge Summary & hospital bill
from the Nursing Home, c) Self Contained Note. D) Policy copy.
AWARD
Taking into account the fact & circumstances of the case and the submissions made by both the parties during
the course of hearing and after going through the documents on record it is revealed as per the recorded
documents that the decision of the Insurer towards settlement of claim seems to be justified based on Policy
Terms & Conditions.
The subject complaint is therefore dismissed without any relief to the Complainant. With this the complaint is
closed without further reference. The complaint of the complainant is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017:
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt
of the award and intimate compliance of the same to the Ombudsman.
If the decision is not acceptable to complainant, he is at liberty to approach any other Forum/Court of the
Land against the respondent insurer.
Dated at Kolkata on 28th Day of September, 2021 P K RATH
INSURANCE OMBUDSMAN
KOLKATA
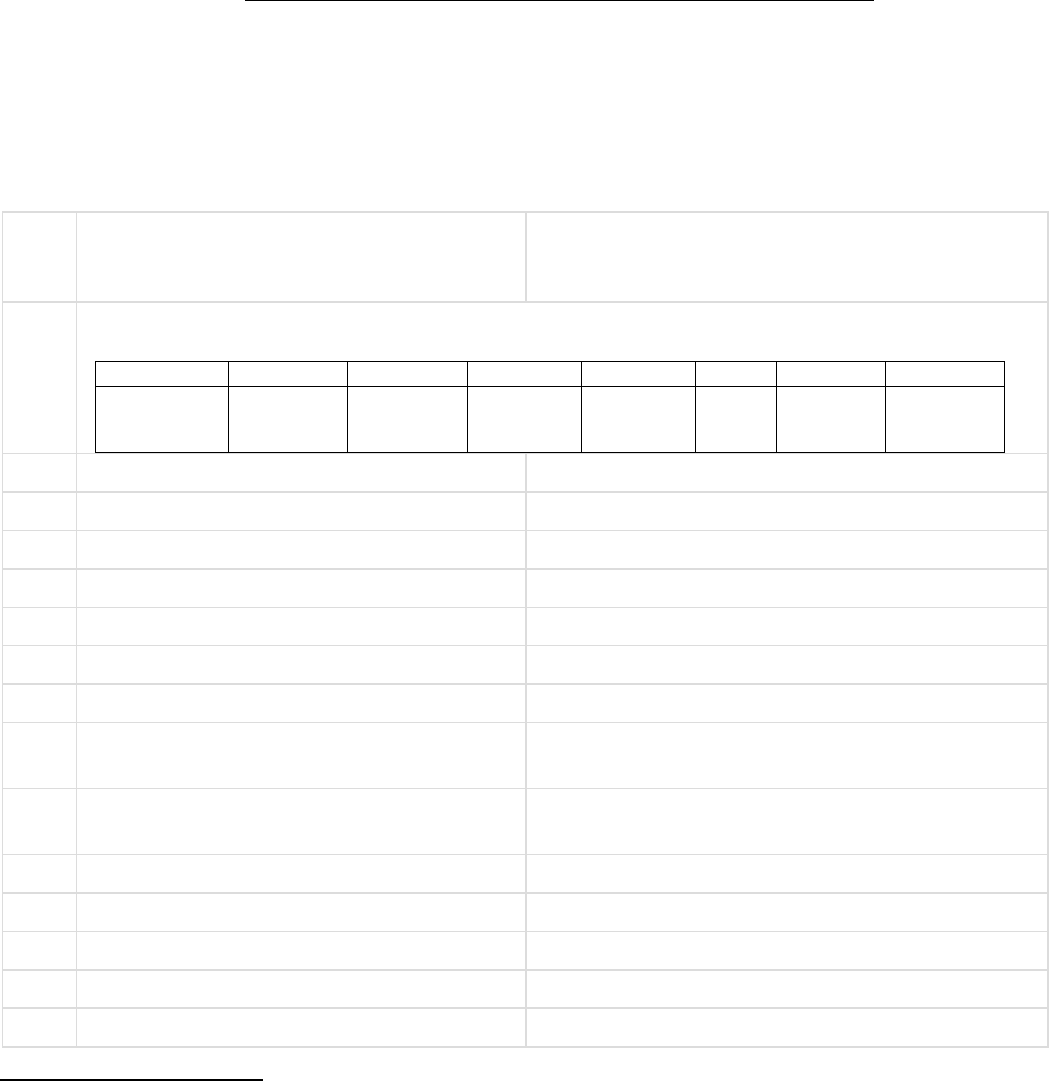
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: Shri P.K. RATH
CASE OF COMPLAINANT – SOURENDRA NATH MUKHERJEE
VS
RESPONDENT: NEW INDIA ASSURANCE CO.LTD.THAKURPUKUR
COMPLAINT REF: NO: KOL-H-049-2122-0266
AWARD NO: IO/KOL/A/HI/0239/2021-2022
1.
Name & Address of The Complainant
Sourendra Nath Mukherjee
181A Bhuban Mohan Roy Road
PO: Barisha, Kolkata – 700008.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
510603/34/1
9/04/000001
94
3 lac
27.11.2019
26.11.2020
18644
3.
Name of insured
Sourendra Nath Mukherjee
4.
Name of the insurer
New India Assurance Co. Ltd.
5.
Date of receipt of the Complaint
12-August-2021
6.
Nature of Complaint
Repudiation of Claim
7.
Amount of Claim
26000.00
8.
Date of Partial Settlement
9.
Amount of relief sought
26000
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
13(1)(b)
11.
Date of hearing
Place of hearing
22 September-2021
Kolkata
12.
Representation at the hearing
a) For the Complainant
Sourendra Nath Mukherjee
b) For the Insurer
Deb Kumar Bhattacharyya
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
28-September-2021
Brief Facts of the Case: The Complainant underwent Cataract Surgery (R) on 16.10.2020 at Amulya Jyoti
Eye Foundation and claimed for Rs. 26000/- and hie intimated the matter on 7.7.2021 resting with a letter issued
by the TPA dated 17.8.2021 asking for all the relevant documents viz. Claim form Part A and Part B duly filled
up by concerned Nursing Home, Bills, Money Receipts and Investigation Report with related Prescription along
with a clarification for delay in submission of documents. Claim was repudiated as per Policy condition No. 5.3
which speaks that claim form should be submitted within 30 days from discharge of hospital which was not
adhered to by the claimant.
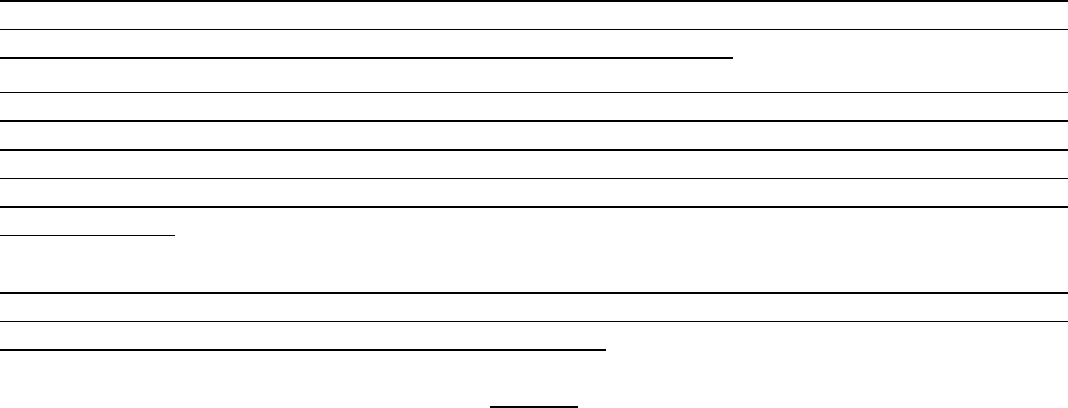
Contention of the complainant: The claim has been repudiated which relates to Cataract Surgery on right eye
on 16.10.2020. Earlier claim was settled as per the Award dated 26.2.2021. Similarly, this case can be settled
in the light of the earlier Award issued for the same surgery on the left eye.
Contention of the Respondent: As per SCN - Operation on his right eye was done on 16.10 2020 and claim
papers were submitted by the Insured on 7
th
July 2021. The Insured forwarded his claim papers after a period
of 9 months without citing a reasonable ground for such delay which is subversive to policy terms and condi-
tion. The claim has been repudiated for violation of policy terms and condition No.5.3 which states that Final
claim with all original documents to be submitted to the Office not later than 30 days from the date of discharge
from the hospital.
Observation and conclusions: It is observed that the Complainant have failed to submit the original docu-
ments in spite of written intimation from the authority which is subversive to policy terms and condition. As
per policy terms and condition the claim has been repudiated.
AWARD
Taking into account the fact & circumstances of the case and the submissions made by both the parties during
the course of hearing and after going through the documents on record it is revealed as per the recorded
documents the decision of the Insurer towards rejection of claim seems to be justified based on Policy Terms &
Conditions.
The subject complaint is therefore dismissed without any relief to the Complainant. With this the complaint is
closed without further reference. The complaint of the complainant is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017:
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt
of the award and intimate compliance of the same to the Ombudsman.
If the decision is not acceptable to complainant, he is at liberty to approach any other Forum/Court of the
Land against the respondent insurer.
Dated at Kolkata on 28th Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
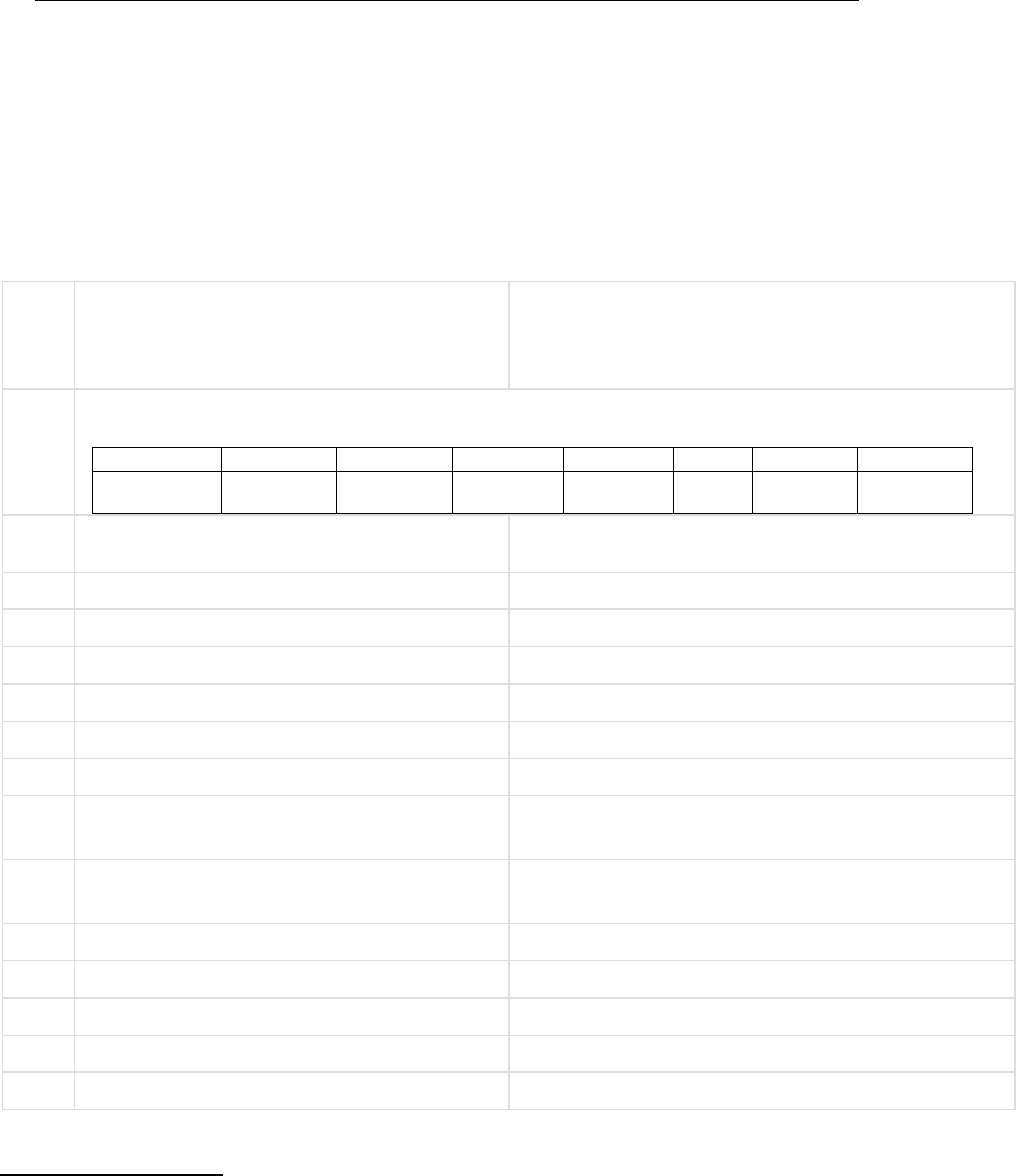
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDER RULE NO.16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Ombudsman Name: Shri P.K. RATH
CASE OF COMPLAINANT – UTTAM KUMAR JAIN
VS
RESPONDENT: MANIPAL CIGNA HEALTH INSURANCE CO
LTD
COMPLAINT REF: NO: KOL-H-053-
2122-0194
AWARD NO:IO/KOL/A/HI/0241/2021-
2022
1.
Name & Address of The Complainant
Uttam Kumar Jain
39 Bangur Avenue Block C
Kolkata 700055
[9339362602]
2.
Type Of Policy: Life / Health / General
Policy Details: FAMILY FLOATER
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
PROHLR0101
71981
25 LACS
12.3.2021
11.302022
28.02.2018
3.
Name of insured
Uttam Kumar Jain
4.
Name of the insurer
MANIPAL CIGNA HEALTH INSURANCE
5.
Date of receipt of the Complaint
20-July-2021
6.
Nature of Complaint
Non-settlement of claim
7.
Amount of Claim
Rs. 52052.00
8.
Date of Partial Settlement
9.
Amount of relief sought
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
13(1)(b)
11.
Date of hearing
Place of hearing
22 September-2021
Kolkata
12.
Representation at the hearing
a) For the Complainant
Rachit Jain
b) For the Insurer
Swetha Nair
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
28-September-2021
Brief Facts of the Case: The Complainant was admitted with the complaint of pain in right hip with difficulty
in walking. He was suffering from Avascular Necrosis (R) Hip and admitted for Bone Marrow Aspiration at
Spandan Hospital on 18
th
March 2020 discharged on the same day. As per policy terms & condition Clause VI
and Exclusion 23 the claim was repudiated on following two grounds: 1) Charges for diagnostic, x-ray and
pathological investigation not consistent with or incidental to diagnosis even if the same require hospitalization
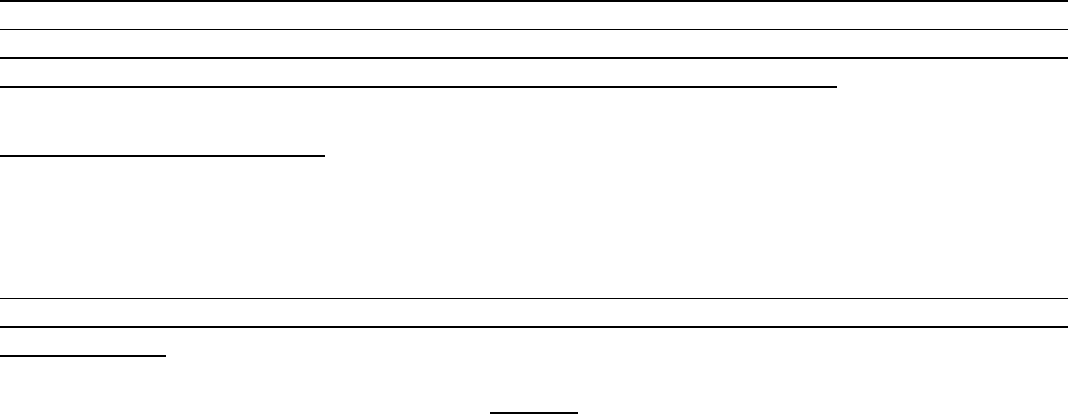
2) Cover medically necessary hospitalization is for more than 24 consecutive hours.
Contention of the complainant: It is stated that there was two claims for the same ailment. First claim was
reimbursed and second one got repudiated. Due to Covid situation my treatment got deferred. First claim was
for getting the material from the body and second one during the surgery using the material taken out from
the body. Under the circumstances the reason for denial of the claim is not hold valid.
Contention of the Respondent: claim was repudiated on following two grounds: 1) Charges for diagnostic, x-
ray and pathological investigation not consistent with or incidental to diagnosis even if the same require
hospitalization 2) Cover medically necessary hospitalization is for more than 24 consecutive hours. In the instant
case hospitalisation procedure is permanently excluded under the policy as per policy terms and condition.
Observation and conclusions: It is observed that there was a significant gap of time period between first and
second hospitalisation. Besides above there was no hospitalisation for more than 24 hours. Earlier claim was
duly reimbursed.
AWARD
Taking into account the fact & circumstances of the case and the submissions made by both the parties during
the course of hearing and after going through the documents on record it is revealed that medical expenses are
covered where hospitalisation is medically necessary and that also for more than 24 consecutive hours as per
Policy Terms & Conditions, hence the decision of the Insurer towards rejection of claim seems to be justified.
The subject complaint is therefore dismissed without any relief to the Complainant. With this the complaint is
closed without further reference. The complaint of the complainant is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of Insurance
Ombudsman Rule 2017:
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt
of the award and intimate compliance of the same to the Ombudsman.
If the decision is not acceptable to complainant, he is at liberty to approach any other Forum/Court of the
Land against the respondent insurer.
Dated at Kolkata on 28
th
Day of September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
KOLKATA
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – Sri Ranjan Kumar Jain
VS
RESPONDENT: -- Max Bupa Health Insurance Co. Ltd
COMPLAINANT REF: NO: KOL-H-031-
2122-0190
AWARD NO: IO/KOL/A/HI/0210/2021-2022
1.
Name &Address 0f the Complainant
Sri Ranjan Kumar Jain
C/o- Ashok Kumar Jain, Moti kunj
Neheru Road Khalpara, Moti Mills Compound
Siliguri, Dist- Darjeeling- 734005
West Bengal.
2.
Type Of Policy: Health
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
30720652202
003
3 lakh basic
S.I + 15 lakh
floater.
06.12.2020
05.12.2021
16.05.2021
12052/
-
Mediclaim
Annual
3.
Name of insured
Ms Akriti Jain
4.
Name of the insurer
Max Bupa Health Insurance Co. Ltd
5.
Date of receipt of the Complaint
09.08.2021
6.
Nature of Complaint
Partial settlement
7.
Amount of Claim
149966/-
8.
Date of Partial Settlement
26.06.2021
9.
Amount of relief sought
35758/-
10.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1) (b).
11.
Date of hearing
Place of hearing
06.09.2021
Kolkata
12.
Representation at the hearing
--
a)For the Complainant
Sri Ranjan Kumar Jain
b)For the Insurer
Sri Bhuban Bhaskar
13.
Complaint how disposed
Through on line hearing.
14.
Date of Award
08/09/2021
Brief Facts of the Case:
This is a claim against treatment of COVID-19 of Ms Akriti Jain (Insured) during hospitalization period
16.05.2021 to 23.05.2021 at Maharaja Agrasen Health care, Siliguri. Total claim submitted by Complainant for
Rs 149966/- of which Rs 114208/- been approved & paid by Insurer. Considering the following as being outside
the scope of cover, Rs 39903/-- not allowed by Insurer , details of which are—1) 24500/- as COVID care Charges
2) 5600/- -- RMO Charges 3) 4900/- Nursing charges as it is included in room rent. 4) 358/- cost of mask 5) 45/-
cost of cotton. 6) 4500/-( in absence of bill).
Complainant not agreed as every expenditure done in relation to treatment for the said suffering & paid as a part
of treatment. So he is claiming for his balance non paid amount.
Contention of the complainant:-
The deducted amount is also a part of treatment cost & as per advice of the Doctor. Hence it is payable under
the claim.
Contention of the Respondent:
Out of total claim for Covid treatment, expenses for Rs 114208/- allowed. Rest amount not paid as these
expenses are not coming under the purview of Policy cover , as also not having bills/ cash memo of the same
as stated in SCN.
Observation and conclusions:
1) The subject policy is Max Bupa Health Insurance Policy under which the claim is lodged.
AWARD
Taking into account the facts & circumstances of the case & the submissions made by both the parties in
hearing, also on going through the submitted papers it is observed that the decision of the Insurer towards
settlement of the claim is primarily based on as per provision & extent of cover under the subject Policy.
But the amount of Rs 2500/- ( non allowable amount for misplaced bill as claimed by Insurer ) towards
cost of PPE KIT & HRCT OF THORAX vide money receipt dated 16.05.2021 (Rs4500/- & its discount
by 50% as substantiated by document) is further allowable in the context of ailment & policy cover.
Therefore, Insurance Company is directed to consider further payment of Rs 2250/- towards final disposal
of the claim. With this, the Complaint is closed & treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the provisions of Insurance
Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of the
Award and shall intimate the compliance to the Ombudsman.
SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. AHMED ABDUL SHAIKH V/S UNIVERSAL SOMPO GEN INS CO LTD
COMPLAINT NO: PUN-H-052-2021-0684
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. AHMED ABDUL SHAIKH
PUNE
2.
Policy No:
Type of Policy:
2856/OL/0007685/000
Corona Rakshak Policy
3.
Policy period:
16.10.2020 to 28.01.2021
4.
Sum Insured
Rs.250000/-
5.
Date of inception of first policy:
16.10.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr. Ahmed Abdul Shaikh, 27 yrs
Himself
7.
Name of the Insurer:
The Universal Sompo Gen Ins Co Ltd
8.
Reason for repudiation/Partial
Settlement:
Misrepresentation
9.
Date of receipt of the Complaint:
14.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
SI Rs.250000
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
c) For the Complainant:
Himself
d) For the insurer:
Dr. Ahmed Ali
15.
Complaint how disposed:
Dismissed
Brief facts of the case:-
• The complainant had taken Corona Rakshak Policy with Respondent Insurer, Universal
Sompo Gen Ins. Co Ltd. for self for SI (Sum Insured) of Rs. 2.5 lakh. He lodged claim
of self-hospitalization in Kamshet Hospital, Pune from 05.12.2020 to 14.12.2020 for
Covid 19 positive. This claim was rejected by RI.
Contentions of the Complainant:-
• Complaint’s hospitalisation claim under another policy was settled cashless. Investiga-
tor had done verification and on that basis cashless claim and hospital cash claim both
are settled. But instant claim is rejected on account of statement mismatch.
• He contends that, the said statement was never given by him in any form. Co. has de-
liberately made fake statement to reject the claim.
• The complainant is requesting forum to instruct the insurer to settle the claim.
Contentions of the Respondent Insurer (RI):-
As per the SCN received, RI has contended that,
On scrutiny of documents, the irregularities were observed. On the basis of that the insurance
company deputed the investigator for verification of hospitalization who furnished his
verification report to the insurance company. The below mentioned discrepancies observed:
Copy of the Investigation report is annexed and marked as (“Annexure 5”).
As per insured statement he was not admitted in the ICU but as per hospital authority insured
was admitted in the ICU for 8 days
As per insured statement, he was not monitored and on oxygen within hospitalization but as
per hospital documents insured was on oxygen
As per insured statement, he can be treated on home quarantine and he was admitted in the
hospital only to avail money from the IC.
All ICP and sisters notes are seems to be in single stretch
No single notes of treating doctor available in the ICP.
No any pre consultation was done before the admission in the hospital
Hence the claim has been repudiated as per the terms and conditions of the policy.
Claim is not admissible as per following policy clause:
3.5 Disclosure of information norm: The policy shall be void and all the premiums paid thereon
shall be forfeited to the company in the event of misrepresentation, mis-description or non-
disclosure of any material fact by the policyholder
Result of personal hearing with both the parties (Observations & Conclusions):
During the hearing both the parties contended their respective stand.
On hearing both the sides and going through the documents placed on record, forum feels that
there is substance in the allegations of misrepresentation/discrepancies found by RI through
their investigations. During the hearing also, complainant could not explain the query raised
by the forum based on the information received. Claim papers do not seem to be genuine. It is
understood that the complainant had taken two online policies. Corona Kavach & Corona
Rakshak. RI has approved his cashless claim for Rs. 1,57,300/- vide final authorization letter
dt. 14.12.2020. They have also paid him Rs. 22,500/- vide claim settlement letter dt. 30.01.2021
towards hospital cash. However, they have rejected his this claim under benefit policy for the
reasons mentioned above and the forum is not inclined to intervene in their decision.
It seems in the chaos conditions in the covid rush, some people have misused the policy by
being hand in glove with the hospitals/doctors.
Under the facts and circumstances, forum finds that the RI’s decision of repudiation of claim
is in order.
Complaint disallowed.
Award follows:
AWARD
Under the facts and circumstances, it is found that the decision of repudiation of claim needs
no intervention. Complaint therefore stands dismissed.
Dated: at Pune on this 16
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Ajeet Harakchand Jain V/S Bajaj Allianz General Insurance Co. Ltd.,
COMPLAINT NO: PUN-H-005-1920-0608
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Ajeet Harakchand Jain, Bazarpeth, At
post
Nagothane, Taluka Roaad, Dist- Raigad.
2.
Policy No:
Type of Policy:
OG-18-1910-8430-00000027
Health Guard- Family Floater (silver plan)
3.
Policy period:
14/06/2017 to 13/06/2018
4.
Sum Insured/IDV
Rs. 200,000/-
5.
Date of inception of first policy:
01/06/2009 to 31/05/2010
6.
Name & age of the Insured:
Name of the Policyholder:
Mrs. Reshma Ajit Jain, 40 Years; wife
Mr. Ajeet Harakchand Jain
7.
Name of the Insurer:
Bajaj Allianz General Insurance Co. Ltd.,
8.
Reason for repudiation/Partial
Settlement:
Proportionate co-payment @26% applied on
all bills as room rent exceeded INR 2000/-
9.
Date of receipt of the Complaint:
22/11/2019
10.
Nature of complaint:
Deduction @26% from bill has not justified.
11.
Amount of Claim:
Rs.44,516/-
12.
Rule of IO Rule under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
22/07/2021; Online
14.
Representation at the hearing
e) For the Complainant:
Himself
f) For the insurer:
Mr. Irfan Shaikh; Dr. Ravindra Shingte
15.
Complaint how disposed:
Partially Allowed
Brief facts of the case:
Complainant has health insurance with the RI (Respondent Insurer) under which he had
reported a claim of his wife for hospitalisation in Poona Hospital from 10 Dec 2017 to 16 Dec
2017 for Acute Small Intestinal Obstruction. While settling the claim, RI had disallowed Rs.
44516/- from total claimed amount, on the ground that availed room rent (Rs. 2700/- per day)
has exceeded the eligible room rent (Rs. 2000/- per day).
Contentions of the Complainant:
The Complainant is having this health insurance policy with the RI since 2009 without any
break. RI has changed their rules in the year 2017 without proper guidance. He is ready to
bear the cost of extra room rent @ 700/- rupees per day, which exceeded the eligible room
rent of Rs. 2000/- per day. But RI has deducted 26% from the total billed amount, which is
unreasonable and not fair.
In the grievance mail to the company, he submits that when he first took this policy, that time
there was no any capping in that policy. So he renewed it every year and also got claims from
the company without any capping.
In June 2017, while renewing the policy, his agent informed him that his plan is silver plan and
in that category, only 1% of Sum Insured room charges are applicable. He is agreeable to 1%
hospital room rent but he is not aware of the clause which says proportionate co-payment will
be applicable on all bill heads. If he knew this condition, then he would have chosen a room
below 2000/- per day. If the agent had explained all these things, then he would have decided
whether to renew the policy with RI or to port it.
He further states that the company had mentioned it in their policy certificate but he did not
read it because he was having this policy since 2009 and at that time no capping was there.
Hence, aggrieved by the inappropriate deduction of his wife’s claim, complainant filed
complaint with this forum for resolution of his grievance.
Contentions of Respondent Insurer (RI):
At the outset RI have informed that mediclaim of the complainant is honored by them. They
have paid an amount of Rs. 1,25,458/- from the total bill of Rs. 1,69,974/-. Complainant is
aggrieved by the non-payment of Rs. 44,516/- which is termed as room rent differential co-
pay. Eligible per day room rent is Rs. 2000/-. Availed per day room rent is Rs. 2700/-. As per
policy terms and condition proportionate co-payment 25.92% is applicable on all bill heads
excluding medicines consumables & non-medical expenses.
In their SCN (Self Contained Note) alongwith details of deductions amounting to Rs. 8,231/-
(on account of non-medical items, admission fees, bio medical waste, hospital cash,
registration fees and no bills) they have shown the deduction of Rs.34215/-towards
proportionate deductions based on the room rent. The clause is reproduced below:
‘A. COVERAGE
1. In-patient Hospitalisation Treatment
i. Room, Boarding and Nursing Expenses as provided by the Hospital/Nursing Home up to 1%
of Sum Insured per day (Excluding Cumulative Bonus) or actual, whichever is lower.
Note: In case of admission to a room at rates exceeding the limits as mentioned under 1.(i) ,
the reimbursement of all other expenses incurred at the Hospital, with the exception of cost of
medicines, shall be payable in the same proportion as the admissible rate per day bears to the
actual rate per day of room rent charges’.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 22/07/2021 (through video-conferencing), both the parties
reiterated their respective stand.
On perusal of the papers and the policy wordings, forum is satisfied with the express condition
of proportionate deductions in case where the opted room rent exceeds the eligible room
rent. Said term is mentioned at ‘Note’ column of section A of the policy. Though there is a
mention of proportionate deduction on the entire amount of hospital bill, except medicines,
forum finds that reduction in bill amount strictly on percent basis must not be intended while
formulating this clause. Without looking into the actual expenses required to be charged for
the room rent of Rs.2000/- per day, RI’s decision of deduction in the hospital bill on per cent
basis is not acceptable. Especially, professional fees and pathology, radiology charges do not
differ much on room rent basis.
Hence, following amounts are awarded for the further payment against these heads:
Professional fees: Rs.5000
Pathology charges: Rs. 500
Cardiology charges: Rs.500 __
Total additional amount payable: Rs.6000/-
In view of this, Rs.6000/- is being considered for further payment of the claim.
Award follows:
AWARD
Under the facts and circumstances, the RI is directed to pay Rs.6000/- to the complainant,
towards full and final settlement of the complaint. The award is to be settled within one
month from the date of receipt of this award failing which it will attract interest at the
prevailing bank rate plus 2% extra from the date of rejection of the claim till the date of
payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award
and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: 29/09/2021 at Pune
VINAY SAH
INSURNCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. AMOL ANNASAHEB JAWALE V/S CHOLAMANDALAM MS GEN INS
CO LTD
COMPLAINT NO: PUN-H-012-2021-0630
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. AMOL ANNASAHEB JAWALE
OSMANABAD
2.
Policy No:
Type of Policy:
2894/00008158158/000/00
Corona Rakshak Policy, Chola
3.
Policy period:
24.07.2020 to 04.05.2021
4.
Sum Insured
Rs.250000
5.
Date of inception of first policy:
24.07.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr. Amol Annasaheb Jawale,42 yrs
Mr. Amol Annasaheb Jawale
7.
Name of the Insurer:
Cholamandalam MS Gen Ins Co Ltd
8.
Reason for repudiation/Partial Settlement:
Hospitalisation not warranted
9.
Date of receipt of the Complaint:
10.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Rs.250000/-SA
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
g) For the Complainant:
Himself
h) For the insurer:
Mr.Rushabh; Dr.Sudipta Thakur
15.
Complaint how disposed:
Disallowed
Contentions of the Complainant:-
• The complainant had taken Corona Rakshak Policy with Respondent Insurer, Chola-
mandalam MS Gen Ins. Co Ltd for self for SI (Sum Insured) of 2.50 lakh. He lodged a
claim of self-hospitalization in Govt. Ayurvedic hospital, Osmanabad from 06.09.2020
to 15.09.2020. The complainant is claiming for SI Rs. 2,50,000/-.
• Claim was repudiated on the grounds of no active line of treatment. According to com-
plainant AIIMS had issued guidelines that are not meant to replace the clinical judgment
or the decision of the treating doctor of the hospital and health ministry.
• The complainant was having high grade fever, hence admitted in the hospital. Thus the
hospitalization was a necessity to control lung infection.
• The complainant is requesting forum to intervene for settlement of full claim amount,
hence the complaint
Contentions of the Respondent Insurer (RI):-
As per the SCN, RI has contended that,
On scrutiny of the claim documents submitted, they observed that the claim is not admissible
for the following reasons:
The treatment given during the hospitalization period didn’t warrant inpatient admission. Only
oral medications were administered and insured’s medical condition was within normal limits
and not requiring hospitalization as per the ministry of health guidelines.
Result of personal hearing with both the parties (Observations & Conclusions):
During the hearing both the parties contended their respective stand.
On hearing both the sides and scrutinizing the documents placed on record, forum has
following observations:
From the documents produced, it is observed that the complainant was admitted in a
Government Ayurvedic Hospital. During the hearing, he informed that after trying in 2-3
hospitals, somehow he could get admission in this ayurvedic hospital.
1. The admission notes of the hospital states as: ’the patient admitted to GAC, Osmanabad
due to rapid antigen positive on 06/09/2020 for complaints of breathlessness.’

2. In the complaint, he has mentioned as he was having high grade fever. Whereas, the
IPD papers show the remark on 06/09/2020 of only breathlessness. No fever notings
are recorded there. Even, throughout the hospitalization period also, no high fever is
recorded.
3. The prescription of Civil Hospital, Osmanabad dt.06/09/2020 stated as ‘Pt.to be admin-
istered in TPS’;
4. All the claim papers of the hospital carry the OPD registration no. 16262 for the patient
insured.
5. There are two discharge cards submitted for the same hospitalization of the same hos-
pital, one carrying the remark of ‘Revised’. ‘Revised’ discharge card has h/o patient and
investigations carried out.
6. As per IPD, on all the dates of his admission, there is remark of no fresh complaints.
His SPO2 level was normal in the range of 94% to 100% also. All other parameters like
temperature etc. were in normal limits.
7. The complainant has also submitted hospital papers of the treatment taken in Nov.2020,
for post covid general weakness for which no relevance is mentioned by the complain-
ant.
In view of the above, forum does not find the need of hospitalization as prescribed by the
AIIMS guidelines is fulfilled here. Being detected as positive, he must have been kept under
observations and precautionary medicines for not to aggravate the conditions, but it could have
been managed by mere isolation also.
Under the facts and circumstances, forum finds that the RI’s decision of repudiation of claim
is in order.
Complaint disallowed.
Award follows:
AWARD
Under the facts and circumstances, it is found that the decision of repudiation of claim
needs no intervention. Complaint therefore stands dismissed.
It is particularly informed that in case the award is not agreeable to the complainant, it would
be open for him/her, if he/she so decides to move any other Forum/Court as he/she may
consider appropriate under the Laws of the Land against the Respondent Insurer.
Dated: at Pune this on 16
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Amol Vitthalrao Kadam Vs Aditya Birla Health Insurance Co. Ltd
COMPLAINT NO: PUN-H-055-1920-0695
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Amol Vitthalrao Kadam, pune
2.
Policy No:
Type of Policy:
51-19-00081-00-00
Group Health Policy
3.
Policy period:
18/5/2019-17/5/2020
4.
Sum Insured
Not mentioned
5.
Date of inception of first policy:
Not mentioned
6.
Name and age of the Insured:
Name of the Policyholder:
Snehal- Spouse
TNS India Pvt. Ltd.
7.
Name of the Insurer:
Aditya Birla Health Insurance Co. Ltd.
8.
Reason for repudiation/Partial
Settlement:
Inj. Rituximab is biological medicine, not
covered under policy
9.
Date of receipt of the Complaint:
10/2/2020
10.
Nature of complaint:
Total Rejection of claim
11.
Amount of Claim:
127055/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the Complaint
was registered:
13 1(b)
13.
Date of hearing/Place:
Online hearing on 13.08.2021
14.
Representation at the hearing
i) For the Complainant:
Himself
j) For the insurer:
Ms. Manali Shukla
15.
Complaint how disposed:
Allowed
Brief Facts of the Case:
The complaint is the employee of TNS India Pvt. Ltd covered under Group Mediclaim floater
Policy issued by Respondent Insurer (herein after is called RI). Wife of the complainant was
admitted in hospital for relapsing remittary multiple sclerosis two times. Both claims of the
complainant were rejected by the RI stating that the patient admitted for Rituximab infusion
which is biological agent. It is not listed daycare procedure hence, cashless was denied.
Complainant filed complaint before this Forum for resolution after representing his complaint
before grievance department of RI but he did not get response from RI.
Contention of the Complainant:
As per contention of the complainant, his wife is diagnosed with relapsing remitting multiple
sclerosis in August 2019 by well known neuro physician Dr. Rahul Baviskar from Nasik. As
per his diagnosis he said this ‘Multiple Sclerosis’ is a disease which is not curable forever. It
can occur sometimes in between. If patient observed with symptoms like imbalance, vertigo,
vomiting etc. then patient will need treatment of Inj. Solumedrol or Methyl Prednisionine and
lnj. Rituximab to keep this attack in control. Also, to provide this treatment patient needs to be
hospitalized under observation at least 24 hours.
As per internal Employee Benefit Manual given to employee for reference, nowhere is
mentioned that particular injection is excluded from standard exclusion so complainant has
requested Forum for intervention in this issue and direct the RI to settle the claim.
Contention of the Respondent Insurer:
As per rejection mail, member submitted document of IPD bills, diagnosis- Multiple Sclerosis,
treatment done was Rituxirel (rituximab Intravenous) Inj-2 times. The said treatment is not
listed for the present ailment, hence claim is repudiated as per policy terms and conditions-1.2
Day Care treatment.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 13.08.2021 (through video-conferencing) both the parties
reiterated their respective stand.
It is observed from RI’s contention that the rejection was on the ground that the treatment is
not listed in the day care treatment. Whereas, from the Discharge card it is observed that the
insured patient was admitted in hospital for more than 24 hours. The treating doctor also has
clarified that this injection carries a risk of anaphylactic reaction so needs to be monitored in
ICU for which hospitalisation is a must.
As the hospitalization for more than 24 hours is established and its need is convinced forum
allows the complaint in favour of complainant.
Award follows;
AWARD
Under the facts and circumstances, the RI is directed to pay Rs.127055/-less
deductibles as per the terms and conditions of the policy to the complainant,
towards full and final settlement of the complaint.
The award is to be settled within one month from the date of receipt of this award
failing which it will attract interest at the prevailing bank rate plus 2% extra from
the date of rejection of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the
award and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune, on this 30
th
day of September, 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Anil Pawankumar Murarka Vs. Max Bupa Health Insurance Company Ltd.
COMPLAINT NO: PUN-H-031-1920-0538
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. Anil Pawankumar Murarka
Azad Nagar, Mira Bhayander Road,
Bhayander (East), Mumbai - 401105
2.
Policy No:
Type of Policy:
30251153201805
Health Insurance – Hearbeat Silver
3.
Policy period:
04/09/2018 to 03/09/2019
4.
Sum Insured/IDV
Rs.3,00,000/- + 90,000/- accrued loyalty
addition.
5.
Date of inception of first policy:
04/09/2013
6.
Name & age of the Insured:
Name of the Policyholder:
Mr. Anil Pawankumar Murarka, 37 years
Same as above
7.
Name of the Insurer:
Max Bupa Health Insurance Co. Ltd.
8.
Reason for rejection /Partial Settlement:
Admission only for evaluation and
observation.
9.
Date of receipt of the Complaint:
22/11/2019
10.
Nature of complaint:
Rejection of health claim
11.
Amount of Claim:
Rs.69,879/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021, Online. Pune.
14.
Representation at the hearing
k) For the Complainant:
Himself and his wife Kanakbala
l) For the insurer:
Sheetal Patwa
15.
Complaint how disposed:
Allowed.
Contentions of the Complainant:
The Complainant was admitted in Aditi Hospital, Kandivali on 12/04/2019 with complainants
of Stricture Urethra. He had undergone Urethrocystoscopy with Visual internal urethrotomy
and discharged on 13/04/2019.
The Respondent Insurer rejected reimbursement claim of Rs. 69,879/- stating that admission
was done just for investigation and evaluation purpose.
Complainant clarified from treating doctor that Visual Internal Urethrotomy (VIU) surgery
requires admission in hospital. His previous claim was settled few days back and rejection of
present claim is unexpected and uncalled-for.
Grievance department also maintained the rejection of claim on the same ground.
Aggrieved with this decision, the complainant has approached the forum for resolution of his
grievance.
Contentions of the Respondent Insurer (RI):
After receipt of claim documents, the respondent company scrutinized the claim documents
carefully and repudiated the claim by stating that as per submitted document & investigation
done it was found that the admission of the patient was done only for evaluation/observation
purpose. As per discharge summary, insured is a k/c/o the diagnosed ailment and admitted for
investigation. During hospitalisation majorly diagnostics and physiotherapy has been done and
no active line of treatment was given. Hence, claim was rejected as per policy clause 8.16
which is reproduced as under:
Clause 8.16–Hospitalization not justified – “Admission solely for the purpose of
Physiotherapy, evaluation, investigations, diagnosis or observation services or not consistent
with standard treatment guidelines as defined by Clinical Establishments (Registration and
Regulation) Act, 2010 and amendments thereafter or Evidence Based Clinical Practices.”
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (through video-conferencing) both the parties
reiterated their respective stand.
On reviewing the medical papers in the file, it is observed that his ailment is such that it is
requiring periodical evaluation and treatment. Before this admission, he was admitted twice in
Jan’19. RI has paid his earlier claim. As carcinoma is detected, his treatment is still continuing.
During the hearing, he informed that every three months endoscopy needs to be done and he
still uses catheter whenever he feels that urine is blocked.
As seen from discharge card and ICP of current admission, required procedures are carried out
and treatment given. They are consistent with and incidental to the diagnosis. Treating doctor
has clarified that the procedure VIU surgery requires hospital admission. As such, it is not
correct to say that no active line of treatment is given.
Forum feels that the claim is admissible.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent is directed to settle the
admissible amount of claim towards full and final settlement of his complaint.
The award is to be complied with within one month from the date of receipt of this award
failing which it will attract interest at the bank rate plus 2% extra from the date of
rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award
and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insure
Dated: On 9
th
day of September 2021. Pune.
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– MR VINAY SAH
CASE OF MR ANIL R SONI V/S CHOLAMANDALAM MS GEN INS CO LTD
COMPLAINT NO: PUN-H-012-2021-0697
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr Anil R Soni
Jalna 431203
2.
Policy No:
Type of Policy:
2894/00009529/000/00
CORONA RAKSHAK POLICY, CHOLA
3.
Policy period:
25.07.2020 TO 05.05.2021
4.
Sum Insured
Rs.1,00,000/-
5.
Date of inception of first policy:
25.07.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr Anil R Soni, 51 years old
- do -
7.
Name of the Insurer:
Cholamandalam MS Gen Insurance Co Ltd
8.
Reason for repudiation/Partial
Settlement:
Inpatient admission not warranted
9.
Date of receipt of the Complaint:
05.03.2021
10.
Nature of complaint:
Total repudiation of claim
11.
Amount of Claim:
Rs.1,00,000/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
14.07.2021 (Virtual Hearing)
14.
Representation at the hearing
c) For the Complainant:
Mr Abhishek
d) For the insurer:
Mr Abhijit Santikar assisted by Dr Sudipta
15.
Complaint how disposed:
Dismissed
Brief facts of the case:
Complainant was self-hospitalized at Covid Care Centre-SRPF-E, Covid-19 District Jalna from
11.11.2020 to 15.11.2020 for treatment of Covid-19. He approached this Forum with a
complaint against the total repudiation by the Respondent, Cholamandalam MS General
Insurance Co Ltd of a claim lodged under the policy in respect of the said hospitalization.
Contentions of the complainant:
The complainant contended that his claim was repudiated by RI stating that his vitals were
normal and he did not require hospitalization. He needed self-isolation by home quarantine,
only. He was not agreeable to the repudiation and hence approached this Forum for settlement
of his genuine claim.
Contentions of the Respondent Insurer (RI):-
It was contended on behalf of the Respondent that on scrutiny of the claim documents, it was
observed that the Insured was admitted in a Covid Care Center and treatment given during
hospitalization period didn’t warrant inpatient admission. It was pointed out that only oral
medication was administered and the Insured’s medical condition was within normal limits,
not requiring hospitalization as per Ministry of Health guidelines. Hence, the claim was
inadmissible and repudiated.
Forum’s Observations & Conclusions :
On scrutiny of the documents produced on record coupled with the depositions of both the
parties to the dispute, the Forum observed that in the instant case, the Insured was treated with
oral medication like Vit C, Multivitamin, Paracetamol during the entire hospitalization of 9
days. Moreover, his vitals were within normal limits and hence his condition did not require
hospitalization as per Ministry of Health Guidelines. Under the circumstances, the decision of
the Respondent to deny the claim being based on policy terms and conditions is in order. The
Forum does not find any valid reason to intervene with the same and pass the following Order.
AWARD
Under the facts and circumstances of the case, the complaint lodged by Mr Anil
R Soni against Cholamandalam MS General Insurance Co Ltd does not sustain.
Dated: This 25
th
day September 2021 at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MRS.ANJALI M JOSHI V/S STAR HEALTH & ALLIED INS CO LTD
COMPLAINT NO: PUN-H-044-1920-0493
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mrs. ANJALI M JOSHI
THANE
2.
Policy No:
Type of Policy:
P/171115/01/2019/001321
Senior citizen red carpet health
insurance policy
3.
Policy period:
26.05.2018 to 25.05.2019
4.
Sum Insured
300000
5.
Date of inception of first policy:
26.05.2017
6.
Name & Age of the Insured:
Name of the Policyholder:
Shakuntala Sham Gowande, 67 yrs
(M)
Mrs. Anjali Mahesh Joshi
7.
Name of the Insurer:
Star health & allied Ins Co Ltd
8.
Reason for repudiation/Partial Settlement:
Paid as per capping on Major Surgeries
9.
Date of receipt of the Complaint:
18.11.2019
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Total Sum Insured of Rs. 3,00,000/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
28/05/2021; Online
14.
Representation at the hearing
m) For the Complainant:
Herself
n) For the insurer:
Dr. Smita Sonawane
15.
Complaint how disposed:
Disallowed
Brief Facts of the case:
The complainant had taken Senior citizen red carpet health insurance plan with Respondent
Insurer The Star Health & Allied Ins. Co Ltd, Thane for her mother for Sum insured of Rs. 3
lakhs. She lodged claim of her mother -hospitalization from 22.03.2019 to 03.04.2019 in
Deenanath Mangeshkar Hospital, Pune for Koch’s Spondylolisthesis. The total expenditure on
hospitalization was Rs. 403810/-. The claim was settled for Rs.1,50,000/- only i/o full SI.
Contentions of the Complainant:
Complainant’s mother underwent an emergency surgery for infective spondylodiscitis D4-D5
with paraparesis on 23
rd
March 19 at Deenanath hospital. She submitted application for
cashless facility which was rejected with a reason that ‘claim for spondylosis is not admissible
for a period of 2 years from date of inception of first policy.’
She informed customer care that said treatment is not for spondylosis and supported with clarification
from operating surgeon Dr. Amol Rege. Even post clarification of the surgeon, cashless was denied
& was informed to submit the claim under reimbursement facility. Post discharge, they submitted
reimbursement form with supporting reports, hospital bills etc.
On 9
th
may 19, an amount of 1,41,152/- was credited to her bank account which was less than even
50% of the total claim. After raising grievance, on 10
th
Sept 19, further amount of Rs. 8,848/- was
paid. Company thus settled the reimbursement claim with amount of Rs. 1,50,000/-. She was given
to understand that the claim is settled under “All Major Surgeries” which has a capping of 1.5L.
She contends that the policy document /product brochure of the company has defined the treatments
covered under term “All other major surgeries”. However, Kochs spondylolisthesis also referred as
spine Tuberculosis is not mentioned under the said definition, hence settlement of claim under this
category is not correct.
She has summarized her grievance as under;
a) The company rejected cashless facility.
b) The company has not provided rightful information repeatedly sought by the policy holder.
c) The reimbursement claim settlement amount is short of their expectations. This creates a doubt on
genuinity of settlement process & finalization of reimbursement.
d) The Company has not provided list of “All other major surgeries” in spite of repeatedly requesting
for the same which amounts to concealing of information to the policy holder.
She is requesting the forum to intervene for settlement of full Sum Assured.
Contentions of the Respondent Insurer (RI):-
As per their SCN, they have contended that,
The insured made a claim in the 2
nd
year of the medical insurance policy. The insured took treatment
in Deenanath Mangeshkar Hopsital, Pune for KOCH’S SPONDYLODISCITIES” The insured
submitted a claim for Rs.425010/- Initially a sum of Rs.141152/- was settled, and on review, further
amount of Rs.8848/- was settled.
As per the coverage Clause G of the policy, the maximum amount payable for ALL OTHER MAJOR
SURGERIES was Rs.150000/- only for the sum Assured of Rs.300000/-
The maximum amount was already settled to the insured as per the terms and conditions of the policy,
there is no further amount liable for payment under policy for the present claim.
Result of personal hearing with both the parties (Observations & Conclusions):
As per the discharge summary of the patient insured, diagnosis is D4-5 Koch’s Spondylodiscitis k/c/o
HTN ?IHD.
Upon going through the policy terms and conditions, Forum came across the policy clause stated
below, by which it can be inferred that the present claim was otherwise not payable, as this patient
underwent spine decompression for D4-D5 spondylosis and empirical treatment for Koch
(tuberculosis). Report for tuberculosis is negative (pathology report dated 26-3-3019, Deenanath
Mangeshkar hospital).
**Clause 3.d excludes diseases of spine, bones, joints, tendon (policy page 5)
In view of this, forum is convinced that there is a waiting period of 2 years for the deceases of spines
and bones. As spondylodiscitis is a disease of spine, the waiting period of 2 years is applicable for
this.
It is noted from the discharge card that ‘Pt. had upper back pain since 1 month, H/o fall down before
7 days.’
The RI representative has clarified that,
‘This claim has been settled for haematoma in the spine due to fall for which debridement was done,
this being a major surgery , sublimit of Rs 150000 was allowed as per policy norms’.
Complainant, hereby is made to understand that though the claim for spondylodiscitis had waiting
period of 2 years; the RI has considered her claim for haematoma. Now, the question remains whether
it falls under major surgery as defined in the policy for which complainant has objections.
Major surgery, as defined in the policy norms as ‘Major Surgery means Intestinal obstruction – acute
/ sub acute / chronic, Bilo Pancreatic surgery, Gastro-Intestinal surgeries, Total Knee Replacement
surgery, Total Hip Replacement surgery, Other major surgeries of joints, Hemi-Orthro Plasty
surgeries, Surgeries on Prostrate, Surgery related to Genito-Urinary Tract.’
As the haematoma had happened at the spine, it is considered under the surgeries of joints. For this,
the forum noted following observations to see the correctness of the information given by the RI.
‘The spinal column also has real joints (just like the knee or elbow or any other joints) called facet
joints. The facet joints link the vertebrae together and give them the flexibility to move against each
other’.
In view of this, forum finds that the surgery for hematoma in the spine falls under major surgeries,
for which policy has provided capping in proportion to the sum insured. For sum insured of Rs.3lacs,
policy has provided the capping of Rs.1,50,000/-. Hence, the payment of Rs.1,50,000/-as assured in
the policy terms, is in order. Hence, no further amount falls payable in this case.
Complaint therefore is disallowed. Award follows,
AWARD
Under the facts and circumstances, the complaint is not sustainable, hence dismissed.
Dated: at Pune on this 15
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
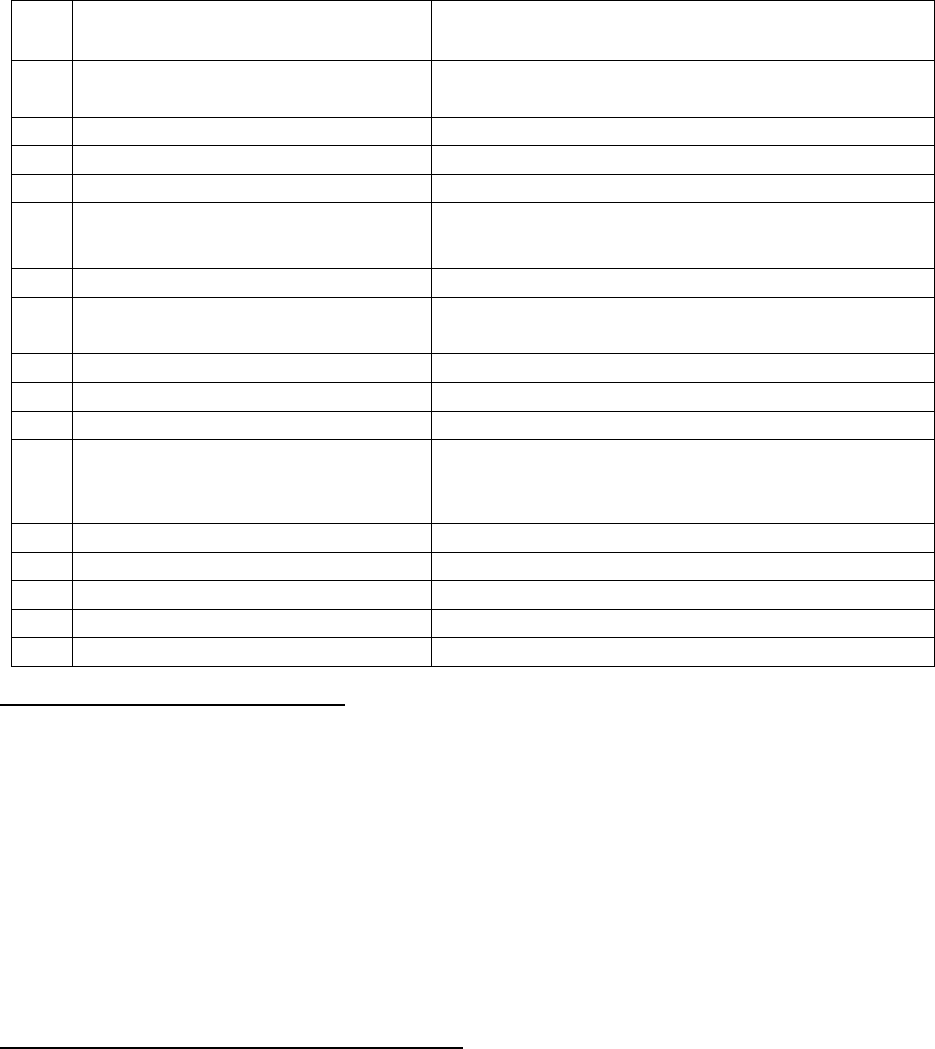
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR.ANKIT AGARWALV/S STAR HEALTH &ALLIED INS CO LTD
COMPLAINT NO: PUN-H-044-2021-0584
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Ankit Agarwal
Thane
2.
Policy No:
Type of Policy:
P/700002/01/2021/032910
Corona Rakshak Policy
3.
Policy period:
03.08.2020 to 15.05.2021
4.
Sum Insured
Rs. 2,50,000
5.
Date of inception of first policy:
03.08.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Mrs Renu Agarwal, 57 yrs (M)
Mr. Ankit Agarwal
7.
Name of the Insurer:
The Star Health & Allied Insurance Co Ltd
8.
Reason for repudiation/Partial
Settlement:
Insured needs only self-isolation & Home
quarantine Covid-19 Positive
9.
Date of receipt of the Complaint:
11.02.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
SI Rs.2,50,000/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
o) For the Complainant:
Himself
p) For the insurer:
Dr. Smita Sonawane
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:-
• The complainant had taken Corona Rakshak Policy with Respondent Insurer, Star Health &
Allied Insurance Co Ltd for spouse and dependent parent for Sum Insured (SI) 2.5 lakh each.
He lodged claim of his mother’s hospitalization in Bethany Hospital, Thane from 08.11.2020
to 13.11.2020 for Covid 19 Pneumonia, K/c/o DM & HTN. The total expenditure of the treat-
ment was Rs.97920 /- The complainant is claiming for SI Rs.250000/- The RI regretted the
claim stating that based on the documents submitted, the insured Patient needed only self-
isolation by home quarantine.
• He contends that his mother was admitted in consultation with the doctor. Also, that he does
not find the rejection clause (condition regarding AIIMS protocol) in any policy document
sent to him on purchase.
Contentions of the Respondent Insurer (RI):-
As per the SCN submitted, RI has contended that,
As per discharge summary, the insured was diagnosed covid 19 positive pneumonia in k/c/o DM/HTN
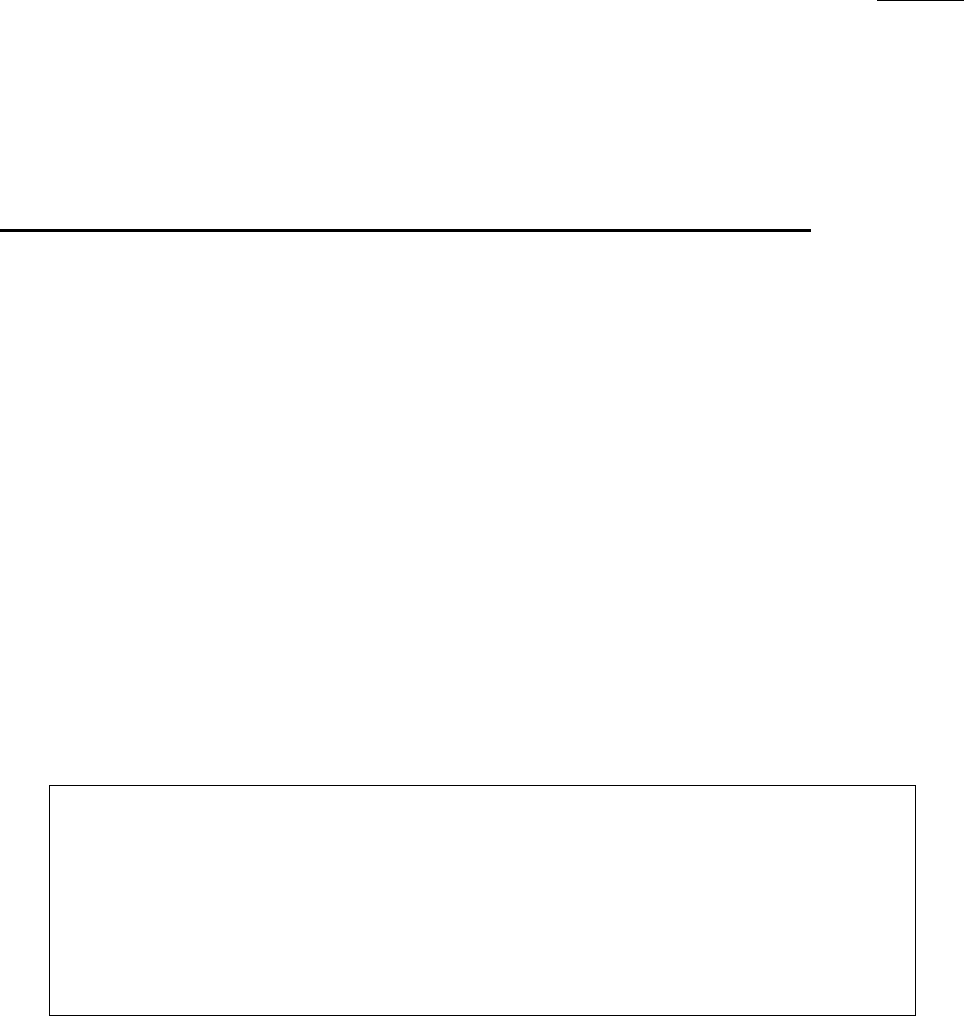
and underwent conservative treatment.
It is observed from the medical records that the insured patient’s clinical picture and vital charts
indicate that the patient falls under category A of AIIMS protocol. Moreover as per the policy terms
and conditions, coverage is only for a person who is contracted and diagnosed with Covid 19 requiring
hospitalization.
As per the guidelines from All India Institute of Medical sciences, New Delhi and Ministry of health
and family welfare, government of India regarding the treatment of Covid 19 patients, the patient
needed only self-isolation by home quarantine based on submitted claim documents, instead the
patient was admitted and treated, which is not payable.
The RI was thus unable to settle the claim under the above policy and hence repudiated the claim.
Result of personal hearing with both the parties (Observations & Conclusions):
During the hearing both the parties contended their respective stand.
On hearing both the sides and perusing the documents placed on record, forum has following
observations:
5. The patient insured is a 57 yrs old lady having co-morbidities of HTN and DM. Forum is
aware of the guidelines to admit such patients in hospital.
6. During the hospitalisation, she was not just kept under observation, but was treated with med-
icines including Remedesivir injection also, which needs to be administered under the medical
supervision.
7. There is a certificate from Bethany hospital which states that the patient was admitted with
c/o cough, throat infection, general weakness, decreased appetite, Covid 19 pneumonia. Also,
had c/o constipation in which admission required for further Rx. All the above Rx required
admission which is not possible on OPD basis or home quarantine.
Looking to the age and co-comorbid conditions of the patient insured, her admission in the hospital
is justified. She was admitted in the hospital for 5-6 days. Hence, as per the policy terms, she fulfils
all the criteria for eligibility to receive the insured amount granted under this benefit policy.
Complaint admitted. Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed
to pay to the complainant Rs.2,50,000/- towards the full and final settlement of this
complaint.
The award is to be complied with one month from the date of receipt of this award
failing which it will attract interest at the applicable bank rate plus 2%extra from
the date of rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurers.
Dated: at Pune this 15
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
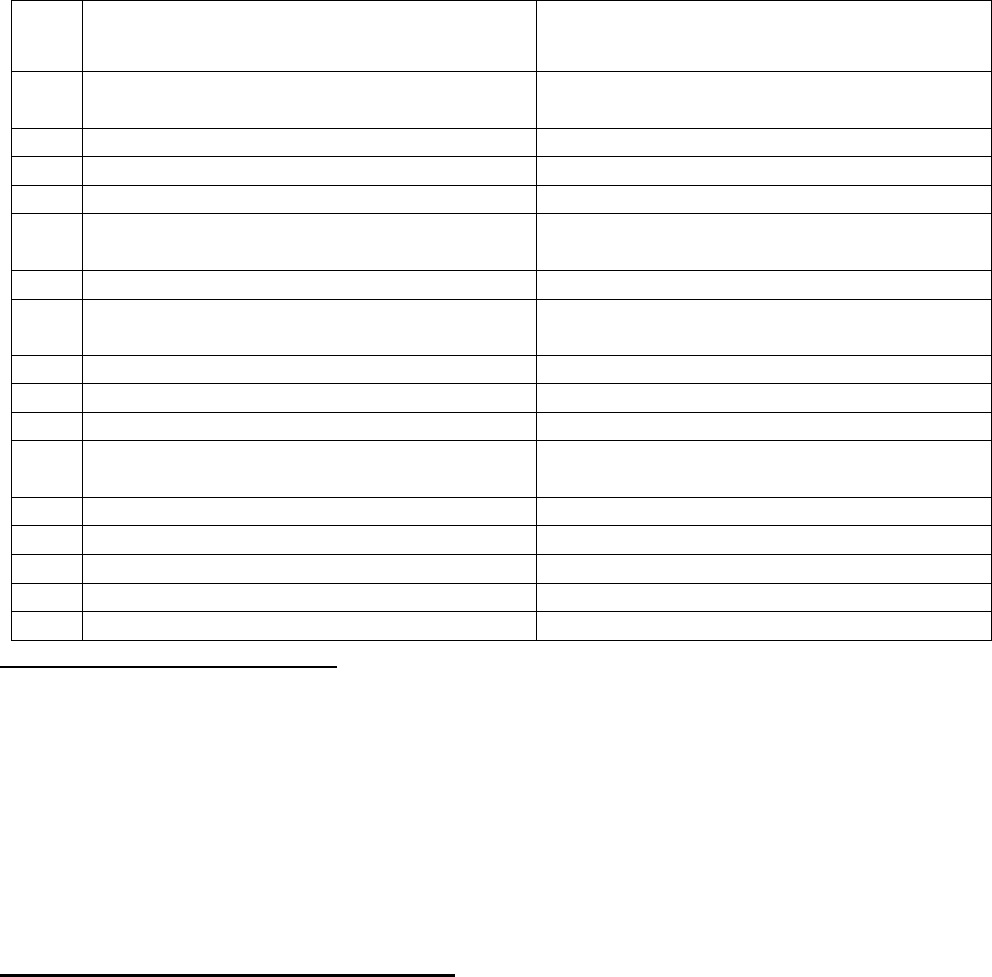
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– SHRI VINAY SAH
CASE OF Mr. Balasaheb Gamaji Adhav v/s United India Insurance Company Ltd
COMPLAINT NO: PUN-H-051-2021-0074
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Balasaheb Gamaji Adhav, Ahmednagar
2.
Policy No:
Type of Policy:
162503/28/19/P10516830
Family Medicare policy 2014
3.
Policy period:
26/7/2019-25/7/2020
4.
Sum Insured
Rs.250000/-
5.
Date of inception of first policy:
24/4/2016
6.
Name and age of the Insured:
Name of the Policyholder:
Mrs. Vanita Balasaheb Adhav; Wife; 41 yrs.
Mr. Balasaheb Adhav
7.
Name of the Insurer:
United India Insurance Company Ltd
8.
Reason for repudiation/Partial Settlement:
Procedure could have been managed on
OPD basis.
9.
Date of receipt of the Complaint:
29/6/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
81150/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
13 1( b)
13.
Date of hearing/Place:
22/09/2021; Online
14.
Representation at the hearing
q) For the Complainant:
Himself
r) For the insurer:
Mr. Dattatray Natha Katkar
15.
Complaint how disposed:
Allowed Partially
Contentions of the Complainant:
The complainant is having floater Health policy with Respondent Insurer (hereinafter is called RI)
from 24/4/2016 for his family members (himself, his spouse, his daughter and his son). He has filed
claim for his wife for Degenerative Lumber spondylitis for the period 14/11/2019 to 20/11/2019 i.e.
in fourth year of policy.
RI has rejected the claim stating that procedure/treatment usually done in outpatient department
are not payable under the policy even if converted as an inpatient in the hospital for more than 24
hours or carried out in day care Centre.
Complainant aggrieved with the rejection of the claim and filed complaint before this Forum with
request to settle this claim.
Contentions of the Respondent Insurer (RI):
RI has not submitted its Self-Contained Note.
However, as per rejection letter, patient was treated for Degenerative lumber spondylitis from
14/11/2019 to 20/11/2019. It is evident that as per claim documents received it is observed that the
treatment given to the patient does not support the need for hospitalization and treatment can be
availed on OPD Basis hence claim is repudiated under 1.21(b).
Clause 1.21(b)
‘Procedure/ treatment usually done in outpatient department are not payable under the policy even
if converted as an inpatient in the hospital for more than 24 hours or carried out in day care Centre.
‘
Result of personal hearing with both the parties (Observations & Conclusions):
During the online hearing held on 22/09/2021, both the parties reiterated their respective stand.
As per discharge card patient was having severe backache with inability to walk since two to three
days. Patient was kept under observation for 3 days after doing SNRB procedure. No MRI
investigation is done during the hospitalization. Procedure is done without any investigation.
Physiotherapy is done during hospitalisation as per case bill.
It is observed from the papers submitted by the complainant that SNRB procedure was done on
16/11/2019 under local anesthesia. As per net search:
‘A selective nerve block (SNRB) is the injection of a local anesthetic along a specific nerve root. This
procedure is used primarily to diagnose nerve root compression. SNRB injections are isolated to
various locations along the spine to determine which nerve root is causing the pain. If the patient’s
pain dissipates after the injection at a particular nerve root, it can be inferred that the source of pain
was being generated at the selected nerve root. Along with acting as a diagnostic tool, SNRBs can
alleviate the discomfort associated with nerve root compression when used with an injectable ster-
oid.
Administering a selective nerve block only takes a few minutes, but it is recommended to allow an
hour for the entire visit, including a pre-operative consultation with the physician as well as post-
operative observation.’
In view of the above observations, this treatment can be considered under day care treatment only.
As conveyed by the complainant, for physiotherapy, it was not possible for the patient to visit the
hospital everyday as they stay 60-70 km away from the hospital. Complainant is made aware that
stay in hospital due to this reason is not payable under the policy terms and conditions. Policy grants
stay in hospital if the patient needs medical observation for more than 24 hours continuously.
It is observed that the hospital bill is exorbitantly on higher side. Surgeon fees, anesthesia and as-
sistant charges for one injection, charged at Rs.38500/-in total, is not justifiable. Forum finds follow-
ing charges as payable considering the admissibility of claim under day care treatment.
Room charges inclusive of nursing for one day
Rs.2000
Instrument handling charges
Rs.2500
Theatre charges
Rs.5000
Dressing, saline, physio, x-ray
Rs.4150
Anesthetist
Rs.2000
Surgeon fees
Rs.5000
Total
Rs.20650
Complainant has not produced bills for medicines. The RI may consider the genuine bills for the
same if produced by the complainant within 10 days from the receipt of this award.
Complaint is thus allowed partially.
Award follows:
AWARD
Under facts and circumstances of the cases, the Respondent Insurer is directed to pay Rs. 20,650/-
plus genuine bills for the medicines incurred for SNRB treatment, if produced by the complainant
within 10 days from the receipt of this award, to the Complainant towards full and final settlement
of this complaint.
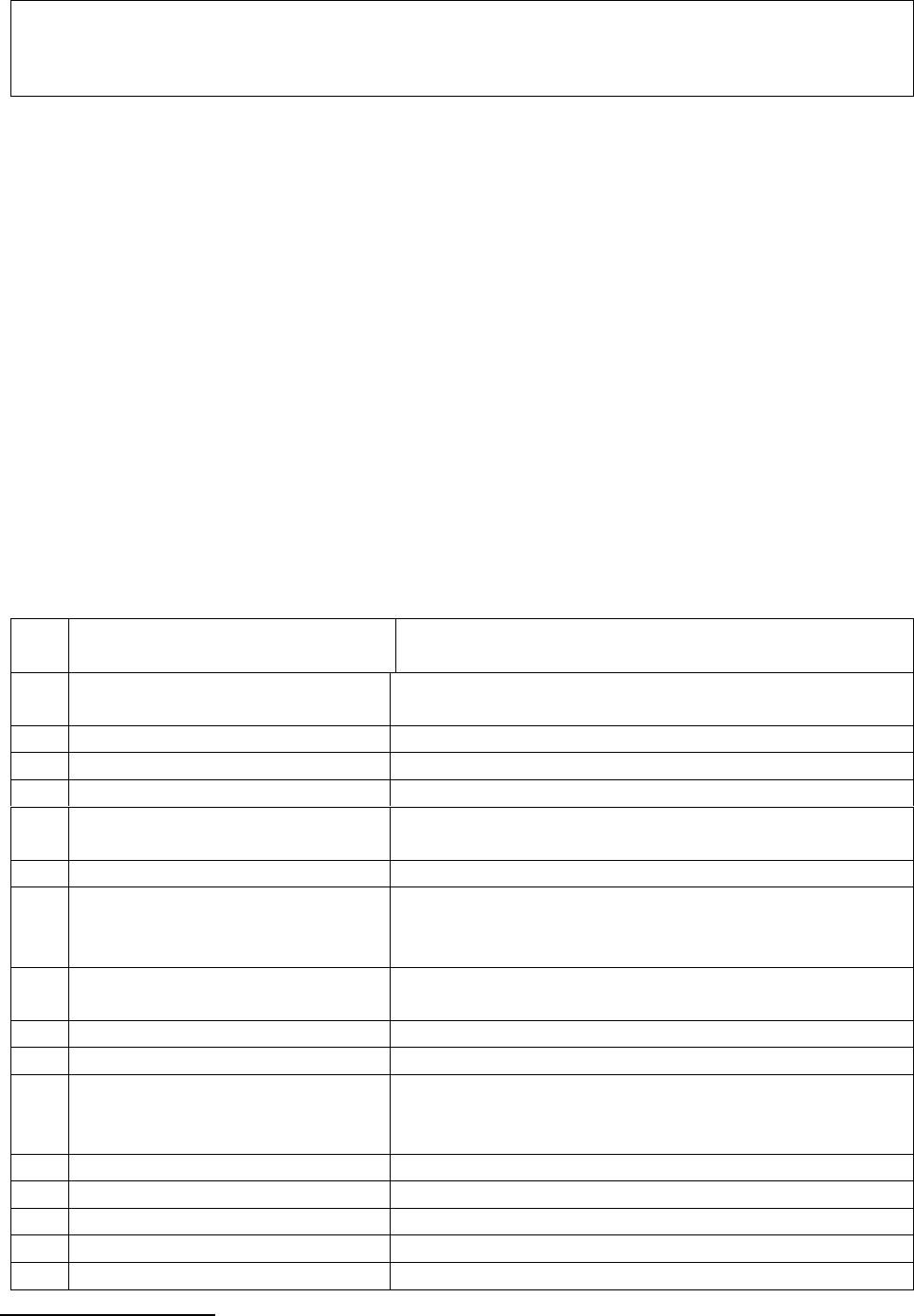
The award is to be satisfied within one month from the date of receipt of this award failing which
it will attract interest at the applicable bank rate plus 2% extra from the date of rejection of the
claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune on this 30
th
day of September 2021
VINAY SAH
Insurance Ombudsman,
Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Bharat M. Thakkar Vs The Oriental Insurance Co. Ltd
COMPLAINT NO: PUN-H-050-1920-0696
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Bharat Mohanlal Thakkar, Thane
2.
Policy No:
Type of Policy:
131401/48/2019/6049
Happy Family Floater 2015. Silver Plan
3.
Policy period:
14/12/18-13/12/19
4.
Sum Insured
300000/-
5.
Date of inception of first policy:
14/12/2011
6.
Name and age of the Insured:
Name of the Policyholder:
Mrs. Asha-spouse, Age 50
Mr. Bharat Thakkar
7.
Name of the Insurer:
The Oriental Insurance Co. Ltd
8.
Reason for repudiation/Partial
Settlement:
Dental treatment or surgery unless arising from disease
or injury and which requires Hospitalization for
treatment is not covered
9.
Date of receipt of the
Complaint:
07/02/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
59387+10000/-(penalty) =69387/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
13 1(b)
13.
Date of hearing/Place:
Online hearing on 13.08.2021
14.
Representation at the hearing
s) For the Complainant:
Himself
t) For the insurer:
Mr. Mithilesh Choubey; Ivy Ghosh
15.
Complaint how disposed:
Allowed
Brief facts of the case:
The complainant is having Happy family floater policy since 2011 for his family members for sum
insured of Rs.300000/-. The complainant submitted two claims for his wife for mouth abscess.
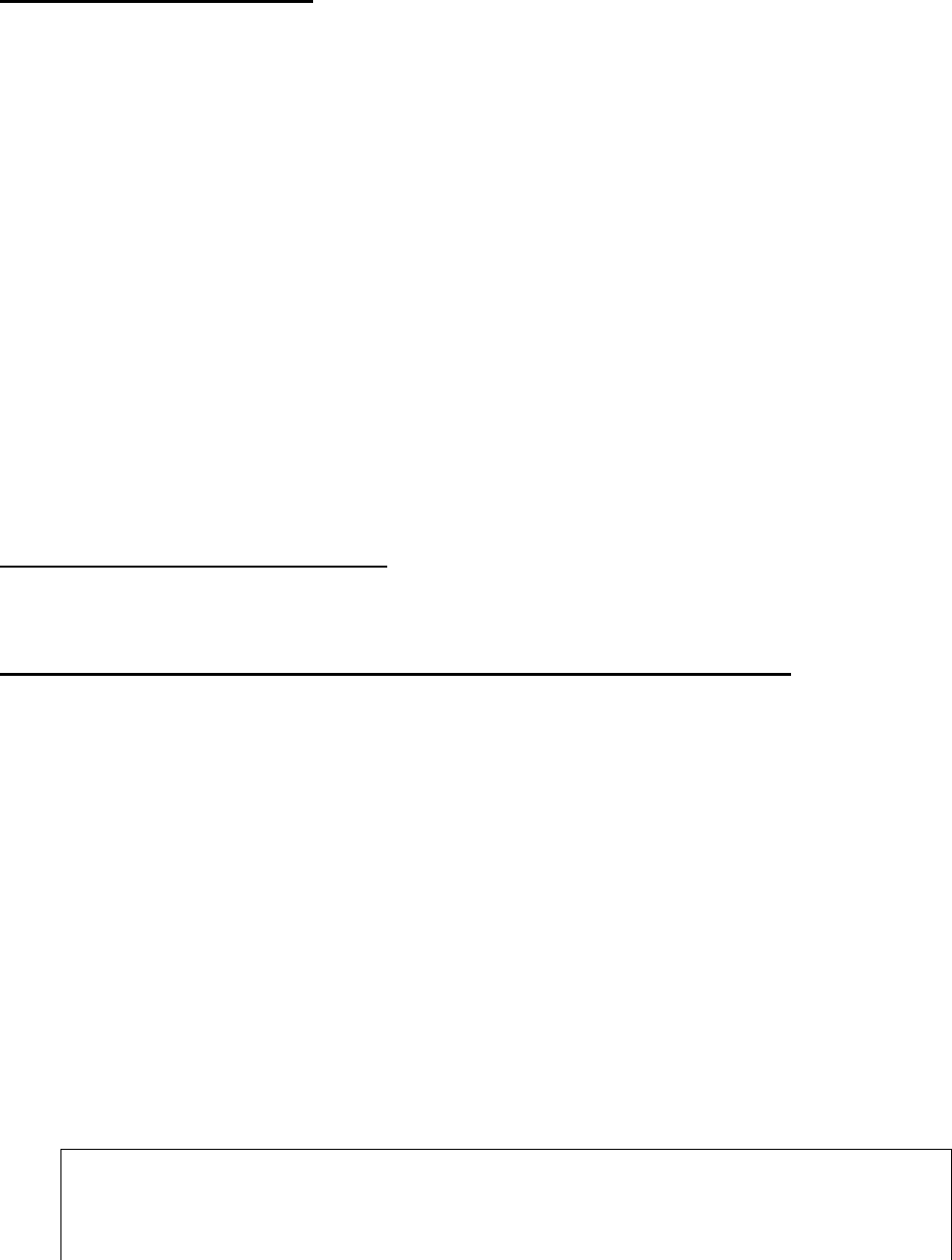
The claim of D Y Patil hospital for Buccal Abscess for the period 25/2/2019-2/3/2019 is settled by
the RI. The second claim of Param Hospital for same problem for the period 13/3/2019 to 19/3/2019
is rejected.
Hence, complainant has filed complaint before this Forum for resolution of the issue and settlement
of his claim.
Contention of the complainant:
The complainant had submitted reimbursement claim of his wife for admission in Param Hospital for
the period 13/3/2019-19/3/2019 for the treatment of abscess in mouth. The claim was not settled
despite follow up for more than 5 months. When he was expecting settlement of his rightful claim,
he received rejection letter stating:
“Dental treatment or surgery which is corrective, cosmetic or of aesthetic procedure, filling of cavity,
crowns, root canal treatment including treatment of wear and tear etc. unless arising from disease or
injury and which requires Hospitalization for treatment is not covered”
To this he clarified as below:
➢ My wife’s medical treatment was done for abscess in mouth (Tuberculosis) and not for dental
treatment.
➢ The treatment given required proper hospitalization.
➢ Hospitalization was must as she was there for 6 days and IV antibiotics were given which
cannot be given on OPD basis.
➢ Diagnosis of Tuberculosis was detected from the abscess histopathology report and at present
she is on anti TB medicine.
➢ Earlier claim was paid at D Y Patil hospital for the same disease.
➢ Param hospital has given clarification for erroneously written as Dental abscess.
As per complainant rejection of his claim is on wrong grounds and for wrong interpretation of the
policy claim document clause 4.7.
Contention of the Respondent Insurer:
As per rejection letter, patient has undergone Dental treatment which is excluded from the scope of
the policy. Hence, claim falls under exclusion clause no. 4.7 of the policy Terms and condition.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 13.08.2021 (through video-conferencing) both the parties reiterated
their respective stand.
RI representative submitted that diagnosis mentioned in Param Hospital discharge card is ‘Dental
abscess’. Hence, current claim is purely a dental treatment. Moreover, they have taken 2
nd
opinion of
maxofacial doctor also, who endorsed their views.
It is observed by the forum that the treatment was for buccal space infection (MRSA). The treatment
was not done by a dentist but by a physician Doctor Seetha Raju (MD, DTCD). Param Hospital
certifies that this treatment is a continuous treatment from D Y Patil Hospital. Histopathology report
of SRL diagnostics mentions IMPRESSION: GRANULOMATOUS INFLAMMATION OF LIKELY
MYCOBACTERIAL ETIOLOGY. After param Hospital, P D Hinduja Hospital prescriptions dt.
24/4/19, 10/7/19 & 6/11/19 are found for patient taking TB treatment. Which the RI has overlooked.
The focus is also drawn on the correct interpretation of the policy clause. The exclusion applies if the
dental treatment/surgery is 1) Corrective or 2) cosmetic or 3) aesthetic procedure and filing of cavity,
root canal. The current treatment is 1) not corrective 2) not cosmetic 3) not aesthetic procedure and
also not root canal/filing of cavity.
In view of this, complaint is admissible. Award follows,
AWARD
Under the facts and circumstances, the RI is directed to pay Rs. 59387/-less deductible
as per the terms and conditions of the policy to the complainant, towards full and final
settlement of the complaint.
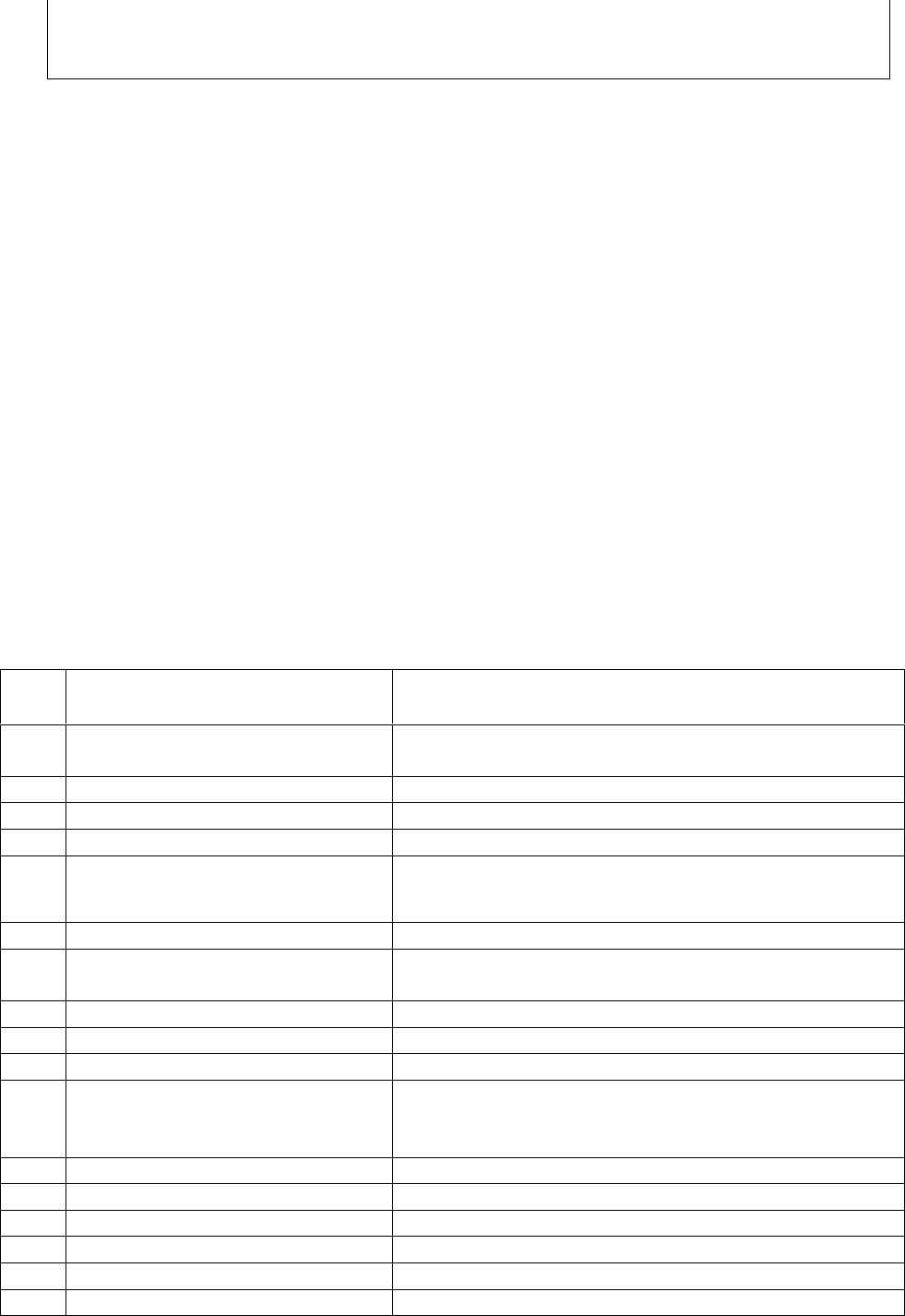
The award is to be settled within one month from the date of receipt of this award failing
which it will attract interest at the prevailing bank rate plus 2% extra from the date of
rejection of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award
and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune, this on 15
th
day of September, 2021.
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– SHRI VINAY SAH
CASE OF Mrs. Binu Mathew v/s Manipal Cigna Health Insurance Company Ltd
COMPLAINT NO: PUN-H-053-2021-0073
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mrs. Binu Mathew,
Nagpur
2.
Policy No:
Type of Policy:
PROHLN000274555
Pro- Health Plus Insurance
3.
Policy period:
28/11/2019-27/11/2020
4.
Sum Insured:
10,00,000/- per insured
5.
Date of inception of first policy:
28/11/2019
6.
Name and age of the insured:
Name of the Policyholder:
Sanju Mathew Sam; 29 years; Husband
Binu Mathew
7.
Name of the Insurer:
Manipal Cigna Health Insurance Company Ltd
8.
Reason for repudiation/Partial
Settlement:
First 30 days waiting period
9.
Date of receipt of the Complaint:
27/7/2020
10.
Nature of complaint:
Repudiation of claim
11.
Amount of Claim:
24078/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
13 1( b)
13.
Date of hearing/Place:
On line hearing on 22.09.2021
14.
Representation at the hearing
u) For the Complainant:
Herself with husband Sanju Mathew
v) For the insurer:
Mr Jaswinder Singh Shekhawat
15.
Complaint how disposed:
Dismissed
16.
Date of Award:
23.09.2021
Brief facts of the case:
Complainant is having Pro Health plus policy with Respondent Insurer (hereinafter is called RI) for
the period 28/11/2019-27/11/2020. After 30 days from the inception of the policy, complainant has
filed claim for her husband, Mr. Sanju who was admitted in Wockhardt Hospital for the period
29/12/2019 to 31/12/2019 for the illness Pneumonia.
RI has rejected the claim giving reason that illness was contracted during first 30 days from the
inception of the policy. Complainant aggrieved with the decision of the RI filed complaint before this
Forum for resolution of the issue.
Contentions of the Complainant:
Complainant admits that her husband, Mr. Sanju was having fever one week before the date of
admission i.e. 29/12/2019, but it was cured by common home remedies and he was feeling better.
They informed the Doctor about the same. But it was wrongly assumed by the insurance claim team
and they rejected his claim stating pre-existing disease/illness. They came to hospital on 29/12/2019,
as Mr. Sanju had chest discomfort and weakness in that morning. After blood test and x ray they came
to know that he was having typhoid, Pneumonia. Before that they were not aware of this.
She has requested the forum to settle their claim considering the above facts as it has nothing to do
with the previous common fever.
Contentions of the Respondent:
The complainant had made cashless request for hospitalisation of her husband for Left lower lobe
Pneumonia. However, since it was observed from the treatment papers that the claim was not
admissible as the ailment/illness was contracted during the initial 30 days from policy inception.
Hence the cashless request was denied. Further, the complainant registered reimbursement claim for
Rs. 24,645/- incurred for this hospitalisation due to fever with chills, cough, weakness and chest
discomfort since last one week.
It is submitted that the discharge summary clearly specifies that the complainant had been suffering
from the symptoms since 1 week prior to hospitalisation on 29/12/2019 which implies that the ailment
was contracted during the initial 30 days from policy inception. As per the policy terms & conditions,
claims for illness/ailments contracted during the initial 30 days from policy inception are not payable.
Therefore the claim was rejected under clause V.2 as follow
V.2. 30 days Waiting Period “Any disease contracted and/or Medical Expenses incurred in respect of
any Disease/Illness by the Insured/Insured Person during the first 30 days from the inception date of
the Policy will not be covered”.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 22.09.2021 (through video conferencing), both the parties reiterated
their respective stand.
Complainant contended that her husband had suffered from fever, cough and cold, which any person
can suffer from. Hence, it should not be considered as any pre-existing disease. RI representative
clarified that the claim was rejected on the grounds of 30 days waiting period; not on the grounds of
pre-existing disease. Forum finds the Discharge summary of Wockhardt hospital, Nagar clearly
specifies that Mr Sanju was suffering from the symptoms since one week prior to hospitalization on
29.12.2019 (although, it was diagnosed on 29 December, i.e. after 30 days of policy inception).
Complainant is not objecting to having fever and other symptoms one week before. But their
objection is on calling as minor as the common flu as “illness”. They contend that as the 30 days are
completed on the date of hospitalisation, as per policy terms the claim should be paid.
Forum clarifies that the term ‘disease’ or ‘illness’ is not necessarily used only for serious types of
health problems. It can also mean any ailment or condition which required treatment and/or
hospitalisation. In the instant case, the ailment having been contracted within the waiting period,
attracts the exclusion clause V2 as stated above.
In view of above, complaint does not sustain.
Award follows,
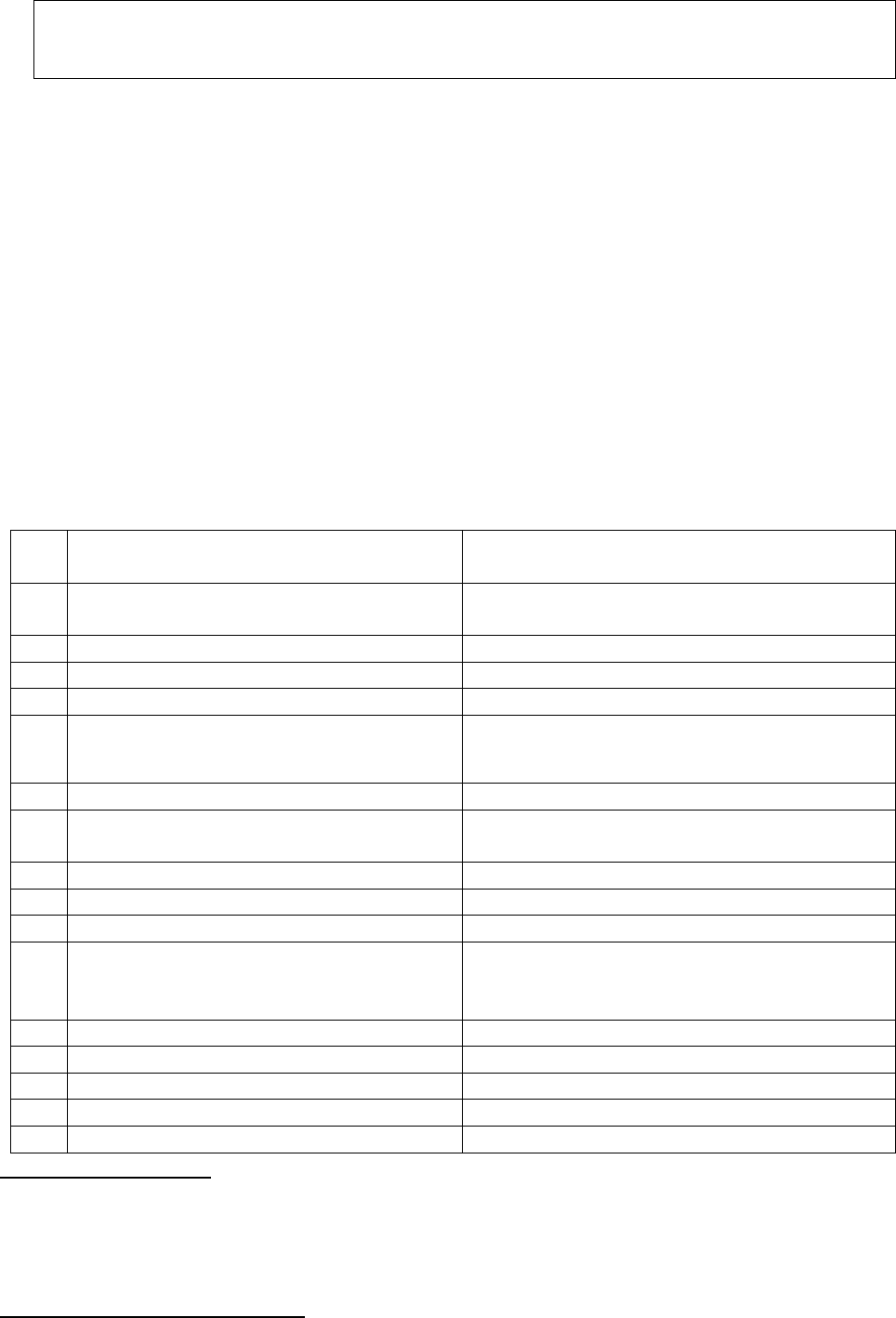
AWARD
Under the facts and circumstances, the decision of rejection of claim is found correct and
needs no intervention. Complaint therefore stands dismissed.
Dated: On this 23rd day of Sept, 2021, Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Champalal Rathi Vs Star Health and Allied Insurance Co. Ltd.
COMPLAINT NO: PUN-H-044-1920-0379
Award No IO/PUN/A/HI/ /2020-21
1.
Name & Address of the Complainant
Champalal Rathi, Pune
2.
Policy No:
Type of Policy:
P/151112/01/2019/017334
Family Health Optima Insurance Plan
3.
Policy period:
31/12/2018-30/12/2019
4.
Sum Insured
Rs. 500000/-
5.
Date of inception of first policy:
31/12/2016
6.
Name and age of the Insured:
Name of the Policyholder:
Devibai Rathi; wife; 58 years
Champalal Rathi
7.
Name of the Insurer:
Star Health and Allied Insurance Co. ltd
8.
Reason for repudiation/Partial
Settlement:
Total Repudiation of Claim for non-disclosure
of surgery for Acromegaly
9.
Date of receipt of the Complaint:
20/09/2019
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
Rs.25000/- and to restart the insurace
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
13 1(b)
13.
Date of hearing/Place:
Online hearing on 14/06/2021
14.
Representation at the hearing
w) For the Complainant:
Mr. Rakesh Rathi (son)
x) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Disallowed
Brief facts of the case:
The complainant was having health insurance policy with Respondent Insurer (herein after is called
RI) since December 2016. The spouse of the complainant was admitted in Kamal Nursing Home,
Pune from 10/6/2019 to 13/6/2019. Her claim was rejected by the RI on the grounds of non-disclosure
of her pre-existing disease of Acromegaly. Also, her name was cancelled from the policy.
Contention of the Complainant:
As per complainant, while taking the policy, they have done proper medical check up & given all the
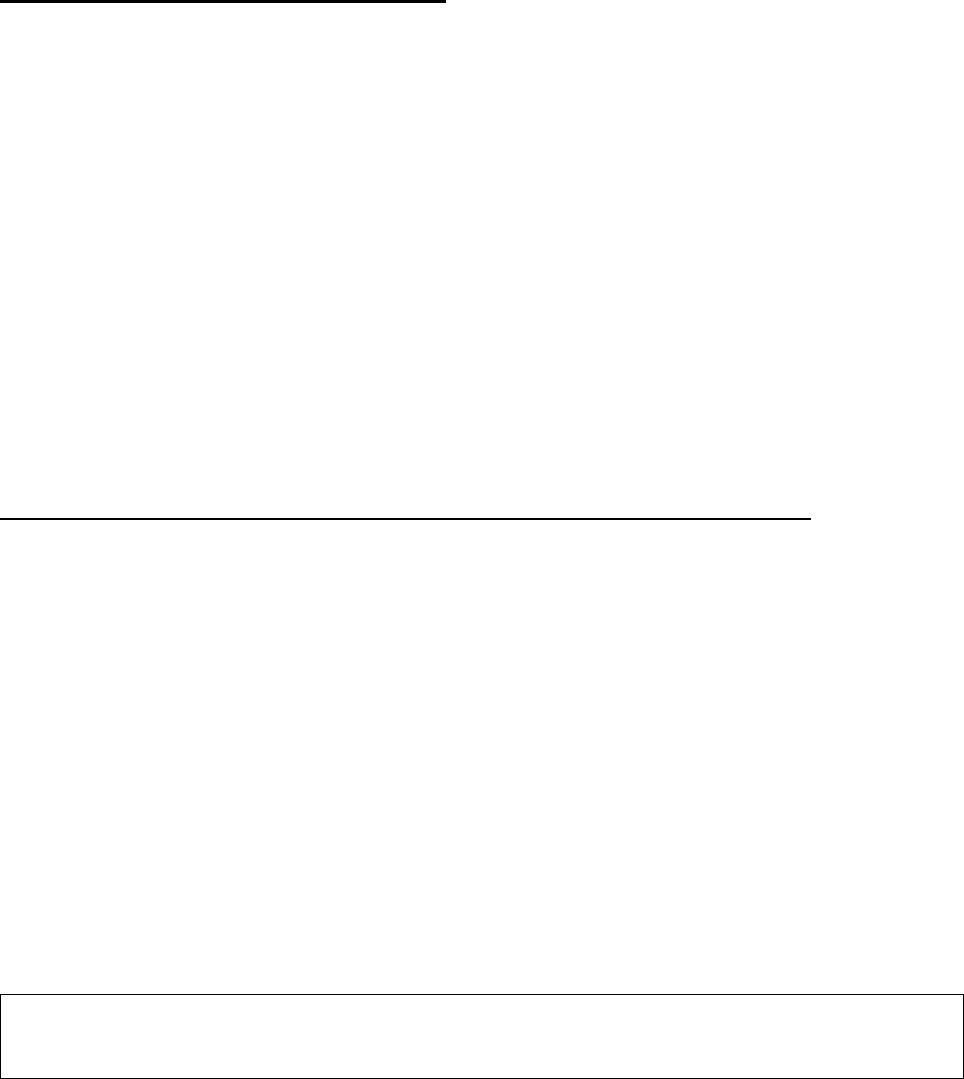
details of her medicines, treatment and operation honestly but Mrs. Rathi forgot to disclose the
operation of Acromegaly done in 2007 since the operation was done 12 years ago. It is natural human
tendency to forget the things done 12 years back. There was no intention to non-disclose the fact.
Also, there is no relation between this operation and the admitted disease. He is requesting the forum
to consider this issue and approve the claim as well as restart the policy.
Contention of the Respondent Insurer (RI):
The insured Mrs. Devibai Rathi was covered under the Family Health Optima policy with declared
PED Calculus of urinary system, Diabetes & Hypertension and their complications. The insured
person Devibai Rathi was hospitalized at Kamal nursing home, Pune on 10/06/2019 for UTI with
Anemia with AKI. The proposer preferred a request for cashless treatment on 11/06/2019. As per the
consultation report of Dr. Kaustubh Dindorkar dated 16/11/2018, the insured was operated for
Acromegaly 12 years back in 2007 in KEM, Pune. This was not disclosed at the time taking the policy.
In the proposal form, all the health related questions asking about any diseases, treatment, surgery,
hospital admission are replied in the negative. It is clearly evident that the proposer was well aware
of the past medical history of the insured person and deliberately did not disclose the above mentioned
medical history/health details which tantamounts to mis-representation/non-disclosure of material
facts.
Hence, RI has rejected the claim as per condition no. 6 of the policy vide letter dated 12/06/2019.
Also, as per condition no. 12 of the policy, company cancelled the risk of Mrs. Devibai from the
policy with effect from 27/07/2019.
They further submit that they had rejected only the cashless authorization and the insured has not
approached for reimbursement of medical expenses.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 14/06/2021 (through video-conferencing), both the parties
reiterated their respective stand.
Complainant is not disagreeing to the fact of non-disclosure of PED pointed out by the RI. His
contention of his forgetting of these material fact while opting for the insurance is not acceptable, as
the same history, he had given to the hospital. The health history is a vital information to be disclosed
in health insurances; the non-disclosure of the same deprives the insurer in evaluating the risk.
Consequently the insurance contract between the parties becomes voidable and unenforceable.
Complainant was insisting for the continuation of policy. RI submitted that it is a declined risk, cannot
be considered for reinstatement.
In view of this, forum does not want to intervene in their decision in view of the clear cut violation
of the underlying principle of ‘Utmost Good faith’ of insurance contract.
Complaint thus disallowed.
Award follows:
AWARD
Under the facts and circumstances, it is found that the decision of repudiation of claim and
cancellation of policy needs no intervention. Complaint therefore stands dismissed.
Dated: at Pune on this 27
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
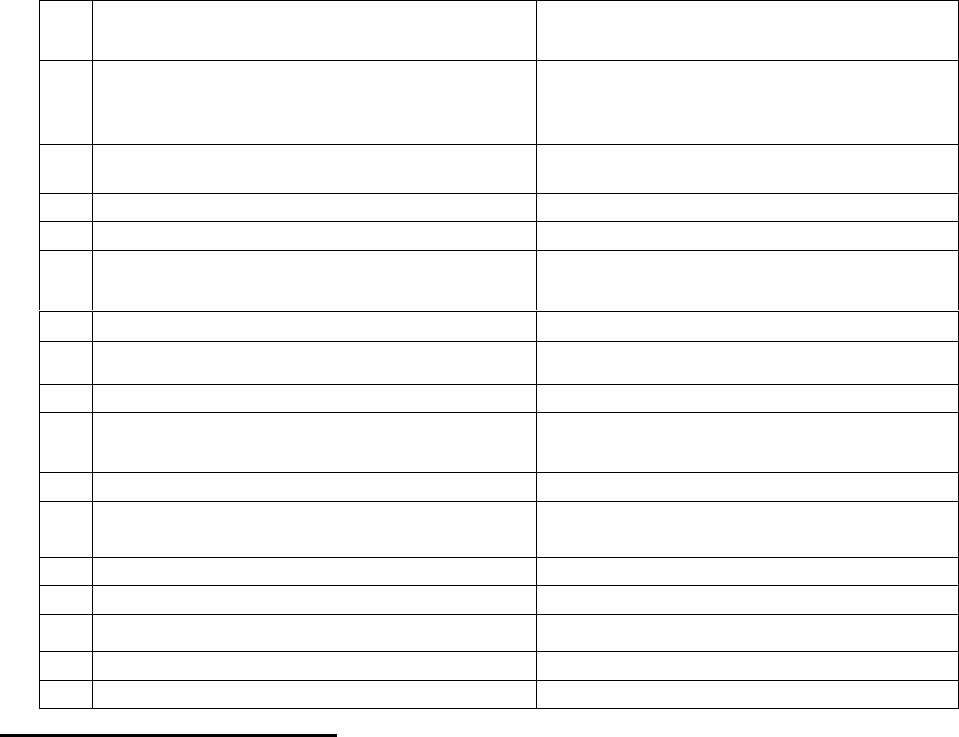
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Deepak Uttam Mane V/S Star Health & Allied Insurance Company Limited
COMPLAINT NO: PUN-H-044-1920-0514
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Deepak Uttam Mane,
Indapur Road, Baramati, Dist- Pune.
2.
Policy No:
Type of Policy:
P/151119/01/2020/003407
Senior Citizen Red Carpet Health
Insurance Policy.
3.
Policy period:
15/06/2019 to 14/06/2020
4.
Sum Insured/IDV
Rs. 5,00,000/-
5.
Date of inception of first policy:
15/06/2019
6.
Name & age of the Insured:
Name of the Policyholder:
Mrs. Shalan Uttam Mane, 61 Years.
Mr. Deepak Uttam Mane.
7.
Name of the Insurer:
Star Health & Allied Insurance Co. Ltd,
8.
Reason for repudiation/Partial Settlement:
Pre-existing disease.
9.
Date of receipt of the Complaint:
20/11/2019
10.
Nature of complaint:
Reinstatement of Pol. & approval of
claim.
11.
Amount of Claim:
Rs. 45,701/-
12.
Rule of IO Rule under which the Complaint
was registered:
13(1)(b)
13.
Date of hearing/Place:
18/06/2021; Online
14.
Representation at the hearing
y) For the Complainant:
Himself
z) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:
Complainant purchased a Senior Citizen Red Carpet Insurance Policy for his mother Mrs. Shalan
Uttam Mane, 61 years, from RI (Respondent Insurer) having Sum Insured of Rs.500,000/-. The period
of insurance was from 15/06/2019 12:52: 00 Hrs to midnight of 14/06/2020.
She was diagnosed with CARCINOMA LEFT BREAST on 17/07/2019 and was admitted in Deenanath
Mangeshkar Hospital & Research Centre, Pune on 30/07/2019 for treatment and underwent LEFT
BREAST CONSERVATION SURGERY and SENTINAL LYMPH BIOPSY. She was discharged on 31/07/2019.
Complainant submitted a claim for reimbursement of medical expenses for Rs. 45,701/-. RI rejected
his mother’s hospitalization claim stating that she had this disease prior to the commencement of
first year policy which is termed as ‘Misrepresentation/non-disclosure of material facts’. In
response,he provided a letter from Dr. Seema Gawasne of Baramati who had first diagnosed her
mother on 17/07/2019. The Dr. has certified that Mrs. Shalan came to her on 17.7.2019. That was
the first time she noticed breast swelling on left side. Because of small size and being pain less, she
couldn’t have noticed it before that. This certificate was also not taken into consideration while
rejecting the claim.
RI, in addition to repudiation of claim also cancelled the policy due to non-discloser of material facts
while obtaining the policy for first time.
Hence, aggrieved by the rejection of his claim, complainant filed complaint with this forum for
resolution of his grievance.
Contentions of Respondent Insurer (RI):
As per Self Contained Note submitted by RI, the insured preferred a claim for reimbursement of
medical expenses incurred for sum of Rs. 45,701/- for treatment of his mother Mrs. Shalan Uttam
Mane, who was admitted at Deenanath Mangeshkar Hospital & Research Centre, Pune for treatment
of LEFT BREAST CANCER. She underwent left breast conservation surgery and sentinel lymph node
biopsy.
Complainant submitted a Pre-authorization Request for Cashless treatment on 30/07/2019 and the
same was denied immediately stating that further evaluation is required. Subsequently he has
submitted a claim for reimbursement of medical expenses on19/08/2019. On scrutiny it was observed
that
• As per the Cytology Report dated 25/07/2019 FNAC, Left breast lump was positive for malig-
nant cells and was suggestive of DUCT CARCINOMA.
• As per the USG report of the Breast dated 20/07/2019, the extent of breast lesion was 1.8x1.3
cm with 8 mm depth. Within the short span of 1 month, the insured could not have developed
this condition.
It is evident that the onset of the diagnosed disease was prior to the commencement of the policy. As
per submitted documents the insured was symptomatic of the diagnosed disease which is a Pre-
Existing disease that was not disclosed at the time of proposing the policy which would tantamount
to Non-disclosure of material facts. The present hospitalization is for treatment of the Pre-existing
disease and the non-disclosure of the same deprived the right of the insurer to evaluate the risk before
accepting the proposal. Hence, the claim was repudiated vide letter dated 20/09/2019 as per Condition
no. 9 of the policy which read as under,
“The Company shall not be liable to make any payment under the policy in respect of any claim if
information furnished at the time of proposal is found to be incorrect or false or such claim is in any
manner fraudulent or supported by any fraudulent means or device, misrepresentation whether by
the insured Person or by any other person acting on his behalf”
Subsequently, the policy was canceled w.e.f. 2/11/2019 as per condition no. 13.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 18/06/2021 (through video-conferencing), both the parties
reiterated their respective stand.
From the papers submitted on record and the contentions of complainant, it is observed that the
breast lump was first detected on 17/07/2019, which is after 33 days of the issue of the first policy
and on 20/07/2019 she was diagnosed with breast lesion was 1.8x1.3 cm with 8 mm depth. As
defended by the RI, to see the legitimacy of the duration which might require to develop a lump
upto this size, the forum took a web search on the subject and found following information:
"Doubling time" is the amount of time it takes for a tumor to double in size. But it's hard to actually
estimate, since factors like type of cancer and tumor size come into play. Still, several studies put the
average range between 50 and 200 days.
Insured in her representation to RI, is writing that on 17/07/2019, due to body ache and feverish
feeling, she visited Dr. Seema Gavasane, MBBS, DGO; who after checking her, advised to undergo
sonography & mammography. It is to be noted that for these complaints of general nature, she did
not go to a general physician but went to a gynecologist.
In view of this, there is scope to believe that the patient insured must be having symptoms and or
lump since many days, more than a month. Complainant could have produced more
documents/prescriptions/reports in support of his contention to prove that there was no such
symptom, prior to first policy inception date. In absence of no such proof, forum has to believe the
said studies and the fact of non-disclosure has to be relied upon.
Complaint is thus not admissible for claim payment and also for policy reinstatement.
Award follows:
AWARD
Under the facts and circumstances of the case, forum finds that the complaint is devoid of
merits, hence dismissed.
Dated: at Pune this 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. DHARMARAJ D LUBAL V/S UNIVERSAL SOMPO GEN INS CO LTD
COMPLAINT NO: PUN-H-052-2021-0683
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. DHARMARAJ D LUBAL
SOLAPUR
2.
Policy No:
Type of Policy:
2825/58739159/02/000
COMPLETE HEALTHCARE
POLICY(family floater )
3.
Policy period:
31.07.2020 TO 30.07.2021
4.
Sum Insured
300000 + 60000 Bonus
5.
Date of inception of first policy:
31.07.2018
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr. Vijaylaxmi D Lubal, 59 yrs
Mr. Dharmaraj D Lubal
7.
Name of the Insurer:
Universal Sompo Gen Ins Co Ltd
8.
Reason for repudiation/Partial Settlement:
Partial repudiation.
9.
Date of receipt of the Complaint:
05.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Equal to full SI
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
aa) For the Complainant:
Absent
bb) For the insurer:
Dr. Ahmed Ali
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:-
• The complainant had taken complete health care Policy with Respondent Insurer (RI) The
Universal Sompo Gen Ins Co Ltd for self and wife for Sum insured (SI) of Rs.3L. He lodged
a claim of his wife’s hospitalization in Ashwini co-op hospital & Research Centre from
27.10.2020 to 07.11.2020 for Covid 19 positive. Total claim amount came to Rs.4,68,512 and
his SI was Rs.360000/- of that RI has paid the claim in two instalments viz. Rs.2,98,000 + Rs.
5,650 = 3,03,650/-. The complainant himself is a doctor DMS(DIP) MBBS(GOVT MAH)
Prajakta Hospital, Solapur.
• The complainant is requesting forum to intervene for settlement of claim amount equal to his
full SI and bonus.
Contentions of the Respondent Insurer (RI):-
As per SCN, DEDUCTION AMOUNT details are as shown below:
Expense head
Deduction
Reason
1) Room &
Nursing
charges
3500
Inclusive in covid package
Medicine &
Consumable charges
83429
Paid for high end antibiotics and anti-viral
and rest inclusive of covid package
Profession fees
charges
700
Inclusive in covid package
Investigation charges
24070
Paid for D-Dimer, covid test, ferritin, abg,
pct and rest inclusive of covid package
Misc charges
23234
Inclusive of covid package
3) Medicine &
Consumable
charges
29950
As per Maharashtra state govt.norms Covid
19 package applicable for ICU ward
Rs.7500/- day
Investigation charges
15110
Same as above
Misc Charges
500.00
Other charges not payable
Result of personal hearing with both the parties (Observations & Conclusions):
Dispute here is pertaining to the less amount received by the complainant. The major deduction made
by the RI is based on Maharashtra Govt. guidelines and GI council package rates. The same are not
conveyed to the insured public by the RI. The policy does not have such condition in the policy.
Hence, the deductions on these counts are not acceptable. In view of the clear cut instructions of
IRDAI to settle the claims as per policy terms and conditions, the forum finds that these amounts are
payable. Whereas, the balance sum insured is Rs. 56,350/- only. The deduction of Rs. 83,429/-
towards the medicines itself is crossing this amount. The RI therefore, is ordered to pay the balance
amount of sum insured rounded off to Rs. 56,000/-
Complaint thus allowed.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to
pay to the complainant Rs.56,000/- towards full and final settlement of this complaint.
The award is to be complied with one month from the date of receipt of this award
failing which it will attract interest at the applicable bank rate plus 2% extra from the
date of rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers
Dated: at Pune on this 15
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR.GAURAV S RAISONI V/S STAR HEALTH &ALLIED INS CO LTD
COMPLAINT NO: PUN-H-044-2021-0561
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Gaurav S Raisoni,
Jalgaon
2.
Policy No:
Type of Policy:
P/151122/01/2020/000493
Family Health Optima Insurance Plan
3.
Policy period:
05.05.2020 to 04.05.2021
4.
Sum Insured
Rs.400000
5.
Date of inception of first policy:
05.05.2018
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr. Subhash K Raisoni, 60 yrs
Mr Subhash Khupchandji Raisoni
7.
Name of the Insurer:
Star Health & Allied Insurance Co Ltd
8.
Reason for repudiation/Partial Settlement:
Paid as per make shift package charges
9.
Date of receipt of the Complaint:
22.02.2021
10.
Nature of complaint:
Payment of Balance claimed amount
11.
Amount of Claim:
Rs.42165/-(Ann VI A)
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
cc) For the Complainant:
Himself
dd) For the insurer:
Dr.Anjali Rathod
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:-
• The complainant is the son of Shri Subhash Raisoni. Mr. Subhash Raisoni had taken Family
health optima insurance plan with Respondent Insurer Star Health & Allied Insurance Co Ltd
for self and his family for Sum Insured of Rs. 4 lakh. The complainant lodged claim of his
father’s hospitalization in Jito Covid care center, Tarsod, Jalgaon from 03.10.2020 to
12.10.2020 for Covid 19 positive. The total expenditure of the treatment was Rs.55495 /- .
Approved amount Rs.13330/- and deduction amount Rs.42165/-.
• The Complainant is requesting forum to intervene for full settlement of claim amount
Contentions of the Respondent Insurer (RI):-
As per SCN, initially, they had settled the claim for Rs.13330/- on 03/12/2020.
On receipt of notice from this office, they reviewed the claim once again and considered for settlement
for Rs.32813/- as detailed below:
Payable amount for hospitalization Rs.
40323
Pre hospitalization claim Rs.
5820
Total Amount payable Rs.
46143
Less amount already paid Rs.
13330
Balance amount payable Rs.
32813
Result of personal hearing with both the parties
Complainant has raised objection for the deductions of Rs.3856/- (Rs.460/-pre hospitalization bill for
no prescription, Rs.416/- for post hospitalization for same reasons and Rs.2980/- for no reports).
Complainant has forwarded the scanned copies of these documents alleging that he had already
submitted these documents to the RI. In view of this, forum directs the RI to consider this amount
also, if the submission of those documents are upto their satisfaction.
Complaint allowed.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to pay balance
amount of Rs.32,813/-plus the deducted amount of Rs. 3856/- if that amount is found payable,
to the complainant towards full and final settlement of the complaint.
The award is to be complied with within one month from the date of receipt of this award failing
which it will attract interest at the bank rate plus 2% extra from the date of rejection of claim
till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: On 21/09/2021 at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
The deductions of Rs.3856/- are:
Rs.460/-pre hospitalization bill for no
prescription,
Rs.416/- for post hospitalization for same
reasons and
Rs.2980/- for no reports
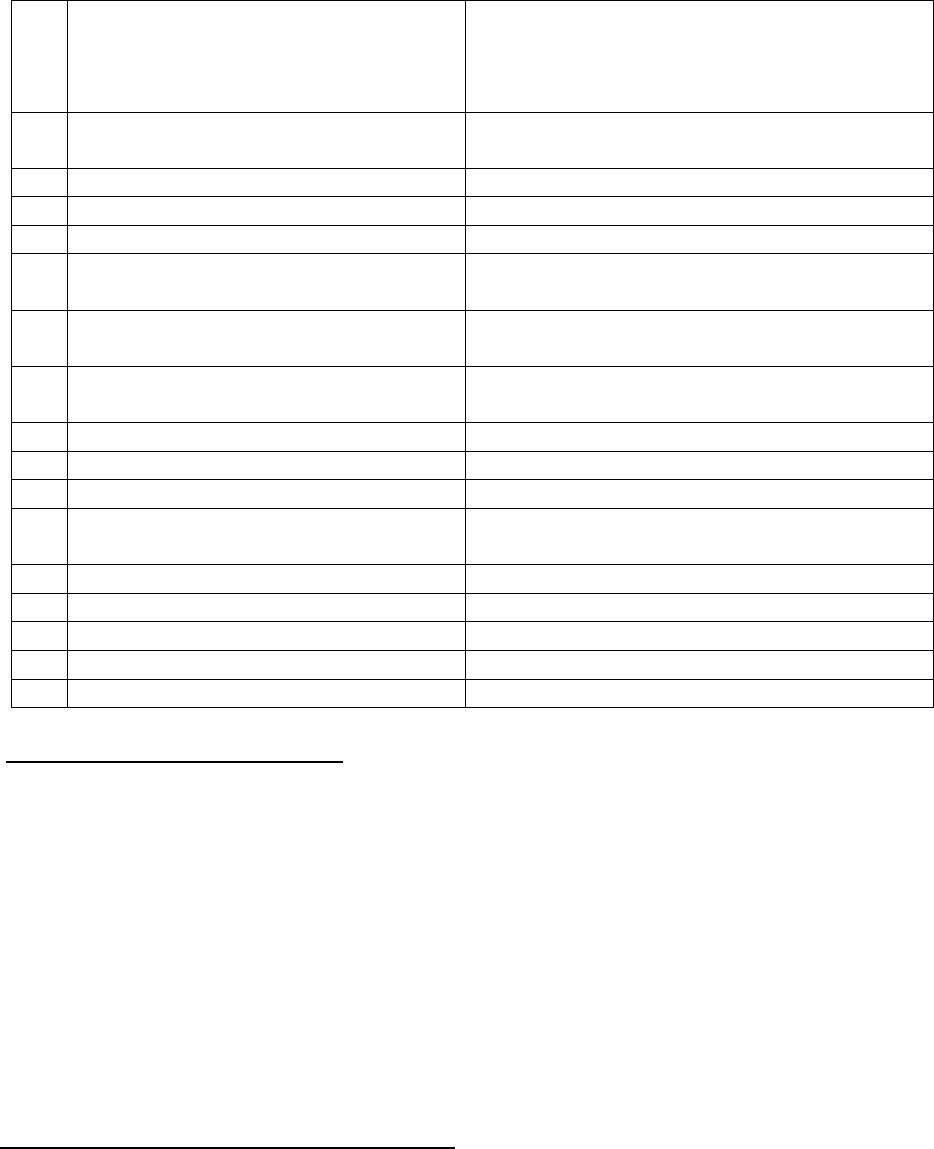
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Hansraj Mali Vs. Bajaj Allianz General Insurance Company Ltd.
COMPLAINT NO: PUN-H-005-1920-0547
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. Hansraj D. Mali
Plot No.45, Sec-18/A, Nerul,
PO Area – Nerul NOD, Thane – 400706
(M.S.)
2.
Policy No:
Type of Policy:
OG-19-1911-8430-00001752
Health Guard (Floater) Policy
3.
Policy period:
16/03/2019 to 15/03/2020
4.
Sum Insured/IDV
Rs.2 lakhs
5.
Date of inception of first policy:
6/03/2014
6.
Name & age of the Insured:
Name of the Policyholder:
Ms. Vidhi Mali – Age: 17 years; Daughter
Mr. Hansraj D. Mali
7.
Name of the Insurer:
Bajaj Allianz General Insurance Company
Ltd.
8.
Reason for rejection /Partial
Settlement:
Misrepresentation – discrepancies noted in
claim documents
9.
Date of receipt of the Complaint:
12/05/2019
10.
Nature of complaint:
Rejection of health claim
11.
Amount of Claim:
Rs.33,207/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021, Online. Pune
14.
Representation at the hearing
ee) For the Complainant:
Himself.
ff) For the insurer:
Mr. Irfan and Dr. Ravindra Shingte.
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:
Complainant and his family (Spouse, son and two daughters) were insured with the Respondent
Insurer (RI) under the above policy for the period 16/03/2019 to 15/03/2020. His youngest daughter
Vidhi, aged 17 years was hospitalized at Shree Siddhivinayak Hospital, Mumbai on 22/03/2019 with
history of high grade fever, nausea, body ache, headache, weakness, giddiness and lethargy. Final
diagnosis was Enteric Fever. After treatment she got discharged on 26/03/2019. After the claim
documents of the insured patient were submitted to the RI for reimbursement, the RI rejected the
claim stating that as discrepancies were noted
in the hospital documents, the claim is not payable as per the policy conditions. Grievance Cell of the
RI also not considered favorably.
Aggrieved with this decision, the complainant has approached the forum for resolution of his
grievance.
Contentions of the Respondent Insurer (RI):
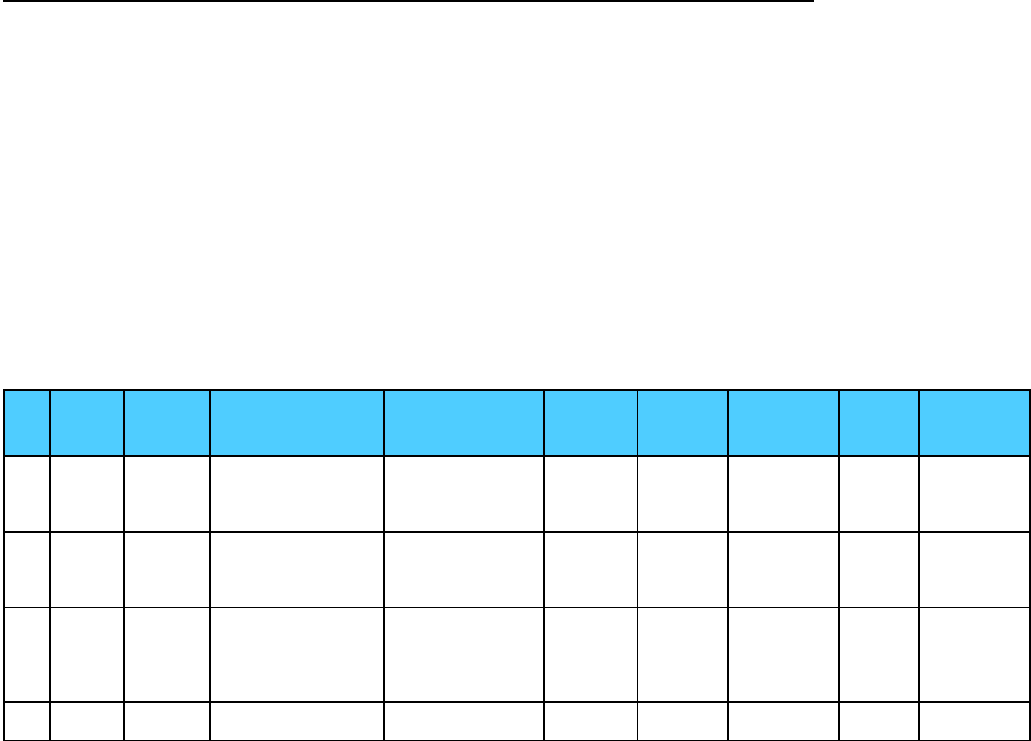
The RI has stated that the patient was admitted to Shree Siddhivinayak Hospital, Navi Mumbai on
22/03/2019 for treatment of enteric fever and was discharged on 26/03/2019. RI received
hospitalization claim of Rs.33,207/-. They appointed an investigator to investigate the claim. After
scrutiny of the claim documents and as per the report of the investigator, following discrepancies
were found in the claim documents.
• Dengue profile not done in view of high grade fever & headache. Inj. Hydrocort is used.
• As per widal test dt. 22 March, widal titre is not much high.
• culture sensitivity is not done,
• 3 vein flow used in 5 days admission,
• 2 consultants involved in enteric fever case,
• As per final bill, charges applied for A/C deluxe room. However, patient was admitted in
general ward. Rs. 2000/- applied for general ward charges & Rs. 550/- for nursing charges.
However, as per tariff list, general room rent is 800/- and nursing charge is 300/-.
• Investigation team also found discrepancies in the version of complainant as per the claim
files and the actual events as per records.
As a result, the RI repudiated the claim vide letter dated 27/08/2019 as per Definition B-17,
which is reproduced as under:
Definitions-B17 – “Disclosure to information norm – the policy shall be void and all premium paid
hereon shall be forfeited to the Company, in the event of misrepresentation, mid-description or
non-disclosure of any material fact.”
The RI has finally concluded that the claim has been rejected as per the policy terms and conditions
issued to the policyholder.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (through video-conferencing) both the parties reiterated
their respective stand.
Complainant was questioned about the RI’s findings on this hospitalization during their investigation.
To that he replied that he was at his home town in Rajasthan at that time; as such has no idea about
type of room, room rent etc. he could not satisfy any queries of Forum. Apart from RI’s findings viz.
hospital bill inflation, line of treatment not followed for enteric fever, cortico steroid used which is
generally used for 3
rd
stage of fever; on perusal of hospital papers, forum finds that everyday TPR
chart is recorded at midnight also at 12 am, 2 am, 4
am. On 26/03/2019, initially there were entries after 1 pm which were later scratched off as the patient
was shown discharged at 1 pm in discharge card.
During hearing Respondent Insurer was asked to submit the past claim history of the insured patient
Vidhi. The past claim details submitted by RI is as under:
Sr
No.
Patient.
Policy
No.
Hospital
Final Diagnosis
Actual
Date of
Admission
Actual
Date of
Discharge
Pay Status
Claimed
Amt
Approved
Amount
1
VIDHI
H
MALI
OG-10-
1911-
6001-
00000160
Shree Siddhivinayak
Hospital - Navi
Mumbai
LRTI
06-Aug-10
10-Aug-
10
PAID
9970
8793
2
VIDHI
H
MALI
OG-10-
1911-
6001-
00000160
Shree Siddhivinayak
Hospital - Navi
Mumbai
MALARIA
18-Jan-11
22-Jan-11
PAID
13415
11893
3
VIDHI
H
MALI
OG-11-
1911-
6001-
00000221
Shree Siddhivinayak
Hospital - Navi
Mumbai
SUB
MANDIBULAR
SWELLING WITH
HIGH GRADE
FEVER
18-Apr-11
22-Apr-11
PAID
14005
12424
4
VIDHI
H
OG-15-
1911-
Shree Siddhivinayak
Hospital - Navi
AFI with Enteric
Fever
29-Apr-15
04-May-
15
PAID
42566
38129
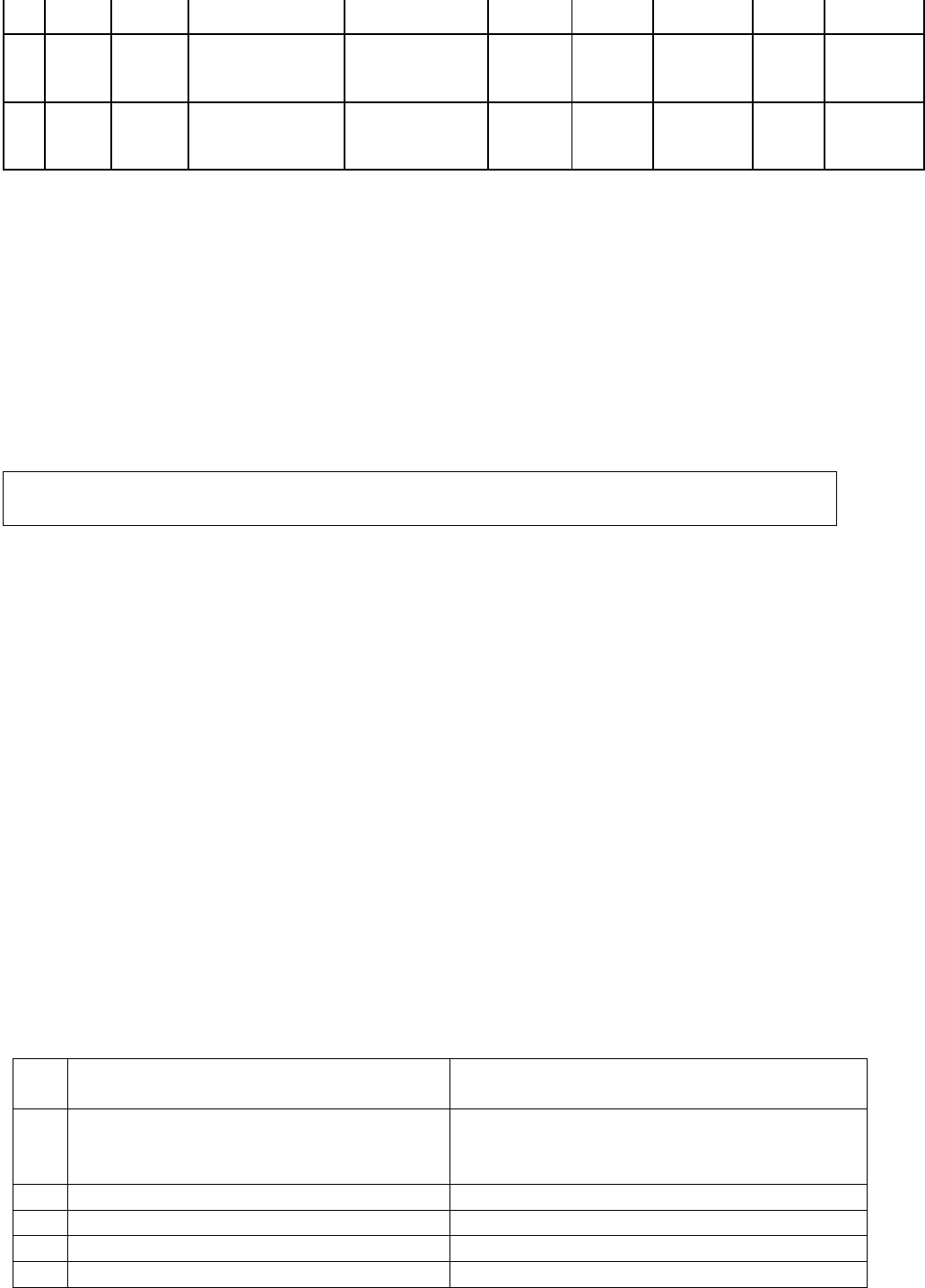
MALI
8417-
00000392
Mumbai
5
VIDHI
H
MALI
OG-18-
1911-
8430-
00001370
TERNA SPECIALITY
HOSPITAL AND
RESEARCH CENTRE
- Nerul
Granular Tonsillitis
with Viral Hepatitis
11-May-18
15-May-
18
PAID
14091
10786
6
VIDHI
H
MALI
OG-19-
1911-
8430-
00001752
Shree Siddhivinayak
Hospital - Navi
Mumbai
Enteric fever
22-Mar-19
26-Mar-
19
LITIGATION
33207
LITIGATION
Going through the above claim history, it is seen that during Aug ‘10 to Mar ‘19, there were 5 claims
of Ms. Vidhi for similar types of ailments viz. LRTI, Malaria, Sub Mandibular Swelling with high
grade fever, Granular Tonsillitis with viral hepatitis. Hospital admission for 4 to 6 days. Claimed
amount 9000/- to 42000/-. Four out of five times admitted to Siddhivinayak Hospital and once to
Terna Hospital. All the earlier claims are settled by RI. However, the current claim is repudiated on
account of discrepancies narrated above. After hearing both the parties and going through the papers
on record, forum feels that the inconsistencies pointed out seem to be correct. Forum therefore,
upholds the repudiation.
Award follows:
AWARD
Under the facts and circumstances of the case, the complaint stands dismissed.
Dated: On 23
rd
day of September, 2021 Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Hasmukh Parmar Vs Care Health Insurance Limited.
COMPLAINT NO: PUN-H-037-1920-0641
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the Complainant:
Mr. Hasmukh Parmar,
Ambernath, Mumbai.
2.
Policy No:
Type of Policy:
10583336
Individual Health Policy (Care with NCB
super)
3.
Policy period:
30/4/2016-29/4/2019 (three years).
4.
Sum Insured:
Rs.500000/- each
5.
Date of inception of first policy:
30/4/2015 ( Cholamandalam)
6.
Name and age of the insured:
Neeta Parmer, 45 yrs & Hasmukh, 51yrs
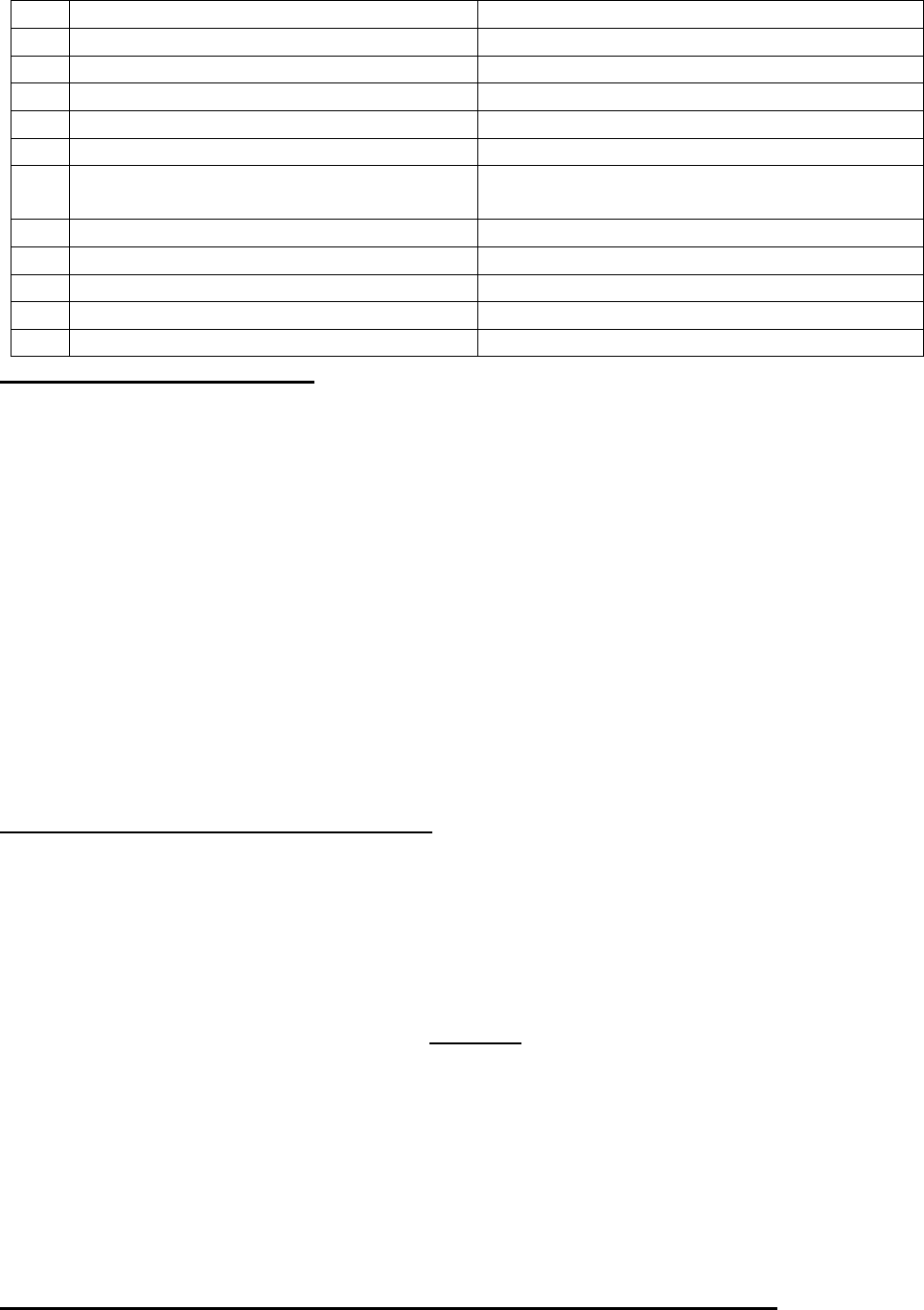
Name of the Policyholder:
Mr. Hasmukh Parmar.
7.
Name of the Insurer:
Care Health Insurance Limited.
8.
Reason for repudiation:
Non discloser of pre-existing Heart disease.
9.
Date of receipt of the Complaint:
7/1/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
1)Rs. 343577/- & 2) Rs. 15285/-
12.
Rule of IO Rule under which the
Complaint was registered:
13 (1)(b)
13.
Date of hearing/Place:
28/07/2021, Online hearing, Pune
14.
Representation at the hearing
gg) For the Complainant:
Shweta Parmar, Daughter.
hh) For the insurer:
Dr. Ashutosh
15.
Complaint how disposed:
Allowed.
Contention of the Complainant:
The Complainant ported his one year old health insurance policy from Cholamandalam General
Insurance Co Ltd., to the Respondent Insurer (RI). Date of inception of the policy with
Cholamandalam was form 30/4/2015. RI collected three years premium and issued policy with effect
from 30/04/2016 to 29/04/2019. The complainant had lodged two claims, one for his wife
for Coronary Heart ailment and second one for himself for the illness Cholecystitis.
RI rejected his wife’s claim on the ground that her Pre-existing disease of Heart problem has not been
declared at the time of inception of the policy. Complainant informed RI that his wife didn’t have any
past history of ischemic heart disease and it was an incidental finding during routine health check-up
with family doctor Chandrakant Sinkar. RI made an issue of the non-discloser of material fact and
cancelled the policy.
Complainant approached to Grievance department of RI and pleaded that as he is having Mediclaim
Policy since April 2015, continuity benefit since inception of the policy should be considered. Hence,
both the claims should be satisfied.
Aggrieved with the repudiation of both the claims, Complainant has approached this forum for
redressal and resolution of his grievance.
Contentions of the R I (Rspondent Insurer):
Insured Mrs. Neeta Hashmukh Parmar filed a reimbursement claim for the hospitalization from
15/03/2017 to 18/03/2017. As per discharge summary dated 18/03/2017 of P D Hinduja National
Hospital, Mumbai she was diagnosed with Coronary Artery Disease and underwent the treatment of
PCI to LAD and PCI to RCA.
Certificate issued by Dr. Gautam S jatale states that insured was having Ischemic Heart Disease for
last 1.5 years. This history of heart disease was not disclosed during the portability of the policy which
shall be classified as Non-disclosure of material facts. Accordingly, the claim of the insured patient
was denied as per policy terms and conditions clause 7.1 which read as under:
“if any untrue or incorrect statement are made or there has been a misrepresentation,
misdescription or non-discloser of any material particulars or any material information having
been withheld or if the claim is fraudulently made or any fraudulent means or devices are used by
the policy holder or the insured person or any one acting on his/her behalf, the company shall have
no liability to make payment of any claims and the premium paid be forfeited ab initio to the
company”
Regarding the claim of Mr. Hasmukh Parmar, they are willing to settle the same for Rs. 13,665/-
against the claimed amount Rs. 15,285/-.
Result of personal hearing with both the parties (Observations & Conclusions):
A personal hearing was held on 28/07/2021 (through video-conferencing) where Complainant and
Respondent Insurer reiterated their contention.
Ms. Shweta, daughter of the complainant participated in the hearing on behalf of the Complainant.
She informed the forum that, representatives of the RI visited their residence multiple times to enquire
about her mother’s pre-existing heart disease. By showing the medical certificate of Dr. Gautam Jatale
of Ambarnath (E) dated 12/04/2017 they were pressurizing them to accept that her mother is having
IHD for the last one and half years and since then she is under treatment of Dr. Jatale.
The forum has perused the documentary evidence available on record and heard the submissions
made during the online hearing by both the parties. After analyzing the same, the forum notes that
the claim of the insured patient Mrs. Neeta Hasmukh Parmer was repudiated mainly on the basis of
a letter addressed to Dr. Rajani issued by Dr. Gautam Jatale on 12/04/2017. The letter goes ‘sending
herewith Mrs. Neeta Parmar a k/c/o IHD for further of CAG and angioplasty. She is under my
treatment since 1 ½ yr. for IHD.’ Forum observed that this letter is dated 12/04/17 and the patient
was already admitted to P D Hinduja Hospital on 15/03/2017 and Coronary Angiography plus
Angioplasty was done on 16/03/2017. RI’s investigators have tried to obtain IHD history just so, that
it goes back by some months before porting. But in the process, making the doctor refer Mrs. Neeta
to Dr. Rajani for angioplasty one month after it has already been performed by the same Dr. Rajani,
suggests that this letter is concocted. Forum has strong objection to such methods and
manipulations resorted to by RI for avoiding claim liability.
Forum asked complainant’s representative whether they questioned their doctor about this letter.
She said that the doctor agreed to having issued the letter wrongly by his RMO. But at the same time
expressed helplessness to issue a counter letter for the fear of getting his hospital blacklisted.
The discharge summary of Hinduja hospital has mention of exact duration of her other ailments like
DM since 5 months and Hypothyroidism since 1 month. But no such history is mentioned against
coronary artery disease. The RI also has not produced any supporting documents before the forum
which can prove that the complainant had IHD before buying this policy.
It is also observed that the policy was cancelled after giving notice on 21.11.2019.
Forum hereby directs the Respondent Insurer to settle the amount of admissible claim of Mrs. Neeta
Hasmukh Parmer. RI is also directed to reinstate the cancelled policy from the date of cancellation
keeping in mind that continuity benefit of the policy should not be disturbed.
Respondent is willing to settle the other claim of the complainant for Acute Cholethisis bearing claim
no CL- 91131966 for Rs. 13665/-.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent is directed to settle the
admissible amount of both the claims and reinstate the policy without any break in
insurance from the date of cancellation of the policy by collecting the premium if the
complainant is willing for the same, towards full and final settlement of his complaint.
The complainant to decide about reinstatement of the policy and comply with the
requirements within one month from the receipt of this award.
The award is to be complied with within one month from the date of receipt of this award
failing which it will attract interest at the bank rate plus 2% extra from the date of rejection
of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insure
Dated: On 20
th
day of Sept 2021, Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Hemant Sharma Vs. Star Health & Allied Insurance Company Ltd.
COMPLAINT NO: PUN-H-044-1920-0543
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. Hemant Ramesh Sharma
B52, Seelam Srishti CHS Ltd., Sector-3,
Mira Road (East), Mumbai – 401107 (Thane)
2.
Policy No:
Type of Policy:
P/171131/01/2019/005086
Star Comprehensive Insurance Policy
3.
Policy period:
22/09/2018 to 21/09/2019
4.
Sum Insured/IDV
Rs.7,50,000/-
5.
Date of inception of first policy:
22/09/2015
6.
Name & age of the Insured:
Name of the Policyholder:
Ms. Poonam Sharma – Age: 21 years (D)
Mr. Hemant Ramesh Sharma
7.
Name of the Insurer:
Star Health & Allied Insurance Company Ltd.
8.
Reason for rejection /Partial
Settlement:
Claim has been settled as per policy conditions
after deducting non-payable / medical items.
9.
Date of receipt of the Complaint:
05/12/2019
10.
Nature of complaint:
Repudiation of partial claim
11.
Amount of Claim:
Rs.36,784/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021, Online. Pune
14.
Representation at the hearing
ii) For the Complainant:
Himself.
jj) For the insurer:
Dr. Smita Sonawane
15.
Complaint how disposed:
Allowed.
Contentions of the Complainant:
Complainant was insured with the Respondent Insurer (RI) under the above policy for the period
22/09/2018 to 21/09/2019. His daughter was admitted in Sportsmed Mumbai Pvt. Ltd., from
26/08/2019 to 28/08/2019 and underwent Arthroscopic Left Knee ACL reconstruction. Out of a total
claimed amount of Rs. 229958/-, the RI has settled the claim for Rs. 185674/-.
RI clarified that they have approved maximum amount of the claim with deductible on non-medical
and non-payable items. Being dissatisfied with considerable amount of deduction, Complainant has
now approached the forum for redressal of his grievance.
Contentions of the Respondent Insurer (RI):
On receiving the Notice from the Forum, the RI has reviewed the claim and considered for payment
of an additional amount of Rs. 9315/-. The details of deductions are as under:
Se-
rial
no.
Description
Total
amount as
per hospi-
tal bill
Not paya-
ble
Amount
paid
Reasons given by RI
1
OT charges
18150
1815
16335
Due to non submission
of package charges, 10%
is deducted.
2
Professional fees
108470
7500
100970
Surgeon charges maxi-
mum payable amount
3
Medicines-within
hospital
37175
19297
17878
Refer note 1
Note
1.
Camera cover
70
Cap
75
Apron
63
Sterillum
367.1
Steri strips
158
Plain sheet
125
Knee brace
1063
Stoickinett
22.64
Cool pack
220
Becosules
17.16
Walker
1900
Pendrive
500
Storrad Cassette
10008
Total amount as
per hospital bill
14588.9
Total deduction
19297
Difference
4708.1
4
Miscellaneous
charges
7920
5920
2000
Drill charges not payable
5
Others
10650
9650
1000
Refer note 2
Note
2
Arthroscopy
charges not paya-
ble
6050
Registration
charges
2000
Food charges not
payable
1600
Result of personal hearing with both the parties (Observations & Conclusions):
Forum has observed that out of total claimed amount of Rs. 2,29,958/- Respondent Insurer has settled
for Rs. 185674/- and after receiving notice from the forum an additional amount of Rs. 9315/- ( OT
charges deducted for Rs. 1815 plus Surgeons charges deducted for Rs. 7500/- Total= Rs. 9315/-) has
been considered for payment. Forum further observed that out of Rs. 19297/- deducted towards
Medicines- within hospital, Respondent Insurer could supply details of Rs. 14589/-. Therefore, in
absence of details of deductions the difference of Rs. 4708/- has been considered by the forum for
payment. Hence, in view of the above observations, RI is directed to pay Rs. 9315/- + Rs. 4708/-
Total Rs. 14023/- towards full and final settlement of the claim.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to release
an additional amount Rs. 14023/- towards full and final settlement of his claim.
The award is to be complied with within one month from the date of receipt of this award
failing which it will attract interest at the bank rate plus 2% extra from the date of rejection
of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: On 9
th
September 2021 at Pune
VINAY SAH
Insurance Ombudsman, Pune.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MRS.JAYASHRI PATIL V/S IFFCO TOKIO GEN INS CO LTD
COMPLAINT NO: PUN-H-023-2021-0627
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mrs. Jayshri Patil, Mira Road
Thane
2.
Policy No:
Type of Policy:
H0517352
Corona Rakshak Policy
3.
Policy period:
09.11.2020 TO 21.02.2021
4.
Sum Insured
250000
5.
Date of inception of first policy:
09.11.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Mrs. Jayshri Patil, 29 yrs
Mrs. Jayashri Patil
7.
Name of the Insurer:
IFFCO TOKIO GEN INS CO LTD
8.
Reason for repudiation/Partial Settlement:
Covid report submitted has not been in
compliance with standard covid report
format
9.
Date of receipt of the Complaint:
10.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
SI 250000
12.
Insurance Ombudsman Rule (IOR)2017
Rule 13 1 (b)
under which the Complaint was registered:
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
kk) For the Complainant:
Absent
ll) For the insurer:
Mr. Suraj Singh Negi
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:-
• The complainant had taken Corona Rakshak Policy with Respondent Insurer IFFCO TOKIO
GEN INS CO LTD for self for Sum Inusred of Rs.2.5 lakh. She had lodged a claim of self-
hospitalization in Neptune hospital Thane from 13.12.2020 to 22.12.2020 for Covid 19 posi-
tive.
• The insured in this case is claiming for benefit under Corona Rakshak Policy, as she under-
went treatment of covid 19 at Neptune Hospital, Thane.
• The complainant would like to draw attention that the claim team of the company had rejected
her covid benefit under the Corona Rakshak policy on administrative grounds that the sub-
mitted covid report has not been in compliance with the standard covid report format. The
report carries ICMR registration no. under patient id 1975330 dated 12.12.2020.
• The hospitalization expenses claim for this hospitalization was settled for Rs.199653/- by Ba-
jaj Allianz gen ins. co ltd under cashless claim in favour of the hospital for the treatment of
covid positive.
• The operative clause clearly states that if during the policy period a person is diagnosed with
covid and hospitalized for more than 72 hours the company will pay the agreed amount. The
complainant had fulfilled the criteria of the policy
• The complainant is requesting forum to intervene for settlement of SI.
Contentions of the Respondent Insurer (RI):-
As per their SCN, they have contended that,
6) The insured in this claiming for benefit under Corona Rakshak policy for treatment of covid
19 , She had undergone treatment in Neptune Hospital, Thane
7) Indoor case records submitted, referring to admission history and physical assessment form,
credentials are blank.
8) The RI had received multiple claims of this hospital from different insured for claiming ben-
efits under CRB policy. The policy of CKI is also purchased for the same insured from other
insurer.
9) The company has received 18 claims from this hospital from CRB policy and all the claims
are reported to RI i/r/o the policies that have been purchased through on line mode. Most of
the patient/insured admitted in this hospital are residing very far away, approximately distance
observed ranges between 22kms to 412 kms whereas many designated covid hospitals are
available within the nearby vicinity. This clearly shows that these patients are admitted to this
particular hospital for the sake of insurance claims.
10) Going through the submitted records of all the patients admitted in the hospital for manage-
ment of Covid19, a repetitive pattern is observed in regards to presenting complaints and bills.
Even the line of treatment give is more or less same and in a fixed pattern. This refers the
documents are prepared by a single person for the sake of claim purpose without giving actual
treatment.
11) In all the cases, CT scan chest was not advised to see the lung involvement on account of the
fact patient was maintaining inadequate saturation (discrepant history as per nursing chart and
IPD records) and were in respiratory failure. ABG report is also not advised in any of the cases
to access the type of respiratory failure.
12) As the patient was critical as per IPD records, however anesthetist notes or notes from ICU in
charge are not available round the clock. As per indoor records, initially patient was on mag-
nex forte till 16
th
and was suddenly changed to meropenem without any clinical condition.
Indication of higher antibiotics is not understood.
In this regard, the RI had drawn attention to clause 3.5of “definition” of CRB policy
CLAUSE 3.5 Disclosure to information norm: The policy shall be void and all premium paid
thereon shall be forfeited to the company in the event of misrepresentation, is description or
non-disclosure of any material fact by the policyholder. In view of the same this case is
rejected.
Result of personal hearing with both the parties (Observations & Conclusions):
During the hearing, held online on 19/05/2021; complainant did not appear even after sending her the
hearing link well in advance and could not be contacted over the mobile number provided by her.
The allegations made by the RI are serious in nature and do not warrant review of the claim that too
in absence of any document submitted by the complainant to cross object their contentions. The
findings of the RI in the claim papers are convincing. In such grievous scandal of mis-use of public
money, the RI should take an appropriate action against the defaulting parties. Complaint is thus
disallowed. Award follows:
AWARD
Under the facts and circumstances, forum is not willing to intervene in the decision of
rejection of the claim, as the allegations are falling under IPC and needs action from
Government level investigations.
Dated: On 7
th
day of September, 2021 Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Kamal Kumar Rajesth Vs The Oriental Insurance Company Ltd.
COMPLAINT NO: PUN-H-050-1920-0687
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. KamalKumar Pitamberdas Rajesth
B5, Kajol Complex, Vidya Nagari,
Behind Utsav Hall, Nasik Road, Nasik -
422101
2.
Policy No:
Type of Policy:
163600/48/2019/1229
PNB ORIENTAL MEDICLAIM
POLICY 2017
3.
Policy period:
22/05/2018 to 21/05/2019
4.
Sum Insured/IDV
Rs.3 lakhs
5.
Date of inception of first policy:
22.05.2017
6.
Name & age of the Insured:
Mrs. Rekha; wife; Age:67 yrs.
Name of the Policyholder:
Mr. Kamal Kumar Pitamberdas Rajesth
7.
Name of the Insurer:
The Oriental Insurance Company Ltd.
8.
Reason for rejection /Partial Settlement:
Pre-existing disease
9.
Date of receipt of the Complaint:
05/11/2019
10.
Nature of complaint:
Rejection of health claim due to PED
11.
Amount of Claim:
Rs.1,26,465/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
14/06/2021; (Online)
14.
Representation at the hearing
mm) For the Complainant:
Himself & Mr. Rahul Rajseth, son
nn) For the insurer:
Ms. Sumitra Bhangare
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:
Complainant and his family were insured with the Respondent Insurer (RI) under the above policy
for the period 22/05/2018 to 21/05/2019. The insured patient aged 67 years was admitted on
03/04/2019 to Bhagwati Superspeciality Endoscopy Hospitals, Nasik for treatment of severe gastritis
+ ketosis + hyponatremia and after treatment was discharged on 08/04/2019. The claim was rejected
by the RI on the grounds that the insured patient was a k/c/o DM and HTN for the past seven years
and the policy was in the second year, hence due to PED condition, claim was rejected as per policy
terms and conditions.
He has paid an amount of Rs.1,26,465/- to the hospital towards the treatment.
The complainant has stated that earlier, too she was admitted for similar symptoms and RI had settled
the claim for Rs.26,465/- during April 2018 and in the subject case, RI is denying the claim which is
not acceptable to him. He has also represented to the Grievance Cell of the RI vide his letter / mail
dated 24/08/2019 stating that the hospital has mistakenly written in their document that patient was
having the ailment since 7 years and they have issued a certificate to this effect admitting their mistake.
They also clarified that the blood sugar level was fluctuating and not uncontrolled as stated as one of
the reasons in denial letter. Despite the clarification letter, RI has denied the claim. Aggrieved with
this situation; the complainant has approached the forum for the resolution of his grievance.
Contentions of the Respondent Insurer (RI):
The RI has stated that the patient was admitted to the hospital for treatment of Gastritis and Duodenitis
at Bhagwati Superspeciality Hospitals, Nasik and the hospitalization reimbursement claim was
rejected on the grounds that the insured patient was a k/c/o Diabetes and Hypertension since the last
7 years as per letter dated 24/04/2019 by Dr. Jayant Wagh, which is prior to inception of the policy
cover and this fact was not disclosed to the RI. The claim is rejected as per Clause No.4.1 which is
reproduced as under:
4. GENERAL EXCLUSIONS: The Company shall not be liable to make any payment under this Policy
in respect of any expense whatsoever incurred by any Insured Person in connection with or in respect
of:
4.1 All Pre-existing Diseases (whether treated / untreated, declared or not declared in the Proposal
Form), are excluded upto 36 months of the Policy being in force and shall be covered only after the
Policy has been continuously in force for 36 months. For the purpose of applying this condition, the
date of inception of the first PNB-Oriental Royal Mediclaim shall be considered, provided the
Renewals have been continuous and without any break in the policy period. This exclusion shall also
apply to any complication(s) arising from Pre-existing Diseases. Such complications will be
considered as part of the Pre-existing health condition or Disease.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 14/06/2021 (Online), both the parties reiterated their respective stand.
The RI has repudiated the claim by quoting Clause No.4.1 as mentioned above stating that the insured
patient had a pre-existing condition of DM and HTN and also had a stroke in 2017. The policy in
question has an inception date of 22/05/2017 and was in its second year. The present ailment is related
to pre-existing condition;
From the papers submitted on record, it is found that there is a query reply given by Dr. Jayant Wagh,
dt.24/04/2019 stating that the exact duration of HTN, DM of the insured patient is of 7 years. The
certificate produced by the complainant in support of his counter argument, states ‘There is mistake
in duration of DM and HTN. It is not from 7 years. Duration of DM & HTN is not mentioned anywhere
in IPD paper & consultation sheets.’ But the said certificate has not given correct duration of the said
ailments. Complainant has also not disclosed the duration of DM/HTN. However, on instructions of
forum, he sent discharge card of his wife’s admission in June 2017 for perusal. The said discharge
card of Jairam Hospital has noting ‘k/c/o DM, HTN’. It is to be noted that the policy inception was
on 22/05/2017 and within a month, at the time of hospital admission on 9/06/2017, she was already
a known case of DM. which proves beyond doubt that the condition was pre-existing prior to the
inception and as such, waiting period of 36 months applies as per clause 4.1. It does not matter
whether the duration of DM & HTN is seven years or less or more.
Forum therefore, supports the RI’s decision of rejection of the claim. Regarding payment of earlier
claim for the similar cause, RI has not given any comments.
Complaint thus disallowed.
Award follows:
AWARD
Under the facts and circumstances of the case, the complaint does not sustain. Rejection
of claim does not warrant forum’s intervention. Complaint therefore stands dismissed.
Dated: at Pune this 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mrs. Khurshid Marolia Vs. Bajaj Allianz General Insurance Company Limited
COMPLAINT NO: PUN-H-005-1920-0654
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mrs. Khurshid Darayas Maroliya
Kranti Chowk,
Aurangabad – 431005 (M.S.)
2.
Policy No:
Type of Policy:
1. Health Ensure Floater Policy No.
OG-19-2006-8436-00000039; SI: 5 Lacs
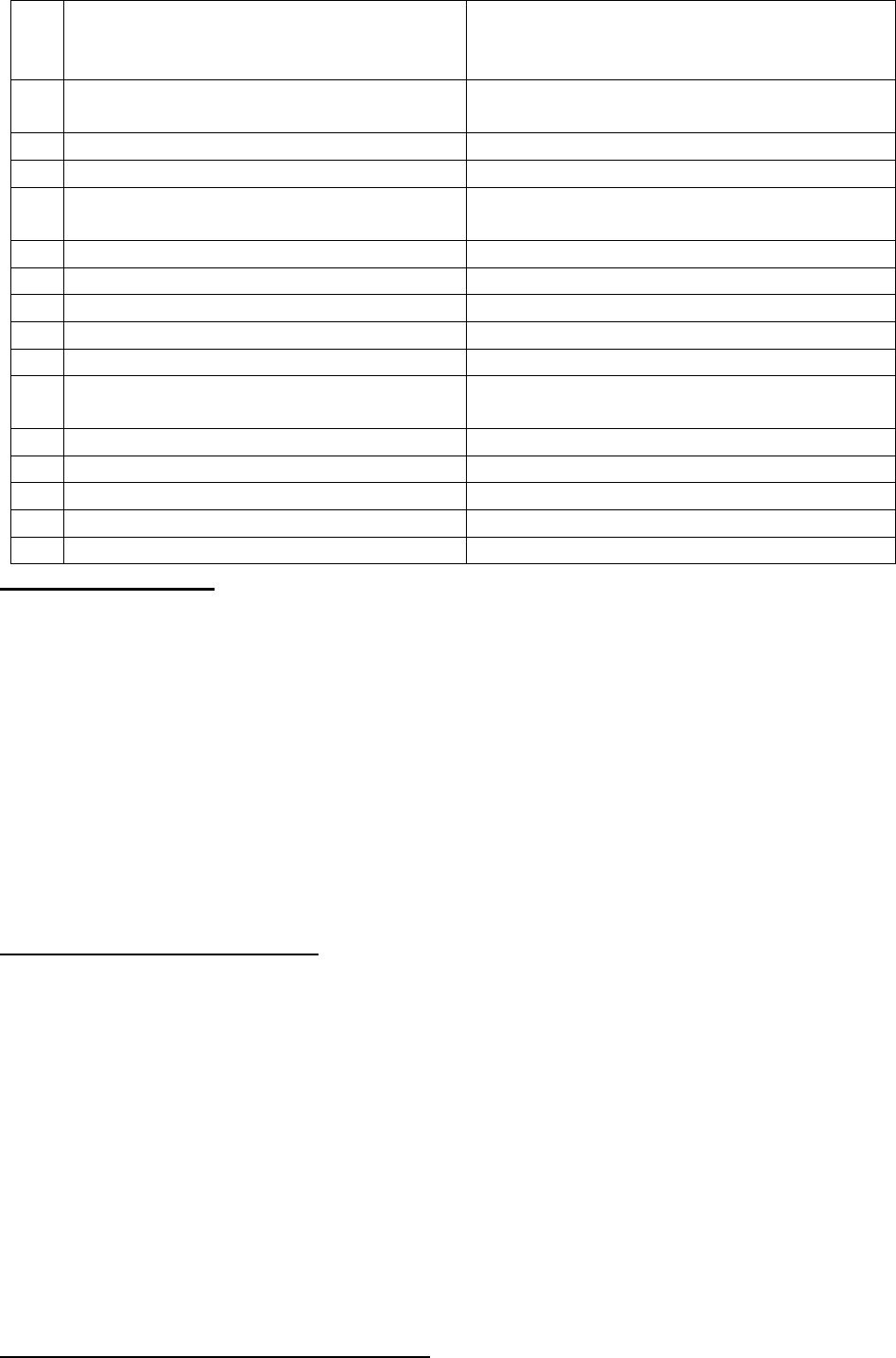
Ported from Oriental Insurance Co. Ltd.
2. Extra Care Policy No.
OG-19-2006-8432-00000258 SI:10 lacs
3.
Policy period:
01/12/2018 to 30/11/2019 for both the
policies
4.
Sum Insured
Rs.5 lacs and Rs.10 lacs
5.
Date of inception of first policy:
With OIC since 25 yrs; now Ported to RI
6.
Name & age of the Insured:
Name of the Policyholder:
Mrs. Khurshid Maroliya – Age: 62 years
Mr. Darayas Nariman Maroliya
7.
Name of the Insurer:
Bajaj Allianz Gen. Insurance Company Ltd.
8.
Reason for rejection /Partial Settlement:
Non-disclosure of PED
9.
Date of receipt of the Complaint:
20/01/2020
10.
Nature of complaint:
Rejection of entire health claim
11.
Amount of Claim:
Rs.4,87,201/- (2 claims) of Ca. breast
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
06.08.2021(Online )
14.
Representation at the hearing
oo) For the Complainant:
Herself & husband Darayus
pp) For the insurer:
Mr. Irfan Shaikh & Dr. Ravindra Shingte
15.
Complaint how disposed:
Allowed
Brief facts of the case:
Complainant and her husband were insured with the Respondent Insurer (RI) under the above policies
for a SI of Rs. 5 lakhs and Rs.10 lakhs for the period 01/12/2018 to 30/11/2019. Complainant Mrs.
Khurshid aged 62 years was hospitalized at Sir H.N. Reliance Hospital, Mumbai on 13/06/2019 with
complaints of focal asymmetry and micro calcifications in Rt. breast and diagnosed as ductal
carcinoma in situ of Rt. breast and after treatment, she was discharged on 16/06/2019. RI rejected the
claim on the grounds that the insured patient is known to be suffering from benign discrete
calcifications bilateral breast with BI-RADS 2 category since 2012 and rheumatoid arthritis since
28/11/2018. The illness was a pre-existing disease and was not disclosed in the proposal form while
opting for the insurance. Incidentally, the complainant had ported the policy from Oriental Insurance
Company Ltd. and she was with the earlier insurer for more than 25 years until 2018 before porting
the policy with Bajaj Allianz. The complainant has incurred an amount of Rs.4,87,201/- towards
cancer treatment.
Contentions of the Complainant:
The complainant contends that all her mammography reports from 2012 to 2016 are consistent to
reflect BI-RADS as “category 2” wherein category 2 is given on “benign findings”. Accordingly, BI-
RADS 2 warrants no biopsies, medical treatment or surgery. As such, it is not a medical condition
which requires her to treat it as an ailment necessitating a disclosure.
Regarding Rheumatoid Arthritis she states that, it was first diagnosed on 28.11.2018. i.e. 2 days before
the issuance of her current policies. Moreover, RA is a chronic disease of the musculoskeletal system
which in no extent can directly or indirectly cause or influence the Carcinoma of right breast. Hence,
the omission to disclose Rheumatoid Arthritis is completely inadvertent and inconsequential.
Therefore, denying her claim citing non-disclosure of Rheumatoid Arthritis is simply baseless and
implausible.
RI not only rejected her cashless claim at the time of taking discharge and later reimbursement claim,
but subsequently cancelled both her policies.
Aggrieved with this decision, the complainant has approached the forum for resolution of her
grievance regarding claim payment and restoration of cancelled policies.
Contentions of the Respondent Insurer (RI):
The RI has stated that after verification of the documents, it was revealed that the insured patient was
hospitalized for the treatment of carcinoma of right breast and the policy incepts with them from
01/12/2018. They have rejected the claim vide their letter dated 03/09/2019 stating that the insured
patient is known to be suffering from benign discrete calcifications bilateral breast with BI-RADS 2
category since 2012 and rheumatoid arthritis since 28/11/2018. RI has denied the claim under non-
disclosure of pre-existing disease while porting the policy with them under Definition B16, which is
reproduced hereunder:
Definition B16 – “Disclosure to information norm – the policy shall be void and all premium paid
hereon shall be forfeited to the Company, in the event of misrepresentation, mis-description or
non-disclosure of any material fact.”
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 06.08.2021(Online), both the parties reiterated their respective stand.
During the hearing, complainant and her husband conveyed to the forum that their agent convinced
them to port their policy from OIC, which was there for 25 yrs, stating extra benefits in low cost. He
also convinced them for porting stating that it will be as if policy was with OIC only and they will
continue to get benefits under the policy as before. He got their signatures and money for porting of
the policy and details in the form were filled in by him only. She also informed that she was operated
for hernia in the year 2016.
As a routine checkup she used to do mammography once in two years since the year 2012. Every
time till 2019 she got nonmalignant report and unfortunately, only in 2019, she got positive report of
CA breast. Before porting they had undergone health checkups conducted by RI. Forum has gone
through her routine screening mammograms of 2012, 2014 and 2016. They all have noting of
calcification but remark ‘No abnormality detected’ is there too. As such, there is no question of
declaring it while taking the policy. Complainant being a health conscious lady and going for check
up on her own, she would have started treatment immediately if anything adverse was found and if
her doctor had advised her so.
RI was asked whether they observed all portability norms before porting, they replied as ‘Yes’. Then
the question remains, how the h/o her alleged PEDs have not been noticed by RI from her claim
history/Discharge card. They could have called for those documents before accepting the porting.
Instead of taking all due care before porting, rejecting a claim by digging into PEDs, in portal policies,
puts the policyholder into helpless situation. RI has not asked any explanation from the erring agent,
who allegedly had not disclosed PEDs of the complainant.
In respect of RI’s contention of non-disclosure of OA since 28/11/2018, it is pertinent to note here
that the RI had already issued the ported policy on 19/11/2018 for the period from 01/12/2018 to
30/11/2019. In view of this, it is not correct to say that there was a non-disclosure of OA from the
complainant’s side before porting/issue of the policy.
In view of the above reasons, forum is not convinced with the rejection of the claim on the grounds
of non-disclosure and cancellation of the policies for this reason. RI, therefore is instructed to pay the
present claim and further claims if any, the complainant could not have registered because of
cancellation of the ported policy by reinstating the policies by collecting appropriate premium from
the complainant for the lapsed policy period.
Complaint is admitted in view of the lacunae left at RI’s level before porting and having no substantial
proof of her having CA breast before porting of insurance.
Award follows,
AWARD
Under the facts and circumstances of the case, the RI is directed to pay to the complainant the
claimed amount of Rs. 4,87,201/- less deductibles as per policy terms and conditions, towards
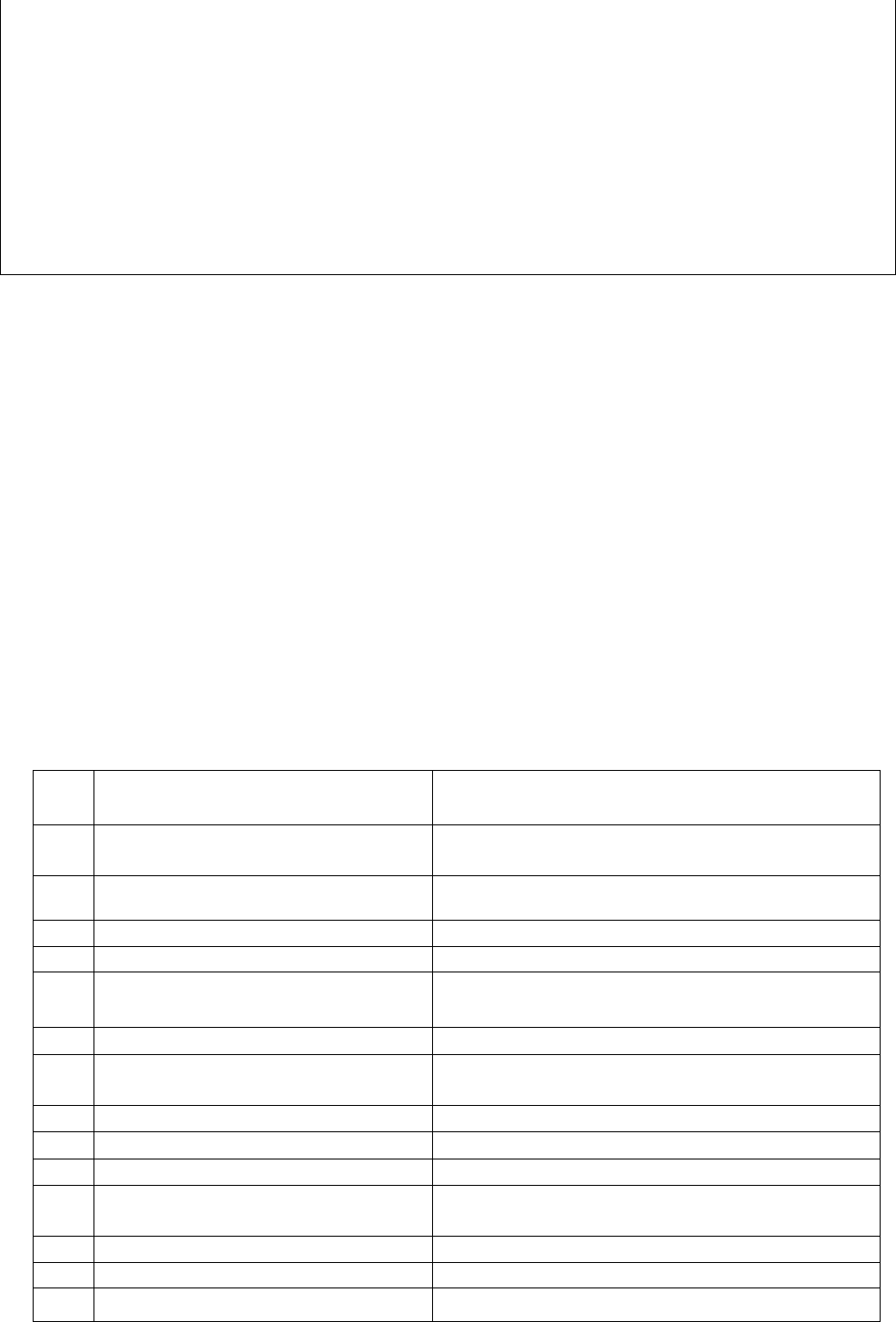
full and final settlement of the complaint. RI is also instructed to pay further claims if any
incurred of the patient insured, which he/she could not have registered because of cancellation
of the ported policy by reinstating the policies by collecting appropriate premium from the
complainant for the lapsed policy period.
Complainant is also instructed to take her decision of continuation of the policy within one
month from the receipt of premium demand from the RI. Failing which, these instructions will
not be binding on RI.
The award is to be settled within one month from the date of receipt of this award failing which
it will attract interest at the prevailing bank rate plus 2% extra from the date of rejection of the
claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: this on 16
th
day of September 2021 at Pune
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Kiran Madan Mhatre V/S Tata AIG General Insurance Company Limited
COMPLAINT NO: PUN-H-047-1920-0523
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Kiran Madan Mhatre, Goddev Gaon,
Bhayander (E), Thane.
2.
Policy No:
Type of Policy:
0236655562
Medi Prime Policy, (Family Floater Plan)
3.
Policy period:
06/09/2018 to 05/09/2019
4.
Sum Insured/IDV
Rs. 300,000/-
5.
Date of inception of first policy:
06/09/2018
6.
Name & age of the Insured:
Name of the Policyholder:
Mr. Kiran Madan Mhatre, 41 Years.
Mr. Kiran Madan Mhatre
7.
Name of the Insurer:
Tata AIG General Insurance Company Limited,
8.
Reason for repudiation/Partial
Settlement:
Non-disclosure of material facts.
9.
Date of receipt of the Complaint:
20/11/2019
10.
Nature of complaint:
Rejection of claim.
11.
Amount of Claim:
Rs. 123,612/-
12.
Rule of IO Rule under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
18/06/2021; Online
14.
Representation at the hearing
qq) For the Complainant:
Himself

rr) For the insurer:
Mr. Dhiraj Mhatre on voice call
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:
The Complainant was admitted to Gurukrupa Hospital & Polyclinic on 05/07/2019 with history of
Fever with chills, 15/20 episodes of watery loose motion, Nausea, on and off Abdominal Pain since
two days. He was diagnosed- Acute Gastroenteritis with dehydration Grade II, Sub acute Intestinal
obstruction. He was discharged on 15/07/2019.
RI denied his reimbursement claim of Rs. 123,612/- vide letter dated 16/10/2019 and 26/10/2019
on the ground of Pre-existing disease of Hypertension, which he is suffering for the last 2-3 years.
The same disease-Hypertension has not been disclosed in the Proposal form at the time of obtaining
the fresh policy in 20
th
November 2017.
Complainant had produced a medical certificate from his family Doctor Vivek S Patil clarifying that
in February 2017 he had family related stress leading to High BP problem and was on medication for
a temporary period. His high BP problem was normalized within a short period of time and medicine
was discontinued. While taking the policy for the first time, he was not having any BP problem, hence
it was not declared in the Proposal Form. RI has not taken into consideration of the above certificate/
clarification and stand by their earlier decision of Rejection of claim.
Complaint has now approached to this forum with a request to look into the matter and help him in
getting the admissible claim amount of Rs.123,612/- as he feels that RI has wrongly denied his
legitimate claim.
Contentions of Respondent Insurer (RI):
R I has submitted Self Contained Note on 30/01/2020.
It states that Pre-authorization of Cashless claim approval was reported by Gurukul Hospital &
Polyclinic, Bhayander on 06/07/2019 under the coverage in hospital indemnity for sickness. The
Complainant/Insured was admitted for the period from 05/07/2019 to 15/07/2019. He was with
medical condition of Fever with chills, watery loose motion, nausea and abdominal pain.
Initially RI extended initial Pre-authorization of INR 15,000 & then INR 100,000/-. Afterwards, they
received statement dated 15/07/2019 from Complainant/ Insured patient, in which he has mentioned
that he was suffering from High Blood Pressure since 2-3 years and taking Tablet Gulpress AM 50
mg.
They noticed that in Policy Inception Proposal Form, the medical history of High Blood Pressure was
not mentioned. Hence, they cancelled earlier Pre-authorization approval and denied Pre-authorization
under “Non Discloser” clause.
RI denied reimbursement claim under “Non Discloser” vide letter dated 30/07/2019. Had
Complainant declared about Hypertension to RI, they would not have issued policy at the inception
stage. The claim of the Complainant has therefore been repudiated strictly in accordance with the
terms and conditions of the policy.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 18/06/2021 (through video-conferencing), both the parties
reiterated their respective stand.
During the hearing complainant said that he does not have hypertension. But, the RI kept on asking
him again and again whether he suffered from BP. He said, in the past, he had taken BP tablets as he
was undergoing some tension due to family issues and his doctor had advised him to take BP
medicines. The treating Dr. Vivek Patil’s certificate dt.16/07/2019 supports this contention. The
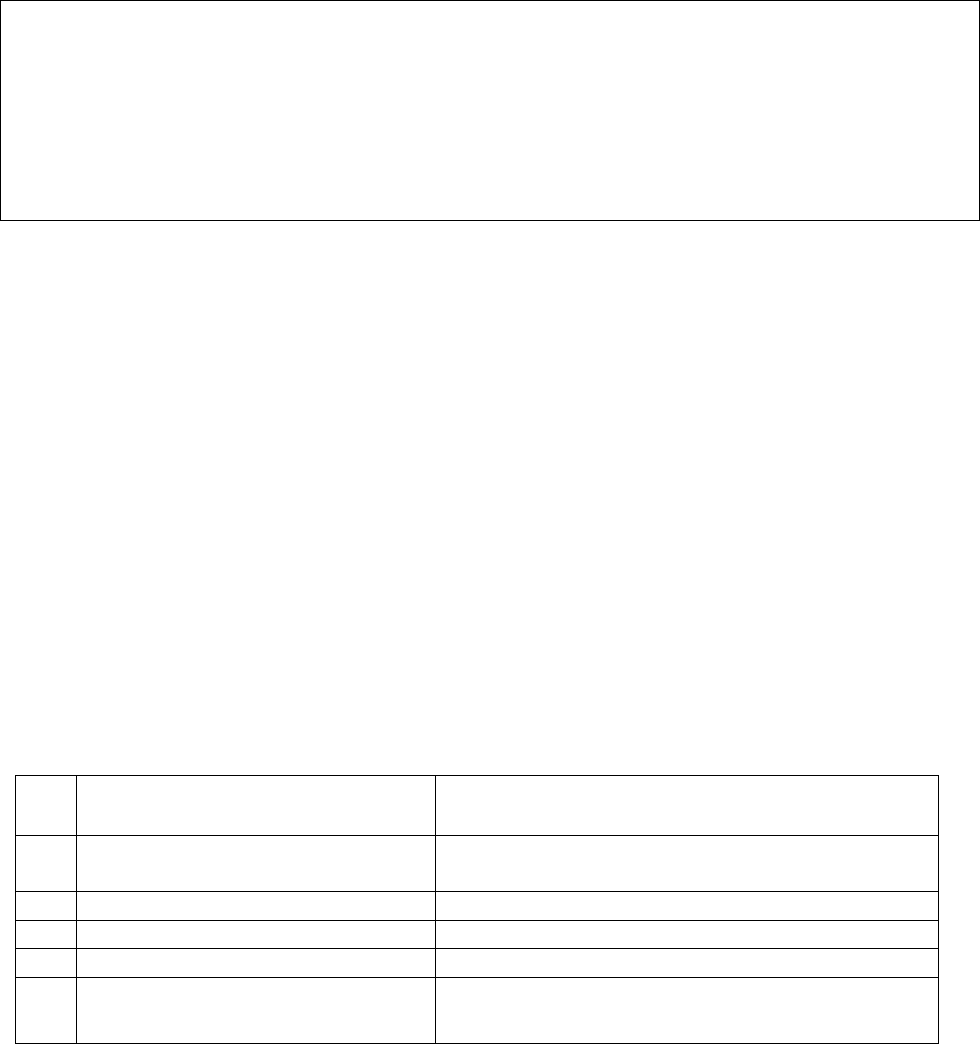
certificate says that in Feb.2017, the complainant had consulted him for headache due to some
family stress and on examination his BP was on higher side. Hence he started antihypertensive
medicines. After 10-15 days, patient came with the complaints of giddiness as his BP was on lower
side, hence he advised him to stop antihypertensive medicines immediately as it was temporary due
to stress. Now he is not having any antihypertensive medicines.
In the current hospitalisation admission notes also, there is no any mention that he is a k/c/o HTN.
Hence, there is scope to believe the doctor’s certificate and complainant’s contention. The present
ailment is also not HTN related one.
In view of the circumstantial evidences and no substantial proof which can prove the HTN state of
the complainant before the issue of first policy, forum finds that the claim is admissible. Complaint
is thus admitted.
Award follows:
AWARD
Under the facts and circumstances, the RI is directed to pay the claimed amount of Rs.1,23,612/-
less compulsory deductible as per the policy terms and conditions, to the complainant, towards
full and final settlement of the complaint.
The award is to be settled within one month from the date of receipt of this award failing which
it will attract interest at the prevailing bank rate plus 2% extra from the date of rejection of the
claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune on this 30
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. KISHOR GUGNANI V/S THE ORIENTAL INS CO LTD
COMPLAINT NO: PUN-H-050-2122-0144
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Kishor Gugnani
Nagpur
2.
Policy No:
Type of Policy:
181300/48/2021/77
HAPPY FAMILY FLOATER-2015
3.
Policy period:
27.04.2020 TO 26.04.2021
4.
Sum Insured
1200000
5.
Date of inception of first policy:
27.04.2019
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr. Kishor Gugnani, 53 yrs
Himself
7.
Name of the Insurer:
The Oriental Ins Co Ltd
8.
Reason for repudiation/Partial
Settlement:
As per Maharashtra Govt. Cir.
9.
Date of receipt of the Complaint:
25.05.2021
10.
Nature of complaint:
Settlement of balance claim amount
11.
Amount of Claim:
Rs.19700/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
29.09.2021 On Line hearing
14.
Representation at the hearing
ss) For the Complainant:
Himself
tt) For the insurer:
Dr. Bharti Motling
15.
Complaint how disposed:
Allowed
16.
Date of Award
30.09.2021
Brief Facts of the case:
The complainant had taken Happy Family Floater with Respondent Insurer The Oriental Ins. Co Ltd
for self for SA 12 lakhs. He lodged claim of self -hospitalization in Radiance Hospital, Nagpur from
06.08.2020 to 07.08.2020 for Covid 19 positive. The total expenditure on hospitalization was
Rs.28000/- out of which the RI has settled an amount of Rs.8300/- deducted an amount of Rs.19700/-
stating claim settled as per Maharashtra Govt. covid circular .
Result of personal hearing with both the parties (Observations & Conclusions):
An online hearing was held on 29.09.2021 which was attended by both the parties.
Dispute here is pertaining to the less amount received by the complainant. The Major deduction made
by the RI is based on Maharashtra Govt. Guidelines. Maharashtra government guidelines are meant
for hospitals and not for Insurance companies. The said guidelines specifically mention that the
persons covered under insurance policy will be governed as per the respective policy terms and
conditions. Hence the deductions on these counts are not acceptable. In view of the clear cut
instructions of IRDAI to settle the claims as per policy terms and conditions, Forum instructed
Respondent Insurer to recalculate the amount as per the terms and conditions of the policy.
Accordingly they have conveyed that an additional amount of Rs. 13,700/- is payable.
Award is passed for the same.
AWARD
Under the facts and circumstances, the RI is directed to pay Rs.13700/- towards
full and final settlement of the complaint.
The award is to be satisfied within 30 days from the date of receipt of this award
failing which it will attract interest at the applicable bank rate plus 2% extra from
the date of rejection of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune this on 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. KUNDALIK B CHAVAN V/S IFFCO TOKIO GEN INS CO LTD
COMPLAINT NO: PUN-H-023-2021-0685
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. KUNDALIK CHAVAN, Malshiras,
Solapur
2.
Policy No:
Type of Policy:
H0452149
Corona Rakshak Policy
3.
Policy period:
24.09.2020 TO 06.01.2021
4.
Sum Insured
250000
5.
Date of inception of first policy:
24.09.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr. Kundalik B Chavan, 48 yrs
Mr. Kundalik B Chavan
7.
Name of the Insurer:
The IFFCO TOKIO GEN INS CO LTD
8.
Reason for repudiation/Partial Settlement:
Fraud & Misrepresentation
9.
Date of receipt of the Complaint:
05.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Sum Insured Rs.250000/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
uu) For the Complainant:
Absent
vv) For the insurer:
Mr.Suraj Singh Negi
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:-
• The complainant had taken Corona Rakshak Policy with Respondent Insurer The IFFCO
TOKIO GEN INS CO LTD for self for SA 2.5 lakh. He lodged claim of self hospitalization
in Rane Hospital, Akluj from 05.11.2020 to 08.11.2020 for Covid 19 positive. The complain-
ant is claiming for SA 250000/-. The claim was rejected on the ground of policy purchased by
Mr Siddhant Waghmare through online mode. In view of the same it was denied on grounds
of non-insurable interest.
• The complainant has given his clarification stating he has no direct or indirect relation with
Mr Waghmare. He was helping people in internet related services. Further the complainant
had booked the policy from his son’s mobile and policy premium was paid through his son’s
credit card.
• The complainant is requesting forum to intervene for settlement of the claim.
Contentions of the Respondent Insurer (RI):-
As per their SCN they have contended that,
1. The RI had received claim documents for reimbursement under the said insurance policy. On
scrutiny of the submitted claim documents kit, it was noted that the insured patient Mr Kund-
alik B Chavan was admitted in Rane Hospital, Akluj from 05.11.2020 to 08.11.2020 with
diagnosis of covid positive
It was noted that RT PCR report was dated 07.11.2020 and was diagnosed Covid 19 and was
discharged on 08.11.2020 without completion of 72 hours of hospitalization.
‘PAYMENT SHALL BE MADE ONLY ON HOSPITALISATION FOR A MNINUM
CONTINOUS PERIOD OF 72 HOURS FOLLOWING POSITIVE DIAGNONSIS FOR
COVID’
2. Thereafter the insured represented and claimed that he was diagnosed as covid positive on
04/11/2020 and also informed that the policy was purchased by Mr. Siddhant Waghmare
through online mode. In view of this, they repudiated the claim stating that
i. They had received multiple claims of this hospital from different insured for claiming
benefits under CRB policy. Hospital is involved in making forged claim documents
for its own employees even when all were on their job or carrying out their hospital
duties as per the roaster on their hospitalization dates.
ii. No HRCT or x-ray reporting done to rule out the severity of symptoms, whereas in the
discharge summary, the severity is indicated as 7/25.
iii. As per ICP record from the date of admission, there is no any major symptoms which
justified the need of admission.
iv. In ICP dyspnea is mentioned but when we check TPR chart, in that throughout admis-
sion respiration rate and oxygen saturation are within normal limit.
v. All TPR and BP charts are in single handwriting.
vi. All policies are purchased by Mr Siddhant Waghmare
vii. In view of the above, purchasing multiple policies for benefit of others who are not
related to Mr Waghmare violates the basic principle of insurance i.e. “Insurable inter-
est”
Result of personal hearing with both the parties (Observations & Conclusions):
Complainant remained absent for hearing conducted online on 19/05/2021. RI reiterated the
discrepancies observed in the claim documents and the suspicious activity of Mr. Siddhant Waghmare,
who is involved in purchasing of many such policies in the name of different people. It has been noted
that the said Siddhant Waghmare and Ganesh Chavan (son of the complainant) were working for
Rane hospital (where the complainant was admitted) as per the attendance record.
Taking into considerations of the contentions of both the parties and the documents placed on record,
forum has following observations:
i. The insured has contended that he was diagnosed covid positive on 4/11/2020 but going
through the indoor case papers, nothing is mentioned about the patient being already di-
agnosed case of covid 19. As per ICP the patient was admitted on 5/11/2020 with diagnosis
of viral pneumonia with suspected covid 19 and he was advised covid test on 6/11/2020.
Final diagnosis report was received on 7/11/2020. He was then discharged on 8/11/2020
without completion of 72 hours of hospitalization post diagnosis of covid 19.
ii. Two different RTPCR reports are found. One with sample collection on 4/11/2020 and
date of reporting 25/11/2020 is from VRDL, Akluj. The other one dated 7/11/2020 is from
Krsnaa Diagnostics Pvt. Ltd., Kothrud.
iii. If the insured was already tested positive on 4/11/2020 as per his contention, then it is not
understood what was the need for doing the report second time again on 7/11/2020.
This, coupled with the so many discrepancies pointed out by RI and apparent involvement of hospital
too, suggests that the documents are made up for grabbing policy benefits only.
Forum therefore, endorses Respondent’s decision of repudiation and dismisses the case.
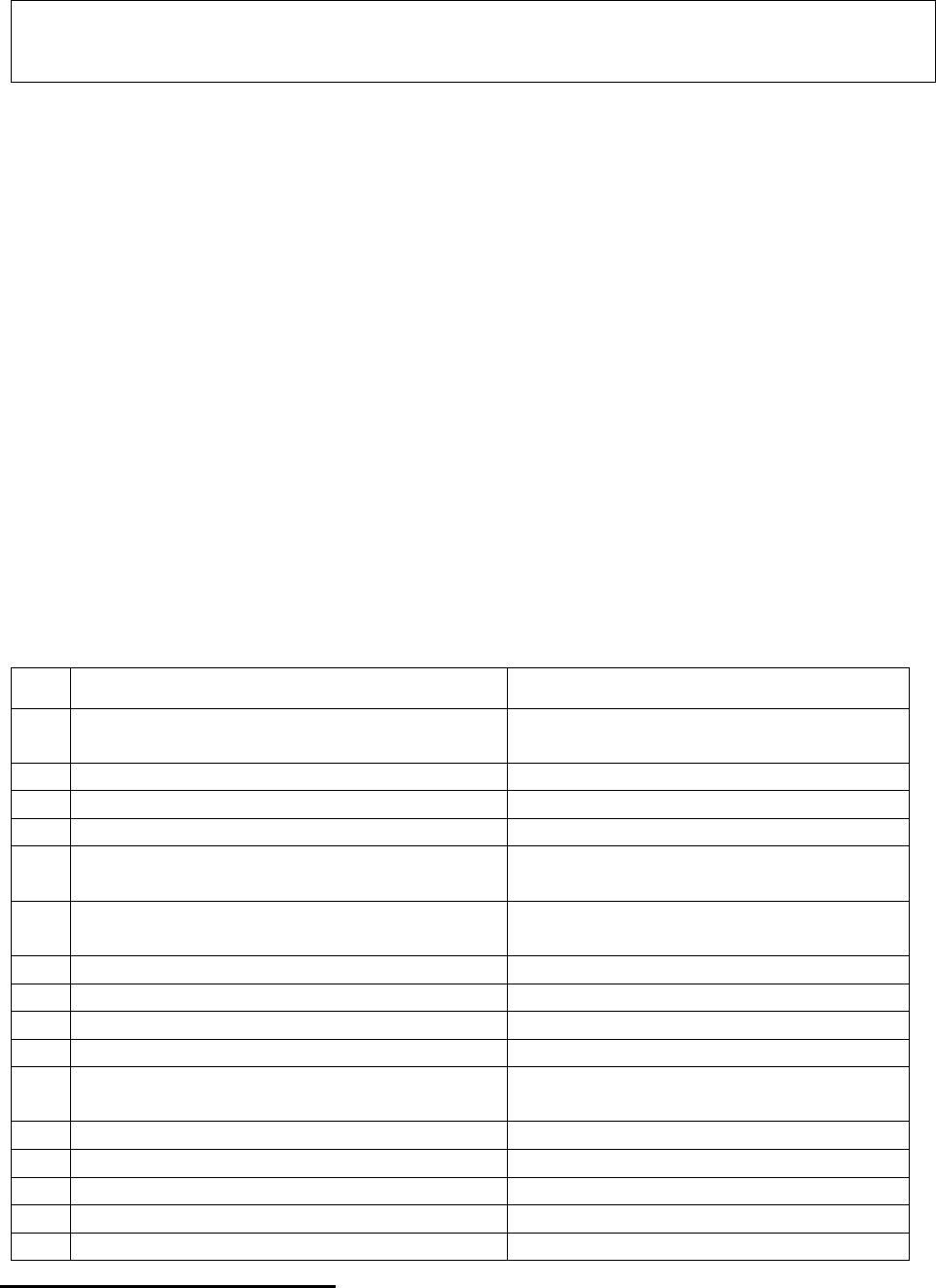
Award follows:
AWARD
Under the facts and circumstances, it is found that the complaint is based on fraudulent
documents, hence liable to be dismissed.
Dated: at Pune this on 17
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Smt. Lalitha Ramesh V/S HDFC ERGO General Insurance Co Ltd
COMPLAINT NO: PUN-H-018-1920-0430
Award No: IO/PUN/A/HI/ /2021-22
1.
Name & Address of the Complainant
Mrs. Lalitha Ramesh, Pune
2.
Policy No:
Type of Policy:
2950200179140100000
Sarv Suraksha Plan
3.
Policy period:
28.12.2011 to 27.12.2015
4.
Sum Insured Rs.
Various; depending upon insured event
5.
Date of inception of first policy:
28.12.2011
6.
Name of the Insured:
Name of the Policyholder:
Late Mr Ramesh Nagarajan; 58 years
Late Mr Ramesh Nagarajan
7.
Name of the Insurer:
HDFC ERGO General Insurance Co.
Ltd.
8.
Reason for repudiation/Partial Settlement:
All documents not received.
9.
Date of receipt of the Complaint:
09.10.2019
10.
Nature of complaint:
Non-settlement of claims
11.
Amount of Claim:
Rs.500000/- As per Ann VI-A
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
25.05.2021; Online
14.
Representation at the hearing
ww) For the Complainant:
Herself
xx) For the insurer:
Mr. Neeraj Shivangikar
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:-
The complainant is wife of the Deceased insured person and nominee under the policy. The Deceased
Insured person Sri Ramesh Nagarajan, had taken Sarva Suraksha Policy from Respondent Insurer
(Referred to as RI hereinafter) on 28.12.2011 to secure loan. The policy was taken for the term of 4
years i.e upto 27.12.2015.
The Insured was suffering from Dementia and was bed ridden also. He had a fall at home due to
imbalance in his right foot on 02.09.2014. He therefore, was admitted on 03.09.2014 at Inamdar
Speciality Hospital, Pune and diagnosed to have fracture of proximal fragment Lt. Femur with Loose
Stem. The insured patient was a k/c/o HTN +Depression Disorder. He was discharged on 12.09.2014
and further the treatment was continued till 26.09.2014 & 11.01.2015 and so on. The Insured person
died on 05.11.2015 after a long treatment and in a completely bed ridden condition for almost a year.
The claim was submitted to RI on 28.06.2019. She asked the RI, whether her claim is payable, the RI
said yes and only then she produced the claim papers in original. Till date the claim was not settled.
Contentions of the Respondent Insurer (RI):
As mentioned in the SCN (Self contained note), the complainant has filed three different claim under
permanent disability on 1.9.17, accidental death coverage on 24.10.19 and critical illness on 30.8.19.
they submitted that all the papers were not received from the claimant to arrive at a decision. During
the hearing, complainant was asked to submit all the claim papers to the RI to relook the matter and
accordingly, complainant conveyed vide her mail dt.26/05/21 forwarded the claim papers to the RI.
On receipt of the same, RI responded us through their mail dt.01/06/2021, contents of the same are
reproduced below:
‘We have gone through the documents submitted by the complainant and we submit as below –
1. Claim under Permanent Total Disability Coverage for INR 5,00,000/-
A. That as per the discharge card submitted Mr. Ramesh Nagrajan sustained fracture of
Proximal Fragment Lt. Femur with loose stem due to fall.
B. The said injury does not comes under the purview of the Permanent Total Disability or
Permanent Partial Disability Coverage.
C. Please refer the Section 2 - Personal Accident Schedule of Permanent Total Disability &
Permanent Partial Disability.
As such the claim under the Permanent Total Disability & Permanent Partial Disability is found
not payable.
2. Claim under Critical Illness coverage for INR 50,000/-
A. There are pre-conditions clearly mentioned in the policy terms and condition for the benefit
of claim under the Critical Illness. As per the said condition there is survival clause of 30 days. The
said condition is reproduced below for kind perusal of Hon'ble Ombudsman.
SECTION 1. CRITICAL ILLNESS
1. First Heart Attack -of Specified Severity:
If the Insured Person named in the schedule is diagnosed as suffering from a Critical
Illness which first occurs or manifests itself during the Policy Period, and the Insured survives for a
minimum of 30 days from the date of diagnosis, the Company shall pay the Critical Illness Benefit
as shown in the schedule.
Further, the complainant has not submitted any document as mentioned in the letters and an email
sent to Insured 25/05/2021.
The requirements documents were -
1. Letter from treating doctor stating exact duration of Coronary Artery Disease, Hypertension
when first diagnosed with all previous treatment papers related to it.
2. Letter from treating doctor stating cause of Coronary Artery Disease with duration of
causative factors.
3. ECG, Cardiac marker and Trop T Report supporting diagnosis of Myocardial Infarction.
There is absolutely NO document to show that Insured has survived for 30 days from the date of
diagnosis and NO document to show that the diagnosis evidenced by all of the following criteria:
• A history of of typical clinical symptoms consistent with the diagnosis of Acute Myocardial
Infarction (for e.g. typical chest pain)
• New characteristic electrocardiogram changes.
• elevation of infarction specific enzymes, Troponins or other biochemical markers
As such the claim under the Critical Illness is found not payable.
3. Claim under Accidental Death Coverage for INR 5,00,000/-
That as per the documents submitted with us, clearly shows that late Mr. Ramesh Nagarajan died
naturally. This claim was repudiated vide our letter dated 24/10/2019 stating that "The claim
documents submitted were reviewed and it was noted that the death of the insured was NON
accidental in nature. The Section 2 of the Policy provides coverage for death due to accidental
injury only during the policy period. Hence this claim is being repudiated by us as the claim did not
fulfil the requirements of accidental death under the Policy.
We would like to draw attention towards the definition of Accident as defined under the policy –
“Accident or Accidental” means a sudden, unforeseen and involuntary event caused by external,
visible and violent means. The copy of the Repudiation Letter filed herewith.
As such the claim under the Accidental Death is found not payable.
Further during the hearing, the complainant was stated that her husband was bed ridden and
unable to move. In this regard we would like to submit that Mr Ramesh Nagarajan is a patient
of Alzheimer’s psychiatric illness since July 2014. The complainant also submitted one certificate
issued by Dr. Deepak Kolekar who mentioned that Mr Ramesh Nagarajan was patient
of "Dementia". The Alzheimer’s psychiatric illness and Dementia is not the ailment which is
covered under the Critical Illness coverage.
Please find the attached statement of Insured confirming Alzheimer’s psychiatric illness since July
2014.’
Result of personal hearing with both the parties (Observations & Conclusion):
During the hearing held online on 25/05/2021, both the parties reiterated their respective stand.
From the depositions of the parties during the hearing and complainant’s narration of her husband’s
illness resulting into his death, it was felt that there might be still some chance to see the feasibility
of admissibility of her claim in either of the listed critical illnesses based on the facts of the case, as
the complainant is unaware of the entire policy cover. She was therefore given a chance to re-submit
all the claim papers to RI and RI was also asked to relook the matter in its entirety and see the
feasibility of admitting of the claim in either of the covers granted under the policy.
However, it is noticed from the detailed reply of the RI as given above and also re-verifying of the
facts with the policy cover it is found that even after giving one more opportunity to submit all the
claim papers in support of eligibility of her claim, complainant failed to establish it.
In view of the above, though the Forum appreciate the complainant’s concern, it has also to be kept
in mind that whenever any dispute arises, it is settled under the terms and conditions of the policy
under which a claim has arisen since these form the very basis of the contract between the parties.
Under the circumstances the Respondent Insurer has acted rightly as per the terms and conditions of
the policy in terms of rejection of claims under the policy and does not warrant any intervention of
the forum. Complaint therefore stands dismissed.
Award follows:
AWARD
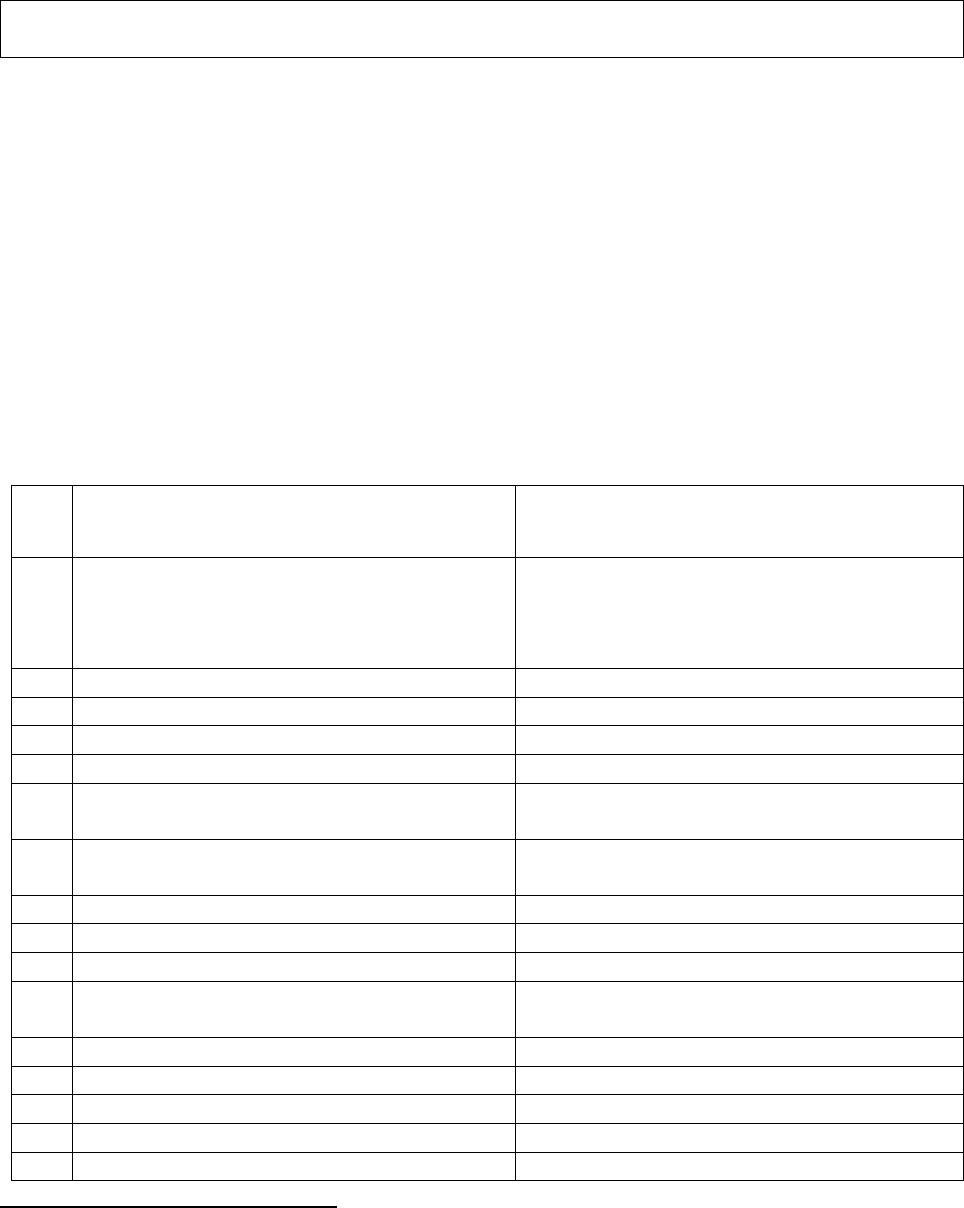
Under the facts and circumstances, it is found that the complaint is lack in merits. Complaint
therefore stands dismissed.
Dated: at Pune, on this 17
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Mahesh Hadiya v/s HDFC Ergo General Insurance Company Ltd
COMPLAINT NO: PUN-G-018-2021-0002
Award No IO/PUN/A/GI/ /2021-22
1.
Name & Address of the
Complainant
Mahesh Hadiya, Devratna-1002, Sector 14,
Taloja Panchanand Phase 1, Navi Mumbai.
2.
Policy No:
Type of Policy:
2311202732316900000
(9/4/2019 to 8/4/2020) RI has not released
renewal policy.
Private car package policy
3.
Policy period:
9/4/2020 to 8/4/2021
4.
Insured Declared Value (IDV):
Not applicable
5.
Date of inception of first policy:
9/4/2018
6.
Name of the Policyholder:
Mahesh Hadiya
7.
Name of the Insurer:
HDFC Ergo General Insurance Company
Ltd
8.
Reason for repudiation/Partial Settlement:
RI collected renewal amount of premium
and not released the policy.
9.
Date of receipt of the Complaint:
18/4/2020
10.
Nature of complaint:
Non-Issuance of renewal policy.
11.
Amount of Claim:
Not applicable.
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
13 1(h) Non Issuance of policy after
payment of premium.
13.
Date of hearing/Place:
28/07/2021; Online
14.
Representation at the hearing
yy) For the Complainant:
Himself
zz) For the insurer:
Mr. Neeraj Shivangikar
15.
Complaint how disposed:
Award
Contentions of the Complainant:
Complainant had taken car insurance policy from the Respondent Insure (RI) last year which was
expiring on 8.4.20. He approached RI for renewal well before expiry. He also mentioned that he has
claim on the existing policy. He was asked to make payment of Rs. 14539/- for renewal and the same
was paid by him on 06/04/2020. RI did not renew his policy and then demanded additional amount
of Rs. 11073/-. To his surprise, they said they have cancelled his OWN Damage (OD) section of his
policy and have paid him Rs. 11073/- which they asked him to repay.
He points out following lapses by RI which put customers into tremendous risk:

1. HDFC ERGO collected renewal premium but did not renew his policy. As a result, his existing
policy expired.
2. HDFC ERGO did not inform of OD cancellation at the time of renewal premium communication,
which they were fully aware. They kept him in dark while cancelling OD section of his policy. They
did not inform him in writing or verbally. This put him at tremendous risk as his car remained
uninsured. Further, he could not approach other insurer for renewal as he would end up applying
double premium & potential double policy.
As it can be seen from above, every time HDFC ERGO has taken unilateral decisions. Such unilateral
actions must be discouraged and customers must be protected.
Complainant requested RI not to mix-up the issue of Renewal of policy and Refund of OD premium
of expired policy.
Complainant approached to various offices of RI, even online complaint filed on their portal but RI
maintain their stands of non renewal and advised him to approach nearest Ombudsman office.
He is requesting the forum to intervene and ask the RI to release the renewed policy immediately.
Contentions of the Respondent Insurer (RI):
Contents of their SCN are reproduced below:
1. Complainant had filled an online proposal form to insure his vehicle. Basis the information given
by the complainant, RI issued a private car package policy. That, simultaneously, in order to verify
the veracity of representations of complainant qua previous policy, we wrote to his previous insurer.
Surprisingly, it is informed by the previous insurer that no such record found. Thus, complainant
made an incorrect statement which materially affected judgment of underwriter while assessing,
rating and accepting risk of the subject vehicle. That, as it was established that complainant made
an incorrect statement and / or declarations qua his previous insurance policy history with previous
insurer.
2.That, we received an information from and / or on behalf of complainant to the effect that on
16/02/2020 complainant’s said vehicle met with an accident and was damaged. That, immediately
we deputed Surveyor to ascertain exact cause of loss and extent of damages and damages are assessed
to the tune of INR 21,621/-.
3. That we further draw your kind attention to Condition number 8 of the above referred policy which
reads as – “The due observance and fulfillment of the terms conditions and endorsement of this Policy
in so far as they relate to anything to be done or complied with by the Insured and the truth of the
statements and answers in the said proposal shall be conditions precedent to any liability of the
Company to make any payment under this Policy”
4. That, in view of statement and declaration made by Complainant in proposal form pertaining to
previous insurance policy being found INCORRECT, however, the claim of the complainant was
processed and paid to the tune of INR 21,621/- by us vide NEFT Number N058201074782738 to the
workshop Fortune Cars Pvt. Ltd. on 26/02/2020.
5. That, further to this, in view of this an incorrect statement and / or declarations, we have cancelled
the OD portion from the policy and refunded the OD section amount of INR 11,073/- in the name of
complainant on 16/03/2020 as per below details - Cheque No Disp Date Courier Name AWB NO
411090 11/03/2020 BLUE DART 37087703365 11.
6. That, In the meantime, we had already sent the renewal quotation and the complainant paid the
amount on 06.04.2020 as per the quotation.
7. That, we had several communications with the complainant and explained him and requested him
to refund the amount of INR 11,073/- (OD premium) back to HDFC ERGO GIC stating that we have
honored the claim of the complainant and are not asking back the claim amount. (as your claim will

be invalid if OD section is not covered). It is only the premium amount that we are requesting you to
refund. That, Ms. Manvi Sharma from our team had also sent a payment link on 08/04/2020 from
HDFC Pazapp for the same amount to initiate the refund from insured's end, but the insured
deliberately avoiding to refund the said premium.
8. That we had also informed insured that once the above amount is refunded, then only we would be
able to release the renewed policy, however the complainant is insisting on either to share the renewed
policy copy or refund the premium he paid to us under renewal which is not possible.’
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 28/07/2021 (through video-conferencing) both the parties reiterated
their respective stand
On hearing both the parties and documents submitted on record, forum found many flaws in the
system from both the sides as detailed below:
1. The policy of 19-20 shows applied OD premium as Rs.9384/- after giving consolidated discount
of Rs.10369/- against discounts head. Whether NCB was applied or not is not clear from the schedule.
The policy shows details of previous policy number with NCB mentioned as 0%.
If no NCB discount was given, then there was no need to cancel the OD part of the policy.
It is also not clear, how RI refunded Rs.11703/- as the actual premium charged is Rs.9384/- only. RI
should keep in mind that they are trustees of public fund and they cannot play with it whimsically
without having strong policy terms in its support. It establishes the fact that the RI paid an OD claim
in absence of having OD premium for the same.
2. RI, in a very hap hazard way has paid the claim without observing all the underwriting formalities
while paying a claim and has wrongly refunded the OD premium.
As per India Motor Tariff, refund is not applicable in case of a cancellation of policy, if there is a
claim reported on the policy. Forum refers following clause for the same.
As per section 5 of the policy wording which states that “5. The Company may cancel the policy by
sending seven days notice by recorded delivery to the insured at insured’s last known address and in
such event will return to the insured the premium paid less the pro rata portion thereof for the period
the Policy has been in force or the policy may be cancelled at any time by the insured on seven days’
notice by recorded delivery and provided no claim has arisen during the currency of the policy, the
insured shall be entitled to a return of premium less premium at the Company's Short Period rates for
the period the Policy has been in force.”
Complainant has also not disclosed the fact of refund of premium by the RI on the earlier policy in
his complaint. In fact, he pleaded innocence about it. Whereas, it is seen that the refund was made by
cheque; not NEFT. Which means he himself has deposited it into his bank account. This is also
considered as suppression of material fact while approaching to this forum and forum strongly objects
to this, with displeasure.
Further, his innocence could have been proved if he had repaid the OD premium, which was asked
on 8/4/2020 by the RI.
Complainant has also not clarified about the wrong information of policy of ICICI mentioned by him
in his earlier policy proposal.
3. By not renewing the policy further, the RI had invited a great risk. Hopefully, there was no claim
in the next year.
In the entire transactions, it is observed that both the parties are at fault and the complainant has tried
to take advantage of flaw in the systems of RI and remained adamant in not repaying the wrongly
credited amount in his account.
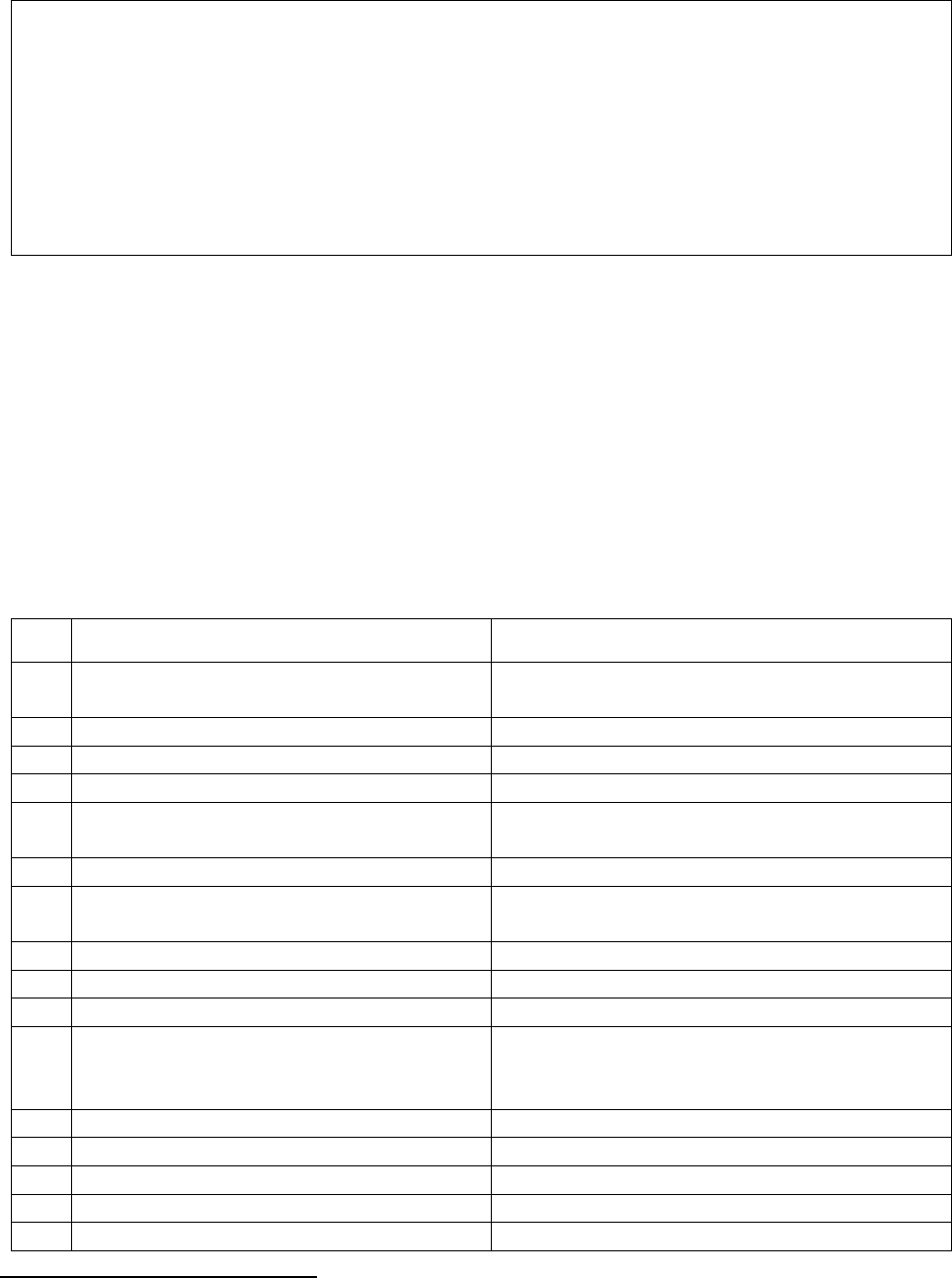
AWARD
Under the facts & circumstances of the case, the Respondent Insurer is directed to refrain
from the unethical business practices exhibited in this case. Any recurrence of this kind of
serious incident can attract serious consequences. Forum would like to have a letter of
confirmation in this respect from the RI.
No order in favour of complainant as the renewal of policy period has also got over and the
complainant must have arranged for a valid insurance for his vehicle. He is also warned to
be honest while disclosing money related information to the authorities.
Dated: On 20
th
of September 2021 at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Mahesh B. Halkeri Vs Star Health and Allied Insurance Co. Ltd
COMPLAINT NO: PUN-H-044-1920-0664
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the Complainant
Mr. Mahesh Bhaskar Halkeri , Thane(w)
2.
Policy No:
Type of Policy:
P/17114/01/2019/000057
Family Health Optima Insurance 2017
3.
Policy period:
1/4/2018-31/3/2019
4.
Sum Insured
10,00000/-
5.
Date of inception of first policy:
1/4/2012
6.
Name of the Policyholder:
Name and age of the insured:
Bhaskar Halkeri
Mahesh Halkeri, age 24 yrs.
7.
Name of the Insurer:
Star Health and Allied Insurance Co. Ltd
8.
Reason for repudiation/Partial
Settlement:
Gerd with ulcer which is treated for alcoholic
Gastritis -not payable
9.
Date of receipt of the Complaint:
27/01/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
Claimed amount + mental agony Rs.25000/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
13 1(b)
13.
Date of hearing/Place:
Online hearing on 06/08/2021
14.
Representation at the hearing
aaa) For the Complainant:
Mr. Bhaskar Halkeri-father
bbb) For the insurer:
Dr. Smita Sonwane
15.
Complaint how disposed:
Allowed
Contention of the complainant:
Complainant and his family are insured with the Respondent Insurer (RI) under health insurance
policy since 7 years. His son Mr. Mahesh, aged 24 yrs. was admitted in World Gastroenterology
Institute Hospital from 05/01/2019 to 06/01/2019 for the complaints of bleeding through rectum,
hyperacidity, reflux esophagitis, bloating, abdominal discomfort, loose motion and constipation
alternate-on and off which was investigated in WG Institute, Mumbai. The same was diagnosed with
Gerd with Ulcer Oseophagus with chronic Duodenitis.
RI has rejected the claim stating that this illness is due to alcoholic consumption which is not payable
as per policy exclusion no.8-“intoxicating drug /Alcohol”.
In complaint, he has agreed to taking alcohol but it is occasionally. He has also submitted certificate
of his treating doctor stating that, ‘patient is suffering from Gerd and itiology of Gerd is not due to
alcohol consumption. In this case cause is idiopathic in nature.’
However, RI has not agreed with the certificate and rejected the claim. Complainant is saying that he
is having policy with RI since 7 years and not a single claim is made by him during the 7 years.
Complainant requested to intervene and instruct the RI to settle the claim.
Contention of the Respondent Insurer (RI):
They have agreed having continuous insurance of the complainant since 7 years. Contents of their
SCN are reproduced below:
‘CLAIM NO. CLI/2019/171114/0607688:
1) The Insured made a claim vide Claim No. CLI/2019/171114/0607688 in the 7
th
year of the
Medical Insurance Policy.
2) The Insured submitted a claim for a sum of Rs. 1,26,490/- and the last documents were sub-
mitted on 23/01/2019.
3) As per the Discharge Summary of the treating hospital, the insured person was diagnosed
with MILD GERD with EROSIVE ATROPHIC PAN GASTRITIS and CHRONIC DUODENI-
TIS with BLUNTING OF VILLI and H PYLORI INFECTION. Additionally insured also diag-
nosed with MULTIPLE ILEAL ULCERS with ONE HYPERTROPHIED LYMPHOID FOLLI-
CLE and RECTUM POLYP with IRRITABLE SPASTIC LEFT BOWEL
As per the Discharge Summary of the treating hospital, the insured person has complaints
HYPERACIDITY, HEART BURN, REFLUX OESPHAGITIS, BLOATING ON AND OFF FOR PAST
3 TO 4 YEARS AND OCCASIONAL CONSUMPTION OF ALCOHOL. The present admission and
treatment of the insured patient is for mild GERD with linear ulcer in lower third of OESOPHAGUS
and CHRONIC DUODENITIS which is a complication of alcohol consumption. Therefore, the claim
for reimbursement was repudiated.’
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 06/08/2021 (through video-conferencing), both the parties reiterated
their respective stand.
Upon hearing contentions of both the sides and the documents submitted, the forum observed that the
document on which the RI has relied upon as the proof of alcoholism, is the hospital’s consultation
dt.05/01/2019, which mentions the personal history as ‘ALCOHOL OCCASSIONALY’.
From the web search for the causes of Gerd, results show as:
Risk factors
Conditions that can increase your risk of GERD include:
• Obesity
• Bulging of the top of the stomach up into the diaphragm (hiatal hernia)
• Pregnancy
• Connective tissue disorders, such as scleroderma
• Delayed stomach emptying
Factors that can aggravate acid reflux include:
• Smoking
• Eating large meals or eating late at night
• Eating certain foods (triggers) such as fatty or fried foods
• Drinking certain beverages, such as alcohol or coffee
• Taking certain medications, such as aspirin
In view of this, as the alcoholism can aggravate the complainant’s said ailment and the fact of
acceptance of having alcohol, even though occasionally, cannot make the insured patient free from
contributing to the said ailment. As alcoholism is not the sole cause of illness, forum, therefore, is of
the view that let the complainant bear 30% cost of the admissible amount of payable claim.
Complainant has not mentioned the claimed amount but has mentioned Rs.25000/- against mental
agony. Complainant is made aware that this forum does not have authority to award any amount on
this count. RI in their SCN have mentioned claim amount as Rs. 1,26,490/-
Complaint allowed partially. Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to pay 70%
of the admissible amount of the claim as per the policy terms and conditions to the
complainant towards full and final settlement of the complaint.
The award is to be complied with within one month from the date of receipt of this award
failing which it will attract interest at the bank rate plus 2% extra from the date of rejection of
claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: On 30/09/2021 at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mrs. Meenal Satish Gosavi Vs The New India Assurance Co. Ltd
COMPLAINT NO: PUN-H-049-1920-0666
Award No IO/PUN/A/HI/ /2020-21
1.
Name & Address of the Complainant
Meenal Satish Gosavi, Kalyan
2.
Policy No:
Type of Policy:
131300/34/18/28/0000/1948
New India Floater Mediclaim
3.
Policy period:
15/11/2018-14/11/2019
4.
Sum Insured
800000/-
5.
Date of inception of first policy:
25/10/2007
6.
Name and age of the insured:
Name of the Policyholder
Meenal Satish Gosavi; 37 years
Same as above
7.
Name of the Insurer:
The New India Assurance Co. Ltd
8.
Reason for repudiation/Partial
Settlement:
The treatment given to the patient does not
support the need for hospitalization, hence
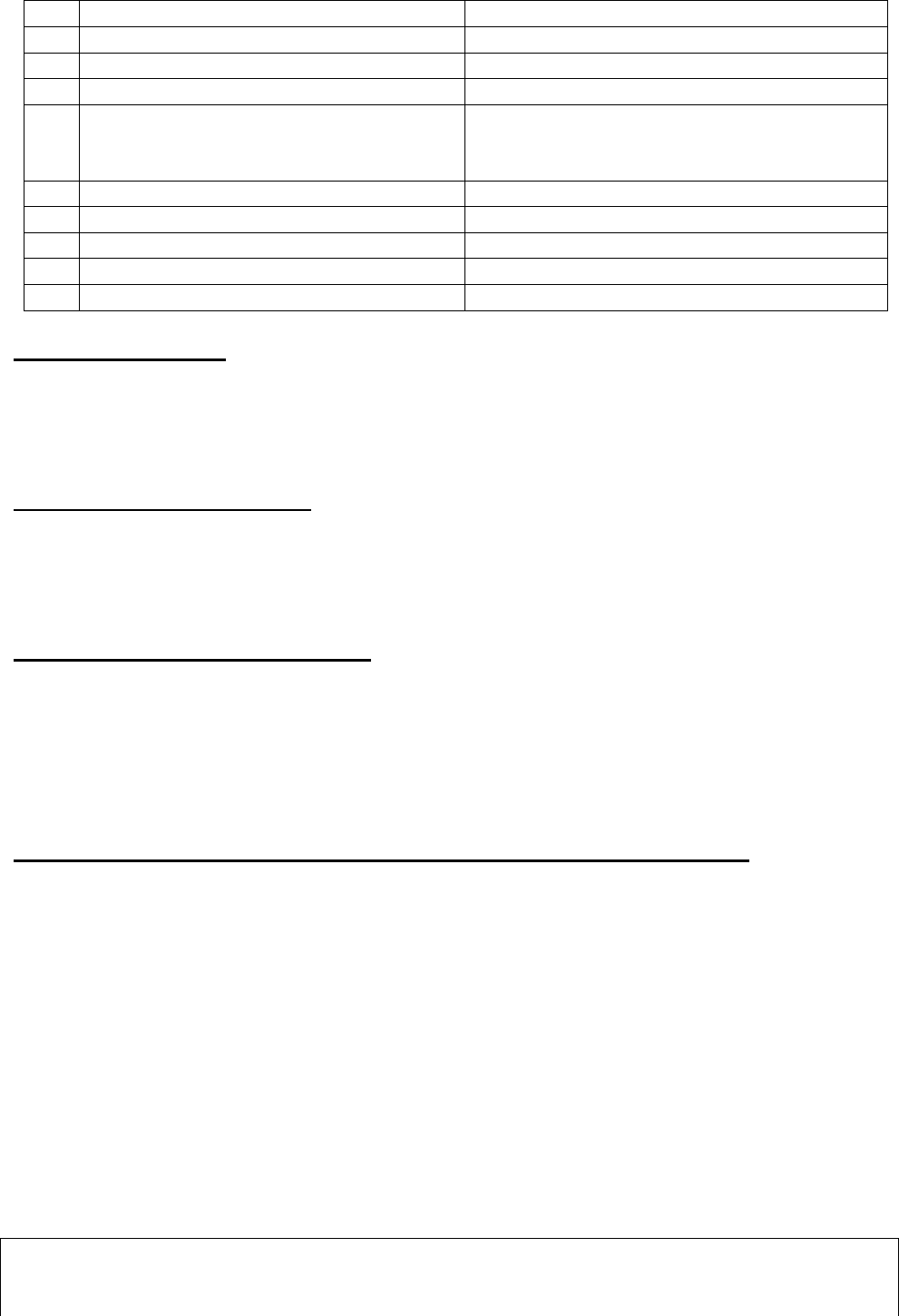
rejected the claim
9.
Date of receipt of the Complaint:
27/01/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
15582/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
13 1(b)
13.
Date of hearing/Place:
Online hearing on 13.08.2021
14.
Representation at the hearing
ccc) For the Complainant:
Herself
ddd) For the insurer:
Mr Satish Khiradkar
15.
Complaint how disposed:
Allowed
Brief facts of the Case:
The Complainant is having Health policy with Respondent Insurer from 2007 for sum insured of
Rs.800000/- covering self and family members. She was admitted in Anu Nursing home for treatment
of UTI from 15.4.2019 to 18.4.2019. RI has rejected the claim stating that there was no need for
hospitalization.
Contention of the Complainant:
She contends that she was suffering from severe Urinary Tract Infection which could be treated only
with hospital admission. Her treating doctor is not such who advises unnecessary admission for
extracting money. She is aggrieved that company has rejected her claim objecting to his advice.
She has supported her complaint with the certificate of Dr. Prashant Jadhav.
Contention of Respondent Insurer(RI)
As per SCN (Self contained note), their Committee has reached to the decision that claim has rightly
been rejected as per rejection letter.
As per rejection letter, patient treated for urinary tract infection from 15/4/2019 to 18/4/2019. It is
evident that as per claim document received it is observed that there was conversion of OPD treatment
to IPD. Patient could have been treated on OPD basis. The treatment given to the patient does not
support the need for hospitalization, hence rejected the claim.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 13.08.2021 (through video-conferencing) both the parties reiterated
their respective stand.
RI contended that the patient was treated by oral medication only which was possible on OPD basis.
They had obtained an independent doctor’s opinion also, who opined that as a general practice, this
treatment is given on OPD basis.
The complainant contended that she was not getting cured by oral medications, tried for 3-4 days, she
was advised to get admitted. There are prescriptions of 28.3.2019 and 11.4.2019. Medicines were
prescribed for 5 days. Treating doctor Prashant Jadhav has given a certificate stating that as the patient
was not responding to oral medication, there was need for admission and give injectable antibiotics.
If this timely management was not given, this could have progressed to pyelonephritis and subsequent
kidney failure also. So, IV antibiotics were given as per her needs.
In view of above, forum does not agree with RI’s stand and their decision of repudiation is set aside
by following order:
AWARD
Under the facts and circumstances, the RI is directed to pay Rs.15582/-less deductible as per the
terms and conditions of the policy to the complainant, towards full and final settlement of the
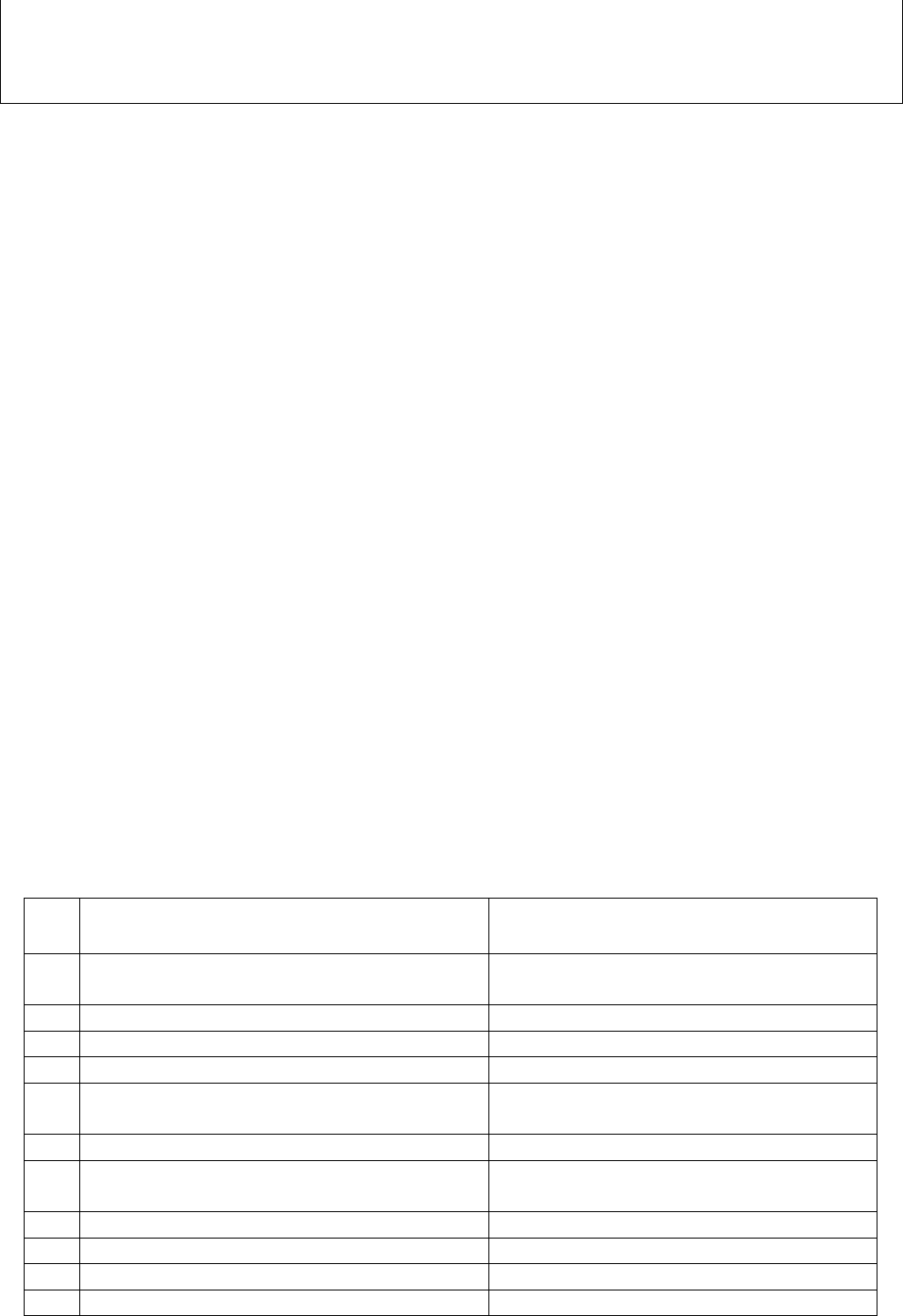
complaint.
The award is to be settled within one month from the date of receipt of this award failing which
it will attract interest at the prevailing bank rate plus 2% extra from the date of rejection of the
claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award
and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: Pune, this on 15
th
day of September, 2021
VINAY SAH
INSURANCE OMBUDSMAN PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. MUKUND C JANRAO V/S STAR HEALTH & ALLIED INS CO LTD
COMPLAINT NO: PUN-H-044-2021-0088
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
MR. Mukund C Janrao
Barshi
2.
Policy No:
Type of Policy:
P/151125/01/2019/000384
Star Comprehensive Insurance Policy
3.
Policy period:
18.07.2018 to 17.07.2019
4.
Sum Insured
Rs.500000
5.
Date of inception of first policy:
14.07.2017
6.
Name and age of the Insured:
Name of the Policyholder:
Mr. Mukund Chandrabhan Janrao, 60 yrs
Same as above
7.
Name of the Insurer:
Star Health & Allied Ins Co Ltd
8.
Reason for repudiation/Partial Settlement:
Pre existing Disease and papers of the
same not produced by complainant
9.
Date of receipt of the Complaint:
07.03.2020
10.
Nature of complaint:
Settlement of full claim amount
11.
Amount of Claim:
Not mentioned
12.
Insurance Ombudsman Rule (IOR)2017
Rule 13 1 (b)
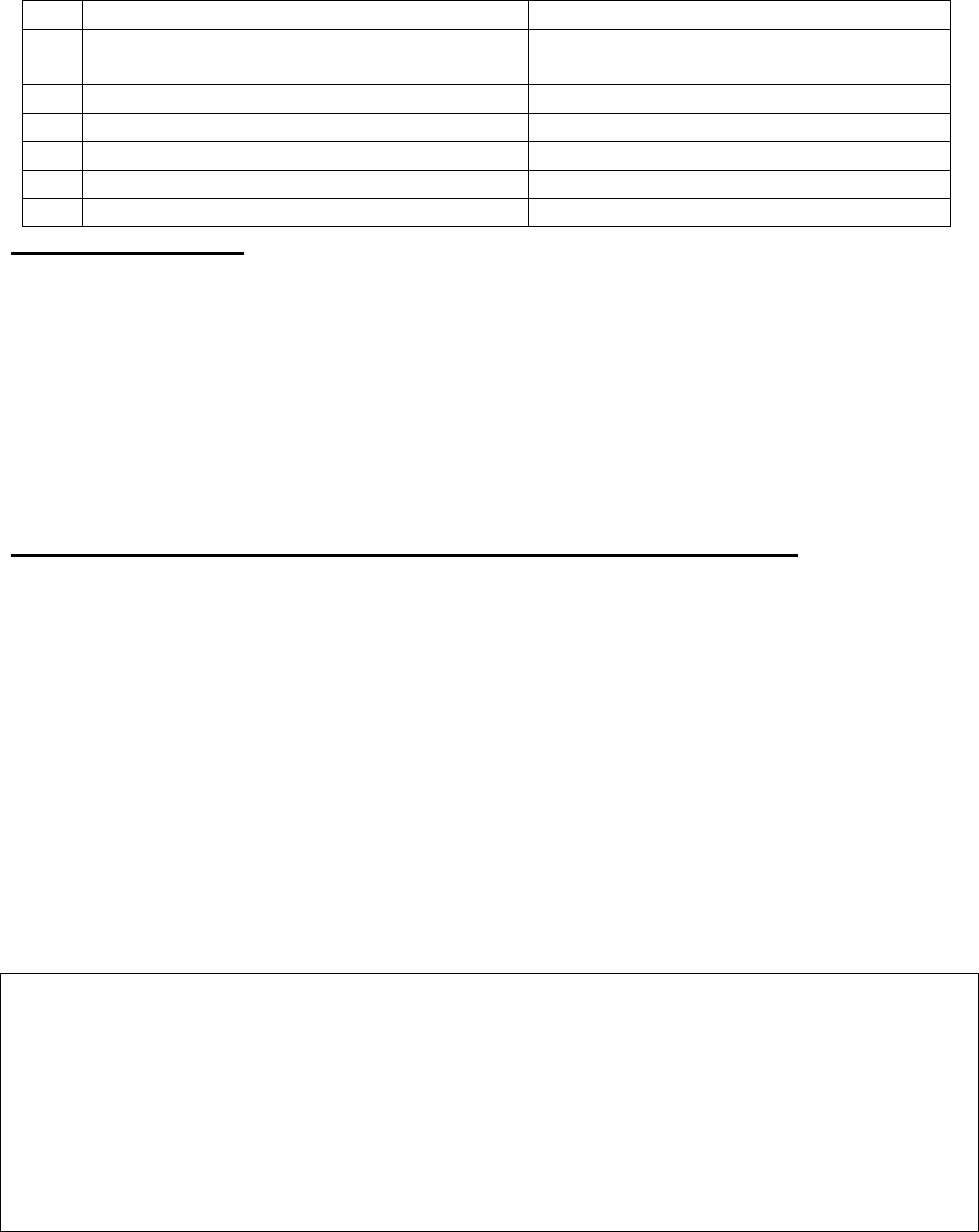
under which the Complaint was registered:
13.
Date of hearing/Place:
On line hearing on 22/09/2021
14.
Representation at the hearing
eee) For the Complainant:
Sudarshan (son)
fff) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Award
16.
Date of Award:
30/09/2021
Brief facts of the case:-
• The complainant has given a complaint to this forum about cashless pre authorization of his knee
replacement surgery to be performed at Dinanath Hospital on 6/2/2020 declined by the RI (Re-
spondent Insurer) saying that some documents pertaining to hospitalisation at Jagdale Hospital
on 2/3/2019 not submitted.
• He is contending that in reality there is no any record dated 2/3/2019 because he had not taken
any treatment at this hospital on the alleged date. But Insurance Company without any documen-
tary proof denied his request for cashless treatment.
• He has requested forum to take appropriate action against Star Health & Allied Ins. Co Ltd and
order them to allow his cashless claim.
Result of personal hearing with both the parties (Observations & Conclusion)
During the personal hearing on 22/09/2021 held Online, it came to light that the claim pertaining to
Jagdale Mama Hospital where the complainant was admitted and operated for Left frontal and partial
burr hole in April 2019 and May 2019 is not paid. The knee replacement claim for which the
complaint was raised is already settled for Rs. 2,76,100/-. Complainant also agreed to having received
this claim.
Regarding his earlier claim, RI representative submitted that they had raised query on 13.07.2019 for
additional documents which were not submitted by the complainant. In absence of documents, they
are unable to process the claim, hence the claim was repudiated vide letter dated 30/07/2019. The
complainant argued that they never received requirement letter.
In view of this, complainant once again is given a chance to submit the earlier treatment papers of his
CVA within 15 days to the RI and RI has to process the claim within the purview of policy terms and
conditions.
Award follows:
AWARD
Under the facts and circumstances, complainant is again given a chance to submit the papers
as called for by RI within 15 days from receipt of this order to the RI.
RI is advised to process the claim within the purview of policy terms and conditions and convey
the decision to the complainant within 15 days thereafter.
In case the complainant fails to submit the available documents within the given time frame, RI
will not be bound by this order of processing of the claim and this award will get converted into
dismissal of the complaint.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(a) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
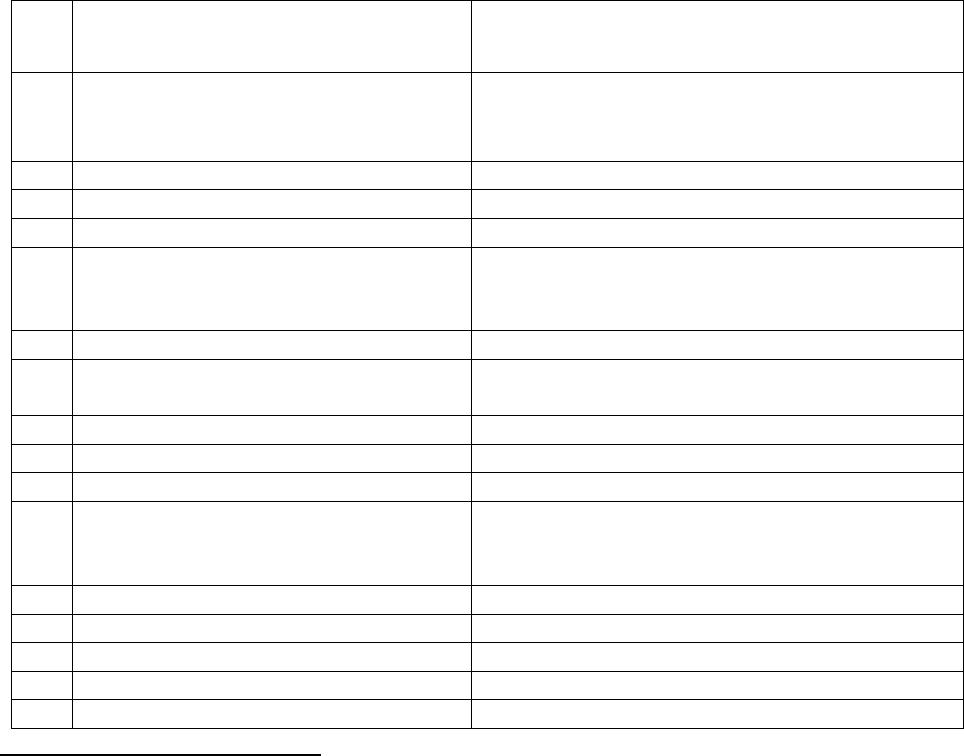
17(b) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: on this 30
th
day of September 2021 at Pune
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr.N.P.Hariharan V/s United India Insurance Company Ltd
COMPLAINT NO: PUN-H-051-2021-0007
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr.N.P.Hariharan,Navi Mumbai
2.
Policy No:
Type of Policy:
500100/28/18/P1/11142519
Tailor made Group Mediclaim Policy for Retirees
of Union Bank
3.
Policy period:
1/11/2018-31/10/2019
4.
Sum Insured
4,00,000
5.
Date of inception of first policy:
Not mentioned
6.
Name and age of the Insured:
Name of the Policyholder:
Mr. N P Hariharan; 73 years
Indian Banks Association a/c Union Bank of
India (Retired)
7.
Name of the Insurer:
United India Insurance Co. ltd
8.
Reason for repudiation/Partial
Settlement:
Neither listed in Day care nor in inpatient
9.
Date of receipt of the Complaint:
16/3/2020
10.
Nature of complaint:
Total Rejection of claim
11.
Amount of Claim:
37767/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the Complaint
was registered:
13 1(b)
13.
Date of hearing/Place:
08/09/2021; Online
14.
Representation at the hearing
ggg) For the Complainant:
Himself
hhh) For the insurer:
Ms. Pamela Pinto
15.
Complaint how disposed:
Allowed
Contention of the complainant:
The complainant was covered under a corporate policy of his wife Mrs. Radha who has retired from
Union Bank of India, issued by Respondent Insurer (herein after is called RI) .
The complainant was diagnosed for Non-Hodgkin’s Lymphoma i.e. cancer of lymphatic system in
July2018. Doctor advised 6 sessions of Chemotherapy beginning Sept.2018 at interval of 23 days and
this ended in Feb. 2019. Further as a matter of abundant caution the same doctor advised that he needs
to undergo a Remission Chemotherapy from April 2019 for two years with interval of every two
months, ending in Feb.2021.
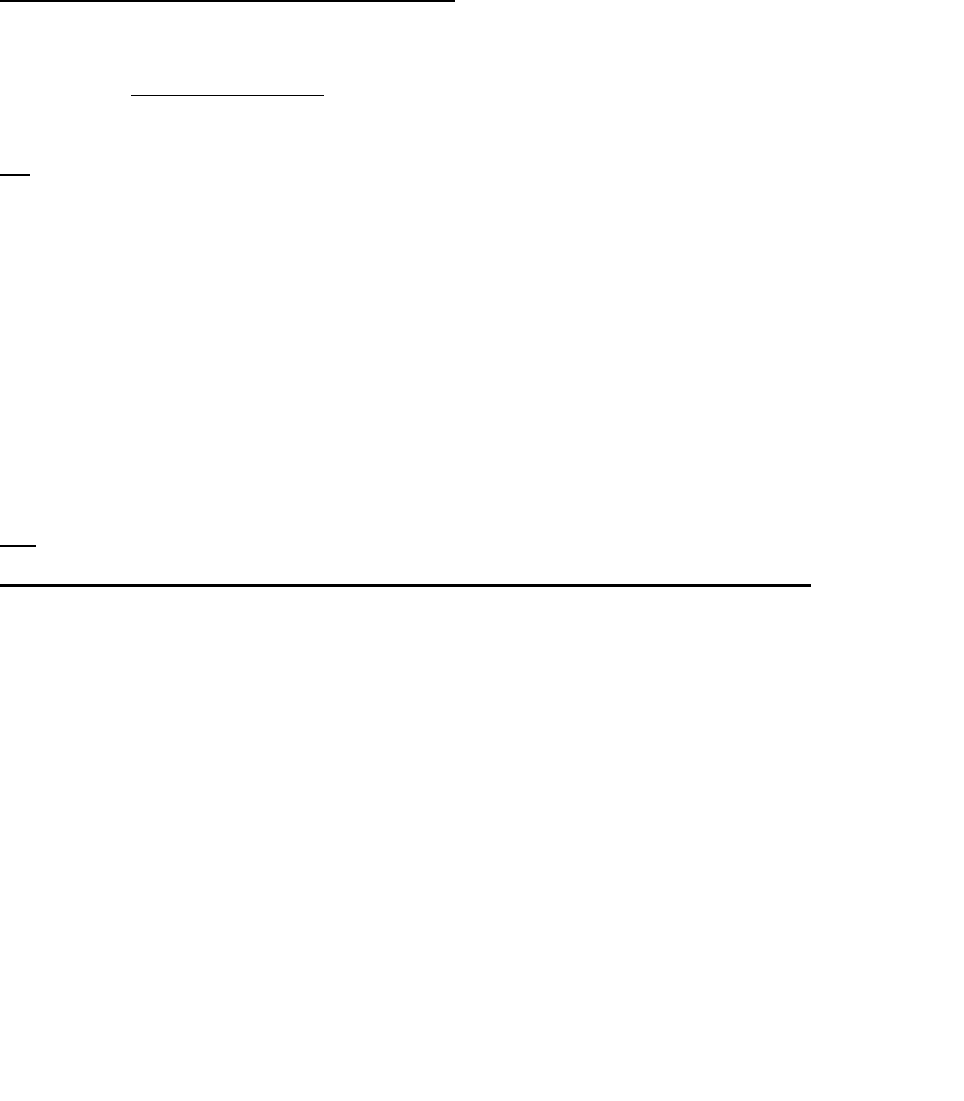
He has one more policy with Star HI also, from whom he had opted cashless claim of Rs. 52920/-out
of hospital’s total Bill of Rs.80503/- and for balance amount of Rs.35767/-, he claimed from RI.
RI has rejected the claim stating that the treatment does not require hospitalization nor it falls under
day care treatment as this injection can be taken on OPD basis. This is adjuvant Chemotherapy and
this is additional (after already curing of the disease) and state that in their policy there is no provision
for reimbursing ADJUVENT CHEMOTHERAPY.
He contends that why should there be a different yardstick for two Insurance companies for the same
medical procedure. Aggrieved with the rejection of claim by RI and filed complaint before this Forum
for resolution.
Contentions of the Respondent Insurer (RI):
As per rejection letter, patient admitted in hospital for injection rituximab and discharged on same
day. This is neither listed in day care procedure nor required inpatient care. Hence the claim is being
denied under clause no. 1.1 & 3.3 of the policy.
Clause reads as follow:
1.1 “Now This policy Witnesses that subject to the terms,conditions,exclusions and definitions
contained herein or endorsed, or otherwise expressed hereon the Company undertakes that if during
the period stated in the schedule or during the continuance of this policy by renewal any insured
person shall contract any disease or suffer from any illness(hereinafter called Disease) or sustain
any bodily injury through accident (hereinafter called Injury) and if such disease or injury shall
require any such insured person, upon the advice of duly qualified Physician /Medical Specialist
/Medical Practitioner (hereinafter called Medical Practitioner) or of duly qualified surgeon
(hereinafter called Surgeon) to incur hospitalization/domiciliary hospitalization expenses for
medical/surgical treatment at any Nursing Home/Hospital in India as herein defined (hereinafter
called Hospital) as an inpatient ,the Company will pay through TPA to the hospital/nursing home or
Insured the amount of such expenses incurred as are Medically Necessary and reasonable and
customary in respect thereof by or on behalf of such Insured Person but not exceeding the Sum Insured
in aggregate in any one period of insurance stated in the schedule hereto”.
3.3 Not listed in day care procedure.
Result of personal hearing with both the parties (Observations & Conclusions):
During the hearing, held online on 8/9/2021, both the parties reiterated their respective stand.
Complainant contended that for the same treatment, RI had paid his earlier claims. For which, RI
replied that those claims were erroneously paid by them and they are correcting their mistakes
happened in past.
From the web search, forum finds that,
‘Adjuvant therapy is often used after primary treatments, such as surgery, to lessen the chance of your
cancer coming back. Even if your surgery was successful at removing all visible cancer, microscopic
bits of cancer sometimes remain and are undetectable with current methods.’
Rituximab is administered for treatment on Cancer. As per definition of Chemotherapy,
Chemotherapy is the use of drugs to destroy cancer cells. It usually works by keeping the cancer
cells from growing, dividing, and making more cells. Because cancer cells usually grow and divide
faster than normal cells, chemotherapy has more of an effect on cancer cells.
The most common way that chemotherapy drugs are given is through a needle into a vein.
This is called intravenous or IV chemotherapy. Chemotherapy can also be taken as a pill,
capsule, or liquid by mouth, as an injection or shot, or as a cream that is put directly on your
skin.
As per the policy, it is observed that the RI has covered ‘Chemotherapy including parental
chemotherapy’ in their policy clause no.3.3 (13). There is no exclusion found for Adjuvant therapy.
Chemotherapy as defined in various dictionaries it means the treatment/drugs which attack on cancer
cells and reduce the cancerous cells to spread. The drugs administered on patient are for this purpose
only. Hence rejection of chemo treatment is against the policy terms.
In view of this, complaint is allowed.
Award follows:
AWARD
As per the offer given by the Respondent and agreed by the complainant, the Respondent
Insurer is directed to pay Rs.35767/- less deductibles if any, as per the policy terms and
conditions to the Complainant towards full and final settlement of this complaint.
The award is to be satisfied within one month from the date of receipt of this award failing which
it will attract interest at the applicable bank rate plus 2% extra from the date of rejection of the
claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune this 17
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Narendra Pawar Vs. Star Health & Allied Insurance Company Ltd.
COMPLAINT NO: PUN-H-044-1920-0544
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. Narendra Madhukar Pawar
1,A Pitreshwar Colony, Shirpur,
Dhule – 425405 (M.S.)
2.
Policy No:
Type of Policy:
P/161130/01/2019/053465
Family Health Optima Insurance Plan
3.
Policy period:
11/05/2019 to 10/05/2020
4.
Sum Insured/IDV
Rs.5 lakhs
5.
Date of inception of first policy:
10/01/2017
6.
Name & age of the Insured:
Name of the Policyholder:
Mrs. Bebibai Madhukar Pawar –49 years (W)
Mr. Madhukar Pandit Pawar
7.
Name of the Insurer:
Star Health & Allied Insurance Company Ltd.
8.
Reason for repudiation:
Misrepresentation of material facts.
9.
Date of receipt of the Complaint:
04/12/2019
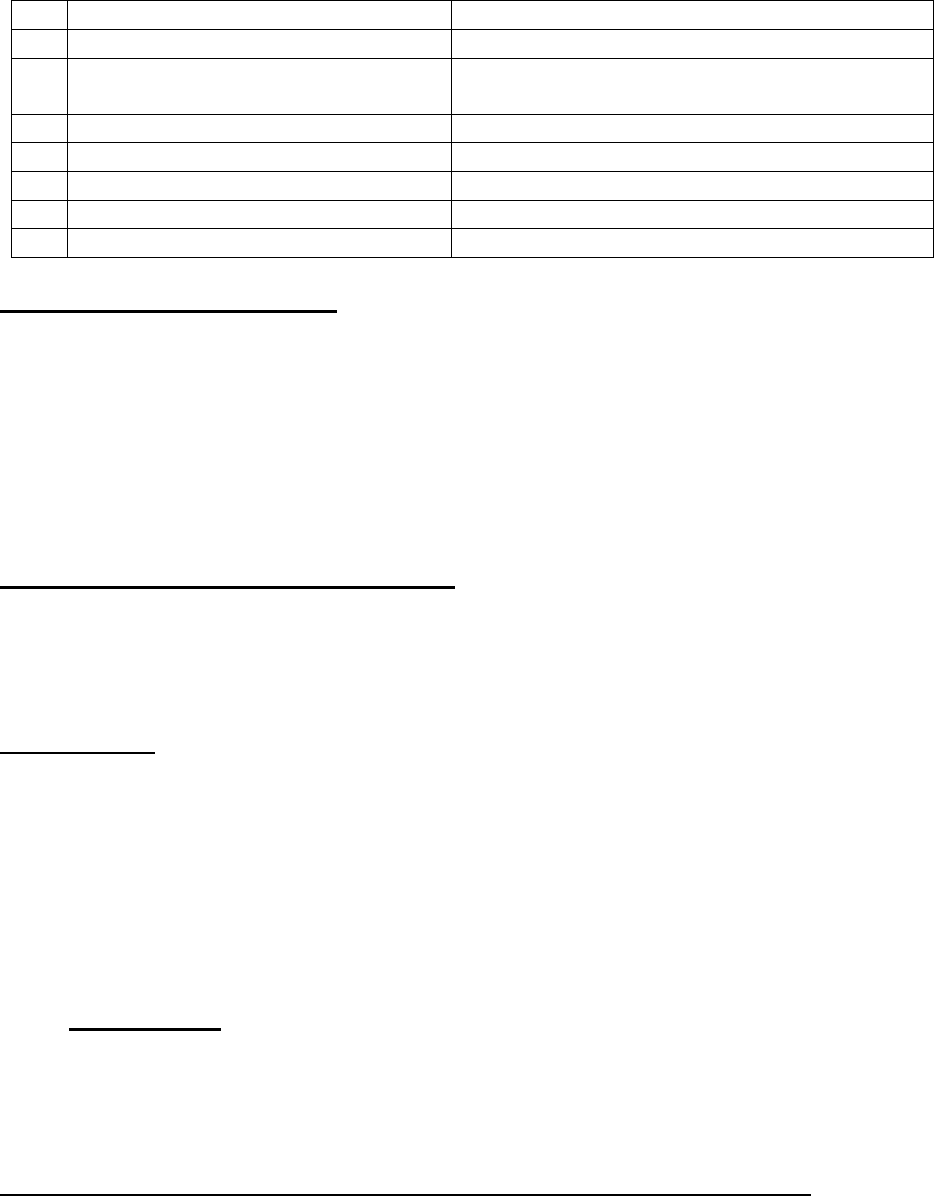
10.
Nature of complaint:
Rejection of claim.
11.
Amount of Claim:
Rs.55,000/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021, Online. Pune.
14.
Representation at the hearing
iii) For the Complainant:
Absent.
jjj) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Dismissed.
Contentions of the Complainant:
Complainant’s mother aged 49 years was insured with the Respondent Insurer (RI) under the above
policy for the period 11/05/2019 to 10/05/2020. She was admitted to Aashay Hospital, Jalgaon on
13/05/2019 and underwent Hysterectomy surgery on 14/05/2019. She was discharged on 18/05/2019.
RI rejected the claim of Rs. 46,000/- specifying that indoor case papers were not shared with them by
the hospital and have noticed tampering/discrepancy in some of the documents.
The complainant has approached the Grievance Cell of the RI to reconsider his rejected claim amount
but they have stood with their earlier decision of repudiation. In view of this, the complainant has
approached the forum for the resolution of his grievance.
Contentions of the Respondent Insurer (RI):
The claim has been rejected by the RI vide their letter dated 28/06/2019 as indoor case papers were
not available at the hospital. The cash paid bill receipts were not available and also the submitted
consultation papers were found tampered. They have further stated that there is discrepancy in the
submitted claim documents, which amounts to misrepresentation. The claim has been rejected as per
Condition No.6, which is reproduced hereunder:
Condition No.6 – “The Company shall not be liable to make any payment under the policy in
respect of any claim if information furnished at the time of proposal is found to be incorrect or
false or such claim is in any manner fraudulent or supported by any fraudulent means or device,
misrepresentation whether by the Insured Person or by any other person acting on his behalf.”
Insured’s policy details are as under:
P/700002/01/2017/068516 from 10/01/2017 to 09/01/2018
P/161130/01/2018/022901 from 06/03/2018 to 05/03/2019
P/161130/01/2019/053465 from 11/05/2019 to 10/05/2020
It is evident from the consultation report dt. 08/05/2019, the insured consulted for the present
diagnosis during the break period i.e. 06/03/2019 to 10/05/2019.
As per condition no. 7 of the policy,
“Any disease/illness contracted or injury sustained during the grace period will be deemed as pre
existing and will be subject to waiting period as stated under 3 iii.”
In view of above, the claim was repudiated and was communicated to the insured vide their letter
dated 24/06/2019.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (through video-conferencing) Complainant remained
absent. He did not pick up the phone when forum tried to contact him. RI reiterated their stand during
the hearing.
The representative of the RI contended that Complainant renewed the policy from Policy Bazar on
11/05/2019, after a gap of 66 days (previous policy P/161130/01/2018/022901 expired on
05/03/2019). During the break in insurance period the insured patient has consulted Dr. Sushma Patil
on 08/05/2019 and as per her advice pathological tests of Urine Analysis, Blood group, Blood sugar
Random and Haemogram was carried out from Bhakti Pathological Laboratory and this fact has not
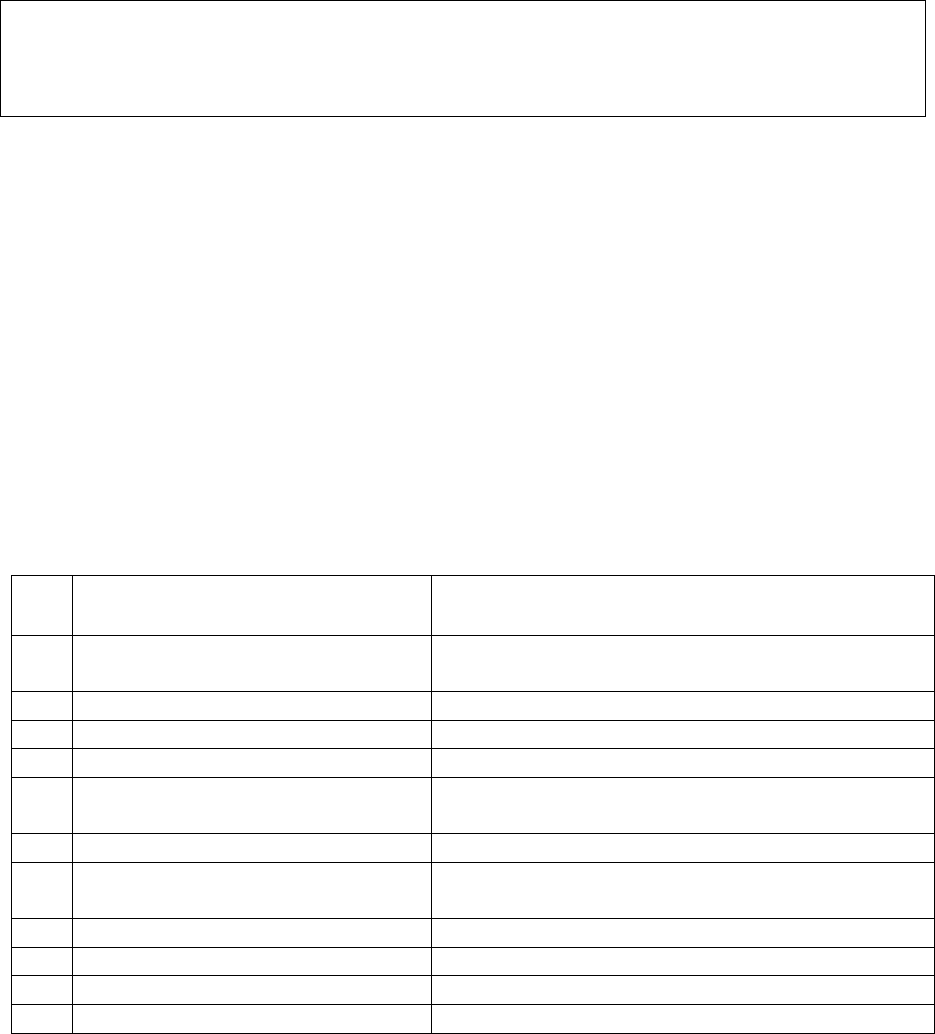
been disclosed during renewal. The complainant has stated in his complaint letter that sonography
was already done while the policy was running in 2
nd
year. But he has not submitted that report.
Instead he has obtained a couple of certificates from Dr. Sushama Patil dt. 23/01/2018 on the
letterhead of Aashay Hospital mentioning findings of USG. In one of these certificates, year is
overwritten to ‘18’. Incidentally, the date 23/01/2018 also falls in the gap between 1
st
and 2
nd
year
policy.
The treating Dr. Sushma Patil vide her letter dated 08/07/2019 has certified that at the time of
discharge all indoor case papers were handed over to the Insured patient. RI has contended that the
indoor case papers and cash paid bills/receipts were not made available to them by the hospital; which
further raises doubt.
Taking into account these observations, forum feels that the complainant has failed to establish the
genuineness of the claim and hence supports RI’s decision of repudiation.
Award follows:
AWARD
Taking into account of the facts and circumstances of the case and the submission made by
respondent insurer during the course of hearing, forum finds that the complaint lacks merit.
Hence, Dismissed.
Dated: On 15/9/2021 at Pune
VINAY SAH
Insurance Ombudsman, Pune.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr.Pankaj Manshi Faria V/S The National Insurance Co Ltd
COMPLAINT NO: PUN-H-048-2021-0629
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Pankaj Manshi Faria
Thane
2.
Policy No:
Type of Policy:
140900501810002103
National Mediclaim Policy
3.
Policy period:
20.07.2018 to 19.07.2019
4.
Sum Insured
Rs.500000
5.
Date of inception of first policy:
20.07.2015
6.
Name of the Insured:
Name of the Policyholder:
Mast. Akshay Pankaj Faria, 14 yrs
Mr. Pankaj Manshi Faria
7.
Name of the Insurer:
The National Insurance Co Ltd
8.
Reason for repudiation/Partial
Settlement:
Hospitalization for investigation purpose only
9.
Date of receipt of the Complaint:
13.01.2020
10.
Nature of complaint:
Settlement of full claim amount
11.
Amount of Claim:
Rs.37468/-
12.
Insurance Ombudsman Rule
Rule 13 1 (b)
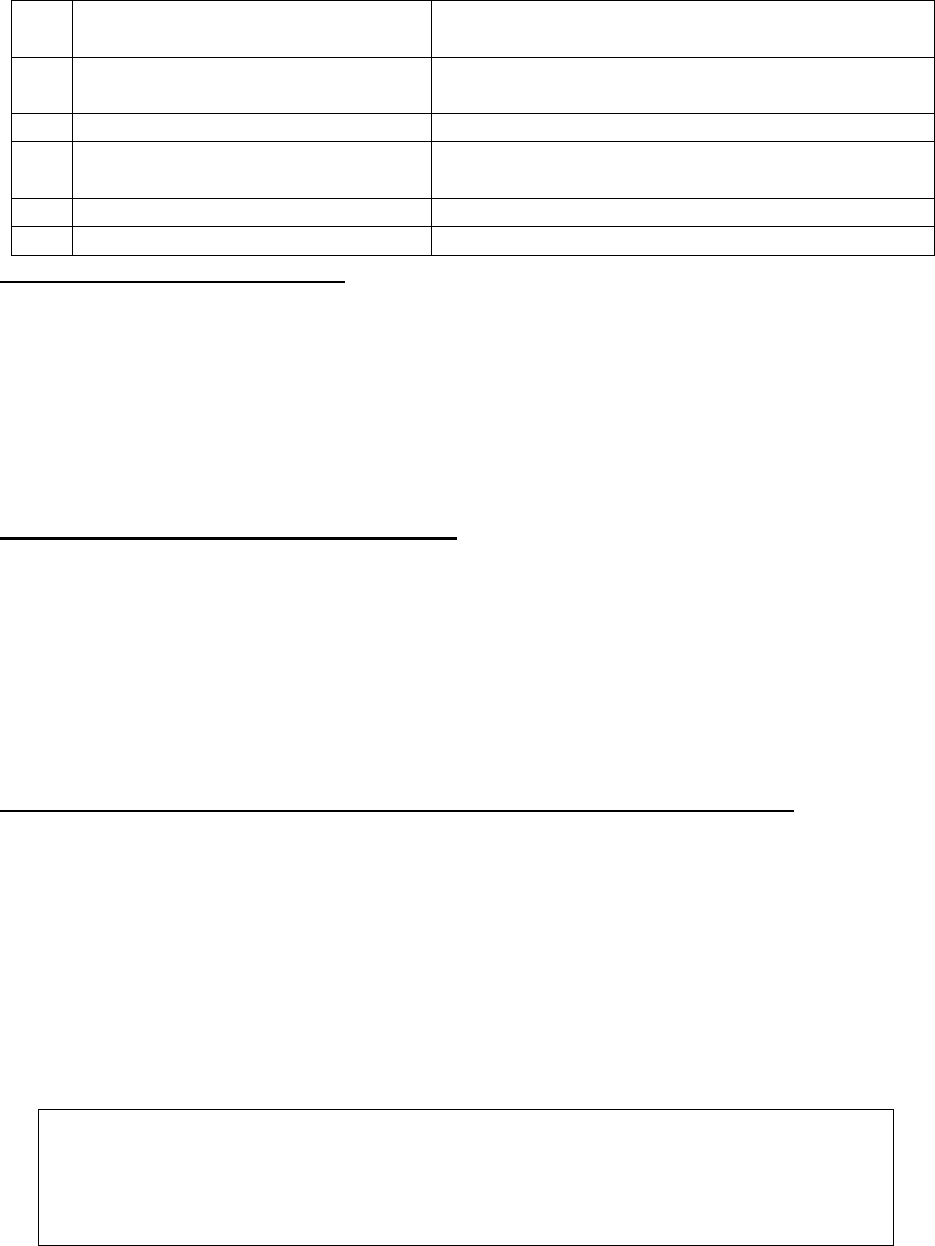
(IOR)2017 under which the
Complaint was registered:
13.
Date of hearing/Place:
Online hearing on 28.07.2021,
14.
Representation at the hearing
kkk) For the Complain-
ant:
Himself
lll) For the insurer:
Ms. Suchita More and Dr. Ketaki Tandel
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:-
The complainant has National Mediclaim policy with Respondent Insurer (RI) covering self and
family for sum assured 5 lakhs by renewing it regularly since inception ie.17.07.2017. He lodged a
claim of his son’s hospitalization in Jupitor Life line hospital Ltd from 08.05.2019 to 09.05.2019 for
DWARFISM. The total expenditure incurred on hospitalization was Rs.37468/-
The RI repudiated the claim stating from the available claim documents it was observed that the
treatment given to the insured patient does not support the need of hospitalization.
The complainant is requesting forum to intervene and resolve his grievance.
Contentions of the Respondent Insurer(RI):-
The insured patient consulted pediatric endocrinologist for poor height and weight. Consultant
advised clonidine stimulation test for evaluation. The patient admitted to Jupitor Hospital on
08.05.2019. Clonidine stimulation test was performed on the same day and discharged from hospital
on 09.05.2019. His Luteinizing Hormone was 0.04 and FSH was 0.23. MRI brain was normal in size
and shows no focal lesion. Clonidine Stimulation test (CST) is the most commonly used pro-active
test to rule out growth Hormone Deficiency. In view of the above it has been observed that need of
hospitalization is not justified. Hence the claim was rejected under policy clause 4.22 which states as
“Stay in hospital for domestic reason where no active regular treatment is given by specialist”.
Result of personal hearing with both the parties (Observations & Conclusion)
During the online hearing on 28.07.2021 both the parties reiterated their respective stand.
Forum replied on the findings appeared in the Discharge summary of Jupitor Hospital. The insured
patient was diagnosed with Short stature under evaluation admitted for Clonidine Stimulation
Test. The test was conducted to find out the root cause of patient’s short stature. No active line of
treatment and medicines has been prescribed by the treating consultant Dr Sudha Rao of Jupitor
Hospital.
In view of the above facts, forum finds the rejection of the claim is in order. The forum upholds the
decision of the Respondent Insurer and disallows the complaint.
Award follows:
AWARD
Taking into account of the facts and circumstances of the case and submissions
made by both the parties, the complaint is found to be devoid of merit. Hence
Dismissed.
Dated: On 21st day of September, 2020 Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– SHRI VINAY SAH
CASE OF Mr. Pankaj Sonawane v/s Star Health and Allied Insurance Company Ltd
COMPLAINT NO: PUN-H-044-2021-0043
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Pankaj Sonawane, Nasik
2.
Policy No:
Type of Policy:
P/151113/01/2019/027595
Family Health Optima Insurance Plan
3.
Policy period:
24/1/2019-23/1/2020
4.
Sum Insured
500000/-
5.
Date of inception of first policy:
24/1/2018
6.
Name and age of the Insured:
Name of the Policyholder:
Mr. Pankaj Sonawane; 38 years
Same as above
7.
Name of the Insurer:
Star Health and Allied Insurance Company Ltd
8.
Reason for repudiation/Partial
Settlement:
2 years waiting period
9.
Date of receipt of the Complaint:
11/6/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
33507/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
13 1(b )
13.
Date of hearing/Place:
On line hearing on 20.09.2021
14.
Representation at the hearing
mmm) For the Complain-
ant:
Himself
nnn) For the insurer:
Dr Anjali Rathod
15.
Complaint how disposed:
Dismissed
16.
Date of Award:
20.09.2021
Brief facts of the case:
The complainant has Family health Optima policy cover for his family (self, spouse, 2 sons) from
2018 for sum insured of Rs. 500000/- with Respondent Insurer (hereafter is called RI). He was
hospitalized from 23.12.2019 to 26.12.2019 for treatment of non healing ulcer on right leg. He
incurred an expense of Rs. 33,708/-. Reimbursement claim for the same is repudiated by RI. Hence
the complaint.
Contentions of the Complainant:
The complaint has stated in his complaint letter that he is diabetic and he had declared the same while
purchasing the policy. After the Company rejected his claim, he produced a certificate from the
operating doctor who stated that cause for ulcer is varicose veins and not DM. in fact his blood sugar
level and HB1AC were within normal limits. Still, RI did not approve his claim.
Aggrieved with the rejection of the claim he has filed complaint before this Forum for resolution.
Contentions of the Respondent:
The insured person took treatment at Samarpan Hospital during 23/12/2019 to 26/12/2019. As per
discharge summary, he was diagnosed as NON HEALING ULCER RIGHT LOWER 1/3
RD
OF LEG
and underwent EXICISION OF ULCER and DEFECT CLOSURE. Initially the claim was declined
as it was a complication of Pre existing disease which is not payable for 48 months of continuous
coverage as per waiting period clause.
The insured then submitted a request to reconsider the same along with treating doctor’s certificate
stating that the cause of above diagnosis was VARICOSE VEINS.
As per waiting period no. 3(ii) (a) the insurer is not liable to make any payment in respect of any
expense incurred in the treatment of the above mentioned disease during the first 24 months of
continuous coverage under the policy. Exclusion No. 3(ii) a reproduced below:
“A waiting period of 24 consecutive months of continuous coverage from the inception of this policy
will apply to the following specified ailments/illness/diseases: treatment of Cataract and diseases of
the anterior and posterior chamber of the Eye, diseases of ENT, Diseases related to Thyroid ,Prolapse
of Intervertebral Disc (other than caused by accident), Varicose veins and Varicose ulcers, Desmoid
Tumor, Umbilical Granuloma, Umbilical sinus, Umbilical Fistula, all Diseases of ‘Prostate, Stricture
Urethra, all Obstructive Uropathies, all types of Hernia, Benign Tumours of Epididymis,
Spermatocele, Varicocele, Hydrocele, fistula, Fissure in Ano, Hemorrhoids, Pilonidal Sinus and
Fistula, Rectal Prolapse, Stress Incontinence and Congenital Internal Disease /defect”
Thus the claim was repudiated and communicated to the insured vide letter dt. 06/05/2020.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 20.09.2021 (through video-conferencing) both the parties reiterated
their respective stand.
During the hearing Complainant defended that he is agreeable to the waiting period for diabetes which
is a declared disease. But this claim had arisen due to Vericose Veins and he has submitted a certificate
from Dr. Tushar Pawar to that effect.
RI representative submitted that treatment of Vericose Veins also carries a waiting period which is 24
months.
Forum has perused the policy terms in respect of waiting period and found that the contention of RI
is correct. The clause no 3(ii) mentioned above specifically excludes claim arising out of varicose
veins for two years waiting period. As the claim has arisen in the 2
nd
year of the policy, the waiting
period applies and hence, Forum is unable to consider the claim in favour of complainant.
Complaint dismissed.
Award follows;
AWARD
Under the facts and circumstances, it is found that the decision of repudiation of claim needs
no intervention. Complaint therefore stands dismissed.
Dated: at Pune, on this 20
th
day of September, 2020.
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– SHRI VINAY SAH
CASE OF Mr. Prafulla R. Wani v/s Star Health and Allied Insurance Company Ltd
COMPLAINT NO: PUN-H-044-2021-0046
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Prafulla Raman Wani, Nasik
2.
Policy No:
Type of Policy:
P/15112/01/2019/014364
Senior Citizens Red Carpet Health Insurance Policy
3.
Policy period:
30/3/2019-29/3/2020
4.
Sum Insured
400000/-
5.
Date of inception of first policy:
30/3/2012
6.
Name and age of the insured:
Name of the Policyholder:
Asha Raman Wani; mother, 70 years
Mr. Prafull Wani
7.
Name of the Insurer:
Star Health and Allied Insurance Company Ltd
8.
Reason for repudiation/Partial
Settlement:
Waiting period for increased Sum Insured
9.
Date of receipt of the Complaint:
11/6/2020
10.
Nature of complaint:
Partial settlement of claim
11.
Amount of Claim:
64175/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
13 1( b)
13.
Date of hearing/Place:
On line hearing on 20.09.2021
14.
Representation at the hearing
ooo) For the Complain-
ant:
Himself
ppp) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Dismissed
16.
Date of Award:
21.09.2021
Brief facts of the case:
The complainant is the son of policyholder who has taken Senior Citizens Red Carpet Health
insurance Policy with Respondent Insurer (hereinafter is called RI) for his mother from 30/3/2012.
Sum Insured under the policy is 4,00,000/-. The complainant has lodged claim of his mother’s
hospitalization in Optimus hospital from 11.12.2019 to 15.12.2019 for B/L OA Knee. The total claim
amount was Rs.364911/- company has settled the claim for Rs. 150000/- only.
Contentions of the Complainant:
Complainant has raised objections to various deductions made by the RI while settling the claim. He
also has grievance about inordinate delay (52 days) in settlement of claim. He is arguing that how the
sub limit of Rs. 1,50,000/- is applied in his claim when it is not mentioned anywhere in the policy.
He contends that as per bill assessment sheet, Rs. 3,05,965/- is admissible amount. (i.e. Rs. 3,02,374/-
hospitalisation exp + Rs. 2,324/- + Rs. 1,267/- pre & post hospitalisation expenses) and after
deducting 30% co pay, net amount payable comes to Rs. 2,14,175/- which is within the sub limit as
per the table. As there is no mention of specific ‘Osteoarthritis’ in policy document, the sub limit
prescribed for ‘Treatment of long bones’ applies in this claim. Which is Rs. 2,25,000/- for the SI of
Rs. 4,00,000/-
He has requested the forum to do justice in his favor and direct the company to settle his claim for an
amount of Rs. 2,14,175/-.
Contentions of the Respondent Insurer:
Mr. Prafulla Raman Wani availed Senior citizen policy covering his mother (Mrs. Asha Wani) for the
sum insured of Rs. 100000/-vide policy no. P/15121/01/2012/00374 for the period from 30/3/2012 to
29/3/2013 and the same was renewed as follow:
P/151121/01/2013/004132
30/3/2013-29/3/2014
RS.100000.00
P/151121/01/2014/004455
30/3/2014-29/3/2015
100000.00
P/151121/01/2015/005369
30/3/2015-29/3/2016
100000.00
P/151121/01/2016/006029
30/3/2016-29/3/2017
200000.00
P/151121/01/2017/008236
30/3/2017-29/3/2018
300000.00
P/151121/01/2018/010279
30/3/2018-29/3/2019
400000.00
P/151121/01/2019/014364
30/3/2019-29/3/2020
400000.00
The Insured reported the claim in the 9
th
year of the policy from commencement and 2
nd
year of the
enhanced sum insured of Rs.400000/-
As per Discharge summary, the Diagnosis was Bilateral Severe Knee Osteoarthritis and underwent
Bilateral Biomet vanguard Total Knee replacement. Documents for reimbursement of medical
expenses were submitted on 23/12/2019.
As per waiting period 3(ii) C of the policy, ‘A waiting period of 24 consecutive months of
continuous coverage from the inception of this policy will apply to the following specified ailments
/illness/diseases: All treatments (Conservative, Operative treatment) and all type of intervention for
diseases related to Tendon, Ligament, Fascia, Bones and Joint including Arthroscopy and
Arthroplasty/ Joint Replacement (other than caused by accident)”
As per condition no. 8 of the policy, “Revision of Sum Insured”
Where the sum insured is enhanced, the amount of such additional sum insured including the
respective sub limit by way of such enhancement shall be subject to the following terms:
A waiting period as under shall apply afresh from the date of such enhancement for the increase in
the sum insured, that is the difference in sum insured between the previous sum insured and the
increased sum insured
ii) 24 months with continuous coverage without break (with grace period) in respect of
diseases/treatment falling under waiting period 3 (ii).
Taking into consideration both the above clauses, applicable SI is Rs. 3,00,000/- in this case. Further,
as per coverage clause I of the policy, “The expenses payable during the entire policy period in respect
of All other major surgeries for the sum insured of Rs. 3,00,000/- is limited to Rs. 1,50,000/-”.
Hence, claim is settled for Rs. 1,50,000/- on 11/02/2020 vide NEFT.
Result of personal hearing with both the parties (Observations & Conclusions):
A personal hearing was arranged on 20.09.2021 (through video-conferencing). The complainant
argued that at the time of hospitalisation, SI was 4,00,000/-. Policy is from 2012, this disease is not
pre existing. As such, capping is not applicable here. He also reiterated his complaint about 52 days
delay in settling the claim. RI maintained their stand regarding the amount settled.
On going through the contentions of both the parties and the policy clauses, forum notes that;
The Insured while renewing the policy for the period 30/3/2018-29/3/2019 enhanced the sum insured
from Rs. 300000/- to Rs. 400000/-. Even though the waiting periods are completed for the basic sum
insured of Rs. 100000/- the same are applicable to the Enhanced sum insured of Rs. 400000/-. Hence,
as per the Exclusion No.3 (ii) C, the sum insured available for this claim is Rs. 300000/-only and the
enhancement of Rs. 400000/- is not payable during the first two years of continuous operation of this
Senior Citizen red carpet Health Insurance policy. Further, there is sub limit for certain treatments. In
this case, operation being ‘knee replacement’, sub limit under the heading ‘All other major
surgeries’ is applicable, which is Rs. 1,50,000/- for SI of Rs. 3,00,000/- and not under the heading
‘ Cerebro vascular …….. Treatment of long bones’ which is Rs. 2,25,000/-.
The settlement done by RI is thus found correct according to the T&C of the policy. Hence, forum
cannot consider payment of the balance claim amount. However, as the complainant has rightly
complained, delay in settlement is found at RI’s end. The claim documents were submitted on
23/12/2019 and the claim was settled on 11/02/2020. RI to take note of the same and see to it that the
claims are settled within ‘TAT’ so as not to cause hardship to the policyholders.
Award follows:
AWARD
Under the facts and circumstances, the complaint is found devoid of merits therefore stands
dismissed.
Dated: Pune, on this 29
th
day of September, 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Pranit Pansare Vs. Liberty General Insurance Limited
COMPLAINT NO: PUN-H-028-1920-0537
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. Pranit Pansare
Flat B-304, Sadguru Darshan, SN-16/1,
Ambegaon Bk, Haveli, Pune – 411046
2.
Policy No:
Type of Policy:
4213-200101-17-7000646-00-000
Liberty Hospi-Cash Connect Policy
3.
Policy period:
30/01/2018 to 29/01/2020 (2 year policy)
4.
Sum Insured/IDV
Rs.10 lakhs
5.
Date of inception of first policy:
30/01/2018
6.
Name & age of the Insured:
Name of the Policyholder:
Mr. Pranit Pansare – Age: 31 years
Same as above
7.
Name of the Insurer:
Liberty General Insurance Limited
8.
Reason for rejection /Partial Settlement:
Beyond free look period
9.
Date of receipt of the Complaint:
14/11/2019
10.
Nature of complaint:
Mis-sale of health product
11.
Amount of Claim:
Rs.38,764/- (incl. GST)
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021; (Online)
14.
Representation at the hearing
qqq) For the Complainant:
Himself
rrr) For the insurer:
Ms. Shraddha Kinare
15.
Complaint how disposed:
Dismissed
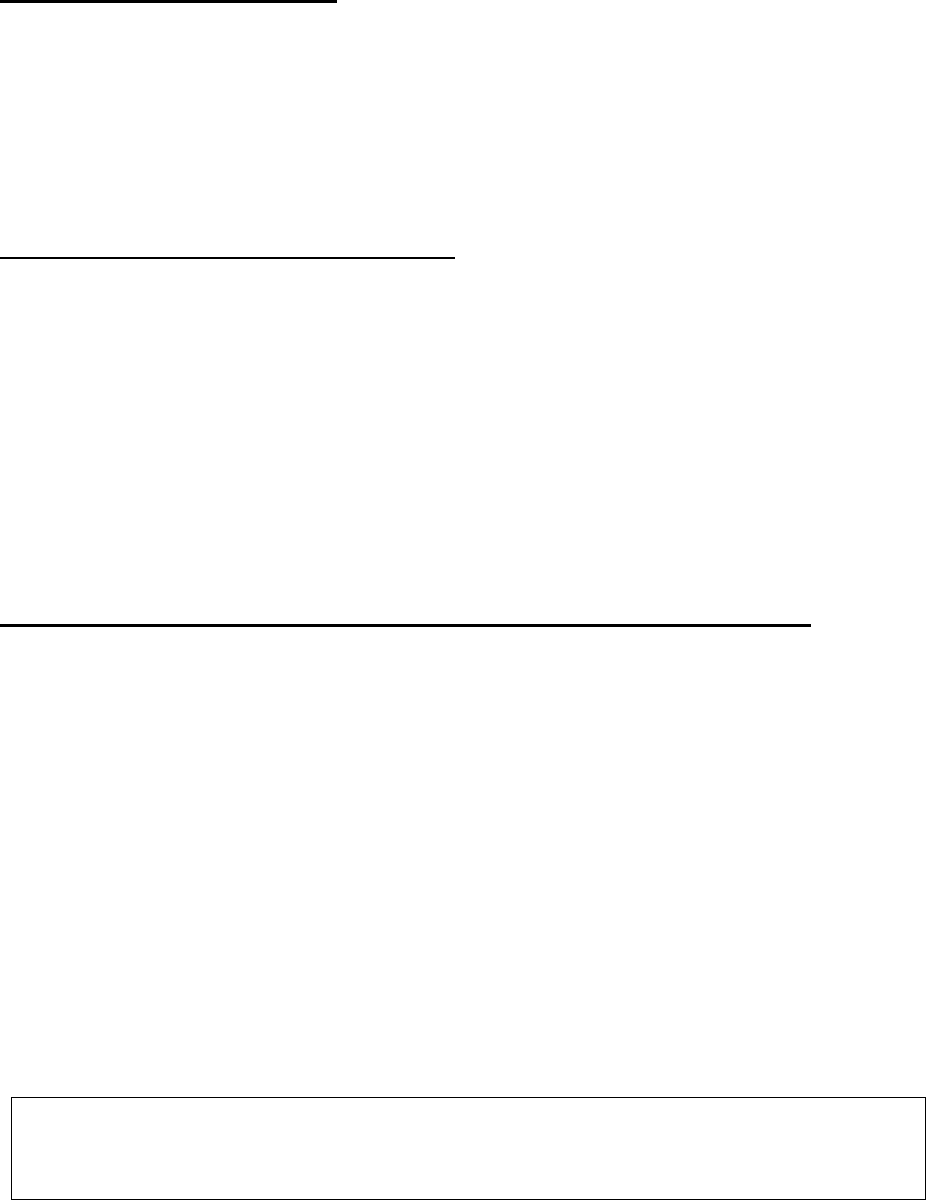
Contentions of the Complainant:
Complainant was holding a policy with the Respondent Insurer (RI) for SI 10 lakhs for two years
period 30/01/2018 to 29/01/2020.
The policyholder has lodged complaint with the Ombudsman forum about the mis-sale of health
policy by the RI through M/s GVR Insurance Brokers Private Ltd. The complainant has in his
complaint letter dated 21/08/2019 alleged that the intermediaries sold him the subject health policy
assuring him that the amount lying with the other insurer shall be returned to him. On realizing fraud,
despite request for cancelling the policy, the RI has denied the refund.
Contentions of the Respondent Insurer (RI):
The RI has stated that the complainant was sold the health policy based on the signed proposal form
received through the broker. The subject policy is effective from 30/01/2018 to 29/01/2020 (2 years
policy) to cover the medical expenses which would be incurred by the complainant. The RI has CD
recording of the verification call between the complainant and the broker wherein he was explained
about the product and that he had understood the terms and conditions of the product.
The RI has also stated that the complainant had not approached to cancel the policy within the free
look period or anytime during the policy period earlier. No grievance apart from a request to correct
the name in the policy has been received. They had received the cancellation request letter dated only
on 21/08/2019 i.e. after 19 months of the tenure of the policy and as per their cancellation table, no
amount was due to him. As per the cancellation table, for the cancellation period 19 months to 24
months, for a two year policy, no refund of premium can be made.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (Online), both the parties reiterated their respective stand.
From the available documents, forum notes that:
The complainant was sold the Health Policy through the broker after obtaining the duly filled and
signed proposal form from the complainant along with necessary premium for a 2 years policy ending
29/01/2020. The complainant has sent his request for cancellation vide his letter dated 21/08/2019 to
the RI but they have replied that he was not eligible for any refund as per policy terms and conditions.
On the basis of call recordings, they could prove their stand that the policy was genuinely issued after
the verification call.
In counter argument to the contentions of the RI, complainant has not produced any documents/call
recordings or any legal action taken by him against the defaulters for the alleged mis-sale by
allurements.
In absence of any such proof, it is difficult to hold the RI responsible for the alleged mis-sale.
Complaint therefore is not sustainable.
Award follows:
AWARD
Under the facts and circumstances of the case, forum finds that the complaint is devoid of
merits, hence dismissed.
Dated: at Pune this 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
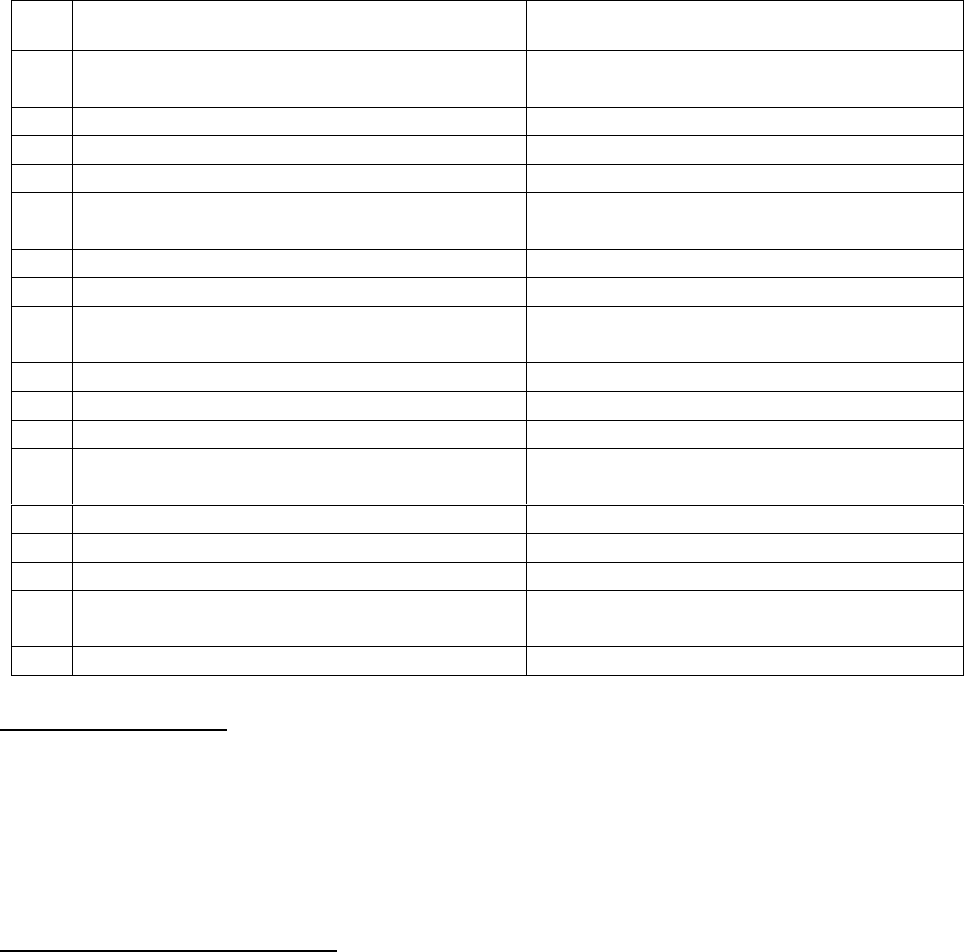
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– SHRI VINAY SAH
CASE OF Mr. Rajesh Waghmare v/s National Insurance Company Ltd
COMPLAINT NO: PUN-H-048-1920-0733
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the Complainant
Rajesh Waghmare, Pune
2.
Policy No:
Type of Policy:
270100/50/18/10004608
Baroda Health Policy
3.
Policy period:
30/8/2018-29/8/2019
4.
Sum Insured
250000/- floater SI
5.
Date of inception of first policy:
Aug 13
6.
Name and age of the insured:
Name of the Policyholder:
Sheetal Waghmare; 31 years; wife
Rajesh-himself
7.
Name & Age of the Insured
Mrs. Sheetal Waghmare, wife, 31yrs.
7.
Name of the Insurer:
National Insurance Company Ltd
8.
Reason for repudiation/Partial Settlement:
OPD based treatment, hospitalization not
required.
9.
Date of receipt of the Complaint:
02/03/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
28288/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
13 1(b)
13.
Date of hearing/Place:
23/08/2021; Online
14.
Representation at the hearing
sss) For the Complainant:
Himself
ttt) For the insurer:
Ms. Rimpi Kapoor;
TPA Dr. Sameer Shelke
15.
Complaint how disposed:
Partially allowed
Brief facts of the case:
The complainant is the bank account holder of the Bank of Baroda and enrolled his name in Baroda
Health policy from March 2014. He has submitted claim for his wife, Mrs. Sheetal for Lumbosacral
Sprain for one day admission from 23/7/2019 to 24/7/2019.
However, RI has rejected the claim stating that procedure carried during the hospitalization was for
Nerve root Block, which does not need hospitalization and which could have been managed on OPD
basis.
Contentions of the Complainant:
Complainant has contended that, his wife started back pain in the last week of May 19. He visited his
family physician Dr. Gharge who prescribed medication for it but she did not get any relief from the
pain.
Then he consulted Orthopedic Dr. Sachin Abane, as per advice of the family physician. Doctor called
for x ray report and prescribed oral medications, gel and physiotherapy which she tried till 17/7/2019
in spite of the same she didn’t get any relief.
She was having Severe Low Back Pain and continuous Numbness and Tingling in her leg because of
which she could not Stand and Sit or do anything for more than 5 minutes. Then Dr. Abane decided
to go for MRI which they did on 20/7/2019 which shows slip disc and pressure on the nerve which
was causing back pain and leg pain and numbness and tingling.
On the basis of the MRI report Dr. Abane advised that Nerve Root Block is the final option to give
her relief from severe low back pain and Numbness and Tingling. Based on his advice, complainant
consulted Spine Expert Dr. Sachin Patil for which she was admitted and kept under observation from
23/7/2019 to 24/7/2019 in Dr. Abane Hospital. After that treatment she got relief from low back pain.
However, she was having pain in her leg for which he consulted Dr. Raman and he gave medication
for it.
Nerve Root block is a special procedure which is given only by Spine Expert Surgeon and in
specialized Operation Theater only. Complainant argues that nowhere it is written on the policy
regarding deletion of the Nerve Root Block expenses.
Complainant requested the Forum through this complaint to look into the matter and resolve this issue.
Contentions of the Respondent Insurer (RI):
On 23.7.2019, insured Mrs. Shhetal Waghmare was admitted in Abane Hospital with complaint of
pain and numbness to right lower limb. As per discharge card, course in the hospital is shown as
“XYCOCAINE SENSITIVITY TEST”
As per Mediassist TPA, the claim was not admissible under the clause ‘Hospitalization was not
justified’.
RI took Medical opinion of Dr. Samir Shelke. As per his opinion, patient was admitted only for
administration of intra articular injection. Net search report submitted by the RI and concluded that
treatment can be taken on OPD basis for which hospitalization is not required for this type of
treatment i.e intra articular injection. This type of treatment can easily be administered on OPD basis.
Their policy covers only such treatments where the hospitalization of the patient is inevitable for
further management of his/her ailment, as an inpatient only. In view of the above claim has been
repudiated as per policy clause 4.13 which read as follow:
‘Hospitalization for the purpose of the diagnosis and evaluation, irrelevant investigation charges, all
expenses incurred at hospital primarily for diagnostic, X-ray or Laboratory examinations or other
diagnostic studies not consistent with or incidental to the diagnosis and treatment of positive existence
or presence of any ailment, sickness or injury, for which confinement is required at a hospital.’
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 23/08/2021 (through video-conferencing), both the parties reiterated
their respective stand.
Upon hearing the contentions of both the parties and documents submitted on record, forum has
following observations.
There is no dispute that the procedure of lumbar nerve root injection was performed on the insured
patient. From the web search of this procedure, forum has following findings.
‘A lumbar nerve root injection is a procedure to inject medicines at the nerve roots of your lumbar
(lower back) spine. This procedure is done to decrease inflammation and pain.
After your procedure:
You will be taken to a recovery room to rest. Healthcare providers will watch you closely for any
problems. Do not get out of bed until your healthcare provider says it is okay. When healthcare
providers see that you are okay, you may be able to go home.
• Bandages will cover the procedure area. The bandages keep the area clean and dry to prevent infec-
tion. A healthcare provider may remove the bandages soon after your procedure to check the injection
sites.
• Medicines may be given to treat pain, swelling, or fever, or to prevent an infection.
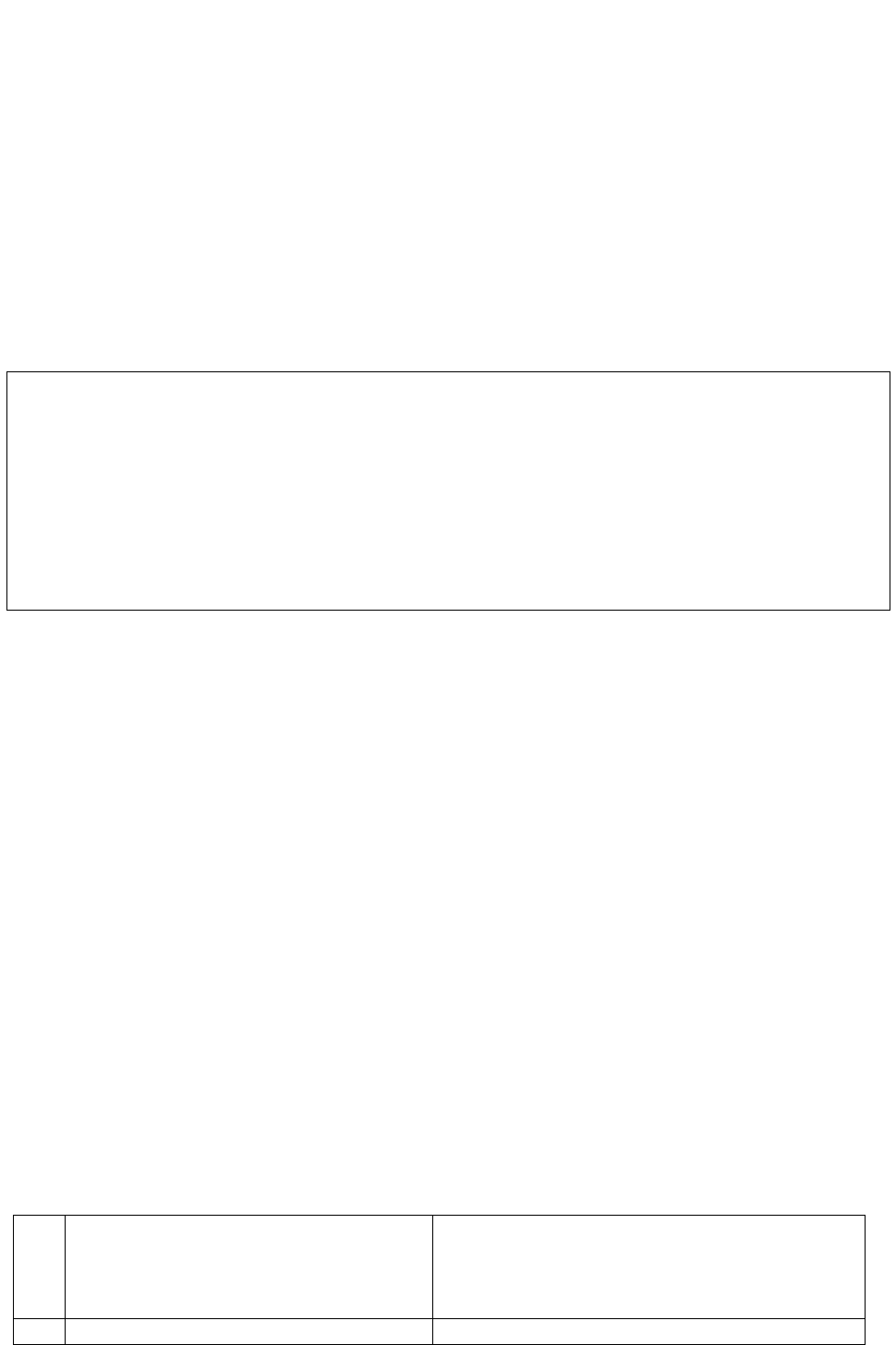
RISKS:
You may get an infection or have bleeding. Other parts near your spine, such as nerves, blood vessels,
ligaments, muscles, and bones, may be damaged. The medicines may spread in areas near the lum-
bar nerve root and cause numbness in these areas. You may still have leg or lower back pain.’
This implies that the injection is required to be taken under medical supervision. Even though, it does
not need 24 hours hospitalization, definitely it is a day care treatment. In view of this, forum browsed
the policy terms and found in clause no.3.13 (ii) the expenses in such treatments for which involves
specialized infrastructural facilities available in the hospitals and due to technological advances
hospitalization is required for less than 24 hours only, are covered under the policy. In view of this,
RI is instructed to pay only injection and medicines charges incurred on the day of hospitalization
under day care by deleting hospital stay expenses.
Complaint allowed partially.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to pay to
the complainant only injection and medicines charges incurred on the day of
hospitalization by treating the claim under day care treatment by deleting hospital stay
expenses towards the full and final settlement of this complaint.
The award is to be complied with one month from the date of receipt of this award failing
which it will attract interest at the applicable bank rate plus 2% extra from the date of
rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurers.
Dated: this, on 16
th
day of September 2021, at Pune
VINAY SAH
Insurance Ombudsman,
Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN – VINAY SAH
CASE OF Mr. Ramesh Pokharnikar Vs. Star Health & Allied Insurance Company Ltd.
COMPLAINT NO: PUN-H-044-1920-0549
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. Ramesh Pokharnikar
Saraswati Krupa CHS, Bldg. No.B4, Flat
No.7,
Tadiwala Road, B/H Kumar Pinnacle, Pune-1
2.
Policy No:
P/151112/01/2019/022220
Type of Policy:
Family Health Optima Insurance Plan
3.
Policy period:
18/02/2019 to 17/02/2020
4.
Sum Insured/IDV
Rs.15 lakhs (floater)
5.
Date of inception of first policy:
27/10/2017
6.
Name & age of the Insured:
Name of the Policyholder:
Mrs. Ratnamala Pokharnikar; wife – Age: 61
Mr. Ramesh Pokharnikar
7.
Name of the Insurer:
Star Health & Allied Insurance Company Ltd.
8.
Reason for rejection /Partial
Settlement:
Disease contracted during break in policy
9.
Date of receipt of the Complaint:
06/12/2019
10.
Nature of complaint:
Rejection of health claim
11.
Amount of Claim:
Rs. 3,15,114/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021; (Online)
14.
Representation at the hearing
uuu) For the Complainant:
Himself
vvv) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Disallowed
Brief facts of the case:
Complainant and his family were insured with the Respondent Insurer (RI) under the above policy
for the period 18/02/2019 to 17/02/2020. The insured patient aged 61 years was hospitalized at R.M.
Dhariwal Hospital, Pune on 07/04/2019 for treatment of coronary artery disease (CAD). Complainant
has paid the bill of Rs. 3,15,114/- to the treating hospital. The RI has rejected the hospitalization claim
on the grounds that the amount is not payable in view of the renewal of the policy being done after a
lapse of 114 days and that the stress test done in the interim period was found positive which was not
disclosed while renewing the policy.
The complainant has approached the Grievance Cell of the RI vide his letter dated 11/09/2019 but the
request for reconsideration of the rejected claim was also rejected by the RI. Aggrieved with this
decision, the complainant has approached the forum for the claim amount and resolution of his
grievance.
Contentions of the Complainant:
Complainant submits that the RI rejected the claim on the grounds that the stress test done on
15/2/2019 was positive which falls during the break period. That, according to his doctor, even if a
person’s stress test is positive, from that, one cannot jump to a conclusion that the person has a heart
disease. A person’s stress test may be positive due to some other reason also. His wife had an acidity
problem. Their doctor advised her to go for a stress test which was done on 15/02/2019. After that
doctor suggested her to take some medicines to reduce the problem of acidity. But even after taking
these medicines her acidity problem increased. Then ultimately, doctor asked her to go for
angiography. Finally, she underwent angiography on 1/4/2019, i.e. after 45 days from the date of her
stress test on 15/02/2019.
That in the light of above mentioned circumstances, his wife did not find it necessary to disclose the
above fact in the ‘good health declaration’ at the time of renewal of policy.
Further, at the time of renewal, his wife had already crossed the age of 61 years. The Insurance
Company ought to have got her medical check-up done through their panel of doctors. But this was
not done probably because they just wanted to grab an opportunity to increase their business. It just
amounts to professional negligence on the part of said Insurance Company.
Contentions of the Respondent Insurer (RI):
The RI has stated that the above policy was renewed after a break period of 3 months and 22 days i.e.
from 27/10/2018 to 17/02/2019.
It is observed from the indoor case records dated 01/04/2019 of Jahangir Hospital that the stress test
done on 15/2/2019 is positive which falls during the break in policy period. Based on this finding, the
RI has summarized that the insured patient was diagnosed to have heart disease during the break in
policy and the same was not disclosed on the good health declaration at the time of renewal of the
policy.
Hence, the claim was denied as per Condition No.7 of the policy condition, which is reproduced
hereunder:
Condition No.7– “the Company is not liable to protect the Insured person for disease contracted
between the policy expiry date and the date of payment of premium for renewal.”
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (Online) both the parties reiterated their respective stand.
From the available documents, forum notes that:
From the facts and the documents submitted on record, it is revealed that the insured patient’s stress
test done on 15/02/2019 was found positive. On this date there was no insurance cover as the policy
was not renewed. Contrary to the contention of the complainant, it had no relation with acidity
because even after taking medicines for acidity, her problem increased and hence, angiography was
suggested. The same was done on 01/04/2019. This clearly indicates that the positive stress test was
due to underlying heart ailment only. That there was a gap of 45 days between the stress test and
angiography is of no significance.
Also, his allegations of not conducting medical test for renewing policy, does not hold water; as the
policies are issued basis set underwriting practices of Insurance Companies. Moreover, that does not
absolve the insureds from their duty to disclose all material aspects regarding their health.
In view of this, as stated in the policy clause mentioned above, disease contracted between the policy
expiry date and the date of payment of premium for renewal, is not admissible.
Forum is unable to admit this complaint.
Award follows:
AWARD
Under the facts and circumstances of the case, forum finds that the complaint is devoid of
merits. Complaint therefore stands dismissed.
Dated: at Pune this 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN – VINAY SAH
CASE OF Mr. Ramesh Pokharnikar Vs. Star Health & Allied Insurance Company Ltd.
COMPLAINT NO: PUN-H-044-1920-0550
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mr. Ramesh Pokharnikar
Tadiwala Road, Pune-1
2.
Policy No:
Type of Policy:
P/151112/01/2019/022220
Family Health Optima Insurance Plan
3.
Policy period:
18/02/2019 to 17/02/2020
4.
Sum Insured/IDV
Rs.15 lakhs (floater)
5.
Date of inception of first policy:
27/10/2017
6.
Name & age of the Insured:
Name of the Policyholder:
Mr. Pratik Pokharnikar – Age: 22
Mr. Ramesh Pokharnikar
7.
Name of the Insurer:
Star Health & Allied Insurance Co. Ltd.
8.
Reason for rejection /Partial Settlement:
Congenital disease not payable.
9.
Date of receipt of the Complaint:
06/12/2019
10.
Nature of complaint:
Rejection of health claim
11.
Amount of Claim:
Rs.46,841/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021; (Online)
14.
Representation at the hearing
www) For the Complainant:
Himself
xxx) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Dismissed
Brief facts of the case:
Complainant and his family were insured with the Respondent Insurer (RI) under the above policy
for the period 18/02/2019 to 17/02/2020. Son of the complainant, aged 22 years underwent 6
th
toe
excision in Yogesh Hospital, Pune in June 2019. Respondent company repudiated his claim as per
‘Exclusion No.3’. Hence the complaint.
Contentions of the Complainant:
Complainant contends that while processing his above Mediclaim, the said company has not perused
the case papers of treatment of his son carefully and thoroughly. In the column ‘clinical features’ it is
clearly mentioned, ‘pain on wearing footwear’ and ‘strain while running’. The company has
deliberately overlooked/ignored the column ‘clinical features’ and wrongly and illegally repudiated
his mediclaim. He further contends that his Mediclaim is quite an exception to ‘Exclusion No. 3’
Contentions of the Respondent Insurer (RI):
RI has submitted that the insured person was diagnosed with POLYDACTYLY underwent excision
of the 6
th
toe in left foot which is a CONGENITAL EXTERNAL CONDITION. Hence, the claim was
repudiated vide letter dated 29/07/2019 stating that the same was not liable to be paid as per Exclusion
No.3 of the policy.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (Online) both the parties reiterated their respective stand.
From the available documents, forum notes that:
1. The insured patient was admitted to the hospital on 28/06/2019 for undergoing the treatment of
6
th
toe excision on his left foot and after the procedure was discharged on 29/06/2019;
2. The RI has repudiated the claim on the grounds that as per Exclusion No.3 of the policy, any
treatment incurred towards external congenital disease is not payable;
3. The complainant has contended that the case papers state ‘Pain on wearing footwear’ and ‘Strain
while running’. The insured patient is a cricketer and while playing cricket, he was under pain
due to the 6
th
toe and in order to safeguard his cricketing career, they had to do the excision to his
6
th
toe on his left foot.
In view of this, forum tried to seek the feasibility of payment of claim in case of medical expenses
required to be incurred for the difficulty/ pains suffered by the insured person due to congenital
anomaly. For this, forum reviewed the exclusion clause in detail, stated below:
4. EXCLUSIONS:
The Company shall not be liable to make any payments under this policy in respect of any expense
whatsoever incurred by the Insured Person in connection with or in respect of:
3. the Company is not liable to make any payment in respect of any expenses incurred by the
insured person for treatment of congenital external condition / defects / anomalies.
It is thus observed from the above exclusion that ‘any expenses whatsoever’ means all the expenses
in respect of excluded conditions are excluded from the policy cover. Hence, the expenses incurred
due to difficulty or pain also cannot be covered under the said policy. Forum, therefore is unable to
consider the complaint in his favour. Complaint is thus disallowed.
Award follows:
AWARD
Under the facts and circumstances of the case, forum finds that the complaint is not
tenable. Complaint therefore stands dismissed.
Dated: at Pune this 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– SHRI VINAY SAH
CASE OF Mr. Ravi Rajaram Modak v/s National Insurance Company Ltd
COMPLAINT NO: PUN-H-048-2021-0072
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Ravi Rajaram Modak,
Thane
2.
Policy No:
Type of Policy:
240100201810005292
Pariwar Mediclaim
3.
Policy period:
23/8/2018-22/8/2019
4.
Sum Insured
200000/-
5.
Date of inception of first policy:
23/8/2018
6.
Name and age of the Insured:
Name of the Policyholder:
Ravi Rajaram Modak; 46 years
Same as above
7.
Name of the Insurer:
National Insurance Company Ltd
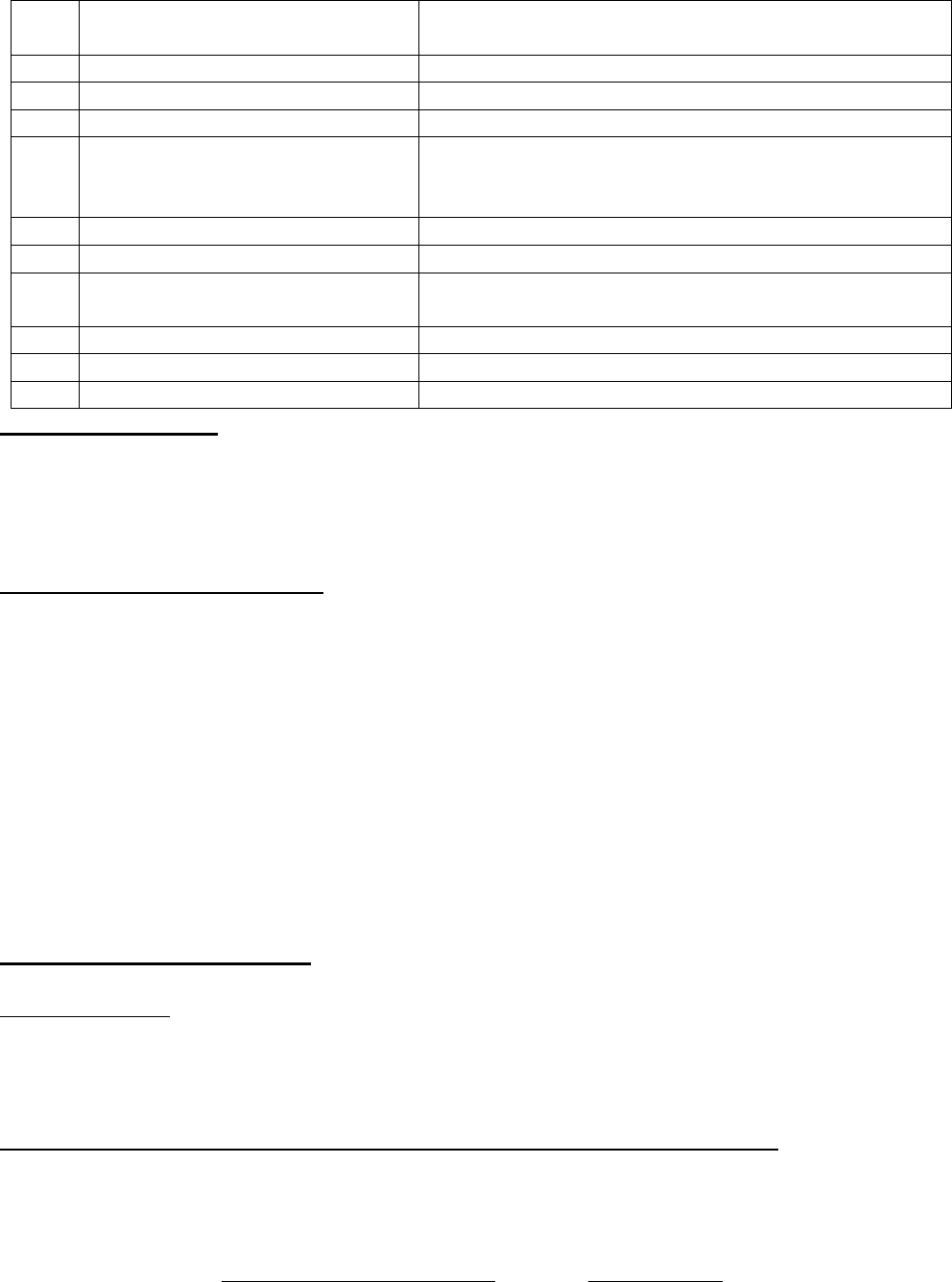
8.
Reason for repudiation/Partial
Settlement:
2 yrs waiting period applicable
9.
Date of receipt of the Complaint:
27/7/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
33749/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
13 1( b)
13.
Date of hearing/Place:
Online hearing on 22.09.2021
14.
Representation at the hearing
yyy) For the Complain-
ant:
Absent
zzz) For the insurer:
Mrs. Suman Kulkarni
15.
Complaint how disposed:
Dismissed
16.
Date of award:
30.09.2021
Brief facts of the case:
The complainant is having family floater policy for himself, his spouse and his daughter for sum
insured of Rs.200000/- with Respondent Insurer (hereinafter is called RI) from 2018.
He lodged a claim for his hospitalisation from 2/8/2019 to 7/8/2019 for ‘Burning Micturition with
Hematuria with Feverish feeling.’ RI has rejected the claim stating that this is 1
st
year of policy and
there is waiting period of 2 years for prostatomegaly with DM hence rejected the claim.
Contentions of the Complainant:
In the grievance letter sent to the RI, he contends that, his claim was denied on account of
Prostatomegaly. In this connection, symptoms of prostate problems are as under;
Frequent urge to urinate
Need to get up many times during the night to urinate
Blood in urine or semen
Pain or burning urination
Painful ejaculation
Frequent pain or stiffness in lower back, hips, pelvic or rectal area or upper thighs.
Dribbling of urine.
He submits that none of the above symptoms were there at the time of admission. Hospital has not
treated for prostate. The same can be verified with the medical documents lodged. Further, it was
diagnosed as “MILD PROSTATOMEGALY”.
Contentions of the Respondent:
As per Rejection letter dated 26.09.2019;
Rejection Reason: “Conservative treatment given for Enteric fever with mild Prostatomegaly with
DM, after scrutiny of documents found that policy is in 1
st
year and for prostatomegaly, waiting period
is 2 years. Hence, claim is recommended for rejection under the clause 4.3.”
Clause No. 4.3. The said disease/illness is specifically excluded under the first two years waiting
period.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 22.09.2021 (through video conferencing), both the parties reiterated
their respective stand.
Although the complainant has contended in the letter written to grievance that he had none of the
symptoms of prostate problem, his discharge summery mentions complaints on admission as
‘ADMITTED WITH BURNING MICTURITION WITH HEMATURIA WITH FEVERISH
FEELING’. And diagnosis was ‘RESISTENT ENTERIC FEVER WITH MILD
PROSTATOMEGALY WITH DM (N/D).
As per expert opinion taken by RI, the enteric fever in this case is extremely mild as noticed from
temperature 96.8 at the time of admission in the nursing home. It hence does not require admission
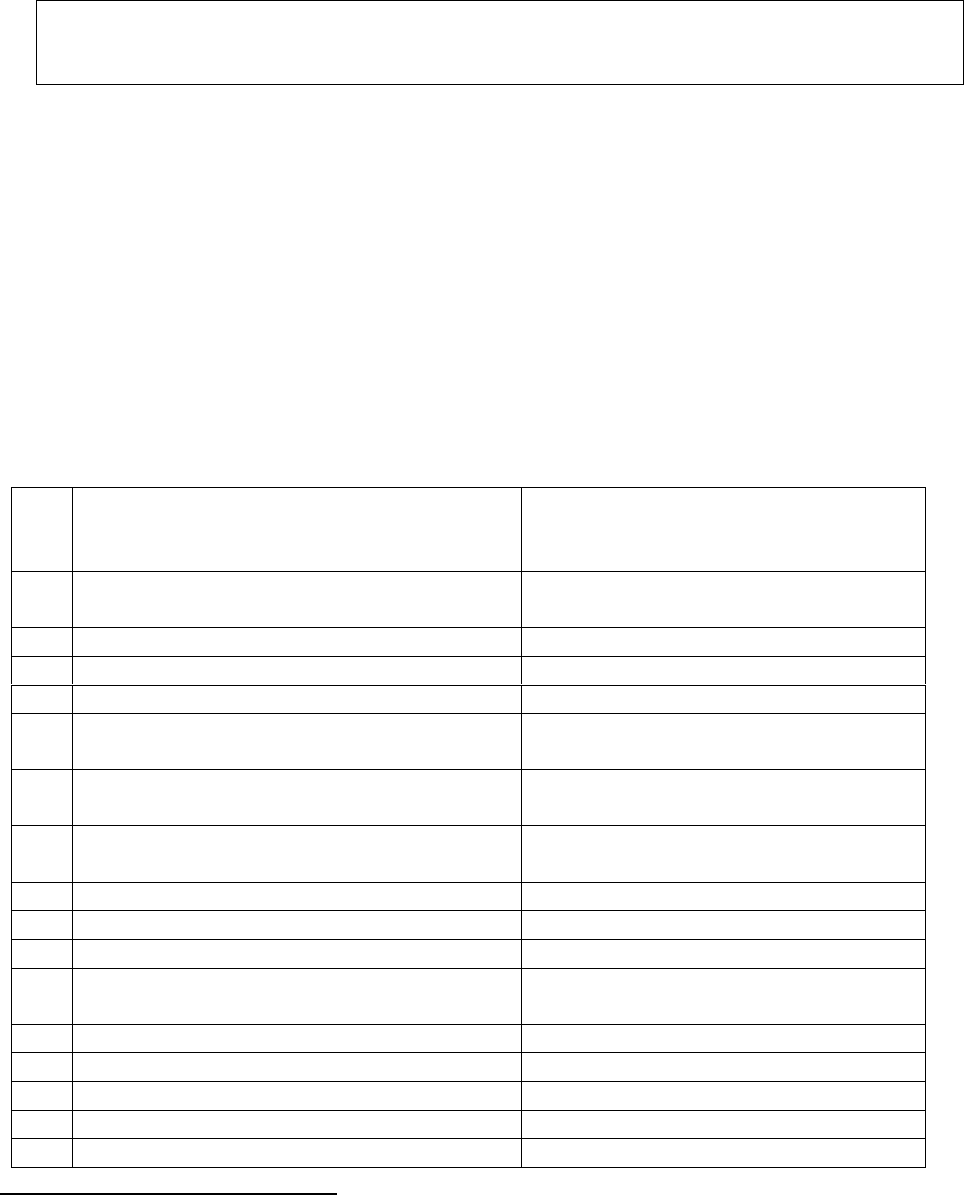
at the hospital. The entire treatment was for prostate problem which falls under waiting period.
Forum concurs with the above conclusion. The policy issued date is 23.08.2018, hence it is
established that the ailment was contracted within 2 years of issue of first policy and hence the claim
attracts the exclusion clause 4.3 as stated above.
In view of the above the complaint not sustains.
Award follows,
AWARD
Under the facts and circumstances, the decision of rejection of claim is found correct
and needs no intervention. Complaint therefore stands dismissed.
Dated: On this 30
th
day of Sept, 2021, Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN – VINAY SAH
CASE OF MR. SACHIN PAWAR V/S UNITED INDIA INSURANCE COMPANY LTD.
COMPLAINT NO: PUN-H-051-1920-0554
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Dr. Sachin Lalasaheb Pawar
Bail Bazar, Market Yard, Karad –
415110 , Dist. Satara, M.S.
2.
Policy No:
Type of Policy:
1613062818P1083444107
Family Medicare Policy 2014
3.
Policy period:
08/10/2018 to 07/10/2019
4.
Sum Insured
Rs.7 lakhs
5.
Date of inception of first policy:
08/10/2012
6.
Name & age of the Insured:
Name of the Policyholder:
Mr. Sachin Pawar – Age: 45 years
Same as above
7.
Name of the Insurer:
UNITED INDIA INSURANCE CO.
LTD.
8.
Reason for repudiation/Partial Settlement:
Correction of Refractive Error of eye
less than -7 not payable
9.
Date of receipt of the Complaint:
05/12/2019
10.
Nature of complaint:
Rejection of claim
11.
Amount of Claim:
Rs.1,20,000/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021; (Online)
14.
Representation at the hearing
aaaa) For the Complainant:
Himself
bbbb) For the insurer:
Mr. Sunil Desai
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:
The Complainant and his family were covered under the subject policy for a SI of Rs.7 lakhs for the
period 08/10/2018 to 07/10/2019. The insured patient, Mr. Sachin Pawar was admitted to New Vision
Laser Center, Mumbai on 18/07/2019 for treatment of Anisometropia in both eyes.
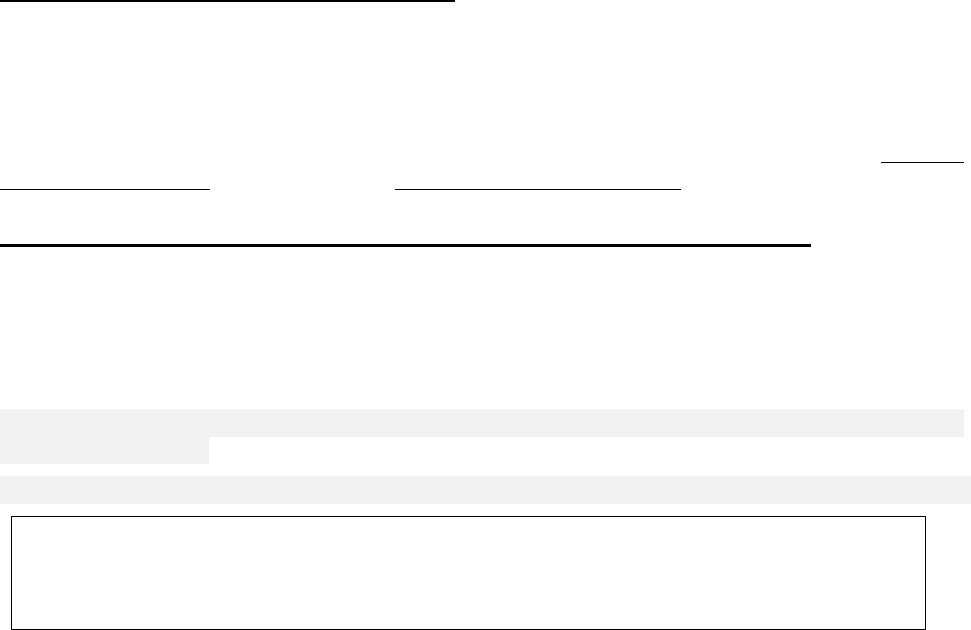
The complainant incurred an amount of Rs.1,20,000/- towards the treatment and the RI has repudiated
the claim stating that the said treatment was for refractive error to both eyes which was not payable
as per the policy terms and conditions.
He has further alleged that the RI in their rejection letter have mentioned that if refractive reading
error of eye is more than (+ or-7), then the claim is payable in his case refractive reading error of right
eye is (-5.75) and of left eye is (-2.25). But the limits of the refractive reading error are not shown
anywhere in the policy terms and conditions of his policy. The grievance cell has mentioned that
SMILE is a laser vision correction surgery i.e. similar to LASIK and is not payable as per exclusion
no. 4.6. The word LASIK is not mentioned in the said exclusion.
Due to high refractive error in both eyes, he was suffering from headache and mental stress which
affected his smooth performance. He has not treated his eyes for beauty and art as well as to get
benefit from insurance company. Eye surgery is not easy task, there is some risk which may cause
loss of eye sight.
He is a M.S. (General Surgeon) and doing full time micro and delicate surgeries such as hair transplant.
It was very necessary to perform both eyes surgery for better results considering high refractive
reading error in both eyes. He has also submitted the treating Dr. Yogesh Rajguru’s certificate dt.
18/06/2019 in its support.
Contentions of the Respondent Insurer (RI):
The RI has contended that the claim has been rejected as per Clause No.4.6 of the policy clause,
which is reproduced hereunder:
4. Exclusions The company shall not be liable to make any payment under this policy in respect of
any expenses whatsoever incurred by any Insured Person in connection with or in respect of:
4.6 b. Vaccination or inoculation of any kind unless it is post animal bite, change of life or cosmetic
or aesthetic treatment of any description such as correction of eyesight, etc.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (Online), both the parties reiterated their respective stand.
During the hearing, forum specifically asked the RI representative, about the admissibility of claim
in case of refractive error having more than -7. In support of which he submitted their internal
guideline showing admissibility of claim in case of Myopia with plus or minus 7. The forum also
found that as per the latest guidelines issued by IRDAI in their circular no.
IRDAI/HLT/REG/CIR/177/09/2019 dt.27/09/2019 they have approved the exclusion of refractive error
less than 7.5 dioptres.
In view of this, rejection of claim is appropriate. Complaint therefore is not admissible. Award follows:
AWARD
Under the facts and circumstances of the case, forum finds that the claim falls in the
exclusion clause, hence complaint stands dismissed.
Dated: at Pune this 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. SALEEL YARDI V/S HDFC ERGO GEN INS CO LTD
COMPLAINT NO: PUN-H-018-2021-0554
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Saleel Yardi
Thane
2.
Policy No:
Type of Policy:
2861 1008 5781 2400 000
Corona Kavach Policy
3.
Policy period:
10.09.2020 to 21.06.2021
4.
Sum Insured
450000
5.
Date of inception of first policy:
10.09.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Mr. Saleel Yardi, 29 yrs
Mr. Saleel Yardi
7.
Name of the Insurer:
The HDFC ERGO Gen Ins Co Ltd
8.
Reason for repudiation/Partial Settlement:
Treatment taken on OPD basis.
Repudiated under section 7.6
9.
Date of receipt of the Complaint:
05.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
SI
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
cccc) For the Complainant:
Himself
dddd) For the insurer:
Dr. Ravikant Upadhyay
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:-
• The complainant had taken Corona Kavach Policy with Respondent Insurer The HDFC
ERGO Gen Ins Co Ltd for self for Sum insured of Rs.4.5 lakhs. He lodged claim for expenses
incurred on home-quarantine medications in consultation with Shri Mahavir Jain Hospital on
22.11.2020 for Covid 19. The RI regretted the claim stating that the treatment was taken on
OPD basis under policy clause no.7.6.
• The treating doctor advised him for home quarantine due to non-availability of beds and pre-
scribed medicines for 14 days. He was in continuous follow up with the doctor and took online
consultations.
Contentions of the Respondent Insurer (RI):-
As per their SCN, their contentions are reproduced below:
1. That, we issued Corona Kavach Policy bearing Number 2861 1008 5781 2400 000 for the period from
10/09/2020 to 21/06/2021 subject to the term/s and/or condition/s incorporated and to the extent of
limits mentioned in the said Policy. Copy of Policy Schedule along with terms and conditions
2. That we have received an intimation of a claim from and / or on behalf of the complainant to the effect
that complainant detected Covid-19 and took Home Care treatment.
3. It is submitted that as per the policy Home care treatment is allowed as per the below terms and
conditions of the policy –
Home Care Treatment Expenses:
Home Care Treatment means Treatment availed by the Insured Person at home for Covid on positive
diagnosis of Covid in a Government authorized diagnostic Centre, which in normal course would require
care and treatment at a hospital but is actually taken at home maximum up to 14 days per incident
provided that:
a) The Medical practitioner advices the Insured person to undergo treatment at home.
b) There is a continuous active line of treatment with monitoring of the health status by a medical
practitioner for each day through the duration of the home care treatment.
c) Daily monitoring chart including records of treatment administered duly signed by the treating doctor
is maintained.
d) Insured shall be permitted to avail the services as prescribed by the medical practitioner. Cashless or
reimbursement facility shall be offered under homecare expenses subject to claim settlement policy
disclosed in the website.
e) In case the insured intends to avail the services of non-network provider claim shall be subject to
reimbursement, a prior approval from the Insurer needs to be taken before availing such services.
4. Now considering the symptoms of the complainant such as No fever, Oxygen level is above 90, No
cough, No cold and treatment was taken on OPD basis as such the claim was repudiated vide letter dated
21/01/2021.
5. That after the repudiation of claim, upon the representation of the complainant, we have reviewed
the case and send the letter dated 15/02/2021, 02/03/2021, 17/03/2021, for submission of –
1. CT chest report as per the submitted bill.
2. Datewise vital chart with treatment record during home quarantine certified by the treating doctor.
6. However, till date we have not received the abovementioned documents thus the claim is closed vide
our letter dated 01/04/2021.
Result of personal hearing with both the parties (Observations & Conclusions):
Upon going through the documents submitted and the SCN, it is observed that the RI themselves have
agreed in their SCN that their policy covers the expenses incurred in home quarantine for covid
positive treatment on the advise of medical practitioner. Hence, it is apparent that initially, the RI have
repudiated this claim on incorrect grounds. Afterwards, they have asked certain documents for
processing of the claim. The forum advised the complainant to submit the same and accordingly, the
complainant has provided it through mail. The documents are forwarded to RI over mail for assessing
of the payable amount in this case.
Complaint is admitted.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to pay the
admissible amount in this case to the complainant towards the full and final settlement of
this complaint.
The award is to be complied with one month from the date of receipt of this award failing
which it will attract interest at the applicable bank rate plus 2% extra from the date of
rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
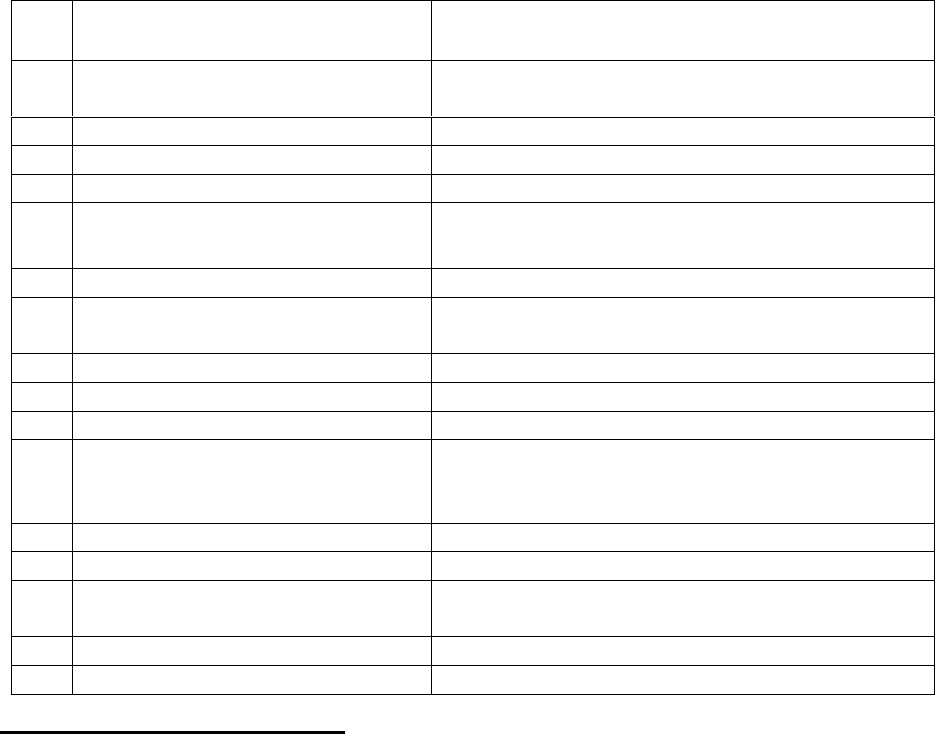
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurers.
Dated: this, on 16
th
day of September 2021, at Pune
VINAY SAH
Insurance Ombudsman,
Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF DR. SANDEEP P TIWARI V/S RELIANCE GENERAL INS CO LTD
COMPLAINT NO: PUN-H-035-2021-0590
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Dr. SANDEEP P TIWARI
PALGHAR
2.
Policy No:
Type of Policy:
110492028521022370
Reliance Covid 19 Protection Insurance
3.
Policy period:
13.05.2020 to 12.05.2021
4.
Sum Insured
Rs. 100000
5.
Date of inception of first policy:
13.05.2020
6.
Name & Age of the Insured:
Name of the Policyholder:
Dr. Sandeep P Tiwari, 37 yrs
Same as above
7.
Name of the Insurer:
The Reliance General Ins Co Ltd
8.
Reason for repudiation/Partial
Settlement:
As per exclusion clause section 4 : Specific
exclusion related to co-habitation
9.
Date of receipt of the Complaint:
21.02.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Rs.100000/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
eeee) For the Complain-
ant:
Himself
ffff) For the insurer:
Mr.Dhruv Kumar; Dr.Amit
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:-

• The complainant had taken Reliance Covid 19 protection insurance Policy with Respondent
Insurer Reliance General Insurance Co Ltd for self for Sum Insured (SI) of Rs. 1 lakh. He
lodged claim of self-hospitalization in Cardinal Gracias Memorial Hospital, Palghar from
28.06.2020 to 12.07.2020 for Covid 19 positive. The complainant is claiming for SI 1 lac.
• The RI repudiated the claim stating the reason that he was working in a covid dedicated hos-
pital at the time of filing of proposal, hence the claim is rejected in view of the specific exclu-
sion clause related to section 3 of policy “Co-habitation”
• According to him the hospital started admission of covid 19 due to government policy from
15.06.2020 and that ward was in different building. The complainant had never worked in
Covid ward or never went to covid building.
• The complainant is requesting forum to intervene for settlement of SA
Contentions of the Respondent Insurer (RI):-
As per the SCN received, RI has contended that,
• The complainant Dr Sandeep Premshankar Tiwari was duly insured with the company under
Reliance Covid 19 protection insurance vide policy no 110492028521022370 period
13.05.2020 to 12.05.2021 subject to terms and conditions of the policy
• After perusal of documents submitted by the complainant of hospitalization and investigation
in the matter it was observed that insured was diagnosed with Covid 19 and got admitted in
Cardinal Gracious memorial Hospital from 28.06.2020 to 12.07.2020.
• The said hospital was a covid 19 designated hospital. That the Insured was a health worker
working as RMO in cardinal hospital at the time when policy application was signed on
13.5.2020. The insured himself admitted that he was working in the said hospital at the time
of proposal of policy. In para 16 of questionnaire complainant has clearly answered in affirm-
ative that he is symptomatic health care worker/frontline worker.
• As per underwriting guidelines insured is supposed to disclose their profession/source of in-
come in order to categories the risk levels. His profession is considered under Risk Level III
– Very High Risk (Doctors, Nurses or any healthcare service providers)
• Since the insured was sharing the same address of the said covid 19 designated hospital at the
time of proposal of policy, the claim not payable due to Co-habitation as per policy terms and
conditions.
• If at the time of policy inception the insured had disclosed his occupation, then the Insurance
Company would have had the opportunity to avoid the policy or otherwise.
• CLAUSE 4 SPECIFIC EXCLUSIONS RELATED TO SECTION 3 SPECIFIES ABOUT CO
HABITATION
• CO-HABITATION: NO CLAIM SHALL BE PAYABLE WHERE THE INSURED PERSON
WAS LIVING WITH AND SHARING THE SAME ADDRESS AS THAT OF PERSON(S)
WHO WERE DIAGNOSED WITH COVID 19 OR QUARANTINED AT THE TIME OF
PROPOSAL.HENCE CLAIM STANDS REJECTED
• POLICY CONDITION SECTION 6 : NON DISCLOSURE OR MISRESPRESENTATION
Result of personal hearing with both the parties (Observations & Conclusions):
During the hearing both the parties contended their respective stand.
On hearing both the sides and scrutinizing the documents placed on record, forum has following
observations:
RI has taken baseless and contradictory pleas in their defense which is not at all appreciated by the
forum. The RI is saying in point no.10 of their SCN that the complainant was sharing the same address
of the covid 19 designated hospital. Whereas, the address on the policy differs from the address of
the hospital.
RI contention of same address is not clear. Ideally, it should be a house or flat or room in case of a
hostel. Entire building cannot be considered as the same address.
It is found that the questions in proposal form ‘occupation’ and ‘annual income’ have been not
answered. If the occupation was so important for RI to decide the risk category, then how the
underwriting was done and policy issued even when it was left blank. Besides, the complainant
submitted during the hearing that he had told company representative that he was a doctor and asked
if he can purchase the policy. He has submitted whatsApp chat with one Mr. Sachin in support of his
contention; wherein the said Sachin has replied that he can take the policy.
Forum did not see any term in the policy document or any of their broachers for considering the health
workers to be termed as high risk factors. On the contrary, there are government guidelines to cover
the health workers and in its accordance IRDAI had issued guidelines to insure them at discounted
rates.
Thus, forum quashes the plea taken by RI. Rest of the eligibility criteria are fulfilled by the
complainant for getting the claim under this benefit policy. Complaint admitted.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to pay
to the complainant Rs.1,00,000/- towards the full and final settlement of this complaint.
The award is to be complied with one month from the date of receipt of this award failing
which it will attract interest at the applicable bank rate plus 2% extra from the date of
rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurers.
Dated: at Pune this 15
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR.SANJAY DALVI & INDIRA SANJAY DALVI
V/S
THE ORIENTAL INSURANCE CO.LTD.
COMPLAINT NO: PUN-H-050-2021-0555 and
PUN-H-050-2021-0556
Award No IO/PUN/A/HI/ , /2021-22
1.
Name & Address of the
Complainant
Mr.Sanjay Dalvi &
Mrs.Indira Sanjay Dalvi; Pune
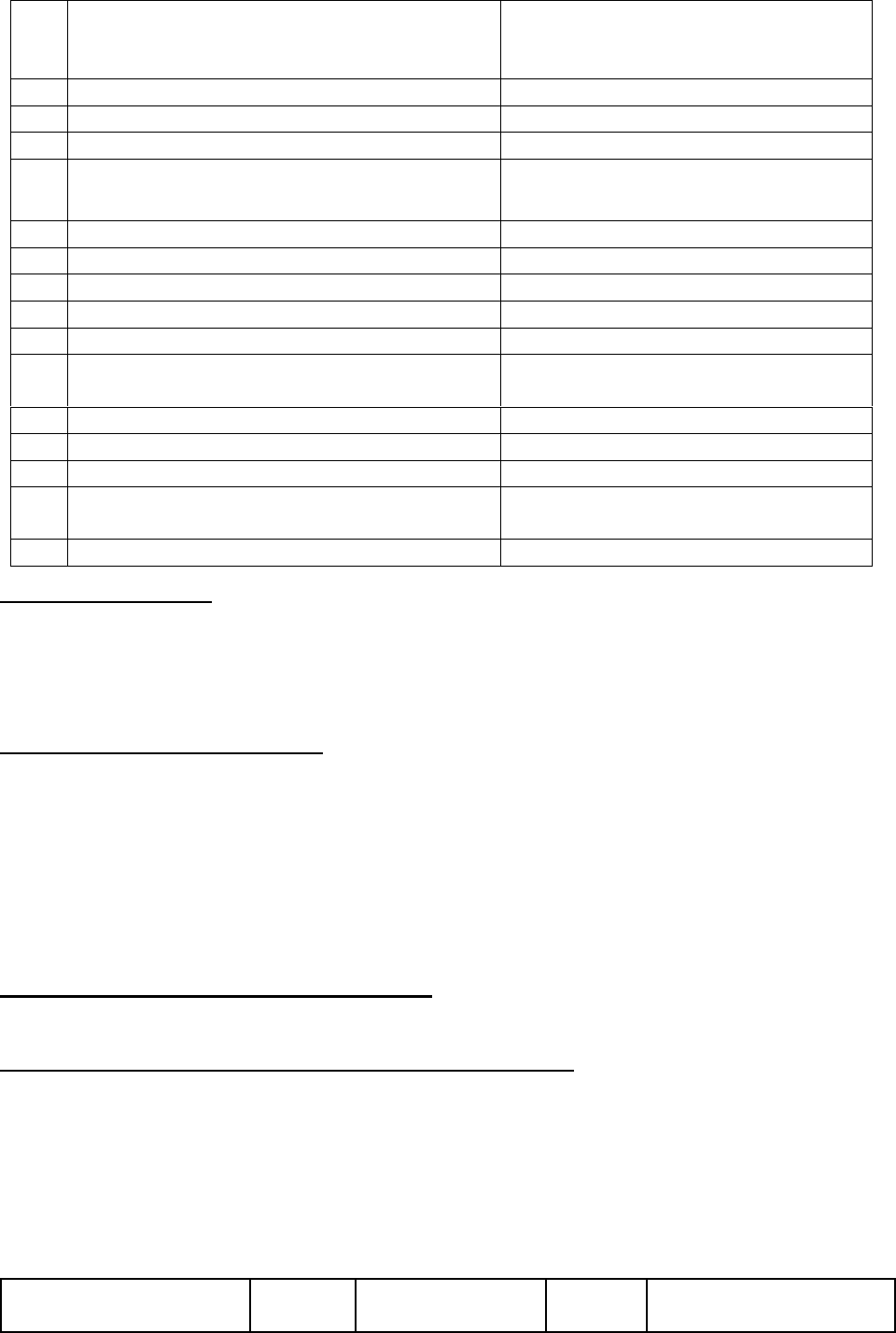
2.
Policy No:
Type of Policy:
412400/48/2020/1845SGroup
Mediclaim Policy
Corporate policy(Flsmidth Pvt Ltd)
3.
Policy period:
14.02.2020 to 13.02.2021
4.
Sum Insured
--
5.
Date of inception of first policy:
NA
6.
Name & Age of the Insured:
Name of the Policyholder:
MR Sanjay & Mrs. Indira Dalvi
FLSmidth Pvt. Ltd.
7.
Name of the Insurer:
The Oriental Insurance Co Ltd
8.
Reason for repudiation/Partial Settlement:
As per Maharashtra Govt. Circular
9.
Date of receipt of the Complaint:
12.02.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
SA.29530/- + Rs. 1,64,414/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021;Online
14.
Representation at the hearing
gggg) For the Complainant:
Himself
hhhh) For the insurer:
Hemlata Saktikumar; Mr. Anand
Shridhar; Dr. Kamla Nathan
15.
Complaint how disposed:
Allowed
Brief facts of the case:
Both the above complaints are of husband and wife covered in the family under a group policy issued
by the Respondent insurer (RI) for the group of Flsmidth Pvt Ltd. As the complaints of both of them
have arisen on account of short payment of their covid claims in the same period, forum has
considered both the complaints under a common judgment.
Contentions of the Complainants:
• The complainant Mr. Sanjay Dalvi and his family were covered under Group Mediclaim Pol-
icy with Respondent Insurer (RI) The ORIENTAL Insurance Co Ltd for Sum Insured of Rs
3.5 lakh. Both have lodged claims for their hospitalizations in Gunjkar Multispecialty Hospital,
Pune from 14.08.2020 to 28.08.2020 & 18.08.2020 to 22.08.2020 respectively for Covid 19.
• They have filed these complaints for short payment of their claimed amount and have re-
quested forum to intervene for settlement for full claimed amounts.
Contentions of the Respondent Insurer (RI):-
Contents of their SCN are reproduced below:
Re: 1. Claim no. 23083403 – Policy No. 412400/48/2020/1845
Employee Name: Sanjay Dalvi
Patient Name: Sanjay Dalvi/Self
Corporate Name: FLsmidth P. Ltd.,
Mr. Sanjay Dalvi and his family is covered under the above GMC policy.
Mr. Sanjay Dalvi was diagnosed Covid -19 + and taken treatment at Gunjkar Multispecialty
Hospital, Pune, from 14/08/2020 to 28/08/2020.
He has claimed an amount of Rs.264744/- towards the hospitalization expenses and Mediassist
TPA has settled the claim for Rs. 100330/- as shown below:
Category
Actual
Payable
Deducti
on
Reason
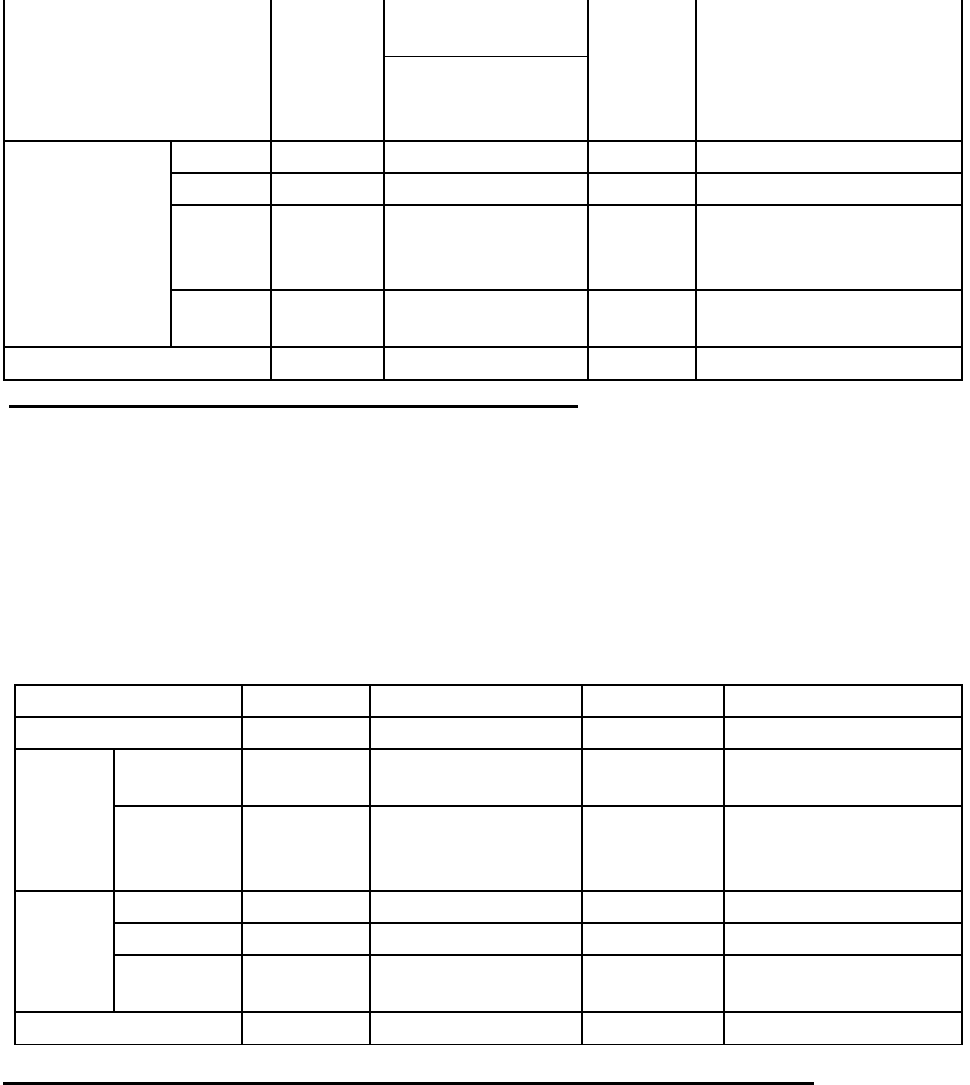
Hospitalisation Bill
181250
ICU 4 days -
7500*4 = 30000
103050
As per Maharashtra
circular
RR 11 days -
4000*11 = 44000
+lab 4200
Pre & Post
Hospitalisatio
n
Lab
21000
21000
0
Doctor
200
200
0
Miscell
aneous
61364
61364
R60764 – No bills
enclosed – Rs 600 only
receipt
Pharma
cy
930
930
0
Total
264744
100330
164414
2. Claim no. 23083628 – Policy No. 412400/48/2020/1845
Employee Name: Sanjay Dalvi
Patient Name: Indira Sanjay Dalvi/spouse
Corporate Name: FLsmidth P. Ltd.,
Mr. Sanjay Dalvi and his family is covered under the above GMC policy.
Mrs. Indira Sanjay Dalvi was diagnosed Covid -19 + and taken treatment at Gunjkar
Multispecialty Hospital, Pune, from 18/08/2020 to 22/08/2020.
She has claimed an amount of Rs.63011/- towards the hospitalization expenses and Mediassist TPA
has settled the claim for Rs. 33445/-
In PUN-H-050-2021-0555
Claim
23083628
Category
Actual
Payable
Deduction
Reason
Hospita
l Bill
Final bill
44050
20600 (RR 4000*5
+ Lab 600 )
23450
As per Maharashtra
circular
Medicines
12061
5995
6066
As per Maharashtra
circular only high end
medicines are paid.
Pre &
Post
Expens
es
Lab
6650
6650
0
Doctor
200
200
0
Miscellane
ous
50
0
50
Registration
Total
63011
33445
29566
Result of personal hearing with both the parties (Observations & Conclusions):
Online hearing was held on 19/05/2021 through video conferencing wherein, both the parties
reiterated their respective stand.
It was noticed that the complainant had forwarded original claim papers to this office mistakenly. It
was therefore told to the insured to collect all the originals he has submitted from this office and
submit it to the RI/TPA for processing of the claim afresh. From the deductions, it is observed that
the RI had made heavy deductions on the grounds of Maharashtra circular, high end medicines etc.
During the hearing, RI was instructed that the government guidelines on rates of the hospital are not
meant for the insurance companies but are issued to the hospitals and in the same circular, they have
instructed that the claims of the patients who have insurance, will have to be governed as per their
respective policy terms and conditions only. As also, there are clear cut instructions from IRDAI to
settle the claims as per policy terms and conditions only.
Besides, instructing the RI, during the hearing, to reassess the claims, it is observed that the RI has
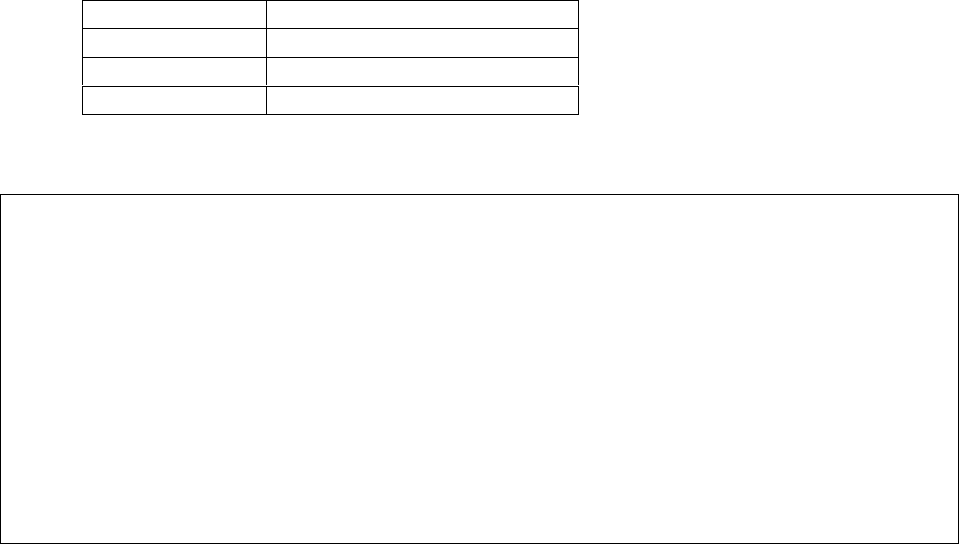
now paid Rs.60764/- towards medical bills only after submission of the originals mentioned above.
They have not resolved the other issues mentioned by the forum to consider while reassessing of the
amounts as per policy terms and conditions and not as per the State Govt. guidelines, as those are
formulated for hospitals and not for the insurance companies. Forum waited till this date for their
reassessment of the amounts, but they did not bother to comment on it in the subsequent mails. They
did not bother to mention the sum insured also of the insured members in their SCNs. In absence of
which, the forum is not able to calculate the payable amount.
In view of this, the forum has no alternative but to allow the balance amount in full.
i. In claim no.23083403 of Mr. Sanjay Dalvi; PUN-H-050-2021-0555 Rs.1,03,050/-balance
amount of hospital bill.
ii. In claim no.23083628 of Mrs. Indira Sanjay Dalvi; PUN-H-050-2021-0556 Rs.29516/- as
detailed below:
Payment head
Amount Deducted by RI, Rs.
Hospital bill
23450
Medicines
6066
Total
29516
Complaints allowed. A common award for both the complaints follows:
AWARD
Under facts and circumstances of the cases,
i. The Respondent Insurer is directed to pay Rs. 1,03,050/- to the Complainant towards
full and final settlement of complaint no. PUN-H-050-2021-0555;
ii. The Respondent Insurer is directed to pay Rs. 29,516/- subject to the terms mentioned
above, to the Complainant towards full and final settlement of complaint no. PUN-H-
050-2021-0556
Payment is to be made within the balance SI and the award is to be implemented within one
month from the date of receipt of this award failing which it will attract interest at the
applicable bank rate plus 2% extra from the date of rejection of the claim till the date of
payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune this on 29
th
day of September2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Sanjay Narayan More v/s Manipal Cigna Health Insurance Company Ltd
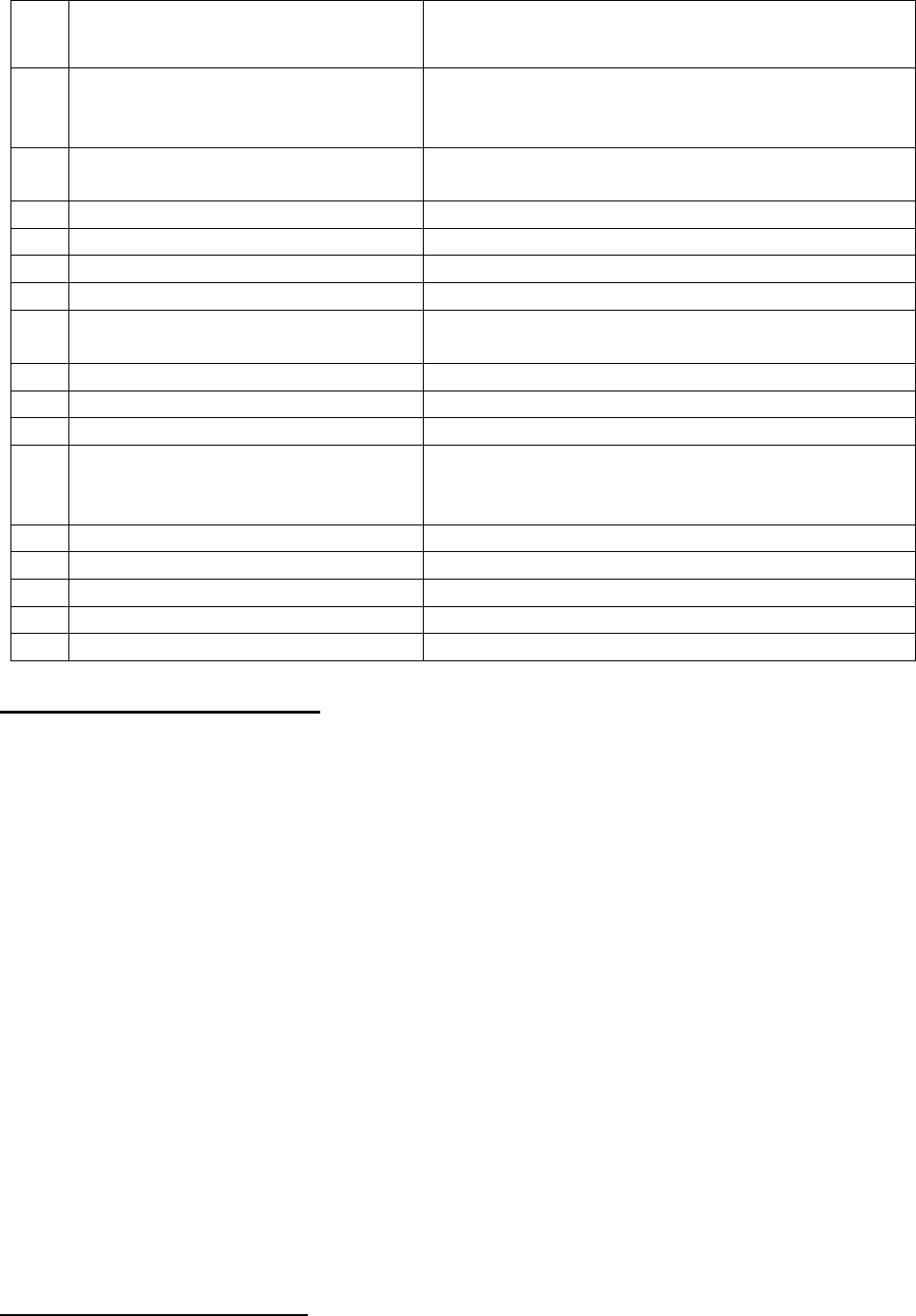
COMPLAINT NO: PUN-H-053-1920-0685
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Sanjay Narayan More,
Dighi, Pune
2.
Policy No:
Type of Policy:
PROHLR 010308590-PREM-Rs.18204/-
PROHLR 010302709-PREM-Rs.72000/-
Both policies are of -Pro-Health Accumulate Plan
3.
Policy period:
27/2/2017-26/2/2018
9/3/2017-8/3/2018
4.
Sum Insured
NOT MENTIONED
5.
Date of inception of first policy:
27/2/2017 &9/3/2017
6.
Name of the Policyholder:
Mr. Sanjay More.
7.
Name of the Insurer:
Manipal Cigna Health Insurance Company Ltd
8.
Reason for repudiation/Partial
Settlement:
Cancelation request not received in Free look
period.
9.
Date of receipt of the Complaint:
12/02/2020
10.
Nature of complaint:
Missale-Refund of premium
11.
Amount of Claim:
Rs.90204/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
13 1(b)
13.
Date of hearing/Place:
On line hearing on 13.08.2021
14.
Representation at the hearing
iiii) For the Complainant:
Himself
jjjj) For the insurer:
Mr. Jaswinder Shekhawat
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:
Complaint is for mis-sale.
The complainant was contacted by Broker’s officials and compelled to purchase several policies from
different companies for releasing payment of existing policy of Bharti Axa Life Insurance Co. Ltd.
Even after purchasing 23 policies (16 Life and 7HI) for annual premium amounting to Rs.873957/-.
The complainant did not get promised benefits. As such he had approached RI for cancellation of
policies issued by them and refund of premium but his request was rejected stating that application
for cancellation of both the policies are not made within free look period. Hence, complainant
approached to this Forum for resolution of issue.
Complainant has filed cluster complaint for various policies including the policies (mentioned above)
issued by respondent Insurer (herein after is called RI). As per contention of the Complainant, he is
an Army person and Government is providing medical facilities for himself and his family. Also,
Army persons are not allowed to admit in hospital other than the hospital provided for Army.
Therefore, there was no need for taking the Mediclaim policies. SB Insurance Broker’s Company of
the RI has issued two policies with the gap of one month only. Policies were sent on village address
where his old mother aged 60yrs stays. Complainant visits his home town every six month. Hence,
he could not get the policy in time to cancel it in free look period.
Application for refund of premium was rejected by the RI stating that refund is not allowed because
it is not made in free look period.
Complainant has filed FIR against the SB Broker persons, copy of the complaint sent to Finance
Minister of the, IRDA.
Complainant is contending that Cigna TTK has cheated him therefore requesting to direct the RI to
refund the premium, through Forum.
Contentions of the Respondent:
Regret letter dated 21.02.2020
As regards concerns raised, RI had re-examined the complaint and wish to inform that the proposal
forms for the captioned policy was duly signed by complainant and the policy has been issued with
the agreed terms and conditions.
After careful evaluation of complainant’s request, RI regret to inform that they are unable to honour
the request for free look cancellation of the aforesaid policy. The policy is not eligible for any
payout.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 13.08.2021 (through video-conferencing) both the parties reiterated
their respective stand.
During the hearing RI contended that policies were marketed through independent agents and not
through Insurance brokers. Policies were issued based on proposal forms duly signed by complainant.
On 24.08.2017 they received policies cancellation request from the complainant.
Accordingly, they calculated the refund at 35% of premium and forwarded him consent letter for his
signature. Then again on 07.9.2017, they received a request from the insured stating that he doesn’t
want to cancel but continue with it. Thereafter after lapse of the policy again he requested for
cancellation of policy, but because of lapse of policy, cancellation could not take place.
These facts were cross verified with the complainant. He agreed that he had asked to continue with
the policy on advice of the broker, who again showed him lure of getting money subject to
continuation of the policies.
In view of these facts, it is evident that the complainant was falling prey to the fraudsters again and
again. This cannot be termed as mis-sale but it is sheer negligence on the part of investor. He is a
learned person. Government keeps sending alert messages to the general public through various
media. By asking for continuation of policy complainant himself has deviated from his own
allegations of mis-sale. Complaint cannot be allowed under this situation.
Award follows,
AWARD
Under the facts and circumstances, complaint stands dismissed as the act of mis-sale is
not proved.
Dated: at Pune, on this 15
th
day of September, 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Shantilal Sureka v/s National Insurance Co. Ltd
COMPLAINT NO: PUN-H-048-1920-0701
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Shantilal K. Sureka,
Aurangabad
2.
Policy No:
Type of Policy:
270608501810000562
National Mediclaim Policy
3.
Policy period:
21/1/2019-20/1/2020
4.
Sum Insured
250000/- each
5.
Date of inception of first policy:
20/1/2016
6.
Name & age of the Insured:
Name of the Policyholder:
Shantilal Sureka 72 years
same as above
7.
Name of the Insurer:
National Insurance Co. Ltd
8.
Reason for repudiation/Partial Settlement:
Surgeon Charges deducted on reasonable
and Customary basis.
9.
Date of receipt of the Complaint:
6/2/2020
10.
Nature of complaint:
Partial Repudiation of claim
11.
Amount of Claim:
11280/-
12.
Insurance Ombudsman Rule (IOR)2017 under
which the Complaint was registered:
13 1(b)
13.
Date of hearing/Place:
14.
Representation at the hearing
On line hearing on 13.08.2021
kkkk) For the Complainant:
Himself
llll) For the insurer:
Mr. Shreyas
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:
The complainant has Health policy for himself and spouse for sum insured of Rs.250000/- each from
2016. He made one claim for his left eye cataract operation (hospitalization from 12/11/2019 to
13/11/2019). Amount claimed by complainant is Rs.36409/- out of this Respondent insurer (herein
after is called RI) has sanctioned the amount of Rs.25129/-
Complainant has submitted complaint with certificate of the treating Doctor explaining why they have
charged Rs. 34000/- for surgery. As per explanation, they are using phacoemulsification technique
with separate cassette for each individual patient.
On the basis of the certificate of treating doctor complainant has filed complaint before this Forum
for settlement of balance amount Rs. 11,280/-
Contentions of the Respondent:
As per SCN, RI has given explanation that amount of Rs.11000/- were disallowed from claim, as
these charges of Shri Krishna Netralaya are on higher side. The charges were compared with other
hospital including tertiary care hospital in metro cities. Where the treatment charges are on lower side.
Which shows that same charges claimed by the complainant are exorbitant.
Since the surgery charges are on higher side, Rs. 11,000/- has been deducted as per policy clause 3.29
it states as under:
“Reasonable and customary charges means the charges for services of supplies, which are the
standard charges for the specific provider and consistent with the prevailing charges in the
geographical area for identical or similar services, taking into account the nature of the illness/injury
involved.”
Lab Charges of Rs.180/- dated 31/7/2019 and Rs. 100(ECG) dated 10/8/2019 are deducted since
these bills falls before 30 days of hospitalization hence disallowed.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 13.08.2021 (through video-conferencing) both the parties reiterated
their respective stand.
During the hearing RI was informed that forum finds the claimed amount for cataract surgery is quite
reasonable after handling of similar complaints filed before this forum. IRDAI have also prescribed
25% or 40K of SI for cataract surgery as per the recent guidelines. Here SI is 2.5lakhs
Complaint therefore is admitted for Rs.11,000/-. Award follows:
AWARD
Under the facts and circumstances, the RI is directed to pay Rs.11000/- as per the terms and
conditions of the policy to the complainant, towards full and final settlement of the complaint.
The award is to be settled within one month from the date of receipt of this award failing which
it will attract interest at the prevailing bank rate plus 2% extra from the date of rejection of
the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award
and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: at Pune, on this 15
th
day of September, 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mrs. Sunita Bankar V/S Star Health and Allied Insurance Company Limited
COMPLAINT NO: PUN-H-044-1920-0513
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mrs. Sunita Bankar, Bankar Vasti, Baramati
2.
Policy No:
Type of Policy:
P/700002/01/2020/018618
Family Health Optima Insurance Plan-Floater.
3.
Policy period:
14/08/2019 to 13/08/2020
4.
Sum Insured/IDV
Rs. 300,000/- Family Floater.
5.
Date of inception of first policy:
14/08/2019
6.
Name & age of the Insured:
Name of the Policyholder:
Mayur S Bankar, 22 Years.
Mrs. Sunita Bankar
7.
Name of the Insurer:
Star Health and Allied Insurance Company Ltd.
8.
Reason for repudiation/Partial
Settlement:
False information furnished by the complainant.
9.
Date of receipt of the Complaint:
20/11/2019
10.
Nature of complaint:
Rejection of claim
11.
Amount of Claim:
Rs. 17,744/-
12.
Rule of IO Rule under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
18/06/2021; Online
14.
Representation at the hearing
mmmm) For the Complainant:
Ms. Sunita Bankar and Mr. Mayur Bankar (son)
nnnn) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:
Complainant is a resident of Sonakaswadi, Pandare, Tal- Baramati, Dist- Pune. Her son Mayur
Sandeep Bankar had a fall from Motorcycle at Raut Vasti, Vidani, Tal- Phaltan on 16/08/2019 at about
02.00 AM. Due to which he received nasal injuries and his nose was bleeding profusely. He was
feeling unwell and dizzy, so initially visited nearby local doctor for first aid and consultation. As
wound was very deep, local doctor advised him to visit Shree Sai Multispeciality Hospital at Phaltan.
He was admitted there at 02.30 A.M. 16/08/2019 under Dr. Saurabh Kharade. He was treated and
discharged on 18/08/2019.
Complainant submitted a claim before RI for reimbursement of medical expenditure for sum of Rs.
17,744/- on 28/08/2019. Complainant received a letter from RI dated 11/09/2019 asking to submit
additional following documents/ information to processes the claim:
1. Self declaration letter stating Circumstances of injury with date, time and place.
2. Treatment details taken immediately after injury. &
3. Pre and Post OP investigation reports.
Complainant submitted self declaration dated 11/09/2019 to RI on 13/09/2019 clarifying all three
points. She received claim repudiation letter dated 03/10/2019 from RI stating that insured patient
Mayur Sandeep Bankar sustained injury on 16/08/2019. But as per the MRI request Form, he visited
MRI centre on 15/08/2019 for MRI study. She has contended that as it was midnight of 15/08/2019,
the staff at the reception counter of the said hospital must have written it mistakenly. She has also
obtained a clarification letter from the hospital dated 13.11.2019 to that effect.
Aggrieved by the rejection of her claim, complainant filed complaint with this forum for resolution
of his grievance.
Contentions of Respondent Insurer (RI):
SCN (Self Contained Note) from RI states that the claim was reported in the 1
st
month of the policy.
Insured preferred a claim for reimbursement of medical expenses incurred for sum of Rs. 17744/-
for treatment of her son Mr. Mayur S Banker who was admitted at Sri Sai Multi Speciality Hospital,
Phaltan for treatment of MILD DIFFUSE CEREBRAL EDEMA WITH LEFT NASAL BONE FRACTURE.
On scrutiny of the Discharge Summary and Self Declaration of the insured person that the injury was
sustained on 16/08/2019 but as per the MRI request form, the insured person visited MRI Centre on
15/08/2019 for MRI study. Thus, there is discrepancy in the documents regarding time of injury
sustained. Therefore, the claim was repudiated as per Condition no. 6 of the policy which read as
under,
“The Company shall not be liable to make any payment under the policy in respect of any claim if
information furnished at the time of proposal is found to be incorrect or false or such claim is in any
manner fraudulent or supported by any fraudulent means or device, misrepresentation whether by
the insured Person or by any other person acting on his behalf”
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 18/06/2021 (through video-conferencing), both the parties
reiterated their respective stand.
1. During the hearing complainant said, the accident happened at home only; whereas, her son
said that he fell from bike in front of his house as the road was slippery it being rainy days.
For these mismatch declarations, they contended that they are illiterate and don’t under-
stand Hindi, which is not convincing.
2. In the complaint letter, it is ‘Fall from M. Bike’ whereas, in hospital papers, it is ‘Fall at Home’.
3. Shriram CT scan center shows date as 15/08/2019, which is prior to the date of accident
(16/08/2019 at 2.30 am, as contended by the RI). Even if we accept the explanation regarding
mistake in date on MRI request form, there is no explanation for the other discrepancies
narrated here below;
4. Discharge card as well as Indoor sheet show admission date as 16/08/2019 which is over-
written. There is overwriting in timings also as: 2.30am/2.30 pm. Overwriting in both of these
forms cannot be an error but is considered as manipulation. Entries are recorded in TPR chart
in the midnight also on both days, 16/8 & 17/8 at 12 am, 2 am, 4 am. On 16/8, in Intake-
Output chart, 200 ml juice is given at 12 midnight.
5. Policy was purchased online with inception from 14/08/2019 and the claim is reported within
2 days of its issue date and there is no substantial proof of date, time and place of the said
accident. Even the hospital notes are not very descriptive so as to present a clear picture.
In view of the above observations, having no proof of accidental injuries, discrepancies in the
narration of the cause, spot and date of the accident, forum is not convinced with the genuineness
of the claim. Complaint, therefore stands dismissed.
AWARD
Under the facts and circumstances of the case, genuineness of the claim and complaint is
not established, hence dismissed.
Dated: at Pune this 30
th
day of September 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. SUNNY J OSWAL V/S STAR HEALTH & ALLIED INS CO LTD
COMPLAINT NO: PUN-H-044-2021-0628
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. SUNNY J OSWAL
PUNE
2.
Policy No:
Type of Policy:
P/151112/01/2020/017270
Star comprehensive insurance policy-2019
3.
Policy period:
26.11.2019 to 25.11.2020
4.
Sum Insured
1000000 floater
5.
Date of inception of first policy:
6.
Name & Age of the Insured:
Name of the Policyholder:
Mrs. Pramila Oswal, 53 yrs
Mr. Sunny Jayantilal Oswal
7.
Name of the Insurer:
Star Health & Allied Ins co ltd
8.
Reason for repudiation/Partial
Settlement:
Reasonable & Customary charges
9.
Date of receipt of the Complaint:
15.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Rs.28770/-
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
19/05/2021; Online
14.
Representation at the hearing
oooo) For the Complain-
ant:
Himself
pppp) For the insurer:
Dr. Anjali Rathod
15.
Complaint how disposed:
Allowed
Contentions of the Complainant:-
• The complainant had taken Star comprehensive insurance policy with Respondent Insurer,
Star Health & Allied Ins co Ltd covering his mother Mrs. Pramila for SI (sum insured) of
Rs.10 lakh. He lodged a claim of his mother’s hospitalization in Jai Jinendra Pratishthan from
01.09.2020 to 11.09.2020 for Covid 19 positive. The claim was partially settled. Total claim
amount was of Rs.64600/-; settled by RI for Rs.35830/- and outstanding amount Rs.28770/-
• The complainant contends that one of his relatives had same covid claim at Jai Jinendra Iso-
lation Centre which was settled in full by New India Assurance.
Contentions of the Respondent Insurer (RI):-
RI submits that the insured submitted claim documents for an amount of Rs. 64,600/- on 30/09/2020.
On scrutiny of the claim documents, company repudiated the claim on 22/10/2020. Thereafter the
claim was paid in piecemeal on each occasion after he represented 3 times. Rs. 19,030/- on
13/01/2021, Rs. 15,000/- on 26/01/2021 and Rs. 1,800/- on 06/02/2021. In total, Rs. 35,830/- were
paid.
As per SCN and the Bill assessment sheet of deducted amount dated 01.02.2021, the details of
deductions are:
Nature of exp.
Amount
claimed
Non
payable
Approved
amt
Remarks
Investigation &
Diagnosis
6500
800
5700
Covid test @Rs2200/- & CT
test @Rs.3500/- payable as per
GIC capping.
Package charges
41300
27970
13330
As per make shift package
Rs.1333/- per day payable
Total deducted
amount
28770
Result of personal hearing with both the parties (Observations & Conclusions):
During the hearing both the parties contended their respective stand.
On hearing both the sides and the documents placed on record, forum has following observations:
The RI has deducted the amounts stating the reasons of customary and reasonability clause, but have
not produced any competitive rates of the other hospitals in the vicinity. Forum does not find any
extra ordinary high rates from the bill submitted as compared to the other bills the forum is coming
across in other similar matters. The abrupt deduction based on make shift arrangement (which the RI
uses for domiciliary hospitalisation), is not acceptable in view of the genuine hospitalization of the
present claim. Hence, total deductions of Rs.28770/-is payable in view of no inadmissible amount
seen in it.
Complaint is admitted.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed
to pay to the complainant Rs.28770/- less registration charges towards the full and
final settlement of this complaint.
The award is to be complied with one month from the date of receipt of this award
failing which it will attract interest at the applicable bank rate plus 2% extra from
the date of rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurers.
Dated: at Pune this 24
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Saurav Chuni Versus Manipal Cigna General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-053-2122-0177
17. Brief Facts of the Case: Shri Saurav Chuni (hereinafter referred to as the Complainant) has filed this com-
plaint against the decision of the Manipal Cigna General Insurance Company Ltd. (hereinafter referred to as
the Insurers or the Respondent Insurance Company) alleging wrong rejection of his kidney transplantation
claim.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant had taken the Prohealth Policy from the Respondent for the
period 06.12.2020 to 05.12.2021. He was admitted in Indraprastha Medical Corporation on 26.12.2020 for
dialysis and discharged on 27.12.2020. He was admitted for Renal Transplantation in the same hospital on
27.12.2020 and discharged on 04.01.2021. He has complained that Respondent denied the cashless
authorization of his hospitalization claim. He then filed the claim for reimbursement of the medical expenses
incurred during hospitalization. The insurance company rejected his claim stating that he had CKD for past five
years but he did not disclose the same in the proposal form. He has denied their contention and stated that he
learnt about the same in February 2020 while undergoing angioplasty. He represented against the rejection on
08.02.2020 and subsequently. He then approached this forum to get relief.
Case of Saurav Chuni Versus Manipal Cigna General Insurance Company Ltd.
1.
Name & Address of the Complainant
Shri Saurav Chuni,
A-212, Street No. 9, West Vinod Nagar, Delhi -110092
2.
Policy No:
Type of Policy
Duration of policy/Policy period
PROHLR410046176
Mediclaim
06.12.2020-05.12.2021
3.
Name of the insured
Name of the policy holder
Saurav Chuni
Saurav Chuni
4.
Name of the insurer
Manipal Cigna General Insurance Company Ltd.
5.
Date of repudiation
02.04.2021
6.
Reason for repudiation
Pre-existing disease non disclosure
7.
Date of receipt of the complaint
08.04.2021.
8.
Nature of complaint
Rejection of claim
9.
Amount of claim
Rs.850700/-
10.
Date of partial settlement
NA
11.
Amount of partial settlement
NA
12.
Amount of relief sought
Rs.850700
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1) (b) – any partial or total repudiation of claim
by insurer.
14.
Date of hearing/place
01.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
1. Shri Saurav Chuni, the Complainant
2. Smt. Anuradha Kapoor, w/o the Complainant
For the insurer
Ms Swetha Nair, Deputy Manager (Legal)
16.
Date of Award/Order
Award under Rule 17/ 01.09.2021
Complaint Ref. No.: DEL-H-053-2122-0177
b) Insurers Argument: The Insurer in their SCN has stated that Complainant was first insured with them on
06.12.2017 and had renewed the policy consecutively every year till 06.12.2020. He was admitted to the
Indraprastha Medical Corporation for dialysis on 26.12.2020 and discharged on 27.12.2020 to undergo kidney
transplantation. His cashless authorization for Rs. 937300/- was denied as they could not rule out the disease
as chronic kidney disease (CKD). The insured was asked to file for possible reimbursement and provide the
duration of CKD. They have noted from the available documents that the complainant is an alcoholic and
habitual smoker. They have noted from the claim documents that he was suffering from CKD for past five
years i.e. before the inception of the first policy with insurers. The same was not disclosed by him in proposal
form or in the pre-policy medical examination. The insurers rejected the claim for non-disclosure of material
facts under Clause VIII.1 of the policy conditions.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal:
a) SCN, Insurance policy, Proposal Form.
b) Hospital records, discharge summaries.
c) Letter to GRO
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Insurers had repudiated the claim and terminated the policy on the grounds of non-disclosure of the
material facts relating to the past medical history (CKD 5 years ago) by the insured in the policy proposal form.
The Complainant has denied the same and states that the treating doctor had written ‘5 years’ in place of ‘5
months’ by mistake. However, such an error by a senior doctor cannot be expected. In any case, the Insurers
have presented other evidence also that lead to the conclusion that the Complainant had history of renal disease.
The Consultation record dated 06.11.2020 had noted that the Complainant had history of micro hematuria 4
years back. Another documents had indicated that the Complainant was a chronic alcoholic and a habitual
smoker which was not disclosed in the proposal form. In these circumstances, the Insurers were justified in
repudiating the proposal and cancelling the policy on the grounds that the Complainant had not disclosed
material information at the time of submitting the policy proposal form. Pursuantly, the complaint shall deserve
rejection.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 01, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Amar Nath Mago Versus Universal Sompo General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-052-2122-0286
1.
Name & Address of the Complainant
Shri Amar Nath Mago, H. No. M-311, 2
nd
Floor,
Guruharkishan Nagar, Paschim Vihar, Delhi-110087
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2828/61315616/00/000
Mediclaim
30.05.2020-29.05.2021
3.
Name of the insured
Name of the policy holder
Amar Nath Mago
Amar Nath Mago
18. Brief Facts of the Case: Shri Amar Nath Mago (hereinafter referred to as the Complainant) has filed
this complaint against the decision of the Universal Sompo General Insurance Company Ltd. (hereinaf-
ter referred to as the Insurers or the Respondent Insurance Company) alleging wrong deductions from
his hospitalization claim.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant had taken the K Bank Healthcare Policy from the Respondent for the
period 30.05.2020 to 29.05.2021. He was admitted in Shree Aggarsain International Hospital on 03.07.2020 and
diagnosed to be suffering from pneumonitis, HTN and found to be Covid Positive. He was discharged from the
hospital on 18.07.2021. The insurers paid an amount of Rs.124066/- to the hospital towards approved
preauthorized amount. The complainant has stated that there were deductions made by the Respondent from his
hospitalization bills. He submitted his claim for reimbursement of the balance amount of Rs. 2,31,201. He
represented against non-payment of the said amount on 04.11.2020 but there was no outcome of the same. He
has now approached this forum for relief.
Case of Amar Nath Mago Versus Universal Sompo General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-052-2122-0286
b) Insurers Argument: The Insurers have stated in their SCN that the cashless request following the
hospitalization of the complainant was initially linked to a critical care policy taken by the insured. Since
the ailment of the complaint was not admissible under that policy, the claim for cashless authorization
was denied. Later they linked it to his K Bank Health Insurance policy and paid an amount of Rs.124066/-
to the hospital. They have stated that the complainant again claimed the expenses he paid to the hospital
during hospitalization. But those expenses were deducted by the insurer as per policy guidelines. The final
settlement letter indicates the deductions have been made towards Room Rent and Nursing Charges; OT
charges; Medicine/ consumable charges and miscellaneous charges from the claim amount. They have
stated the claim has been paid as per the policy terms and conditions.
19. Reason for registration of Complaint: Inadequate settlement of claim.
20. The following documents were placed for perusal:
a) SCN, Insurance policy, Settlement letter.
b) Repudiation letter, discharge summary, hospital bill.
c) Letter to GRO
21. Result of hearing of the parties (Observations and Conclusion):
4.
Name of the insurer
Universal Sompo General Insurance Company Ltd.
5.
Date of repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the complaint
06.08.2021.
8.
Nature of complaint
Inadequate settlement of claim
9.
Amount of claim
Rs 355367/-
10.
Date of partial settlement
18.07.2020
11.
Amount of partial settlement
Rs 124066/-
12.
Amount of relief sought
Rs 231201/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1) (b) – any partial or total repudiation of claim
by insurer.
14.
Date of hearing/place
13.09.2021 Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Amar Nath Mago, the Complainant
For the insurer
1. Dr. Ahmad Ali, AGM (Health Claims)
2. Ms Anita Raghuvanshi, Sr. Executive (Legal)
16.
Date of Award/Order
Recommendation under Rule 16/ 13.09.2021
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to review the claim and settle the same as per the terms and conditions of
the policy, after procuring the required information/documents from the hospital concerned and the
Complainant, for which they require about one week’s time. The Complainant accepts this offer. Thus an
agreement of conciliation could be arrived at between the Complainant and the Insurers, which I consider
as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall review the claim and settle the same as
per the terms and conditions of the policy, after procuring the required information /documents from
the hospital concerned and the Complainant.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 13, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Amar Nath Mago Versus Universal Sompo General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-052-2122-0280
19. Brief Facts of the Case: Shri Amar Nath Mago (hereinafter referred to as the Complainant) has filed this
complaint against the decision of the Universal Sompo General Insurance Company Ltd. (hereinafter re-
ferred to as the Insurers or the Respondent Insurance Company) alleging wrong deductions from the hos-
pitalization claim of his late wife Sunita Mago.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant had taken the K Bank Healthcare Policy from the Respondent for the
period 30.05.2020 to 29.05.2021. His wife was admitted in Shree Aggarsain International Hospital on 30.06.2020
in gasping state with fever and shortness of breath. She suddenly collapsed and CPR was done to revive her. She
expired on 01.07.2020.The complainant has stated that there were deductions made by the Respondent from her
hospitalization bills. In his complaint he has stated that his claim was for Rs 83345/- but insurers passed it for
Rs.38372/-. He represented and claimed the balance amount on 04.11.2020 but there was no outcome of the
same. He has now approached this forum for relief.
1.
Name & Address of the Complainant
Shri Amar Nath Mago, H. No. 311,2
nd
Floor,
Guruharkishan Nagar, Paschim Vihar, Delhi-110087
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2828/61315616/00/000
Mediclaim
30.05.2020-29.05.2021
3.
Name of the insured
Name of the policy holder
Late Sunita Mago
Amar Nath Mago
4.
Name of the insurer
Universal Sompo General Insurance Company Ltd.
5.
Date of repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the complaint
05.08.2021
8.
Nature of complaint
Inadequate settlement of claim
9.
Amount of claim
Rs 96018/-
10.
Date of partial settlement
30.10.2020
11.
Amount of partial settlement
Rs 38372/-
12.
Amount of relief sought
Rs 57646/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1) (b) – any partial or total repudiation of claim
by insurer.
14.
Date of hearing/place
13.09.2021 Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Amar Nath Mago, the Complainant
For the insurer
Dr. Ahmad Ali, AGM (Health Claims)
16.
Date of Award/Order
Recommendation under Rule 16/ 13.09.2021
Case of Amar Nath Mago Versus Universal Sompo General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-052-2122-0280
b) Insurers Argument: The Insurers have stated in their SCN that they paid an amount of Rs.30698/- towards
settlement of the hospitalization claim of the insured person. The claim approval letter indicates the
various deductions that have been made from the claim amount. They have stated the claim has been paid
as per the policy terms and conditions.
19. Reason for registration of Complaint: Inadequate settlement of claim.
20. The following documents were placed for perusal:
a) SCN, Insurance policy, Approval letter.
b) Settlement letter, discharge summary.
c) Letter to GRO
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to review the claim and settle the same as per the terms and conditions of
the policy, after procuring the required information/documents from the hospital concerned and the
Complainant, for which they require about one week’s time. The Complainant accepts this offer. Thus an
agreement of conciliation could be arrived at between the Complainant and the Insurers, which I consider
as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall review the claim and settle the same as
per the terms and conditions of the policy, after procuring the required information /documents from
the hospital concerned and the Complainant.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 13, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Parul Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Saaransh Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Noopur Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Rajni Khakha Versus Universal Sompo General Insurance Company Ltd.
Case of Pinki Versus Universal Sompo General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-052-2122-0326 to 330
20. Brief Facts of the Case: Smt. Parul Narang, Shri Saaransh Narang, Ms Noopur Narang, Ms Rajni Khakha
and Ms Pinki (hereinafter, individually and collectively, ‘the Complainant’) have filed these complaints
against the decision of the Universal Sompo General Insurance Company Ltd. (hereinafter, ‘the Insurers’)
alleging wrong rejection of their respective Corona benefit claim.
Case of Parul Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Saaransh Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Noopur Narang Versus Universal Sompo General Insurance Company Ltd.
1.
Name & Address of the Complainant
Smt. Parul Narang, Shri Saaransh Narang, Ms Noopur
Narang, Ms Rajni Khakha & Ms Pinki
All R/o Flat No. 1101 Tower D1, Pranayam Apartments,
Sector 82, Faridabad 121004
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2856/IMD/OL/0003553/00; 2856/IMD/OL/0003554/00;
2856/IMD/OL/0003559/00; 2856/IMD/OL/0003605/00; &
2856/IMD/OL/0003608/00
Corona Rakshak Policy (Benefit Policy)
07.09.2020-22.06.2021 (First 3 policies)
08.09.2020-23.06.2021 (Last 2 policies)
3.
Name of the insured
Name of the policy holder
Parul Narang, Saaransh Narang, Noopur Narang, Rajni
Khakha & Pinki, respectively
- Same -
4.
Name of the insurer
Universal Sompo General Insurance Company Ltd.
5.
Date of repudiation
18.05.2021
6.
Reason for repudiation
Admission for diagnostic purposes and hospitalization was
not necessary
7.
Date of receipt of the complaint
23.08.2021
8.
Nature of complaint
Rejection of claim
9.
Amount of claim
Rs 250000/- (each case)
10.
Date of partial settlement
NA
11.
Amount of partial settlement
NA
12.
Amount of relief sought
Rs 250000/- (each case)
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1) (b) – any partial or total repudiation of claim by
insurer.
14.
Date of hearing/place
27.09.2021 Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
1. Smt. Parul Narang, Shri Saaransh Narang, Ms Noopur
Narang, Ms Rajni Khakha & Ms Pinki, the Complainants
2. Shri Kamal Narang (See Table in Para 21 for relationship)
For the insurer
Dr. Ahmad Ali, Assistant General Manager (Health Claims)
16.
Date of Award/Order
Award under Rule 17/ 27.09.2021
Case of Rajni Khakha Versus Universal Sompo General Insurance Company Ltd.
Case of Pinki Versus Universal Sompo General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-052-2122-0326 to 330
18. Cause of Complaint:
a) Complainant's Argument: Each Complainant had taken Corona Rakshak Policy from the Insurers for the
period 07.09.2020-22.06.2021 (First 3 cases) and 08.09.2020-23.06.2021 (Last 2 cases). Each had tested
positive for Corona and was admitted in QRG Health City, Faridabad on with the complaints of fever,
weakness, cough, cold, sore throat and body ache. Each was diagnosed mild Covid and pneumonia etc. Each
of them, except for one (Rajni Khakha) was discharged from the hospital on request. The dates of admission
and of discharge are indicated in the table in Para 21 below. Their respective claim under Corona Rakshak
Policy was denied by the insurers on the grounds that hospitalization was not necessary and s/he could have
managed with self-medication and self-quarantine. Each has stated that s/he was not having a separate room
for self-quarantine. They represented against the rejection of their respective claim on 21.05.2021 but there
was no outcome of the same. S/he has now approached this forum for relief.
b) Insurers Argument: The Insurers in their SCN dated 23.09.2021 have stated that each of the complainants had
taken the Corona Rakshak Policy from them and was hospitalized from in April 2021 due to Covid 19 infection.
As per documents provided to them, it is observed that his vitals were within normal limits during
hospitalization. It was primarily for monitoring/isolation purpose, which could have been managed, in-home
isolation. They have invoked Exclusion 6(i) stating “no payment under the policy shall be made in respect of
expenses related to any admission for diagnostic and evaluation purpose.” It further excludes as per Exclusion
6(ii) “any diagnostic expense not related to the current diagnosis and treatment.” They have also referred to the
Clinical Guidance for Management of Adult Covid 19 patients issued by AIIMS/ICMR for Home Isolation of
mild/asymptomatic COVID cases dated 02.07.2020 & 28.04.2021. They have stated that the claim is rejected
on the basis of policy terms and conditions.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal:
a) SCN, Insurance policy.
b) Clinical Guidance, discharge summary.
c) GRO Correspondence.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
These five cases relate to the family and personal staff of Shri Kamal Narang. All cases relate to the repudiated
claim under Corona Rakshak, which is Benefit Policy. Each of the 5 Complainants had undergone
hospitalisation for Covid in April 2021. Details are presented in a tabular form as below:
Case of Parul Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Saaransh Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Noopur Narang Versus Universal Sompo General Insurance Company Ltd.
Case of Rajni Khakha Versus Universal Sompo General Insurance Company Ltd.
Case of Pinki Versus Universal Sompo General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-052-2122-0326 to 330
Complaint Ref. No.
Name
Relation with
Shri Kamal
Narang
Date of
Admission
(DoA)
Date of
Discharge
(DoD)
SOP2 level
on DOA
(Normal: >
94%)
Respiration
Rate on DOA
(Normal: 18-
24/Minute)
DEL-H-052-2122-
0326
Parul
Wife
04.04.2021
09.04.2021
99%
20
DEL-H-052-2122-
0327
Saaransh
Son
13.04.2021
17.04.2021
99%
20
DEL-H-052-2122-
0328
Noopur
Daughter
09.04.2021
13.04.2021
96%
20
DEL-H-052-2122-
Rajni
Maid servant
07.04.2021
15.04.2021
95%
20
0329
Khakha
DEL-H-052-2122-
0330
Pinki
Maid servant
09.04.2021
14.04.2021
98%
20
Each Complainant has stated that s/he was declared Covid Positive per RTPCR Test and an MBBS Doctor
had recommended hospitalisation. S/he has also stated that their house had 8 residents including the two
maidservants, but only 3 bedrooms and, as such, home isolation was not possible. The Insurers had
repudiated the claim on the ground that the incidence of Covid in each case was ‘mild’ and as per the
norms notified by the Ministry of Health & Family Welfare (MoH&FW) dated 02.07.2020, these cases
required home isolation and there was no need for hospitalisation. The Insurers have pointed out that in
each case, all the vital parameters such as BP, Body Temperature, Pulse Rate, SPO2 level and Respiration
Rate were normal on the date of admission. Two of these parameters are noted in the table above. The
complications for Covid patients start after 4 days, but they all, except for Rajni Khakha, got discharged
on request after 4-5 days of admission. As all members of the household had suffered from mild Covid
almost at the same time, they could have stayed together in the same house in home isolation with due
care and caution. But if they were really serious about their isolation, they should not have got discharged
on request prematurely to stay together in the same house. All these factors lead to the conclusion that the
Complainants could have managed with home isolation and did not require hospitalisation in terms of the
MoH&FW norms cited above, which was a necessary requirement for admissibility of the claim as per
the Operative Clause of the Policy. Hence the Insurers were justified in repudiating the claim and,
pursuantly, all the complaints deserve rejection.
Award
The complaints are rejected.
(Sudhir Krishna)
Insurance Ombudsman
27.09.2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 & 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Suman Nagpal Versus HDFC ERGO General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-018-2122-0295
17.Brief Facts of the Case: Shri Suman Nagpal (hereinafter referred to as ‘the Complainant’) has filed
this complaint against the decision of the HDFC ERGO General Insurance Company Ltd. (hereinafter
referred to as ‘the Insurers’) alleging excess premium collection against his mediclaim policy.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant was having the Health Medisure Classic Policy of the HDFC
ERGO GIC dated 26.03.2019. The said policy was renewed as Suraksha Classic Family Policy with effect
from 26.03.2020. The premium collected was in excess on 04.05.2020 but the policy was renewed from
the retrospective date i.e. 26.03.2020. He was getting a discount of 10% ever since he purchased the first
policy from L&T GIC Ltd. in March 2012, which was acquired by the Insurers. The discount has also been
withdrawn by the Insurers. When he represented to the Respondent, they apologized for the unpleasant
experience faced by the complainant but did not offer any monetary relief. He then approached this forum
to get his complaint redressed.
b) Insurers Argument: The Insurers in their SCN of 23.09.2021 have stated that complainant was residing
in Mumbai when he was covered under Medisure Classic Policy for the period 26.03.2019-25.03.2020.
The product was withdrawn by the insurer and the intimation of the same was sent to all existing
policyholders 3 months in advance. The renewal notice of 20.03.2020 was sent to the complainant that
sought a premium of Rs. 39937/-
1.
Name & Address of the Complainant
Shri Suman Nagpal,
WW0803, Ireo Grand Arch, Sector 58, Gurugram-122011
2.
Policy No:
Type of Policy
Duration of policy/Policy period
285720215152170/000
Suraksha Classic Family Policy
26.03.2020-25.03.2021
3.
Name of the insured
Name of the policy holder
Suman Nagpal
Suman Nagpal
4.
Name of the insurer
HDFC ERGO General Insurance Company Ltd.
5.
Date of repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the complaint
10.08.2021
8.
Nature of complaint
Increase in Premium, withdrawal of discount, Date of
commencement of policy
9.
Amount of claim
Rs 22211.00 + 10% Discount on premium amount
10.
Date of partial settlement
NA
11.
Amount of partial settlement
NA
12.
Amount of relief sought
Rs 22211.00 + 10% Discount on premium amount
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules, 2017
Rule 13(1)(f) –policy servicing matter.
14.
Date of hearing/place
27.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Suman Nagpal, the Complainant
For the insurer
Smt. Shweta Pokhriyal, Manager (Legal Claims)
16.
Date of Award/Order
Recommendation under Rule 16 & Award under Rule 17/
27.09.2021
applicable for Tier 1b city. The complainant had also informed about the change of residence to Gurugram,
a Tier 1A city. He was asked for a revised premium of Rs. 49497/-. The policy was issued with
retrospective date to maintain the continuity benefits for the insured. They have admitted the delay in
renewal of policy. The discount was given to him under earlier policies as an employee. It was withdrawn
since he was no longer an employee of the organization. They have stated that there was no deficiency
in policy servicing.
19. Reason for registration of Complaint: Excess Premium Collection.
20. The following documents were placed for perusal:
a) SCN, Insurance policy.
b) Renewal notice, New product intimation.
c) Correspondence with GRO.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The first issue of the complaint is that the Premium was increased on renewal without justification and
without notifying him. The Insurers state that they had discontinued the Health Medisure Classic Policy
after following the due procedure and notified all policyholders including the Complainant. The premium
was enhanced owing to change of the city of residence by the Complainant. The action of the Insurers
was thus devoid of error.
The second issue of the complaint is that the Insurers had withdrawn the 10% discount abruptly. The
Insurers state that the discount was applicable only for the working persons and was given by the previous
Insurers (L&T), which was merged with HDFC Ergo in 2016. The discount was continued as the database
of the Insurers was not updated even after the merger of the previous company. However, once they
updated the database to record the employment status of the Complainant as a retiree, they had to
withdraw the discount. The action of the Insurers was thus devoid of error.
The third issue of the complaint is that the Policy was issued with retrospective effect without his consent.
The Insurers state that this was done to provide continuity benefit to the Complainant, but they have no
problem is making the policy prospective in effect. The Complainant states that he does not wish to lose
the continuity benefit and agrees not to pursue this part of his complaint.
In the result, the the first and the second parts of the complaint are rejected, while the third part is
considered as resolved by conciliation between the Complainant and the Insurers.
Award
The complaint is resolved partly by conciliation between the Complainant and the Insurers inasmuch
as the Complainant agreed not to seek reversal of the issuance of the policy retrospectively. The other
parts of the complaint are rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 27, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Deepak Gupta versus Star Health and Allied Insurance Company Ltd.
Complaint Ref. No.: DEL-H-044-2122-0312
1.
Name & Address of the Complainant
Shri Deepak Gupta
F-17/139, Sector 8, Rohini, Delhi-110085
2.
Policy No.
Type of Policy
Policy term/policy period
P/161211/01/2021/010804
Young Star Insurance Policy
30.12.2020 to 29.12.2021
3.
Name of the insured
Name of the policy holder
Deepak Gupta
Deepak Gupta
4.
Name of insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of repudiation
26.03.2021
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
26.07.2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of claim
Rs.30690/-
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
12.
Amount of relief sought
Rs.30690/-
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims
by an Insurer
14.
Date of hearing
06.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
Shri Deepak Gupta, the Complainant
For the Insurer
1. Dr. Madhukar Pandey, Chief Manager (Health Claims)
2. Shri Mantosh Kumar, Sr. Manager (Claims)
16.
Date of Award/Order
Recommendation under Rule 16, 06.09.2021
25. Brief Facts of the Case: Shri Deepak Gupta (hereinafter referred to as the Complainant) has filed
this complaint against the decision of Star Health and Allied Insurance Company Ltd. (hereinafter
referred to as the Insurers) alleging incorrect rejection of Mediclaim.
26. Cause of Complaint:
a) Complainant's Argument: The Insured had stated that he was admitted at Jain Surgical Clinic from
03.02.2021 to 05.02.2021for nausea, vomiting and fever. As the hospital was not in panel, he paid the money
and filed the reimbursement claim with the Insurance Company. Insurance Company rejected his claim, first
on the grounds of multiple tampering with hospital record and second on the ground that Covid protocols
were not followed. He requested the Insurance Company for reconsideration of claim. A surveyor came to
his house and enquired and took the documents from him but his claim was not settled. Then he approached
the Grievance Cell of the Insurance Company but there was no relief from GRO.
Case of Deepak Gupta versus Star Health and Allied Insurance Company Ltd.
Complaint Ref. No.: DEL-H-044-2122-0312
b) Insurer's Argument: The Insurance Company, vide Self Contained Note dated 24.08.2021, has stated
that the insured was admitted at Jain Surgical Clinic from 03.02.2021 to 05.02.2021 and was diagnosed
with Eneteric fever. On scrutiny of the submitted documents, it was observed that the indoor case
papers were written in the same handwriting/pen for all the days and there was no Doctor’s signature
in the discharge summary, IPD progress notes as well as in the first prescription. No Covid protocol
was followed and patient was admitted without COVID test. Further, it was also observed that there
was multiple tampering in indoor case records i.e. temperature reading in indoor case record and
discharge summary was different. Thus there was discrepancy in the records, which amounts to
misrepresentation. Hence, claim was repudiated as per Condition No.6 of the Policy, “Disclosure to
information norms” & Condition No.9 relating to “Fraud”.
19. Reason for registration of Complaint: Rejection of Mediclaim as stated in para 18 (a) above.
20. The following documents were placed for perusal:
a) Copy of policy.
b) Copy of GRO Letter, discharges summary, bill, claim form, rejection letter.
c) SCN of the Insurers along with enclosures.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to settle the claim for hospitalization of one day and full reimbursement
for medicines and tests (CT etc.) as per the reasonable & customary clause. The Complainant accepts
this offer. Thus an agreement of conciliation could be arrived at between the Complainant and the
Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall settle the claim for hospitalization of
one day and full reimbursement for medicines and tests (CT etc.) as per the reasonable & customary
clause.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 06, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Harinder Kumar Dandora versus The United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-2122-0308
1.
Name & Address of the Complainant
Shri Harinder Kumar Dandora
19/6, 1
st
Floor, Old Rajinder Nagar, New Delhi-110060
2.
Policy No.
Type of Policy
Policy term/policy period
0216002819P105856699
Individual Health Insurance Policy
09.08.2019 to 08.08.2020
3.
Name of the insured
Name of the policy holder
Harinder Kumar Dandora
Harinder Kumar Dandora
4.
Name of insurer
The United India Insurance Company Ltd.
5.
Date of repudiation
25.01.2021
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
30.07.2021
8.
Nature of complaint
Non settlement of Mediclaim
9.
Amount of claim
Rs.1,97,114/-
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
12.
Amount of relief sought
Rs.1,97,114/-
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims by
an Insurer
14.
Date of hearing
06.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
1. Shri Harinder Kumar Dandora, the Complainant
2. Smt. Savita Dandora, w/o the Complainant
For the Insurer
Smt. Disha Maladkar, AO, DO-16, Mumbai
16.
Date of Award/Order
Recommendation under Rule 16/ 06.09.2021
27. Brief Facts of the Case: Shri Harinder Kumar Dandora (hereinafter referred to as the Complainant)
has filed this complaint against the decision of The United India Insurance Company Ltd. (hereinafter
referred to as the Insurers) alleging wrong rejection of Mediclaim.
28. Cause of Complaint:
b) Complainant's Argument: The Complainant was hospitalized in Sir Ganga Ram Hospital for treatment from
14.02.2020 to 22.02.2020. He filed the reimbursement claim for Rs.1,97,114/- towards hospitalization, with
the Insurers as the hospital was not on cashless. After discharge from the hospital and before filing docu-
ments with the Insurance Company, original documents were lost when he was going to the doctor. Later on
he submitted the duplicate bills, dully attested by the Hospital. Further, as desired by the Insurers, he lodged
the FIR and submitted the indemnity bond and completed all the formalities as told to him but the Insurers
rejected his claim. He approached the Grievance Cell of the Insurers but his claim was not settled.
Case of Harinder Kumar Dandora versus The United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-2122-0308
b) Insurer's Argument: The Insurers, vide its Self Contained Note dated 17.08.2021, has stated that the
Complainant has taken the Individual Health Policy – Gold for the period 09.08.2019 to 08.08.2020
for Sum Insured of Rs.5 lakh. After scrutiny of the documents, the TPA informed that the documents
submitted in support of the claim were not original. Further, the insured failed to submit the required
documents in prescribed time limit under the policy. Hence, claim was not payable as per Clause 5.6.6
of policy terms and conditions. Clause 5.6.6 stated that “the insured person shall obtain and furnish to
the TPA with all original bills, receipts and other documents upon which a claim is based and shall also
give the TPA/company such additional information and assistance as the TPA/Company may require
in dealing with the claim including an authorization to obtain Medical and other records from the
hospital, lab, etc.”
19. Reason for registration of Complaint: Rejection of Mediclaim as stated in para 18 (a) above.
21. The following documents were placed for perusal:
d) Copy of policy.
e) Copy of GRO Letter, discharge summary, bill, claim form, rejection letters.
f) SCN of the Insurers along with enclosures.
22. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage the Insurers offer to settle the claim as per the terms and conditions of the policy, based on
the copies of the documents submitted by the Complainant. The Complainant accepts this offer. Thus
an agreement of conciliation could be arrived at between the Complainant and the Insurers, which I
consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall settle the claim as per the terms and
conditions of the policy, based on the copies of the documents submitted by the Complainant.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 06, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Mukesh Kumar Goyal versus Care Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-037-2122-0311
1.
Name & Address of the Complainant
Shri Mukesh Kumar Goyal,
240-A, Vijay Nagar, Bawana, Delhi-110039
2.
Policy No.
Type of Policy
Policy term/policy period
11857973
Religare Health Insurance
21.12.2019 to 20.12.2020
3.
Name of the insured
Name of the policy holder
Santosh Devi
Mukesh Kumar Goyal
4.
Name of insurer
Care Health Insurance Company Ltd.
5.
Date of repudiation
22.01.2021
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
10.08.2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of claim
Rs.383941/-
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
12.
Amount of relief sought
Rs.383941/-
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims by
an Insurer
14.
Date of hearing
06.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
Shri Mukesh Kumar Goyal, the Complainant
For the Insurer
Dr. Nisha Sharma, Corporate Manager (Health Claims)
16.
Date of Award/Order
Award under Rule 17/ 06.09.2021
17Brief Facts of the Case: Shri Mukesh Kumar Goyal (hereinafter referred to as the Complainant) has
filed this complaint against the decision of Care Health Insurance Company Ltd. (hereinafter referred
to as the Insurers) alleging wrong rejection of Mediclaim.
18.Cause of Complaint:
c) Complainant's Argument: The Complainant had stated that his mother, Smt. Santosh Devi, was admitted in
hospital on 23.10.2020 due to heart related problem. The Insurance Company rejected the claim on the ground
of PED. Although his mother was Diabetic, which was declared at the time of taking the policy but she was not
having any heart related problem. Further, nothing was mentioned about the duration of PED in the policy
documents. He approached the Grievance Cell of the Insurance Company also but his claim was not settled.
Now, he approached this forum for relief.
d) Insurer's Argument: The Insurers, vide Self Contained Note dated 03.09.2021, have stated that Smt. Santosh Devi
was admitted in National Heart Institute from 23.10.20 to 29.10.20 with complaint of giddiness and generalized
weakness for the last 5-6 days and finally diagnosed with hypertensive urgency, NSVT, DCMP EF=36%, Post AICD,
Mild MR, DM type – 2, Systematic hypertension. Same observations were made in Discharge Summary dt.
29.10.20 as well as in Patient Care Chart dt. 23.10.20. Further, the Face sheet of Cardiac clinic of hospital also
proves that insured had a risk factor of diabetic. Hence based on the said observations it was proved that the
captioned ailment was attributable to “pre-existing disease of Diabetes” for which 48 months waiting period was
applicable in the policy. Hence the claim was denied in accordance to clause 4.1(iii) and clause 1.58 pertaining to
“Waiting period/PED” of the policy terms and conditions.
19. Reason for registration of Complaint: Rejection of Mediclaim as stated in para 18 (a) above.
22. The following documents were placed for perusal:
g) Copy of policy.
h) Copy of GRO Letter, discharges summary, bill, claim form, rejection letters, query letter.
i) SCN of the Insurers along with enclosures.
23. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant had taken the Policy on 21.12 2017 for one year and renewed it annually. This claim
relates to the hospitalization of his mother from 23.10.2020 to 29.10.2020. The Insurers had issued a
letter to the Complainant on 03.01.2018 informing that the premium for the policy was being revised in
view of the PED of diabetes of his mother and HTN of his father and also informed him that the PED
coverage would be subject to the policy terms & conditions (T&C). The Complainant states that he did
not receive the detailed policy T&C. However, as he has been having the policy since 2017 and had
renewed it from time to time and had also received the aforesaid letter dated 03.01.2018 from the Insurers,
it was for him to have secured the full T&C from the Insurers.
In these circumstances, the Insurers were justified in holding that the illness of the insured was directly
relatable to her PED of diabetes and thus subject to the waiting period of 48 months vide Clause 4.1(iii)
read with clause 1.58, and repudiating the claim accordingly. Pursuantly, the complaint will deserve
rejection.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 06, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Atul Seth versus Care Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-037-2122-0324
1.
Name & Address of the Complainant
Shri Atul Seth
A-1/321, Sushant Lok Phase II, Sector 55,
Gurugram (Haryana)- 122001
2.
Policy No.
Type of Policy
Policy term/policy period
17335246
Religare Health Insurance
24.04.2020 to 23.04.2021
3.
Name of the insured
Name of the policy holder
Kailash Nath Seth
Kailash Nath Seth
4.
Name of insurer
Care Health Insurance Company Ltd.
5.
Date of repudiation
25.02.2021
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
08.08.2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of claim
Rs.7,00,000/-
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
12.
Amount of relief sought
Rs.7,00,000/-
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims by
an Insurer
14.
Date of hearing
13.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
1. Ms Meeta Sarin, Nominee in the Policy
2. Shri Atul Seth, the Complainant
For the Insurer
Dr. Nisha Sharma, Corporate Manager (Health Claims)
16.
Date of Award/Order
Recommendation under Rule 16/ 13.09.2021
17.Brief Facts of the Case: Shri Atul Seth (hereinafter referred to as the Complainant) has filed this
complaint against the decision of Care Health Insurance Company Ltd. (hereinafter referred to as the
Insurers) alleging wrong rejection of Mediclaim of his father.

18.Cause of Complaint:
a) Complainant's Argument: The Complainant’s father Late Shri Kailash Nath Seth had taken the subject policy for
the period 24.04.20 to 23.04.21 with the remarks of Asthma indicated as preexisting and covered under the
policy as per the prescribed waiting period. His father developed breathlessness and on the advice of doctor, he
was admitted in the Max Hospital from 02.11.20 to 15.11.20 and diagnosed as for COAD with acute exacerbation,
ACS and CAD etc. Initially, The Insurers rejected the request for cashless on the ground of non-disclosure of
cardiac disease and later on the reimbursement claim was also rejected on the ground that the patient was
diagnosed with COAD with acute Exacerbation. Though Asthma has been marked as pre-existing and any pre-
existing disease comes under the four years waiting period but there is huge difference between the symptoms
and treatment of Asthma and Chronic Obstructive Pulmonary Disease (COPD). He approached the Grievance
Cell of the Company but the claim was not settled.
b) Insurer's Argument: The Insurance Company, vide Self Contained Note dated 30.08.21, has stated
that the patient had taken the Insurance Policy from 24.04.20 to 23.04.21 for Sum Insured of Rs.5 lakh.
As insured had disclosed the pre-existing history of Asthma, the same was marked as “Pre-existing
Disease” in the policy. Initially insured filed a cashless claim request for the hospitalization from
02.11.20 at Max Hospital for the chief complaints of breathlessness and was diagnosed for COAD with
acute exacerbation. Accordingly, query letter dated 03.04.20 & 04.11.20 were sent to provide the exact
duration and past history of the present ailment with first consultation paper. After evaluation of the
claim documents, it was observed that as per the discharge summary of Max Hospital dated 15.11.20,
patient was diagnosed with COAD with acute exacerbation, acute kidney injury etc. Further, as per
the Audio-Video recording made during the examination of the claim, daughter of the insured stated
that the insured was suffering from heart ailment for last 3 years which was not disclosed during the
inception of the policy. Since the mentioned hospitalization of the insured was for the treatment of
pre-existing disease of Asthma, wherein 4 years waiting period was applicable, the claim was
repudiated in accordance to clause 4.1 (iii) & 7.1 of the policy terms & conditions.
19. Reason for registration of Complaint: Rejection of Mediclaim as stated in Para 18 (a) above.
20.The following documents were placed for perusal:
j) Copy of policy.
k) Discharge summary, bills, claim form, authority letter, Dr. Certificate, rejection letter.
l) SCN of the Insurer along with enclosures.
21. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to make a payment of Rs. 4.50 lakh to the nominee in full and final
settlement of the claim. The Complainant accepts this offer. Thus an agreement of conciliation
could be arrived at between the Complainant and the Insurers, which I consider as fair and
reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall make a payment of Rs. 4.50 lakh
to the nominee in full and final settlement of the claim.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 13, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ashok Kumar Kainth Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0301
17.Brief Facts of the Case: Shri Ashok Kumar Kainth (hereinafter referred to as the Complainant) has
filed this complaint against the decision of The Oriental Insurance Company Ltd. (hereinafter referred to
as the Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
a) Complainant's Argument: The Complainant was hospitalized in Max Healthcare Hospital from
21.08.2020 to 25.08.2020 for treatment of coronary artery disease and incurred Rs. 441454/. He filed
reimbursement claim of Rs. 461738/- against hospitalization and pre-post charges. Insurers denied his
claim stating that “all pre-existing disease are excluded up to 36 months of the policy being in force
without any break.” He was having policy continuously from 2005 and from 05.07.2016 to 14.05.2018,
he was in Canada and for that he had taken policy from Canada. He had submitted all policies and
documents /information asked by Oriental/TPA, but Insurance Company rejected the claim. He wrote to
GRO on 31.07.2021 but did not get the claim. Therefore, he has now approached this forum for relief.
Case of Ashok Kumar Kainth Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0301
1.
Name & Address of the Complainant
Shri Ashok Kumar Kainth
3397/1, Desh Bandhu Gupta Road, Karol Bagh,
New Delhi-110005
2.
Master Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
272900/48/2021/5874
PNB-Oriental Mediclaim Policy-2017
20.06.2020 To 19.06.2021
3.
Name of the insured
Name of the policy holder
Ashok Kumar Kainth
Ashok Kumar Kainth
4.
Name of the insurer
The Oriental Insurance Company Ltd.
5.
Date of repudiation
08.01.2021
6.
Reason for repudiation
As per Exclusion Clause-4.1 – All pre-existing diseases are
excluded up to 36 months of the policy being in force
7.
Date of receipt of the complaint
17.03.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 461738/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs 461738/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
14.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Ashok Kumar Kainth, the Complainant
For the insurer
Smt. Updesh Kaur, Admin. Officer, DO-29, New Delhi
16.
Date of Award/Order
Award under Rule 17/ 14.09.2021
b) Insurer's Argument: The Insurers in their SCN dated 03.09.2021 have stated that the complainant was
admitted in Max Healthcare Hospital from 21.08.2020 to 25.08.2020 for treatment of Coronary Artery
disease. Insurers received reimbursement claim of Rs. 461738/- inclusive pre & post expenses. On scru-
tinizing the claim documents, it was found that insured was a known case of pre-diabetes, CAD, history
of Coronary Intervention to left anterior descending artery in 2014, prior to policy inception date. There-
fore, claim was denied under policy exclusion clause-4.1 which states that all pre-existing disease are
excluded up to 36 months of policy being in force. Pre-existing disease shall be covered only after the
policy has been continuously in force for 36 months provided the renewals have been continuous and
without break in policy period. Insured had also not declared in proposal form about his pre-existing
health condition while taking the policy, which is case of concealment of material facts and misrepre-
sentation of facts. This is violation as per policy condition 5.1. Hence Insurers have rightly repudiated
the claim.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
a) Discharge Summaries
b) Repudiation Letter
c) GRO
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The subject policy was first issued on 21.06.2018 for one year and then renewed annually. The subject
claim relates to hospitalization from 21 to 25.08.2020, which was in the third year of the Policy. The
Insurers while processing the claim observed that the Complainant had undergone heart surgery (Stent) in
2014, as mentioned in the Discharge Summary also. As per Exclusion Clause 4.1, all pre-existing diseases,
whether declared on not declared, are excluded up to 36 months from the date of inception of the policy.
Therefore, the Insurers were justified in repudiating the claim. Pursuantly, the complaint shall deserve to
be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 14, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Radhey Shyam Gupta Versus The Max Bupa Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-031-2122-0302
17.Brief Facts of the Case: Shri Radhey Shyam Gupta(hereinafter referred to as the Complainant) has
filed this complaint against the decision of The Max Bupa Health Insurance Company Ltd. (hereinafter
referred to as the Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
c) Complainant's Argument: The Complainant stated that he was hospitalized in Max Healthcare Hospital,
Delhi from 06.03.2021 to 11.03.2021 for the treatment of Fracture Neck of Femur left. Cashless request was
denied by the Insurance Company with reason of non-disclosure of medical history of pre-existing disease.
After discharge, complainant filed reimbursement claim of hospitalization expenses for Rs. 333613/-. Insur-
ers repudiated the claim and sent policy cancellation notice on dated 13.03.2021 stating that there has been
misrepresentation or mis-description of material facts. Complainant submitted clarification to Max
Healthcare that the patient underwent surgery of left cemented bipolar Hemiarthroplasty and had no history
of COPD, heart block or LAD and was not on regular medication for the same. Complainant wrote to GRO
on 16.3.2021, but Insurers again rejected the claim with the same reason. He has now approached this forum
for relief.
Case of Radhey Shyam Gupta Versus The Max Bupa Health Insurance Company Ltd.
1.
Name & Address of the Complainant
Shri Radhey Shyam Gupta
L-15, Naveen Shahdara, Delhi-110032
2.
Master Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
31421762202000
Max Bupa Health Insurance Policy
29.07.2020 To 28.07.2021
3.
Name of the insured
Name of the policy holder
Radhey Shyam Gupta
Radhey Shyam Gupta
4.
Name of the insurer
The Max Bupa Health insurance Company Ltd.
5.
Date of repudiation
13.03.2021
6.
Reason for repudiation
Non-disclosure of Pre-Existing Disease
7.
Date of receipt of the complaint
11.06.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 334413/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 324413/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
14.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
1. Shri Radhey Shyam Gupta, the Complainant
2. Smt. Pushpanjali Bindal, D-i-L of the Complainant
For the insurer
Shri Bhuwan Bhashker, Manager (Legal)
16.
Date of Award/Order
Award under Rule 17/ 14.09.2021
Complaint Ref. No.: DEL-H-031-2122-0302
d) Insurer's Argument: The Insurers in their SCN dated nil have stated that the complainant was hospitalized
in Max Super Specialty Hospital from 06.03.2021 to 11.03.2021 for the treatment of Per trochanteric fracture.
Cashless request was received for pre-authorization which was denied on the basis of patient’s adverse med-
ical condition and non-disclosure of material facts of diseases COPD since 2 years, and LAD Block since
29.03.2020. Complainant filed reimbursement claim of Rs. 343565/-. To know the veracity of claim, insurers
appointed an investigator to investigate the claim. During investigation it was found that patient had history
of pre-existing diseases, which was not disclosed at the inception of policy. Therefore, it is a non-disclosure
of material facts, hence claim was repudiated as per terms and conditions of the policy.
19. Reason for registration of Complaint: Repudiation of Mediclaim.
20. The following documents were placed for perusal:
d) Discharge Summary
e) Repudiation Letter
f) GRO
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant had taken the subject policy through online porting in October 2020. He states that he had
given his PED details to the agent on WhatsApp and if these details were not recorded in the Policy Proposal
Form, the fault did not lie with the Complainant. The Insurers state that Proposal Form was sent along with
the Policy Bond and it was expected of the Complainant to have reviewed the same carefully and got the errors,
if any, corrected suitably.
Upon examination of the arguments and the evidence submitted by both the parties, it is concluded that the
Complainant had a history of pre-existing diseases, which he did not disclose at the inception of policy.
Therefore, the Insurers were justified in repudiating the claim and cancelling the Policy. Pursuantly, the
complaint shall deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 14, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ravinder Singh Versus The Max Bupa Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-031-2122-0303
17.Brief Facts of the Case: Shri Ravinder Singh (hereinafter referred to as the Complainant) has filed
this complaint against the decision of The Max Bupa Health Insurance Company Ltd. (hereinafter referred
to as the Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
e) Complainant's Argument: The Complainant stated that he was admitted in Max Health Hospital, New Delhi
for the treatment and surgery for removal of multiple calculi in kidney and Gall bladder. But complainant
came to know that the Max Bupa Insurance Company had de-paneled the hospital and he was advised by
Insurance agent and Insurance Company to go to any other hospital. Complainant had to make the payment
of bills and could not go to any other hospital for lack of fund. The behavior of agent and Insurance Company
left him in a vulnerable situation to take incomplete treatment and complainant had to suffered extreme pain
and was harassed by Insurance Company to whom he was paying premium. Complainant filed reimbursement
claim of Rs. 31832/-, which was rejected by the Insurance Company stating that hospitalization less than 24
hours. He wrote to GRO on 13.03.2021 but did not get the claim. Therefore, he has now approached this
forum for relief.
Case of Ravinder Singh Versus The Max Bupa Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-031-2122-0303
b) Insurer's Argument: The Insurers in their SCN dated nil have stated that the insured admitted in Max
1.
Name & Address of the Complainant
Shri Ravinder Singh
6-A, Adhchini, Sri Aurobindo Marg, New Delhi-110017
2.
Master Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
30517288202004
Max Bupa Health Insurance Policy
11.04.2020 To 10.04.2021
3.
Name of the insured
Name of the policy holder
Ravinder Singh
Ravinder Singh
4.
Name of the insurer
The Max Bupa Health insurance Company Ltd.
5.
Date of repudiation
23.02.2021
6.
Reason for repudiation
Hospitalization less than 24 hours, hence claim denied as
per Clause-10.37
7.
Date of receipt of the complaint
09.07.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 31832/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 1656832/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
14.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Ravinder Singh, the Complainant
For the insurer
Shri Bhuwan Bhashker, Manager (Legal)
16.
Date of Award/Order
Award under Rule 17/ 14.09.2021
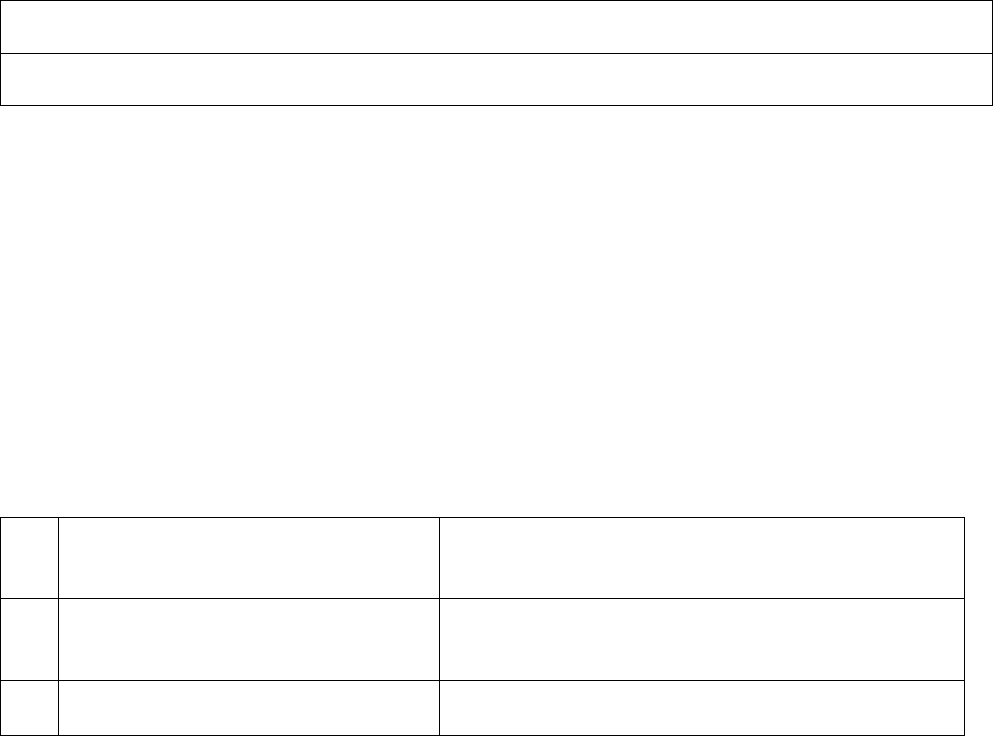
Healthcare hospital on 08.08.2020 for the treatment of severe pain in stomach due to multiple calculi in Gall
bladder and kidneys diagnosed during test and investigation conducted in hospital. Insurers received
reimbursement claim of Rs. 31832/-. On scrutinizing the claim documents, it was found that hospitalization
of insured was for less than 24 hours, hence claim was denied as per clause 10.37 of the policy. Therefore,
claim has rightly been repudiated as per terms and conditions of the policy.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
g) Discharge Summary
h) Repudiation Letter
i) GRO
21.Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant was admitted in Max Hospital on 08.08.2021 at 06.42 am with complaint of abdominal
pain and discharged the same day at 11.41 am. i.e. within 5 hours. The Discharge Summary records his
ailments as Left Ureteric Calculi, Cholelithiasis. The Complainant states that he was informed by the agent
that this hospital was not on the panel of the Insurers and therefore he himself got discharged. The Insurers
state that the Hospital was very much on their panel.
Upon examination of the arguments and the evidence submitted by both the parties, it is concluded that the
hospitalization was for less than 24 hours, and this treatment was not in the list of admissible daycare
procedures and, therefore, the Insurers were justified in repudiating the claim. Pursuantly, the complaint
shall deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 14, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Bijendra Singh versus Star Health and Allied Insurance Company Ltd.
Complaint Ref. No.: DEL-H-044-2122-0315
1.
Name & Address of the Complainant
Shri Bijendra Singh
B-11, 1
st
Floor, Ashok Enclave Part 2, Sector 37,
Amarnagar P.O., Faridabad-121003 (Haryana)
2.
Policy No.
Type of Policy
Policy term/policy period
P/161100/01/2020/028310
Family Health Optima Insurance Plan
03.03.2020 to 02.03.2021
3.
Name of the insured
Name of the policy holder
Bijendra Singh
Bijendra Singh
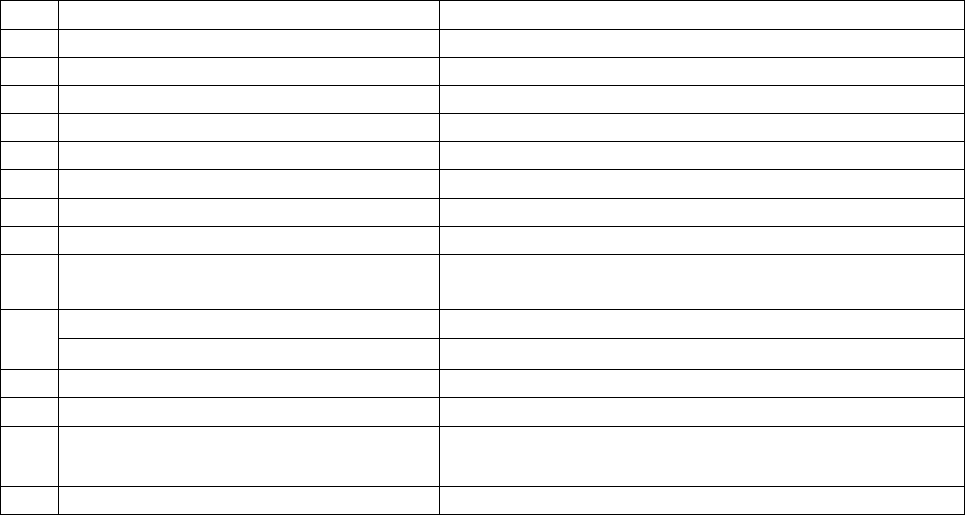
4.
Name of insurer
Star Health and Allied Insurance Company Ltd.
5.
Date of inadequate settlement
02.07.2021
6.
Reason for grievance
Inadequate settlement of Mediclaim
7.
Date of receipt of the complaint
19.08.2021
8.
Nature of complaint
Inadequate settlement of Mediclaim
9.
Amount of claim
Rs.143998/-
10.
Date of partial settlement
Cashless settlement
11.
Amount of partial settlement
Rs.115596/-
12.
Amount of relief sought
Rs.28402/- as per Form VI A
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims
by an Insurer
14.
Date of hearing
15.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
Shri Bijendra Singh, the Complainant
For the Insurer
1. Dr. Madhukar Pandey, Chief Manager (Health Claims)
2. Shri Mantosh Kumar, Senior Manager (Claims)
16.
Date of Award/Order
Recommendation under Rule 16/ 15.09.2021
17.Brief Facts of the Case: Shri Bijendra Singh (hereinafter referred to as the Complainant) has filed
this complaint against the decision of Star Health and Allied Insurance Company Ltd. (hereinafter
referred to as the Insurers) alleging inadequate settlement of Mediclaim.
18.Cause of Complaint:
e) Complainant's Argument: The Complainant had stated that he was admitted in Indraprastha Apollo Hospital
from 08.02.2021 to 09.02.2021 for surgery of Fissure. Hospital sent a claim of Rs.143998/- out of which an
amount of Rs.115596/- was settled by the Insurance Company. After that he sent pre & post treatment claim
of Rs.42156/- (including short payment of Rs.28402/-) out of which a sum of Rs.10037/- was settled by the
Insurance Company. Thus an amount of Rs.32119/- (Rs.28402/- + Rs.3717/-) was deducted. He approached
the Grievance Cell of the Insurance Company but his balance claim was not paid.
f) Insurer's Argument: The Insurance Company, vide its Self Contained Note dated 07.09.2021, has stated
that the insured was admitted in Indraprastha Apollo Hospital from 08.02.2021 to 09.02.2021 and was di-
agnosed with Severe Anal spasm + Fissure in Ano + Internal Haemorrhoids + Perineal nodule. The insured
submitted a Pre authorization request for cashless treatment on 16.12.2020 and the same was initially ap-
proved for a sum of Rs.70000/- against estimated amount of Rs.193000/-. Subsequently the insured sub-
mitted an enhancement request on Pre authorization on 09.02.2021 and the same was enhanced for a
sum of Rs.115596/-. The insured submitted a reimbursement claim for Pre-Post hospitalization expenses of
Rs.42156/- on 27.02.2021, out of which a sum of Rs.10037/- was approved on 02.03.2021. Again the in-
sured submitted a Pre-post reimbursement claim of Rs.7603/- on 27.02.2021. A sum of Rs.2958/- was ap-
proved on 26.04.2021 and Rs.4297/- on 18.05.2021. The total claim was settled for Rs. 115596/- towards
hospitalization expenses in cashless facility and subsequently Rs.17292/- (Rs.10037 + Rs.2958 + Rs.4297)
towards hospitalization expenses in reimbursement for the above claim. Hence, maximum amount was al-
ready settled to the insured as per the terms and conditions of the policy and the detail of deductions
made towards main hospitalization as well as for pre-post hospitalization expenses were informed to the
insured accordingly.
19. Reason for registration of Complaint: Inadequate settlement of Mediclaim.
20.The following documents were placed for perusal.
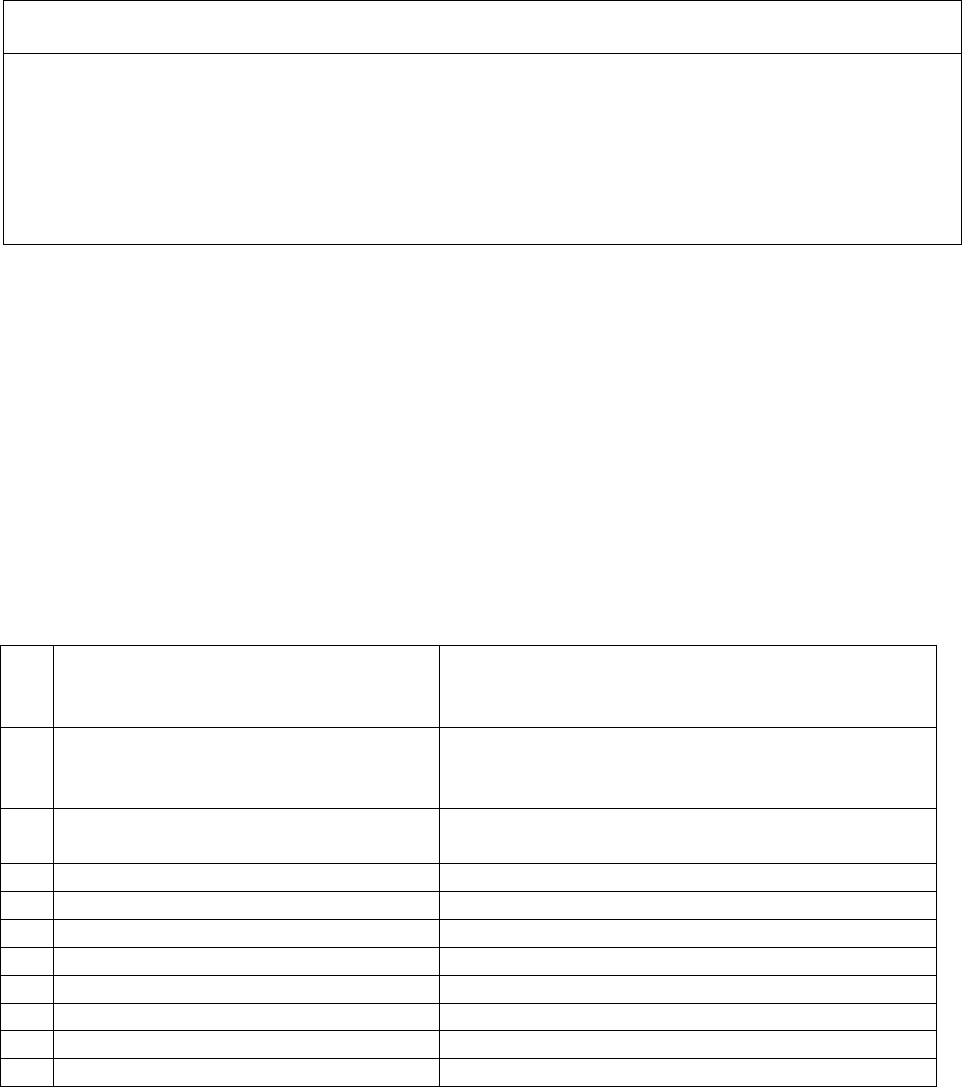
m) Copy of policy.
n) Discharge summary, bills, settlement letter.
o) SCN of the Insurer along with enclosures.
21.Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to pay Rs. 18,000 in full and final settlement of the balance claims
relating to hospitalization of 08-09 January 2021. The Insurers also offer to examine the balance claims
relating to pre- and post-hospitalization and settle the same as per the terms & conditions of the Policy.
The Complainant accepts this offer. Thus an agreement of conciliation could be arrived at between the
Complainant and the Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the Complainant
and the Insurers. Accordingly, the Insurers shall pay Rs. 18,000 in full and final settlement of the balance
claims relating to hospitalization of 08-09 January 2021. The Insurers shall also examine the balance claims
relating to pre- and post-hospitalization and settle the same as per the terms & conditions of the Policy.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 15, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Manish Sharma versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0359
1.
Name & Address of the Complainant
Shri Manish Sharma
2264/172, Ganesh Pura, Tri Nagar,
New Delhi-110035
2.
Policy No.
Type of Policy
Policy term/policy period
360305501910005905
Parivar Mediclaim Policy
05.03.2020 to 04.03.2021
3.
Name of the insured
Name of the policy holder
Manish Sharma
Manish Sharma
4.
Name of insurer
The National Insurance Company Ltd.
5.
Date of repudiation
27.01.2021
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
09.08.2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of claim
Rs.54095/- as per Form VIA
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
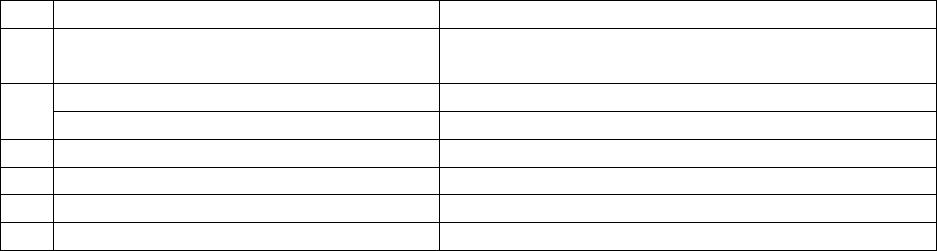
12.
Amount of relief sought
Rs.54095/- as per Form VIA
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of
claims by an Insurer
14.
Date of hearing
22.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx
15.
Representation at the hearing
For the Complainant
Shri Manish Sharma, the Complainant
For the Insurer
Shri Govind Lal, Admin. Officer, DA Br., Punjabi Bagh
16.
Date of Award/Order
Award under Rule 17/ 22.09.2021
17.Brief Facts of the Case: Shri Manish Sharma (hereinafter referred to as the complainant) has filed
the complaint against the decision of The National Insurance Company Ltd. (hereinafter referred to
as the Insurers or the Respondent Insurance Company) alleging wrong rejection of Mediclaim.
18.Cause of Complaint:
a) Complainant's Argument: The Complainant had stated the he made two claims for Injection Rituximab for
Rs.54095/-. Further he stated that he was patient of Acquired homophiles. Doctor prescribed him for In-
jection Rituximab in Govt. Hospital AIIMS and that was not immunotherapy. Insurance Company rejected
his claim by giving irrelevant reasons whereas his claim was genuine. He approached the Grievance Cell of
the Insurance Company but his claim was not settled.
b) Insurer's Argument: The Insurance Company, vide Self Contained Note dated 15.09.2021, has
stated that on scrutiny of the documents, it was observed that the patient availed treatment in
AIIMS Hospital with the diagnosis of ‘Acquired Hemophilia (FVIII INH) & underwent “Rituxi-
mab Therapy”. The Complainant has lodged 2 claims for treatment of Acquired Hemophilia &
underwent Rituximab Therapy on 17.03.2020 & 01.04.2020 on Short admission basis in AIIMS,
New Delhi. The hospitalization was solely for Immunotherapy, which on a standalone basis does
not require hospitalization and was not listed in the day care procedure annexed at appendix 1 of
the policy. Hence the claim was repudiated as per Policy Clause No. 3.11 and list of Day Care
Procedure Appendix 1.
19. Reason for registration of Complaint: Rejection of Mediclaim as stated in para 18 (a) above.
23. The following documents were placed for perusal.
p) Copy of policy.
q) Copy of GRO Letter, discharge summary, bills, rejection letters.
r) SCN of the Insurer along with enclosures.
24. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
I have examined the arguments and the evidence submitted by both the parties. The Complainant
had lodged two claims for treatment of Acquired Hemophilia and underwent Rituximab Therapy
on 17.03.2020 & 01.04.2020 on Short-admission basis in AIIMS, Delhi. The Insurers had
determined that the hospitalization was solely for immunotherapy, which on a standalone basis does
not require hospitalization and was not listed in the admissible day care procedures listed in
Appendix 1 of the policy. There was error on the part of the Insurers in arriving at this determination.
Hence the claims were rightly repudiated as per Policy Clause No. 3.11 read with the list of
admissible Day Care Procedures vide Appendix 1. Pursuantly, the complaint shall deserve to be
rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 22, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Sandeep Saxena versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0421
1.
Name & Address of the Complainant
Shri Sandeep Saxena
151, Vigyapan Lok Apartments, Mayur Vihar Extension
Phase-1, Delhi-110091
2.
Policy No.
Type of Policy
Policy term/policy period
360801502010004633
National Parivar Mediclaim
16.11.2020 to 15.11.2021
3.
Name of the insured
Name of the policy holder
Namita Kapoor Saxena
Sandeep Saxena
4.
Name of insurer
The National Insurance Company Ltd.
5.
Date of repudiation
N.A.
6.
Reason for grievance
Inadequate settlement of Mediclaim
7.
Date of receipt of the complaint
03.09.2021
8.
Nature of complaint
Inadequate settlement of Mediclaim
9.
Amount of claim
Rs.1,12,857
10.
Date of partial settlement
16.06.2021
11.
Amount of partial settlement
Rs.70,634
12.
Amount of relief sought
Rs.42,223
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims by
an Insurer
14.
Date of hearing
22.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
Shri Sandeep Saxena, the Complainant
For the Insurer
Shri Puneet Bhatia, Divisional Manager, DO-34
16.
Date of Award/Order
Recommendation under Rule 16/ 22.09.2021
29. Brief Facts of the Case:
Shri Sandeep Saxena (hereinafter, ‘the Complainant’) has filed this complaint against the decision of
The National Insurance Company Ltd. (hereinafter ‘the Insurers’) alleging inadequate settlement of
Mediclaim.
30. Cause of Complaint:
c) Complainant's Argument: The Complainant had stated that his wife Smt. Namita Kapoor was admitted in
Bansal Hospital from 01.05.2021 to 03.05.2021 for the treatment of COVID-19 Pneumonia. He applied for
the reimbursement of claim for Rs.1,12,857/- but Insurance Company reimbursed only Rs.70,634/-with a

deduction of Rs.42,223/- citing Government guidelines. He approached the Grievance Cell of the Insurance
Company but his balance claim was not settled.
Case of Sandeep Saxena versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0421
d) Insurer's Argument: The Insurance Company, vide Self Contained Note has stated that the patient
Smt. Namita was admitted in Bansal Hospital, Delhi on 01.05.2021 with complaints of Generalised
weakness, shortness of breath, Ghabrahat, Dry cough, low grade fever, dry mouth, and was diag-
nosed with Covid-19 pneumonia. She was discharged on 03.05.2021, after hospitalization for 2 days.
The reimbursement claim was approved and paid for Rs.70,634/- on 21.06.2021 as per circular
dated 20.06.2020 issued by the Govt. of National Capital Territory of Delhi. A sum of Rs.42,223/-
was deducted towards non-payable items and deduction details were informed to the Complainant.
Hence, claim was paid as per Policy clause 6.42 of Reasonable and Customary charges, circular of
Govt. of National Capital Territory of Delhi and Table of Benefits limit for ambulance charges.
31. Reason for registration of Complaint: Inadequate settlement of Mediclaim.
24. The following documents were placed for perusal:
s) Copy of policy.
t) Copy of GRO Letter, Discharge summary, hospital bills, claim form, settlement details.
u) SCN of the Insurer along with enclosures.
25. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to make payment for Pharmacy charges (Rs. 11163), Lab Tests
charges (Rs. 19316), and Physiotherapy charges (Rs. 1491), totaling to Rs. 31970, in full and final
settlement of the balance claim. The Complainant accepts this offer. Thus an agreement of
conciliation could be arrived at between the Complainant and the Insurers, which I consider as fair
and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall make a payment of Rs. 31,970,
as noted above, to the Complainant in full and final settlement of the balance claim.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 22, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Seema Gupta versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0357
1.
Name & Address of the Complainant
Smt. Seema Gupta
G-23/278, Sector-7, Rohini, Delhi-110085
2.
Policy No.
Type of Policy
Policy term/policy period
360400502010000170
Parivar Mediclaim
15.04.2020 to 14.04.2021
3.
Name of the insured
Name of the policy holder
Seema Gupta
Seema Gupta
4.
Name of insurer
The National Insurance Company Ltd.
5.
Date of inadequate settlement
09.03.2021
6.
Reason for grievance
Inadequate settlement of Mediclaim
7.
Date of receipt of the complaint
16.08.2021
8.
Nature of complaint
Inadequate settlement of Mediclaim
9.
Amount of claim
Rs.78831/-
10.
Date of partial settlement
-----
11.
Amount of partial settlement
Rs.65165/-
12.
Amount of relief sought
Rs.13666/-
13.
Complaint registered under Rule No. of the
Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of
claims by an Insurer
14.
Date of hearing
22.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
1. Smt. Seema Gupta, the Complainant
2. Shri Arjun Gupta, s/o the Complainant
For the Insurer
Shri Puneet Kanoria, Sr. Divl Manager DO-9, Rohini
16.
Date of Award/Order
Recommendation under Rule 16/ 22.09.2021
32. Brief Facts of the Case:
Smt. Seema Gupta (hereinafter referred to as the complainant) has filed the complaint against the
decision of The National Insurance Company Ltd. (hereinafter referred to as the Insurers) alleging
inadequate settlement of Mediclaim.
33. Cause of Complaint:
e) Complainant's Argument: The Complainant was admitted at Shree Aggarsain International Hospital from
26.02.2021 to 06.03.2021. Hospital bill was for Rs.78831/- but Insurance Company settled the bill for Rs.
65165/-. She paid a sum of Rs.13666/- to the hospital. After discharge she requested the Insurance Company
for balance claim but they did not pay the balance claim. She approached the Grievance Cell of the Company
but there was no relief.
Case of Seema Gupta versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0357
f) Insurer's Argument: The Complainant was admitted in Shree Aggarsain International Hospital
from 26.02.2021 to 06.03.2021 with complaints of Type 2 Diabetes Mellitus with Acute meningitis.
The claim was settled and a sum of Rs.13666/- was deducted for non-medical items. The Insurance
Company has carefully reviewed all the documents on record and observed that a further payment
of Rs.8536/- can be made as per policy terms and conditions. Further the Insurance Company gave
the detail of balance payment of Rs.5130/- (PPE Kit, examination gloves, dietician, admission
charges, medical evaluation etc.) which were not payable under the policy.
19. Reason for registration of Complaint: Inadequate settlement of Mediclaim.
25. The following documents were placed for perusal.
v) Copy of policy.
w) Copy of GRO Letter, discharge summary, bills, deductions mail.
x) SCN of the Insurer along with enclosures.
26. Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer (a) to pay an additional amount of Rs. 8536 as stated in Para 18b
above and another sum of Rs. 2000 towards the PPE Kit and (b) to write to the Hospital with copy
to the Complainant to explain to the Complainant the reasons for collection of the remaining amount
of Rs. 3130 and if there are no justification, refund the same to the Complainant. The Complainant
accepts this offer. Thus an agreement of conciliation could be arrived at between the Complainant
and the Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall (a) pay to the Complainant an
additional amount of Rs. 8536 as stated in Para 18b above and another sum of Rs. 2000
towards the PPE Kit and (b) write to the Hospital with copy to the Complainant to explain to
the Complainant the reasons for collection of the remaining amount of Rs. 3130 from her and
if there are no justification, refund the same to the Complainant.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 22, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Jitender Arora Versus The Max Bupa Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-031-2122-0366
17.Brief Facts of the Case: Shri Jitender Arora (hereinafter referred to as the Complainant) has filed
this complaint against the decision of the Max Bupa Health Insurance Company Ltd. (now Niva Bupa
Health Insurance Co. Ltd. and hereinafter referred to as the Insurers) alleging wrong repudiation of
Mediclaim.
18.Cause of Complaint:
f) Complainant's Argument: The Complainant stated that his mother Smt. Kiran Arora was infected with
Covid-19 positive and was hospitalized in UK Nursing Home, New Delhi from 07.04.2021 to 12.04.2021.
Hospitalization bill for expenses incurred was Rs. 143015/- for which complainant filed reimbursement
claim on Insurance Company. Insurance Company denied the claim stating that hospitalization was not
justified as per received medical documents. Complainant had submitted all documents Covid-19 positive
report, discharge summary and bills, etc. but claim was rejected vide letter dated 16.05.2021. He wrote to
GRO on 22.05.2021 but claim was denied for the same reason. Therefore, he has now approached his
forum for relief.
Case of Jitender Arora Versus The Max Bupa Health Insurance Company Ltd.
1.
Name & Address of the Complainant
Shri Jitender Arora
63/13, 2
nd
Floor, Front side, Ashok Nagar, Near Tilak Nagar
Metro Station, New Delhi-110018
2.
Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
30650791202104
Health Mediclaim Policy
27.03.2021 to 26.03.2022
3.
Name of the insured
Name of the policy holder
Kiran Arora
Jitender Arora
4.
Name of the insurer
The Max Bupa Health Insurance Company Ltd.
5.
Date of repudiation
16.05.2021
6.
Reason for repudiation
Hospitalization was not required as patient would have
been treated on Home isolation basis.
7.
Date of receipt of the complaint
03.08.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 143015/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 143015/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
28.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Jitender Arora,
For the insurer
Shri Bhashker Bhuwan, Manager (Legal)
16.
Date of Award/Order
Recommendation under Rule 16/ 28.09.2021
Complaint Ref. No.: DEL-H-031-2122-0366
g) Insurer's Argument: The Insurers in their SCN have stated that the complainant’s mother Smt. Kiran
Arora was admitted in UK Nursing Home, Delhi from 07.04.2021 to 12.04.2021 for treatment of Covid-
19. Complainant incurred Rs. 143015/- on treatment for which he filed reimbursement claim. On scruti-
nizing the claim documents, it was found that the admission in the hospital was not necessary as the vitals
were stable. As per discharge summary, SPO2 level- 97, Temperature-100, pulse rate 89/minute, which
clearly suggested that hospitalization was not required and the treatment could have been carried out on
Home Isolation basis. Therefore claim was rejected as per clause 6.15 of the policy terms and conditions.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
j) Discharge Summary
k) Repudiation Letter
l) GRO
21.Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers inform that they have offered to settle the claim for a sum of Rs. 1,41,365 in
full and final settlement. The Complainant states that he has received the offer and accepts the same.
Thus an agreement of conciliation could be arrived at between the Complainant and the Insurers, which
I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall pay to the Complainant a sum of Rs.
1,41,365 in full and final settlement of the claim.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 28, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Khairati Lal Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0344
17.Brief Facts of the Case: Shri Khairati Lal (hereinafter referred to as the Complainant) has filed
this complaint against the decision of The Oriental Insurance Company Ltd. (hereinafter referred to as
the Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
h) Complainant's Argument: His wife Smt. Veena Grover was hospitalized in Fortis Hospital, Delhi
from 13.11.2020 to 15.11.2020 for treatment of heart disease and hypertension. Cashless request was
sent from hospital on 13.11.2020 for estimated treatment cost of Rs. 291400/- but the same was denied
by TPA stating that the patient was admitted for heart disease & hypertension and there is waiting
period of Hypertension and related complications. Complainant had to pay bill of Rs. 284956/- on
discharge. Later, he filed reimbursement claim Rs. 284956/- along with Hospital certificate that patient
had no past history of DM. But Insurance Company rejected the claim with same reason. He wrote to
GRO on 26.07.2021 but did not get the claim. Therefore, he has now approached this forum for relief.
Case of Khairati Lal Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0344
1.
Name & Address of the Complainant
Shri Khairati Lal
B-199, 1st Floor, Gujaranwala Town, Part-I,
New Delhi-110009
2.
Master Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
272900/48/2020/17482
PNB-Oriental Mediclaim Policy-2017
03.01.2020 To 02.01.2021
3.
Name of the insured
Name of the policy holder
Veena Grover
Khairati Lal
4.
Name of the insurer
The Oriental Insurance Company Ltd.
5.
Date of repudiation
27.01.2021
6.
Reason for repudiation
As per Exclusion Clause-4.2(xvii) – Waiting period of
2 years from inception of policy
7.
Date of receipt of the complaint
02.03.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 284956/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 284586/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of
claims by an insurer
14.
Date of hearing/place
28.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Khairati Lal, the Complainant
For the insurer
Smt. Updesh Kaur, Admin. Officer, DO-29, Delhi
16.
Date of Award/Order
Award under Rule 17/ 28.09.2021
i) Insurer's Argument: The Insurers in their SCN dated 13.09.2021 have stated that the Complainant’s
spouse Veena Grover was admitted with acute AWMI, planned for CAG+PTCA, Stent to LAD, HTN.
Reimbursement claims of Rs. 284956/- was received on 01.12.2020 against hospitalization expenses
incurred during hospitalization from 13.11.2020 to 15.11.2020 in Fortis Hospital, Delhi. The claim
was denied as the policy was in first year and as certified by doctor that patient was hypertensive at
the time of admission, which is a risk factor/cause of heart related disease. As per Exclusion Clause
4.2(XVII) “the expenses on treatment of following ailments/diseases/surgeries, if contracted and/or
manifested after inception of first policy, are not payable during the waiting period of 02 years for
Hypertension. Hence cashless request and reimbursement claim was rejected as per terms and condi-
tions of the policy.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
m) Discharge Summary
n) Repudiation Letter
o) GRO
21.Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The subject policy was issued in January 2020. The claim relates to hospitalisation of the insured in
November 2020, which was the first year of the policy. The diagnosis included hypertension (HTN) and
heart related ailments. The policy prescribes a waiting period of two years for HTN. Therefore, the
Insurers were justified in repudiating the claim and, pursuantly, the complaint shall deserve to be
rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 28, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Kunal Bansal Versus Max Bupa Health Insurance Company Limited
Complaint Ref. No.: DEL-H-031-2122-0340
17.Brief Facts of the Case: Shri Kunal Bansal (hereinafter referred to as the Complainant) has filed
this complaint against the decision of Max Bupa Health Insurance Company Ltd. (now Niva Bupa
Health Insurance Co. Ltd. and hereinafter referred to as the Insurers) alleging inadequate settlement
of Mediclaim.
18.Cause of Complaint:
j) Complainant's Argument: The Complainant stated that his father was hospitalized in Surya Hospital,
Krishna Nagar, New Delhi, from 11.04.2021 to 20.04.2021 for treatment of viral pneumonitis and
Covid-19 as CT Score was 9/25 in HRCT Report. Hospitalization bill was of amount Rs. 108790/- for
which complainant filed reimbursement claim. Insurance Company approved Rs. 63490/- only and
deducted Rs. 45300/- stating that patient was not Covid-19 Positive, so isolation room charges Rs.
45000/- @ Rs.5000/- per day and Rs. 300/- registration charge were not payable. Complainant wrote
to GRO on 29.05.2021 but Insurance Company denied the claim for the same reason. Therefore, he
has now approached this forum for relief.
1.
Name & Address of the Complainant
Shri Kunal Bansal
45, Old Anarkali, Krishna Nagar, New Delhi-110051
2.
Policy No:/Certificate No.
Type of Policy
Duration of Policy/Policy Period
30511075202104
Mediclaim Insurance Policy
15.03.2021 To 14.03.2022
3.
Name of the insured
Name of the policy holder
Vijendra Bansal
Kunal Bansal
4.
Name of the insurer
Max Bupa Health Insurance Company Ltd.
5.
Date of repudiation
N.A.
6.
Reason for repudiation
N.A.
7.
Date of receipt of the complaint
02.07.2021
8.
Nature of complaint
Inadequate Settlement of Mediclaim
9.
Amount of claim
Rs. 108790/-
10.
Date of partial settlement
28.05.2021
11.
Amount of partial settlement
Rs. 63490/-
12.
Amount of relief sought
Rs. 45300/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims
by an insurer
14.
Date of hearing/place
28.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Kunal Bansal, the Complainant
For the insurer
Shri Bhashker Bhuwan, Manager (Legal)
16.
Date of Award/Order
Recommendation under Rule 16/ 28.09.2021
Case of Kunal Bansal Versus The Max Bupa Health Insurance Company Ltd.
Complaint Ref. No.: DEL-H-031-2122-0340
k) Insurer's Argument: The Insurers in their SCN dated nil have stated that the insured was admitted in
Surya Hospital, New Delhi for the treatment of viral pneumonitis. During hospitalization period from
11.04.2021 to 20.04.2021, complainant incurred Rs. 108790/- for which insurers filed reimbursement
claim. On securitizing and processing the claim, Insurance Company paid Rs. 63490/- on 28.05.2021
and disallowed Rs. 45300/-. Break-up of disallowed amount is Rs. 300/- registration charges and Rs.
45000/- against isolation room @ Rs.5000/- per day was not payable as the patient was not Covid-19
Positive. Hence Insurance Company has rightly settled the claim.
19. Reason for registration of Complaint: Inadequate settlement of Mediclaim.
20. The following documents were placed for perusal:
p) Discharge Summary
q) Settlement Detail
r) GRO
21.Result of hearing of the parties (Observations and Conclusion:
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers state that while the registration charges (Rs. 300) was inadmissible under the
Policy, they would be willing to review the claim in respect of the charges for the Isolation Ward, if the
Complainant could submit a Certificate from the treating doctor giving justification for the Isolation Ward.
The Complainant accepts this offer and agrees to obtain the said Certificate and provide it to the Insurers
within a week. Thus an agreement of conciliation could be arrived at between the Complainant and the
Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Complainant shall provide to the Insurers a
Certificate from the treating doctor giving justification for the Isolation Ward and thereafter the
Insurers shall review the claim as per the terms & conditions of the policy.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 28, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Tanu Jain Versus The Bajaj Allianz General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-005-2122-0341
17.Brief Facts of the Case: Smt. Tanu Jain (hereinafter referred to as the Complainant) has filed this
complaint against the decision of Bajaj Allianz General Insurance Company Ltd. (hereinafter referred
to as the Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
l) Complainant's Argument: Her minor son was infected with Covid-19 and hospitalized in Indraprashta
Apollo Hospital from 18.03.2021 to 25.03.2021. Cashless request was sent from hospital but the same
was denied by the Insurance Company stating that “insufficient medical information provided by hos-
pital”. Hospital Bill was for amount of Rs. 136614/-, for which she filed reimbursement claim along
with Covid-19 positive report and discharge summary. But Insurers rejected the claim for reason that
hospitalization was not required and patient could have taken treatment on home isolation basis. Com-
plainant represented that she, her husband and her son were admitted into a single three-bed room for
Covid-19 treatment and her husband did not face any problem and availed cashless facility from HDFC
Ergo, while her claim was being rejected. She wrote to GRO on 22.05.2021 but claim was again rejected
with same reason. Therefore, she has now approached his forum for relief.
Case of Tanu Jain Versus The Bajaj Allianz General Insurance Company Ltd.
1.
Name & Address of the Complainant
Smt. Tanu Jain
41, 2
nd
Floor, Ram Vihar, Vikas Marg Extension,
New Delhi-110092
2.
Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
OG-20-1103-8430-00000144
Health Guard Policy
16.06.2020 to 15.06.2021
3.
Name of the insured
Name of the policy holder
Luvayam Jain
Tanu Jain
4.
Name of the insurer
Bajaj Allianz General Insurance Company Ltd.
5.
Date of repudiation
21.05.2021
6.
Reason for repudiation
Hospitalization was not required as patient would have
been treated on outpatient/Home isolation basis.
7.
Date of receipt of the complaint
09.07.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 136615/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 136615/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
28.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Smt. Tanu Jain, the Complainant
For the insurer
Shri Shyama Charan Vats, Manager (Legal)
16.
Date of Award/Order
Award under Rule 17/ 28.09.2021
Complaint Ref. No.: DEL-H-005-2122-0341
m) Insurer's Argument: The Insurers in their SCN dated 08.09.2021 have stated that the complainant’s
son was admitted in Indraprastha Apollo hospital due to infection of Covid-19 and had undergone oral
treatment. Complainant filed reimbursement claim of Rs. 136614/- against hospitalization expenses
incurred during hospitalization period from 18.03.2021 to 25.03.2021. On scrutinizing the claim pa-
pers, it was found that the admission in the hospital was not necessary as the clinical examinations
were in permissible limit, no with fever and breathlessness. The treatment could have been carried out
on Outpatient /Home Isolation basis and no active line of treatment in the hospital had been adminis-
tered and only monitoring, investigations and examinations were being conducted at the hospital.
Hence as per Exclusion Clause C-13 of the policy terms and conditions, claim was rightly denied as
hospitalization expenses incurred for any such examinations and investigations carried out in hospital
without any line of active treatment, are not covered.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
s) Discharge Summary
t) Repudiation Letter
u) GRO
21.Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Insurers had repudiated the claim on the ground that the incidence of Covid for the insured was
asymptomatic as per the Discharge Summary and the vital parameter of SPO2 level was normal and
the insured did not need any oxygen support and had no with fever and breathlessness throughout the
hospitalisation. As such, he required home isolation as per the norms notified by the Indian Council
of Medical Research and there was no need for hospitalisation. The Complainant states that as both
she and her husband were hospitalized, there was no option but to have the insured child also with
them in the hospital when he (the child) had tested Covid Positive, even though he was asymptomatic.
Upon examination of the arguments and the evidence submitted by both the parties, it is concluded
that the hospitalisation of the insured was not medically necessary and that he required home isolation
as per the norms notified by the Government and, as such, there was no need for hospitalisation. Hence
the Insurers were justified in repudiating the claim and, pursuantly, the complaint would deserve
rejection.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 28, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Pradeep Babbar Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0367
17.Brief Facts of the Case: Shri Pradeep Babbar (hereinafter referred to as the Complainant) has filed
this complaint against the decision of The Oriental Insurance Company Ltd. (hereinafter referred to as
the Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
Complainant's Argument: He was hospitalized in Institute of Liver & Biliary Science (ILBS),
Delhi from 01.11.2020 to 03.11.2020 for treatment of liver problem. He incurred expenses of Rs.
55548 on treatment including pre-post expenses. He filed reimbursement claim, which was denied
by the Insurers stating that he was having history of alcohol intake as per Discharge Summary.
Complainant submitted rectified Discharge Summary with remark “wrongly written”, but Insurance
Company did not consider it. Earlier complainant’s claim of hospitalization at Grover Nursing
Home was paid but insurance Company repudiated this claim without any ground in spite of sub-
mission of rectified Discharge Summary. He wrote to GRO on 18.04.2021 but claim was denied
again with the same reason. Therefore, he has now approached this forum for relief.
1.
Name & Address of the Complainant
Shri Pradeep Babbar
11/327, Geeta Colony, Krishna Nagar,
New Delhi-110009
2.
Master Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
271700/48/2021/673
Happy Family Floater -2015
02.07.2020 To 01.07.2021
3.
Name of the insured
Name of the policy holder
Pradeep Babbar
Pradeep Babbar
4.
Name of the insurer
The Oriental Insurance Company Ltd.
5.
Date of repudiation
05.01.2021
6.
Reason for repudiation
Patient having history of alcoholic intake, hence
claim repudiated as per policy clause 4.8
7.
Date of receipt of the complaint
03.08.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 55548/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 55548/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of
claims by an insurer
14.
Date of hearing/place
28.09.2021, Delhi
15.
Representation at the hearing
For the Complainant
Shri Pradeep Babbar, the Complainant
For the insurer
Shri Kushal Kumar, AO, DO-14
16.
Date of Award/Order
Award under Rule 17
Insurer's Argument: The Insurers in their SCN dated 21.09.2021 have stated that the complainant
was hospitalized in Institute of Liver & Biliary Science from 01.011.2020 to 03.11.2020 for the
treatment of Acute
Case of Pradeep Babbar Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0367
Pancreatitis, for which he filed claim of Rs. 36778/-. The claim was repudiated by Insurance Company as
per Clause 4.8 of the policy stating that patient was having a history of alcohol intake as mentioned in
Discharge Summary. Later on, complainant submitted Discharge Summary with some corrections
regarding word Ethanol, taking alcohol, written wrongly. The same was investigated by TPA and they
reverted that as per investigation reports there was no change in Hospital record and that of the status of
the claim. Therefore, claim was repudiated rightly as per policy terms and condition. As regards of earlier
claim of hospitalization in R S Grover Memorial Hospital from 31.10.2020 to 01.11.2020, cashless facility
was availed by the insured because as per referral summary provided by the hospital the facts of “ any
history of alcohol or tobacco intake” were not disclosed by the hospital due to which the claim was
approved. But under the present case, etiology was mentioned as “alcohol” in Discharge Summary, hence
claim was repudiated.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
v) Discharge Summary
w) Repudiation Letter
x) GRO
21.Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Insurers had repudiated the claim citing Clause 4.8 on the ground of the insured having a history of
alcohol intake as mentioned in Discharge Summary, as stated in Para 18b above. The Complainant argues
that the certificate dated 12.02.2021 from the ILBS Delhi, states that he is on treatment for chronic calcific
pancreatitis (and other diseases). The Complainant argues that the ailments mentioned in this certificate
relate to non-alcoholic matters. However, the repudiation involved in this complaint relates to his history
of alcohol intake as mentioned in Discharge Summary for 01-03.11.2020, which were confirmed by the
Investigator appointed by the Insurers. The Insurers clarify that the settlement made for him on an earlier
occasion was not based on such investigation and thus the two settlements are not exactly comparable.
Upon examination of the arguments and the evidence submitted by both the parties, it is concluded that the
Insurers had based their findings about the Complainant’s history of alcohol intake on the Discharge
Summary and further investigations. As such, the Insurers were justified in repudiating the claim and,
pursuantly, the complaint shall deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September28, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Tanu Jain Versus The Bajaj Allianz General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-005-2122-0342
17.Brief Facts of the Case: Smt. Tanu Jain (hereinafter referred to as the Complainant) has filed this com-
plaint against the decision of Bajaj Allianz General Insurance Company Ltd. (hereinafter referred to as the
Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
n) Complainant's Argument: She was infected with Covid-19 and hospitalized in Indraprashta Apollo Hospital
from 16.03.2021 to 25.03.2021. Cashless request was sent from hospital but the same was denied by the
Insurers stating that “insufficient medical information provided by hospital”. Hospital Bill was for amount of
Rs, 100373/- for which she filed reimbursement claim along with Covid-19 positive report and discharge
summary. But Insurers rejected the claim for reason that hospitalization was not required and patient could
have taken treatment on home isolation basis. Complainant represented that she, her husband and her son
were admitted into a single three-bed room for Covid-19 treatment and her husband did not face any problem
and availed cashless facility from HDFC Ergo, while her claim was being rejected. She wrote to GRO on
22.05.2021 but claim was again rejected with same reason. Therefore, he has now approached his forum for
relief.
1.
Name & Address of the Complainant
Smt. Tanu Jain
41, 2
nd
Floor, Ram Vihar, Vikas Marg Extension,
New Delhi-110092
2.
Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
OG-20-1103-8430-00000144
Health Guard Policy
16.06.2020 to 15.06.2021
3.
Name of the insured
Name of the policy holder
Tanu Jain
Tanu Jain
4.
Name of the insurer
Bajaj Allianz General Insurance Company Ltd.
5.
Date of repudiation
21.05.2021
6.
Reason for repudiation
Hospitalization was not required as patient would have
been treated on outpatient/Home isolation basis.
7.
Date of receipt of the complaint
09.07.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 96323/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 96323/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of claims by
an insurer
14.
Date of hearing/place
28.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Smt. Tanu Jain, the Complainant
For the insurer
Shri Shyama Charan Vats, Manager (Legal)
16.
Date of Award/Order
Recommendation under Rule 16/ 28.09.2021
Case of Tanu Jain Versus The Bajaj Allianz General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-005-2122-0342
o) Insurer's Argument: The Insurers in their SCN dated 08.09.2021 have stated that the complainant was ad-
mitted in Indraprastha Apollo hospital from 16.03.2021 to 25.03.2021 due to infection of Covid-19 and had
undergone oral treatment, for which she had filed reimbursement claim of Rs. 100373. On scrutinizing the
claim papers, it was found that her admission in the hospital was not necessary as the clinical examinations
were in permissible limit, no with fever and breathlessness. The treatment would have been carried out on
Outpatient /Home Isolation basis and no active line of treatment in the hospital had been administered and
only monitoring, investigations and examinations were being conducted at the hospital. Hence as per Exclu-
sion Clause C-13 of the policy terms and conditions, claim was denied as hospitalization expenses incurred
for any such examinations and investigations carried out in hospital without any active line of treatment, are
not covered.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
y) Discharge Summary
z) Repudiation Letter
aa) GRO
21.Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant states that her husband Shri Ujjwal Jain had got hospitalized in the same hospital room
for the same ailment for the same period and his claim was settled by his Insurers, namely, HDFC Ergo
GIC. The Insurers offer to review her claim if she submits (a) the Claim Settlement Letter and the Medical
Papers in respect of her husband for his claim from HDFC Ergo GIC, and (b) the Recommendation of the
treating doctor for her hospitalisation. The Complainant accepts this offer and agrees to provide these
documents to the Insurers within a week. Thus an agreement of conciliation could be arrived at between the
Complainant and the Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the Complainant
and the Insurers. Accordingly, the Complainant shall provide the documents as mentioned above to the
Insurers and thereafter the Insurers shall review the claim as per the terms & conditions of the policy.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 28, 2021
