PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman - Shri Sudhir Krishna
Case of Hritek R Khosla V/S Manipal Cigna Health Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-053-2021-0758
1.
Name & Address of the Complainant
Shri Hritek R Khosla S/o Shri Rajinder S Khosla,
House No. 199, Panna Lal Marg, Dhariwal,
Distt. & Tehsil- Gurdaspur, Punjab- 143519
Mobile No.- 8727053799
2.
Policy No:
Type of Policy
Duration of policy/Policy period
100200081905/00/00
Group Health Insurance
31-01-2021 To 30-01-2022
3.
Name of the insured
Name of the policyholder
Poonam Seth
M/S Bajaj Finance Ltd.
4.
Name of the insurer
Manipal Cigna Health Insurance Co. Ltd.
5.
Date of Repudiation
04.02.2021
6.
Reason for repudiation
Non-disclosure
7.
Date of receipt of the Complaint
25-03-2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of Claim
Rs.345977/-
10.
Date of Partial Settlement
N.A
11.
Amount of relief sought
Rs.3,45,977/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claims by an insurer
13.
Date of hearing/place
10.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Hritek R Khosla, the complainant
For the insurer
Shri Jaswinder Singh Shekhawat, Manager (Legal)
15
Complaint how disposed
Recommendation under Rule 16
16
Date of Award/Order
10.09.2021
17. Brief Facts of the Case: Shri Hritek R Khosla (hereinafter, the complainant) has filed this
complaint against Manipal Cigna Health Insurance Co. Ltd. (hereinafter, the insurers) alleging
incorrect denial of claim.
18. Cause of Complaint:
a) Complainant’s argument: His mother Poonam Seth bought a health insurance policy online
of Bajaj Allianz health insurance through Bajaj finance acting as an agent on 1
st
February
2018 and paid premium regularly. On 26
th
December 2020, she got a call from Bajaj Finance
to renew the policy. Firstly, he explained all the benefits which were same as per our
ongoing policy but in the end of call changed the health insurance company’s name from
Bajaj Allianz to Manipal Cigna and got approval from her by misleading her. The
complainant’s mother was detected cancer positive on 29
th
Jan. 2021. Her treatment started
from 1
st
February2021 at DMCH Ludhiana but when hospital requested for cashless
treatment the claim was rejected multiple times by the Manipal Cigna providing the reason
that proposer had not disclosed the disease in proposal form. No proposal form was filled
by us and had requested for renewal of the policy on 26
th
December 2020 which is almost
more than one month before detecting of disease. The complainant further stated that they
have all the records and recordings which prove the fraud and misleading done by insurance
and finance companies.
b) Insurers’ argument: As per SCN, the Complainant on 1st February 2021 had registered a
cashless claim amounting Rs. 2,00,000/- for his mother’s hospitalization at Dayanand
Medical College And Hospital (DMC hospital), Ludhiana for CA CERVIX (cervical cancer). On
perusal of the discharge summary dated 23rd January 2021 from Dayanand Medical College
and Hospital, Ludhiana, it was found that the Complainant’s mother was diagnosed with
cervical carcinova IVa (cervical cancer- stage IV) on 21st January 2021 i.e 9 days before the
policy inception. Since there was a non-disclosure of material fact by the Complainant’s
mother at the time of application, which is material to the policy decision, the claim was
found to be non-admissible. Therefore, the claim was rejected by the Company for non-
disclosure of material information under Clause VI.1 (Duty of Disclosure) of the terms and
conditions and the same and was intimated to the Complainant vide rejection letter dated
04 Feb 2021. In lines with the above referred clause of policy terms & conditions, the
Company terminated the Policy of the Complainant.
19. Reason for Registration of Complaint: Incorrect denial of claim.
20. The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to review the claim and settle it as per the terms and
conditions of the policy, if the Complainant submits the required documents for the
reimbursement claim. The Complainant agrees to submit the required documents within
one week. Thus an agreement of conciliation could be arrived at between the Complainant
and the Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall review the claim and settle it
as per the terms and conditions of the policy, for which the Complainant shall submit the
required documents within one week.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Shri Sandeep Kumar V/S The United India Insurance Co. Ltd.
Complaint Ref. No. : CHD-H-051-2021-0765
1.
Name & Address of the Complainant
Shri Sandeep Kumar
R/o H. No.- 709 B1, New Rathpur Colony, Pinjore,
Distt.- Panchkula, Haryana- 134102
Mobile No.- 9996425099
2.
Policy No:
Type of Policy
Duration of policy/Policy period
5001002819P111085979
Group Mediclaim
01.10.2019 TO 30.09.2020
3.
Name of the insured
Name of the policyholder
Sandeep Kumar
BOB _ IBA
4.
Name of the insurer
The United India Insurance Co. Ltd.
5.
Date of Repudiation
07.12.2020
6.
Reason for repudiation
No active line of treatment
7.
Date of receipt of the Complaint
26-03-2021
8.
Nature of complaint
Non settlement of health claim
9.
Amount of Claim
Rs. 174524/- + Dom. Claim amount
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
All domiciliary amount + balance payable amt out of
Rs. 174524/-.
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claim by an insurer
13.
Date of hearing/place
10.09.2021/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Sandeep Kumar, the Complainant
For the insurer
Smt. Pamela Pinto, Dy. Manager (LCD), Mumbai

15.
Complaint how disposed
Recommendation under Rule 16
16.
Date of Award/Order
10.09.2021
17) Brief Facts of the Case: Shri Sandeep Kumar (hereinafter, the Complainant), has filed
this complaint against the United India Insurance Co. Ltd. (hereinafter, the Insurers) for non-
settlement of his health claim.
i. Cause of Complaint:
a) Complainants argument: He is suffering from some ailment since December 2017 and
since been admitted in many hospitals like PGI, Chandigarh, Alchemist Panchkula. In
Medanta Hospital, after some tests actual ailment was diagnosed as Quona Equeda
Syndrom with G mutation, i.e. Spinal TB with Resistant type. Actual right medicine was
started on 8th April 2019. He was admitted to hospital so many times and all claims were
settled by insurance company. Initially unaware, he came to know about domiciliary claim
from a new colleague and then have sent all the unclaimed bills for the policy period from
November 2019 to September 2020 including hospitalization bill, which were received by
TPA Medi Assist dt. 26.09.2020. On 15.11.2020 they uploaded the status that ‘denial reason
entered’. On follow up, they told him that it was a ‘hospitalization reimbursement claim for
24.01.2020 to 25.01.2020 and patient was on oral medication only’ so claim is not
admissible. In the whole claim amount medicine and consultation bills were of Rs. 141680/-
and hospitalization bills were of Rs. 32844/- only. Company has just classified the whole
claim of Rs. 174524/- as hospitalization expenses reimbursement claim for two days i.e. for
24.01.20 to 25.01.20, although he sent all the medical history papers, original consultation
and medicine bills for the period November 2019 to 15.09.2020. He admitted that
unknowingly he sent both claim papers jointly, because it would have taken a separate
claim form only that needs to be annexed with the 2
nd
claim domiciliary or hospitalization.
b) Insurers’ argument: Company received a claim of Rs.174524/- pertains to Insured
Sandeep Kumar, who was admitted in Medanta Hospital, Gurugram on 24/1/2020 and
discharged on 25/1/2020. He is k/c/o drug resistant TBM on ATT since April 2019 with Right
Lower Poliomyelitis and Cauda Equina Syndrome admitted with c/o back pain. On
Hospitalization, he underwent MRI of dorsal spine. He was treated with ATT (Anti-
Tuberculosis Treatment), intravenous fluids, multivitamins and other supportive treatment.
He responded well and discharged in stable condition. They had denied the claim as the
treatment of the patient was done by oral medications only. No I.V. administration of
medicine was given and no active line of treatment is seen. He was admitted only for pain
management. Hence the claim is not admissible and stands repudiated under Clause No.
1.1. of the policy.
19) Reason for Registration of Complaint:- Non settlement of health claim.
20) The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
a) Result of Personal hearing with both parties (Observations & Conclusion):
b) Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Insurers offer to admit the claim and settle the same as per the provisions for
Domiciliary Treatment under the Policy.
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to review the claim and settle it as per the terms and
conditions of the policy for Domiciliary Treatment. The Complainant accepts this offer. Thus
an agreement of conciliation could be arrived at between the Complainant and the Insurers,
which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall review the claim and settle it
as per the terms and conditions of the policy, for Domiciliary Treatment.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case ofAjay KumarV/SBharti AXA GeneralInsuranceCo. Ltd.
Complaint Ref. No.: CHD-H-007-2021-0764
1.
Name & Address of the Complainant
Shri Ajay Kumar
Mata Mohalla, H. No. 259/3,
VPO- Radaur, Dist. Yamunanagar, Haryana- 135133
Mobile No.- 7206895580
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Q1099664
Group Hospital Cash
15-12-2019 To 14-12-2020
3.
Name of the insured
Name of the policyholder
Ajay Kumar
Ajay Kumar
4.
Name of the insurer
Bharti AXA General Insurance Co. Ltd.
5.
Date of Repudiation
06.03.2021
6.
Reason for repudiation
Fraudulent claim
7.
Date of receipt of the Complaint
26-03-2021
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 1,10,000/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs. 1,10,000/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claim by an insurer
13.
Date of hearing/place
17.09.2021 / On line hearing
14.
Representation at the hearing
For the Complainant
Shri Ajay Kumar, the complainant
For the insurer
Shri Rishi Kant, Senior Manager (Legal)
15
Complaint how disposed
Award under Rule 17
16
Date of Award/Order
19.09.2021
17. Brief Facts of the Case:Shri Ajay Kumar (hereinafter, the Complainant), has filed this complaint
against the Bharti AXA General Insurance Co. Ltd.(hereinafter, the Insurers) for non-settlement of
his health claim.
18. Cause of Complaint:
a) Complainants argument:He had bought a policy no. Q1099664 from the Insurers andhad filed a claim in
Oct. 2020 for repayment of his medical treatment expenses. After follow up through mails and calls for
five months, they rejected his claim in the month of March 2021.
b) Insurers’ argument: He got admitted at Krishna Hospital, Radaur, Yamuna Nagar from 09-09-2020 to
18-09-2020 for the first time and then again on 21-09-2020 to 02-10-2020 having complaint of vomiting,
abdomen pain & fever. The Insured was managed with conservative treatment from 09-09-2020 till 18-09-
2020 thereafter the Insured complained of the same issue after 3 days & thereafter got admitted in the
same hospital from 21-09-2020 till 02-10-2020.However, there was discrepancy found in the hospital
records as the hospital did not maintain the ICP and has provided a declaration regarding the same.ICP
(indoor case paper) is mandatorily & routinely maintained by Hospital for patients that are admitted for
treatment. The hospitalization of the Insured could not be ascertained because of incomplete Indoor
Papers provided by the Hospital coupled with the fact that none in the vicinity of the Insured confirmed
much about the Hospitalization during investigation done at the residence of Patient.Also, as per the
Registration certificate, the treating Doctor is a Bachelor of Ayurveda, Medicine but the treatment
provided is allopathic which happens to be an exclusion of the Policy. The relevant provisions of exclusion
applicable in this case are Section 4– Disclosure of information and section 4.VI – Fraud. The complainant
is guilty of Misrepresentation of Facts and violation of Policy Terms and Conditions. In light of the above,
the claim of the Complainant was repudiated vide repudiation letter dated 06-03-2021.
19. Reason for Registration of Complaint: Repudiation of health claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion)
Case called. Parties are present and recall their arguments as noted in Para 18 above. At the
outset, the Insurers inform that their company is now merged with ICICI Lombard GIC. The
Complainant states that he had submitted all the documents in his possession to the Insurers.
The Insurers state that the Indoor Case Papers for the days of both the hospitalization were not
made available either by the Complainant or by the Hospital, as a result of which, it was not
possible to ascertain the facts of the treatment. Also, the treating physician was Ayurvedic, who
had administered allopathic drugs to the Complainant, which was against the norms. Upon
examination of the arguments and the evidence submitted by both the parties, it is concluded
that the definition of Medical Practitioner clause was not satisfiedby the treating physician and
also the required documents were not made available to the Insurers. In these circumstances,
the Insurers were justified in repudiating the claim.Pursuantly, the complaint would deserve to
be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 19, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Sudhir Krishna
Case of Sham Sunder Garg V/S The United India Insurance Co. Ltd.
Complaint Ref. No.: CHD-H-051-2122-0007
1.
Name & Address of the Complainant
Shri Sham Sunder Garg
1/1, Old Jawahar Nagar, Ladowali Road, Jalandhar
City, Jalandhar, Punjab- 144001
Mob. no. 9417327577, 9056374506
2.
Policy No:
Type of Policy
Duration of policy/Policy period
5001002819OP111833956
Group Health Mediclaim Policy
01-11-2019 To 31-10-2020
3.
Name of the insured
Name of the policyholder
Sham Sunder Garg
Indian Bank’s Association
4.
Name of the insurer
The United India Insurance Co. Ltd.
5.
Date of Repudiation
Not applicable
6.
Reason for repudiation
Not applicable
7.
Date of receipt of the Complaint
30-03-2021
8.
Nature of complaint
Deduction in health claim
9.
Amount of Claim
Rs. 26946/- (Out of this Rs.9420/- recd.)
10.
Date of Partial Settlement
09.04.2021
11.
Amount of relief sought
Rs.26946/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claim by an insurer
13.
Date of hearing/place
24.09.2021/ Online hearing
14.
Representation at the hearing
• For the Complainant
Shri Sham Sunder Garg, the complainant
• For the insurer
Smt. Srijani S., Asstt. Manager (LCB), Mumbai
15
Complaint how disposed
Recommendation under Rule 16
16
Date of Award/Order
24.09.2021
17. Brief Facts of the Case: Shri Sham Sunder Garg (hereinafter, the Complainant), has filed this
complaint against the United India Insurance Co. Ltd. (hereinafter, the Insurers) for non-
settlement of his claim.
18. Cause of Complaint:
a) Complainants argument: Initially he had filed a complaint regarding non-settlement of medical
bills of heart bypass surgery at Fortis Mohali on 24.06.2020. He informed that all original
documents sent to Health India TPA by speed post dt. 28.10.2020 and delivery confirmed on
02.11.2020, but no action was taken. Later on, Complainant vide form VI-A has informed that he
received Rs. 9420/- on 09.04.2021 that is after 8 moths. He insisted that out of deduction of Rs.
17526/-, company must pay essential charges for Covid test before surgery, medicines, and
consumables etc.
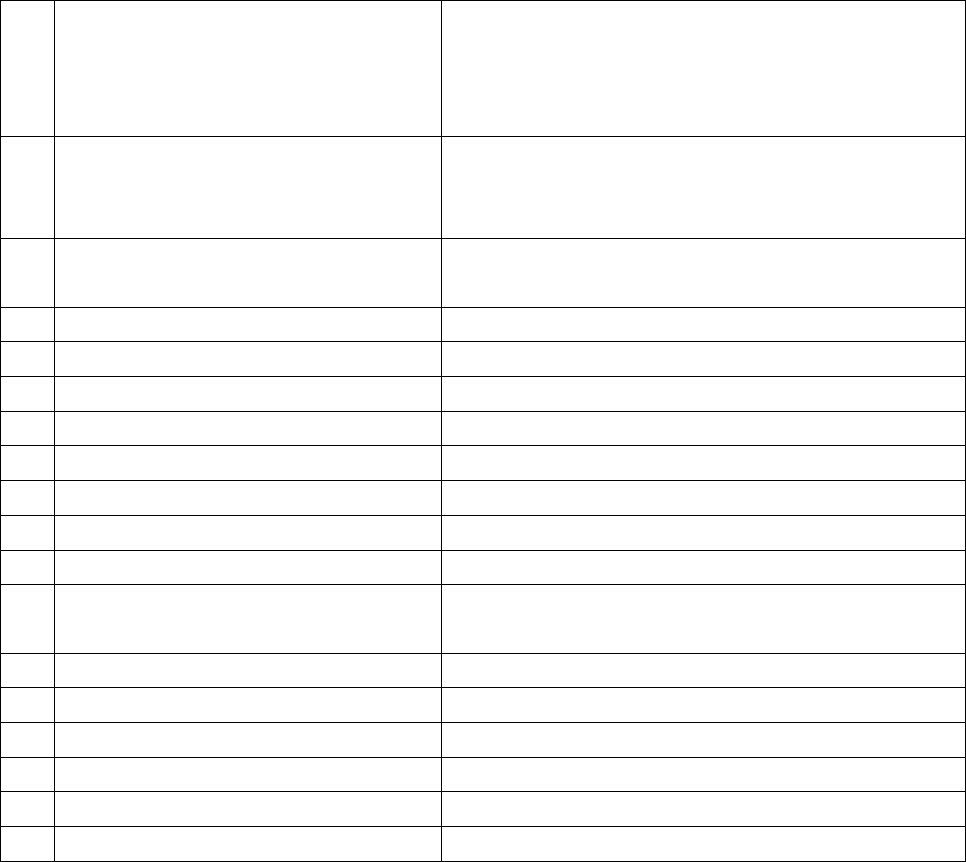
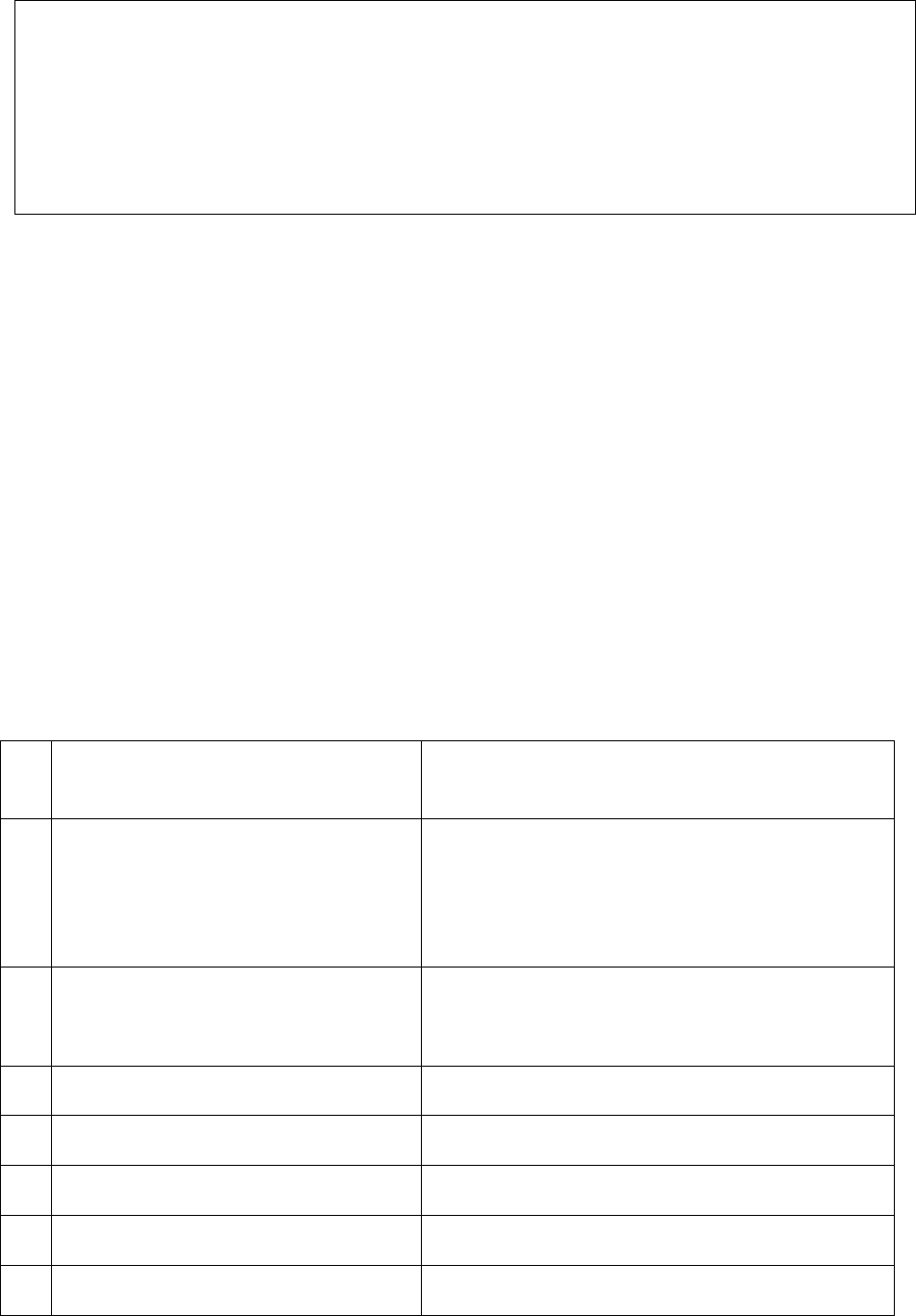
b) Insurers’ argument: As per SCN submitted by Insurers, a claim of Rs. 26946/- from the
Complainant for his hospitalization from 22.06.2020 to 03.07.2020 in Fortis Hospital, Mohali with
diagnosis of CAD-TVD, HTN, DM, LVEF has been received by company. Against claimed amount of
Rs. 26946/-, company settled the claim for Rs. 9420/- and paid on 09.04.2021 subsequent to
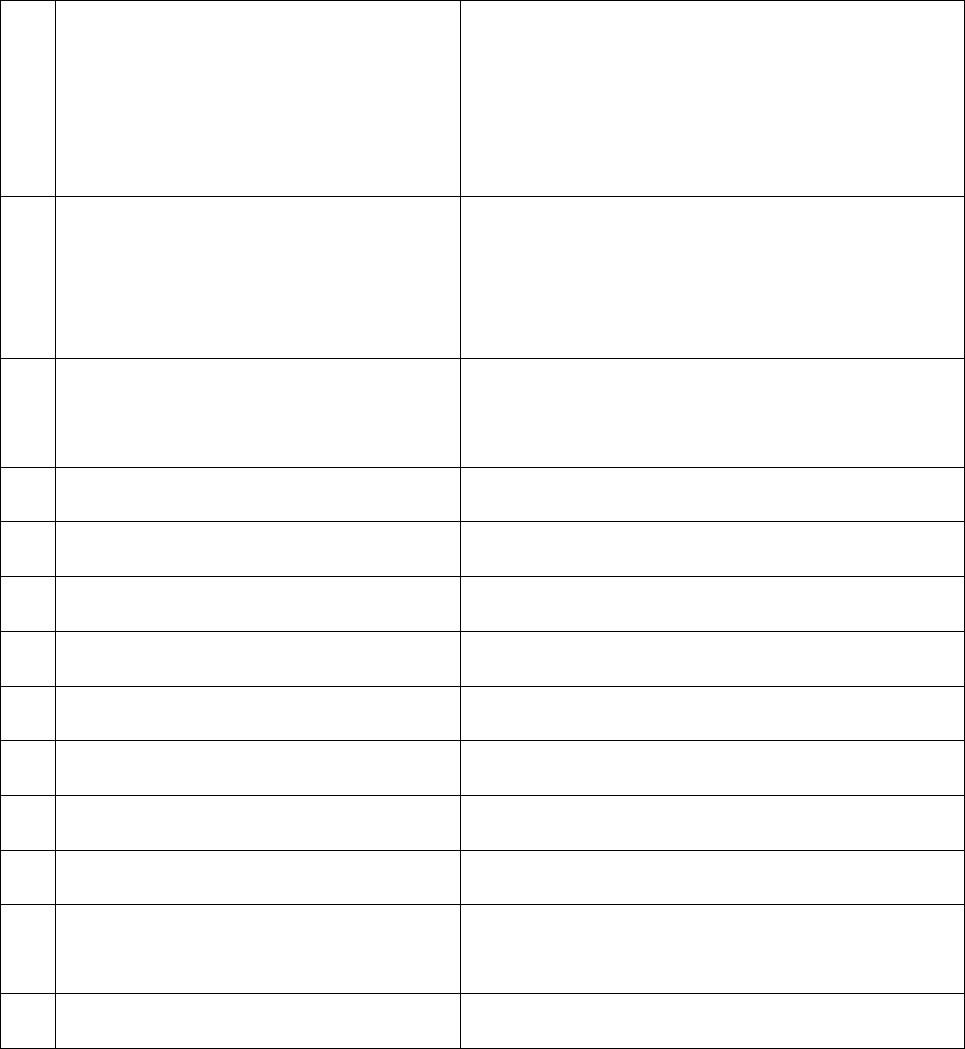
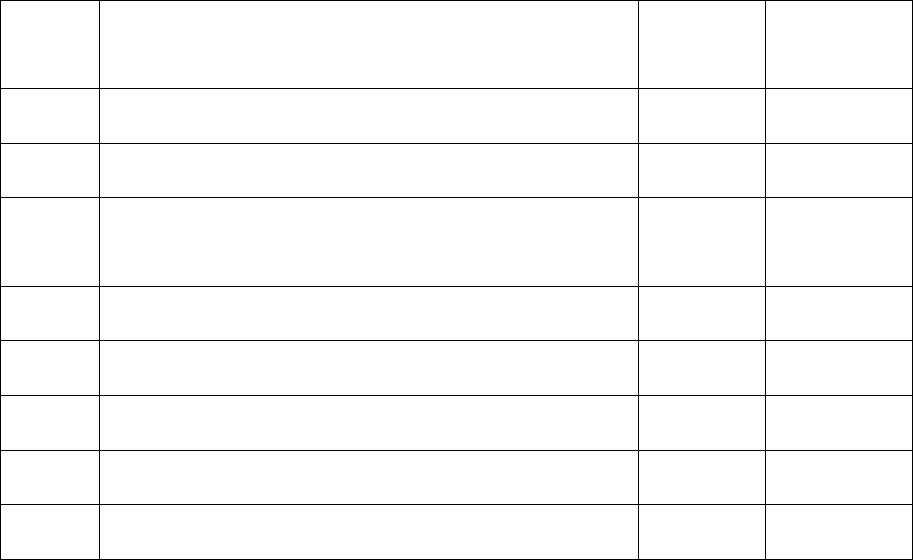
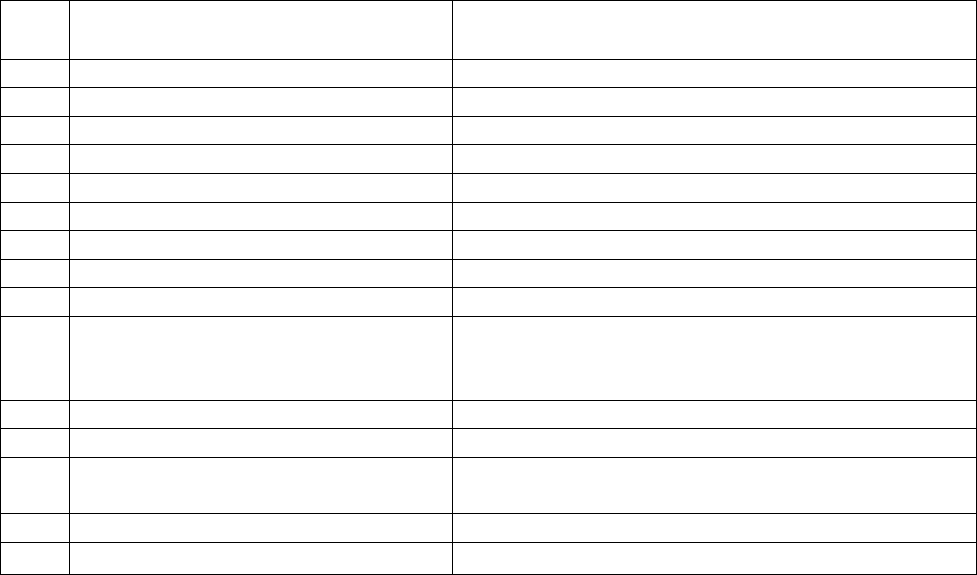
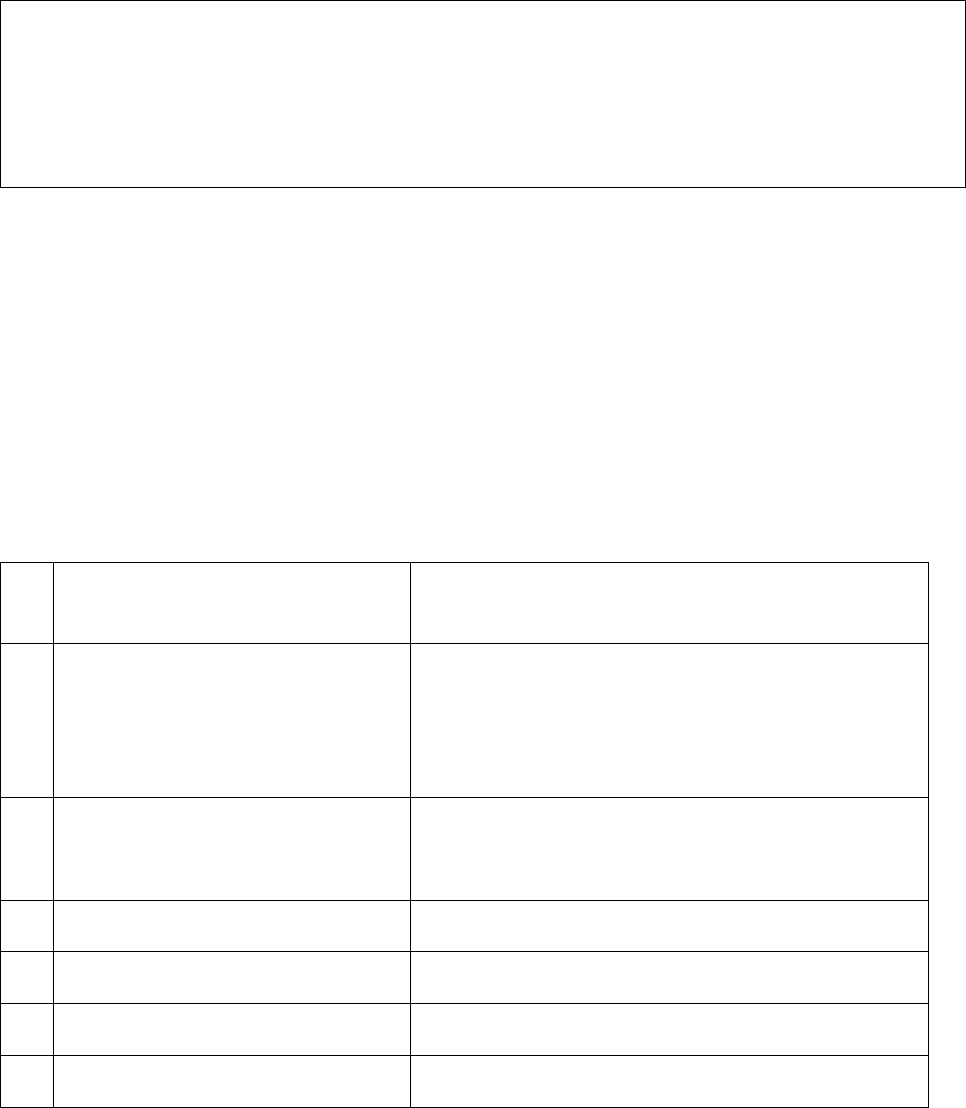
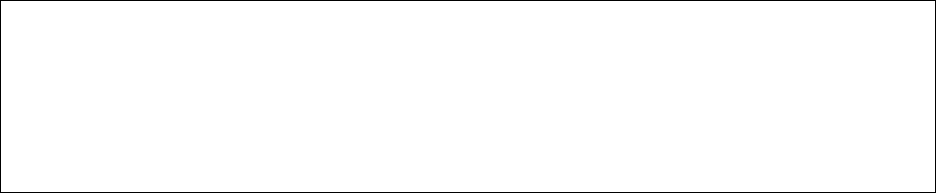
Ombudsman complaint. Details of deduction of Rs. 17526/- is as under:
Bill date
Remark/reason
Bill Amt
Deducted
Amt.
27.07.20
Consultation charges/Consulting note not submitted
1850
1850
22.06.20
COVID 19 SARS COV/ Not related to current ailment
4500
4500
29.07.20
Home health care charge/ No details available not
payable
10000
10000
21.08.20
Medicines charges (betadine)/Non medical items ded.
4905
306
27.07.20
Medicines charges (gloves)/Non medical items ded.
4558
500
22.06.20
Registration charges N.P.
100
100
27.07.20
X ray charges / Report is not submitted
270
270
Total
17526
19. Reason for Registration of Complaint: Deduction in health claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of hearing with the parties (Observations & Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage the Insurers offer to settle the balance claim as follows:
(a) Consultation charges (Rs. 1850) shall be paid upon submission of an undertaking by the
Complainant, for which the contents shall be conveyed by the Insurers shortly;
(b) Covid-19 Test charges (Rs. 4500) shall be paid;
(c) Post-hospitalisation Home Healthcare charges (Rs. 10000) shall be paid on submission of
details from the Wecare; and
(d) X-ray charges (Rs. 270) shall be paid on submission of X-ray film/copy.
(e) The remaining 3 items are non-admissible/not payable.
The Complainant accepts this offer and assures to provide the required documents very shortly.
Thus an agreement of conciliation could be arrived at between the Complainant and the insurers,
which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the insurers. Accordingly, the Insurers shall reimburse the balance claim in
respect of 4 items as mentioned above, for which the Complainant shall provide the required
documents.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 24, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Abhay Aggarwal Versus New India Assurance Company Ltd.
Complaint Ref. No.: DEL-H-049-2122-0281
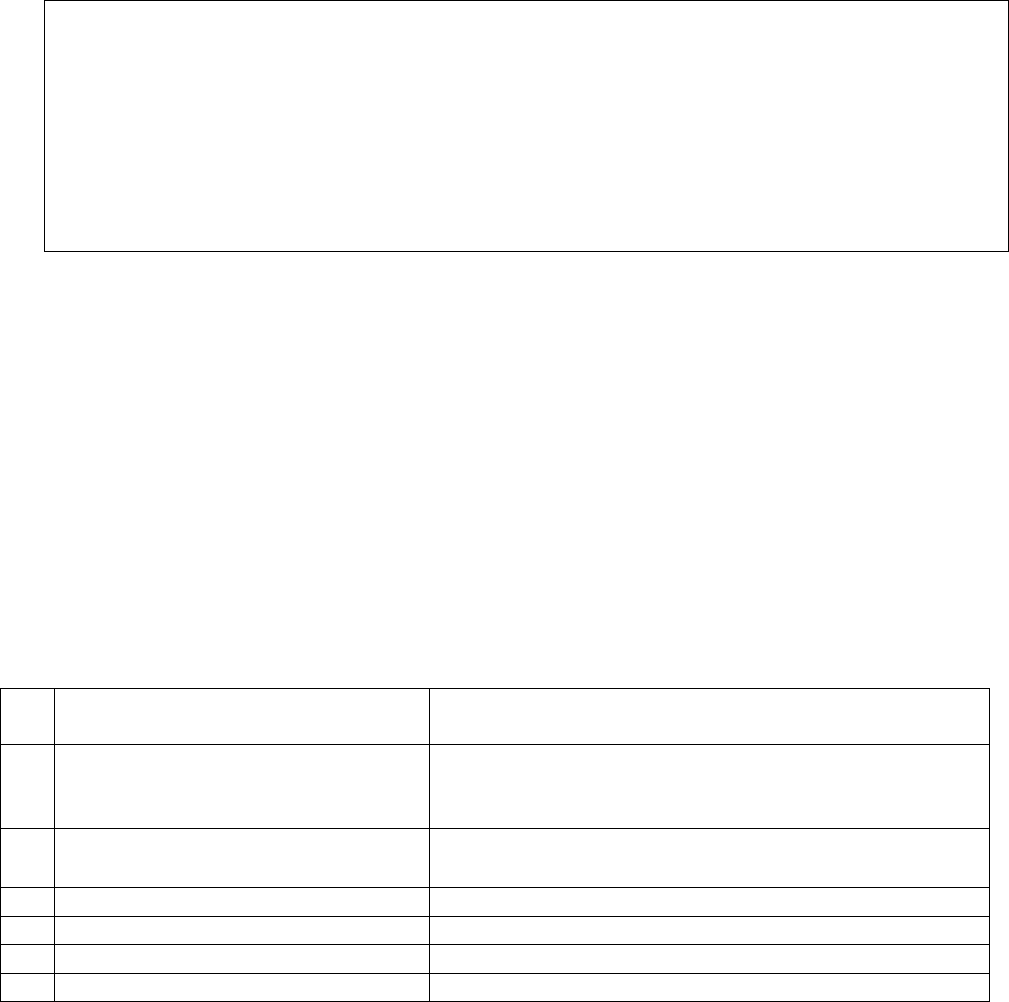
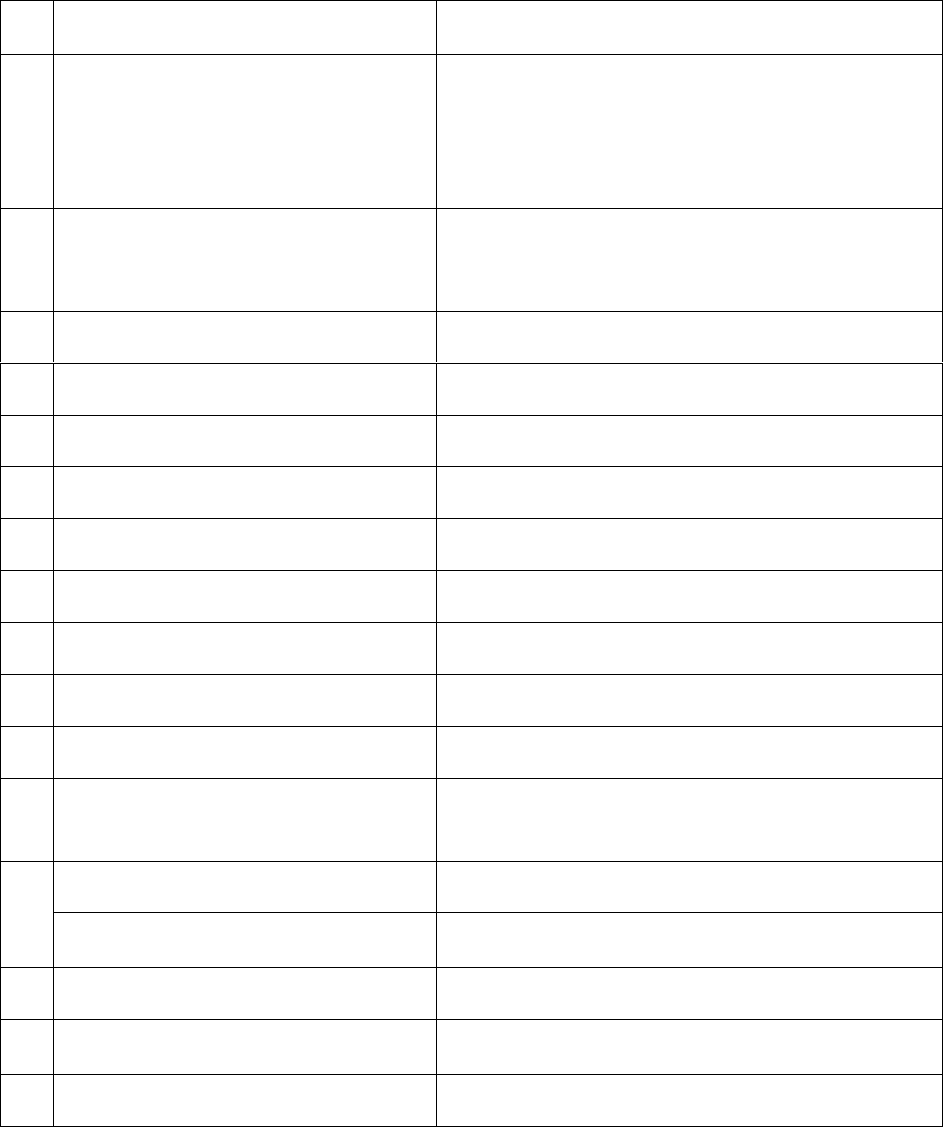
1.
Name & Address of the
Complainant
Shri Abhay Aggarwal, Cedar 3/406, Gulmohar
Enclave, Nehru Nagar-3, Ghaziabad-201001 (U.P.)
2.
Policy No:
Type of Policy
Duration of policy/Policy period
32370034190400000016
Group Mediclaim
07.10.2019-06.10.2020
3.
Name of the insured
Name of the policy holder
Abhay Aggarwal
Abhay Aggarwal
4.
Name of the insurer
New India Assurance Company Ltd.
5.
Date of repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the complaint
02.08.2021.
1. Brief Facts of the Case: Shri Abhay Aggarwal (hereinafter referred to as the Complainant) has filed this
complaint against the decision of the New India Assurance Company Ltd. (hereinafter referred to as the
Insurers or the Respondent Insurance Company) alleging wrongly crediting the hospital an additional
amount actually due to the complainant.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant was covered under the Group Mediclaim Policy. His new born
child was admitted in Yashoda Hospital, Ghaziabad from 05.04.2020 to 24.05.2020. The insurers had
made payment under cashless mode to the hospital towards the said hospitalization. The hospital had
wrongly recovered an amount of Rs 18109/- towards non-medical items from him. He represented to the
TPA for reimbursement of this amount along with an additional amount of Rs. 5417/-, which the Hospital
staff had inadvertently failed to incorporate. An amount of Rs 22142/- was approved by the insurer but
wrongly credited to the hospital account. The complainant has not received the amount as yet. He has
approached this forum to get his complaint redressed.
b) Insurers Argument: The Insurers in their SCN have stated that the complainant’s wife Vaishali was
admitted in the hospital for 32 weeks breach pregnancy with IVGR with severe PET with previous LSCS.
Case of Abhay Aggarwal Versus New India Assurance Company Ltd.
Complaint Ref. No.: DEL-H-049-2122-0281
They had settled an amount of Rs. 480019/-with the hospital and had deducted Rs 18109/- towards non-
medical items. The insurers reviewed the claim and it was found that the complainant was asking for the
non-payable items. The hospital also approached them for short payment. The insurer made the payment
to the hospital after review. The payment that was made by the insured to the hospital was on account of
non-medical items and is not recoverable under the policy. The Insurers have subsequently sent an email
intimating that they are ready to settle the balance amount of Rs. 5427/ -subject to original bills, if it is
payable as per policy terms and conditions.
19. Reason for registration of Complaint: Incorrect reimbursement to the hospital.
20. The following documents were placed for perusal:
a) SCN, Insurance policy, Claim Processing Sheet.
8.
Nature of complaint
Additional claim amount credited wrongly
9.
Amount of claim
Rs 22142/-
10.
Date of partial settlement
24.05.2020
11.
Amount of partial settlement
Rs.480019/-
12.
Amount of relief sought
Rs 23526/-+ Rs. 20000/-
13.
Complaint registered under Rule
No. of the Insurance Ombudsman
Rules, 2017
Rule 13(1) (b) – any partial or total repudiation of claim
by insurer.
14.
Date of hearing/place
13.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
1. Shri Abhay Aggarwal, the Complainant
2. Shri Arvind K Aggarwal, F/o the Complainant
For the insurer
Shri Neeraj Sharma, Asst. Manager, Broker DO,
Laxminagar
16.
Date of Award/Order
Award under Rule 17/ 14.09.2021
b) List of Non Medical Items.
c) Letter to GRO
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Claim was for Rs. 5,45,550, against which Insurers have paid Rs. 4,80,019 to the Hospital after
adjusting for Hospital Discount of Rs. 47,422, leaving a balance of Rs. 18,109, which is the repudiated
sum. The main item disallowed was Incubator (Rs. 15750), treating it is an instrument. Other disallowed
items were Tegaderm paid for limited number and excess number was disallowed, Urobags & IV sets
treated as non-medical items, and admission charge as not payable. However, none of these items are
specifically disallowed in the policy, as the Insurers admitted during the hearing. The Insurers states that
in regard to the Tegaderm, they have followed some norm set by IRDAI, but admit that the same is not
stated in the Policy. In these circumstances, the repudiation of each of these items was not justified.
Pursuantly, the complaint would deserve to be allowed. The Insurers would also need to pay interest on
this amount in terms of the provision of the IRDAI (PPHI) Regulations 2017. As for the additional claim of
Rs. 5417, the Insurers have conveyed that they are ready to settle it, subject to original bills, if it is
payable as per policy terms and conditions.
Award
The complaint is allowed and the Insurers are directed to pay the repudiated amount of Rs. 18,109,
along with interest in terms of the provisions of the IRDAI (PPHI) Regulations 2017, to the
Complainant. As for the additional claim of Rs. 5417, the Insurers should settle the same, after
verifying the original bills, as per the terms and conditions of the policy.
Parties should implement this award within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 14, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
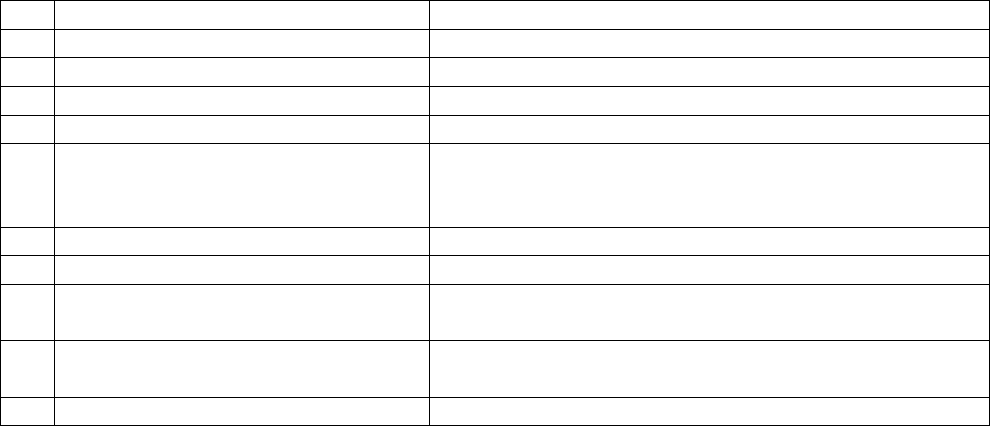
Case of Anil Kumar Bansal Versus HDFC ERGO General Insurance Company Ltd.
Complaint Ref. No.: DEL-H-003-2122-0294
1.
Name & Address of the Complainant
Shri Anil Kumar Bansal,
1170, Kuchapati Ram, Bazar Sita Ram, Delhi-
110006
2.
Policy No:
Type of Policy
Duration of policy/Policy period
PE01880435G
Group Mediclaim-Individual Plan (Bank customer)
Policy
29.11.2019-28.11.2020
17.Brief Facts of the Case: Shri Anil Kumar Bansal (hereinafter referred to as the Complainant) has filed this
complaint against the decision of the HDFC ERGO General Insurance Company Ltd. (hereinafter referred to
as the Insurers or the Respondent Insurance Company) alleging wrong rejection of his hospitalization claim
and cancellation of his mediclaim policy.
18. Cause of Complaint:
a) Complainant's Argument: The Complainant has stated that he was having the insurance cover under Easy
Health Group Insurance Plan of Apollo Munich Health Insurance since 21.10.2016. The said policy was auto-
renewed in 2017 and 2018. In 2019 the policy was not auto-renewed on 21.10.2019 as in previous years.
The insurers issued a new policy namely Group Assurance Health Plan via Canara Bank effective from
29.11.2019. He was admitted in Fortis Escorts Heart Institute on 01.02.2020 following a fall in the bathroom
with symptoms of slurred speech and drowsiness. He was diagnosed as a case of ICH with Hypertension
Left Hemiplegia. His cashless authorization was denied by the insurers on the ground of non-disclosure of
ailment of Obstructive Sleep Apnea (OSA) in the declaration form. Subsequently his policy was also
cancelled on 05.02.2021 for the same reason. He has stated that the attending doctor also certified that
OSA was not the cause of the stroke suffered by the complainant. He represented against the rejection of
his cashless claim and policy cancellation by reporting to IRDA. However the Respondents did not change
their stand. He then approached this Office to get his complaint redressed.
b) Insurers Argument: The Insurers in their SCN dated 20.09.2021 have stated that complainant had failed to
pay the renewal premium in October 2019 in spite of the repeated reminders sent by them. His policy
expired on 20.10.2019. They have stated that they received a fresh proposal from the Complainant on
29.11.2019 and he had provided the Health details as per Clause 7 of this form. Based on his declaration,
the insurance policy was issued to him from 29.11.2019-28.11.2020. The insurers received a Cashless
Preauthorization request from Escorts Heart Institute on 02.02.2020. On review of the documents
received from the hospital for preauthorization, they noted that the complainant had a history of OSA for
preceding 5 years. They have stated that the insured did not produce any document to prove his
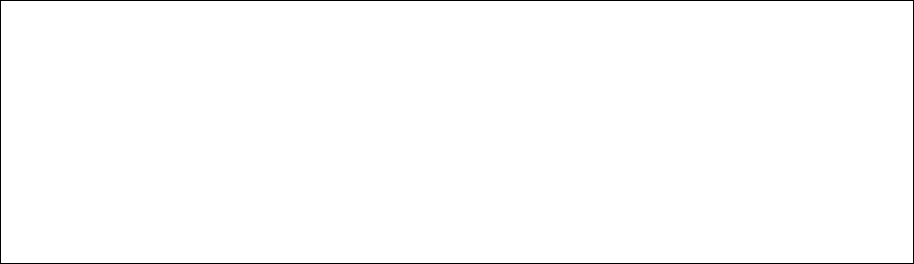
3.
Name of the insured
Name of the policy holder
Anil Kumar Bansal
Anil Kumar Bansal
4.
Name of the insurer
HDFC ERGO General Insurance Company Ltd.
5.
Date of repudiation
29.03.2020
6.
Reason for repudiation
Non-disclosure of pre-existing disease
7.
Date of receipt of the complaint
10.08.2021
8.
Nature of complaint
Rejection of claim; Cancellation of policy
9.
Amount of claim
Rs 92536/-
10.
Date of partial settlement
NA
11.
Amount of partial settlement
NA
12.
Amount of relief sought
Rs 92536/-
13.
Complaint registered under Rule No.
of the Insurance Ombudsman Rules,
2017
Rule 13(1) (b) – any partial or total repudiation of
claim by insurer.
14.
Date of hearing/place
27.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
1. Shri Anil Kumar Bansal, the Complainant
2. Shri Ayushman Bansal, s/o the Complainant
For the insurer
Shri Manoj K Prajapati, Manager (Corporate Legal)
16.
Date of Award/Order
Award under Rule 17/ 27.09.2021

contention of suffering from OSA for previous 5 months only. They rejected the cashless claim on account
of Non-disclosure of material fact in the proposal form. They invoked Section 7 of the policy terms and
conditions and rejected his claim. Since the complainant did not adhere to the principle of utmost good
faith, the existing policy was cancelled too.
19. Reason for registration of Complaint: Rejection of claim.
20. The following documents were placed for perusal:
a) SCN, Insurance policy.
b) Proposal Form, Discharge summary, Doctor’s certificate.
c) Letter of GRO.
21. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Complainant states that the Insurers had defaulted in not auto-renewing his policy, as they had done
in the past. The Insurers state that they renew the policy only after getting consent of the policyholder,
for which they had issued the renewal notice on 14.8.2019. The Complainant denies having received the
renewal notice. It was, however, incumbent upon the Complainant to have got his policy renewed on
time and he cannot pass on this responsibility onto the Insurers.
The Complainant denies having submitted the proposal form for the fresh policy. However, on one hand
the Complainant is expecting auto renewal and on the other hand he is objecting to the issuance of policy,
for which he paid the premium. This makes his argument unreasonable.
The Insurers had noted from the documents received from the hospital for preauthorization that the
Complainant had a history of OSA for preceding 5 years. Subsequently, the Complainant secured an
undated certificate from the treating physician stating that the words ‘5 years’ should be read as ‘5
months’. Such casual approach on the hospital/physician makes the entire hospital records suspect.
Upon examination of the arguments and the evidence submitted by both the parties, it is concluded that
(a) the Complainant had failed to get his policy renewed on time, (b) the new policy was issued upon
receipt of fresh proposal form, and (c) the complainant had a history of OSA for preceding 5 years that he
did not disclose in the proposal form, which would justify the action of the Insurers in repudiation of the
claim and cancellation of the policy.
Pursuantly, the complaint shall deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman
September 27, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Mahavir Prasad Soni versus The United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-2122-0316
1.
Name & Address of the Complainant
Shri Mahavir Prasad Soni
101, Avlon Apartment, New Manglapuri, Delhi-110030
2.
Policy No.
Type of Policy
Policy term/policy period
5001002818P109894215
Group Health Insurance Policy
01.10.2018 to 30.09.2019
3.
Name of the insured
Name of the policy holder
Mahavir Prasad Soni
Indian Banks’ Association A/c Punjab National Bank
4.
Name of insurer
The United India Insurance Company Ltd.
5.
Date of repudiation
28.01.2020
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
26.07.2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of claim
Rs.7635/-
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
12.
Amount of relief sought
Rs.7635/-
13.
Complaint registered under Rule No.
of the Insurance Ombudsman Rules
2017
Rule 13(1)(b)- Any Partial or total repudiation of claims
by an Insurer
14.
Date of hearing
07.09.2021
Place of hearing
Delhi, Online via Cisco WebEx & Telecall
15.
Representation at the hearing
For the Complainant
Shri Mahavir Prasad Soni, the Complainant
For the Insurer
Smt. Pamela Pinto, Deputy Manager (LCD), Mumbai
16.
Date of Award/Order
Recommendation under Rule 16, 06.09.2021
(i) Brief Facts of the Case:
Shri Mahavir Prasad Soni (hereinafter referred to as the Complainant) has filed this
complaint against the decision of The United India Insurance Company Ltd. (hereinafter
referred to as the Insurers) alleging wrong rejection of Mediclaim.
(ii) Cause of Complaint:
Complainant's Argument:
The Complainant has stated that thetotal bills for domiciliary mediclaim of his wife at AIIMS
were 15 and the claim amount was Rs.13614/-. He submitted all the bills to the Insurance
Company but his claim was repudiated on the ground of claim document deficiency.
Further he raised this issue with the Grievance Deptt. of the Insurance Company and
requested to settle the claim at least for Rs.7635/- for which original bills have been
received by the TPA but Insurance Company refused to settle the claim.
Case of Mahavir Prasad Soni versus The United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-2122-0316
b) Insurer's Argument:
The Insurance Company, vide Self Contained Note dated 13.08.2021, has stated that the
Complainant and his dependent members were covered under Group Mediclaim Policy issued
to Indian Banks Association – Punjab National Bank. After receiving the domiciliary claim of
23.08.2019 at AIIMS, the query for deficient documents were raised but there was no reply
from the Complainant even after sending stipulated query reminders to insured. Hence, claim
was repudiated as per Clause No.5.6 for claim document deficiency.
19. Reason for registration of Complaint: Rejection of Mediclaim.
a) The following documents were placed for perusal:
1. Copy of policy.
2. Copy of GRO Letter, query letter, reply of query, bills, claim form, rejection letters.
3. SCN of the Insurers along with enclosures.
b) Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.

At this stage the Insurers inform that they are agreeable to settle the claim for Rs. 7585. The
Complainant accepts this offer. Thus an agreement of conciliation could be arrived at between the
Complainant and the Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall settle the claim for Rs. 7585.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman
September 06, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ashutosh Sinha versus Star Health and Allied Insurance Company Ltd.
Complaint Ref. No.: DEL-H-044-2122-0309
1.
Name & Address of the Complainant
Shri Ashutosh Sinha
J-1101, Pioneer Park, Sector 61,
Gurugram, Haryana-122005
2.
Policy No.
Type of Policy
Policy term/policy period
P/161219/01/2020/000059
Group Health Insurance Policy
08.09.2019 to 07.09.2020
3.
Name of the insured
Name of the policy holder
Sneha Sinha
Axtria India Private Limited
4.
Name of insurer
Star Health and Allied Insurance Company Ltd.
5.
Date of repudiation
17.12.2019
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
06.08.2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of claim
Rs.120000/- as per Form VI A
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
12.
Amount of relief sought
Rs.120000/- as per Form VI A
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims
by an Insurer
14.
Date of hearing
15.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
Shri Ashutosh Sinha, the Complainant
For the Insurer
1. Dr. Madhukar Pandey, Chief Manager (Health Claims)
2. Shri Mantosh Kumar, Sr. Manager (Claims)
16.
Date of Award/Order
Recommendation under Rule 16/ 15.09.2021
17.Brief Facts of the Case: Shri Ashutosh Sinha (hereinafter referred to as the Complainant) has
filed this complaint against the decision of Star Health and Allied Insurance Company Ltd.
(hereinafter referred to as the Insurers) alleging wrong rejection of Mediclaim.
18.Cause of Complaint:
Complainant's Argument: His wife had a planned surgery for fibroid removal via uterine
artery/fibroid embolization (UAE/UEF) for which pre-authorization approval for Rs.30000/- was
given by the Insurance Company. On the date of the procedure 5
th
Nov’19, a representative
from Star Health visited hospital and inquired about the condition, procedure as well as for pre-
authorization approval. Next day, on 6
th
Nov. 2019, i.e. on the day of discharge, they waited for
10 hours for final cashless settlement but Insurance Company refused to settle the cashless
claim on the ground that Gynecologist opinion was not taken. He then filed reimbursement
claim but the same was not settled. He approached the Grievance Cell who also reiterated the
same reasons for rejection of his claim. He has now approached this forum for relief.
Case of Ashutosh Sinha versus Star Health and Allied Insurance Company Ltd.
Complaint Ref. o.: DEL-H-044-2122-0309
b) Insurer's Argument: The Insurance Company, vide Self Contained Note dated 24.08.2021, has
stated that the insured was admitted in Fortis Hospital from 05.11.2019 to 06.11.2019 and was
diagnosed with Diffuse Adenomyosis. Insured submitted a Pre authorization request for cashless
treatment on 02.11.2019 and the same was initially approved for a sum of Rs.30000/- and
subsequently the cashless approval was withdrawn because Gynecologist opinion was not
obtained for uterine fibroid embolization. The insured submitted the reimbursement claim for
medical expenses. From the Discharge Summary, it was observed that the insured patient was
admitted for Uterine Artery Embolization for Uterine Fibroids/Adenomyosis without prescription
or advice from a Gynecologist. Hence, the claim was repudiated as per Exclusion Clause no. 14 of
the policy. Exclusion Clause 14 states: “The Company shall not be liable to make any payment
under this policy in respect of any expenses what so ever incurred by the insured person in
connection with or in respect of Dietary supplements and substances that can be purchased
without prescription, including but not limited to Vitamins, minerals and organic substances
unless prescribed by a medical practitioner as part of hospitalization claim or day care
procedure”.
19. Reason for registration of Complaint: Rejection of Mediclaim as stated in para 18 (a) above.
c) The following documents were placed for perusal.
4. Copy of policy.
5. GRO letter, pre-authorization approval, pre-authorization withdrawal, discharge, query
letter, rejection letter.
6. SCN of the Insurer along with enclosures.
d) Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to admit and settle the claim as per the policy terms and
conditions as a one-time exception. The Complainant accepts this offer. Thus an agreement of
conciliation could be arrived at between the Complainant and the Insurers, which I consider as
fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall admit and settle the claim as per
the policy terms and conditions as a one-time exception.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 15, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Vineet Kapoor versus The United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-2122-0360
1.
Name & Address of the Complainant
Shri Vineet Kapoor
Kedar Square, L-29/5, DLF Phase-2,
Gurugram, Haryana-122008
2.
Policy No.
Type of Policy
Policy term/policy period
2214002817P104805321
Tailor Made Group Health Policy
03.06.2017 to 02.06.2018
3.
Name of the insured
Name of the policy holder
Vineet Kapoor
M/s Welue Strategic Alliances Pvt. LTd
4.
Name of insurer
The United India Insurance Company Ltd.
5.
Date of repudiation
02.07.2021
6.
Reason for grievance
Inadequate settlement of Mediclaim
7.
Date of receipt of the complaint
30.08.2021
8.
Nature of complaint
Inadequate settlement of Mediclaim
9.
Amount of claim
Rs.5,30,000/-
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
Rs.2,00,000/-
12.
Amount of relief sought
Rs.3,30,000/-
13.
Complaint registered under Rule No.
of the Insurance Ombudsman Rules
2017
Rule 13(1)(b)- Any partial or total repudiation of claims
by an Insurer
14.
Date of hearing
22.09.2021 & 29.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
Shri Vineet Kapoor, the Complainant
For the Insurer
1. Shri Sanjeev Kumar, Deputy Manager, DO-14,
Gurgaon
2. Ms Rajni Ahuja, Dy. Manager, RO-2 Delhi
16.
Date of Award/Order
Award under Rule 17/ 30.09.2021
17.Brief Facts of the Case: Shri Vineet Kapoor (hereinafter referred to as the Complainant) has
filed this complaint against the decision of The United India Insurance Company Ltd. (hereinafter
referred to as the Insurers) alleging inadequate settlement of Mediclaim.
18.Cause of Complaint:
Complainant's Argument: The Complainant had taken the subject Group Mediclaim Tailor-
made Policy for Sum Insured of Rs.35 lakh for himself, spouse, parents and parents-in-law and
the policy cover the dental treatment without any limits and without any riders. His mother-in-
law was treated for dental treatment between 17.04.2017 to 21.08.2017 and paid Rs.5,30,000/-
in 9 parts during the treatment period, which involved full mouth rehabilitation workup through
multiple long restoration sessions. He filed the claim for Rs.5,30,000/- and Insurance Company
settled the claim for Rs.2,00,000/- with a large deduction of Rs.3,30,000/-. He approached the
Grievance Cell of the Insurance Company and the claim was still rejected under the reasonably
and customary clause.
Case of Vineet Kapoor versus The United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-2122-0360
b) Insurer's Argument: The Insurance Company, vide Self Contained Note dated 20.09.2021, has
stated that the Complainant was covered under Group Health Policy covering himself, spouse,
parents and Parent-in-laws. The Complainant lodged a claim for Rs.5,30,000/- on 30.11.2017 for
dental treatment of his Mother-in-law, Smt. Ashima Gupta. As the dental treatment was taken on
OPD basis, the claim was assessed and settled for Rs.2,00,000/- as per Policy Condition No.2.35-
Reasonable and Customary Charges. In order to verify the comparative charges with the prevailing
fees in the region, a local investigation was carried out. Accordingly , the claim was settled as per
policy condition 2.35 and informed to the Complainant.
19. Reason for registration of Complaint: Inadequate settlement of Mediclaim.
e) The following documents were placed for perusal.
7. Copy of policy.
8. Copy of GRO Letter, discharges summaries, bill, claim form, settlement letters.
9. SCN of the Insurers along with enclosures.
f) Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The claim relates to the treatment of Smt. Ashima Gupta, Mother-in-law of the Complainant for
the period from 17.04.2017 to 21.08.2017 in 9 sittings. Out of these, 4 were on 17.4.2017 (Rs.
10000), 22.04.2017 (Rs. 20000), 18.05.2017 (Rs. 1 lakh) and 29.05.2017 (70000), which were prior
to the commencement of the policy, i.e. 03.06.2017, and hence inadmissible for reimbursement
under the policy. The rest of the 5 sittings were during the policy period and the bills paid
amounted to Rs. 3.30 lakh. The Insurers have examined the rates for their Network Hospital (Aster
Hospital, Bengaluru), which is Rs. 97,500, which is lower than the amount of Rs. 2 lakh that they
had settled the claim for. The Insurers have argued that they have thus settled the claim under the
definition of ‘medical expenses’ and ‘reasonable and customary charges’ per clauses 2.22 and 2.35
of the Policy. However, while these clauses are generally applicable for claims under the policy,
this Tailor-made Policy has made specific provision of ‘OPD coverage without any limit’. Therefore,
the clam will have to be examined for the 5 sittings without any limit. The complaint deserves to
be allowed to this extent only.
Award
The complaint is allowed partially as stated above. Accordingly, the Insurers should settle the
claim for the five OPD sittings of the insured falling under the Policy period, without any monetary
limit, as per the terms and conditions of the Policy, after adjusting for the partial settlement
already made, within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 30, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Rakesh Ranjan versus Star Health Insurance Company
Complaint Ref. No.: DEL-H-044-2122-0443
1.
Name & Address of the Complainant
Shri Rakesh Ranjan S/o Chandramani Singh,
At+ Post, Dariapur, P.S. Muffasil,
Distt. Munger, Pin-811201, Bihar
2.
Policy No.
Type of Policy
Policy term/policy period
P/161211/01/2020/005099
Group Health Insurance Policy
14.08.2019 to 13.08.2020
3.
Name of the insured
Name of the policy holder
Rakesh Ranjan
Somani Kanak Seedz Pvt. Ltd.
4.
Name of insurer
Star Health Insurance Company
5.
Date of repudiation
17.09.2020
6.
Reason for grievance
Repudiation of Mediclaim
7.
Date of receipt of the complaint
08.09.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs.1,75,000/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs.2,00,000/- as per Form VI
13.
Complaint registered under Rule No.
of the Insurance Ombudsman Rules
2017
Rule 13(1)(b)- Any Partial or total repudiation of claims
by an Insurer
14.
Date of hearing
29.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx
15.
Representation at the hearing
For the Complainant
Shri Rakesh Ranjan, the Complainant
For the Insurer
1. Dr. Madhukar Pandey, Chief Manager (Health
Claims)
2. Shri Matosh Kumar, Senior Manager (Claims)
16.
Date of Award/Order
Recommendation under Rule 16/ 29.09.2021
17.Brief Facts of the Case: Shri Rakesh Ranjan (hereinafter, ‘the Complainant’) has filed this
complaint against the decision of The Star Health Insurance Company (hereinafter, ‘the Insurers’)
alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
i. Complainant's Argument: The Complainant had stated that his newborn baby son had some
breathing complication after birth and was hospitalized in Silliguri Neotia Getwell Health Care
,West Bengal from 20.02.2020 to 29.02.2020. As the hospital was expensive, after getting LAMA
discharge, they continued the treatment in Bachha Hospital, Katihar from 01.03.2020 to
11.03.2020. They had informed the insurance company for baby addition and submitted
reimbursement claims but insurance company had not settled the claim as new baby was not
covered from day one and baby treatment is not covered under their policy. He represented to
Insurance company on 09.08.2020 but they have not settled the claims.
Case of Rakesh Ranjan versus Star Health Insurance Company
Complaint Ref. No.: DEL-H-044-2122-0443
ii. Insurer's Argument: The Insurance Company, vide Self Contained Note dated 16.09.2021 has
stated that Complainant was a member covered under Group Medical Health Insurance Policy.
The insured raised two reimbursement claims in respect of Baby of Mrs. Roji Kumari, wife of
insured , in 2
nd
year of Mediclaim policy, one for Rs.1,40,341/- towards hospitalization expenses
at Neotia Getwell Healthcare Centre, Siliguri, West Bengal for the period 20.02.2020 to
29.02.2020 and 2
nd
claim for Rs.35,011/- towards medical expenses incurred in Bachcha
Hospital, Katihar for the period 01.03.2020 to 11.03.2020. As per discharge summary, the new
born baby was diagnosed with Sepsis with Neonatal Jaundice and was kept in observation and
was given vaccination and screening test, which was not covered, as per terms and conditions
of the policy. Moreover, the baby is not endorsed in policy as member covered. Hence they had
repudiated the claims as per Exclusion No.5 of the policy and special condition regarding
midterm inclusion of any employees and dependents.
19. Reason for registration of Complaint: Repudiation of Mediclaim.
20. The following documents were placed for perusal:
10. Copy of policy.
11. Copy of GRO Letter, discharge summary, bills
12. SCN of the Insurer along with enclosures.
21.Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offers to review and settle the claim as per the terms & conditions of
policy in respect of the hospitalisation of the baby in Neotia Getwell Healthcare Centre, Siliguri
and Bachcha Hospital, Katihar, subject to submission of the Bills of tests done and medicine
bills. The Complainant accepts this offer. Thus an agreement of conciliation could be arrived at
between the Complainant and the Insurers, which I consider as fair and reasonable for both the
parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall review and settle the claim as per
the terms & conditions of policy in respect of the hospitalisation of the baby in Neotia Getwell
Healthcare Centre, Siliguri and Bachcha Hospital, Katihar, subject to submission of the Bills as
mentioned above.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 29, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Ranjana Sinha versus The United India Insurance Company Ltd.
Complaint Ref. No.: DEL-H-051-2122-0442
1.
Name & Address of the Complainant
Smt. Ranjana Sinha, H.No. 283, 2
nd
Floor, Hauz Rani,
Malviya Nagar, New Delhi-110017
2.
Policy No.
Type of Policy
Policy term/policy period
5001002819P112786266
Group Health Insurance Policy
01.11.2019 to 31.10.2020
3.
Name of the insured
Name of the policy holder
Hari Prakash Sinha (Husband)
Indian Bank Association A/c Allahabad Bank
4.
Name of insurer
The United India Insurance Company Ltd.
5.
Date of repudiation
N.A.
6.
Reason for grievance
Inadequate settlement of Mediclaim
7.
Date of receipt of the complaint
10.09.2021
8.
Nature of complaint
Inadequate settlement of Mediclaim
9.
Amount of claim
Rs.5,09,493/-
10.
Date of partial settlement
30.12.2020 & 15.02.2021
11.
Amount of partial settlement
Rs.1,72,205/-
12.
Amount of relief sought
Rs.3,50,000/- as per Form VI
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of
claims by an Insurer
14.
Date of hearing
29.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx
15.
Representation at the hearing
For the Complainant
1. Smt. Ranjana Sinha, the Complainant
2. Ms Neha Sinha, D/o the Complainant
For the Insurer
Smt. Pamela Pinto, Dy. Manager (LC&B), Mumbai

16.
Date of Award/Order
Recommendation under Rule 16/ 29.09.2021
17.Brief Facts of the Case: Smt. Ranjana Sinha (hereinafter, ‘the Complainant’) has filed this
complaint against the decision of The United India Insurance Company Ltd. (hereinafter, ‘the
Insurers’) alleging inadequate settlement of Mediclaim.
18.Cause of Complaint:
iii. Complainant's Argument: Her husband, Dr. Hari Prakaksh Sinha was admitted to
Pushpanjali Hospital, Agra on 21.07.2020 and was transferred to Nayati Hospital (Covid
hospital) after being diagnosed of corona positive on 26.07.2020, where he expired on
06.08.2021. She submitted the claim for reimbursement for Rs.5,81,713/- but insurance
company had credited Rs.33,947/- on 30.12.2020 and Rs.1,38,258/- on 15.02.2021 after
several reminders without any details of deduction. Insurance Company had again credited
Rs.8,150/- on 02.07.2021 without any intimation or details. She approached the insurance
company but her balance claim was not settled.
iv. Insurer's Argument: The Insurance Company, vide revised Self Contained Note dated
27.09.2021 has stated that they had received two reimbursement claims towards
hospitalization expenses in respect of the insured Dr. Hari Prakash Sinha for Rs. 72,278/-
incurred at Pushpanjali Hospital and Rs. 5,09,493/- at Nayati Health Care, Agra. Out of
the claimed amount, Rs. 33,947/-were settled under Base Policy (Sum Insured
Exhausted) and Rs. 1,38,258/- under Top Up policy totaling to Rs. 1,72,205/-. Out of
Balance claim of Rs. 4,09,566/-, Rs. 3,37,289/- deducted as per G.I. Council Rates and Rs.
72,278/- not paid through oversight. They had further stated that they had paid Rs.
14350/- per day towards treatment cost in Nayati Health Care, which is as per
Reasonable & Customary Clause of the policy. Hence the claim was settled as per GI
Council Rates and Policy Terms & Conditions.
19. Reason for registration of Complaint: Inadequate settlement of Mediclaim
20. The following documents were placed for perusal:
13. Copy of policy.
14. Copy of GRO Letter, discharge summary, bills
15. SCN of the Insurer along with enclosures.
g) Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offers to review and settle the claim as per the Policy terms &
conditions up to the SI under the Top-up Policy and also to pay interest in terms of the
provisions of the IRDAI (Protection of the Policyholders’ Interest) Regulations 2017. The
Complainant accepts this offer. Thus an agreement of conciliation could be arrived at
between the Complainant and the Insurers, which I consider as fair and reasonable for
both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall review and settle the claim as per the
Policy terms & conditions up to the SI under the Top-up Policy and also to pay interest in terms of
the provisions of the IRDAI (PPHI) Regulations 2017.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 29, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Manish Sharma versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0359
1.
Name & Address of the Complainant
Shri Manish Sharma
2264/172, Ganesh Pura, Tri Nagar,
New Delhi-110035
2.
Policy No.
Type of Policy
Policy term/policy period
360305501910005905
Parivar Mediclaim Policy
05.03.2020 to 04.03.2021
3.
Name of the insured
Name of the policy holder
Manish Sharma
Manish Sharma
4.
Name of insurer
The National Insurance Company Ltd.
5.
Date of repudiation
27.01.2021
6.
Reason for grievance
Rejection of Mediclaim
7.
Date of receipt of the complaint
09.08.2021
8.
Nature of complaint
Rejection of Mediclaim
9.
Amount of claim
Rs.54095/- as per Form VIA
10.
Date of partial settlement
N.A
11.
Amount of partial settlement
N.A
12.
Amount of relief sought
Rs.54095/- as per Form VIA
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of
claims by an Insurer
14.
Date of hearing
22.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx
15.
Representation at the hearing
For the Complainant
Shri Manish Sharma, the Complainant
For the Insurer
Shri Govind Lal, Admin. Officer, DA Br., Punjabi Bagh
16.
Date of Award/Order
Award under Rule 17/ 22.09.2021
17.Brief Facts of the Case: Shri Manish Sharma (hereinafter referred to as the complainant) has filed
the complaint against the decision of The National Insurance Company Ltd. (hereinafter referred to
as the Insurers or the Respondent Insurance Company) alleging wrong rejection of Mediclaim.
18.Cause of Complaint:
v. Complainant's Argument: The Complainant had stated the he made two claims for Injection
Rituximab for Rs.54095/-. Further he stated that he was patient of Acquired homophiles.
Doctor prescribed him for Injection Rituximab in Govt. Hospital AIIMS and that was not
immunotherapy. Insurance Company rejected his claim by giving irrelevant reasons
whereas his claim was genuine. He approached the Grievance Cell of the Insurance
Company but his claim was not settled.
Case of Manish Sharma versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0359
vi. Insurer's Argument: The Insurance Company, vide Self Contained Note dated 15.09.2021,
has stated that on scrutiny of the documents, it was observed that the patient availed
treatment in AIIMS Hospital with the diagnosis of ‘Acquired Hemophilia (FVIII INH) &
underwent “Rituximab Therapy”. The Complainant has lodged 2 claims for treatment of
Acquired Hemophilia & underwent Rituximab Therapy on 17.03.2020 & 01.04.2020 on
Short admission basis in AIIMS, New Delhi. The hospitalization was solely for
Immunotherapy, which on a standalone basis does not require hospitalization and was
not listed in the day care procedure annexed at appendix 1 of the policy. Hence the
claim was repudiated as per Policy Clause No. 3.11 and list of Day Care Procedure
Appendix 1.
19. Reason for registration of Complaint: Rejection of Mediclaim as stated in para 18 (a)
above.
h) The following documents were placed for perusal.
16. Copy of policy.
17. Copy of GRO Letter, discharge summary, bills, rejection letters.
18. SCN of the Insurer along with enclosures.
i) Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
I have examined the arguments and the evidence submitted by both the parties. The Complainant
had lodged two claims for treatment of Acquired Hemophilia and underwent Rituximab Therapy
on 17.03.2020 & 01.04.2020 on Short-admission basis in AIIMS, Delhi. The Insurers had
determined that the hospitalization was solely for immunotherapy, which on a standalone basis
does not require hospitalization and was not listed in the admissible day care procedures listed in
Appendix 1 of the policy. There was error on the part of the Insurers in arriving at this
determination. Hence the claims were rightly repudiated as per Policy Clause No. 3.11 read with
the list of admissible Day Care Procedures vide Appendix 1. Pursuantly, the complaint shall
deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 22, 2021
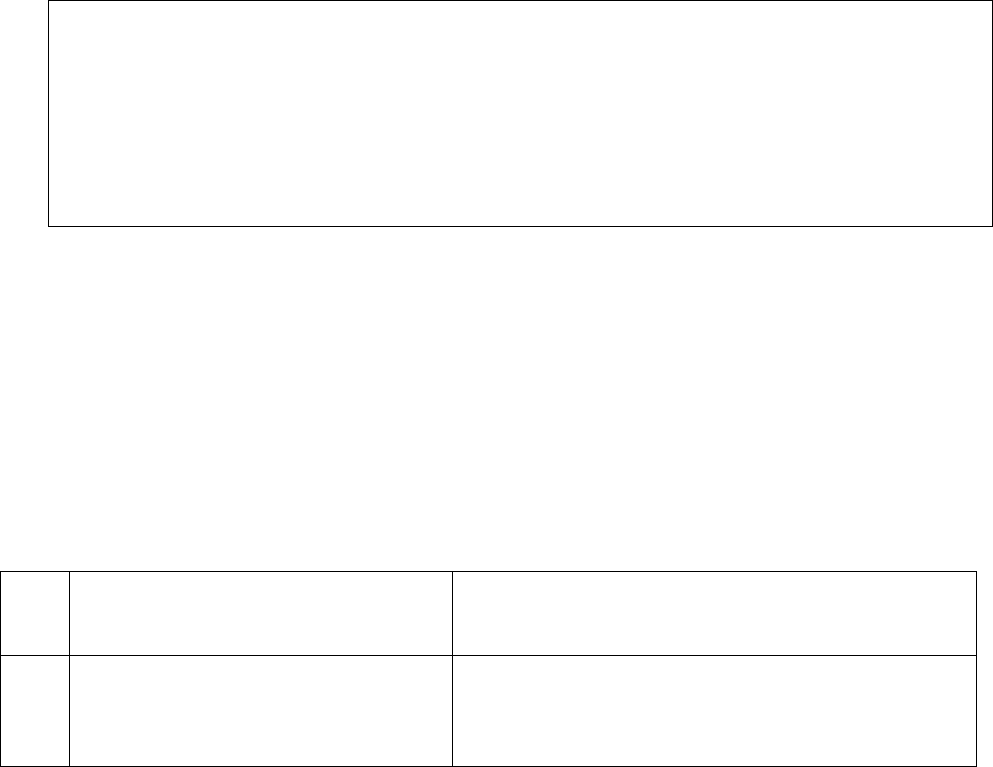
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Sandeep Saxena versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0421
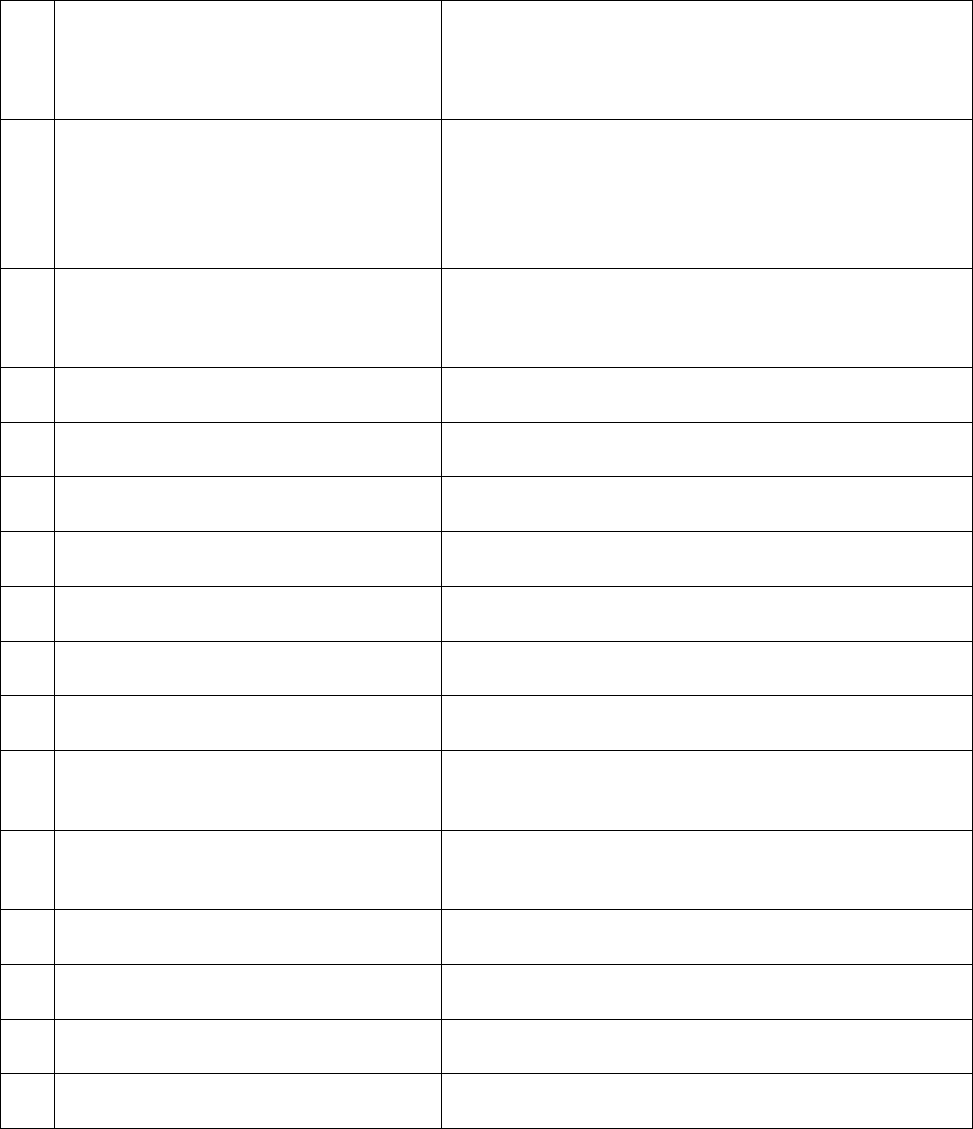
1.
Name & Address of the Complainant
Shri Sandeep Saxena
151, Vigyapan Lok Apartments, Mayur Vihar Extension
Phase-1, Delhi-110091
2.
Policy No.
360801502010004633
National Parivar Mediclaim
16.11.2020 to 15.11.2021
Type of Policy
Policy term/policy period
3.
Name of the insured
Name of the policy holder
Namita Kapoor Saxena
Sandeep Saxena
4.
Name of insurer
The National Insurance Company Ltd.
5.
Date of repudiation
N.A.
6.
Reason for grievance
Inadequate settlement of Mediclaim
7.
Date of receipt of the complaint
03.09.2021
8.
Nature of complaint
Inadequate settlement of Mediclaim
9.
Amount of claim
Rs.1,12,857
10.
Date of partial settlement
16.06.2021
11.
Amount of partial settlement
Rs.70,634
12.
Amount of relief sought
Rs.42,223
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of claims
by an Insurer
14.
Date of hearing
22.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx App
15.
Representation at the hearing
For the Complainant
Shri Sandeep Saxena, the Complainant
For the Insurer
Shri Puneet Bhatia, Divisional Manager, DO-34
16.
Date of Award/Order
Recommendation under Rule 16/ 22.09.2021
17.Brief Facts of the Case:
Shri Sandeep Saxena (hereinafter, ‘the Complainant’) has filed this complaint against the
decision of The National Insurance Company Ltd. (hereinafter ‘the Insurers’) alleging
inadequate settlement of Mediclaim.
18.Cause of Complaint:
vii. Complainant's Argument: The Complainant had stated that his wife Smt. Namita Kapoor
was admitted in Bansal Hospital from 01.05.2021 to 03.05.2021 for the treatment of
COVID-19 Pneumonia. He applied for the reimbursement of claim for Rs.1,12,857/- but
Insurance Company reimbursed only Rs.70,634/-with a deduction of Rs.42,223/- citing
Government guidelines. He approached the Grievance Cell of the Insurance Company but
his balance claim was not settled.
Case of Sandeep Saxena versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0421
viii. Insurer's Argument: The Insurance Company, vide Self Contained Note has stated that the
patient Smt. Namita was admitted in Bansal Hospital, Delhi on 01.05.2021 with complaints
of Generalised weakness, shortness of breath, Ghabrahat, Dry cough, low grade fever, dry
mouth, and was diagnosed with Covid-19 pneumonia. She was discharged on 03.05.2021,
after hospitalization for 2 days. The reimbursement claim was approved and paid for
Rs.70,634/- on 21.06.2021 as per circular dated 20.06.2020 issued by the Govt. of National
Capital Territory of Delhi. A sum of Rs.42,223/- was deducted towards non-payable items
and deduction details were informed to the Complainant. Hence, claim was paid as per
Policy clause 6.42 of Reasonable and Customary charges, circular of Govt. of National
Capital Territory of Delhi and Table of Benefits limit for ambulance charges.
(iii) Reason for registration of Complaint: Inadequate settlement of Mediclaim.
j) The following documents were placed for perusal:
19. Copy of policy.
20. Copy of GRO Letter, Discharge summary, hospital bills, claim form, settlement details.
21. SCN of the Insurer along with enclosures.
k) Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer to make payment for Pharmacy charges (Rs. 11163), Lab Tests
charges (Rs. 19316), and Physiotherapy charges (Rs. 1491), totaling to Rs. 31970, in full and final
settlement of the balance claim. The Complainant accepts this offer. Thus an agreement of
conciliation could be arrived at between the Complainant and the Insurers, which I consider as fair
and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall make a payment of Rs. 31,970, as
noted above, to the Complainant in full and final settlement of the balance claim.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 22, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Seema Gupta versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0357
1.
Name & Address of the Complainant
Smt. Seema Gupta
G-23/278, Sector-7, Rohini, Delhi-110085
2.
Policy No.
Type of Policy
Policy term/policy period
360400502010000170
Parivar Mediclaim
15.04.2020 to 14.04.2021
3.
Name of the insured
Name of the policy holder
Seema Gupta
Seema Gupta
4.
Name of insurer
The National Insurance Company Ltd.
5.
Date of inadequate settlement
09.03.2021
6.
Reason for grievance
Inadequate settlement of Mediclaim
7.
Date of receipt of the complaint
16.08.2021
8.
Nature of complaint
Inadequate settlement of Mediclaim
9.
Amount of claim
Rs.78831/-
10.
Date of partial settlement
-----
11.
Amount of partial settlement
Rs.65165/-
12.
Amount of relief sought
Rs.13666/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules 2017
Rule 13(1)(b)- Any Partial or total repudiation of
claims by an Insurer
14.
Date of hearing
22.09.2021
Place of hearing
Delhi, Online Video Conferencing via Cisco WebEx
App
15.
Representation at the hearing
For the Complainant
1. Smt. Seema Gupta, the Complainant
2. Shri Arjun Gupta, s/o the Complainant
For the Insurer
Shri Puneet Kanoria, Sr. Divl Manager DO-9, Rohini

16.
Date of Award/Order
Recommendation under Rule 16/ 22.09.2021
17.Brief Facts of the Case:
Smt. Seema Gupta (hereinafter referred to as the complainant) has filed the complaint
against the decision of The National Insurance Company Ltd. (hereinafter referred to as the
Insurers) alleging inadequate settlement of Mediclaim.
18.Cause of Complaint:
ix. Complainant's Argument: The Complainant was admitted at Shree Aggarsain International
Hospital from 26.02.2021 to 06.03.2021. Hospital bill was for Rs.78831/- but Insurance
Company settled the bill for Rs. 65165/-. She paid a sum of Rs.13666/- to the hospital.
After discharge she requested the Insurance Company for balance claim but they did not
pay the balance claim. She approached the Grievance Cell of the Company but there was
no relief.
Case of Seema Gupta versus The National Insurance Company Ltd.
Complaint Ref. No.: DEL-H-048-2122-0357
x. Insurer's Argument: The Complainant was admitted in Shree Aggarsain International
Hospital from 26.02.2021 to 06.03.2021 with complaints of Type 2 Diabetes Mellitus with
Acute meningitis. The claim was settled and a sum of Rs.13666/- was deducted for non-
medical items. The Insurance Company has carefully reviewed all the documents on
record and observed that a further payment of Rs.8536/- can be made as per policy terms
and conditions. Further the Insurance Company gave the detail of balance payment of
Rs.5130/- (PPE Kit, examination gloves, dietician, admission charges, medical evaluation
etc.) which were not payable under the policy.
19. Reason for registration of Complaint: Inadequate settlement of Mediclaim.
20.The following documents were placed for perusal.
22. Copy of policy.
23. Copy of GRO Letter, discharge summary, bills, deductions mail.
24. SCN of the Insurer along with enclosures.
21.Result of hearing with the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
At this stage, the Insurers offer (a) to pay an additional amount of Rs. 8536 as stated in Para 18b
above and another sum of Rs. 2000 towards the PPE Kit and (b) to write to the Hospital with copy to
the Complainant to explain to the Complainant the reasons for collection of the remaining amount
of Rs. 3130 and if there are no justification, refund the same to the Complainant. The Complainant
accepts this offer. Thus an agreement of conciliation could be arrived at between the Complainant
and the Insurers, which I consider as fair and reasonable for both the parties.
Award
The complaint is resolved in terms of the agreement of conciliation arrived at between the
Complainant and the Insurers. Accordingly, the Insurers shall (a) pay to the Complainant an
additional amount of Rs. 8536 as stated in Para 18b above and another sum of Rs. 2000 towards
the PPE Kit and (b) write to the Hospital with copy to the Complainant to explain to the
Complainant the reasons for collection of the remaining amount of Rs. 3130 from her and if there
are no justification, refund the same to the Complainant.
Parties should implement this agreement within 30 days.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 22, 2021
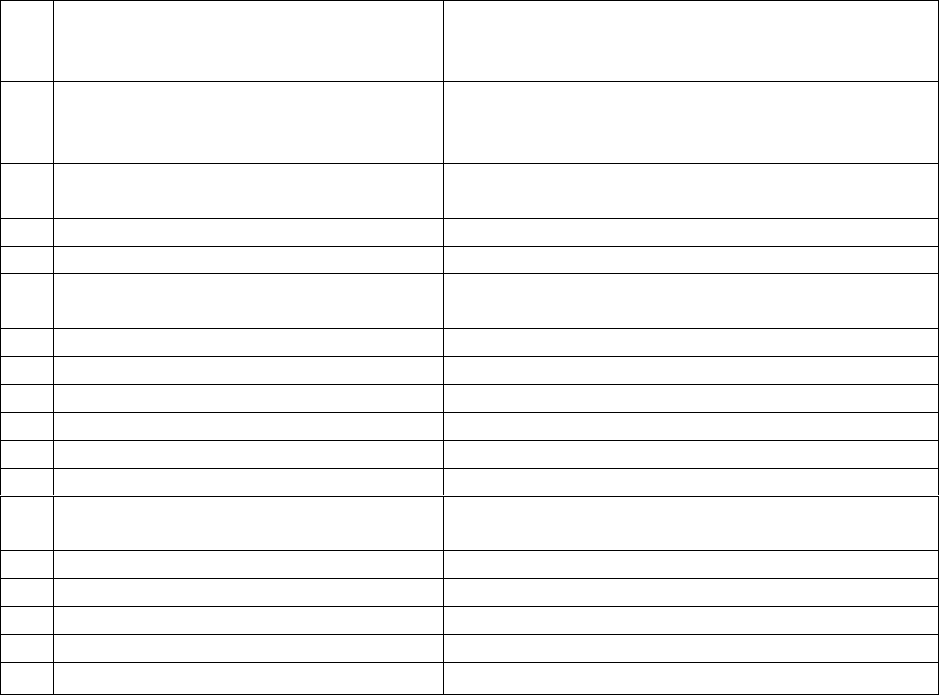
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Khairati Lal Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0344
17.Brief Facts of the Case: Shri Khairati Lal (hereinafter referred to as the Complainant) has filed this
complaint against the decision of The Oriental Insurance Company Ltd. (hereinafter referred to as the
Insurers) alleging wrong repudiation of Mediclaim.
2. Cause of Complaint:
Complainant's Argument: His wife Smt. Veena Grover was hospitalized in Fortis Hospital, Delhi
from 13.11.2020 to 15.11.2020 for treatment of heart disease and hypertension. Cashless request
was sent from hospital on 13.11.2020 for estimated treatment cost of Rs. 291400/- but the same was
denied by TPA stating that the patient was admitted for heart disease & hypertension and there is
waiting period of Hypertension and related complications. Complainant had to pay bill of Rs.
284956/- on discharge. Later, he filed reimbursement claim Rs. 284956/- along with Hospital
certificate that patient had no past history of DM. But Insurance Company rejected the claim with
same reason. He wrote to GRO on 26.07.2021 but did not get the claim. Therefore, he has now
approached this forum for relief.
Case of Khairati Lal Versus The Oriental Insurance Company Ltd.
1.
Name & Address of the Complainant
Shri Khairati Lal
B-199, 1st Floor, Gujaranwala Town, Part-I,
New Delhi-110009
2.
Master Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
272900/48/2020/17482
PNB-Oriental Mediclaim Policy-2017
03.01.2020 To 02.01.2021
3.
Name of the insured
Name of the policy holder
Veena Grover
Khairati Lal
4.
Name of the insurer
The Oriental Insurance Company Ltd.
5.
Date of repudiation
27.01.2021
6.
Reason for repudiation
As per Exclusion Clause-4.2(xvii) – Waiting period of
2 years from inception of policy
7.
Date of receipt of the complaint
02.03.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 284956/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 284586/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of
claims by an insurer
14.
Date of hearing/place
28.09.2021, Delhi, Online, Via WebEx
15.
Representation at the hearing
For the Complainant
Shri Khairati Lal, the Complainant
For the insurer
Smt. Updesh Kaur, Admin. Officer, DO-29, Delhi
16.
Date of Award/Order
Award under Rule 17/ 28.09.2021
Complaint Ref. No.: DEL-H-050-2122-0344
Insurer's Argument: The Insurers in their SCN dated 13.09.2021 have stated that the
Complainant’s spouse Veena Grover was admitted with acute AWMI, planned for CAG+PTCA, Stent to
LAD, HTN. Reimbursement claims of Rs. 284956/- was received on 01.12.2020 against hospitalization
expenses incurred during hospitalization from 13.11.2020 to 15.11.2020 in Fortis Hospital, Delhi. The
claim was denied as the policy was in first year and as certified by doctor that patient was
hypertensive at the time of admission, which is a risk factor/cause of heart related disease. As per
Exclusion Clause 4.2(XVII) “the expenses on treatment of following ailments/diseases/surgeries, if
contracted and/or manifested after inception of first policy, are not payable during the waiting period
of 02 years for Hypertension. Hence cashless request and reimbursement claim was rejected as per
terms and conditions of the policy.
3. Reason for registration of Complaint: Repudiation of Mediclaim.
4. The following documents were placed for perusal:
Discharge Summary
Repudiation Letter
GRO
5. Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The subject policy was issued in January 2020. The claim relates to hospitalisation of the insured in
November 2020, which was the first year of the policy. The diagnosis included hypertension (HTN) and
heart related ailments. The policy prescribes a waiting period of two years for HTN. Therefore, the
Insurers were justified in repudiating the claim and, pursuantly, the complaint shall deserve to be
rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September 28, 2021
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, DELHI
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Ombudsman: Shri Sudhir Krishna
Case of Pradeep Babbar Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0367
17.Brief Facts of the Case: Shri Pradeep Babbar (hereinafter referred to as the Complainant) has filed
this complaint against the decision of The Oriental Insurance Company Ltd. (hereinafter referred to as
the Insurers) alleging wrong repudiation of Mediclaim.
18.Cause of Complaint:
Complainant's Argument: He was hospitalized in Institute of Liver & Biliary Science (ILBS), Delhi
from 01.11.2020 to 03.11.2020 for treatment of liver problem. He incurred expenses of Rs. 55548 on
treatment including pre-post expenses. He filed reimbursement claim, which was denied by the Insurers
stating that he was having history of alcohol intake as per Discharge Summary. Complainant submitted
rectified Discharge Summary with remark “wrongly written”, but Insurance Company did not consider it.
Earlier complainant’s claim of hospitalization at Grover Nursing Home was paid but insurance Company
repudiated this claim without any ground in spite of submission of rectified Discharge Summary. He wrote
1.
Name & Address of the Complainant
Shri Pradeep Babbar
11/327, Geeta Colony, Krishna Nagar,
New Delhi-110009
2.
Master Policy No:/Certificate No.
Type of Policy
Duration of policy/Certificate period
271700/48/2021/673
Happy Family Floater -2015
02.07.2020 To 01.07.2021
3.
Name of the insured
Name of the policy holder
Pradeep Babbar
Pradeep Babbar
4.
Name of the insurer
The Oriental Insurance Company Ltd.
5.
Date of repudiation
05.01.2021
6.
Reason for repudiation
Patient having history of alcoholic intake, hence
claim repudiated as per policy clause 4.8
7.
Date of receipt of the complaint
03.08.2021
8.
Nature of complaint
Repudiation of Mediclaim
9.
Amount of claim
Rs. 55548/-
10.
Date of partial settlement
N.A.
11.
Amount of partial settlement
N.A.
12.
Amount of relief sought
Rs. 55548/-
13.
Complaint registered under Rule No. of
the Insurance Ombudsman Rules, 2017
Rule 13(1)(b) – any partial or total repudiation of
claims by an insurer
14.
Date of hearing/place
28.09.2021, Delhi
15.
Representation at the hearing
For the Complainant
Shri Pradeep Babbar, the Complainant
For the insurer
Shri Kushal Kumar, AO, DO-14
16.
Date of Award/Order
Award under Rule 17
to GRO on 18.04.2021 but claim was denied again with the same reason. Therefore, he has now
approached this forum for relief.
Insurer's Argument: The Insurers in their SCN dated 21.09.2021 have stated that the complainant
was hospitalized in Institute of Liver & Biliary Science from 01.011.2020 to 03.11.2020 for the treatment of
Acute
Case of Pradeep Babbar Versus The Oriental Insurance Company Ltd.
Complaint Ref. No.: DEL-H-050-2122-0367
Pancreatitis, for which he filed claim of Rs. 36778/-. The claim was repudiated by Insurance Company as
per Clause 4.8 of the policy stating that patient was having a history of alcohol intake as mentioned in
Discharge Summary. Later on, complainant submitted Discharge Summary with some corrections
regarding word Ethanol, taking alcohol, written wrongly. The same was investigated by TPA and they
reverted that as per investigation reports there was no change in Hospital record and that of the status of
the claim. Therefore, claim was repudiated rightly as per policy terms and condition. As regards of earlier
claim of hospitalization in R S Grover Memorial Hospital from 31.10.2020 to 01.11.2020, cashless facility
was availed by the insured because as per referral summary provided by the hospital the facts of “ any
history of alcohol or tobacco intake” were not disclosed by the hospital due to which the claim was
approved. But under the present case, etiology was mentioned as “alcohol” in Discharge Summary, hence
claim was repudiated.
19.Reason for registration of Complaint: Repudiation of Mediclaim.
20.The following documents were placed for perusal:
Discharge Summary
Repudiation Letter
GRO
21.3Result of hearing of the parties (Observations and Conclusion):
Case called. Parties are present and recall their arguments as noted in Para 18 above.
The Insurers had repudiated the claim citing Clause 4.8 on the ground of the insured having a history of
alcohol intake as mentioned in Discharge Summary, as stated in Para 18b above. The Complainant argues
that the certificate dated 12.02.2021 from the ILBS Delhi, states that he is on treatment for chronic calcific
pancreatitis (and other diseases). The Complainant argues that the ailments mentioned in this certificate
relate to non-alcoholic matters. However, the repudiation involved in this complaint relates to his history
of alcohol intake as mentioned in Discharge Summary for 01-03.11.2020, which were confirmed by the
Investigator appointed by the Insurers. The Insurers clarify that the settlement made for him on an earlier
occasion was not based on such investigation and thus the two settlements are not exactly comparable.
Upon examination of the arguments and the evidence submitted by both the parties, it is concluded that
the Insurers had based their findings about the Complainant’s history of alcohol intake on the Discharge
Summary and further investigations. As such, the Insurers were justified in repudiating the claim and,
pursuantly, the complaint shall deserve to be rejected.
Award
The complaint is rejected.
(Sudhir Krishna)
Insurance Ombudsman, Delhi
September28, 2021
AWARD NO.IO/KOC/A/HI/0254/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0229
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 10.09.2021
1.
Name and Address of the complainant
:
Ms. Saramma Jacob as Saramma Mathew
L-102 Julee Villa,Changampuzha Nagar P O,
Cochin 682033
2.
Policy Number
:
0504002820P102561452

3.
Name of the Insured
:
Ms. Saramma Jacob as Saramma Mathew
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
02.06.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
10.08.2021
9.
Parties present at the hearing
For the Complainant
:
Ms. Saramma Jacob as Saramma Mathew
(Online)
For the Insurer
Mr. I Muralidhar (Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Ms. Saramma
Jacob as Saramma Mathew is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that she is a holder of Insurance policy no.0504002819P103946127 valid for
the period from 18/03/2018 to 18/03/2021. She has been paying her insurance premium without
fail and as per the insurance premium, for any hospitalization or activity leading to the civil are
entitled to claim upto 5,00,000/-. She was admitted in Caritas Hospital, Thellakom, Kottayam dated
on 13/09/2020 vide IP No.A299326. She had done her Angioplasty to SVG to D1, OM1 and
Rotablation with the prior approval of Health Insurance HITPA and same is dated on 15/09/2020.
Before the surgery, she intimated to the insurance agency and remitted a caution deposit of
Rs.5000/- as per the hospital instruction. Subsequently to the surgery, she received a letter and the
same is stating that her claim has been rejected and it is due to ineligibility. But the reason for
ineligibility (Sec. 2.37 – pre-existing disease) stated in the letter are faulty. She wanted to tell the
forum that she do not have any pre-existing disease within 36 months prior to the first policy. Also
wanted to inform that she is a widow living with pension only.
2. The Respondent Insurer entered appearance and filed a self contained note. It is
submitted that Mrs. Saramma Jacob has taken AB Arogyadaan Group Medical Insurance
Policy No.0504002820P102561452 with the period of insurance from 09.06.2020 to
08.06.2021 for a sum Insured of 5,00,000/- and the policy is serviced by the Third Party
Administrators - M/s Health Insurance TPA of India Limited.
HOSPITALISATION DETAILS:
Mrs. Saramma Jacob was admitted at M/s Caritas Hospital, Thellakom PO, Kottayam, Kerala on
13.09.2020 due to the complaints of Coronary Artery Disease - Post CABG 2009 - Recent Acute
Coronary Syndrome, Coronary Angiogram - Triple vessel disease — Satisfactory LV Function - Now
Angioplasty to SVG to D1 OM1 and Rotablation of RCA done on 15.09.2020 and discharged on
17.09.2020.
CLAIM DETAILS
The complainant has lodged a claim for Rs.3, 25,549/-/- with the servicing TPA towards the
expenses incurred by her in connection with treatment at the above said hospital. The TPA
has registered the claim with them. The f1edical Team of the TPA M/s Family Health Plan
Limited has decided to repudiate the claim on the grounds that the present hospitalization
and treatment under the present policy is for a Pre-existinq disease.
CAUSE OF GRIEVANCE
Aggrieved with the repudiation of the claim, the claimant has approached the O/o the
Honorable Insurance Ombudsman, Kochi. This led to the present complaint before the
Honorable Insurance Ombudsman, Kochi.
DECISIO N OFDIVISIONAL OFFICE: HYDERABAD

The respondent submit herewith the grounds on which they have repudiated the claim and
highlight the following facts in support of our decision.
The company submit the Certificate of Insurance, Hospital records before Honorable
Insurance Ombudsman, Kochi for their kind perusal. Further we furnish herewith the
following in support of our claim.
The Insured has taken Insurance Policy for the first time with period of insurance from
08.03.2018 to 08.06.2018 subsequently it was renewed for further period of one year up
to 08.06.2021.
As per Discharge summary of Hospital, it was established that the Patient already
undergone CABG (Coronary Artery Bypass Graft) on 2009 itself and also suffering from
Type 2 Diabetes Miletus, Hypertension & Dyslipidemia.
On the date of surgery i.e. 15.09.2020, the policy was not completed 36 months from the
date of issuance of policy i.e. on 08.03.2018. Hence the present treatment comes under
pre-existing disease.
Based on the above points, the treatment is for a Pre-existinq disease as on the date of
the issue of the policy and therefore rightfully construed to be a case of Pre-existinq nature.
The Medical Team of the TPA M/s Health Insurance TPA of India Limited has also decided
to repudiate the claim on the g rounds that the complaints mentioned in Discharge
summary are related to Pre-existing disease under exclusion No.5.1 which reads as:
The Company shall not be liable to make any payment under this policy in respect of any
expenses whatsoever incurred by any Insured Person in connection with or in respect of:
The company shall not be liable to ma ke any payment under the policy in connection with
or in respect of the following expenses till the expiry of waiting period mentioned below:
Pre-Existing Diseases (Code-Excl.01)
Expenses related to the treatment of a pre-existing disease (PED) and its
direct complications shall be excluded until the expiry of 36 months of
continuous coverage after the date of inception of the first policy with us.
In case of enhancement of sum insured the exclusion shall apply afresh
to the extent of sum insured increase.
If the Insured Person is continuously covered without any brea k as
defined under the portability norms of the extant IRDAI (Health Insurance)
Reg ulations, then waiting period for the same would be reduced to the extent
of prior coverage.
Coverage under the policy after the expiry of 36 months for any pre-
existing disease is subject to the same being declared at the time of application
and accepted by us.
Hence, they submit that our stand in repudiation of the claim is in order.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that She she is a
widow, living with pension only. She was admitted in Caritas Hospital, Thellakom, Kottayam had
done her Angioplasty to SVG to D1, OM1 and Rot ablation with the prior approval of Health
Insurance HITPA. Before the surgery, she intimated to the insurance TPA and remitted a caution
deposit of Rs.5000/- as per the hospital instruction. Subsequently to the surgery, she received a
letter stating that her claim has been rejected for the reason of pre-existing disease. She submitted
the forum that she do not have any pre-existing disease within 36 months prior to the first policy.
Also submitted that she got his cashless claim approved for the treatment done in Renai Medicity in
the month of August 2020 from 10/08/2020 to 14/10/2020 for the same illness. The Respondent
Insurer submitted that as per the discharge summary issued by M/s Renai Medicity Multi Super
Speciality Hospital, Palarivattom, Kochi with the date of admission as 10/08/2020 and discharge date
as 14/08/2020, wherein it was clearly mentioned that Coronary Artery Disease, S/P CABG. But they
have not mentioned previous history of the patient. Hence inadvertently the company processing
TPA has processed the claim for Rs.73,771/-, even though the discharge summary clearly mentioned
about the CAGG. The claim was processed erroneously and claim approved wrongly. This was
recoverable from the TPA. In the present claim, the discharge summary of M/s Caritas Hospital,
Thellakom, Kottayam, it was clearly mentioned about the past history of the patient, hence the TPA
has rejected the claim based on the past history of the patient.
4. After hearing the Respondent Insurer and perusing the complaint and the exhibits produced
before the forum, I find that the policy was not completed 36 months from the date of issuance of
policy i.e.08/03/2018 and as per discharge summary it was established that the patient already
undergone CABG on 2009 itself and also suffering from T2DM, HTN and Dyslipidemia and therefore I
find no reason to interfere with the decision of the insurer in repudiating the claim for non
disclosure of material facts which is the cardinal rule governing any insurance contract.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 10
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0255/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-003-2122-0369
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 13.09.2021
1.
Name and Address of the complainant
:
Mr. Chandrasekharan P V
'SREYAS', Karumala P O, Balussery Via,
Kozhikode - 673612
2.
Policy Number
:
PE02152597
3.
Name of the Insured
:
Mr. Chandrasekharan P V
4.
Name of the Insurer
:
HDFC Ergo Health Insurance Ltd
5.
Date of receipt of Complaint
:
12.07.2021

6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
09.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. Chandrasekharan P V (Online)
For the Insurer
:
Mr. Aneesh Bhaskaran (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Mr.
Chandrasekharan P V is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he is a health insurance policy holder with HDFC ERGO General Health
Insurance Co. with policy no.P02152597/2811203858435600000. The claim preferred by him was
repudiated and the request for reconsideration also was rejected. Canara Bank , the agent ,didn`t
respond to any of the letter, email despite repeated reminders. Neither the Proposal nor the policy
certificate was given to him though the bank had assured that it will be send through registered
post. Originally the health insurance policy was with the Apollo Munich in 2019, but was intimated
by HDFC Ergo to make renewal premium in their name. On 19.2.21, he was admitted at the Malabar
Medical College Hospital, Kozhikode and underwent Angioplasty and was discharged on 23.2.21. On
submitting the claim form on 2.3.21 for Rs.1,32,432/-, the claim was rejected stating that on
verification there was a past history of Renal Cell carcinoma Nephrectomy in 2017, prior to the
policy inception, under section 7 of the policy whereas he had not made any incorrect health
decleration.
2. The Respondent Insurer entered appearance and filed a self contained note. It is
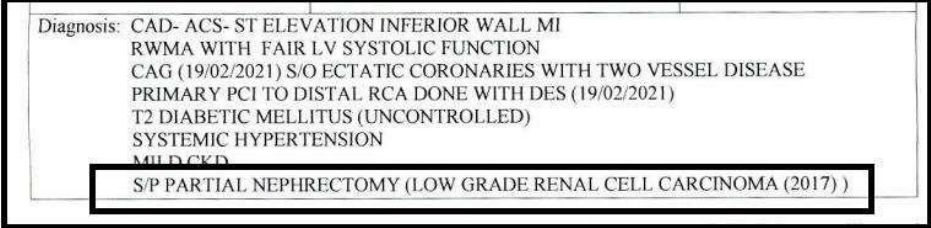
submitted that
the Insured had taken a Group Assurance Health Plan viz Group Policy
No 2999203834944600000 , Policy NO 2811203858435600000 for the period from
25/ 04/2020 to 24/ 04/ 2021 for self at a Sum Insured of Rs. 2,00,000/ -. The policy
was issued to the complainant with express terms, conditions and exclusions
thereon. The said terms and conditions of the policy are binding on the parties to the
contract of insurance. The Complainant states that he was hospitalized at Malabar
Medical College Hospital
and
Research Centre for the period from 19/ 02/ 2021 to 23/
02/ 2021 diagnosed with Coronary Artery aneurysm.
The Respondent Insurer further
submit that, on receipt of claim papers, medical records related to the alleged
treatment including bills and after due verification, it was observed that the
discharge summary shows that the
Insured had low grade Renal
Cell
Carcinoma
in 2017. Copy of the Discharge Summary is shown below:
As per the Discharge Summary, the insured was diagnosed with Coronary artery
aneurysm but it was observed that, Insured had a history of Carcinoma which was
not disclosed to the Insurer amounting to Non-Disclosure. The Insurance contract
is dominated by the legal maxim “the utmost good faith”. The observance of
utmost good faith by the parties is vital to a contract of insurance. The non-
disclosure of a material fact by the Insured whether fraudulent or innocent,
has the same effect of avoiding the contract. If the proposer conceals or
misrepresents material facts, the contract is vitiated. Deliberate concealment
or misrepresentation amounts to fraud, and the policy is legally void. Innocent
misstatement or misrepresentation renders the policy voidable at the option of
the insurer. The Respondent Insurance company addressed letter of
repudiation dated 06/ 04/ 2021 repudiating the claim on the ground of Non-
Disclosure of material facts.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that . On
19.2.21, he was admitted at the Malabar Medical College Hospital, Kozhikode and underwent
Angioplasty and was discharged on 23.2.21. On submitting the claim form on 2.3.21 for
Rs.1,32,432/-, the claim was rejected stating that on verification there was a past history of Renal
Cell carcinoma Nephrectomy in 2017, prior to the policy inception, under section 7 of the policy
whereas he had not made any incorrect health declaration. . The Respondent Insurer submitted that
The Complainant was hospitalized at the Malabar Medical College Hospital
and
Research
Centre for the period from 19/ 02/ 2021 to 23/ 02/ 2021, diagnosed with Coronary Artery
aneurysm.
On receipt of claim papers, medical records related to the treatment including
bills, on verification, it was observed that the
complainant had low grade Renal
Cell
Carcinoma in 2017 as per
the discharge summary. The complainant therefore had a history
of Carcinoma which was not disclosed to the Respondent Insurer amounting to Non-
Disclosure. The claim was denied.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted by them. In this complaint where the claim for Angioplasty was denied, the respondent
insurer argued that on verification of the claim related records, it was noticed that
the
complainant
had low grade Renal
Cell
Carcinoma in 2017, not
disclosed to the Respondent Insurer
amounting to Non-Disclosure of material facts and the policy was cancelled; are all tenable.
I therefore do not want to interefere in the decision of the respondent insurer in rejecting
the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 13
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0259/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-050-2122-0356
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.

AWARD PASSED ON 15.09.2021
1.
Name and Address of the complainant
:
Mr. Aleyas K V
Aleyas K V, Kumamkottil House,
Pothanicad P O, Ernakulam-686671
2.
Policy Number
:
441700/48/2021/1519
3.
Name of the Insured
:
Mr. Aleyas K V
4.
Name of the Insurer
:
The Oriental Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
09.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
07.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. Aleyas K V (Online)
For the Insurer
:
Mr. Rajan M (online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is Rejection of mediclaim. The complainant, Mr. Aleyas K V is the
policyholder.
Averments in the complaint are as follows:
The Complainant stated that he suffered severe headache and was under the treatment of doctor
at Pothanikad. On advice, he approached Rajagiri Hospital for MRI scan , where he got admitted on
15/1/2021 and discharged on 16/1/2021. He was then referred to Ophthalmologist there, and after
tests was advised cataract surgery and treatment for migraine. His claim for hospitalization in
Rajagiri Hospital was lodged with TPA at their office but was rejected.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
the complainant was insured under PNB ORIENTAL MEDICLAIM POLICY from 16/11/20 to
15/11/2021 and the insured admitted at Rajagiri Hospital on 15/01/21 and discharged on
16/01/2021.
Mr. Aleyas K.V. submitted the claim with Good Health Insurance TPA for Rs 15,735/- and they
repudiated the claim. Then he gave a complaint at Regional Office Kochi. The R.O authority agreed
with the decision of the TPA and denied the claim and now the insured has given complaint at the
Hon. Insurance Ombudsman.
From verification of the medical reports, it is found that the insured was admitted for diagnosis . As
per exclusion clause 4 of the policy, expenses incurred at hospital or nursing home primarily for
evaluation/ diagnostic purposes which is not followed by active treatment for the ailment during the
hospital period is excluded from the scope of the policy.
In view of the above, pray that Hon'ble Ombudsman may be pleased to accept the submission and
the complaint may be dismissed.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he had
taken policy through Punjab National Bank . He suffered persistent headache and was advised to
consult neurologist. He was also referred to ophthalmologist. Both the doctors advised him to get
MRI scan done and he was admitted for taking the scan. He was not given room and was admitted
in the ward . On 16/1/2021 , he was taken on wheel chair , for the scan. He was prescribed medicine
for 14 days and asked to take treatment for migraine and cataract. The Respondent Insurer
submitted that there was no active line of treatment during hospitalization. The claim was denied
because the admission was only for taking MRI Brain.
4. I have heard both the sides and perused the documents. The Discharge Summary states diagnosis
as ‘ New onset headache-probable primary’ and the course in the hospital is mentioned as ‘
Magnetic Resonance Imaging is done , which is unremarkable.’
According to GENERAL EXCLUSIONS under the policy, Exclusion 4.9, ‘Expenses incurred at Hospital or
Nursing Home primarily for evaluation / diagnostic purposes which is not followed by active
treatment for the ailment during the hospitalized period, ’ are not payable. The claim is therefore,
not tenable.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 15
TH
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0265/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(c) READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-003-2122-0253
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 15.09.2021
1.
Name and Address of the complainant
:
Mr. Muraleedharan N R
Krishna, KRA 64, Kesari College Road,
North Parur - 683513
2.
Policy Number
:
PE01516132|PE01516077
3.
Name of the Insured
:
Mr. Muraleedharan N R
4.
Name of the Insurer
:
HDFC Ergo Health Insurance Ltd
5.
Date of receipt of Complaint
:
07.06.2021
6.
Nature of complaint
:
Non issue of policy document
7.
Amount of relief sought
:
--

8.
Date of hearing
:
04.08.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. Muraleedharan N R (Online)
For the Insurer
:
Mr. Aneesh Bhaskaran (Online)
AWARD
This is a complaint filed under Rule 13 1(c) read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding non issue of policy document. The complainant, Mr.
Muraleedharan N R is the policyholder.
1. Averments in the complaint are as follows:
The Complainant submitted that he was holding a policy with Appolo Munich through Canara Bank
vide policy No.PE01516132(2019-2020). He is a senior citizen and PF pensioner. He had renewed the
policy on 29 April 2020 through SBI net banking amount shown by HDFC Ergo system was Rs.2360/-
Renewal date was 4
th
May 2020. He had got renewal confirmation Email from the respondent
insurer29th April 2020 itself. Copy attached for reference. Then he got Email message from the
insurer on 5
th
June that his policy is not renewed due to insufficient funds in his canara Bank
account. He replied to the customer care Grievance cell by Email and he had represented his case to
Executive level.
The complainant had tele con with their Mr. Deepak, Mr.Azhar Muhammed on different dates0n
02.07.2020, 16.09.202009.10.2020,03.10.2020,08.10.2020 and 13.10.2020. Finally Mr Prabhakar
told him that their team will be contacting him to solve the problem. So far nothing happened.The
complainant had communicated to them that he is ready to pay the exact premium amount, if they
agreed to issue continuous coverage of policy. Since he know, the premium they have collected less,
even though it is mistake by them. And also kindly note that they have not returned the amount so
collected through their site. So he requests this forum to instruct them to give continuous coverage
this year also and ready to pay this year premium. It is submitted that he is in perfect health without
any severe health problem. Now he is in 2
nd
year without any Health insurance.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
At the Outset, we are agreeable to submit to the mediation of the Hon’ble Insurance Ombudsman in
the instant complaint and for him to give his recommendation for the resolution of the Complaint.
With reference to the Complaint we submit as follows:
Insured, 66 yrs., had taken a Group Assurance Health Plan vide policy no 120100/ 12586/
2019/A012950/PE01516131 valid from 04/May/2019 to 03/May/2020 , Group Policy Holder is
Canara Bank viz Member ID EA01245246 . A premium amount of Rs 4684.12/- was paid.
The Policy was due for a renewal on 03/May/2020. It is the version of the Insured that, he had
initiated a renewal via online on 29/Apr/2020 advance of the last date of renewal however, renewal
was not successful due to insufficient fund, which was conveyed by this Insurer, and this fact has
been admitted by the Insured. It is the Insured averment that, when he tried to renew the policy
through HDFC ERGO Health Insurance Co Ltd website, the amount reflecting on the website was Rs.
23.60/-. This is only a self-serving version of the Insured and he is subjected to strict proof of the
same. The respondent denies the same. That we had sent a Renewal Intimation letter to the Insured
stating that, his Group Assurance Individual / Accidental Death for SI of Rs. 2,00,000/- is due for
renewal.
That we confirm policy was not renewed. However, we would not be able to provide him a renewal,
as we do not have a tie up with Canara bank, however, we can provide him an alternate retail
product, which would have a different premium and issuance of the said policy is subject to
underwriting approval. Our Company is a customer oriented organization, apart from providing the
best service; it has also been our endeavor to retain every customer who had taken Insurance with
us. We further wish to submit that, regardless of sending the renewal intimation, the Insured for
reason best known had not chosen to renew the policy and is now making evasive reasons to
vindicate his dereliction.
The policy was not renewed only due the lapse on the part of the Insured for which this Insurer
cannot be held liable. All the averments made by the Insured are herewith denied.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he was
holding a policy with Appolo Munich through Canara Bank vide policy No.PE01516132(2019-2020).
He had renewed the policy on 29 April 2020 through SBI net banking amount shown by HDFC Ergo
system was only Rs.23.60/- Renewal date was 4
th
May 2020. He had got renewal confirmation Email
from the respondent insurer29th April 2020 itself. Then he got Email message from the insurer on 5
th
June that his policy is not renewed due to insufficient funds in his canara Bank account. He replied to
the customer care Grievance cell by Email and he had represented his case to Executive level. But no
reply was received from the respondent insurer. Being a senior citizen he requires an insurance
coverage . He also submitted that he is ready to pay the premium as required by the insurer for
renewing his policy. The Respondent Insurer submitted that Insured, had taken a Group Assurance
Health Plan vide policy no 120100/ 12586/ 2019/A012950/PE01516131 valid from 04/May/2019 to
03/May/2020 , Group Policy Holder is Canara Bank viz Member ID EA01245246 . A premium amount
of Rs 4684.12/- was paid. The Policy was due for a renewal on 03/May/2020. It is the version of the
Insured that, he had initiated a renewal via online on 29/Apr/2020 advance of the last date of
renewal however, renewal was not successful due to insufficient fund, which was conveyed by this
Insurer, and this fact has been admitted by the Insured. It is the Insured averment that, when he
tried to renew the policy through HDFC ERGO Health Insurance Co Ltd website, the amount
reflecting on the website was Rs. 23.60/-. The insurer confirmed that the policy was not renewed.
However, as they do not have a tie up with Canara bank, the policy cannot be renewed. however,
they could provide him an alternate retail product, which would have a different premium and
issuance of the said policy is subject to underwriting approval.
4. I heard both the parties. The complainant was holding the Policy with Appolo Munich through
Canara Bank. As submitted by him he had renewed the policy on 29 April 2020 through SBI net
banking. The amount shown by HDFC Ergo system was only Rs.23.60/-. Renewal date was 4
th
May
2020. Even though he found that the premium shown through online mode was less compared to
what he was paying, he didn’t get any communication from the respondent insurer regarding more
premium to be paid. He had got renewal confirmation Email from the respondent insurer29th April
2020 itself. The same is submitted before this forum. But he didn’t receive his policy or any further
communication from the insurer. The respondent insurer submitted that the Tie-up with Canara
ended on 15.04.2020 and hence they are not able to renew the policy. The respondent insurer’s
official site has agreed that they have received the premium. Showing a meager premium by the
respondent insurer’s system is a glitch on their part. The respondent insurer didn’t communicate
with the complainant at the Proper time and hence he was not able to renew the policy with any
other insurer. As such this forum feel that the complainant should be provided with a renewal policy
with continuity. As the respondent insurer is not having Tie-up with the Canara Bank since
15.04.2020, they have informed their willingness to offer a retail product “optima Senior”.The
approximate premium amount for a sum insured of Rs.2,00,000/- will be Rs.15137/- plus GST. For
continuity of the policy with the new retail product of the respondent insurer, the complainant has
to pay premium for two policy periods, ie from 04.05.2020 to 03.05.2021 and for 04.05.2021 to
03.05.2022.
In the result, an award is passed, directing the Respondent Insurer to renew the policy wef
04.05.2020 provided the complainant remits adequate premium to that effect, within the period
mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply with the
award within 30 days of receipt of the award and intimate compliance of the same to the
Ombudsman.
Dated this the 15
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0269/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(e)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0361
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the complainant
:
Mr. Baby P Xavier
Pallippadan House, CNRA-56, Karukutty P O,
Ernakulam - 683576
2.
Policy Number
:
1013032818P109971817
3.
Name of the Insured
:
Mr. Baby P Xavier

4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
12.07.2021
6.
Nature of complaint
:
Terms and conditions of policy
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. Baby P Xavier (Online)
For the Insurer
:
Ms. L Ambili (Online)
AWARD
This is a complaint filed under Rule 13 1(e) read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding terms and conditions of policy. The complainant, Mr. Baby
P Xavier is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had taken Synd Arogya policy of the respondent insurer United India
Insurance company w.e.f 01/11/2018, the same was continued for 2 years i.e. upto 31/10/2020.
When he approached the Syndicate Bank for third renewal, the bank informed him that they
stopped the agency tie up with United India Insurance Company and started tie up with Bajaj
Alliance General Insurance company. The Bajaj Alliance company offered fresh policy only, so he
taken Arogya Raksha Policy of the same insurance company through another corporate agency
Indian Bank with exactly the same terms and conditions without any break in insurance. Now the
respondent insurer clarified his grievance about the continuity benefit of the present policy that
there will not be any continuity when he changed from one Bank group policy to another Bank group
policy as per guidelines issued by IRDA on Migration and Portability of health insurance policies.
Denying the renewal of his policy by the respondent insurer with the same terms and conditions as
group policy after completing 2 years period is unethical and illegal action.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
the complainant insured Mr.Baby P Xavier was covered under IBA Group policy till 31/10/2018 by
their LCB office, Mumbai vide policy No.5001002817P112454676. Then he had taken fresh
Syndarogya Group Health policy from Branch Office No.3, Ernakulam for the period from
01/11/2018 to 31/10/2019 vide policy no.1013032818P109971817, it is renewed further for another
period from 01/11/2019 to 31/10/2020 vide policy no.1013032819P109478152. Then he took the
policy Indian Bank Arogya Raksha Group Health policy bearing No.0105002020484100001044288 for
the period from 28/10/2020 to 31/09/2021.
Reason for rejection: The company has examined his grievance and observed that the Company is
not in a position to consider his request favourable in view of the IRDA circular
No.IRDA/HTR/REG/CIR/003/01/2020 dated 01/01/2020 on Migration and Portability of health
Insurance policies. In all the cases of switching from one product to another by the complainant
insured, the customer did not follow the Migration/Portability rules as per IRDA guidelines on
Portability / Migration. In view of the above, the company has taken the decision of not giving
continuity is strictly in accordance with the IRDA Circular No.IRDAI/HLT/REG/CIR/003/01/2020 dated
01/01/2020 and further circular No.IRDA/HLT/REG/CIR/249/10/2020 dated 07/10/2020. Hence the
respondent insurers humbly request the Hon’ble Ombudsman to dismiss the complaint.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he took
Indian Bank Arogya Raksha Group Health Policy through Indian Bank issued by the respondent
insurer with an intention to get the continuity benefit from his previous insurance policy Synd
Arogya Group Health Policy issued by the same insurer. The terms and conditions of both the
policies are similar and the intermediary is different. He took the policy without any break in
insurance. In response to his query regarding the continuity benefit, the respondent insurer clarified
that there will not be any continuity when he changed from one bank to another bank. The
Respondent Insurer submitted that the complainant insured was covered under IBA Group Health
Policy till 31/10/2018 and the reason for discontinuation of this policy is known to him only. Then he
had taken fresh Synd Arogya Group Health policy from one of their branches for the period from
01/11/2018 to 31/10/2019. After the second renewal, he took the Indian Bank Arogya Raksha
Group Health Policy for the period from 28/10/2020 to 31/09/2021. The company is not in a
position to favorably consider his request for continuity, as the insured did not follow the
Migration/Portability rules as per IRDA issued guidelines.
4. While scrutinizing the submitted documents and evidences I find that the policy inception date of
IBA Retirees policy was 01/11/2017 and the Arogya Raksha (Group Health Insurance Scheme) policy
with policy inception date is 28/10/2020. The complainant insured has not taken the policy through
the portability facility provided by the insurers for getting the continuity benefit from the previous
policies. Although the complainant is said to have the previous health insurance policies with the
respondent insurer United India Insurance, it is not noted in the current policy. The insured’s should
renew the health insurance policy through the portability facility only, and then only they will get the
continuity benefits. As per the norms on Portability under Group Health Insurance policies issued by
IRDA – Members of an indemnity based group health insurance policy offered to account holders
of a bank are allowed portability of their coverage to another indemnity based group health
insurance policy offered by a different insurer to the account holders of the same bank. After
hearing the complainant and the respondent insurer and perusing the exhibits produced before the
forum, I find that the complainant insured is a retired bank employee and he is well aware of the
terms, conditions and limitations of the policies. If possible, the insured persons should continue
with their existing health insurance policies to avoid further complications. So I find no reason to
interfere with the decision of the respondent Insurance Company in denying continuity.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0270/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0320
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 17.09.2021
1.
Name and Address of the complainant
:
Mr. C Gopalakrishnan
H-42,'Gopavatom' Rose Gardens, Thiruvambady
P O, Thrissur-680022
2.
Policy Number
:
5001002819P100000001
3.
Name of the Insured
:
Mr. C Gopalakrishnan
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
28.06.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. C Gopalakrishnan (Online)

For the Insurer
:
Mr. Pushkaraj S Bandal (Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Mr. C
Gopalakrishnan is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his wife has been undergoing treatment for breast cancer in Amala
Institute of Medical Science, Thrissur since the year 2017. The respondent insurer United India
Insurance Co has been taking care of his insurance needs covered under the above referred policy
since then. After his retirement, during the policy period from 01/11/2019 to 31/10/2020, the
respondent insurer repudiated his wife’s claim for the reason that targeted therapy is not admissible
as per policy conditions. This targeted therapy is suggested to continue in patients with HER2
positive MBC who get positive response, optimal duration of which is unknown and needs to be
balanced against treatment toxicity, logistical burden and cost as per the second opinion of
concurrence from the Regional Cancer Centre, Trivandrum.
The following reimbursement claims are pending with the insurer for payment after processing:-
20200908B005RH01979 for Rs.67050/- DOA-04/09/2020 & 2020201102B005RH03213 for
Rs.67246/- DOA-30/10/2020. The illness under treatment is of a ‘Chronic condition’ that is not
curable and only treatable under ‘Medically Necessary Treatment’ as envisioned as per term 2.21
and 2.29 respectively of the policy and it is not at all covered under Term 4, Exclusion. The Hon’ble
Insurance Ombudsman, Kochi under Award No.IO/KOC/A/HI/0318/2020-21 dated 21/12/2020
passed on his earlier complaint in pursuance of the 4 past repudiated claims wherein the Hon’ble
Ombudsman rightly highlighted that “With the technological advancement in the field of medicine,
drugs which would have otherwise required 24 hours hospitalization are being administered as day
care procedures.”
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
they have issued a group Mediclaim policy to Indian Bank retirees without domiciliary
benefit : 5001002819P112203988 for period 01-Nov-2019 To 31-Oct-2020. Gopalakrishnan C along
with his spouse Sasikala K is included by Indian Bank in the list of insured persons. A true certified
photocopy of the policy issued to Indian Bank retirees without domiciliary
benefit : 5001002819P112203988 covering their retirees along with spouse with full terms &
conditions is submitted herewith. Sasikala K was the patient in the claims regarding which the
complaint has been made. The complaint is pertaining to claim number TPA claim numbers
20200908B005RH01979 and 20201102B005RH03213 . On receiving the complaint copy , the claims
are scrutinized by the servicing TPA . The details of the claims are represented under accordingly.
The claim details are :
1. Claim file No. 20200908B005RH01979 in this claim the insured Ms. Sasikala K was
admitted at Amala Cancer Hospital & Research Centre on 04/09/2020 and was discharge the
same day i.e. 04/09/2020. The diagnosis as per the discharge summary was carcinoma right
breast and was admitted for administration of injection transtuzumab and pertuzumab,
which is a monoclonal antibody and not a main chemotherapy drug.
2. Claim file No. 20201102B005RH03213 in this claim the insured Ms. Sasikala K was
admitted at Amala Cancer Hospital & Research Centre on 30/10/2020 and was discharge the
same day i.e. 30/10/2020. The diagnosis as per the discharge summary was carcinoma right
breast and was admitted for administration of injection transtuzumab and pertuzumab,
which is a monoclonal antibody and not a main chemotherapy drug .
The insured patient was admitted for administration of injection transtuzumab and pertuzumab,
which is a monoclonal antibody and not a main chemotherapy drug. These are not payable
standalone and also not covered on day care list. Accordingly the claim has been repudiated. The
claim has been processed as per policy terms and conditions.
Clause 2.10 of the policy reads as under :
DAY CARE TREATMENT: Day care Treatment refers to medical treatment and or surgical
procedure which is : i. undertaken under general or local anesthesia in a hospital/day care
Centre in less than a day because of technological advancement, and ii. Which would have
otherwise required a hospitalization of more than a day. Treatment normally taken on an
outpatient basis is not included in the scope of this definition
As per clause 3.3 of policy : Expenses on Hospitalization for minimum period of a day are admissible.
However, this time limit is not applied to treatments such as:
1
Adenoidectomy
20
Haemo dialysis
2
Appendectomy
21
Fissurectomy /
Fistulectomy
3
Ascitic / Plueral tapping
22
Mastoidectomy
4
Auroplasty not Cosmetic
in nature
23
Hydrocele Surgeries
5
Coronary/ Renal
24
Hysterectomy
Angiography
6
Coronary angioplasty
25
Inguinal/ ventral/
umbilical/ femoral
hernia surgeries
7
Dental surgery
26
Parenteral
chemotherapy
8
D&C
27
Polypectomy
9
Excision of cyst/
granuloma/lump/tumor
28
Septoplasty
10
Eye surgery
29
Piles/ fistula surgeries
11
Fracture including
hairline fracture
/dislocation
30
Prostate surgeries
12
Radiotherapy
31
Sinusitis surgeries
13
Chemotherapy including
parental chemotherapy
32
Tonsillectomy
14
Lithotripsy
33
Liver aspiration
15
Incision and drainage of
abscess
34
Sclerotherapy
16
Varicocelectomy
35
Varicose Vein Ligation
17
Wound suturing
36
All scopies along with
biopsies
18
FESS
37
Lumbar puncture
19
Operations/Micro surgical operations on
the nose, middle ear/internal ear, tongue,
mouth, face, tonsils & adenoids, salivary
glands & salivary ducts, breast, skin &
subcutaneous tissues, digestive tract,
female/male sexual organs.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that his
reimbursement claims pertains to his wife’s treatment for breast cancer are pending with the
respondent insurer. The reason mentioned by the respondent for not settling the claims is ‘targeted
therapy’ is not admissible. His earlier claims were awarded and settled with the interventions of the
Hon’ble Ombudsman, when he was a regular bank employee covered under the Bank Employees
Group insurance. The Respondent Insurer submitted that the subject policy is Group Mediclaim
policy issued to the retirees without domiciliary extension. If at all, the complainant insured had
taken the domiciliary extension by paying an additional premium, these pending claims can be
settled under domiciliary treatment. When he was an employee of the bank, his family is covered
under the group mediclaim policy issued to IBA with wider coverage of domiciliary treatment also.
Hence these claims are not payable as per the Indian Bank retires without domiciliary benefit policy.
4. After hearing the complainant and the respondent insurer and perusing the exhibits produced
before the forum, I find that the complainant being a retired bank employee, the complainant
insured should know the terms, conditions and limitations of the policy he opted. Hence I find no
reason to interfere with the decision of the Insurance Company in repudiating the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 17
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0284/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)g READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-044-2122-0434
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the
complainant
:
Mrs. Jayamani K K
N M Salim & Associates Nikarthil Chambers
Bypass Road Puthiyara Calicut 673004
2.
Policy Number
:
P/181316/01/2022/002146
3.
Name of the Insured
:
Mrs. Jayamani K K
4.
Name of the Insurer
:
STAR HEALTH AND ALLIED INS. CO. LTD.
5.
Date of receipt of Complaint
:
22.07.2021

6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
16.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mrs. Jayamani K K (Online)
For the Insurer
:
Mr. Manu Mohan (Online)
AWARD
This is a complaint filed under Rule 13(1)g read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Mrs. Jayamani K K
is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that she had a mediclaim policy with the respondent insurer since 2019. It
was a group policy of M/s. N.M Salim & Associates, Calicut -673004. During the policy period, her
husband on diagnosis was advised for dialysis, which he was undergoing regularly . The hospital
expenses were duly reimbursed by the respondent insurer. Due to the higher premium for the group
policy, she along with the other policy holders decided to change to retail policy(FHOP) . The details
of premium to be paid by individuals were provided by the respondent insurer, which included her
husband and son. While waiting for the new policy, the renewal of the existing policy expired. It was
then informed verbally that her husband cannot be included in the new policy(FHOP), since his
treatment of dialysis was a continuous process and it may be for a life time. This was not justifiable
since at the time of the change over, her husband was holding a valid insurance policy. Moreover the
premium was also received by the respondent insurer for the new policy. The omission of her
husband`s name was not informed before the expiry of the earlier policy. The complainant further
stated that she had her first policy with the National Insurance Co. Ltd., since May 2012 and the
same was continued till May 2019, when the respondent insurer took over. The complainant prayed
to look into te matter seriously.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
M/s N.M.Salim & Associates had taken a group health insurance policy for their employees from the
insurer for the period from 24/05/2019 to 23/05/2020 and the same was renewed from 24/05/2020
to 23/05/2021 vide Policy No. P/181316/01/2021/000740. In the said policy, the complainant,
Mrs.Jayamani, her husband and son was covered with a sum insured of Rs.2,00,000/-. During the
aforesaid policy period, the complainant had submitted 5 claims before the insurer with regard to
the treatment availed by her husband for the disease, Chronic Kidney Disease. It is submitted that
the insurer had paid all the claim pertaining to the insured based on policy terms and conditions of
the group health insurance policy. As per policy, “ All Pre existing diseases are covered. Since
Chronic Kidney Disease was Pre existing disease, the company has approved claim as per policy
terms and conditions. Thereafter on 24/05/2021, during the renewal of the group policy, the
complainant for the reason only known to her had decided not to continue with the group policy and
had taken a retail policy as Family Health Optima Insurance and also submitted a proposal form for
covering herself, her husband, and their son. In the proposal form, the complainant had revealed
about the previous policy and also stated that an amount of Rs.164000/- was given by the insurer as
claim amount in previous policy period.
After scrutiny of the declaration of the proposal form and the previous claim history, the company’s
medical team had observed that complainant’s husband, was suffering from Chronic Kidney Disease
which was a declined risk. Considering these aspects, the company had decided not to accept the
risk & hence, the company had issued the policy in the name of the complainant and her son for a
sum insured of Rs.3,00,000/- vide Policy No.P/181316/01/2022/002146, excluding her Husband.
It is submitted that as per Protection of Policyholders’ Interests Regulations, 2017 clearly mentioned
the definition of “Proposal form” means a form to be filled in by the prospect in written or electronic
or any other format as approved by the Authority, for furnishing all material information as required
by the insurer in respect of a risk, in order to enable the insurer to take informed decision in the
context of underwriting the risk, and in the event of acceptance of the risk, to determine the rates,
advantages, terms and conditions of the cover to be granted. The risk analysis and underwriting are
matters falling under the discretion of the respective insurer to assess risk and grant cover.
The discretion to accept or reject a proposal is with the company, and only on account of the fact
that the proposal had been submitted by the complainant; she wa s not entitled to compel the
company to insure her husband.. If the health status of the proposer is found satisfactory based on
the facts in the proposal, the insurer would accept the risk and issue policy. If the health status is not
satisfactory, the insurer would deny the policy. The insurer therefore had acted only as per terms
and conditions of the policy. It is submitted that there is no deficiency of service from the side of the
company.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that she was
covered under the group health policy from 2019.taken by M/s N.M.Salim & Associates. Her
husband covered under the policy weas undergoing dialysis for which the respondent insurer was
paying the claim regularly. Since the premium of the said policy was higher, the complainant and
some policy holders decided for retail policy (FHOP) in which her spouse and son was included. The
premium payable was also informed. While waiting for the new retail policy(FHOP), the renewal of
the existing group health policy expired. In the meantime it was also informed by the respondent
that her husband cannot be included. since his treatment of dialysis was a continuous process and it
may be for a life time. This was not justifiable since at the time of the change over, her husband was
holding a valid insurance policy. The complainant prayed to look into the matter seriously. The
Respondent Insurer submitted that the Respondent Insurer entered appearance and filed a self
contained note. M/s N.M.Salim & Associates had taken a group health insurance policy for their
employees from the insurer for the period from 24/05/2019 to 23/05/2020 and the same was
renewed from 24/05/2020 to 23/05/2021 wherein the complainant, her husband and son were
covered for a sum insured of Rs.2,00,000/-. During the aforesaid policy period, the complainant had
submitted 5 claims with regard to the treatment of her husband for the disease, Chronic Kidney
Disease. . It is submitted that the insurer had paid all the claim pertaining to the insured based on
policy terms and conditions of the group health insurance policy. As per policy, “ All Pre existing
diseases are covered. Since Chronic Kidney Disease was Pre existing disease, the company has
approved claim as per policy terms and conditions. Thereafter on 24/05/2021, during the renewal of
the group policy, the complainant for the reason only known to her had decided not to continue
with the group policy and had taken a retail policy as Family Health Optima Insurance and also
submitted a proposal form for covering herself, her husband, and their son. In the proposal form,
the complainant had revealed about the previous policy and also stated that an amount of
Rs.164000/- was given by the insurer as claim amount in previous policy period.
After scrutiny of the declaration of the proposal form and the previous claim history, the company’s
medical team had observed that complainant’s husband, was suffering from Chronic Kidney Disease
which was a declined risk. Considering these aspects, the company had decided not to accept the
risk & hence, the company had issued the policy in the name of the complainant and her son for a
sum insured of Rs.3,00,000/- vide Policy No.P/181316/01/2022/002146, excluding her Husband.
4. I heard the complainant and the respondent insurer and had gone through the records
submitted. In this complainant, the complainant, spouse and son were covered in a group health
policy of her employer since 2019 till 2020. Her spouse’s claim for dialysis were had a higher
premium some of the policy holders along with the complainant decided to switched over to a retail
policy(FHOP). The premium for the same was also informed . While awaiting for the new poilcy, the
previous policy renewal expired. In the meantime the respondent insurer informed that the her
spouse paid regularly by the respondent insurer. During the 2021 renewal as the group policy cannot
be covered since her husband had Chronic Kidney Disease. The respondent insurer argued that
:since his treatment of dialysis was a continuous process and it may be for a life time. This was not
justifiable. The respondemnt insurer argued that during the renewal of the group policy, the
complainant for the reason only known to her had decided not to continue with the group policy and
had taken a retail policy - Family Health Optima Insurance and also submitted a proposal form for
covering herself, her husband, and their son. . In the proposal form, the complainant had revealed
about the previous policy and also stated that an amount of Rs.164000/- was given by the insurer as
claim amount in previous policy period. After scrutiny of the declaration of the proposal form and
the previous claim history, the company’s medical team had observed that complainant’s husband,
was suffering from Chronic Kidney Disease which was a declined risk. Considering these aspects, the
company had decided not to accept the risk & hence, the company had issued the policy in the name
of the complainant and her son for a sum insured of Rs.3,00,000/- vide Policy
No.P/181316/01/2022/002146, excluding her Husband
Considering the tenable arguments put forth by the respondent insurer, I do not want to interfere in
the decision of the respondent insurer in dismissing the complaint.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 29
th
day of September 2021.
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0290/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0287
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 29.09.2021
1.
Name and Address of the complainant
:
Mrs. Lucy Jarard
Qr. No.522, KVB Quarters,Ram Nagar, Salem Bye
pass Road, Karur 639006, Tamilnadu
2.
Policy Number
:
5001002819P111919556
3.
Name of the Insured
:
Mrs. Lucy Jarard
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
23.06.2021
6.
Nature of complaint
:
Rejection of mediclaim (Covid)
7.
Amount of relief sought
:
--
8.
Date of hearing
:
12.08.2021
9.
Parties present at the hearing
For the Complainant
:
Mrs. Lucy Jarard (Online)
For the Insurer
:
Ms. Pamela Pinto(Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Mrs. Lucy Jarard is
the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that when she was residing in quarters in Karur with her family, on
24/8/2020, she was critically ill due to severe fever, cough, body pain, fatigue, severe headache and
loss of smell and taste. Around 17 persons in the locality had Covid 19 then and all were treated in
hospitals or Covid Care Centres to avoid spread of disease. The next day she tested Covid positive
and the Doctor, after examining her , decided to treat her as inpatient considering her previous
records of life threatening conditions and asked her to get admitted in Covid Care Centre in
Coimbatore. She was admitted to Atlas Covid Care Centre, Coimbatore on 26/8/2020 and discharged
on 4/9/2020. She spent Rs. 1,61,676/- but her claim was rejected stating treatment was possible in
OPD. There was no response to her Griev letter Other similar claims have been paid by the Ins. Co.
She requests the Ombudsman to pass an award so that she can realize the amount.

2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
the complainant was insured under Policy No. 5001002819P111919556 / Without dom. for the
period 1-11-2019 to 31-10-2020.
Details:
Name of the Insured Indian Banks’ Association A/C. Federal Bank Ltd.
Name of the Insured Person : Ms. Lucy Jarard
Relationship Self
Claimed Amount 161676/- Claimed for Reimbursement
Hospital Name : Atlas Covid Care ,
Dateof Admission :26/08/2020
Received Date 17/09/2020
Diagnosis / Type of Treatment : Covid -19 Positive,
Cause
The above claim could not be considered for payment due to the following reasons and stands as
repudiated :
As treatment was possible on OPD basis hence this claim is rejected.
The claim has been reviewed again and Respondent Insurer is considering payment of Rs. 1,42,136/-
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that she was
residing in quarters in Karur with her family, on 24/8/2020. Some others in the locality had Covid 19.
She tested Covid positive and she got admitted in a hospital in Coimbatore. The Respondent Insurer
submitted that they are ready to settle the claim.
4. I have heard both the sides and perused the documents. It is observed that a package rate is
charged for room which included food. The respondent insurer has confirmed that room rent is
payable at Rs. 5000/- per day under the policy. The admissible claim amount is Rs. 1,22,136 /-
Bill
Bill Date
Acc. Head
Days/Nos
Req.
Disa.
Allwd.
Remarks
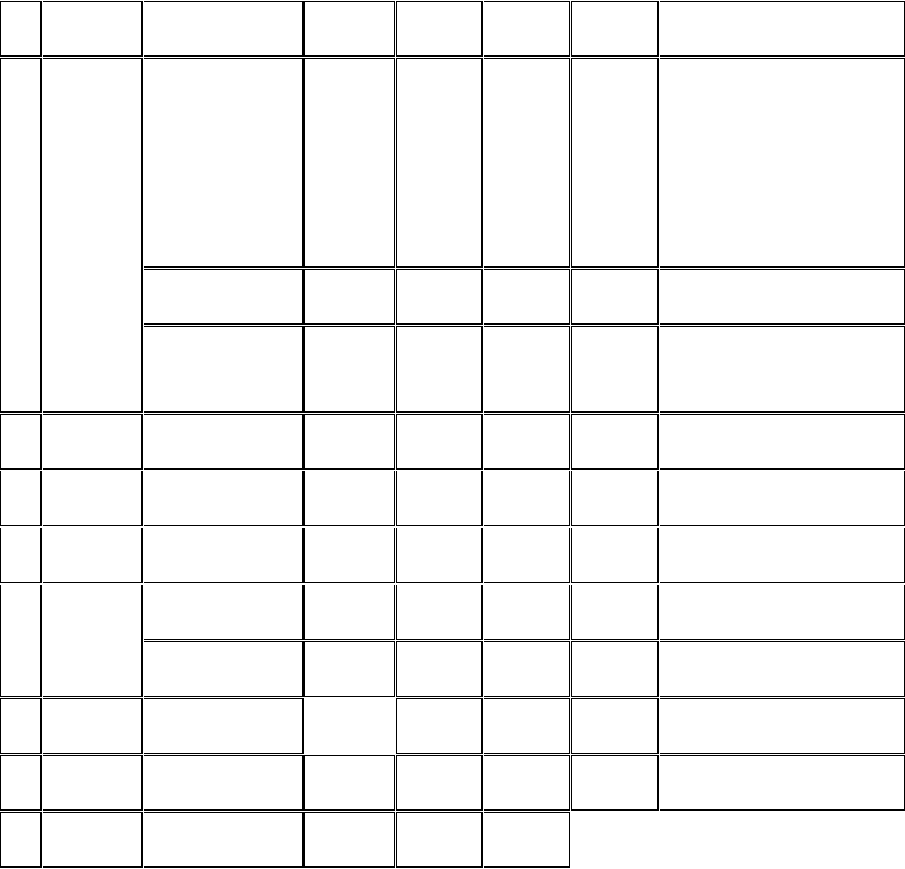
No.
Amt.(Rs)
Amt.(Rs)
Amt.(Rs)
99
04/09/20
Covid package
including
rent,nursing ppe
kit,food,
infection control
etc
10
120000
20000
100000
Laboratory
11020
0
11020
Pharmacy
4501
4039
462
starter
kit,vapouriser,misc.charge
Main bill Total
135521
4039
111482
418
04/09/20
Pharmacy
197
0
197
309
05/09/20
Pharmacy
207
0
207
205
24/8/2020
CT scan
3250
0
3250
Laboratory
4500
0
4500
40
26/8/2020
Ambulance
18000
15500
2500
as per ambulance limit
161675
39539
122136
Payable
122136
In the result, an award is passed, directing the Respondent Insurer to pay an amount of Rs. 122136/-
, within the period mentioned hereunder. No cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply with the
award within 30 days of receipt of the award and intimate compliance of the same to the
Ombudsman.
Dated this the 29
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0298/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13 1(b)READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No.KOC-H-051-2122-0330
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the complainant
:
Mr. K Murugeshan
PNRA 97 MAYURI Changampuzha Nagar Cochin
682033
2.
Policy Number
:
0504002818P103444696
3.
Name of the Insured
:
Mr. Murugesan
4.
Name of the Insurer
:
The United India Insurance Co. Ltd.
5.
Date of receipt of Complaint
:
29.06.2021

6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
08.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. Murugesan (Online)
For the Insurer
:
Mr. Muralidhar (Online)
AWARD
This is a complaint filed under Rule 13 1(b) read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Mr. K
Murugeshan is the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his wife Mrs.K Prabhavathy was submitted a health insurance claim on
06/08/2018 for a total amount of Rs.3,53,561.62 along with all original documents with claim
No.219072 (claim ref no.0504002818C059547001). After almost 2 years and several follow up calls
and emails to Good Health Insurance TPA(GHTPA) and the respondent insurance company United
India Insurance company(UIIC), the claim was repudiated on 01/07/2020. Subsequently, a complaint
with the Grievance Department of UIIC was lodged on 29/07/2020 and on 26/11/2020, he was
informed via email that the claim repudiation was found to be in order. The GHTPA and UIIC have
purposely caused inordinate delays and have wrongly repudiated their claim. The claim was
rejected with reason for repudiation stated as : “As per the details and documents provided it was
noted that the Hospital is registered under the Name Divine, and documents are being generated
under a different name of Maxcare, hence due to discrepancy of hospital name across documents
submitted claim is being recommended for repudiation.”
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
the complainant insured has taken AB Arogyadaan Group Medical Insurance policy
No.0504002818P103444696 with period of insurance from 09/06/2018 to 08/06/2019 for a sum
insured of Rs.5,00,000/- and the policy is serviced by GHTPA. Mrs.K Prabhavathy, w/o Mr.K
Murugesan was admitted at M/s Max Care Hospital, Ottupura, Wadakanchery, Kerala on
18/07/2018 due to the complaints of severe Osteo Arthritis both knee with Genuvaram and
underwent surgery on 19/07/2018 and discharged on 26/07/2018.
The complainant has lodged a claim for Rs.3,53,651/- with the servicing TPA towards the expenses
incurred by her in connection with treatment at the above said hospital. The TPA had registered the
claim No.219072. The medical team of the TPA M/s Good Health Insurance TPA has sent
recommendation to Divisional Office for repudiation of the claim on the grounds that “As per the
documents provided by the insured that the Hospital was registered in the Name of Devine Medical
Centre Limited, Wadakkanchery and Discharge summary and other documents are in the name of
Max Care Hospital, Ottupura. Hence due to the discrepancy of Hospital name across documents
submitted, the claim is being recommended for repudiation as per the Clause 7.14, Disclosure to
information – In the event of misrepresentation, mis-description or non-disclosure of any material
fact. The Divisional Office has sent repudiation letter on 01/07/202 to the insured. Aggrieved with
the repudiation of the claim, the claimant has approached the Grievance cell of the respondent
insurer. The respondent insurer submitted the following points in support of their contention:-
The company reiterate that Final Cash Bills and Discharge summary should be in the Name of
Registered Treating Hospital only.
In this case all the Cash bills are in the name of Devine Medical Centre whereas Discharge
Summary in the name of Max Care Hospital.
Indoor case sheets in the name of Max Care Hospital and also in the name of Devine Medical
Centre.
If the cash bills, Discharge Summary & Indoor case papers in the name of Max Care Hospital,
Registration Certificate has to be submitted for Max Care Hospital.
As per the policy condition No.5.11 HOSPITAL / NURSING HOME: A hospital means any
institution established for in-patient care and day care treatment of illness and / or injuries
and which has been registered as a Hospital with the local authorities under the Clinical
establishments (Registration and Regulation) Act, 2010 or under the en
actments specified under the Schedule of Section.56(1) of the said Act.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that the
respondent insurance company purposefully delayed and denied their long pending hospital
reimbursement claim. The clarification regarding the registration and discrepancies in the
documents produced along with the claim for was already given to the TPA and the Grievance Cell of
the respondent insurance company. The Respondent Insurer submitted that the discrepancy found
across documents submitted like, final cash bill, discharge summary, indoor case sheets and
registration certificate. Hence the claim is being recommended for repudiation by the TPA and
finally by the Grievance cell as per clause 7.14 – disclosure to information – in the event of
misrepresentation, mis-description or non-disclosure of any material fact.
4. After hearing the complainant and the respondent insurer and perusing the exhibits produced
before the forum, I find that the hospital registered in one name and the documents produced are in
different names. Although as per the instruction from this forum the complainant insured produced
a copy of clarification letter submitted to the insurance company stating that both the hospital
names are one and same, this forum find this as a doubtful case. Hence I find no reason to interfere
with the decision of the Insurance Company in repudiating the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO. IO/KOC/A/HI/0301/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-049-2122-0436
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the complainant
:
Mr. T V Shaji
Thaiparambil House Edakochi Kochi
682010
2.
Policy Number
:
120700/34/20/04/00000008
3.
Name of the Insured
:
Mr. T V Shaji
4.
Name of the Insurer
:
The New India Assurance Co. Ltd.

5.
Date of receipt of Complaint
:
22.07.2021
6.
Nature of complaint
:
Rejection of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
15.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. T V Shaji (Online)
For the Insurer
:
Ms. Hyma Soman (Online)
AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Mr. T V Shaji is
the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that his son, Sri.Ajay Shaji, Aged 23 years is physically and mentally
challenged, was admitted in Indira Gandhi Co-operative Hospital, Ernakulam on 08/02/2021 vide IP
No.21-13435 for treatment for Severe Pain on lower right back teeth and discharged on 11/02/2021.
On 11/02/2021, the hospital authority has forwarded a detailed estimate for his treatment to TPA,
Vidal Health Services Ltd. The same was denied and an amount of Rs.40,452/- was paid at the
hospital. Subsequently reimbursement claim was submitted and the same was also denied. Again
on 13/04/2021, he had submitted a request to the Grievance Redressal Manager, New India
Assurance Co Ltd for reconsideration of his claim, but till date, no response received from the
respondent insurers.
2. The Respondent Insurer entered appearance and filed a self contained note. It is
submitted that the Policy issued is :New India Group Mediclaim Policy for LIC of India
12030034200400000008; Policyholder: LIC of India .Policy covers employees and agents of
LIC of India, Policy Period : :1stApril,2020 to 31
st
March,2021; Sum Insured : Rs.5lakhs.
Policy is subject to New India Flexi Floater Mediclaim Claude as attached
The present complaint arose out of expenses incurred by Mr T V Shaji for
treatment of his son Mr Ajay Shaji at Indira Gandhi Cooperative Hospital, Ernakulam
for the period 08/02/2021 to 11/02/2021
The claim was processed by the TPA :VidalHealthTPAPvt. And rejected per
the policy exclusion
Not satisfied with the settlement, the insured has represented to the Hon'ble Ombudsman
In this regard we would like to represent as follows
Mr Ajay Shaji, S/O Mr T V Shaji, was admitted in Indira Gandhi Cooperative
Hospital, Ernakulam with complaint of severe pain on lower right back tooth. He has
history of pai on upper and lower tooth back area. He was diagnosed with chronic
irreversible pulpits. He had undergone minor surgical procedures including
extraction of teeth under general anesthesia at the hospital.
All types of Dental treatments except arising out of an accident are excluded
under the policy as per exclusion F (v)
In view of the facts mentioned above, the respondent insurer submit that the claim was processed
and rejected as per the mutually agreed terms of the policy and no further amount is admissible for
the claim preferred as per the terms of the policy issued. The respondent insurer humbly request the
Hon'ble Ombudsman to dismiss the complaint.
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he is an
employee of LIC of India. His son Ajay Shaji, 23 years is differently abled physically and mentally. He
was admitted in Indira Gandhi Co-operative hospital, Ernakulam on 08/02/2021 due to severe pain
on lower right back teeth, treated there and discharged on 11/02/2021. The reimbursement claim
submitted under Group Mediclaim Insurance Policy issued to cover LIC Employees and Agents and
their families. The respondent insurance company rejected his claim stating that all dental
treatments except arising out of accidents are excluded from the scope of the policy. The
Respondent Insurer submitted that Mr.Ajay Shaji S/o the complainant insured Mr.T.V.Shaji was
admitted in Indira Gandhi Hospital with complaint of severe pain on lower right back tooth. He was
diagnosed with chronic irreversible pulpitis. He had undergone minor surgical procedures including
extraction of teeth under general anesthesia at the hospital. The claim was processed and rejected
as per the policy clause – All types of Dental treatments except arising out of an accident are
excluded under the policy.
4. After hearing both the complainant and the respondent insurer and perusing the documents
produced before the forum, I find that the respondent insurance company repudiated the claim as
per the terms, conditions and limitations of the policy. Hence I do not find any reason to interfere in
the decision of the respondent insurer in repudiating the claim.
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
AWARD NO.IO/KOC/A/HI/0304/2021-2022
PROCEEDINGS OF
THE INSURANCE OMBUDSMAN, KOCHI
(UNDER RULE NO. 13(1)b READ WITH RULE 14 OF
THE INSURANCE OMBUDSMAN RULES, 2017)
Complaint No. KOC-H-012-2122-0411
PRESENT: Ms. POONAM BODRA
INSURANCE OMBUDSMAN, KOCHI.
AWARD PASSED ON 30.09.2021
1.
Name and Address of the complainant
:
Mr. Shaji John
I/185, Vilavarthottathil,
Seminaryppady, U C College P.O, Aluva,
Ernakulam - 683102
2.
Policy Number
:
2876/00098245/000/00
3.
Name of the Insured
:
Mr. Shaji John
4.
Name of the Insurer
:
Cholamandalam MS Gen. Insu.Co. Ltd
5.
Date of receipt of Complaint
:
16.07.2021
6.
Nature of complaint
:
Rejetion of mediclaim
7.
Amount of relief sought
:
--
8.
Date of hearing
:
14.09.2021
9.
Parties present at the hearing
For the Complainant
:
Mr. Shaji John (Online)
For the Insurer
:
Dr Minal (Online)

AWARD
This is a complaint filed under Rule 13(1)b read along with Rule 14 of the Insurance Ombudsman
Rules, 2017. The complaint is regarding rejection of mediclaim. The complainant, Mr. Shaji John is
the policyholder.
1. Averments in the complaint are as follows:
The Complainant stated that he had taken policy through the then Dena bank. The agent visited his
office and got him to sign without disclosing the fact that he should have mentioned all existing
diseases. He had policy with Oriental Insurance for 25 yrs. but took policy from M/s Chola MS for Rs.
3 lakhs out of compulsion by the Ins. Co.’s agent. He had no heart related complaint till Jan, 2021 but
had other slight discomforts. He recollects having left the columns blank except the one on
cholesterol. Unfortunately he developed chest pain on 20/1/2021 night , was admitted in Renai
Medicity and angioplasty was done. His Doctor has certified that the cardiac ailment is not directly
related to HTN, DM or any other existing disease. He approached Griev. Cell but with no positive
response. He requests the Ombudsman to get him his claim of Rs. 2 lakhs and the policy renewed
w.e.f.7/11/2021 since he is a pensioner and his two married daughters are far away and he has no
other income.
2. The Respondent Insurer entered appearance and filed a self contained note. It is submitted that
the subject mentioned policy is a group health policy issued in the name of complainant Mr Shaji
John for the period effective from 08/11/2020 to 07/11/2021 for sum insured of Rs. 3,00,000/-
which is subject to terms , conditions and exclusions of the policy.
The claimant was admitted to Renai Medicity Multi Super Speciality Hospital Cochin from
21/01/2021 to 26/01/2021 for Coronary Artery Disease , EA Class II , TMT Positive for inducible
ischemia , CAG-Single Vessel Disease, PTCA to LAD with 1 DES, Diabetes Mellitus , dyslipidemia ,
albuminuria
Upon submission of medical documents it was mentioned in the discharge summary that he had
past history of Diabetes Mellitus type-2 , dyslipidemia , albuminuria . Hence this respondent had
send query letters dated 11/03/2021, reminder letters dated 26/03/2021 ,12/04/2021 requesting
the complainant to specify when the patient first complained of and sought medical attention with
regard to diabetes along with consultation papers , to furnish the details of onset , duration ,
progress of ailments and treatment taken till date
The complainant upon receipt of the query letter submitted, the medical certificate from his
treating Dr Vinod Thomas, certifying that complainant was under treatment for albuminuria and
diabetes mellitus since 2017 and were controlled on medical management
Hence this respondent had repudiated the claim vide its letter dated 28/04/2021 on the following
grounds which is re-iterated here under-
On perusal of the claims documents, it is observed that the signs and symptoms of the albuminuria
and hypertension were existing since 2017.
Hence present ailment is considered as pre-existing disease and the claim is inadmissible as per
General Exclusion clause which followed; "3.2 Pre-Existing Disease (PED) Benefits will not be
available for any pre-existing condition(s) as defined in the policy, until 24 consecutive months of
continuous coverage have elapsed, since inception of the first policy with Us. " Further, though the
insured is diabetic since 2017 as per the history recorded in the case sheets, this information is not
disclosed in the proposal form while proposing for insurance. In view of this non-disclosure of
material information, the contract of insurance becomes void and no claim is payable under this
policy
Hence for the above mentioned reasons, this respondent is not in a position to honour the claim and
renew the policy . Hence the claims of the petitioner was repudiated on just and reasonable grounds
of the policy wordings , so the complaint is to be dismissed
3. I heard the Complainant and the Respondent Insurer. The Complainant submitted that he had
taken policy through Dena Bank from where he had availed Car loan . He had policy with Oriental
Insurance for 25 yrs. but took policy from M/s Chola MS for Rs. 3 lakhs out of compulsion by the Ins.
Co.’s agent . The agents of Bank and Ins. Co. visited his office and got his signature on the proposal
form without telling him the conditions applicable. He was busy and could not fully read the
proposal form. He was told that after two years he would be eligible for all claims. Both Bank and
ins. Co. cheated him. His coronary block is not due to DM or any other existing disease. The
Respondent Insurer submitted that claim was repudiated on grounds of PED.
4. I have heard both the sides and perused the documents. The complainant is an educated person .
He should have gone through the Proposal form and filled in the particulars.
The complainant was diagnosed with Coronary Artery Disease , EA Class II , TMT Positive for
inducible ischemia , CAG-Single Vessel Disease, PTCA to LAD with 1 DES, Diabetes Mellitus ,
dyslipidemia , albuminuria .
It is observed from the Discharge Summary that he is k/c/o Diabetes Mellitus type-2 , dyslipidemia ,
albuminuria and was ailing from albuminuria and diabetes mellitus since 2017. These have not been
disclosed in the Proposal Form at the time of taking the policy. The claim is not tenable for reasons
of non-disclosure of material facts , in accordance with Exclusion 3.2 and General Condition 4.16 of
the policy on Pre-Existing diseases and Mis-Description respectively..
In the result, an AWARD is passed for Dismissal of the complaint.
Dated this the 30
th
day of September 2021
Sd/-
(POONAM BODRA)
INSURANCE OMBUDSMAN
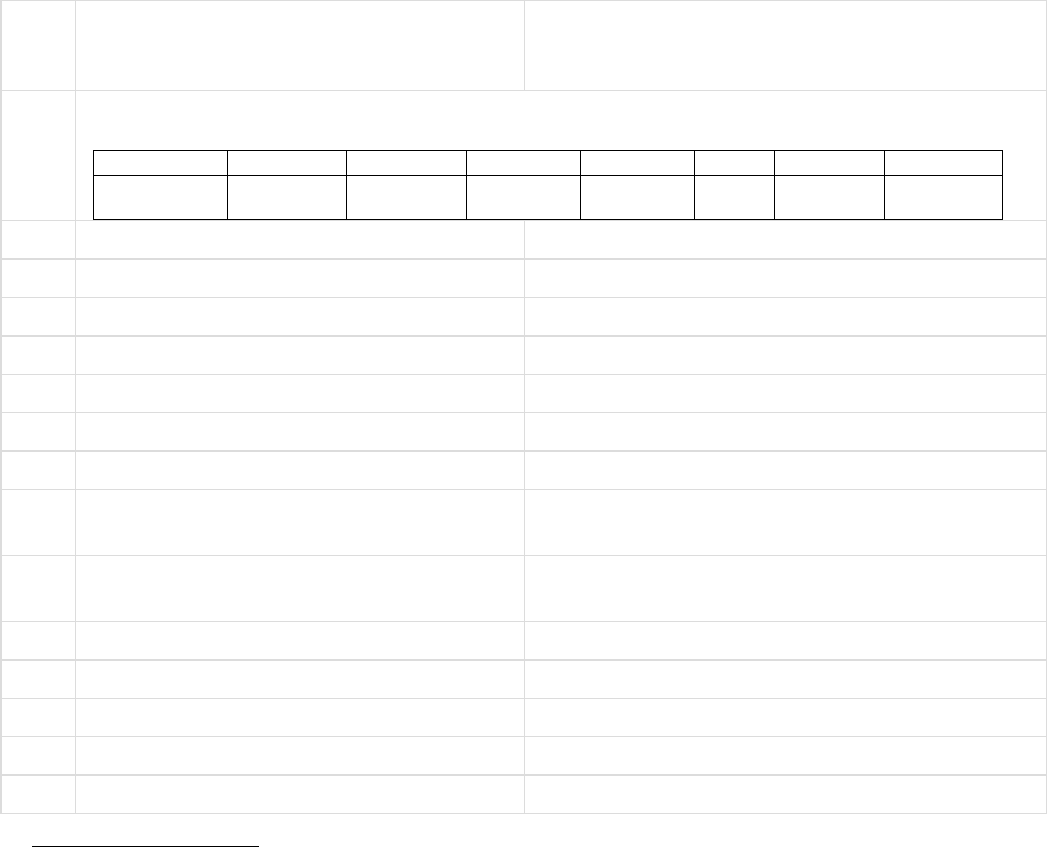
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT– SRI JAGADISH CHANDRA BASU
VS
RESPONDENT: NATIONAL INSURANCE CO. LIMITED
COMPLAINT REF: NO: KOL-H-048-2122-0287
AWARD NO:IO/KOL/
1.
Name &Address OfThe Complainant
Shri Jagadish Chandra Basu
64/11/L, Suren Sarkar Road
Kolkata – 700 010.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
1045005017
10015065
500000
25-03-2018
24-03-
2019
One year
single
3.
Name of insured
Shri Jagadish Chandra Basu`
4.
Name of the insurer
National Insurance Company Limited
5.
Date of receipt of the Complaint
17-Aug-2021
6.
Nature of Complaint
Partial settlement of claim
7.
Amount of Claim
43,805.00
8.
Date of Partial Settlement
9.
Amount of relief sought
5,997.00
10.
Complaint registered under Insurance
Ombudsman Rules 2017
Rule 13(1)(b) - any partial or total repudiation
made by the insurer
11.
Date of hearing
Place of hearing
27-Sep-2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Shri Jagadish Chandra Basu
b)For the Insurer
Shri Ranjit Mallick
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
30-Sep-2021
Brief Facts of the Case:
The complainant-cum-insured, Shri Jagadish Chandra Basu is covered under BOI National Swasthya
Bima Policy with National Insurance Co. Ltd. for the period from 25-03-2018 to 24-03-2019. On 05-
07-2018, the insured was admitted in the hospital for treatment of Advanced Degenerative Disease
Right Knee Prostatomegaly and discharged on 10-07-2018. The Insurance Company allowed
cashless facility for Rs.1,90,281/- during hospitalization. The insured lodged pre and post-
hospitalisation claim for Rs.43,805/- but the Insurance Company settled the claim for Rs.33,209/-.
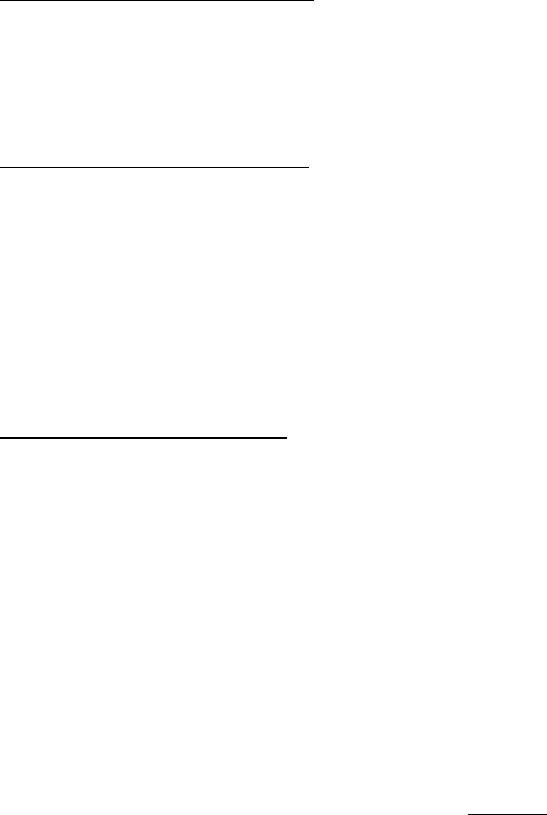
The Insurance Company further settled an amount of Rs.4,999/- out of the claimed amount of
Rs.10,596/-. Inspite of several reminders and request, the Insurance Company did not settle the
balance amount of Rs.5,597/-. Being aggrieved, the insured lodged complaint to this office for
redressal of his grievances.
The Insurance Company has stated in their self-contained note that the insured availed cashless facility
amounting to Rs.1,90,281/-. The pre and post-hospitalisation claim was for Rs.43,805/- and the
Insurance Company settled the claim for Rs.33,209/-. The Insurance Company reviewed the claim
and settled further Rs.4,599/-. and the balance amount was deducted for excess medicines,
medicines purchased without doctor’s advice and attendant charges.
Contention of the complainant:
The complainant has stated in the hearing that the Insurance Company has settled the hospitalization
claim and later the insured lodged pre and post hospitalization claim for Rs.43,805/- but the
Insurance Company did not settle an amount of Rs.5,997/-.
Contention of the Respondent:
The representative of the Insurance Company has stated that the insured has lodged pre and post
hospitalization claim for Rs.43,805/- and the Insurance Company has already paid Rs.37,808/-. The
balance amount of Rs.5997/- is deducted for the following reasons :
Rs.1,279.00 - for purchase of excess medicines;
Rs.168.00 - medicines purchased without doctor’s advice;
Rs.4,550.00 - Attendant/Care Assistant Charges;
Observation and conclusions:
It is observed that the complainant as well as the representative of the Insurance Company both have
attended the hearing online. The complainant has stated in the hearing what he already stated in
his written complaint submitted to this office. The representative of the Insurance Company has
stated in the hearing that the deductions are made as per policy terms and conditions.
It is found from the submitted documents as well as submissions made by both the parties during the
hearing that the Insurance Company has deducted an amount of Rs.5,997/- towards purchase of
excess medicines, medicines purchased without doctor’s advice and Attendant charges as it is not
payable as per policy terms and conditions.
AWARD
Taking into account the facts and circumstances of the cases and submissions made by both the parties
during the course of hearing and after going through the documents on record, it is observed that
the Insurance Company has settled the pre and post claim after deduction of Rs.5,997/- for
purchase of excess medicines, medicines purchased without doctor’s advice and Attendant Charges.
It is found from the submitted documents as well as submissions made by both the parties during the
course of hearing that the deductions made by the Insurance Company is in order. As such, the
Insurance Company is not liable to make any payment further. Hence, the complaint is dismissed
without any relief to the complainant.
If the decision is not acceptable to the complainant, he/she is at liberty to approach any other
Forum/Court as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on Day of 30
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
( States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K. RATH
CASE O FCOMPLAINANT– MS. MONICA CHOPRA PATEL
VS
RESPONDENT: THE ORIENTAL INSURANCE CO. LTD.
COMPLAINT REF: NO: KOL-H-050-2122-0196
AWARD NO:IO/KOL/A/HI/0232/2021-2022
1.
Name &Address OfThe Complainant
Ms. Monica Chopra Patel
Shiv Parbati Apartment, Flat 3B
47A, Padmapukur Road
Kolkata – 700 020.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
311604/48/2
021/4963
1000000
29-03-2021
28-03-
2022
17382
One year
3.
Name of insured
Ms. Monica Chopra Patel
4.
Name of the insurer
The Oriental Insurance Company Limited
5.
Date of receipt of the Complaint
09-Jul-2021
6.
Nature of Complaint
Partial Settlement of Claim
7.
Amount of Claim
2,05,330.00
8.
Date of Partial Settlement
9.
Amount of relief sought
97,742.00
10.
Complaint registered under Insurance
Ombudsman Rules 2017
Rule - 13(1)(b) - any partial or total repudiation
of claims by the insurer
11.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Ms. Monica Chopra Patel
b)For the Insurer
Shri K Chandrasekhar
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
20-Sep-2021
Brief Facts of the Case:
The complainant, Ms. Monica Chopra Patel has stated in the complaint that her husband, Shri Pinaki M
Patel, who is covered under PNB Oriental Mediclaim Policy-2017, was admitted in Belle Vue Clinic Hospital
for Dialysis many times during the period from 2019 to 2020. The Insurance Company settled the claims for
the period from 24-01-2019 to 11-07-2020. The Insurance Company paid full monthly claims of March, 2019,
April, 2019, October, 2019, November, 2019, December, 2019, January, 2020, February, 2020 and June, 2020.
But the Insurance Company did not pay the claims for the month of January 2019, February 2019, May 2019,
June 2019, August 2019, September 2019, March 2020, April 2020, May 2020 and July 2020 stating the
reason by TPA “PPN” Agreement.
The Insurance Company has stated in their self-contained note that the insured patient is having a history of
Hypertension, Diabetes Mellitus and Chronic Kidney Disease and availing dialysis from Belle Vue Nursing
Home. The Belle Vue Clinic was not in PPN tie-up on/from 01-09-2019 to 29-02-2020. Despite of that the
Insurance Company have deducted claims amount during that period after processing as per PPN rate as per
Policy Conditions 3.42 and 5.2(d) of PNB Royal Mediclaim Policy. The Insurance Company have reopened
those claims for part payment and made payment of Rs.1,07,079.00. The total claimed amount was for
Rs.2,05,330.00. The Insurance Company have denied an amount of Rs.98,250.00 as per policy conditions of
the Policy.
The Insurance Company is bound to pay the claims if any insured is availed treatment in the PPN Hospital as
per PPN Package. As per PPN Package, the multi-use dialysis rate is Rs.1,125.00 (till 31-05-2019) and later the
rate has been changed to Rs.1,320.00 (till now). But the Hospital has charged Rs.1,875.00. The Insurance
Company have settled the claims as per PPN Package agreement with the Belle Vue Clinic.
Contention of the complainant:
The complainant, Ms. Monica Chopra Patel has stated in the hearing that the insured, Pinaki Madhusudan
Patel is suffering from Kidney disease and availing Dialysis. The insured patient was admitted many
times in Belle Vue Clinic for dialysis during 2019-2020 and the Insurance Company settled the all
claims. But the Insurance Company did not pay the claims for the month of January 2019, February
2019, May 2019, June 2019, August 2019, September 2019, March 2020, April 2020, May 2020 and
July 2020 stating the reason by TPA “PPN” Agreement.
Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured patient is
suffering from Hypertension, Diabetes Mellitus and Chronic Kidney Disease and availing dialysis from
Belle Vue Nursing Home. The Insurance Company paid all claims for dialysis earlier. The total claimed
amount was for Rs.2,05,330.00. The Insurance Company have denied an amount of Rs.98,250.00 as
per policy conditions of the Policy. As per PPN Package, the multi-use dialysis rate is Rs.1,125.00 (till
31-05-2019) and later the rate has been changed to Rs.1,320.00 (till now). But the Hospital has
charged Rs.1,875.00. The Insurance Company have settled the claims as per PPN Package agreement
with the Belle Vue Clinic.
Observation and conclusions:
It is observed that the complainant has attended the hearing online whereas the representative of the
Company has attended the hearing physically at this office premises. The complainant has stated in
the hearing what she already stated in her written statement submitted to this office. The
representative of the Insurance Company has stated that the claims have been settled as per PPN
Package.
It is found from the submitted documents as well as submissions made by both the parties during the
course of hearing that as per PPN Package, the multi-use dialysis rate is Rs.1,125.00 (till 31-05-2019)
and later the rate has been changed to Rs.1,320.00 (till now). But the Hospital has charged
Rs.1,875.00. The Insurance Company have settled the claims as per PPN Package agreement with the
Belle Vue Clinic.

AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties
during the course of hearing and after going through the documents on record, it is observed that the
Hospital Authority has charged the Dialysis rate beyond PPN Package Agreement with the Hospital and
the Insurance Company has settled the claims as per PPN package rate.
After considering all the documents and statements, the settlement of claims is found to be as per Policy
terms and conditions. As such, the Insurance Company is not liable to make any payment further to
the complainant. Hence, the complaint is dismissed without any relief to the Complainant.
If the decision is not acceptable to the complainant, she/he is at liberty to approach any other
Forum/Court as per Law of the Land against the Respondent.
Dated at Kolkata on Day of 20
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
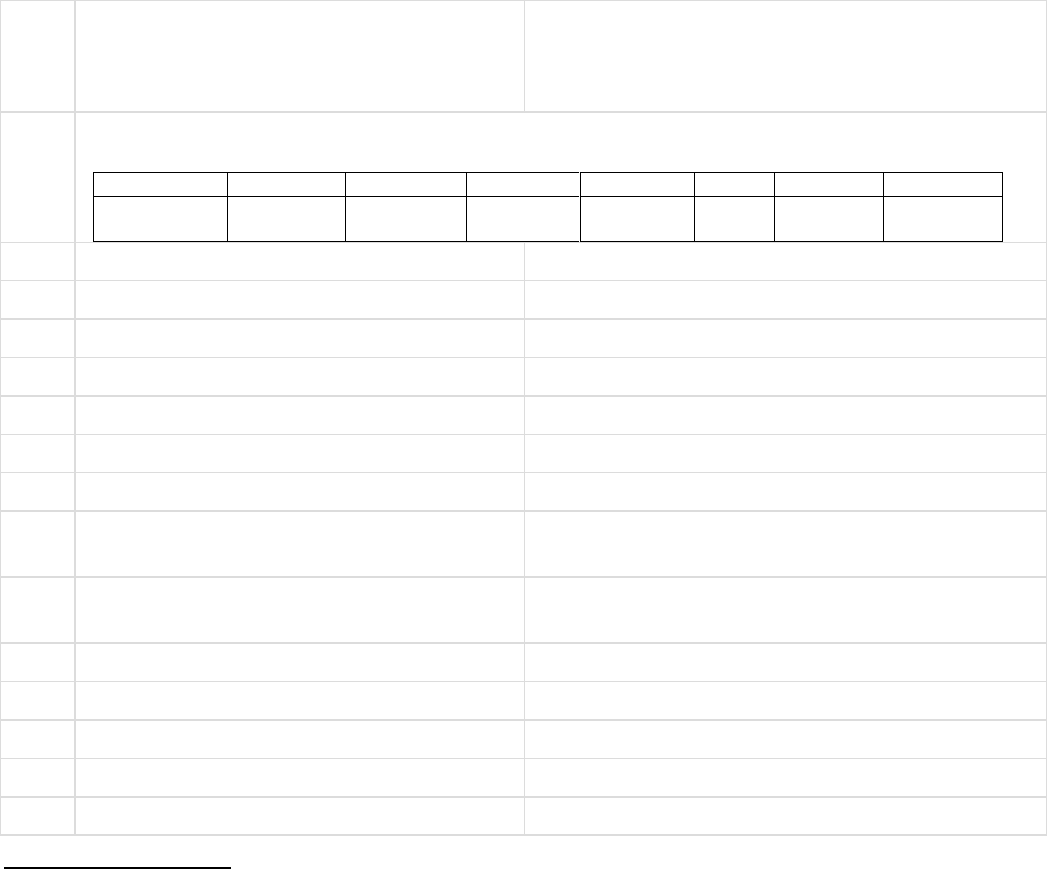
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K. RATH
CASE OF COMPLAINANT– SHRI BENOY KUMAR DUTTA
VS
RESPONDENT: UNITED INDIA INSURANCE CO. LTD.
COMPLAINT REF: NO: KOL-H-051-2122-0205
AWARD NO:IO/KOL/A/HI/0214/2021-2022
1.
Name &Address OfThe Complainant
Shri Benoy Kumar Dutta
Kharida Nayapara, Ward No.9
Kharagpur,
Dist: Paschim Midnapore - 721 301.
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
5001002819
P111091052
400000
3.
Name of insured
Shri Benoy Kumar Dutta
4.
Name of the insurer
United India Insurance Company Limited
5.
Date of receipt of the Complaint
08-Jul-2021
6.
Nature of Complaint
Partial settlement of claim
7.
Amount of Claim
6,06,292.00
8.
Date of Partial Settlement
9.
Amount of relief sought
2,06,000.00
10.
Complaint registered under Insurance
Ombudsman Rules 2017
Rule 13(1)(b) - any partial or total claim
repudiation by the insurer
11.
Date of hearing
Place of hearing
06-Sep-2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Shri Benoy Kumar Dutta
b)For the Insurer
Ms. Srijani Saha
13.
Complaint how disposed
By conducting online hearing
14.
Date of Award
13-Sep-2021
Brief Facts of the Case:
The complainant-cum-insured, Shri Benoy Kumar Dutta has stated in his written complaint that he is a Sr
Branch Manager of Indian Bank, Kharagpur Branch and covered under Group Mediclaim Policy with
United India Insurance Company. On 18-09-2020, he was admitted in Medica Super Speciality Hospitality
Hospital for treatment of Covid-19 and discharged on 06-10-2020. The final diagnosis was Acute
Respiratory Distress Syndrome, COVID Pneumonia and Type-2 Diabetes Mellitus. The total hospital bill
was for Rs.6,06,292.00 and the Insurance Company approved and paid to the hospital for an amount of
Rs.4,00,000.00. The Insurance Company did not settle the balance claimed amount of Rs.2,06,000.00
inspite of several request/reminders. The balance amount was approved by the Corporate Office but the
Insurance Company did not settle the same. Being aggrieved, the insured lodged complaint to this office
for redressal of his grievances.
The Insurance Company has stated in their self-contained note that the insured patient was covered
under Group Mediclaim Policy with sum insured Rs.4,00,000/-. The insured patient was admitted with
diagnosis Acute respiratory distress syndrome, Covid 19 Pneumonia, Diabetes Mellitus from 18-09-2021
to 06-10-2021. Out of the total final bill amount of Rs.6,06,292/-, the TPA has settled Rs.4,00,000/- as per
policy sum insured as cashless settlement. Rs.2,06,292/- was not settled as the sum insured exhausted.
The complaint is mainly due to non-payment of the remaining Rs.2,06,292/-. As confirmed by the TPA,
they have neither received Buffer Approval from the Corporate Office nor any documents for processing
the reimbursement claim, hence, the same was not processed.
However, the last date for submission of claim documents under IBA active employee 2019-2020 was 15-
11-2020 (policy expired on 30-09-2020). If the insured would have submitted the reimbursement claim
documents on time and too Buffer Approval, the Insurance Company would have processed the claim as
per policy terms and conditions. Unless and until, the insured submits a claim form, we cannot process
any claim.
Contention of the complainant:
The complainant has stated in the hearing that he was admitted in the hospital for treatment of Covid and
during the hospitalization period, the Insurance Company approved an amount of Rs.4,00,000/- towards
cashless facility. The total claim was Rs.6,06,292/- but the Insurance Company did not settle the balance
amount of Rs.2,06,292/-. The Corporate Office i.e. Bank already forwarded the Buffer Utilisation Format
duly approved in the month of January, 2021 to the TPA for payment.
Contention of the Respondent:
The representative of the Insurance Company has stated that the insured patient was covered under Group
Mediclaim Policy with sum insured Rs.4,00,000/-. The insured patient was admitted with diagnosis Acute
respiratory distress syndrome, Covid 19 Pneumonia, Diabetes Mellitus from 18-09-2021 to 06-10-2021.
Out of the total final bill amount of Rs.6,06,292/-, the TPA has settled Rs.4,00,000/- as per policy sum
insured as cashless settlement. Rs.2,06,292/- was not settled as the sum insured exhausted. The insured
did not forward the claim form alongwith documents duly approved by the Corporate Office within the
stipulated time.
Observation and conclusions:
It is observed that the complainant has attended the hearing physically at this office premises whereas the
representative of the Insurance Company has attended the hearing online. The complainant has stated in
the hearing what he already stated in his written complaint submitted to this office. The representative
of the Insurance Company has stated that the claim is pending for non-availability of required documents.
It is found from the submitted documents as well as submissions made by both the parties during the course
of hearing that the insured was covered under Group Mediclaim Policy with sum insured of Rs.4,00,000/-.
The insured was admitted in the hospital for treatment of Covid and availed cashless facility of
Rs.4,00,000/-. The Insurance Company did not settle the claim for non-availability of required

documents. But it is observed from the mail dated 11-01-2021 and 20-01-2021 of the Corporate Office
that the required documents for settlement of the balance claimed amount of Rs.2,06,292/- are
forwarded. Though the last date for submission of documents under IBA Active Employee Policy (2019-
2020) is 15
th
November, 2020.
AWARD
Taking into account the facts and circumstances of the cases and submissions made by both the parties
during the course of hearing and after going through the documents on record, it is observed that the
Insurance Company did not settle the balance claimed amount due to non-availability of claim form
alongwith required documents duly approved by the Corporate Office.
It is found from the submitted documents and the submissions made by both the parties during the course of
hearing that the Corporate Office has forwarded the Corporate Buffer Utilization Format duly approved in
the month of January, 2021.
In view of the above, the Insurance Company is directed to settle the claim on merit subject to submission of
required documents by the insured.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the receipt of
the acceptance letter of the Complainant and shall intimate the compliance to the Ombudsman.
Dated at Kolkata on Day 13
th
September, 2021 SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant: Mr. Sukha Ranjan Chowdhury
VS
Respondent: HDFC ERGO General Insurance Company Ltd.
COMPLAINT REF NO: KOL-H-018-2122-0238
AWARD NO:IO/KOL/A /HI/ 0225 / 2021-2022
1.
Name & Address of the Complainant
Mr. Sukha Ranjan Chowdhury
20, Kapali Para Budge Budge, Kolkata - 700137
2.
Type of Policy: Group Mediclaim
Policy Number
Sum
Assured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
PE02100112
3,00,000
15/03/2020
14/03/202
1
3.
Name of the insured
Mr. Sukha Ranjan Chowdhury
4.
Name of the insurer
HDFC ERGO General Insurance Company Ltd.
5.
Date of Receipt of the Complaint
28-Jul-2021
6.
Nature of Complaint
Rejection of Claim
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.3,53,740/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
c) For the Complainant
Mr. Sukha Ranjan Chowdhury
d) For the insurer
Ms. Saswata Banerjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021
Brief Facts of the Case:
Policy Name :: Group Health Insurance Plan for Bandhan Bank Customers,
Policy Type :: Health Insurance,
Period of Insurance :: 15/03/2020 to 14/03/2021,
Sum Insured :: Rs.3,00,000/-
Hospitalisation date/s:: 23/07/2020 to 05/08/2020.
The complainant lodged complaints against the Insurance Company in connection with
repudiation of his hospitalisation claim. Hence, this complaint lodged with this office for
settlement of claim.

Contention of the complainant:
The complainant stated that:
(i) He, aged 66 years, tested Covid-19 positive on 21/07/2020 with severe breathing
difficulties and received treatment at Arti Nursing Home (22/07/2020 to
23/07/2020) and subsequently at Horizone Life Line, Kolkata from 23/07 t
05/08/2020.
(ii) His reimbursement claim has been rejected on the ground of undisclosed history
of COPD. However, he never had COPD in the past.
(iii) He has given them the copies of his old medical records, doctor’s certificates,
and hospital records which corroborate that he never had any sing of COPD in
the last 3 years before contracting COVID – 19. Still they never accepted his
claim.
(iv) He has duly paid all his insurance premiums and have never kept anything from
his insurer. He deserves to have his medical expenses covered, particularly at the
time of the pandemic.
(v) He has provided documents in support of “No history of COPD:
→Medical Certificate from Dr. P. K. Das with supporting prescription and
test reports (PFT) from 6/8/2018 to 12/1/2021. Dr. Das was his regular
physician during that period.
→Certificate from Dr. A. B. Nath, his local physician who initially treated
him for Covid symptoms from 12/07/2020 to 21/07/2020 with supporting
prescription and chest X-ray reports.
→Medical Certificate from Arti Nursing Home with supporting in house
treatment records and test reports
Being aggrieved and dissatisfied with the Non-settlement of claim by the Insurance
Company, the complainant has approached this office for redressal of his grievance. The
complainant has also given his unconditional and irrevocable consent to the Insurance
Ombudsman to act as a mediator between himself and the insurance company and to
give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(iv) The Complainant had initially been admitted to Arti Nursing Home and
diagnostic centre on 22/07/2020 and a cashless claim was lodged for treatment
of acute lower respiratory infection. The complainant took LAMA and transferred
to another hospital on his own. Hence, his cashless claim was denied on the
following ground:

“Cashless request / authorisation stands cancelled based on the
confirmation received for non-utilisation of cashless facility. All previous
authorisation related to the captioned case also stands cancelled ab
initio”.
(ii) The risk bond issued by Arti Nursing Home clearly mentions that complainant
was suffering from COPD and had been on medication. Also the in patient record
and treatment sheet shows that he was suffering from COPD. Copy of the risk
bond request, the inpatient record and treatment sheet is enclosed.
(iii) Reimbursement claim for Covid 19 was received on 14/08/2020 for his
hospitalisation at Horizon Life line Pvt. Ltd. for the period of admission between
23/07/2020 to 05/08/2020.
(iv) There was a history of COPD and Hypertension, so query was raised for
documents when the aforementioned ailments were diagnosed for the first
time.
(v) The investigation into the history of the aforementioned disease was also made
so as to rule out the present case of pre-existing disease and through
investigation, it was discovered that insured was suffering from respiratory
distress (COPD) since 3 years as noted from the prescription of Dr. A. B. Nath
(snapshot given in the SCN and copy enclosed).
(vi) Based on the documents collected, the claim was repudiated on the ground:
“The medical history details of known case of COPD since 3 years i.e.
before policy inception was not revealed in the proposal form while
taking the policy. Hence the Policy is cancelled and claim is repudiated
due to Non-disclosure and concealment of facts under policy terms and
conditions”.
(vii) The complainant during investigation admitted that he had been suffering from
hypertension for the last 7 years but same was not disclosed in the proposal
form.
The Insurance Company has also given their consent to the Insurance Ombudsman to
act as a mediator between the Complainant and themselves and to give his
recommendation for the resolution of the complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents
were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A
& (d) Self Contained Note from the insurer.
AWARD
Taking into account the facts & circumstances of the case and the submissions made
by both the parties during the course of hearing & after going through the documents
on record and as evident from the medical records, the patient is suspected COPD by
symptoms, repudiation of the claim is not justified.
In view of the above, the Insurer’s repudiation is set aside and the Insurance Company
is directed to admit the claim and pay the claim amount of Rs.3,53,740/- to the
Complainant towards full and final settlement of the claim subject to deductions,
limitations, cappings, non-payables, Co-payment (if any) as per Policy Terms &
Conditions.
Hence, the complaint is treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following
provisions of the Insurance Ombudsman Rules-2017:
(f) As per Rule 17(6) of the said rules the Insurer shall comply with the Award within
30 days of the receipt of the AWARD and shall intimate the compliance to the
Ombudsman.
(g) As per the Rule 17(7), the Complainant shall be entitled to such interest at a rate
per annum as specified in the regulations framed under the Insurance Regulatory
and Development Authority of India Act 1999, from the date of the claim ought to
have been settled under the regulations, till the date of payment of amount
awarded by the Ombudsman.
(h) As per Rule 17(8) of the said rules and award of the Insurance Ombudsman shall be
binding on the Insurers.
Dated at Kolkata on the 17
Th
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N
ISLAND
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
STATES OF WEST BENGAL, SIKKIM AND UT OF ANDAMAN & NICOBER ISLANDS
(Under Rule No.16(1)/17 of The Insurance Ombudsman Rules -2017)
OMBUDSMAN–SHRI P. K. RATH
Case of Complainant: Mrs. Debika Mukherjee Gupta
VS
Respondent: HDFC ERGO General Insurance Company Ltd.
COMPLAINT REF NO: KOL-H-018-2122-0239
AWARD NO:IO/KOL/A /HI/ 0229 / 2021-2022
1.
Name & Address of the Complainant
Mrs. Debika Mukherjee Gupta
A-38, Lake Gardens, Flat No. 36, Kolkata - 700045.
2.
Type of Policy: Group Mediclaim
Policy Number
Sum
Assured
From Date
To Date
DOC
Premium
Policy
Term
Paying Term
PE02298862
15,00,00
0
05/09/2020
04/09/202
1
3.
Name of the insured
Mrs. Debika Mukherjee Gupta
4.
Name of the insurer
HDFC ERGO General Insurance Company Ltd.
5.
Date of Receipt of the Complaint
26-Jul-2021
6.
Nature of Complaint
Repudiation of Claim & Termination of the Policy
7.
Amount of Claim
8.
Date of Partial Settlement
9.
Amount of relief sought
Rs.80,611/-
10.
Complaint registered under IOR-2017
13 (1) (b)
11.
Date of hearing
Place of hearing
09- September-2021
Kolkata
12.
Representation at the hearing
e) For the Complainant
Mrs. Debika Mukherjee Gupta
f) For the insurer
Ms. Saswata Banerjee
13.
Complaint how disposed
By Conducting online Hearing
14.
Date of Award/Order
17-September-2021
Brief Facts of the Case:
Policy Name :: Group Assurance Health Plan for Bandhan Bank Customers,
Policy Type :: Health Insurance,
Period of Insurance :: 05/09/2020 to 04/09/2021,
Sum Insured :: Rs.15,00,000/- + Rs.1,50,000/- (CB),
Hospitalisation date/s:: 14/11/2020 to 18/11/2020.

The complainant lodged complaints against the Insurance Company in connection with
repudiation of her hospitalisation claim and termination of the policy. Hence, this
complaint lodged with this office for settlement of claim.
Contention of the complainant:
The complainant stated that:
(i) She received an email and a letter from the Apollo Munich Health Insurance
company stating her claim has been rejected and Policy
No.150100/12586/2020/A022934/PE02298862 has been terminated stating the
reason “on account of Non-Disclosure of Material Facts”.
(ii) She opted for this policy via Bandhan Bank because of the better facilities and
better product features than her previous Insurance Company. She has been
paying higher premium as well compared to the previous Company.
(iii) The employees of Bandhan Bank approached her to buy a new policy from them.
They took care of all the formalities regarding the issuance of the policy. Neither
she was asked to go for a medical check-up nor did the advisors asked for any
relevant information from her. She was not aware of any terms and conditions of
the policy / proposal, nor did she has proper guidance for any. She just did what
she was told to do by the Bandhan Bank employees. Had they done their job
professionally and not like an amateur, her policy would not have been
terminated and she would not have been terminated and she would not have
wasted the premiums of the last 3 years.
(iv) In her opinion, neither she has manipulated the documents nor is it serious case
in which they can take such a hard step against her for cancelling the policy and
not paying the claim.
Being aggrieved and dissatisfied with the Non-settlement of claim & termination of the
policy by the Insurance Company, the complainant has approached this office for
redressal of her grievance. The complainant has also given her unconditional and
irrevocable consent to the Insurance Ombudsman to act as a mediator between himself
and the insurance company and to give recommendation as per consent form.
Contention of the Respondent:
The Insurance Company vide their SCN (Self Contained Note) has stated that:
(i) Cashless claim for Covid 19 was received on 16/11/2020 for her hospitalisation
at AMRI.
(ii) It was noted from the documents that the complainant had undergone PTCA in
2002 (Copy of the general information record is enclosed)
(iii) Based on the history and physical record & history of past illness, the cashless
claim of the complainant was denied on the below mentioned ground:

“As per the available documents, we have observed that there is a non-
disclosure of PTCA in 2002 (ailment) which may have an impact on policy
and hence cashless approval would not be possible at this juncture”.
(iv) Since the cashless claim had been denied, the termination notice was issued, and
the claim was also rejected for the same reason:
“The medical history details of heart disease and PTCA in 2002 is not
revealed while taking the policy. Hence, the claim is repudiated and
policy is terminated due to incorrect good health declaration under
section 3 (i) of policy terms and conditions” (Copy of the repudiation
letter dated 11/12/20 is enclosed).
(v) The patient who underwent PTCA need long life cardiac medicines. Post
termination of the policy, premium was also refunded vide UTR
No.N188211557494792 Dated 14/07/2021 for an amount of Rs.9,238/-
The Insurance Company has also given their consent to the Insurance Ombudsman to
act as a mediator between the Complainant and themselves and to give his
recommendation for the resolution of the complaint.
Observation and conclusions:
Both the parties were present and participated in the hearing and following documents
were placed for perusal:
(a) Complaint letter along with annexures, (b) Policy Copy, (c) Annexure–VI-A
& (d) Self Contained Note from the insurer.
AWARD
Taking into account the facts & circumstances of the case and the submissions made
by both the parties during the course of hearing & after going through the documents
on record it is observed that the decision of the insurance company is in consonance
with the policy issued to the Complainant.
Hence, the complaint is dismissed without any relief to the complaint.
If the decision is not acceptable to the Complainant, She/He is at liberty to approach
any other Forum/Court as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on the 17
TH
Day of September, 2021.
SRI P. K. RATH
INSURANCE OMBUDSMAN
STATES OF WEST BENGAL, SIKIM, A & N
ISLAND
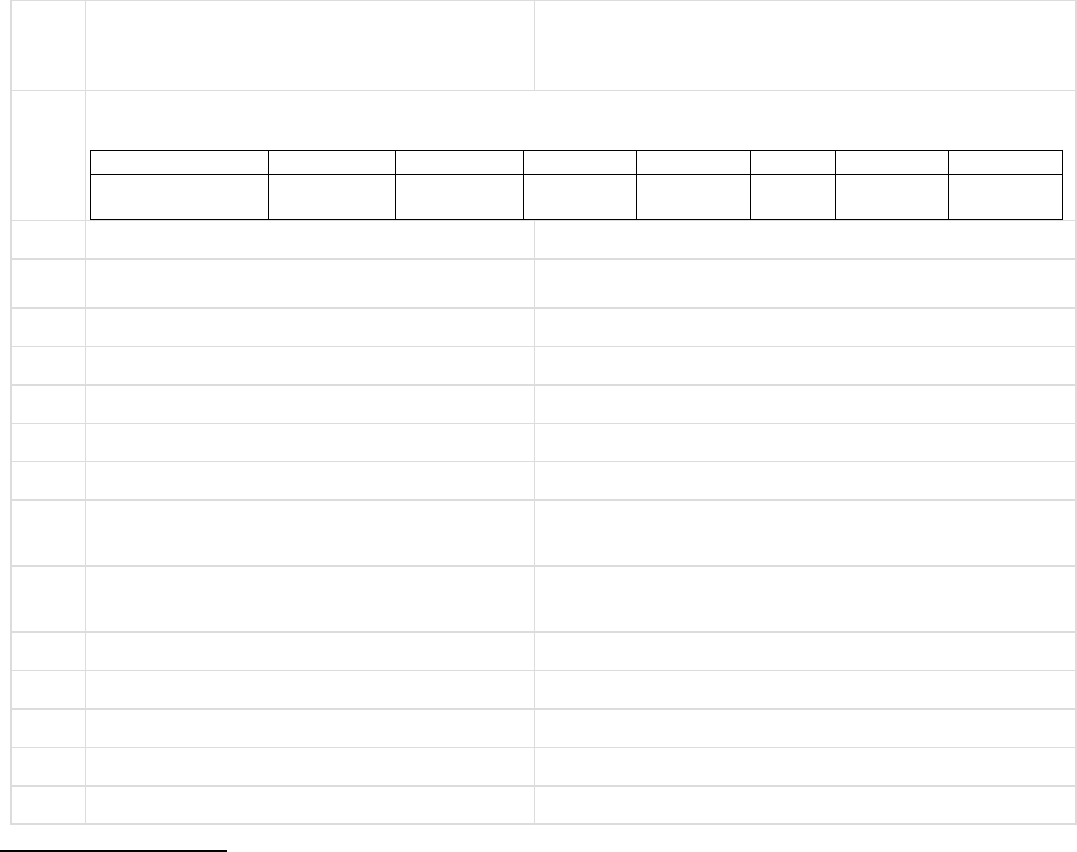
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K.RATH
CASE OF COMPLAINANT – Sri Amitabha Bagchi
VS
RESPONDENT: --Max Bupa Health Insurance Company Ltd
COMPLAINANT REF: NO: KOL-H-031-
2122-0208
AWARD NO:
IO/KOL/A/HI/0206/2021-2022
1.
Name &Address OfThe Complainant
Sri Amitabha Bagchi
HB-10/3, Salt Lake city, Sector- 3
Kolkata- 700106, West Bengal
2.
Type Of Policy: Health
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
00209500201903
5 lakh
26.05.2020
25.05.2021
19.10.2020
15511/-
Mediclaim
Annual
3.
Name of insured
Sri Amitabha Bagchi
4.
Name of the insurer
Max Bupa Health Insurance Company Ltd
5.
Date of receipt of the Complaint
05.08.2021
6.
Nature of Complaint
Non settlement of claim
7.
Amount of Claim
23045/-
8.
Date of Partial Settlement
NA
9.
Amount of relief sought
23045/-
10.
Complaint registered under Insurance
Ombudsman Rules 2017
Rule 13(1) (b)
11.
Date of hearing
Place of hearing
06.09.2021
Kolkata
12.
Representation at the hearing
--
a)For the Complainant
Sri Amitava Bagchi
b)For the Insurer
Sri Bhuban Bhaskar
13.
Complaint how disposed
Through online hearing.
14.
Date of Award
08.09.2021
Brief Facts of the Case: --
The Complainant cum Insured Sri Amitabha Bagchi, on confirmation of Covid Infection, been
advised by Medical Doctor to have treatment at domestic level. He also suggested that if
oxygen level comes down below 92%, then have to take admission in Hospital. However, finally
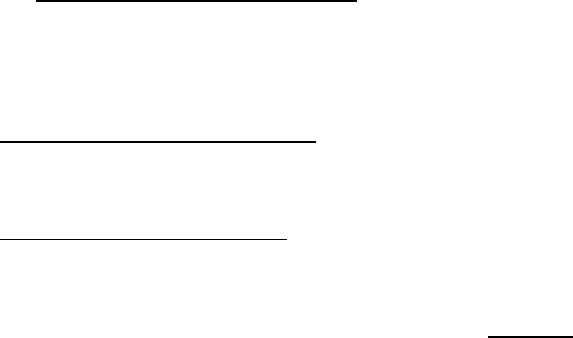
he got recovered after taking medicines & other suggestive medical measures while staying in
residence. Total expenses claimed by him as Rs 23045/-. But Insurer informed the claimant by
mail on 29.05.2021 stating the provision of domiciliary treatment & requested the Insured to
provide documents in order to final conclusion of the claim. In SCN, Insurer further claimed
that Complainant had not submitted reimbursement claim via online mode as suggested by
them. Hence claim is pending as yet. Under rejection letter Insurer stated that as per policy
condition, claim is not payable as per criteria of policy domiciliary provision. On the contrary,
Complainant urged that domiciliary treatment is covered up to 20% of Sum Insured & he had
already submitted claim papers on line.
Contention of the complainant:-
Complainant stated that he took treatment as per advice of Doctor in residence following
COVID 19 infection. Claim bill submitted to Insurer. Yet to receive the payment.
Contention of the Respondent:-
Insurer agreed to consider the claim as per submitted documents including bills & cash memos
under the cover of Policy.
Observation and conclusions:
Insurance company , in hearing agreed on principle to consider the claim as per eligibility of the
policy & based on bills & cash memos as submitted by Insured.
AWARD
Taking into account the facts & circumstances of the case & the submission made by both
the parties in hearing, also on positive consideration of claim by the Insurer it is hereby
concluded & directed to Insurance Company to go for settlement of claim for an amount of Rs
23045/- as claimed by Complainant & agreed by Insurer subject to verification of bills/ Cash
memos & as per eligibility on the limit of policy. With this, the Complaint is ended, closed &
disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the
receipt of the Award and shall intimate the compliance to the Ombudsman.
SHRI P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: P.K. RATH
CASE OF COMPLAINANT – Smt. Monisha Das
VS
RESPONDENT: -- National Insurance Co. Ltd
COMPLAINANT REF: NO: KOL-H-048-
2122-0216
AWARD NO:
IO/KOL/A/HI/0208/2021-2022
1.
Name &Address OfThe Complainant
Mrs Monisha Das
C/o Gopal Chandra Das, Balitkuri Kalitala
Naskarpara, ( Dhopar Math )
P.O- DASNAGAR, HOWRAH—711113
West Bengal.
2.
Type Of Policy: Health
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
25110050201
0000329
Not
mentioned.
01.11.2020
31.10.2021
12.04.2021
Not
mentio
ned.
Mediclaim
Annual
3.
Name of insured
Mrs Monisha Das
4.
Name of the insurer
National Insurance Company ltd.
5.
Date of receipt of the Complaint
05.08.2021
6.
Nature of Complaint
Rejection of claim.
7.
Amount of Claim
20.05.2021
8.
Date of Partial Settlement
NA
9.
Amount of relief sought
44222/-
10.
Complaint registered under Insurance
Ombudsman Rules 2017
Rule 13(1) (b).
11.
Date of hearing
Place of hearing
06.09.2021
Kolkata
12.
Representation at the hearing
a)For the Complainant
Mrs. Monisha das
b)For the Insurer
Sri Atul Malhotra
13.
Complaint how disposed
Through on line hearing.
14.
Date of Award
08.09.2021
Brief Facts of the Case: --
This is a claim under Group Mediclaim Policy (Period- 1.11.2020 to 31.10.2021) when Mr. Gopal
Das, husband of claimant Smt. Monisha Das, is an ex officer of formerly United Bank of India,
Now- Punjab National Bank. Mrs Monisha Das, in continuation of her treatment of CA- Breast,
admitted to Narayani Superspeciality Hospital on 12.04.2021 for infusion of Inj. Zoledronic Acid(
once in 6 month ) when she was also had investigation of USG, whole Abdomen, USG right
breast, TSH, creatinine & TC. Mrs. Das released on 14.04.2021.
Both cashless & Reimbursement claim rejected by Insurer with the reason that the concern
treatment, is a hormonal therapy & which is usually taken in OPD & also not included in Day
care treatment. Hence rejected (exclusion clause – 2.19). Claim amount is 44222/-.
Complainant stated that treatment being part of cancer treatment, included under the policy
coverage.
Here the Concern Hospital is Narayani Hospital whereas in denial letter of Insurer both in
cashless & reimbursement, it is stated as West Bank Hospital- New Unit.
Contention of the complainant:-
This is a continued treatment of CA Breast Cancer When treatment taken in Hospital for a
period of two days as per medical advice. Not in day care or OPD. Treatment as well as
various investigations done as per medical advice. Hence claim amount of Rs 44222/- may
please be considered under ambiguous decision.
Contention of the Respondent:
The said treatment is usually taken in OPD. If done in day care, this is also not taken care by the
policy list of cover. Hence claim rejected.
Observation and conclusions:
Treatment taken in hospital for a period of two days when various tests done to assess the status
of cancer & to have follow up treatment of cancer as is revealed from the discharge Summary
of NH Narayana Super specialty Hospital.
AWARD
Taking into account the facts & circumstances of the case & the submissions made by both
the parties in hearing, as also from the submitted documents it is observed that the decision
of the Insurer towards rejection of claim seems to be not justified. The present treatment,
being in Hospital for a period of two days & being part of follow up cancer therapy, the cause
of rejection by the Insurer does not stand valid here & the Insurer is directed to consider the
claim for an amount of Rs 44222/- as claimed by Complainant subject to terms, conditions,
limitations, sublimit & other prevailing provisions of the policy. With this, the Complaint is
closed without further reference. The Complaint of the Complainant is herewith closed &
treated as disposed of.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rule 2017.
As per Rule 17(6) of the said rules the Insurer shall comply with the Award within 30 days of the
receipt of the Award and shall intimate the compliance to the Ombudsman.
SHRI P K RATH
INSURANCE
OMBUDSMAN
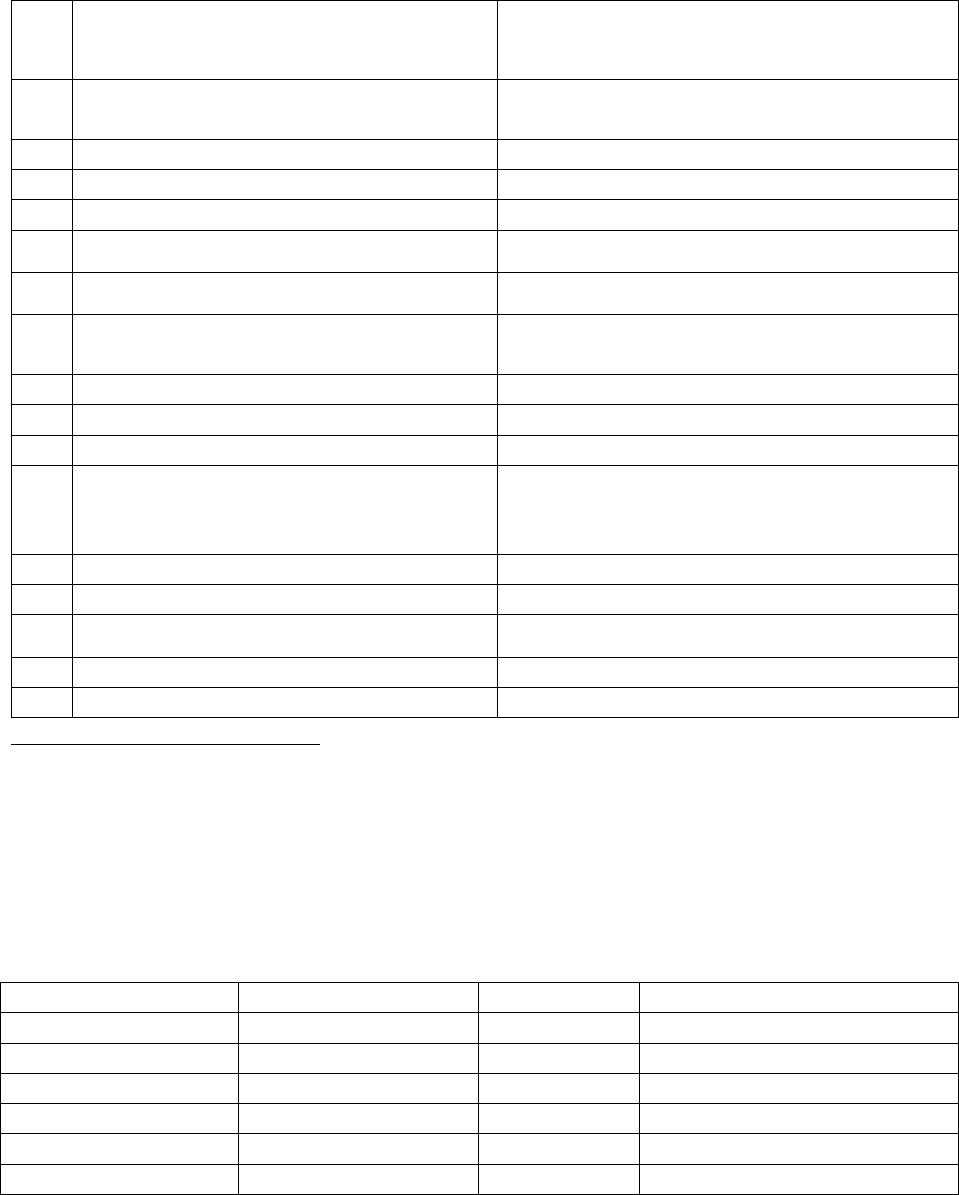
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Amit Bhandari Vs The Oriental Insurance Co. Ltd
COMPLAINT NO: PUN-H-050-1920-0688
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the Complainant
Mr. Amit Bhandari, Pune
Employee no. 11233739
2.
Policy No:
Type of Policy:
Group policy- Accenture
3.
Policy period:
NOT MENTIONED
4.
Sum Insured
300000/-
5.
Date of inception of first policy:
NOT MENTIONED
6.
Name of the Policyholder:
Mr. Amit Bhandari, 39 years
7.
Name of the Insurer:
The Oriental Insurance Co. Ltd
8.
Reason for repudiation/Partial
Settlement:
Inj. Rituximab is not covered under the
policy. Hence rejected the claim.
9.
Date of receipt of the Complaint:
29/1/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
Rs.64923/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
13 1(b)
13.
Date of hearing/Place:
Online hearing on 13.08.2021
14.
Representation at the hearing
l) For the Complainant:
Himself
m) For the insurer:
Ms. M. S. Indira 2) Dr. Fulendra Kumar
15.
Complaint how disposed:
Allowed
Contention of the Complainant
The complainant was covered under Corporate policy issued to ‘Accenture’ Company.
Complainant is covered for sum insured of Rs.300000/-. On 8.8.19, complainant was admitted
in hospital for the symptoms of right lower limb numbness (since 15 days prior to
hospitalization), left hip pain (since 1 month prior to hospitalization) and loss of bowel and
bladder control (since 1 month prior to hospitalization) discharged on 9.8.19. He is diagnosed
with Multiple Sclerosis. Treating doctor started the treatment with inj. Rituximab. RI has settled
the five claims and rejected one claim. The details are shown below:
Claim no.
Period -from
to
Amount
BLR-0218-CL-0001503
30/1/2018
31/1/2018
6841.00
BLR-0218-CL-0007454
30/1/2018
31/1/2018
33680.00
BLR-0218-CL-0007455
30/1/2018
31/1/2018
2483.00
BLR-0219-CL-0002593
6/12/2018
7/12/2018
101172.00
BLR-0518-CL-0009315
2/3/2018
3/3/2018
46057.00
BLR-1019-CL-0005907
6/8/2019
9/8/2019
64923.00 Rejected claim
RI has rejected the claim stating that treatment taken is for injecting Rituximab injection. This
treatment is not covered under policy. More over this treatment is not also included in Day care
procedure. This treatment is possible on OPD basis and opd procedure is not covered under the

policy. He is surprised that the RI had paid his five claims for same injection and why not the
present.
Complainant aggrieved with the decision of the RI and filed complaint before this Forum for
resolution of issue.
Contention of the Respondent Insurer:
Rejction mail dated 20.11.2019
The claim is rejected correctly because treatment taken is for Injecting Rituximab injection. The
treatment is not covered under the policy. Moreover treatment is not included in the day care
procedures. 2) The treatment is possible on OPD basis, the OPD procedures not covered under
the policy.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 13.08.2021 (through video-conferencing) both the parties
reiterated their respective stand.
During the hearing complainant described his ailment. Objecting to RI’s contention of less than
24 hours hospitalization, he said that his doctor treats him with this injection, whenever his
symptoms get aggravated. He is wheel chair bound. His immunity is low. He is susceptible to
infection. The injection has side effect too. 24 hours observation for administration of this
injection is necessary.
RI contended that there was no active line of treatment. Vide their mail dt. 16.8.21 they have
stated that the complainant had lodged 8 claims and in 7 claims there is active line of treatment
along with administering of the injection. Only in this claim there is no active line of treatment.
Hence the claim is rejected. Forum is surprised why the RI does not understand that the
administration of this injection itself is an active line of treatment. At the time of admission he
had Rt. limb numbness, hip joint pain and loss of bowel and bladder control. At the time of
discharge also medicines are prescribed. The complaint is genuine. Rejection of claim is set
aside and forum asks the RI to pay the claim.
Award follows;
AWARD
Under the facts and circumstances, the RI is directed to pay Rs.64923/-less deductible
as per the terms and conditions of the policy to the complainant, towards full and final
settlement of the complaint.
The award is to be settled within one month from the date of receipt of this award
failing which it will attract interest at the prevailing bank rate plus 2% extra from the
date of rejection of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the
award and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: Pune, on this 20
th
day of September, 2021
VINAY SAH
INSURANCE OMBUDSMAN PUNE
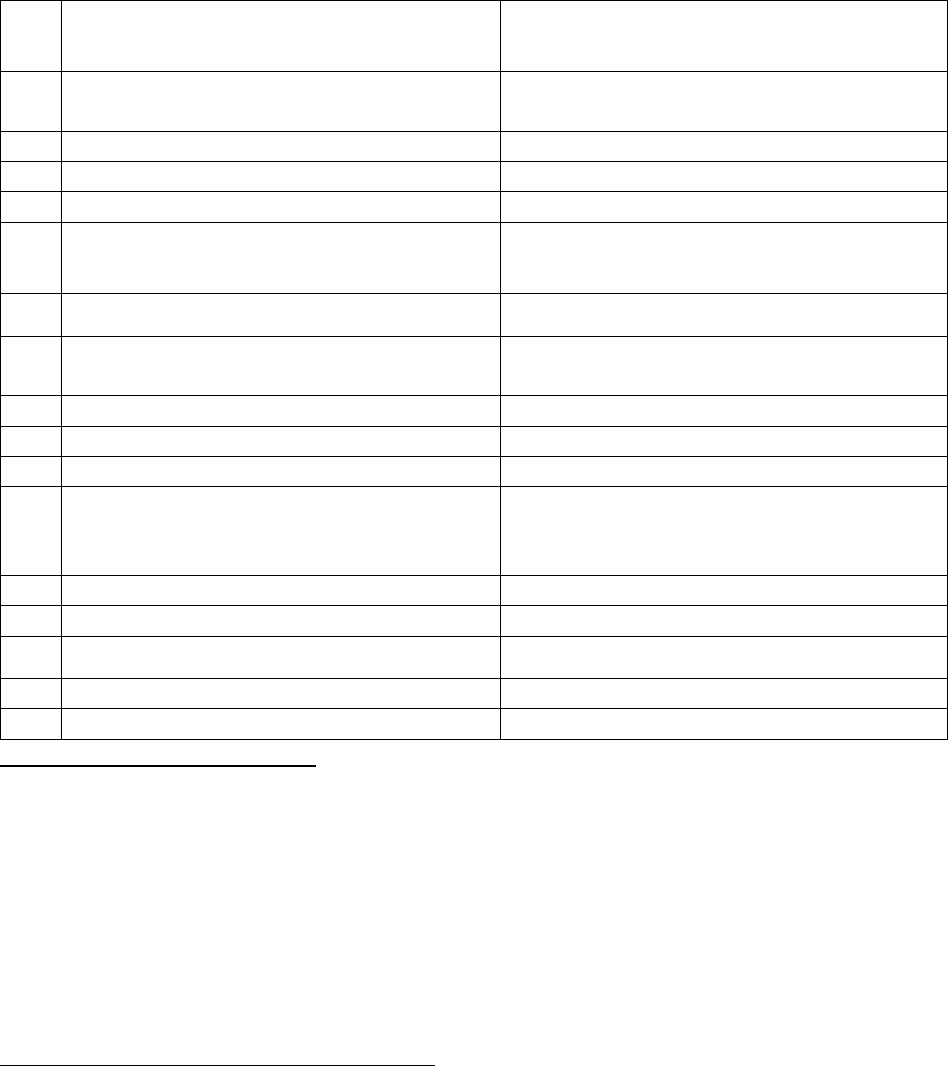
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Avinash Deshpande v/s SBI General Insurance Company Ltd
COMPLAINT NO: PUN-H-0040-2021-0032
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Avinash Arvind Deshpande, Mahad,
Raighad
2.
Policy No:
Type of Policy:
180892-0000-01
Group Health Insurance Policy
3.
Policy period:
9/4/2019 - 8/4/2020
4.
Sum Insured
Not mentioned
5.
Date of inception of first policy:
09.04.2018
6.
Name of the insured:
Name of the Policyholder:
Ayush Avinash Deshpande; 12 years, son
M/s Vinati Organics ltd.
7.
Name of the Insurer:
SBI General Insurance Company Ltd
8.
Reason for repudiation/Partial Settlement:
Deviated Nasal Septum is under policy
exclusion
9.
Date of receipt of the Complaint:
25/5/2020
10.
Nature of complaint:
Total Rejection of claim
11.
Amount of Claim:
69349/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
13 1(b)
13.
Date of hearing/Place:
15/09/2021; Online
14.
Representation at the hearing
n) For the Complainant:
Himself on voice call
o) For the insurer:
Ms. Chynikca Modie
15.
Complaint how disposed:
Dismissed
Contention of the Complainant:
Complainant is having health cover under Group Mediclaim Policy issued to M/s Vinati Organics
Ltd. He is the employee of the policy holder and his son master Ayush is covered in this policy.
He was admitted in Deenanath Mangeshkar Hospital on 26/12/2019 for operation of DNS
(Deviated Nasal Septum) and discharged on 29/12/2019. Complainant has submitted claim for
reimbursement. However, RI has rejected the claim stating that DNS is the exclusion under the
policy.
Complainant aggrieved with the rejection of the claim has filed complaint before this Forum for
resolution of the issue.
Contentions of the Respondent Insurer (RI):
As per the SCN submitted, they have contended that, initially the complainant had applied for
cashless; which was rejected. Thereafter he submitted reimbursement claim.
Based on submitted documents vis-à-vis policy terms & conditions, the Company observed that
the Insured underwent a corrective Surgery for deviated nasal septum which falls under the
Exclusion Clause No. 24 of the subject policy.
Exclusion Clause No. 24 is reproduced hereunder for ready reference and records of Ld.
Ombudsman:
EXCLUSIONS: That Accordingly as per policy exclusion clause No. 24 – “Surgery to correct
Deviated Nasal septum and hypertrophied turbinate unless necessitated by an accidental
body injury and proved to our satisfaction that the condition is a result of an accidental
injury.”
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 15/09/2021 (through video-conferencing), both the parties
reiterated their respective stand.
Complainant submitted that the child was having severe breathing problem due to blocked
nose. Doctor advised for surgery. That he has submitted a doctor’s certificate also to that
effect. He further contended that he has not received such clause along with the group policy,
by which the RI has repudiated his claim. In view of this, the policy is examined by the forum,
wherein in clause no.18 it is mentioned as: ‘All other terms and conditions as per Group Health
Insurance Policy wordings as attached.’ The complainant could have obtained it from his
employer/group administrator.
Upon going through this clause, forum noticed the above clause at exclusion no. 23. In view of
the clear cut exclusion in the policy, present claim is not admissible as the surgery was not
necessitated due to accidental injury.
In view of the above, though the Forum appreciate the complainant’s concern, it has also to be
kept in mind that whenever any dispute arises, it is settled under the terms and conditions of
the policy under which a claim has arisen since these form the very basis of the contract
between the parties. Under the circumstances the Respondent Insurer has acted rightly as per
the terms and conditions of the policy in terms of rejection of hospitalisation claim under the
policy and does not merit any intervention of the forum
Complaint thus disallowed. Award follows:
AWARD
Complaint stands dismissed in view of the clear cut exclusion in the policy.
Dated: at Pune this 16
th
day of September 2021
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Avinash Sangle v/s The New India Assurance Company Ltd
COMPLAINT NO: PUN-H-0049-2021-0015
Award No IO/PUN/A/HI/ /2021-22
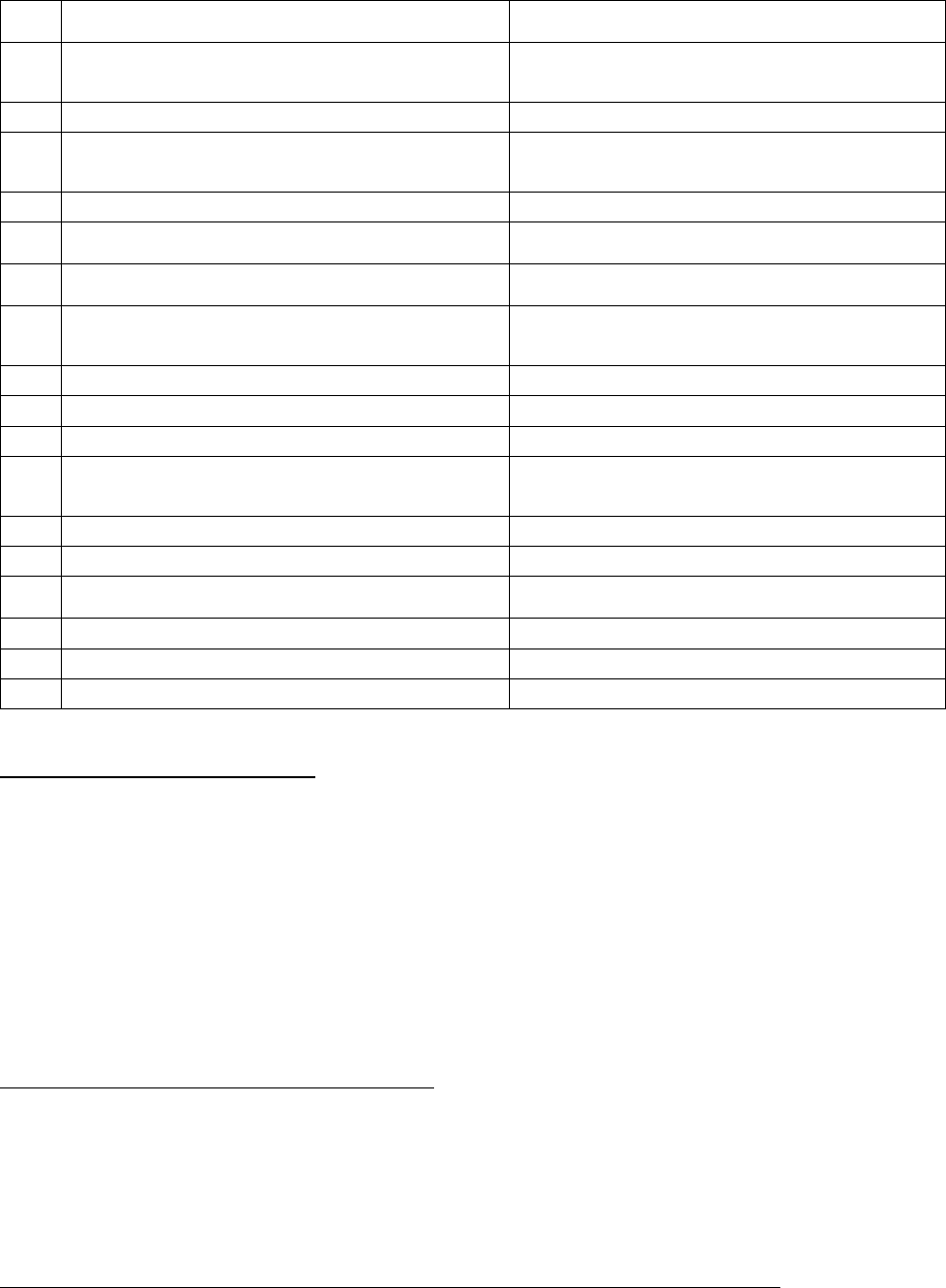
1.
Name & Address of the Complainant
Mr. Avinash P. Sangle, Nasik
2.
Policy No:
Type of Policy:
712500/34/18/21/00000019
Good Health Group mediclaim policy
3.
Policy period:
1/1/2019-31/12/2019
4.
Sum Insured
1,50,000/-+Cumulative Bonus 15% on
Rs.1 lakhs Total Rs.1,65,000/-
5.
Date of inception of first policy:
2017
6.
Name and age of the Insured:
Mrs. Hemlata P. Sangle 61 yrs
7.
Name of the Insurer:
The New India Assurance Company Ltd
8.
Reason for repudiation/Partial Settlement:
Not parenteral chemo and therapy not
covered in day Care
9.
Date of receipt of the Complaint:
18/5/2020
10.
Nature of complaint:
Delay in settlement of claim
11.
Amount of Claim:
74633/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
13 1(b)
13.
Date of hearing/Place:
08.09.2021;Online
14.
Representation at the hearing
p) For the Complainant:
Himself
q) For the insurer:
Mrs Preeti Narayanan
15.
Complaint how disposed:
Allowed
16.
Date of Award:
29.09.2021
Contention of the Complainant:
The complainant has lodged the complainant for delay in settlement of his claim submitted for
his mother, who is covered under Master policy issued to Citibank Account holders by
Respondent Insurer (herein after is called RI)
As per additional details submitted by the complainant, his first claim for cancer in respect of
his mother was settled by the RI for Rs.112520/- on 27/3/2019. Another claim for Rs.74633/- is
pending with RI. Web site of the TPA shows claim is under process. Still after one year also it is
in process as per information given by the complainant.
Contentions of the Respondent Insurer (RI):
As per Self-Contained Note submitted by RI, they have rejected this claim. Their policy covers
only Parental Chemotherapy under day care treatment as per the Good Health Policy clause no.
2.10 and transzutumab being human epidermal growth factor receptor 2 positive which is not a
parental chemotherapy drug. Hence, it is not covered as a day care procedure and is not under
the listed day care procedures.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 08.09.2021 (Online), both the parties reiterated their
respective stand.
The most common way that chemotherapy drugs are given is through a needle into a vein. This
is called intravenous or IV chemotherapy. Chemotherapy can also be taken as a pill, capsule, or
liquid by mouth, as an injection or shot, or as a cream that is put directly on your skin.
Transzutumab is administered for treatment of Cancer. As per definition of Chemotherapy,
Chemotherapy is the use of drugs to destroy cancer cells. It usually works by keeping the cancer
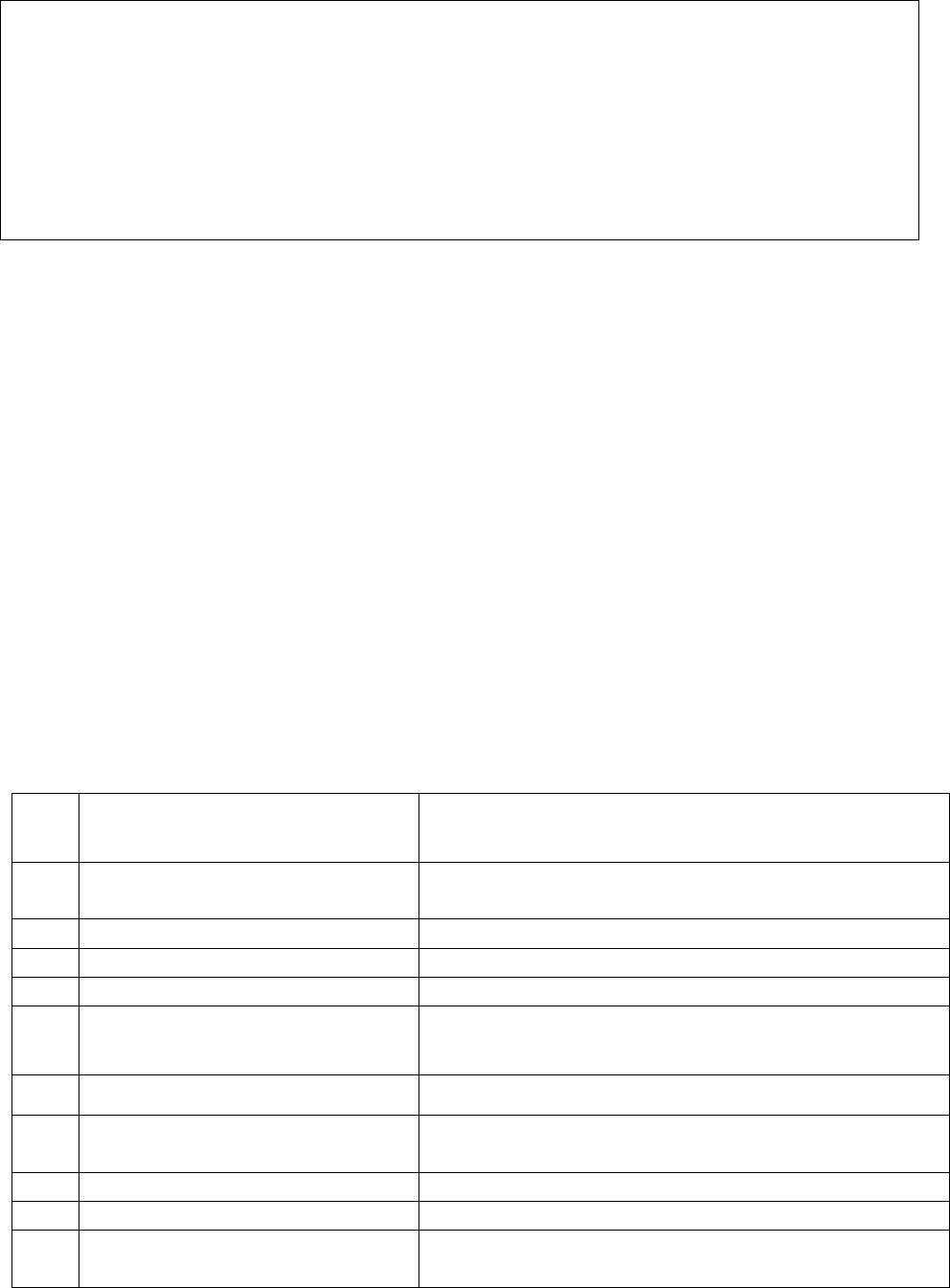
cells from growing, dividing, and making more cells, as cancer cells usually grow and divide
faster than normal cells.
The drug, Transzutumab is administered on patient for this purpose only. Hence rejection of
chemo treatment will be against the policy terms.
In view of this, complaint is allowed. Award follows:
AWARD
Under the facts and circumstances, Respondent Insurer is directed to pay the claim maximum
upto the balance amount of sum insured inclusive of Cumulative Bonus as per terms and
conditions of the policy, to the complainant towards full and final settlement of this complaint.
The award is to be satisfied within one month from the date of receipt of this award failing
which it will attract interest at the applicable bank rate plus 2% extra from the date of rejection
of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17 (8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: On 29
th
day of Sept, 2021
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– SHRI VINAY SAH
CASE OF Mr. Rashmikant K. Pawar v/s United India Insurance Company Ltd
COMPLAINT NO: PUN-H-051-2021-0071
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Rashmikant K. Pawar,
Pune
2.
Policy No:
Type of Policy:
5001002819P111085979
Group Health Insurance Policy
3.
Policy period:
1/10/2019-30/9/2020
4.
Sum Insured
Rs. 4,00,000/-
5.
Date of inception of first policy:
Not applicable
6.
Name and age of the Insured:
Name of the Policyholder:
Neeta Pawar – 35, wife of the complainant
Indian Banks association A/C Bank of Baroda
7.
Name of the Insurer:
United India Insurance Company Ltd
8.
Reason for repudiation/Partial
Settlement:
Reasonable & Customary clause
9.
Date of receipt of the Complaint:
24/7/2020
10.
Nature of complaint:
Partial settlement of claim
11.
Amount of Claim:
10000+interest+1 lakh for mental agony and
harassment.
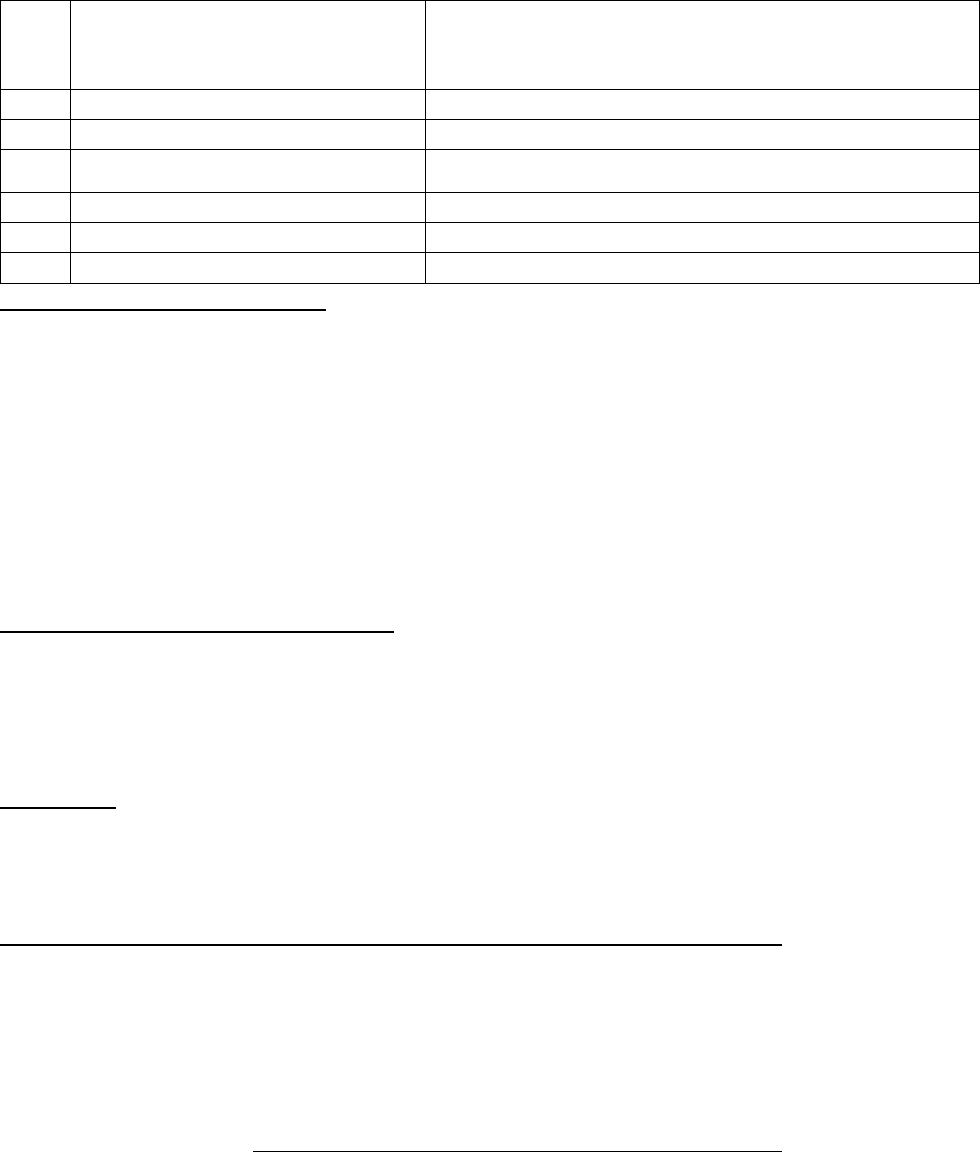
12.
Insurance Ombudsman Rule
(IOR)2017 under which the
Complaint was registered:
13 1( b)
13.
Date of hearing/Place:
Online hearing on 22.09.2021
14.
Representation at the hearing
r) For the Complainant:
Himself
s) For the insurer:
Mrs. Pamella Pinto
15.
Complaint how disposed:
Allowed
16.
Date of Award:
23.09.2021
Contentions of the Complainant:
The complainant is covered under Group Health policy of RI (Respondent Insurer) being
employee of Bank of Baroda. He lodged a reimbursement claim for C section delivery of his
wife.
Total claim amount was Rs.99889/- and an amount of Rs.57500/- was honored by RI against
BOB policy cap of Rs.75000/- for C section with reason Excess of reasonable and customary
charges. Later an additional amount of Rs.7576/- was settled.
Hence, complainant aggrieved with the partial settlement of the claim filed complaint before
this Forum for balance amount with penalty of 12% interest plus 1 lakh for mental Agony and
harassment.
Contentions of the Respondent Insurer:
RI submit that the said policy has a capping of Rs. 75,000/- for LSCS. They have settled this case
as per Reasonable & Customary clause by comparing charges with Niramay Hospital,
Chinchwad, Pune Rs. 40,644/- and Lokmanya hospital Rs. 42,543/-
The (Shashwat) Hospital has charged on higher side for LSCS, so as per Reasonable & Customary
charges, for the surgery as per tariff RI have deducted Rs. 42,389/- and paid Rs. 57,500/-.
Clause 2.42: “Reasonable and customary charges mean the charges for services or supplies,
which are the standard charges for the specific provider and consistent with the prevailing
charges in the geographical area for identical or similar services, taking into account the nature
of illness/injury involved”
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 22.09.2021 (through video conferencing), both the parties
reiterated their respective stand.
During the hearing the Respondent Insurer contended that the amount paid was as per the
geographical area for identical or similar services.
Forum finds that as per clause No 3.5 Maternity expenses benefit extension The Maximum
benefit allowable under this clause will be up to Rs.50000/- for Normal Delivery and Rs.75000/-
for Caesarean section. In view of the clear-cut cover/ceiling provided under the policy forum
finds that maximum payable amount for LSCS is Rs. 75000/-. Actual expenses incurred by the
complainant are more than this amount. There is no need to compare the rates in the vicinity.
Hence RI is liable to pay balance amount of Rs.9924/- in this case.
Forum is not mandated to compensate for the mental Agony and harassment claimed by the
complainant.
Complaint allowed,
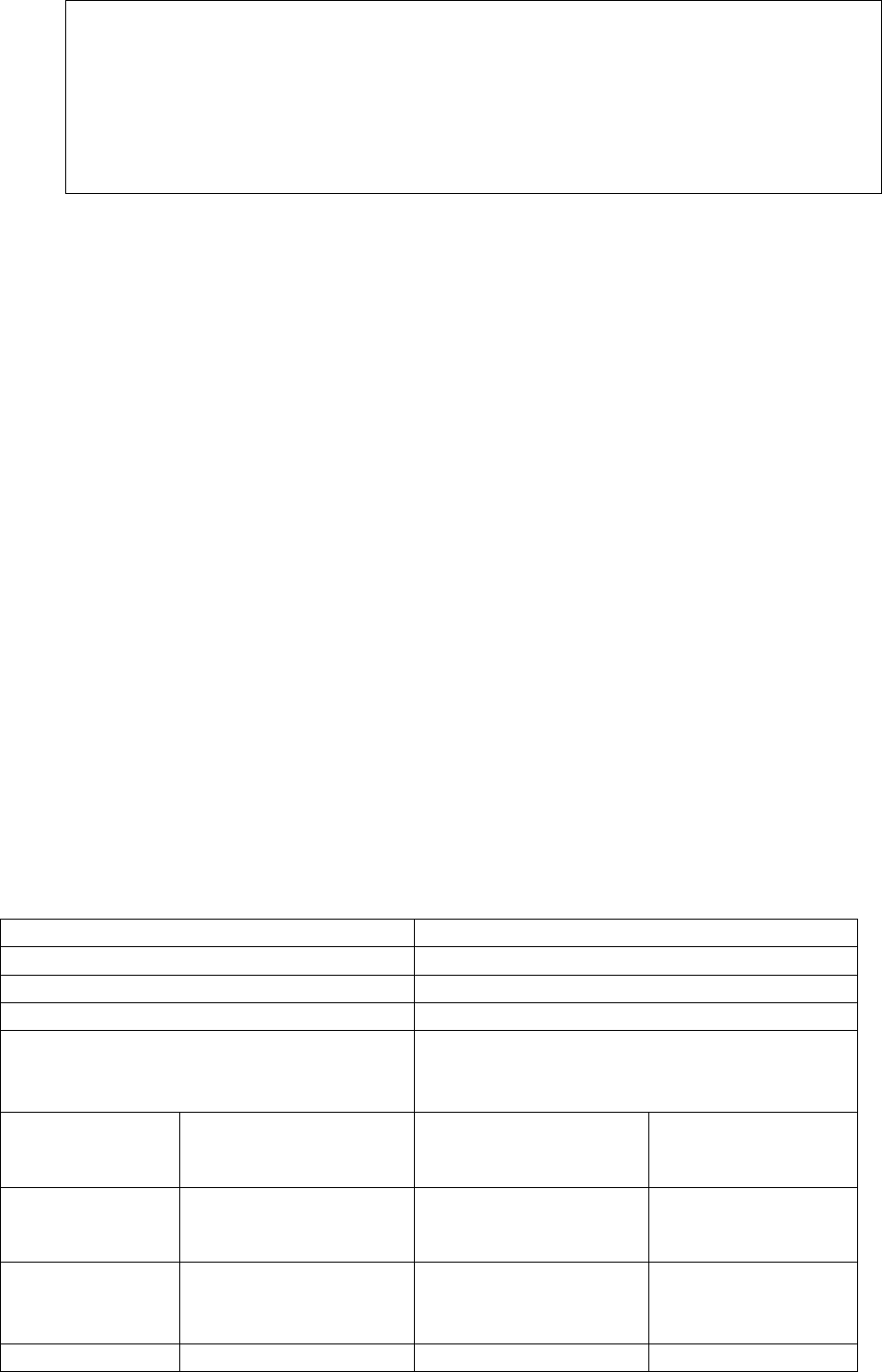
Award follows;
AWARD
Under the facts and circumstances, the RI is directed to pay Rs.9924/- as per the terms
and conditions of the policy to the complainant, towards full and final settlement of
the complaint.
The award is to be settled within one month from the date of receipt of this award
failing which it will attract interest at the prevailing bank rate plus 2% extra from the
date of rejection of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the
award and intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: On this 23
rd
day of Sept 2021, Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE.
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN–VINAY SAH
CASE OF Mr. Sandip Kute; Mr. Santosh Dubey; Mr. Mahesh Gurnani
Vs.
The Oriental Insurance Company Limited
COMPLAINT NO: PUN-H-050-1920-0540; 0541; 0542
Award No IO/PUN/A/HI/ ; ; /2021-2022
Policy No.
112200/48/2018/708
Policy Period
01/09/2017 to 31/08/2018
Type of Policy:
Group Mediclaim Tailormade Policy
Name of the Policyholder
M/s Vero Moda Retail Pvt. Ltd.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
13(1)(b)
Complaint No.
PUN-H-050-1920-0540
PUN-H-050-1920-0541
PUN-H-050-1920-
0542
Name of the
complainant
Mr.Sandip Kute
Mr.Santosh Dubey
Mr.Mahesh Gurnani
Nature of
complaint:
Partial Repudiation of
claim
Partial Repudiation of
claim
Partial Repudiation
of claim
Amount of
52,276/-
24,590/-
10,305/-
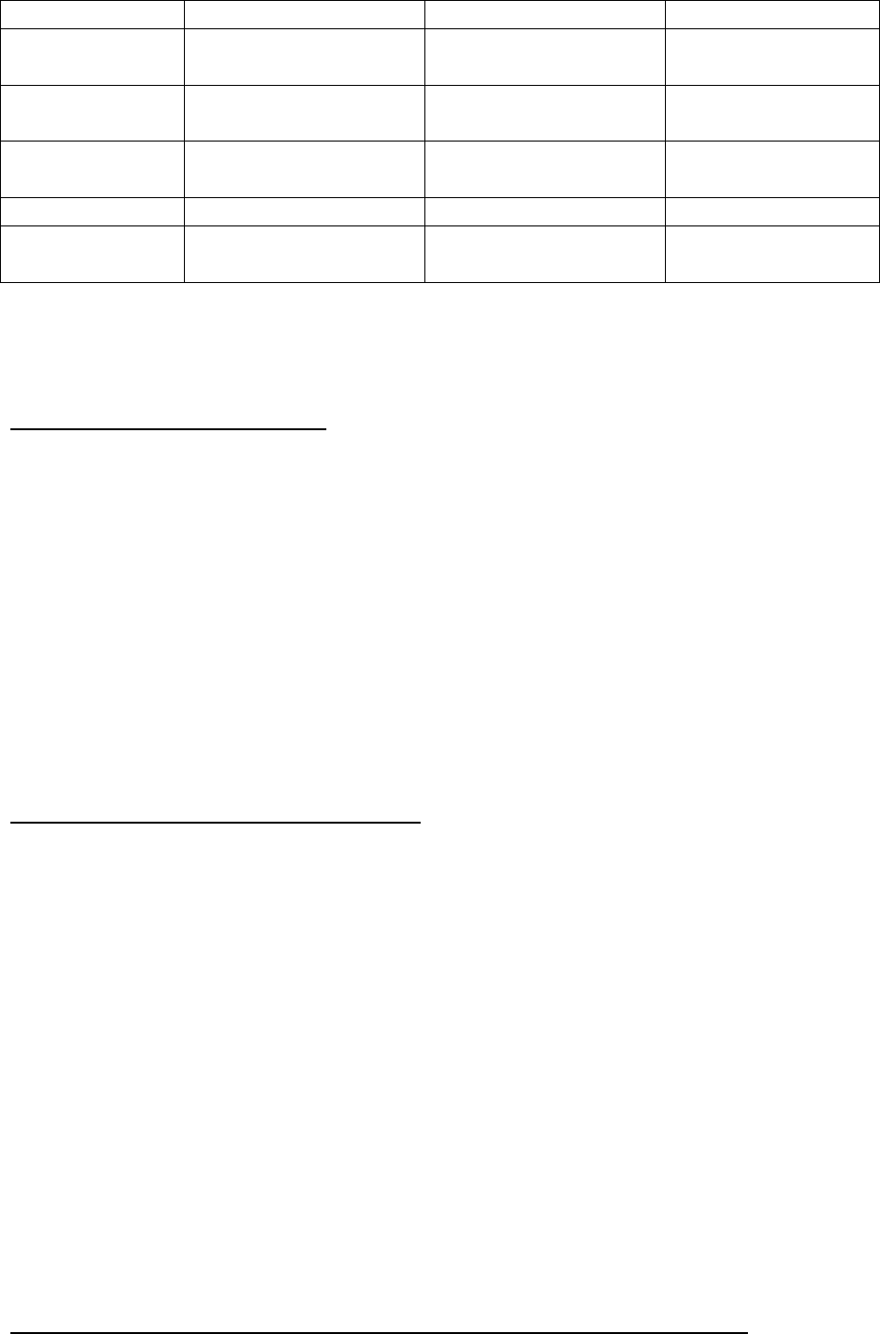
Claim: Rs.
Date of
hearing/Place:
25/06/2021; Online
25/06/2021; Online
25/06/2021; Online
Representation
at the hearing
For the
Complainant:
Mr. Sandip Kute
Mr. Santosh Dubey
Mr. Mahesh Galani
t) For the insurer:
Mr. Ganesh Meshram
Mr. Ganesh Meshram
Ganesh Meshram
Complaint how
disposed:
Allowed
Allowed
Allowed
All the above three complainants have common issue of dispute on short payment of their
claims against The Oriental Insurance Co. Ltd., under a common group health insurance policy
provided by their employer. Hence, all these three complaints were heard on the same day
and are being disposed of under a common judgment as detailed below:
Contentions of the Complainants:
The Complainants are beneficiary/members of the Group Mediclaim Tailor made Policy bearing
no.112200/48/2018/708 valid from 01/09/2017 to 31/08/2018. Their hospitalization claims
were short paid by the Respondent insurer (RI) by applying Co-pay clause. The complainants, by
raising an objection on 20% deductions on their admissible claim amounts, have filed the
complaints before this forum for resolution.
They have contended that at the beginning of the policy, the co-payment clause was not there.
This clause was inserted in the policy without their knowledge. They have not received any
communication or information from their employer or by insurance company about inclusion of
Co-payment clause in the middle of the policy period. Complainants have lodged complaints
with this forum alleging that co-pay clause was wrongly applied by the Respondent Insurer.
Despite repeated reminders to the RI to reconsider the deducted amount they did not receive
any communication from the RI.
Contentions of the Respondent Insurer (RI):
The contents of RI are reproduced below:
‘1) This policy was renewed with our DO for the year 2017-2018. Endorsement was
passed under policy No. 112200/48/2018/708 for 20% co pay applicable since inception
of the policy (Endt already sent). The reason for incorporating Co-Pay under the renewal
policy was due to adverse ICR (343%) under expiring policy.
2) The policy was placed through intermediary (Broker), M/s Edelweiss Insurance
Brokers and as per IRDA guidelines Broker can arrange quote/terms from the Insurer on
behalf of client and they can communicate with Insurer and receive communication from
the Insurer on behalf of their client. Please refer functions of Broker in the attached
guidelines of IRDA (Insurance Brokers Regulations, 2013 & 2018).
3) Mail dated 25th September 2017 was sent by our official to TPA regarding co pay
and cc to broker Mr Atul Pawar of Edelweiss Broker, Ms Ameeta Pawar and Kirti Pawar
of Edelweiss Broker. ( Pl refer 1st attachment)
4) The terms were accepted by the broker and no representation received by us from
Broker or Corporate Client on incorporation of Co-Pay in the renewal policy.’
Result of personal hearing with both the parties (Observations & Conclusions):
Personal hearings were conducted on 25/06/2021 (through video-conferencing), which were
attended by all the parties.
Complainants submitted that change in the policy terms and conditions regarding imposition of
20% co-pay was not communicated to them by their employer and/or Respondent Insurer.
Therefore, they are entitled to get back the deducted amounts, as the same were deducted
wrongly.
Respondent Insurer contended that due to adverse claim ratio (343%) of the policy holder it
was decided to impose 20% co-pay, and the same was communicated to Edelweiss Gallagher
Insurance Broker through e-mail on 25/09/2017 i.e. after 25 days from the commencement of
the policy (pol. Period- 01/09/2017 to 31/08/2018). He also contended that if any insurance
business is placed through broker, modification/s if any, are communicated to the broker only,
as per prescribed norms for businesses placed by the brokers.
Having listened to the both the parties, forum has asked Complainant to submit copies of
communications received from Insurance Broker and his employer wherein it was
communicated that they were not informed by the Respondent Insurer pertaining to Co-
payment clause at any point of time. The RI was also asked to submit the communication
initiated and exchanged between them and the concerned broker regarding mid-term inclusion
of co-pay clause in the policy.
Accordingly, both the parties submitted whatever communications they had with each other,
for our perusal. Forum has considered all submissions, contentions and evidences and has the
following observations to make:
25. Forum does not deny the need of imposition of any lawful conditions in a tailor made
group policy, in view of the high claim ratio. But at the same time RI should bear in mind
that insurance being a legal contract, they obviously have to follow its terms and
conditions.
xi. RI has not submitted its Self contained Note in a formal way. They have provided the
information as and when the forum raised its queries, in an informal way and in
piecemeal.
xii. Respondent Insurer have furnished records of emails exchanged between them,
Paramount TPA and two representatives of Edelweiss Gallagher Insurance Broker
namely Mr. Atul Pawar and Kirti Pawar. The e-mail dated 25/09/2017 of RI’s policy
issuing office addressed originally to one official of Paramount TPA and CC to two
officials of the broker states as under:
“pls note that the Renewal Policy nos of Best Seller, Vero Moda and Only retail
numbering 112200/48/2018/707, 112200/48/2018/708 and 112200/48/2018/709 are
subject to 20% Copay Condition for all the Reported Claims from inception”.
xiii. While imposing the co-pay, RI has not referred to any of their discussions with the
broker or the policy holder nor have they produced any acknowledgement of accepting
of the said condition by the broker and ultimately by the insured M/s.Vero Moda.
xiv. The RI’s contention of giving information of copay clause is totally relied upon their
mail dt. 25/09/2017, which was addressed to the TPA and not to the broker. Only cc is
seen as marked to the representatives of the brokers.
However, it is surprising that why the brokers, having received this mail, did not raise
any objection to decision of imposition of copay clause by the RI, if it was unilateral.
xv. It is not clarified by the RI why the mail for imposition of 20% copay was actually
passed by endorsement on 16/11/2017, if it was already decided to impose it as on
date of their mail dt.25/09/2017.
xvi. Complainants have produced a letter dated 5
th
July 2021, which is after the hearing of
these complaints (on 25/06/2021) from their employer Vero Moda Retail Private
Limited confirming that the policy was obtained through the Edelweiss Gallagher
Insurance Broker and there was no such reference to the Co-pay condition in the policy
and the RI had never intimated the inclusion of co-pay condition in the policy.
Complainants have also produced a letter dated 03/02/2020 of Edelweiss Gallagher
Insurance Broker originally addressed to Vero Moda Retail Private Limited stating that
they had not made any reference to the RI for inclusion of Co-pay condition in the
policy. They also confirmed that endorsement of Co-pay was passed by the RI without
their knowledge.
26. It is also not understood why the RI had not taken any objection to the broker for not
intimating to the complainant about the imposition of the said policy clause, if it’s
decision was taken with their consent or after discussions with the brokers at least.
27. It also not clear why the broker did not take any action against the RI, if their contention
was true and proceeded for the cancellation of policies as prescribed in the clause no.
5(d) of the Rights and duties of the brokers, quoted below:
INSURANCE REGULATORY AND DEVELOPMENT AUTHORITY (INSURANCE BROKERS) REGULATIONS, 2013:
5.Conduct in relation to explanation of insurance contract — Every insurance broker shall: (a) provide the
list of insurer(s) participating under the insurance contract and advise any subsequent changes
thereafter; (b) explain all the essential provisions of the cover afforded by the policy recommended by
him so that, as far as possible, the prospective client understands what is being purchased;
(c) quote terms exactly as provided by insurer;
(d) draw attention to any warranty imposed under the policy, major or unusual restrictions, exclusions
under the policy and explain how the contract may be cancelled;
(e) provide the client with prompt written confirmation that insurance has been effected. If the final
policy wording is not included with this confirmation, the same shall be forwarded as soon as possible;
(f) notify changes to the terms and conditions of any insurance contract and give reasonable notice
before any changes take effect;
(g) advise its clients of any insurance proposed on their behalf which will be effected with an insurer
outside India, where permitted, and, if appropriate, of the possible risks involved;
28. The complainants have produced a letter issued by the said broker to the employer M/s
Vero Moda dt. 03/02/2020; wherein they have stated that the said endorsement was passed
by the RI arbitrarily. It is not understood why it took almost one and half years after the
policy period got over (on 30/08/2018).
It is also surprising that why the policy holder M/s Vero Moda has raised the objection
only after hearing date. It was not a formality to complete from the complainant’s side,
but an obvious action an insured would have taken in such a sensitive violation of the
policy terms, if it was made by the RI, unilaterally. Till then, they did not raise any
objection with the RI or with the broker at that time itself when they got the knowledge
of this clause. Keeping silence or not objecting the terms newly imposed, amounts to
acceptance of the terms.
29. RI’s entire approach to such a sensitive issue of imposition of 20% copay, is totally a
callous and unprofessional one.
In view of the flaws on all the counts, done by all the three parties involved in this case,
forum finds that the RI should pay the remaining claim amount deducted towards 20% of
copay and may recover 50% of it from the erring broker if they find that their stand of
imposition of copay was taken by adhering the basic principles of a legal contract.
Under the facts and circumstances, complaints are allowed.
Award follows:

AWARD
Under the facts and circumstances of the case, Respondent Insurer is advised to pay the
remaining claim amount deducted towards 20% of copay and may recover 50% of it from
the erring broker if they find that their stand of imposition of copay was taken by them
adhering to the basic principles of a legal contract.
The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: on this 6
th
day of September 2021 at Pune
VINAY SAH
Insurance Ombudsman, Pune
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Santosh Zalte v/s The New India Assurance Company Ltd
COMPLAINT NO: PUN-H-049-1920-0717
Award No IO/PUN/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Santosh Zalte, Pune
2.
Policy No:
Type of Policy:
142300/34/19/04/00000041
New India Flexi Floater Group Health policy
for Retired employee of Maharashtra Govt.
3.
Policy period:
25/7/2019-24/7/2020
4.
Sum Insured
400000/-
5.
Date of inception of first policy:
25/7/2019
6.
Name and age of the Insured:
Name of the Policyholder:
Sulakshana; 43 years – wife
SWASTHYA Serving and Retired employees
of Maharashtra Govt.
7.
Name of the Insurer:
The New India Assurance Company Ltd
8.
Reason for repudiation/Partial Settlement:
Not a parenteral chemotherapy
9.
Date of receipt of the Complaint:
24/2/2020
10.
Nature of complaint:
Total Repudiation of claim
11.
Amount of Claim:
3 claims –Rs.90277/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
Rule 13 1(b)
13.
Date of hearing/Place:
23/08/2021; Online
14.
Representation at the hearing
u) For the Complainant:
Himself
v) For the insurer:
Mr. Pankaj Ninawe
15.
Complaint how disposed:
Allowed
Brief Facts of the Case:
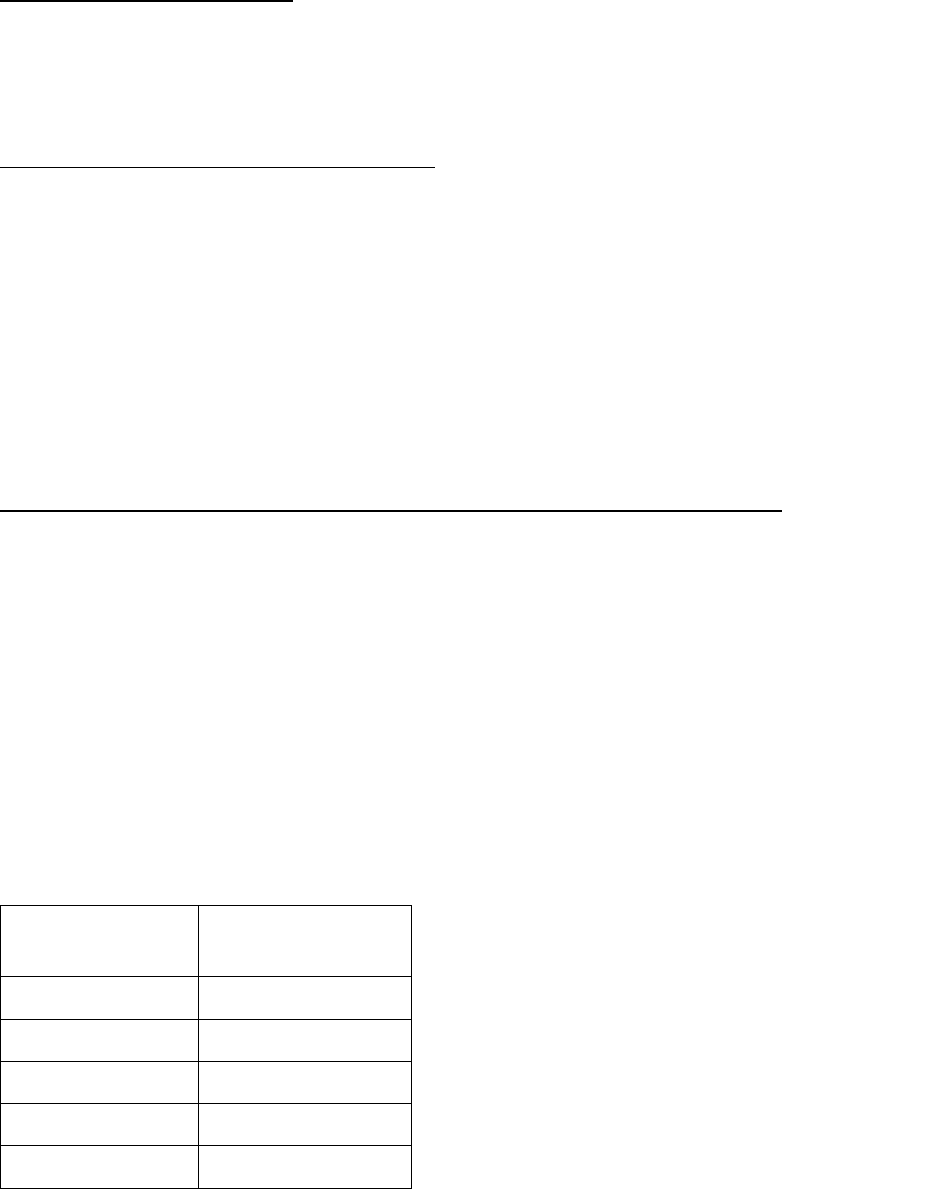
The Complainant is the member of Group policy issued by Respondent Insurer (herein after is
called RI) to Retired Employees of Maharashtra Govt. for sum insured of Rs.400000/-.
Wife of the complainants was suffering from Left breast cancer. For that,
immunotherapy/targeted therapy of Trastuzumab was advised by the treating doctor.
Accordingly, treatment was taken four times on Day care basis. And these expenses were
claimed by the complainant with RI. However, RI has rejected all four claims stating that policy
covers Parenteral administration chemotherapy only and Trastuzumab being Human Epidermal
Growth Factor Receptor 2 Positive which is not a Parental Chemotherapy.
Complainant disappointed with the rejection of all claims, lodged a complaint before this Forum
for resolution of issue.
Contentions of Complainant:
As per complaint three claims for three admissions dated 8/8/2019, 29/8/2019, 19/9/2019 for
his wife were submitted to the RI but all the claims were rejected. Complainant has requested
vide his complaint to settle these claims since amount involved in claims is high. And also, there
is further requirement of treatment since the illness is very serious.
Contentions of the Respondent Insurer (RI):
RI has submitted Self Contained Note dated 11/3/2020.
As per SCN, a 43 years old female patient treated in Phadnis Clinic Pvt. Ltd. Patient was treated
for Carcinoma of Left Breast on Day care basis on 8/8/2019, 29/8/2019, 19/9/2019.
The claims are repudiated under clause no. 3.14.1 (narrated below) as there is hospitalization
for less than 24 hours.
“Hospitalization means admission in a hospital for a minimum period of 24 hours except for
specified procedures /treatment, where such admission could be for a period of less than 24
consecutive hours.”
Result of personal hearing with both the parties (Observations & Conclusions):
A personal hearing was held on 23/08/2021 (through video-conferencing), which was attended
by both the parties.
Regarding chemotherapy, the most common way that chemotherapy drugs are given is through
a needle into a vein. This is called intravenous or IV chemotherapy/ Parenteral Chemotherapy.
Trastuzumab is administered in a similar way.
It is seen that the policy covers 35 procedures under Day Care and one of them is Parenteral
chemotherapy. As per above definition of Parenteral Chemotherapy, the treatment taken by
insured, can be considered in Day care coverage.
During the hearing RI was asked to inform this forum the payable amounts in all the claims
reported in this respect. They have informed the details of claims reported as mentioned
below:
Date of
treatment
Amount claimed
(Rs.)
8/8/2019
31982
29/8/2019
36013
19/09/2019
22282
27/04/2020
18307
Total
1,08,584
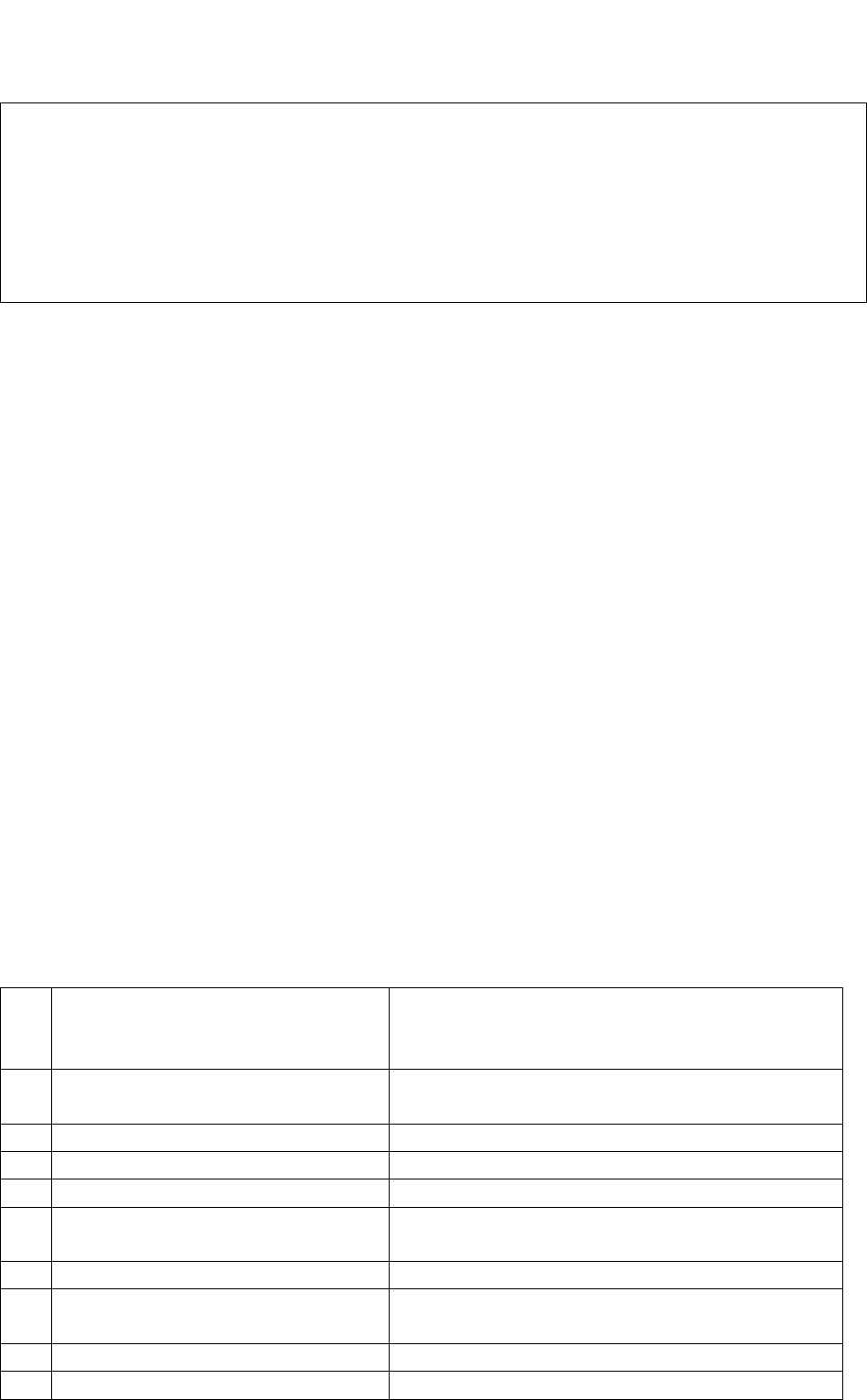
RI has to process these claims for admissible amounts treating those under day care treatment,
only. Complaint admitted.
Award follows:
AWARD
Under the facts and circumstances of the case, the Respondent Insurer is directed to pay
the total of claimed amount of Rs.1,08,584/- less deductibles as per the policy terms and
conditions to the complainant towards full and final settlement of the complaint.
The award is to be complied with within one month from the date of receipt of this award
failing which it will attract interest at the bank rate plus 2% extra from the date of
rejection of claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: On 23/09/2021 at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN – VINAY SAH
CASE OF Mrs. Suvidha Daji Todankar Vs. National Insurance Company. Ltd.,
COMPLAINT NO: PUN-H-048-1920-0545
Award No IO/PUN/A/HI/ /2021-2022
1.
Name & Address of the
Complainant
Mrs. Suvidha Daji Todankar
603, Matri Arcade, Plot No. 12 & 13, Sector 20,
Kamothe, Navi Mumbai - 410209
2.
Policy No:
Type of Policy:
260100/50/18/10000446
Tailormade Group Mediclaim Insurance
3.
Policy period:
16/07/2018 to 15/07/2019
4.
Sum Insured/IDV
Rs. 17,14,00,000/- (for whole group)
5.
Date of inception of first policy:
Details not available.
6.
Name & age of the Insured:
Name of the Policyholder:
Smt. Rupali Lahu Labde – Age: 60 years.
M/s CitiusTech Health care Technology Pvt. Ltd.
7.
Name of the Insurer:
National Insurance Company Ltd.,
8.
Reason for rejection /Partial
Settlement:
Policy cancelled
9.
Date of receipt of the Complaint:
05/12/2019
10.
Nature of complaint:
RI not responding – non-settlement of claim
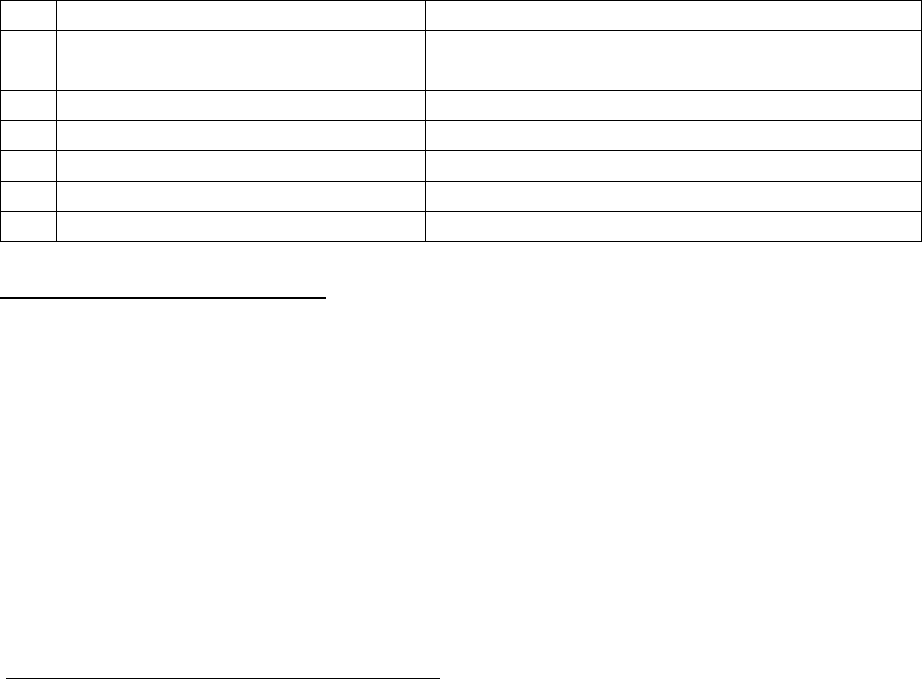
11.
Amount of Claim:
Rs.1,80,000/-
12.
Rule of IOR 2017 under which the
Complaint was registered:
13(1)(b)
13.
Date of hearing/Place:
25/06/2021, Online. Pune
14.
Representation at the hearing
w) For the Complainant:
Absent.
x) For the insurer:
Sachin Mahadik.
15.
Complaint how disposed:
Dismissed.
Contentions of the Complainant:
Complainant is an employee of Citius Tech having employee ID CT3184. Her Mother-in-law Mrs.
Rupali Lahu Labde was covered under ‘GMC policy for parents’ of RI. She was admitted to Jaslok
Hospital, Mumbai on 14/03/2019 with the complaints of severe back and stomach pain. The
Complainant had incurred an amount of Rs.1,80,000/- towards the treatment of her mother in
law. She lodged claim for the same by submitting all claims related documents to the Edelweiss
Insurance Broking Pvt. Ltd., the authorized broker of the Complainant’s employer, for necessary
approval of the claim. For a long time, the broker kept telling her that the claim is under
process. Later, she came to know that her employer has discontinued Group Mediclaim Policy
with Respondent Insurer since February 2019 and all documents have been submitted to
United India Insurance Company Limited (new insurer) for reimbursement.
Losing all hopes of getting her claim settled by National Insurance Co. or Edelweiss Broker, the
Complainant has approached the forum with the request to intervene and resolve the issue.
Contentions of the Respondent Insurer (RI):
Insured Ms. Citius Tech Healthcare Pvt. Ltd. was issued group mediclaim policy covering parents
(918 lives) as per data submitted by the insured.
The policy was issued with a review clause stating that: “The total outgo of the policy (Claims +
Brokerage + IBNR on Earned Premium basis upto 31.12.2018 may be reviewed and in case ICR
is above 95%, we may collect additional premium on as if basis. If insured is unwilling to pay,
we can cancel the policy with due notice period)”.
Accordingly, policy was reviewed in Jan 2019 and claim data was collected from Paramount
TPA. It was found that ICR was above 95%. The insured was asked to pay additional premium of
Rs. 33,22,925 on the basis of total outgo, failing which the policy shall be cancelled. This was
communicated to authorized broker Ms. Edelweiss Insurance Broker Ltd. on 17.01.2019.
Additionally, notice of 30 days vide letter was sent on 25.01.2019 to the insured Ms. Citius
Tech. on its registered address. Further, a telephonic reminder in presence of Deputy General
Manager & Regional Manager was also made to brokers on 28.01.2019. Which was also
recorded vide mail dt. 28.01.2019 to brokers with request to ensure that the insured is also
updated in this matter.
They neither received any communication from Insured/Brokers nor was additional premium
paid. Finally, due to non-receipt of additional premium, after 30 days of notice the policy was
cancelled on 16.02.2019 and refund of premium for remaining period was credited to Cash
Deposit of Insured. The cancellation of the policy was communicated to TPA vide mail dt.
18.02.2019 and Insured Ms. Citius Tech vide letter dt. 18.02.2019 which was acknowledged by
the insured and authorized brokers.
TPA was instructed vide mail dt. 18.02.2019 not to entertain any further intimation/processing
of claims post 15.02.2019 midnight as the policy stands cancelled w.e.f. 16.02.2019.
The insured patient was admitted to hospital on 14.03.2019 which falls after policy cancelation
date 16.02.2019, so the claim is not tenable under the policy.
The complainant had discussion related to mediclaim with her employer and broker. It may be
noted that both the parties were already intimated that the policy was cancelled w.e.f.
16.02.2019.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 25/06/2021 (through video-conferencing) the Complainant
remained absent. RI representative reiterated their stand.
From the available documents, forum notes that there exists a clear condition in the policy, of
calling for additional premium if the claim ratio goes above 95%. And also right to cancel the
policy if the insured in unwilling to pay.
Upon review, as the ICR was found to be 110%, RI had invoked this condition and called for
additional premium from the policyholder. Reminders for additional premium was also sent.
And as the additional premium or any communication was not forthcoming, 30 days’ notice for
cancellation of policy was served. Getting no revert, policy was cancelled w.e.f. 16.02.2019. All
the actions were well communicated to the insured and the authorized broker. Forum finds
that the RI has taken all steps as per laid down procedure and according to policy T & C.
Therefore, this forum does not find any flaw with the cancellation of the policy and as a result
the claim of the insured patient is not payable in the absence of the policy cover. The forum
upholds the decision of RI and disallowed the Complaint.
Award follows:
AWARD
Taking into account of the facts and circumstances of the case the decision of the
Respondent Insurer in cancellation/termination of the policy is in accordance with the
terms and conditions of the policy and does not warrant any interference at the hands of
the Ombudsman.
Hence, the Complaint is Dismissed.
Dated: On 9
th
day of September, 2021 at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
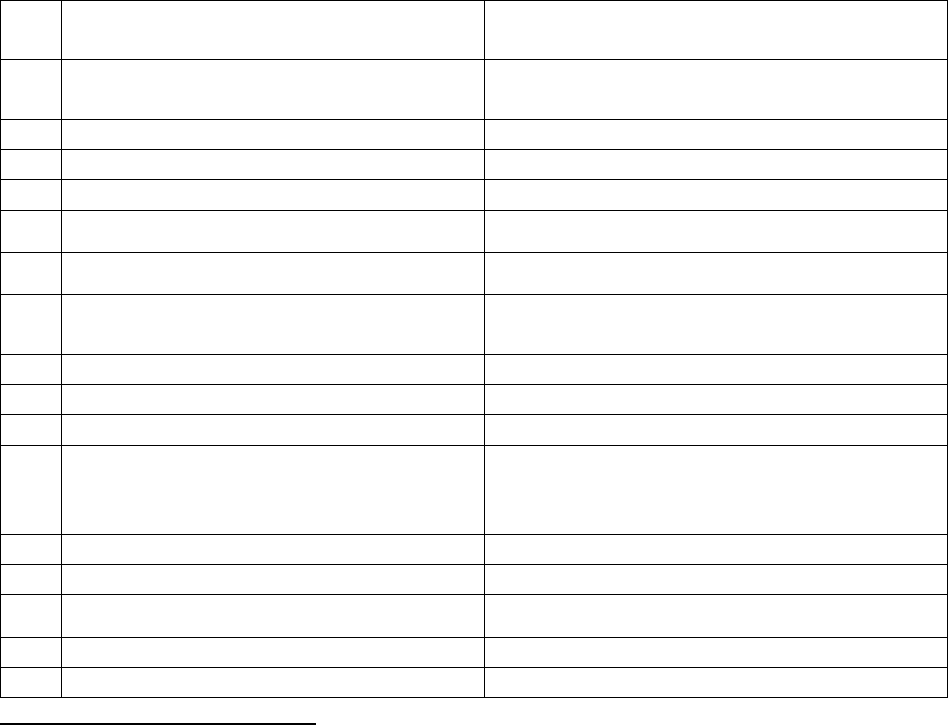
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Vaibhav Yadav Vs Reliance General Insurance Co. Ltd
COMPLAINT NO: PUN-G-035-2021-0094
Award No IO/PUN/A/GI/ /2021-22
1.
Name & Address of the Complainant
Vaibhav Anand Yadav,Thane
2.
Policy No:
Type of Policy:
Group policy 9202962933000058
Reliance Home loan Protect Policy
3.
Policy period:
05/04/2018 to 04/04/2023
4.
Sum Insured
Rs.32,00,000/-
5.
Date of inception of first policy:
5/4/2018
6.
Name of the Policyholder:
Vaibhav Yadav
7.
Name of the Insurer:
Reliance General Insurance Co. Ltd
8.
Reason for the complaint:
Interest and penalty imposed by financer
due to Delayed settlement of claim
9.
Date of receipt of the Complaint:
01/03/2021
10.
Nature of complaint:
Interest and penalty levied by financer
11.
Amount of Claim:
Rs.27408/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
13 1(b)
13.
Date of hearing/Place:
22/07/2021, Online. Pune.
14.
Representation at the hearing
y) For the Complainant:
Himself.
z) For the insurer:
Mr. Samir Pawar & Ms. Vasundhara.
15.
Complaint how disposed:
Allowed.
Contention of the Complainant:
The Complainant had taken home loan of Rs. 32 lakhs from Reliance Home Finance Ltd. to buy a
new flat situated at Bhayander, Thane (w). To protect the interest of the property the financer
also arranged Home loan protect policy from the Respondent Insurer from 05/04/2018 to
04/04/2023. As per policy benefit section C, 6 EMIs @27,771/- are payable in case of loss of
employment.
Due to breakout of Covid 19 the complainant was laid-off from his employment with effect
from 01/08/2020 and due to which he was not in a position to pay monthly EMI from August
2020. He immediately intimated RI about job loss and requested to process 6 months EMI
(From August 2020 to January 2021). RI processed EMIs as detailed below:
6. For the month of August & September 2020 on 13/10/2020.
As both the EMI were not deposited within the stipulated time the Reliance Home
Finance Ltd. started imposing penalty for Bouncing of Cheque, other over dues and ECS
return Charges.

7. Complainant shared home loan account statement and Cheque Bounce letter to RI on
21/12/2020 and requested to process pending 4 EMIs (October 2020 to January 2021).
Looking to the delay in paying the monthly installments, he registered complaint to the
forum on 25/03/2021.
8. After registration of complaint with this forum the RI released two EMIs for the month
of October and November 2020.
9. Finally, on 13
th
April 2021 the RI has paid 2 EMIs for the month of December 2020 and
January 2021.
As the Respondent Insurer has not deposited all six EMIs within the time frame, the
complainant was fastened with penalty for delay, overdue interest charges, Cheque bounce
charges and ECS return Charges from the Reliance Home Finance Ltd. to the tune of Rs.
27,408/-.
Aggrieved with the delayed settlement of monthly EMI and imposition of penalty from the
home finance company RHFL the complainant has approached to the forum for resolution of his
grievance.
Contention of the Respondent Insurer:
Respondent Insurer has not submitted SCN.
Result of personal hearing with both the parties (Observations & Conclusions):
A personal hearing was held through video-conferencing on 22/07/2021 where Complainant
and two representatives of RI have represented their respective stand.
Complainant shared his experience of trauma and mental harassment received from Reliance
Home Finance Ltd. He had received constant mental pressure from Reliance Finance Ltd that his
account will be declared as NPA, house will be sealed and severe action will be initiated for
non-payment of monthly installments. Adding to that, the loan recovery agents also constantly
threatened him for paying monthly EMIs. Ultimately he withdrew money from his EPFO account
and paid EMI for the month of October 2020. He had also been penalized for delayed payment
and heavy fine for cheque bounce. After a long persuasion the RI finally paid remaining 2
installments and thus finally, all 6 installments stood paid as on 13
th
April 2021. Due to delay in
payment of all six installments the Reliance Home Finance Limited imposed bounce charges Rs.
5250/-, Other over dues Rs. 17379/- and ECS return charges Rs. 4779/-, Total Rs. 27,408/- which
the RI should bear the cost. During the hearing, the complainant was asked to forward the
statement of home loan account, in support of his contentions of the financial loss suffered by
him. Accordingly, he has submitted the same.
Forum has gone through the Home Loan Account Statement of the Complainant. It is confirmed
that Reliance Home Finance Limited has imposed Cheque Bouncing Charges of Rs. 5250/- and
other Over dues (OD Charges) of Rs.17,379/- during the period from 05/08/2020 to 05/04/2021
on various dates. All together the total amount comes for Rs.22629/- (Rs. 5250 + Rs. 17379/-).
This financial burden, the Complainant had to bear due to delay in settlement of 6 EMIs by RI
from August 2020 to January 2021.
RI could not give satisfactory replies for the delayed payment. They said they pay the agreed
EMIs to the financers after getting confirmation of default payment from them. In this
procedure, the complainant has no role to comply with. The RI has not produced any specific
clause stating the procedure of payment and time schedule for payment of such claims once
those are approved for settlement.
In view of this, the forum has reasons to believe that the Respondent Insurer has failed to
honor the Section C of the policy which safeguards a policy holder to protect 6 EMIs in case of
Loss of employment. Respondent Insurer has cleared all 6 EMIs of the Complainant but they
were not presented as per schedule of the home loan time table. Therefore, the Respondent
Insurer is directed to release the amount of Rs.22629/-(additional financial liability incurred on
Cheque Bouncing Chares and OD Charges) to the Complainant.
Complaint allowed.
Award follows:
AWARD
Taking into account of the facts and circumstances of the case and the submissions made
by both the parties and documents submitted by the Complainant the Respondent
Insurer is directed to pay Rs.22629/- to the complainant towards full and final
settlement of the complaint.
The award is to be complied with within one month from the date of receipt of this
award failing which it will attract interest at the bank rate plus 2% extra from the date
of receipt of the complaint to this forum till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) the insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) the award of Insurance Ombudsman shall be binding on the insurers.
Dated: On 20/9/2021 at Pune
VINAY SAH
Insurance Ombudsman, Pune
