PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF TAMILNADU & PUDUCHERY
(UNDER RULE NO: 16/17 of the INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Segar Sampathkumar
CASE OF Sri. G. Virabadran vs M/s. National Insurance Company Limited
COMPLAINT REF: NO: CHN-H-048-2122-0964
Award No: IO/CHN/A/HI/0010/2022-2023
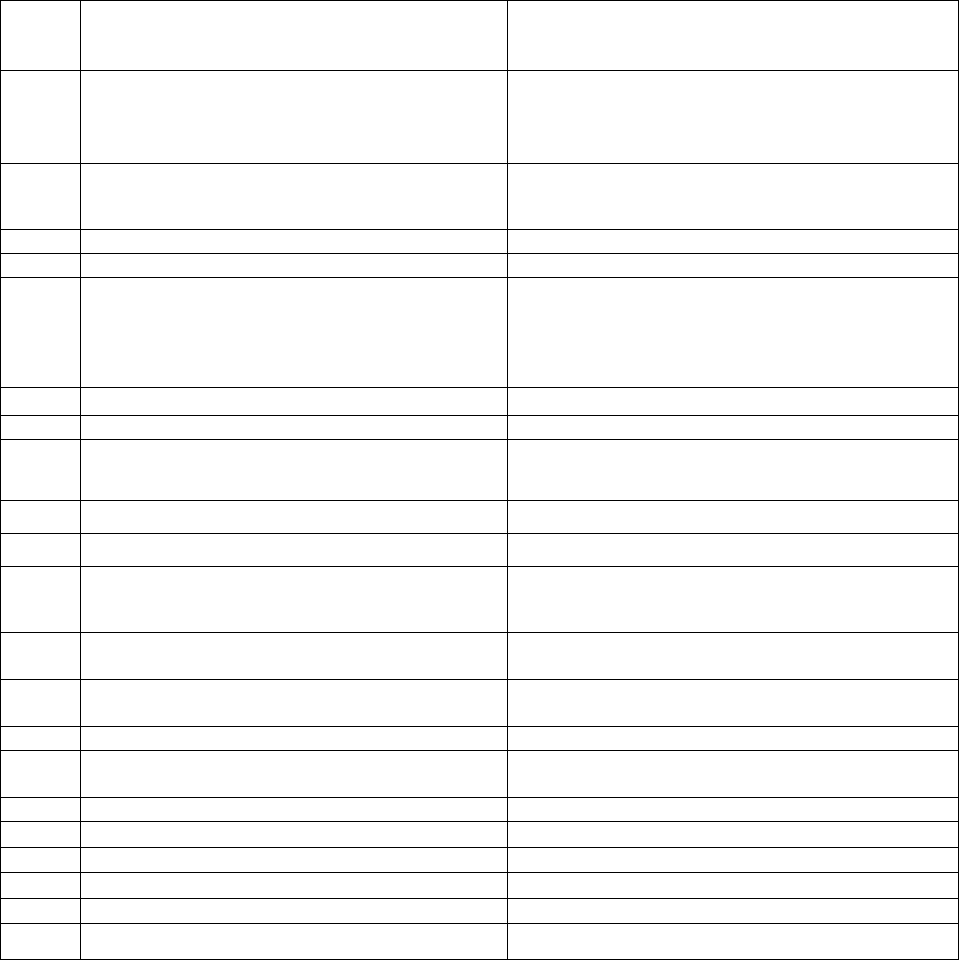
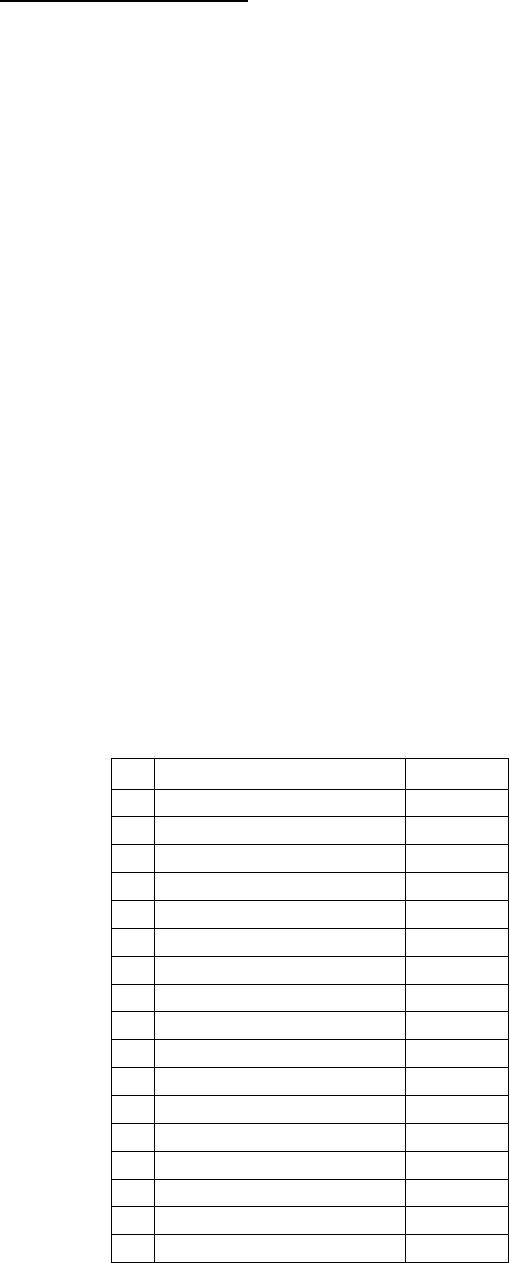
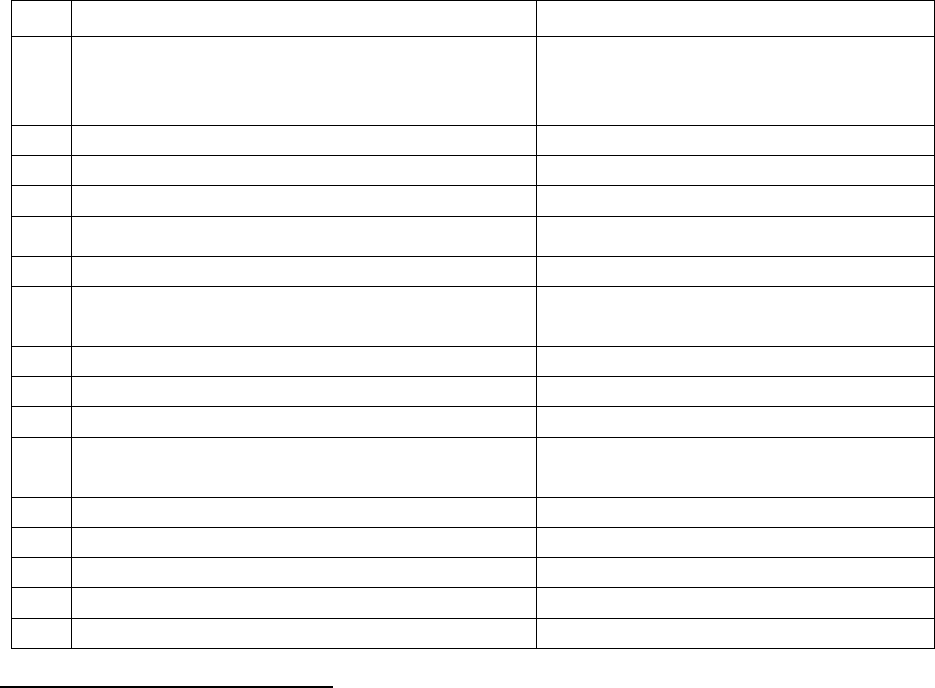
20. Brief Facts of the Case:
1.
Name & Address of the Complainant
MR. G. Virabadran
2/606, Nakeeran Street, Mogappair East,
Chennai 600 037
2.
Policy No.
Type of Policy
Duration of Policy/Policy Period
Floater Sum Insured (SI)
251100502010000403
Tailor made Group Mediclaim policy
01/11/2020 to 31/10/2021
3.
Name of the Insured &
Name of the Policyholder/Proposer
Mr. G. Virabadran
4.
Name of the Insurer
M/s. National Insurance Company Ltd
5.
Date of Short Settlement
July 2021
6.
Reason for Short Settlement
on various heads
7.
Date of receipt of the Complaint
15/12/2021
8.
Nature of Complaint
Short settlement
9.
Date of receipt of Consent (Annexure VI A)
06/01/2022
10.
Amount of Claim
Rs. 2,19,830/-
11.
Amount paid by Insurer, if any
Rs. 1,57,966/-
12.
Amount of Monetary Loss (as per Annexure
VI A)
Rs. 60,000/-
13.
Amount of Relief sought (as per Annexure VI
A)
Rs. 60,000/-
14.a.
Date of request for Self -Contained Note
(SCN)
23/12/2021
14.b.
Date of receipt of SCN
Received by mail on 08/04/2022
15.
Complaint registered under
Rule 13(1)(b) of the Insurance Ombudsman
Rules, 2017
16.
Date of Hearing/Place
VC HEARING ON 13/04/2022
17.
Representation at the Hearing
a) For the Complainant
Mr. G Virabadran
b) For the Insurer
Mr. Ranjan Bhatiya
18.
Complaint how disposed
By award
19.
Date of Award/Order
29/04/2022
Complainant Mr. G Virabadran is a member of Tailormade Group Mediclaim policy
issued by M/s. National Insurance Company Limited Covering Retirees of Bank of Baroda
vide policy bearing number 251100502010000403 for a period of one year effective from
01/11/2020 to 31/10/2021. Insured was admitted in Sai Speed Medical Center Pvt
Limited, Chennai on 22/04/2021 for the treatment of Covid 19 and discharged on
29/04/2021. Complainant submitted reimbursement claim for an amount of Rs. 2,19,830/-
for the expenses incurred for the treatment during the hospitalization. M/s. Medi Assist
TPA processed and approved the claim for an amount of Rs. 1,57,966/- and disallowed
Rs. 60,000/- under the head consultation / visit. Complainant not agreeing with the
settlement made by the Insurer approached the Forum seeking intervention for the
settlement of the balance claim amount.
21(a) Complainant’s submission:
Complainant Mr. G. Virabadran in his complaint stated that he was affected by Covid
19 in the month of April 2021 and was admitted in Sai Speed Medical Center on
22/04/2021 and discharged on 29/04/2021. Complainant further stated that he had
submitted reimbursement claim for an amount of Rs. 2,19,830/- and got settlement for
Rs. 1,57,966/- only. The processing TPA M/s. Medi Assist informed that Rs. 10,000/- per
day is the maximum allowed under the head consultation /visit, hence Rs. 60,000/- was
dis allowed. The settlement was not acceptable to the Complainant and mentioned that
as per policy terms he is entitled to claim the full amount. Aggrieved on the deduction
amount Complainant approached the Forum seeking balance un settled claim amount.
21(b) Insurer’s submission:
As per SCN of RI Company which states that Insured Mr. Virabadran was admitted in
Sai Speed Medical Center on 22
nd
April 2021 and discharged on 29
th
April 2021 for the
treatment of Covid 19 and submitted reimbursement claim for Rs. 2,19,830/-. The claim
was settled for Rs. 1,57,966/- Company processed the claim as per GIC metro charges
accordingly deducted Rs. 61,864/- which is in order.
22) Reason for Registration of Complaint: - Rule 13(1)(b) of the Insurance
Ombudsman Rules, 2017, which deals with “any partial or total repudiation of claims by
the life insurer, General insurer or the health insurer in the regulations, framed under the
Insurance Regulatory and Development Authority of India Act, 1999”
23) Results of hearing of both the parties (Observations and Conclusion):
# The complaint was heard through Video Conference on 13/04/2022 with the consent
of both the parties. The complainant and the Insurer were present for the hearing.
# During the hearing Complainant stated that the deductions made by the Insurer is not
correct and as per terms and conditions of the policy he is entitled to get more.
# During the hearing Insurer reiterated that the claim was processed as per terms and
conditions of the policy. Insured was hospitalized for 8 days and as per the bills submitted
Rs. 17,500/- per day was charged by the hospital which consisting room rent Rs. 5,000/-
, Duty Medical Officer Rs. 4,000/-, Nursing charges Rs. 3,500/- consultant pulmonary
specialist Charges Rs.3,000/- Oxygen consumption charges Rs,2,500/-, safety and
hygiene charges Rs. 1,500/-laundry Rs. 1,000/- Oxygen consumption charges
Rs.2,500/-. Company has considered Rs. 10,000/- per day against Rs. 17,500/-
# After hearing both sides and also going through the documents placed the Forum is
of the opinion that the disallowance of Rs. 2,500/- per day billed by the hospital towards
the Oxygen charges is not correct and directs the Insurer to pay Rs. 2,500/- * 8 days =
Rs. 20,000/- along with the interest.
23) Documents placed before the Forum for perusal:
✓ Written Complaint to the Ombudsman dated 15/12/2021
✓ Complainant’s representation to the insurer b mail dated 29/07/2021
✓ Insurer’s response to the Complainant – no response
✓ Consent (Annexure VI A) submitted by the Complainant – 06/01/2022
✓ Policy copy, terms and conditions
✓ Self-Contained Note of Insurer dated – not submitted
✓ Discharge Summary of Speed Hospitals.
24) .
25. The attention of the Insurer is hereby invited to the following provisions of the
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the
insurer shall comply with the award within thirty days of the receipt of the
award and intimate compliance of the same to the Ombudsman
b) According to Rule 17(7) of the Insurance Ombudsman Rules, 2017, the
complainant shall be entitled to such interest at a rate per annum as specified
in the regulations, framed under the Insurance Regulatory and Development
Authority of India Act, 1999, from the date the claim ought to have been settled
under the regulations, till the date of payment of the amount awarded by the
Ombudsman.
c) According to Rule 17(8) of the Insurance Ombudsman Rules, 2017, the award
of Insurance Ombudsman shall be binding on the insurers.
Dated at Chennai on this 29
th
day of April 2022.
Sd/-
(Segar Sampathkumar)
INSURANCE OMBUDSMAN
FOR THE STATE OF TAMIL NADU AND PUDUCHERRY
AWARD
Taking into account the facts & circumstances of the case and the submissions
made by both the parties during the course of hearing, the Forum hereby
directs the Insurer to pay Rs. 20,000/- in addition to the already settled amount
as per terms and conditions of the Policy along with interest at applicable rates
as provided under Rule 17(7) of the Insurance Ombudsman Rules, 2017.
Thus, the complaint is PARTLY ALLOWED.
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF TAMIL NADU & PUDUCHERRY
(UNDER RULE NO: 16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Segar Sampathkumar
CASE OF Mr. S. Sankaranarayanan Vs HDFC ERGO Genl. Insurance Co. Limited
COMPLAINT REF: NO: CHN-H-018-2122-1065
Award No: IO/CHN/A/HI/0002/2022-2023
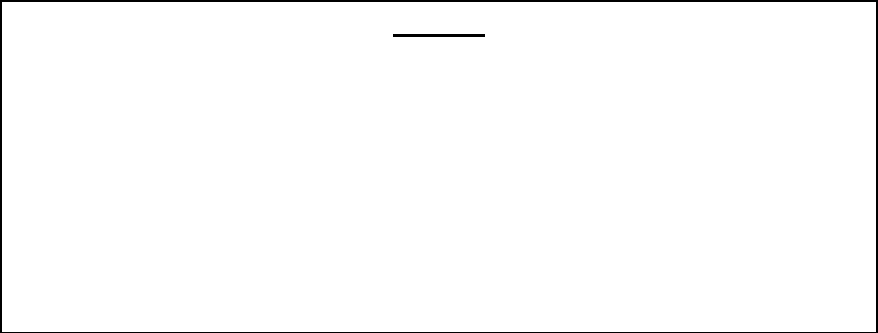
1.
Name & Address of the Complainant
Mr. S. Sankaranarayanan,
2/235-2, Poongavanam Street,
Gomathipuram, MADURAI - 625020
2.
Policy No.
Type of Policy
Duration of Policy/Policy Period
Sum Insured (SI)
2812203779411500001
Easy Health Group Insurance
31/07/2020 to 31/07/2021
Rs.5,00,000/-
3.
Name of the Insured
Name of the Policyholder/Proposer
Mr. Sankaranarayanan.S & Mrs.S. Saradha
Mr. Sankaranarayanan.S
4.
Name of the Insurer
HDFC Ergo General Insurance Co. Ltd.,
5.
Date of Repudiation / Short Settlement
Short settlement of claim – Diet Expenses &
Infection control charges
6.
Reason for repudiation/ Short settlement
Settled as per Terms and conditions of the Policy
7.
Date of receipt of the Complaint
23/11/2021
8.
Nature of Complaint
Short settlement of Covid Claim-Diet Expenses &
Infection control charges
9.
Date of receipt of Consent (Annexure VI
A)
7/4/2022
10.
Amount of Claim
₹ 450943/- (Mr. Sankaranarayana & Mrs. S.
Saradha)
11.
Amount paid by Insurer, if any
₹ 410466/-
12.
Amount of Monetary Loss (as per
Annexure VI A)
₹ 35000/- (Rs.17,500/- each)
(13.
Amount of Relief sought (as per Annexure
VI A)
₹ 35000/-
14. a.
Date of request for Self Contained Note
(SCN)
20/1/22
14. b.
Date of receipt of SCN
5/4/22
15.
Complaint registered under
Rule No. 13(1) b of the Insurance Ombudsman
Rules, 2017
16.
Date of Hearing/Place
By Video Conferencing (VC) on 12/4/22
17.
Representation at the hearing
a) For the Complainant
Mr. S. Sankaranarayanan
b) For the Insurer
Mr. Aneesh Bhaskaran/Mr. S. Desai
18.
Disposal of Complaint
By Award
19.
Date of Award/Order
13/4/2022
20. Brief Facts of the Case:
The complainant states that he and his wife were hospitalised for Covid 19 in April 2021.
He submitted the claims to the insurer and the insurer also settled partially without
considering the dietary expenses of Rs.10,500/- each and infection control charges of
Rs.7,000/- each totalling to Rs.35,000/- was not considered for settlement.
The insurer has replied that they relooked into the claims of the above claimant and both
are fall under non-payable items and thus not-admissible.
21 (a) Complainant’s Submission:
The complainant states that the insurer has not settled the Dietary expenses and infection
control charges of himself and his spouse who were hospitalised in April 21 which
amounts to Rs.35,000/-. Hence he approached the Forum for its intervention and advise
the insurer to settle this amount.
21 (b) Insurer’s Submission: The Insurer in their Self Contained Note has stated that
they have deducted the following heads only from their Claim.
a) MRD Charges (b) Dietary Charges (c) Infection Control Charges (d) Pharmacy Bills
(Bills not legible). In the instant case they relooked into the claim and found that the food
charges and Infection Control charges respectively fall under non-payable items and thus
not admissible.
2. Reason for Registration of Complaint:- Rule No.13(1) (b) of the Insurance
Ombudsman Rules, 2017, which reads as “Any partial or total repudiation of claims by
the Life Insurer, General Insurer or the Health Insurer”.
23. Documents placed before the Forum for perusal.
✓ Complaint letter dated 23/11/21 to the Insurance Ombudsman
✓ Consent (Annexure VI A) submitted by the Complainant dt.7/4/22
✓ Policy copy, terms and conditions
✓ Self Contained Note of the Insurer
24. Result of hearing with both parties (Observations & Conclusion)
➢ The Complainant and the insurer’s representative participated in the hearing and
consented for Video Conferencing.
➢ The Complainant has stated that he and his wife’s covid claim, the insurer has not
settled the dietary expenses of Rs.10,500/- each and Rs.7,000/- towards infection
control charges charged by the hospital amounting to Rs.35,000/- totally for both.
➢ The insurer has informed the Forum that they agree to settle the dietary expenses
incurred during hospitalisation of covid in respect of the complainant and his wife
for Rs.10,500/- each and Rs.7,000/- towards infection control charges does not fall
under their Policy condition.
➢ The Forum has appreciated the spontaneous act of the insurer and advised them
to settle the dietary expenses of both for Rs.10,500/- each and asked the
complainant to furnish necessary details to the insurer to make the payment.
AWARD
The insurer is directed to settle the diet expenses of Rs.10,500/- charged by the
hospital to the Complainant and his wife.
Thus the Complaint is Partly Allowed.
The attention of the Insurer is hereby invited to the following provisions of the Insurance
Ombudsman Rules, 2017:
a) According to Rule 17(6) of the Insurance Ombudsman Rules, 2017, the insurer
shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
b) According to Rule 17(7) of the Insurance Ombudsman Rules, 2017, the
complainant shall be entitled to such interest at a rate per annum as specified in
the regulations, framed under the Insurance Regulatory and Development Authority
of India Act, 1999, from the date the claim ought to have been settled under the
regulations, till the date of payment of the amount awarded by the Ombudsman. –
NOT APPLICABLE.
c) According to Rule 17(8) of the Insurance Ombudsman Rules, 2017, the award of
Insurance Ombudsman shall be binding on the insurers.
Dated at Chennai on this 13
th
day of April 2022.
Sd/-
(Segar Sampathkumar)
INSURANCE OMBUDSMAN
FOR THE STATE OF TAMIL NADU AND PUDUCHERRY
Proceedings of
THE INSURANCE OMBUDSMAN
KERALA, LAKSHADWEEP & MAHE
[Under Rule No.13 1(b) Read with Rule 14 of the Insurance Ombudsman Rules, 2017]
Present: Mr Girish Radhakrishnan
Insurance Ombudsman
Complaint No. KOC-H-048-2122-0797
Complainant : Mr. Babu P
Respondent Insurer : National Insurance Company Ltd.
AWARD
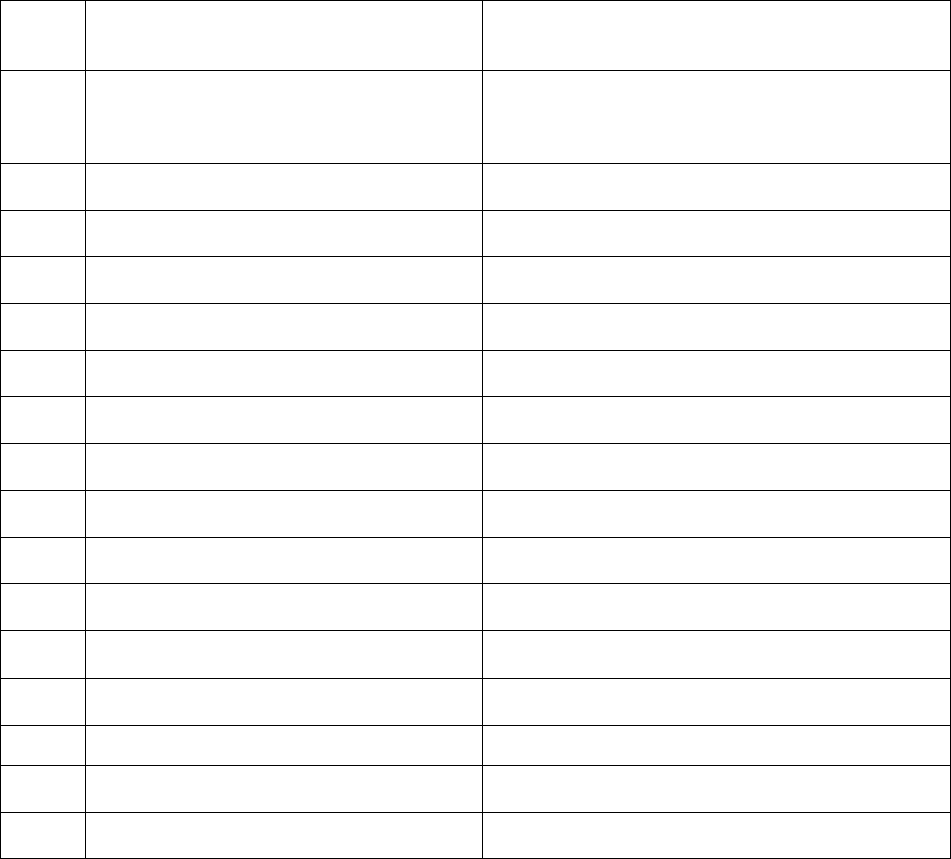
1.
Address of the Complainant
:
Alakapuri,Pudukudi Road,Manjeri (PO),
Malappuram Dist; 676121KERALA
2.
Policy Number
:
251100502010000359
3.
Name of the Insured
:
Mr. Babu p
4.
Type of Policy
:
HEALTH
5.
Date of receipt of Complaint
:
09.09.2021
6.
Nature of complaint
:
Rejection of claim
7.
Date of Hearing
:
16/03/2022
8.
Present at the Hearing for Complainant
:
Mr. Babu P
9.
Present at the Hearing for the Insurer
:
Mr. Atul Malhotra
Award No. IO/KOC/A/HI/0001/2022-23
This is a complaint filed under Rule 13(1)b read with Rule 14 of the Insurance Ombudsman Rules,
2017. The complaint alleges rejection of a claim under a Health Insurance policy issued by the
Respondent Insurer (RI). The Complainant, Mr. Babu P is the policyholder.
1. Complainants’ Averments
The averments, contentions and submissions in the complaint are summarized as follows:
(1) The complaint is related to rejection of reimbursement of treatment expenses of the
Complainanat’s wife who is a cancer patient underwent medical treatment with Regional
Cancer Centre(RCC) Trivandrum, a Government Organisation.
(2) The claim submitted is in connection with the medical expenses incurred for
Immunotherapy – Monoclonal Antibody given as injection to his wife Smt.K Shyamala
who is a cancer patient.
(3) She is suffering from right breast cancer for the last 2 years. RCC prescribed a treatment
cycle consisting of Chemotherapy, Surgery, Radiation and 17 immunisation course of a
combination of Transtusumab and Pertusumab injections at an interval of 21 days.
Chemotherapy was completed on 01/04/2020. Surgery was conducted on 19/05/2020
with removal of right breast.
(4) He is a retiree of The Federal Bank Ltd with employee No.2582 and holding the Group
Mediclaim Health Insurance policy under which the medical treatment expenses incurred
for his wife is reimbursable.
(5) The medical expenses claim amount Is INR 1,24,494/- incurred between 30/11/2020 to
25/02/2021.
(6) They were submitting bills at regular intervals to their previous Insurer United India
Insurance through their TPA, which were reimbursed in due course.
(7) Then the Insurance Company was changed w.e.f 01/11/2020 to National Insurance
Company. Hence they have submitted the bills after the above cut-off date to the TPA of
National Insurance for reimbursement of the medical expenses incurred.

(8) The RI rejected their claim under clause number 2.19 of the policy by informing that the
day care treatment expenses are not covered.
(9) The treatment was a series consisting of Chemotherapy, Surgery, Radiation and
immunotherapy of Monoclonal Antibody injection with Modern Treatment
method/Advanced Technology. The entire course of treatment was prescribed by RCC,
the leading organization for cancer treatment and it is a Government organization.
2. Respondent Insurer’s Contentions
The Respondent Insurer entered appearance and filed a Self Contained Note (SCN). The
averments, contentions and submissions in the SCN are summarized as under:-
(1) The Respondent Insurer had received the reimbursement request of Rs.1,24,494/- from
the above patient towards expenses incurred for administration of Monoclonal antibody
on standalone basis and accordingly the claim was reported vide CCN HH172126981.
(2) On reviewing the claim documents, they found that the treatment documents submitted
by the insured shows that the patient was admitted for Monoclonal antibody of
standalone basis, which found not covered under the scope of IBA policy. This procedure
does not require hospitalization and usually done in OPD. Hence the claim is not
admissible as per policy terms and hence recommended for repudiation under the Clause
2.19 of IBA GMC policy.
(3) The procedures undergone by the insured does not require hospitalization and usually
done in OPD. So the claim is not admissible as per policy terms & conditions and hence
denied under Clause 2.19 of IBA GMC policy.
3. I heard the Complainant and the Respondent Insurer at a Hearing on 16/03/2022
The Complainant reiterated that his wife is a cancer patient, undergone treatment at RCC,
Trivandrum, a Government organization. He is a retired bank employee of Federal Bank Ltd.
He and his wife are insured under the Group Mediclaim – Tailormade policy issued by the RI
for Federal Bank retirees. The claim submitted for the medical expenses incurred for

immunotherapy – Monoclonal Antibody given as injection to his wife, comes to Rs.1,24,494/-
was rejected by the RI. The reason for rejection as stated by the RI is “the procedure does
not require hospitalization and usually done in OPD; hence the claim is rejected under the
Clause No.2.19 of IBA GMT policy.”
His wife’s illness being Breast Cancer comes under Critical Medical Care hospitalization and
related medical treatment undertaken as advised by Regional Cancer Centre. The
reimbursement claims submitted during the previous policy period in connection with the
treatment of Cancer consisting of Chemotherapy, Surgery, Radiation and immunization
courses submitted to the previous Insurers United India Insurance Company at regular
intervals were reimbursed in due course. He has faced this difficulty only with the present
RI.
The Respondent Insurer stated that the procedure done is administration of Monoclonal
antibody on standalone basis, which does not require hospitalization and usually done in
OPD. Hence the claim is non-admissible as per terms and conditions of the IBA GMC policy.
So the claim recommended for repudiation under the Clause 2.19 which reads as:-
2.19 HOSPITALISATION
Means admission in a Hospital/Nursing Home for a minimum period of 24 in-
patient care consecutive ‘in-patient care’ hours except for the specified day
care procedure/treatments, were such admission could be for a period of less
than 24 consecutive hours. For the list of these specified day care
procedures/treatments, please see 3.3.
Note: Procedures/treatments usually done in outpatient department are not
payable under the policy even if admitted/converted as an in-patient in the
hospital for more than 24 hours.
The list of procedures allowable is expressly mentioned in the list. Immunotherapy is not
mentioned in the day care procedures list, although Chemotherapy is included in the list.
4. Having heard both the sides and having perused all the documents submitted in detail, I find
as under:-
(1) The Complainant insured submitted that his wife (the insured person here) is a Cancer
patient and she underwent chemotherapy and surgery as per the doctor’s advice. Her
illness being Breast Cancer comes under Critical Medical Care Hospitalisation and related
medical treatment undertaken as advised by Regional Cancer Centre. The RCC, I may
mention here, is one of the most renowned cancer treatment centres in the country.
(2) A total claim amount of Rs.1,24,494/- incurred by the Complainant from 30/11/2020 to
25/02/2021 for injections given at the RCC to his wife, have been repudiated by the RI
and this is the basis of the dispute herein.
(3) For fighting this insured person’s cancer, the Regional Cancer Centre had evidently
prescribed a treatment cycle consisting of Chemotherapy followed by Surgery, Radiation
and then concluding with a 17-set immunization course of a combination of two drugs,
namely Transtusumab and Pertusumab injections at an interval of 21 days.
Chemotherapy was completed on 01/04/2020, Surgery was conducted on 19/05/2020
with removal of right breast. She was discharged on 20/05/2020. After healing wound 8
Radiations were given from 29/06/2020 to 17/07/2020. Pertusumab injections continued
and the treatment was ended on 24/02/2021.
(4) In support of his contention of the particular expense falling within the ambit of
theinsurance cover, the Complainant points out that the similar medical expenses bills
upto 31/10/2020 (the previous policy end date) were submitted to the previous Insurers
M/s United India Insurance, and were being reimbursed without any objection. The
Complainant would also cite that under Clause number 6.15 IRDA Regulations of the IBA
GMT policy which reads as :-
This policy is subject to Provisions of Insurance Act, 1938, IRDAI (health
insurance) Regulations 2016 and IRDA (protection of policyholder’s interest)
Regulations 2017 as amended from time to time.
(5) In defence, the RI submits that the process involved in this insured person’s case is not
hospitalization as per Clause 2.19 read with Clause 3.3 of the policy for criteria
“hospitalization”. Further they would have it that the procedure is not one that is listed

as allowed Day-Care procedures covered under the policy but is merely something that
could be done in OPD and hence outside the scope of the coverage.
(6) In assessing whether the particular procedure claim for by the Complainant would fall
within the policy coverage, I am guided principally by two factors:
(a)
Firstly, the policy itself indicates that coverage for this procedure claimed for, does
exist in it – as I shall explain below:
(i)
I note that Clauses 3.5 and 3.8 of the policy lay down criteria for “Pre-existing
Diseases/Ailments” and “Advanced Medical Treatment” respectively without any
ambiguity. Pre-existing Diseases/Ailments – Pre-existing diseases are covered
under this insurance scheme from day one. Advanced Medical Treatment – New
advanced medical procedures approved by the appropriate authority eg.Laser
surgery, stem cell therapy for treatment of a disease is payable on
hospitalization/day care surgery. Pertuzumab (Perjeta
®
) and trastuzumab are
known to be specifically only used to treat breast cancers that have too much of
a protein (receptor) called HER2 on the surface of their cells. This is called HER2-
positive breast cancer. It is therefore to be considered essential, approved and
bonafide treatment designed as part of the management of the insured person’s
ailment as I have explained in (3) above.
(ii)
As regards whether this is a mere process of giving an injection to the patient and
can be done in OPD as the RI would have it, I find from easily available literature
that the administration of these strong medicines into the body (and that too of
an otherwise ill person) has a risk of triggering cardiac problems and is hence
given only under specific supervision of her treating doctor who monitors her for
a certain period even after the administration of the drugs.
(iii)
I must therefore conclude that there is ample ground to conclude that the drug
therapy described here as monoclonal antibody administration is a continuing
part of the treatment process for the insurped person’s ailment and must
therefore be part of the policy coverage that includes new advanced medical
procedures as shown above.
(b)
Secondly, the IRDAI itself has mandated inclusion of such a process in their Circular
IRDA/HLT/REG/CIR/177/09/2019 dated 27/09/2019. I draw attention of the RI to
Chapter V of the Circular which reads as under:
1. To ensure that the policyholders are not denied availability of
health insurance coverage to Modern Treatment Methods
Insurers shall ensure that the following treatment procedures shall
not be excluded in the health insurance policy contracts. These
Procedures shall be covered (whichever medically indicated) either
as in-patient or as part of domiciliary hospitalization or as day care
treatment in a hospital.
A. Uterine Artery Embolisation and HIFU
B. Balloon Sinuplasty
C. Deep Brain stimulation
D. Oral chemotherapy
E. Immunotherapy – Monoclonal Antibody to be given as
injection
F. Intra vitreal injections
I believe nothing further needs to be said about the Regulatory mandate on this
subject.
(7) Considering all facts and circumstances of the case, I am of the opinion that the insurance
policy issued by the RI does respond positively to the Complainant’s claim under
discussion here. As to the quantum of claim, I do not find any part of the claimed amount
of Rs. 1,24,494 to be superfluous or indicating deduction or adjustment. I consider on
balance, that the decision to reject the claim was taken by the RI in bonafide manner and
intent and no ususual latches are found in their claim processing, in consideration of
which I do not think allowing of any interest or other compensation is indicated. Found
accordingly.
5. Award
In the result, I hereby order as under:
The Respondent Insurer shall reopen their file on the Complainant’s claim discussed herein
allow the amount of Rs. 1,24,494.00 as a valid claim under the insurance policy no.
251100502010000359 and pay the said amount to the Complainant. No interest or cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 11
th
day of April 2022
Sd/-
Girish Radhakrishnan
INSURANCE OMBUDSMAN
Proceedings of
THE INSURANCE OMBUDSMAN
KERALA, LAKSHADWEEP & MAHE
[Under Rule No.13 1(b) Read with Rule 14 of the Insurance Ombudsman Rules, 2017]
Present: Mr Girish Radhakrishnan
Insurance Ombudsman
Complaint No. KOC-H-050-2122-0833
Complainant : Mr. Lijoy T Varghese
Respondent Insurer : The Oriental Insurance Company Ltd.
AWARD
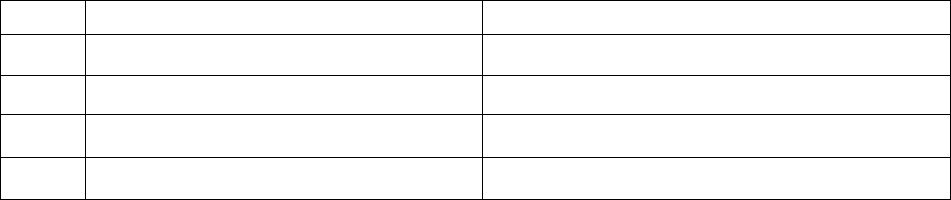
1.
Address of the Complainant
:
Thazhathumuriyil House, SNRA 39 Marana
Road, North P.O. Thripunithura 682036
2.
Policy Number
:
124500/48/2021/7909
3.
Name of the Insured
:
Mr. Lijoy T Varghese
4.
Type of Policy
:
HEALTH
5.
Date of receipt of Complaint
:
29.10.2021
6.
Nature of complaint
:
Rejection of Health Insurance claim
7.
Date of Hearing
:
25.03.2022
8.
Present at the Hearing for Complainant
:
Mr. Lijoy T Varghese
9.
Present at the Hearing for the Insurer
:
Mr.Saurab
Award No. IO/KOC/A/HI/0003/2022-23
This is a complaint filed under Rule 13 (1)b read with Rule 14 of the Insurance Ombudsman Rules,
2017. The complaint is regarding alleged rejection of a claim under a Health Insurance policy
issued by the Respondent Insurer (RI). The Complainant, Mr. Lijoy T Varghese is the policyholder.
1. Complainant’s Averments
The averments, contentions and submissions in the complaint are summarized as follows:
(1) A claim was registered by the complainant during the last week of January 2021.
(2) The TPA Medi Assist was asking for the indoor case sheets from the Hospital. The hospital
provided a letter asking an authorized person to visit and check the indoor case sheets as
their policy doesn`t allow to hand over the indoor papers out side. The TPA did not visit
the hospital for checking the indoor case sheets.
(3) The complainant submitted all medical records with the TPA. His claim was rejected
stating that `no active line of treatment given for hospitalization and the treatment can
be done on OPD basis`.
2. Respondent Insurer’s Averments
The RI entered appearance and filed a Self Contained Note (SCN). The averments, contentions
and submissions in the SCN are summarized as follows:
(1) The Complainant was covered under a GMC (Axis Bank Ltd.) policy
no.124500/48/2021/7909, for the period 1.10.20 to 30.9.2021, for a SI of Rs.4lacs.
(2) Smt. Saritha Krishna Menon (spouse of the Complainant) was admitted in Lakshmi
Ayurvedic Hospital, Ernakulam, on 6.1.2021, with diagnosis Adhosakthi Shool with
complaints of pain in both lower limbs and headache and was discharged on 20.1.2021,
The Insured claimed Rs.35,413/-.
(3) During hospitalization, the patient was treated with ayuevedic procedures – patrapottala
swedam, kadikizhi, shirodhara and internal medicine. Hospitalisation is not justified for
the above procedures as the same can be done on OPD basis.
(4) The claim was denied as per clauses- i).4.22– Any stay in the hospital for any domestic
reason or where no active regular treatment is given by the specialist. ii).2.3-
Hospitalisation period.
3. I heard the Complainant and the Respondent Insurer at a Hearing on 25.03.2022.

The Complainant stated that he insurance claim for the Ayurveda treatment taken by the
Complainant`s spouse was rejected stating that the treatment which she had taken viz.
patrapottala swedam, kadikizhi, shirodhara and internal medicines could have been taken on
OPD basis and thus hospitalistion was not justified. She was admitted in the Lakshmi
Ayurvedic Hospital, with complaints of pain in both lower limbs and headache; the quantum
of settlement sought is Rs.35,413/-. The insurance company’s TPA also delayed the matter
unduly by first saying that they would visit the hospital and verify the records, but did not do
so even after the Complainant produced a letter from the hospital containing their consent.
Then the Complainant himself submitted all the required papers to get a decision and that
decision was a negative one.
The Respondent Insurer stated that the patient underwent treatment under ayurvedic
procedures like patrapottala swedam, kadikizhi, shirodhara and internal medicines, which
their TPA advised them, did not require Hospitalisation since the same can be done on OPD
basis. The claim was denied as per clauses - i).4.22– Any stay in the hospital for any domestic
reason or where no active regular treatment is given by the specialist. ii).2.3- Hospitalisation
period.
4. Having heard both the sides and having perused all the documents submitted in detail, I find
as under:-
(1) The Complainant had a valid policy as on date of the event giving rise to the claim
occurred. He preferred a claim for a set of ayurvedic procedures done on his wife which
has been rejected by the RI and the same forms the basis of this dispute. The RI would
have it that the Ayurvedic procedures the Complainant was subjected to could well have
been done on OPD basis and did not need any hospitalization and they have invoked
Clause (i) 4 22 and (ii) 2. 3 of the policy to justify their decision.
(2) The insured patient, according to the hospital discharge papers, was presented to the
hospital with pain on both lower limbs and headache. This was diagnosed at the hospital
as Adhosakthi Soola (pain on both lower limbs) and she was hospitalised from 06.1.2021
to 20.1.2021 and she underwent the following treatments : patra potala swedam,
kadikizhi, and shirodhara and was given other internal medicines. That the insured
person was treated for a specific diagnosed medical condition/ailment and not for a
general convalescence/rejuvenation process is borne out from the record and is a fact
uncontested by the RI.
(3) Publicly available and accessible literature tell us that patra potala swedam is known in
Malayalam as elakkizhi and kadikkizhi is known in Sanskrit as pinda swedam and both
these involve a long and elaborate process of applying appropriate heated poultices to
the body kept in different poses. Shirodhara is a process of slow dripping of heated
medicinal oils on the forehead and scalp of a prone patient. Each of these processes takes
at least an hour and must be done for the number of days as decided by the doctor but
in any case for a minimum of 7 days for it to have any efficacy at all. These are invariably
accompanied by strictly prescribed diet based on the particular ailment and condition of
the patient and may often involve other requirements like avoiding exertions, avoiding
day-time naps etc.
(4) While in theory, these treatments may be administered without an IP admission, hospitals
ask patients to go through the treatment as inpatients for proper supervision by doctor
and staff. Also, and equally importantly, it behoves a reasonable person to consider the
sheer impracticality and the humanly impossible task of maintaining an OP visit schedule
(from both patient and hospital sides) for a period of 14 continuous days and that too
involving particular specifications about diet, rest, sleep etc. simply to avoid
inconveniencing the insurer by way of a claim. I have therefore no hesitation in noting
here that the RI (via their TPA) have taken a stand that can only be characterized as hyper-
technical to the exclusion of any semblance of reasonableness.
(5) It therefore follows that the decision of the RI to treat the Ayurvedic procedures
undergone by the Complainant’s spouse as ineligible under the policy coverage on
grounds of these purportedly being OP procedures not requiring IP admission in the
hospital is deeply flawed and untenable. The policy must respond positively to the
Complainant’s claim. Found accordingly.
5. Award
In the result, I hereby order as under:
The Respondent Insurer shall reopen the Complainant’s claim file and pay him the admissible
claim amount as per the policy terms, conditions and limits/caps specified. No interest or cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply with
the award within 30 days of receipt of the award and intimate compliance of the same to the
Ombudsman.
Dated this the 11th day of April 2022
Sd/-
Girish Radhakrishnan
INSURANCE OMBUDSMAN
Proceedings of
THE INSURANCE OMBUDSMAN
KERALA, LAKSHADWEEP & MAHE
[Under Rule No.13 1(b) Read with Rule 14 of the Insurance Ombudsman Rules, 2017]
Present: Mr Girish Radhakrishnan
Insurance Ombudsman
Complaint No. KOC-H-005-2122-0866
Complainant : Mr. P A Abraham
Respondent Insurer : Bajaj Allianz General Insurance Co. Ltd.,
AWARD
1.
Address of the Complainant
:
8E Infra Hillock-3 Parijatham Road
Kalamassery Kochi 682033
2.
Policy Number
:
OG 21 1602 6021 00000575
3.
Name of the Insured
:
Mr. P A Abraham
4.
Type of Policy
:
HEALTH
5.
Date of receipt of Complaint
:
08.11.2021
6.
Nature of complaint
:
Rejection of claim
7.
Date of Hearing
:
18.03.2022
8.
Present at the Hearing for Complainant
:
Mr. P A Abraham
9.
Present at the Hearing for the Insurer
:
Ms. Reshma
Award No. IO/KOC/A/HI/0005/2022-23
This is a complaint filed under Rule 13 (1)b read with Rule 14 of the Insurance Ombudsman Rules,
2017. The complaint is regarding alleged rejection of a claim under a Health Insurance policy
issued by the Respondent Insurer. The Complainant, Mr. P A Abraham is the policyholder.
1. Complainant’s Averments
The averments, contentions and submissions in the complaint are summarized as follows:
(1) Complainant’s wife’s claim for Rs.2,97,563/- for an emergency procedure of implanting
pacemaker was totally rejected on technical grounds. Theirs was a 10 years’ continuous
Group policy , first three years for Sum Insured of Rs. 3 lakhs and next seven years for
Sum Insured of Rs.5 lakhs , with United India Insurance, till it was ported to this Insurer
on 25th January, 2021 due to their original Syndicate Bank getting merged with Canara
Bank.
(2) The new bank processed their portal request and passed it to the new Insurer, who took
15 days to enquire and process and issue ported policy starting on 25/1/2021 by
mentioning United India old policy no. and with remark of portability provisions and
acceptance.
(3) His wife used to consult and undergone tests in nearby MAJ Hospital but due to
emergency, she was admitted in Lisie Hospital due to low heartbeat and exhaustion, on
28/6/2021. A pacemaker was implanted and she was discharged on 1/7/2021.
(4) The Insurer interpreted the medical condition narrated by the patient at the time of
admission which was noted in the Discharge summary, that she had 4 months medication
in about May 2018 for HTN and Dyslipidemia and had 22 years old condition of Rheumatic
fever and so, were existing while porting the policy with them on 25/1/2021.
(5) However, she was not having any medical condition or medication in Jan, 2021 or prior to
implantation of pacemaker and the Doctor’s Certificate states that there is no relation
with her short term BP or Cholesterol.
(6) Contention of the insurer, of a non-existing medical condition at the time of porting under
Portability Clause of IRDA, is not understandable. The Complainant’s several mails were
not responded to. He requests the Ombudsman to negotiate and give him justice and get
him the claim and continue the policy, as they are Senior Citizens and cannot get new
Mediclaim Insurance although paying premium for 10 continuous years, for the sake of
benefit in retired life.
2. Respondent Insurer’s Averments
The Respondent Insurer (RI) entered appearance and filed a Self Contained Note (SCN). The
averments, contentions and submissions in the SCN are summarized as follows:
(1) The Respondent Insurer entered appearance and filed a Self Contained Note (SCN). The
averments and submissions in the SCN are summarized as under:-
(2) The Policy number: OG-21-1602-6021-00000575 Group Mediclaim Insurance - Canara Bank
(Previously Syndicate Bank) for the period of 25-JAN-2021 To 24-JAN-2022 in favour of
the petitioner was issued under certain terms, conditions and limitation thereof.
(3) There is no deficiency of service or unfair trade practice on the part of the RI. Hence the
Complaint is liable to be dismissed at the outset for want of cause of action.
(4) Policy is a contract and both the parties are under obligation to obey/fulfill all the terms
and conditions of the same in the strict sense of the words written therein. As the terms
and conditions of the Policy are sacrosanct, the claim arrived is also processed within the
precincts of the Policy only. 5. The policy issued to the complainant is a Group Mediclaim
policy. The Insured was holding Group Health Mediclaim Insurance Scheme: Syndicate
Bank with United India Insurance Co. Ltd. After the Syndicate Bank was taken over by
Canara Bank during bank merger as per RBI guidelines, Canara Bank had tied up with RI
and hence the continuity of their existing policy was ported with this Respondent by
signing a new proposal form and portability form. RI has issued Policy covering 25-JAN-
2021 To 24-JAN-2022 - Plan Chosen: Group Mediclaim Insurance - Canara Bank
(Previously Syndicate Bank)with special continuity conditions –“ It is hereby agreed and
understood that the Mediclaim Insurance policy is issued with Portability Benefit from
Mediclaim policy of United India Insurance Co. Ltd. and Continuity is extended from 20-
01-2014. The Continuity for 7 years is extended on Sum Insured of Rs. 5 lakhs for P A
ABRAHAM, the Continuity for 7 years is extended on Sum Insured of Rs. 5 lakhs for Rachel
Abraham. All other terms, conditions, coverage and exclusions of the policy remain
unaltered, all waiting Periods apply afresh on Enhanced Sum Insured. Any disease/ injury
contracted during breakin period will not be payable.”
(5) As per proposal form and portability form the complainant/insured have not declared any
of the ailments with regards to Hypertension, Dyslipidemia and Rheumatic fever. Medical
Certificate from Lisie Hospital mentions that Mrs. Rachel Abraham has medical history of
Hypertension for past 10 years and was on medication Amlorpes 5 mg and Roseday 5mg.
The same certificate also mentions that Mrs. Rachel Abraham had Rheumatic fever at the
age of 40 years and took penicillin prophylaxis for 5 years. It is humbly brought to the
notice of this Hon’ble Forum that Amlopres 5 mg medicine is used to treat high blood
pressure/Hypertension and to prevent heart attack and strokes. Tab Roseday 5 mg
medicine is used to lower cholesterol and reduce the risk of heart disease. It is used in the
treatment of high blood cholesterol. Cholesterol is a fatty substance that builds up in
blood vessel and causes narrowing, which may lead to a heart attack or stroke. This
medicine blocks the production of unhealthy fats in the body and prevents the risk of
heart problems and stroke. These medicines are being consumed by Mrs. Rachel Abraham
over the past 10 years which shows that she was having a very high risk of heart related
problems. But yet these facts were not disclosed to this Respondent in the Proposal Form.
Hence it was very much important for this Respondent to have known about the pre-
existing ailments of Mrs. Rachel Abraham at the time of accepting her proposal for
insurance by this Respondent.
(6) Discharge Summary from Lissie Hospital also shows that Mrs. Rachel Abraham was
diagnosed with Dyslipidaemia, which is a medical condition involving abnormally elevated
cholesterol or fats in the blood. It increases the chance of clogged arteries and heart
attacks or other circulatory disorders. This medical condition was also not informed to
this Respondent at the time of availing the policy. The Discharge Summary from Lissie
Hospital mentions that Mrs. Rachel Abraham had risk factors – Systematic Hypertension
and Dyslipidemia. This Respondent was not informed of these preexisting conditions as
well.
(7) Medical document from Lissie Hospital mentions that Mrs. Rachel Abraham had Rheumatic
fever at the age of 40 years and took penicillin prophylaxis for 5 years. Rheumatic fever
causes swelling and muscle damage to the heart. This is an infection which causes heart
valve leaflets to stick together, which narrows the valve opening thus damaging the heart
valve and chronic heart failure. Penicillin is administered for curing this infection. From
the said medical document it is seen that Mrs. Rachel Abraham took penicillin prophylaxis
for 5 years. These are medical conditions which must have been intimated to this
Respondent at the time of availing the policy as they form material facts for this
Respondent.
(8) The above stated medical history of Mrs. Rachel Abraham was very much relevant and
material for the RI for accepting the policy. The claim in respect of which the complaint is
filed before this Hon’ble Forum pertains to expenses incurred in Implant of Pacemaker
due to heart failure. The Discharge Summary shows that there is complete heart block.
Hence there was non-disclosure of material facts at the time of availing the policy.
Insurance is a matter of solicitation. Hence the complainant ought to have disclosed all
pre-existing medical conditions to RI at the time of insurance. The Respondent Insurer
was denied an opportunity to decide the correct terms and conditions or to decide
whether to accept the proposal of the complainant.
(9) Point No. 23 in the Proposal form bears the question whether the persons to be insured
suffer from or is investigated with heart disorder or circulatory system , chest pain, high
blood pressure, diabetics, hepatitis etc. As the above mentioned medical conditions have
been existing since 10 years and since medicines such as Amlopres 5 mg and Roseday 5
mg were being taken by Mrs. Rachel Abraham, these facts must have been mentioned in
answer to the question in point 23 and informed to this Respondent. Instead, the
complainant has stated in answer to point 23 that there is “no” such issues. Hence there
is clear non-disclosure of material facts.
(10) Point No. 24 in the Proposal form bears the question whether the persons to be insured
has any health complaint, taking treatment or medication. The fact that Mrs. Rachel
Abraham had Rheumatic fever and had taken penicillin for 5 years must have been
disclosed at this point. The fact of hypertension and Dyslipidaemia must also have been
disclosed. Instead, the complainant mentioned “not applicable” which amounts to non-
disclosure of material facts.
(11) Point No 25 in the Proposal Form bears the question if any of your immediate family
members have Diabetes, Hypertension etc. To this the complainant has answered that his
brother has diabetics. However, the complainant intentionally remained silent about the
medical condition of his own wife Mrs. Rachel Abraham. This is not bonafide act on the
part of the complainant and was only intended to deceive the Respondents and to avail
health policy by concealing essential facts.
(12 The complainant has also signed a “Declaration” in the proposal Form stating that the
facts disclosed in the proposal form are true and that it shall form the basis of the policy.
When material facts are not disclosed in the proposal form, the policy issued by this
Respondent becomes null and void. The Preamble to the Policy Terms and Conditions
reads as “Our agreement to insure You is based on Your Proposal to Us, which is the basis
of this agreement, and Your payment of the premium. …” Hence when the proposal made
to us is silent on material particulars essential to accepting the proposal, there is no
consensus and there is no contract of insurance. Thus the insurance agreement becomes
void. Clause no 16 under Part B of the policy terms and conditions mentions that the
Policy shall be void and all premiums paid hereon shall be forfeited to the Company, in
the event of misrepresentation, mis-description or non-disclosure of any material fact.
(13) The RI submits that they are not liable to pay any claim arising out of pre-existing illness
as per the policy terms and conditions. Clause C1 of the policy terms and conditions
stipulates: What we will not pay (Exclusions) under this policy? We shall not be liable to
make any payment for any claim directly or indirectly caused by, based on, arising out of
or attributable to any of the following: Benefits will not be available for Any Pre-existing
condition, ailment or injury, until 36 months of continuous coverage have elapsed, after
the date of inception of the first Mediclaim Insurance Policy, provided the pre-existing
disease / ailment / injury is disclosed on the proposal form. The above exclusion 1 shall
cease to apply if You have maintained a Mediclaim Insurance Policy with Us for a
continuous period of a full 36 months without break from the date of Your first Mediclaim
Insurance Policy. In case of enhancement of Sum Insured, this exclusion shall apply afresh
only to the extent of the amount by which the limit of indemnity has been increased (i.e.
enhanced Sum Insured) and if the policy is a renewal of Mediclaim Insurance Policy. The
Complainant was obliged to fill the Proposal Form correctly as per the regulation of IRDAI.
As per Schedule-I relating to Portability of Health Insurance Policies offered by General
Insurers and Health Insurers specified in the IRDAI (Health Insurance) Regulations, 2016,
in every portability case, every insurer is mandated to furnish to an applicant the
Portability Form together with a proposal form., and the policyholder is required to fill
the portability form along with proposal form and submit the same to the insurer. So even
if it is a portability case, it is necessary to disclose any existing ailment in order to give
opportunity to the new insurer to determine the policy terms and conditions w.r.t to that
particular customer because insurance is a matter of solicitation. It was following this
regulation of the IRDAI, this Respondent had sought the complainant to fill the Proposal
Form.
(14) RI had issued the policy believing that the complainant had given true disclosure of the
material facts affecting the contract of insurance. Insurance is a matter of solicitation and
since no existing illness was disclosed RI had issued this policy. If the pre-existing ailments
were disclosed to RI as per the principle of Utmost good faith before portability RI would
not have ported the policy with us or would have ported with certain conditions. Hence
RI repudiated the claim. Continuity benefit is given to only those disease/ailments
diagnosed subsequent to the inception of the policy. In such cases where the insured is
diagnosed of a completely new disease, the waiting period is bypassed. But in this case,
Mrs. Rachel Abraham was having Hypertension for past 10 years and was under
medication for same over these years. She was also having Dyslipidemia and had suffered
from Rheumatic fever for which she was taking Penicillin. All these are ailments seriously
affecting the heart functioning. The present claim is for the expenses incurred in
implanting pacemaker. This procedure had to be done as there was complete heart block
for Mrs. Rachel Abraham. So, the ailment/hospitalization for which the claims were made
is not one diagnosed subsequent to policy inception. It was due to pre-existing health
condition not disclosed in Proposal Form. Hence continuity benefit will not apply to this
claim as the claim has arisen of the non-disclosed condition which was existing prior to
the inception of policy with this Respondent.

(15) Thus, under these facts and circumstances, RI says and submits that the claim under the
policy was rightly denied as per terms and condition of the policy and as per guidelines of
IRDAI and all the contents of complaint are denied by this respondent.
(16) A contract of insurance is one of utmost good faith. A proposer who seeks to obtain a
policy is duty bound to disclose all material facts bearing upon the issue as to whether the
insurer would consider it appropriate to assume the risk which is proposed. It is with this
principle that the proposal form requires specific disclosure of pre-existing ailments so as
to enable the insurer to arrive at a considered decision based on the actuarial risk. The
Hon’ble Supreme Court of India in Reliance Life Insurance Co Ltd & Anr v. Rekhaben
Nareshbhai Rathod Civil Appeal No. 4261/2019 has held that the contention that the
signature of the insured was taken without explaining the details of the terms and
conditions cannot be accepted. The Court relied on the decision of the Division Bench of
the Mysore High Court in V K Srinivasa Setty v. Messers Premier Life and General
Insurance Co Ltd wherein it was held that a person who affixes his signature to a proposal
which contains a statement which is not true, cannot ordinarily escape from the
consequence arising therefrom. This respondent is not guilty of any deficiency in service
as alleged in the complaint.
(17) Therefore, it is humbly prayed that this Hon’ble Ombudsman may be pleased to accept
this self-contained notes and to dismiss the complaint with the cost to RI.
3. I heard the Complainant and the Respondent Insurer at a Hearing on 18.03.2022.
The Complainant stated that pacemaker was implanted for his wife at a cost of Rs.2,97,563/-
but his claim was rejected stating non-disclosure of pre-existing diseases. The policy was a
ported one and his wife had no ailment at the time of porting. The insurer cancelled the policy
without any rule to do so. He requested Ombudsman to get the policy revived and also the
opportunity to get his policy renewed without any gap and at the same premium, without any
increase.
The Respondent Insurer stated that they rejected the claim since it was in its first year of
insurance with RI and it was a case of non-disclosure. However, they have now decided to
revoke the non-disclosure since the Complainant had been insuring for Sum Insured of Rs. 5
lakhs for 7 continuous years before porting. They also agreed to reinstate the policy but at
premium applicable as per underwriting guidelines.
4. Having heard both the sides and having perused all the documents submitted in detail, I find
as under:-
(1) RI has offered to reinstate the policy at the applicable premium based on their
underwriting guidelines and also settle the claim for Rs.2,83,195 out of total claim for
Rs.2,97,563, making deductions of Rs. 14,368 for certain items.
(2) However, in the light of IRDAI Master Circular on Health Insurance dated 22nd July 2020,
in which, inter alia, several heads of expenses commonly disallowed by Insurers have
been identified and Insurers have been asked to consider these when computing claim
amounts, I find that several items that have been deducted/disallowed by the RI need to
be reviewed and allowed. The following are the heads of expenses that have been
wrongly deducted and need to be allowed:
Head of Expense
Amt(Rs)
1
Monitoring
940
2
Admission
260
3
Clinical Support
75
4
Gauze
70
5
Sheet
84
6
Alcohol Swab
4
7
Mask
72
8
I D Tag
28
9
Spirit
44
10
Gown
578
11
BMW
100
12
Hand rub
140
13
Tissue Paper
60
14
Preparation
225
15
Dressing
330
16
Cotton Bandage
30
17
Betadine
84
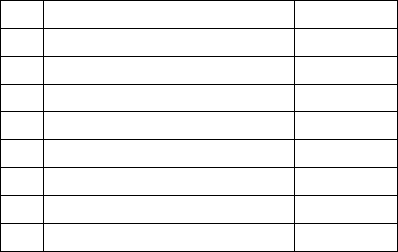
18
Pulse Oximeter charges
360
19
PPE Kit
1,750
20
Blade
404
21
Scrub Solution
161
22
Cotton
15
23
Apron
233
24
Surgiraze
28
25
Energy, Water
900
6975
Hence the correct claim amount due to the Complainant works out to Rs.2,90,170. Found
accordingly.
5. Award
In the result, I hereby order as under
The Respondent Insurer is directed to pay to the Complainant, an amount of Rs.2,90,170.00
in full and final settlement of his claim under policy number OG-21-1602-6021-00000575. No
interest or cost.
The Respondent Insurer is also directed to reinstate the cancelled policy of the Complainant
with the same coverages and limits and other continuity benefits, charging the appropriate
premium as per their underwriting guidelines so as to ensure that the Complainant and his
spouse continue to have unbroken insurance coverage.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 11
th
day of April, 2022.
Sd/-
Girish Radhakrishnan
INSURANCE OMBUDSMAN
Proceedings of
THE INSURANCE OMBUDSMAN
KERALA, LAKSHADWEEP & MAHE
[Under Rule No.13 1(b) Read with Rule 14 of the Insurance Ombudsman Rules, 2017]
Present: Mr Girish Radhakrishnan
Insurance Ombudsman
Complaint No. KOC-H-055-2122-0901
Complainant : Mr. Sreekumaran Nair
Respondent Insurer : Aditya Birla Health Insurance Company Limited
AWARD
1.
Address of the Complainant
:
Sreeji Bhavan Kuttara Mulliliavinmoodu
Aruvikkara 695564
2.
Policy Number
:
GHI-HB-21-2015172-V2
3.
Name of the Insured
:
Mr. Sreekumaran Nair
4.
Type of Policy
:
HEALTH
5.
Date of receipt of Complaint
:
18.11.2021
6.
Nature of complaint
:
Rejection of claim (Covid)
7.
Date of Hearing
:
18.03.2022
8.
Present at the Hearing for Complainant
:
Mr. Sreejith S S (son)
9.
Present at the Hearing for the Insurer
:
Dr. Pranita Godbole
Award No. IO/KOC/A/HI/0013/2022-23
This is a complaint filed under Rule 13 (1)b read with Rule 14 of the Insurance Ombudsman Rules,
2017. The complaint is regarding an alleged rejection of a claim under a Health Insurance policy
issued by the Respondent Insurer (RI). The Complainant, Mr. Sreekumaran Nair is the
policyholder.
1. Complainant’s Averments
The averments, contentions and submissions in the complaint are summarized as follows:
(1) Complainant’s previous Insurer Bajaj Allianz ported his health insurance to Aditya Birla.
Bajaj Finance had informed him that he would have the same insurance cover upon
porting, according to which he is entitled to have cover for Pulmonary Embolism and deep
Vein Thrombosis.
(2) On 21/10/2021, his wife was diagnosed with Covid 19 Pneumonia and was admitted in
SUT Hospital and discharged on 30/10/2021. He incurred Rs.96,141/- His claim was
however denied, on 12/11/2021, due to his non-disclosure of his wife’s Deep Vein
Thrombosis for which she has been under treatment since 2019.
(3) On 12/11/2021, Bajaj Finance enquired about his wife’s medical history. He informed
them that she was diagnosed with Deep Vein Thrombosis in 2019 and that Bajaj Allianz
had settled claim on May 30
th
, 2019.
(4) Since both Bajaj Finance and Bajaj Allianz were aware of his wife’s condition, and they had
informed him that Aditya Birla would be notified, it is sad that they denied the claim for
Covid 19. He requests the ombudsman to help him with his grievance.
2. Respondent Insurer’s Averments
The RI entered appearance and filed a Self Contained Note (SCN). The averments, contentions
and submissions in the SCN are summarized as follows:
(1) Mr. Sreekumaran Nair referred herein as the Proposer approached RI for a policy via Bajaj
Finance Limited under the group policy no. GHI-TB-OL-21-IN5944144 for a Health
Insurance Cover under RI’s “Group Activ Health Policy”.
(2) RI has issued a welcome letter and certificate of insurance dated 15.11.2021 for the period
covering 15.11.2021 till 14.11.2022. The Policy was issued covering the Insured’s Mr.
Sreekumaran Nair and Mrs. Shobhana Kumari.
(3) The proposer Mr. Sreekumaran Nair has filed for cashless request of Rs. 75,000/- vide Pre-
authorization form for the treatment of Insured Shobhana Kumari. The insured was
hospitalized on 21.10.2021 with an expected hospitalization for 7 days at SUT Hospital,
Pattom. The patient was admitted with provisional diagnosis of COVID Infection Cat B – D
Dimers High.
(4) The case was investigated during the cashless process, and it came to notice from the
Cashless form duly filled and submitted by the Claimant that the Insured has a history of
Pulmonary Embolism with Deep Vein Thrombosis (DVT) in the year 2019 which has not
been disclosed while taking the insurance policy. It is important to note that the history
Pulmonary Embolism is an important fact which is relevant for underwriting of the risk as
it may affect the decision of the underwriter based on the underwriting principles and
claimant has precluded RI from adjudicating the proposal in a fair manner by failing to
disclose the same in the proposal form submitted for availing the policy. Further, RI would
also like to apprise the forum that the patients with Pulmonary Embolism tend to report
shortness of breath or impairment or difficulty in functioning of the lungs even after the
treatment of the same.
Pulmonary embolism is a blockage in one of the pulmonary arteries in lungs. In most cases,
pulmonary embolism is caused by blood clots that travel to the lungs from deep veins in
the legs or, rarely, from veins in other parts of the body (deep vein thrombosis)
(5) Thus, the claim was declined stating the reason “On scrutiny of the documents it is
observed that patient is suffering from Pulmonary Embolism with Deep Vein Thrombosis

since 2019 which was not disclosed at the time of inception of the Policy. Hence, this claim
stands denied for Non- disclosure of material facts and hence, we are unable to approve
the claim. ”
(6) The claim is declined in accordance with the terms and conditions of the policy. The clause
reads as under:
Disclosure of Information Norm: means the Policy shall be void and all
premium paid hereon shall be forfeited to the Company, in the event of
fraud, misrepresentation, mis-description or non- disclosure of any material
fact.
(7) Without prejudice to the submissions as made in supra para it is submitted that the
Complainant never filled a reimbursement claim and has directly approached
Ombudsman Forum. Thus, it is important to note that RI has discharged their duty strictly
in accordance with the IRDAI guidelines and hence cannot be compelled to pay something
which is inadmissible.
(8) Insurance policy is given on utmost good faith. Decline of claim is based on the product
structure and the guiding claims and medical principles.
(9) In the view of the above, RI requests the Hon’ble Ombudsman to kindly dismiss the
complaint.
3. I heard the Complainant and the Respondent Insurer at a Hearing on 18.03.2022.
The Complainant’s son reiterated the statements in the written complaint and further stated
that his mother was hospitalized for Covid pneumonia but the claim was denied stating non-
disclosure of Pulmonary Embolism. The policy was ported from Bajaj Allianz with whom the
insurance cover was from 2018 to 2020. During this period a hospitalization claim of his
mother for Pulmonary embolism was paid by Bajaj Allianz. Bajaj Finance had ported the policy
to Aditya Birla Health Insurance Co. Ltd.

The Respondent Insurer stated that the Complainant had sought Cashless facility for
hospitalization of his wife and the same was denied due to Non-disclosure of her pre- existing
disease of pulmonary embolism, at the time of porting the policy. There was no information
received regarding pre-existing disease, from previous insurer during porting.
4. At the Hearing, the RI was asked to submit to this office, a copy of the full wording of the
policy and audio file/transcript of telecall with Complainant, proposal form and policy porting
form to enable a clearer understanding of the matter. The RI reverted on 6
th
April 2022
informing the office of their readiness to settle the claim per terms and conditions of the
policy.
While this is a welcome development, RI’s attention is also drawn to the requirements of the
IRDAI Master Circular on Health Insurance Ref: IRDAI/HLT/REG/CIR/193/07/2020 dated 22
July 2020 including specifically, Lists II, III and IV under its Annxure I.
5. Award
In the result, this Award is passed, directing the Respondent Insurer to process the
Complainant’s claim as per terms and conditions of the policy in question and keeping in mind
IRDAI Master Circular on Health Insurance dated 22 July 2020 and pay him the due claim
amount thereof. No interest or cost.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 11
th
day of April, 2022.
Sd/-
Girish Radhakrishnan
INSURANCE OMBUDSMAN
Proceedings of
THE INSURANCE OMBUDSMAN
KERALA, LAKSHADWEEP & MAHE
[Under Rule No.13 1(b) Read with Rule 14 of the Insurance Ombudsman Rules, 2017]
Present: Mr Girish Radhakrishnan
Insurance Ombudsman
Complaint No. KOC-H-035-2122-0850
Complainant : Ms. Jaya Chacko Cheriyan
Respondent Insurer : Reliance General Insurance Company Ltd.
AWARD
1.
Address of the Complainant
:
T C 19/940 Pearl Gardens Thamalam
Poojappura 695012
2.
Policy Number
:
220392128451000043
3.
Name of the Insured
:
Ms. Jaya Chacko Cheriyan
4.
Type of Policy
:
HEALTH
5.
Date of receipt of complaint
:
02.11.2021
6.
Nature of complaint
:
Rejection of Claim
7.
Date of Hearing
:
24/03/2022
8.
Present at the Hearing for the Complainant
:
Ms. Jaya Chacko Cheriyan
9.
Present at the Hearing for the Insurer
:
Mr. Sujith Krishna,
Dr.Santhosh Kumar
Award No. IO/KOC/A/HI/0016/2022-23
This is a complaint filed under Rule 13 (1)b read with Rule 14 of the Insurance Ombudsman Rules,
2017. The complaint alleges rejection of a claim under a Health Insurance policy issued by the
Respondent Insurer (RI). The Complainant, Ms. Jaya Chacko Cheriyan is the policyholder.
1. Complainants’ Averments
The averments, contentions and submissions in the complaint are summarized as follows:
(1) The Complainant, one of the Directors of Saj Flight Services (P) Ltd is having current
account with Bank of India, Palayam Branch, Trivandrum.
(2) BOI offers to all its customers, insurance coverage under BOI Swasthya Bima Scheme from
2017 onwards. The Complainant and her family were covered under the scheme till date.
(3) On 3rd April 2019, the insurance coverage for BOI customers was taken over by the
Respondent Insurer, Reliance General Insurance Company (RI).
(4) The RI has issued the health insurance policy for the year 2021-22. Till date the she have
not availed any claim from the RI.
(5) During September 2021, the doctor advised her to conduct Cataract operation for her
right eye and she was admitted in Chaithanya Eye Hospital & Research Institute,
Trivandrum.
(6) The operation was planned to conduct on 5th October 2021, so the insurance help desk
of the hospital submitted cashless claim form on 1st of October 2021.
(7) Without any investigation, the RI rejected her claim stating that “As per received claim
documents, patient had past history of DM since 18 years and has undergone Angioplasty
3 years back and the same was not disclosed in the proposal form during the inception of
policy with Reliance General Insurance (RI) dated 11/04/2019, hence the claim is
repudiated under Clause 6.1-Disclosure of information norm.”
2. Respondent Insurer’s Contentions
The RI entered appearance and filed a Self Contained Note (SCN). The averments, contentions
and submissions in the SCN are summarized as under:-
(1) The Complainant Insured applied and purchased RGI-BOI Swasthya Product Insurance
Policy after understanding the policy features, benefits, terms and conditions and
exclusions.
(2) RI have informed the Complainant regarding the necessary documents required for
processing the claim and have requested for the Discharge Summary, Final Bills, all
breakups and paid receipts, cancelled cheque/pass book copy of insured and copy of PAN
Card etc.
(3) RI contacted the Complainant on multiple occasions, for which the Complainant was
hesitant to provide the necessary documents. The RI had requested over phone as well
as through mail for the necessary documents for processing the claim on multiple
occasions but the same has not been submitted even now by the Complainant.
(4) RI is still willing to settle the claim of the Complainant herein as per the terms and
conditions mentioned in the policy by paying the admissible amount. But the same is not
possible to be processed without the required documents.
(5) The Hon’ble forum may graciously direct the Complainant to submit the necessary
documents and accept the admissible amount and to settle the matter amicably in the
interest of justice.
3. I heard the Complainant and the Respondent Insurer at a Hearing on 24/03/2022
The Complainant reiterated her statements in the written complaint and further stated that
she intimated the claim to the RI for pre-authorisation prior to the scheduled date of surgery
(05/10/2021), since for Cataract surgery, pre-authorisation is mandatory as per policy terms.
Continuity benefits allowed in the policy schedule as stated in the policy which reads:
Continuity benefits allowed as per the duration of policy one is holding in earlier/existing
scheme operated by Bank of India and on renewal wishes to renew the policy with us, then
he/she shall be given the benefit of continuity on the expiring policy’s Sum Insured. Hence the
denial of claim by the RI is against the policy conditions. Their allegation about the non-
disclosure of the disease history of the insured is also false as this is a continuity policy.
The Respondent Insurer reiterated their contentions in the SCN and expressed their will to
settle the claim of the Complainant as per the terms and conditions mentioned in the policy
by paying the admissible amount. They asked to produce the necessary documents required
for processing the claim and have requested the submission of the Discharge Summary, Final
Bills, all breakups and paid receipts, cancelled cheque/pass book copy of insured and copy of
PAN Card etc. for an early settlement.
4. Having heard both the sides and having perused all the documents submitted in detail, I find
as under:-
(1) The Complainant and spouse were covered under BOI Swasthya Bima scheme from 2007
onwards. The insurance coverage for BOI Swasthya Bima scheme was taken over by the
RI, Reliance General Insurance Company with continuity benefits.
(2) The date of enrollment to the scheme is clearly mentioned in the policy schedule is 14,
Mar 2014. Continuity benefits allowed in the policy schedule as stated in the policy.
Hence the waiting period for specified diseases and pre-existing illnesses has no relevance
in the scope of the policy issued by the RI.
(3) RI is on record as having expressed their readiness to settle the subject claim of the
Complainant as per the terms and conditions mentioned in the policy by paying the
admissible amount for which they have been requesting the Complainant repeatedly to
submit the relevant documents, viz; Discharge Summary, Final Bills, all breakups and paid
receipts, cancelled cheque/pass book copy of insured and copy of PAN Card etc. for an
early settlement.
(4) I am unable to comprehend why the Complainant is not willing or able to supply the
required documentation to enable settlement of her claim. I find no ground to order any
specific relief except to direct her to provide the required documents to RI who in turn
must process her claim with all due dispatch.
5. Award
In the result, this Award is passed, directing the Complainant to submit the required
documentation to the Respondent Insurer and directing the latter to process the
Complainant’s claim with all due dispatch and pay her the correct and reasonable claim
amount as per terms, conditions, exceptions and limits (caps) specified in the policy.
As prescribed in Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within 30 days of receipt of the award and intimate compliance of the same
to the Ombudsman.
Dated this the 13
th
day of April 2022
Sd/-
Girish Radhakrishnan
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. DATTATRAY S BHOSALE V/S CHOLAMANDALAM MS GEN INS CO LTD
COMPLAINT NO: PUN-H-012-2021-0653
Award No IO/PUN/A/HI/ /2022-23
1.
Name & Address of the Complainant:
Mr. Dattatray S Bhosale ,Pune
2.
Policy No:
Type of Policy:
28XXXX00/00
Group Health Insurance
(Family Floater)
3.
Policy period:
21.07.2020 to 20.07.2021
4.
Sum Insured
500000
5.
Date of inception of first policy:
6.
Name & Age of the Insured and Policyholder:
Mr.Dattatray Bhsoale, 35 yrs
7.
Name of the Insurer:
Cholamandalam MS Gen Ins Co Ltd
8.
Reason for repudiation/Partial Settlement:
Hospitalization period does not
warrant inpatient admission
9.
Date of receipt of the Complaint:
15.02.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Rs.60,822 /-
12.
Insurance Ombudsman Rule (IOR)2017 under
which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
On line hearing on 25.03.2022
14.
Representation at the hearing
c) For the Complainant:
Himself
d) For the insurer:
Mangesh Inamdar, Dr. Minal Vinoth
15.
Complaint how disposed:
Dismissed
Contentions of the Complainant:-
• The complainant had taken Group health insurance (Family floater) with Respondent
Insurer The Cholamandalam MS Gen Ins. Co Ltd for self for SA 5 lakh. He lodged claim of
self-hospitalization in Siddhivinayak Criticare Hospital from 02.09.2020 to 08.09.2020 for
Bilateral Pneumonia with mild ARDS with covid negative. The total expenditure on
hospitalization was Rs.32100/-.
• The RI repudiated the claim stating that the treatment given during the hospitalization
period doesn’t warrant inpatient admission.
• The complainant contends that to secure & balance his family health and financial issues
he had taken insurance but not getting the benefit of it.
• The complainant is requesting forum to look into the matter and resolve the same.
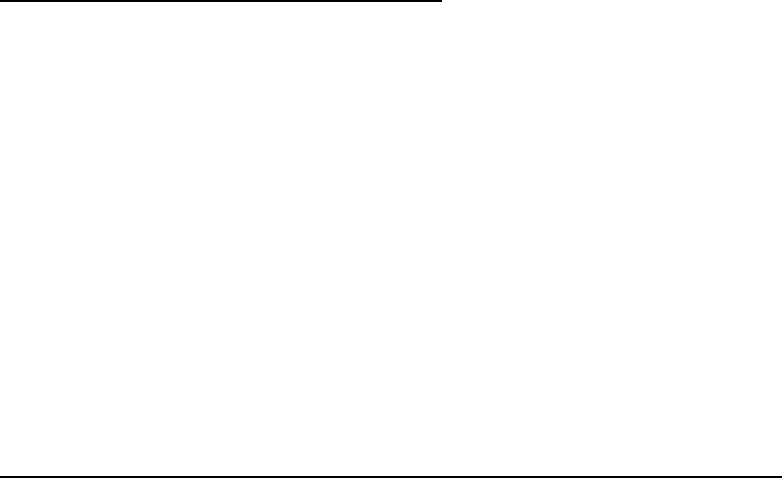
Contentions of the Respondent Insurer (RI):-
The complainant filed the present complaint for the re-imbursement as the (cashless) claim was
repudiated. It is submitted by this opponent that this claim was repudiated on the right ground
as per the policy term and condition. It is submitted that as per the repudiation letter the ground
of repudiation:
On perusal of the claim documents, it is observed that the treatment given during the
hospitalization period doesn’t warrant inpatient admission and can be treated in outpatient
department. No indemnity is available or payable which is outside the scope of policy coverage
part B section 1, which reads as “If the insured is diagnosed with an illness or suffers accidental
bodily injury which necessitates his hospitalization and the insurer will reimburse the insured
persons consequent hospitalization expenses”. In the absence of any illness necessitating the
hospitalization as specified in this coverage, the claim is inadmissible. Enclosed documents
suggest all member vitals are stable and as per MOHFW guidelines member does not require
hospitalization and treatment can be done under home quarantine. Hence claim has been
denied.
Result of personal hearing with both the parties (Observations & Conclusions):
During the on line hearing on 25.03.2022 both the parties reiterated their respective stand.
The RI reiterated that Covid 19 Negative cases with all vitals normal and treated with IV fluids can
be treated on OPD basis.
After hearing contentions of both the parties the forum has following observations/discrepancies
1) Bilateral Pneumonia is shown as diagnosed, as per pathology reports; whereas treating Dr.
Shripad Kere’s certificate dated 04.11.2020 stated as suggestive of pneumonia.
2) Treating Dr. Kere (on 8.06.2020) has stated that the pt was admitted in an emergency,
whereas, any such conditions are not seen from the discharge summary.
3) Test reports are from various places like
i) Chintamani H- Koregaon Mul- dated 29.08.2020
ii) CT scan Jejuri –dated 29.08.2020
iii) Sagar Lab Jejuri dated 29.08.2020-signed by Lab technician only-no sign of MD (Path)
iv) Siddhivinayak –Urli kanchan
v) Meera Diagnostics, Hadapsar-02.09.2020
It is not understood, why a person supposed to be down with sickness with covid symptoms was
travelling from one place to other for tests. These places are not closely situated.
4) Daily nursing & Drug charts seem to have been written in one stroke.
In view of all the above discrepancies, Forum is not of the opinion to consider this case for
payment.Complaint therefore stands dismissed.
Award follows,
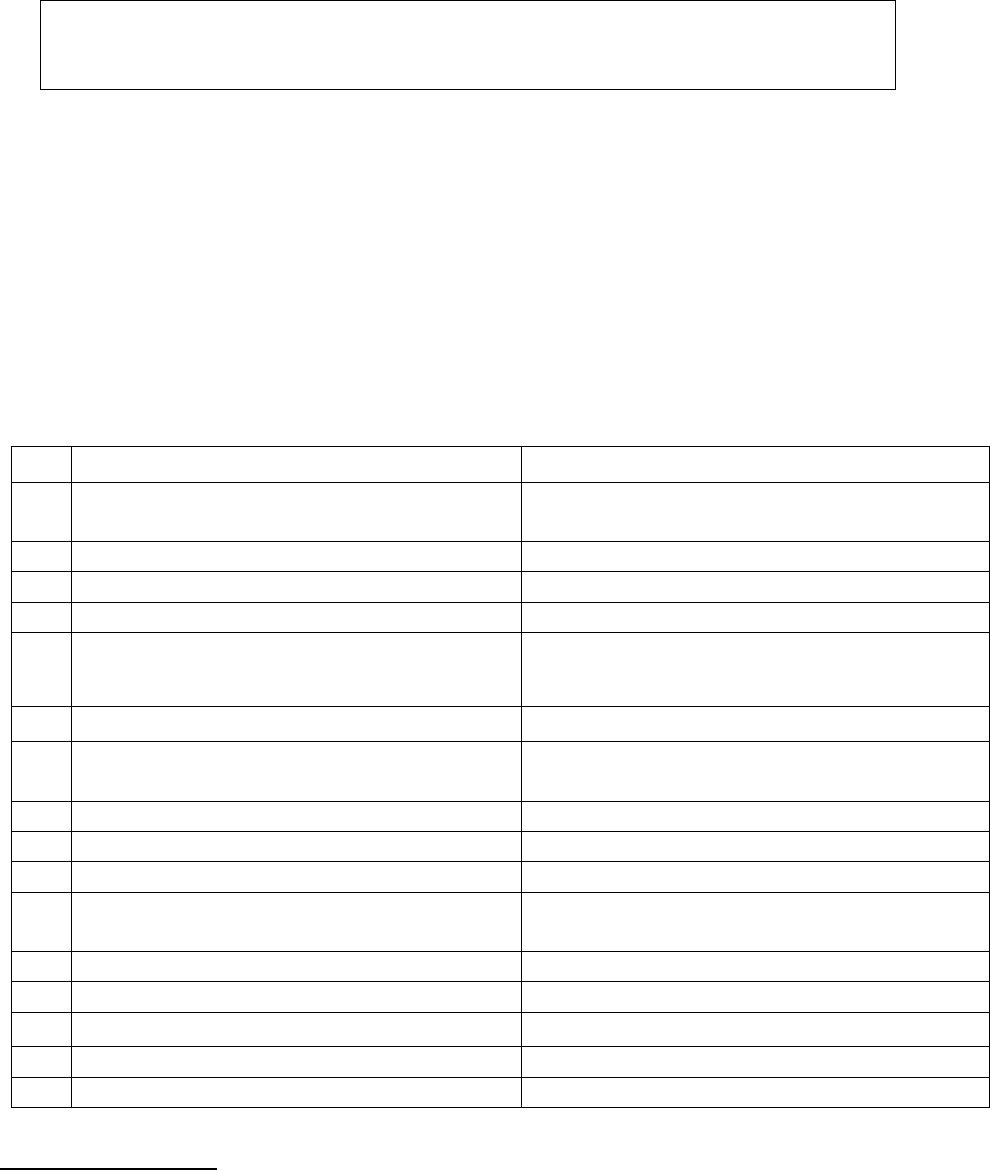
AWARD
Under the facts and circumstances, it is found that the complaint does not hold
merit. Complaint therefore stands dismissed.
Dated: on 29
th
day of April, 2022 at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION16/ 17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Gitesh Dama V/S Bajaj Allianz General Insurance Co. Ltd.
COMPLAINT NO: PUN-H-005-2021-0576
Award No IO/PUN/A/HI/ /2022-23
1.
Name & Address of the Complainant:
Mr. Gitesh Dama, Vashi, Navi Mumbai.
2.
Policy No:
Type of Policy:
OG-XXXX0055
Group Mediclaim (Floater)
3.
Policy period:
18.01.2019 to 17.01.2020
4.
Sum Insured:
Rs. 48,00,000/- (Floater Sum Insured)
5.
Date of inception of first policy:
18.01.2019
6.
Name & Age of the Insured
Policyholder:
Mr. Gitesh Dama, 38 Years.
Dalal Naresh Vasanji (Employer)
7.
Name of the Insurer:
Bajaj Allianz General Insurance Co. Ltd.
8.
Reason for rejection of claim:
Dental Treatment not covered unless due to
accident
9.
Date of receipt of the Complaint:
22.02.2021
10.
Nature of complaint:
Rejection of claim.
11.
Amount of Claim:
Rs. 2,00,00/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 (1)(b)
13.
Date of hearing/Place:
24.03.2022, Online. Pune
14.
Representation at the hearing
e) For the Complainant:
Himself
f) For the insurer:
Mr. Irfan Shaikh; Dr. Yogesh Mandalkar
15.
Complaint how disposed:
Dismissed
Brief Facts of the case:-
The Complainant was covered under the above stated Group Mediclaim (Floater) policy issued
to his employers (policyholder). He was admitted in the hospital from 24.10.2019 to 26.10.2019
for surgery and removal of impacted wisdom teeth as he was suffering from Jaw Disorder called
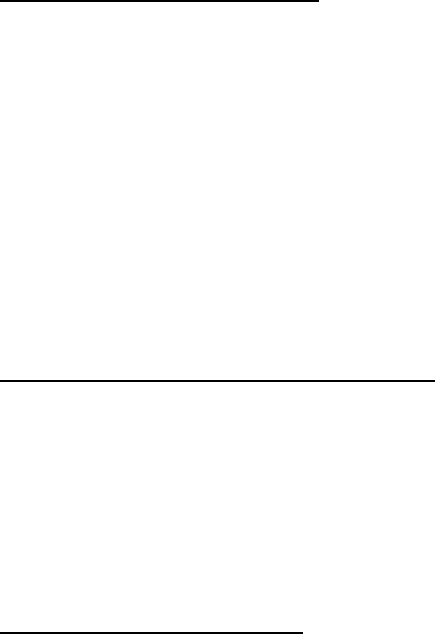
TMJ (Temporomanibular joint). This claim was rejected by the Respondent insurer (hereinafter
called as RI) as the expenses incurred were on dental treatment which is not covered under the
policy. The claim was repudiated as the policy does not extend coverage for any expenses
incurred on dental treatment or surgery of any kind unless arising out of an accident.
Contentions of the Complainant:
The complainant submits that his claim was wrongly repudiated by mis interpreting the surgery
being normal dental surgery. He further submits that he was not able to talk, eat, and open his
mouth due to the extreme pain due to jaw related issues. The Consulting doctors noticed that it
was not a normal teeth problem as he was suffering from TMJ (Temporomanibular joint) as entire
jaw was in pain while biting and not restricted to chewing only.
To rectify the alignment, the treating doctor advised the Complainant for hospitalization. During
hospitalization a surgery was conducted and surgically extracted all the impacted Wisdom teeth.
It was not a normal treatment related to Dental treatment as the gums were OK and without any
infection. The surgery was associated with the temporomanibular joint (TMJ) as pain in jaw point
and in the muscles that control the jaw movement. It was necessary to remove all the wisdom
teeth to improve occlusion and strain of jaw movement.
Contentions of the Respondent Insurer (RI):
The RI contends that on verification of the claim documents they revealed that the claimant
underwent dental surgery for impacted 3
rd
molar. So they informed the Complainant that his
claim stands repudiated as their policy does not extend coverage for any expenses incurred on
dental treatment or surgery of any kind unless arising out of an accident, which is as per Exclusion
No. 7 under the policy:-
Hence the claim was denied.
Observations and conclusions:
The Personal hearing by the way of online Video-conferencing was held on 24.03.2022 and
attended by both the parties. The complainant reiterated that more than dental, it was a jaw
related problem.
In view of the exclusion clause 7 stated below:-
“EXCLUSION-C7-
The Company shall not be liable to make any payment under this Policy in respect of any expenses
whatsoever incurred by any Insured Person in connection with or in respect of: Dental treatment
or surgery of any kind unless as a result of Accidental Bodily Injury to natural teeth and also
requiring hospitalization.
RI’s contention is that, as the surgery is not as a result of Accidental bodily injury it appears that
the claim is out of the purview of this policy.
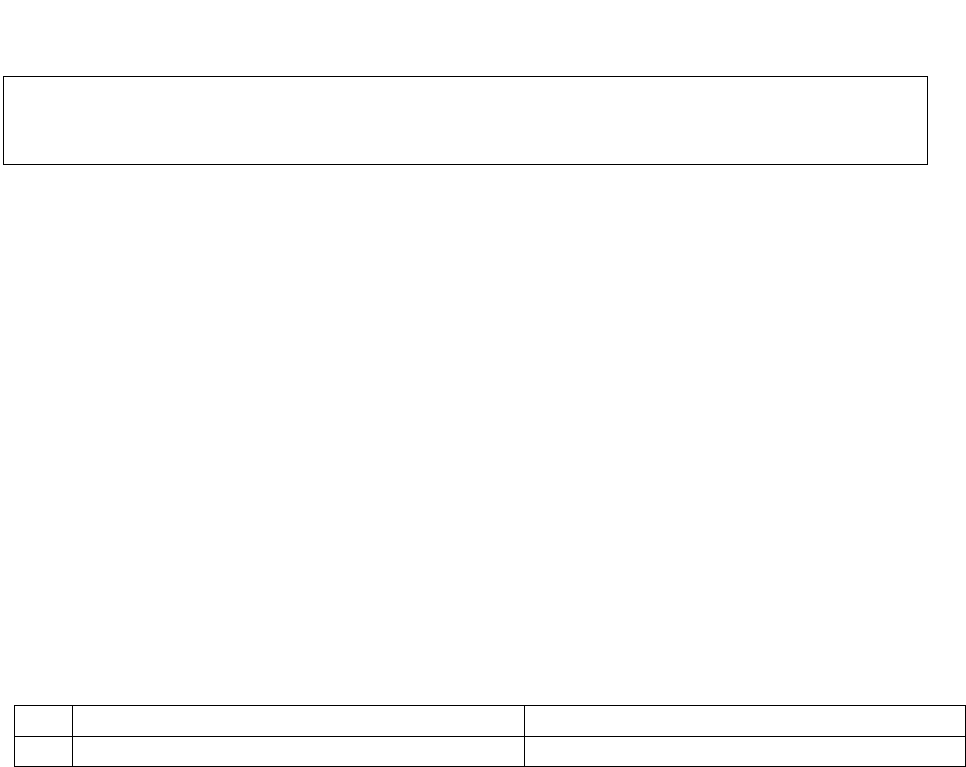
In view of the cross objection of Complainant that it is not a dental problem, but to treat the pain
in his jaw, his wisdom teeth was required to remove, forum has gone through the treating Dr.
Rishi Khosa’s certificate dated 04.09.2020. It is stated therein as: -
This is to inform that Mt, Gitesh Kantilal Dama, 39/M presented to my OPD with pain in both
the Right and Left Temporo Mandibular joint. On examination, he was diagnosed with all four
wisdom teeth impacted.
In another certificate dt. Nil, the same Dr. Rishi Khosa has put a remark ‘TMJ movements are
normal’.
This clarifies that the root cause of jaw pain was due to his impacted wisdom teeth and by its
extraction, he was cured. The entire treatment is given by dentist only. In all these circumstances,
it is purely a dental treatment and it is not due to accident hence, cannot be covered under the
policy clause as stated above.
Complaint is not tenable.
Award follows;
AWARD
Under the fact and circumstances of the case, the complaint is devoid of merits, hence
dismissed.
Dated: at Pune, on 25
th
day of April, 2022.
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF Mr. Iyer Venkataraman V/s. HDFC ERGO General Insurance Co. Ltd
COMPLAINT NO: PUN-H-018-2021-0638
Award No IO/PUN/A/HI/ /2022-23
1.
Name & Address of the Complainant:
Mr. Iyer Venkataraman, Thane
2.
Policy No:
EGXXXX3618
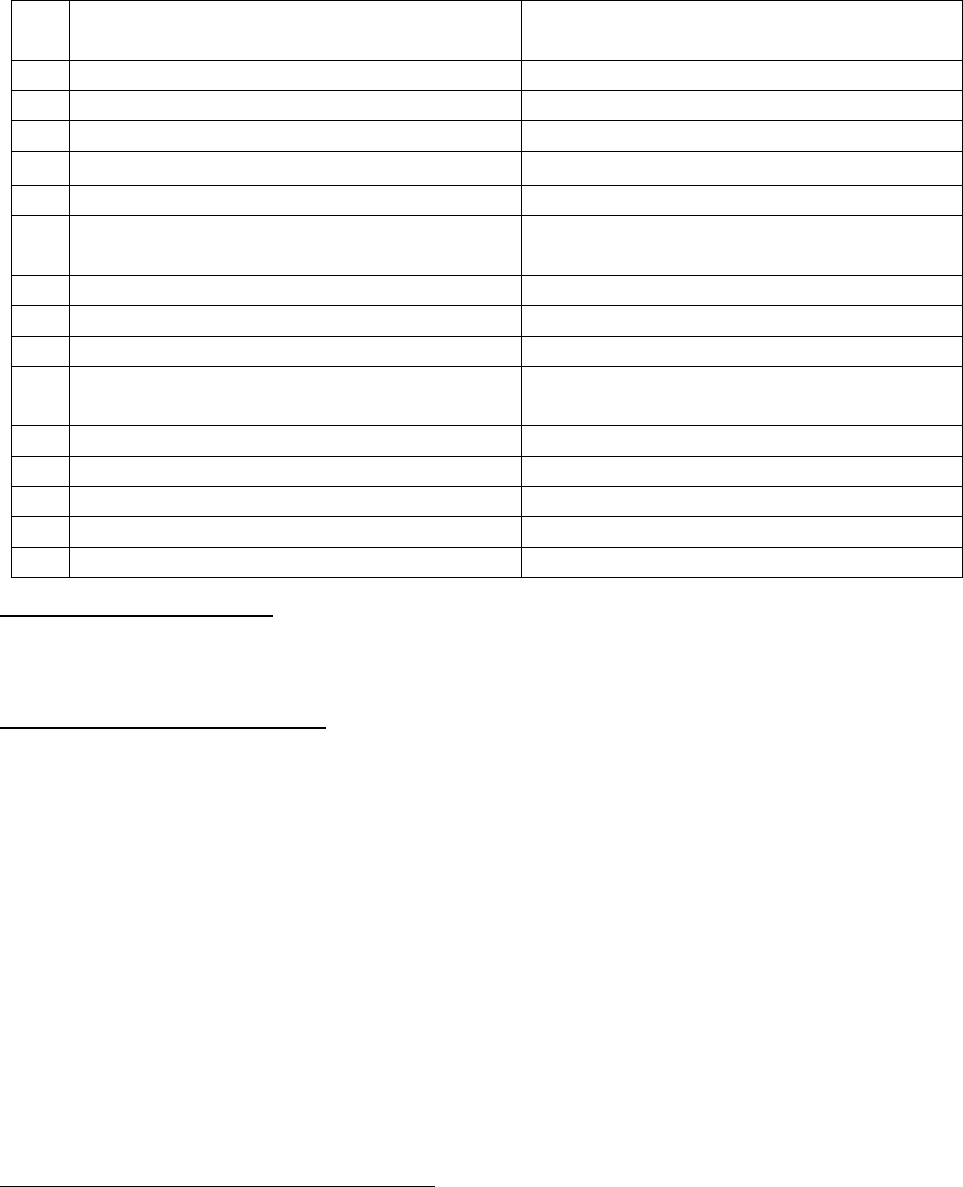
Type of policy:
(120100/12586/2019/A021928/056)
Group Insurance Health plan
3.
Policy period:
09.05.2020 to 08.05.2021
4.
Sum Insured:
Rs. 10,00,000/-
5.
Date of inception of policy:
6.
Name & Age of the Insured:
Mr. Iyer Venkataraman; 58 yrs
7.
Name of the Insurer:
HDFC ERGO General Insurance Co. Ltd
8.
Reason for repudiation/Partial Settlement:
OPD treatment not covered
9.
Date of receipt of the Complaint:
05.03.2021
10.
Nature of complaint:
Settlement of claim amount
11.
Amount of Claim:
Rs. 32,870/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
Online hearing on 25.03.2022
14.
Representation at the hearing
g) For the Complainant:
Himself on voice call
h) For the insurer:
Shrey Baijal
15.
Complaint how disposed:
Dismissed
Brief facts of the Complaint:-
The Complainant is undergoing treatment for tuberculosis. When he visited the Respondent
Insurer (herein after called RI), they refused to accept the claim form.
Contentions of the Complainant: -
The Complainant submits that he is undergoing a treatment for Tuberculosis. When he
approached RI to submit the claim form, it was not accepted by them The Complainant further
submits that earlier he received email from RI that he is eligible for claim. But, now RI is refusing
to accept it. The Complainant in his complaint letter dated 01.03.2021 writes that when the
government is trying to eradicate TB and giving financial support for nutrition, then how the
mediclaim companies have put TB in the exclusion list.
The Complainant contends that the cataract patients are allowed to get discharged with 4 hours.
Further, his TB treating doctor has informed him that there is no need to get hospitalized and
that he can go to office. The treatment has to continue for 9 months.
Initially, RI informed the Complainant over phone that he is not eligible for claim as he has not
completed lock in period. The Complainant replied RI that he is paying the premium since 2017
and since he has completed 3 years lock in period is not applicable for any disease. TB is detected
in December 2020.
Contentions of the Respondent Insurer (RI):-
RI have submitted as under:

1) No exclusion clause applied under the policy for TB.
2) No waiting period for TB under the policy
3) No claim as on date registered for TB by the Complainant.
4) Treatment without hospitalisation and taking only oral medications for TB cannot be
considered admissible under the policy terms and conditions as it constitutes only OPD treatment
and OPD treatment is not admissible under the policy terms and conditions.
5) Hospitalisation of minimum 24 hours is necessary and such hospitalisation should be medically
necessary and treatment taken in the hospital should be justified and necessary to be considered
admissible under the policy terms and conditions.
6) If the treatment could have been taken on OPD basis and only constitutes of oral medications
then such claim even though the patient was admitted in hospital, cannot be considered under
the policy terms and conditions as the hospitalisation is not justified and treatment could have
been done on OPD basis.
7) No bar on the complainant to submit his claim regarding TB, the claim would be decided on
merits based on the policy terms and conditions.
8) 30 day waiting period under the policy for all claims except accident since the start of the first
policy inception period, no specific waiting period for TB under the policy, 36 months waiting
period for all pre-existing disease before the policy inception period which are declared/accepted
at the time of application to get insured under the policy.
Result of personal hearing with both the parties (Observations & Conclusions):
An online hearing was conducted on 25.03.2022. Forum heard both the parties. From the medical
papers submitted by the complainant it is seen that he has been taking medicines for TB since it
was detected. There hasn’t been any hospitalisation or requirement of hospitalisation for the
same. The same has been mentioned in his complaint letter also. The treatment is to continue
for 9 months. The treatment is thus purely of OPD nature.
Forum has perused Terms and conditions of ‘Group Assurance Health Plan’ under which the
complainant insured is covered. As stated therein, the policy covers the medical expenses for; a)
Inpatient treatment, b) day care treatment and c) domiciliary hospitalisation.
As explained by RI, there is no exclusion as such pertaining to TB treatment but the treatment
being taken by the complainant is not falling under any of the above category. Hence, not eligible
for payment.
Award follows,
AWARD
Under the facts and circumstances, the complaint is found devoid of merits. Hence,
dismissed.
Dated: at Pune on 28.04.2022
VINAY SAH
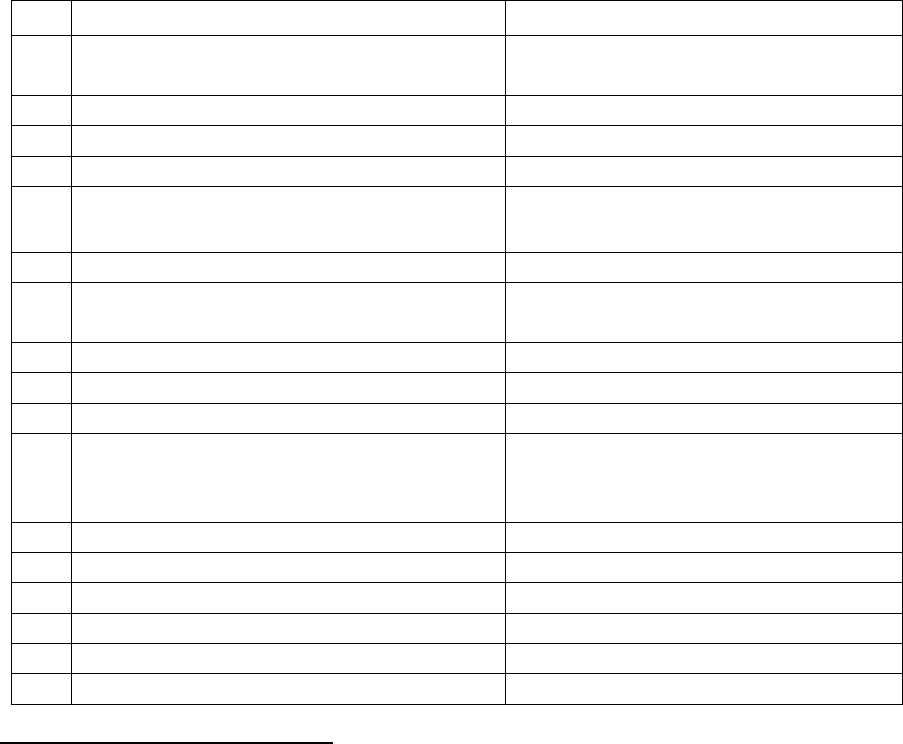
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. PRITHVIRAJ MALI V/S CHOLAMANDALAM MS GEN INS CO LTD
COMPLAINT NO: PUN-H-012-2021-0467
Award No IO/PUN/A/HI/ /2022-23
1.
Name & Address of the Complainant:
Mr. Prithviraj Mali, Pune
2.
Policy No:
Type of Policy:
28XXXX00/00
Group Health Insurance family floater
3.
Policy period:
11.12.2019 to 10.12.2020
4.
Sum Insured
300000
5.
Date of inception of first policy:
11.12.2019
6.
Name & Age of the Insured:
Name of the Policyholder:
Mrs. Indu Maurya Mali, 23 yrs; wife
Mr. Prithviraj Mali
7.
Name of the Insurer:
Cholamandalam MS Gen Ins Co Ltd
8.
Reason for repudiation/Partial
Settlement:
Waiting period for Maternity
9.
Date of receipt of the Complaint:
28.01.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Rs.99456/- (Hosp Bill Rs.47500/-)
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
On line hearing on 16.03.2022
14.
Representation at the hearing
i) For the Complainant:
Absent
j) For the insurer:
Mr. Mangesh Inamdar
15.
Complaint how disposed:
Dismissed
16.
Date of Award
13.04.2022
Contentions of the Complainant:-
The complainant has taken Group Health Insurance with Respondent Insurer (RI) Cholamandalam
MS Gen Ins Co Ltd for Sum Insured 3 lakhs for self and his family. He lodged a claim of his wife’s
hospitalization in Ankur Multispeciality hospital from 25.05.2020 to 28.05.2020 for Tubal ectopic
pregnancy. The total expenditure on hospitalization was Rs.47500/- (total loss to him as per
complaint letter Rs.99456/-)
The complainant contends that the company has wrongly interpreted coverage under the policy
and rejected his wife’s claim for tubal Ectopic pregnancy claim under the normal pregnancy as
per maternity extension of the policy as she was hospitalized within 9 months of the first year
policy. An Ectopic pregnancy cannot proceed normally. The fertilized egg cannot survive and
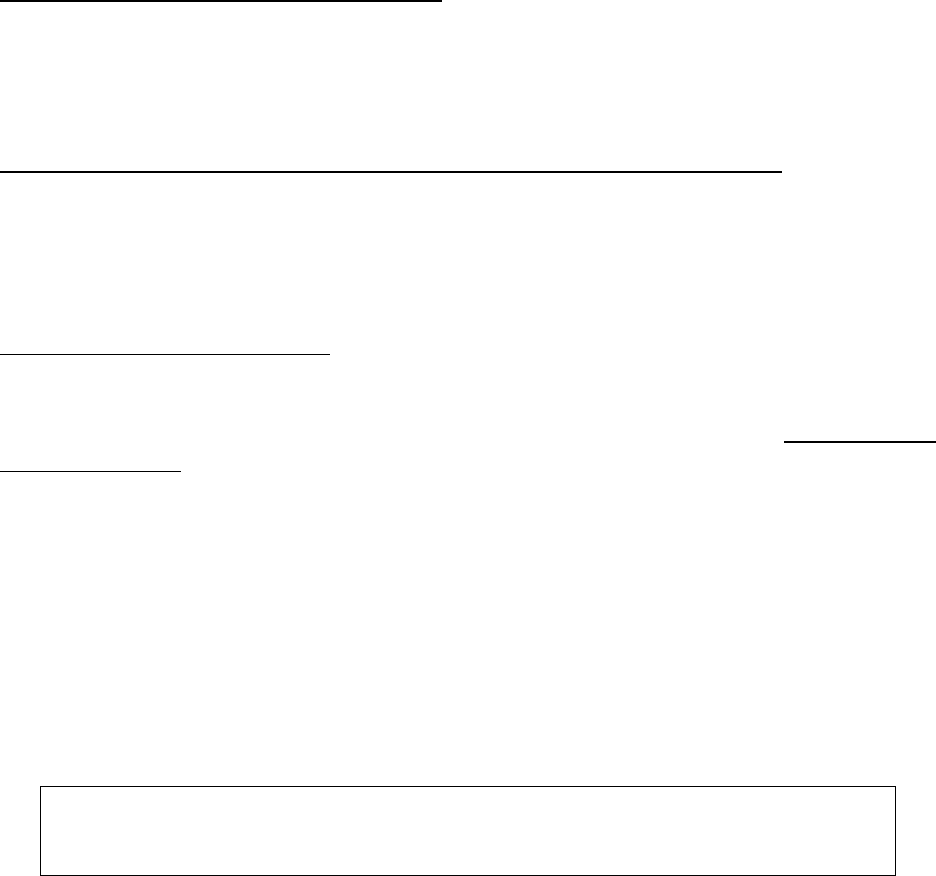
growing tissue may cause life threatening bleeding, if left untreated. His wife was having
emergency symptoms as this caused tube rupture. The complainant contends that
hospitalisation for this life threatening disease falls under the normal policy terms and conditions
and not directly or indirectly related to maternity.
The complainant is requesting forum to interfere in the matter and instructions may be given to
the insurance company to re-open his case and pay the necessary hospitalisation expenses as pr
normal terms and conditions of the policy without any limit.
Contentions of the Respondent Insurer (RI):-
In self-contained note RI submitted that as per the repudiation letter the ground of repudiation
was “On the perusal of the document claimant has been hospitalized for maternity/associated
condition and the same is not covered within the first nine month of policy inception
(11.12.2019), hence claim is not admissible as per the terms and condition”
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 16.03.2022 (Online), the complainant remained absent. Due
intimation and notice of the hearing had been sent to the complainant. RI maintained their stand.
To understand the exact cover granted, Forum checked the wordings of this cover, which is stated
as below:
Coverage of Maternity Expenses: The policy covers medical expenses for delivery (including
caesarian section) while hospitalized or the lawful medical termination of pregnancy during the
policy period excluding elective termination without threat to mother or child’s life, limited to 2
deliveries or terminations or either one of each during the lifetime of the insured. This will include
ectopic pregnancy, pre-natal and post natal expenses per delivery during hospitalization for
delivery or termination and medically necessary treatment of the new born baby within the policy
period provided that:
A waiting period of 9 months is applicable for any claim to be payable under this coverage.
Going by the above clause, Ectopic Pregnancy is covered under Maternity and its related
expenses are payable but not before the waiting period of 9 months. There isn’t any wrong
interpretation of coverage by RI as contended by the complainant.
Therefore, the Company’s stand of denial of claim is sustained. The case is dismissed.
Award follows;
AWARD
Under the facts and circumstances, the complaint is not tenable. The case is
dismissed.
Dated: at Pune, on 18/04/2022
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
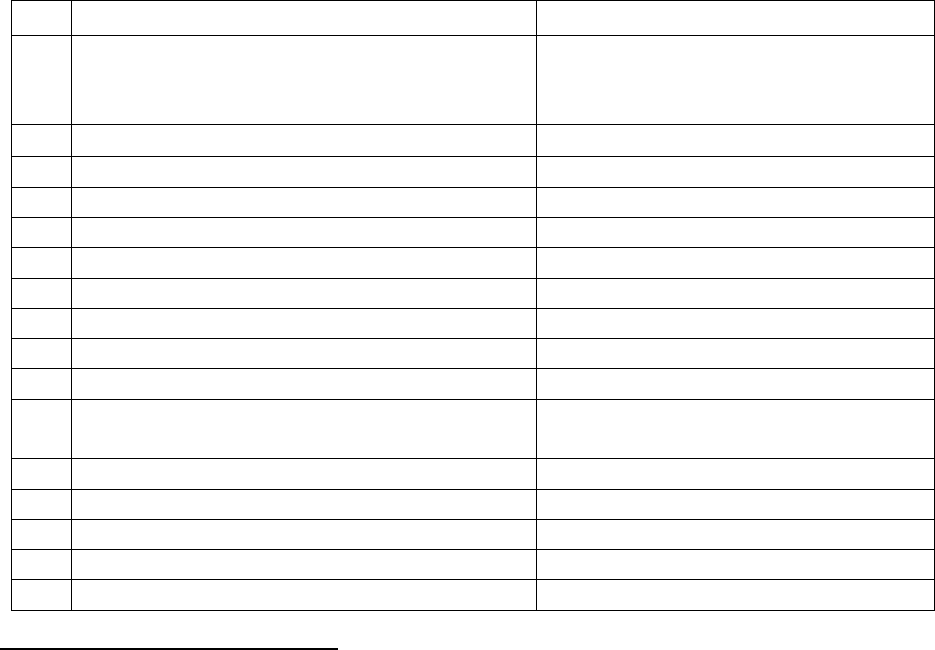
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. SEBASTIAN MENDAS V/S SBI GEN INS CO LTD
COMPLAINT NO: PUN-H-040-2021-0635
Award No IO/PUN/A/HI/ /2022-23
1.
Name & Address of the Complainant:
Mr. Sebastian Mendes, Thane
2.
Policy No:
Type of Policy:
41XXXX48-00
(MIRC Electronic Ltd )
Group Health Insurance Policy
3.
Policy period:
01.04.2019 to 31.03.2020
4.
Sum Insured
Not known
5.
Date of inception of first policy:
Not known
6.
Name & Age of the Insured and policyholder:
Mr. Sebastian Mendes, 54 yrs
7.
Name of the Insurer:
SBI General Insurance Co Ltd
8.
Reason for repudiation/Partial Settlement:
Not falling in day care procedures.
9.
Date of receipt of the Complaint:
18.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Rs.21757/-
12.
Insurance Ombudsman Rule (IOR)2017 under
which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
On line hearing on 24.03.2022
14.
Representation at the hearing
k) For the Complainant:
Himself & wife Ms.Valarie
l) For the insurer:
Ms. Chynikca Modie
15.
Complaint how disposed:
Allowed
Contentions of the Complainant: -
The complainant has taken Group Health Insurance Policy with Respondent Insurer (RI) SBI
General Insurance Co Ltd. The complainant lodged a claim of hospitalization in Shreeji Eye clinic
& Dental care clinic on 09.11.2019 for left eye treatment. The total expenditure on hospitalization
was Rs.21757/-.
The RI repudiated the claim stating that the procedure is not covered under day care list of
procedures in the subject policy and insured was hospitalized for less than 24 hours.
The complainant contends that same treatment for left eye had been undergone at the above
hospital on 28.09.2019 and the claim of Rs.25939/- was settled and paid. The doctor had clearly
said in the beginning of first treatment that the treatment can be repeated if there is no
improvement observed in the 1
st
treatment. He is questioning that why it was highlighted in the
2
nd
treatment and not in the 1
st
treatment which claim was cleared without any problem. He is
further contending that his treatment is coming under day care and he has found out from

reputed eye hospital (Lotus hospital) that any treatment pertaining to eye is under day care and
does not require hospitalization.
The complainant is requesting forum to look into his case and get the claim of his second
treatment settled.
Contentions of the Respondent Insurer (RI):-
It is submitted that the claim of the Complainant has already been assessed through an
independent health claims assessment agency (TPA) and as per their findings, based on
submitted documents vis-à-vis policy terms and conditions, the said reimbursement claim of the
Complainant was closed as inadmissible. The previous Claim bearing no. 99345692 was
erroneously settled by the TPA, which has been accepted and by them and they would share the
acceptance of recovery. That the same is explained and substantiated herewith.
That the insured, Mr. Sebastian Mendes was hospitalized in SHREEJI EYE CLINIC AND DENTAL
CARE CLINIC (Hereinafter referred to as “Hospital”) on day care basis twice, first on 28/09/2019
and then on 09/11/2019 for the treatment of left eye macular edema for which intravitreal anti
vascular endometrial growth factor was given in left eye. That two consecutive claims i.e.claim
no. 99345692 and 99653160 were registered on behalf of the insured under the said policy
bearing no. 4101190500000048-00 towards the expenses related to both the aforesaid
Hospitalization.
That as per the intimation received, a reimbursement claim bearing claim no. 99345692/ SBIG
Claim No. 200319003154-01 under the policy of the Insured, bearing no. 4101190500000048-00
was registered on behalf of the Insured with SBI General through “Medi Assist Insurance TPA
Private Limited” (Hereinafter referred to as TPA) for the treatment of left eye macular edema for
which intravitreal anti vascular endometrial growth factor was given in left eye. That the insured
was hospitalized on 28/09/2019 for the same.
That as per the intimation received, a reimbursement claim bearing claim no. 99345692/ SBIG
Claim No. 200319003154-01 under the policy of the Insured, bearing no. 4101190500000048-00
was registered on behalf of the Insured with SBI General through “Medi Assist Insurance TPA
Private Limited” (Hereinafter referred to as TPA) for the treatment of left eye macular edema for
which intravitreal anti vascular endometrial growth factor was given in left eye. That the insured
was hospitalized on 28/09/2019 for the same.
TPA settled the above claim for Rs. 25,939/- against the claimed amount of Rs. 26,089/- on
05.11.2019.
That thereafter another reimbursement claim bearing claim no. 99653160 / SBIG Claim no.
200319012209-01 was lodged by the Insured under the aforesaid policy bearing no.
4101190500000048-00 registered on behalf of the Insured with SBI General through “Medi Assist
Insurance TPA Private Limited” (Hereinafter referred to as TPA) for the treatment of left eye
macular edema for which intravitreal anti vascular endometrial growth factor was given in left
eye using local eye drops. That the insured was hospitalized on 09/11/2019 for the same. That
upon a close and complete scrutiny of the available documents vis-à-vis policy terms &
conditions, the Company observed that the Insured was hospitalized for less than 24 hours, and

the procedure is not covered under day care list of procedures in the subject policy and thus falls
out of scope of the subject policy. That based on the medical documents received from the
Hospital and other documents available on record, the Company observed that:
i. The insured Mr. Sebastian Mendes was admitted in the “Shreeji Eye Clinic and Dental Care
Clinic” on day care basis on 09/11/2019 for treatment of left eye macular edema for which
intravitreal anti vascular endometrial growth factor was given in left eye.
ii. That the insured was hospitalized for less than 24 hours, thus the said hospitalization does not
fall under the policy definition of hospitalization under the said policy, which requires at least 24
hours hospitalization.
iii. Further, the aforementioned procedure does not require 24 hour hospitalization, and was
done on a day care basis. However, the same procedure is not covered in the daycare list of the
policy. There was also no procedure/ surgical intervention done, and topical anesthesia was
provided using local eye drops.
iv. As per policy terms and conditions, the aforementioned hospitalization and treatment
underwent by the insured is neither covered under the policy definition of Hospitalization, nor
included in the list of daycare treatment, and therefore out of scope of the policy
Upon reviewing the claim documents of the instant case, TPA realized that the claim no.
99345692 was erroneously settled and the same should have been denied under the same clause
as claim no. 99653160, being outside the scope of policy definition of hospitalisation, nor
included in the list of day care. TPA also accepted the recovery of Rs. 25,939/- for the amount
settled erroneously.
Result of personal hearing with both the parties (Observations & Conclusions):
During the personal hearing on 24.03.2022 (Online), both the parties reiterated their respective
stand.
On perusal of claim papers and SCN submitted by RI Forum finds that the claim for Intra vitreal
injection has been denied by RI stating the reason that it is not covered under day care treatment.
Contradictorily, it is found in their own SCN on page no 7 under scope of cover at point F,
intravitreal injection is seen as covered.
Claim is therefore very well admissible. In their SCN and during the hearing RI representation
conveyed that a similar claim was paid earlier erroneously and they are in the recovery
procedure. In view of the clear cut coverage, there is no need of recovery of earlier claim paid
which RI has informed at the time of hearing
Complaint admitted.
Award follows,

AWARD
Under the facts and circumstances, RI to directed to pay Rs. 21757/- less compulsory
deductions as per policy terms and conditions to the complainant towards full and
final settlement of the complaint.
The award is to be satisfied within 30 days from the date of receipt of this award
failing which it will attract interest at the applicable bank rate plus 2% extra from
the date of rejection of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurer
Dated: at Pune on this 28
th
day of April, 2022
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. VIKAS RAMESH CHAVAN V/S CHOLAMANDALAM MS GEN INS CO LTD
COMPLAINT NO: PUN-H-012-2021-0652
Award No IO/PUN/A/HI/ /2022-23
1.
Name & Address of the Complainant:
MR. VIKAS RAMESH CHAVAN, Pune
2.
Policy No:
Type of Policy:
28XXXX00/00
Group Health Insurance.
3.
Policy period:
20.02.2020 to 19.02.2021
4.
Sum Insured
Rs 5,00,000/-
5.
Date of inception of first policy:
20/02/2020
6.
Name & Age of the Insured policyholder:
Mr. Vikas Ramesh Chavan, 42 yrs
7.
Name of the Insurer:
Cholamandalam MS Gen Ins Co Ltd
8.
Reason for repudiation/Partial Settlement:
Hospitalization period does not
warrant inpatient admission
9.
Date of receipt of the Complaint:
15.03.2021
10.
Nature of complaint:
Full settlement of claim amount
11.
Amount of Claim:
Rs.144311 /-
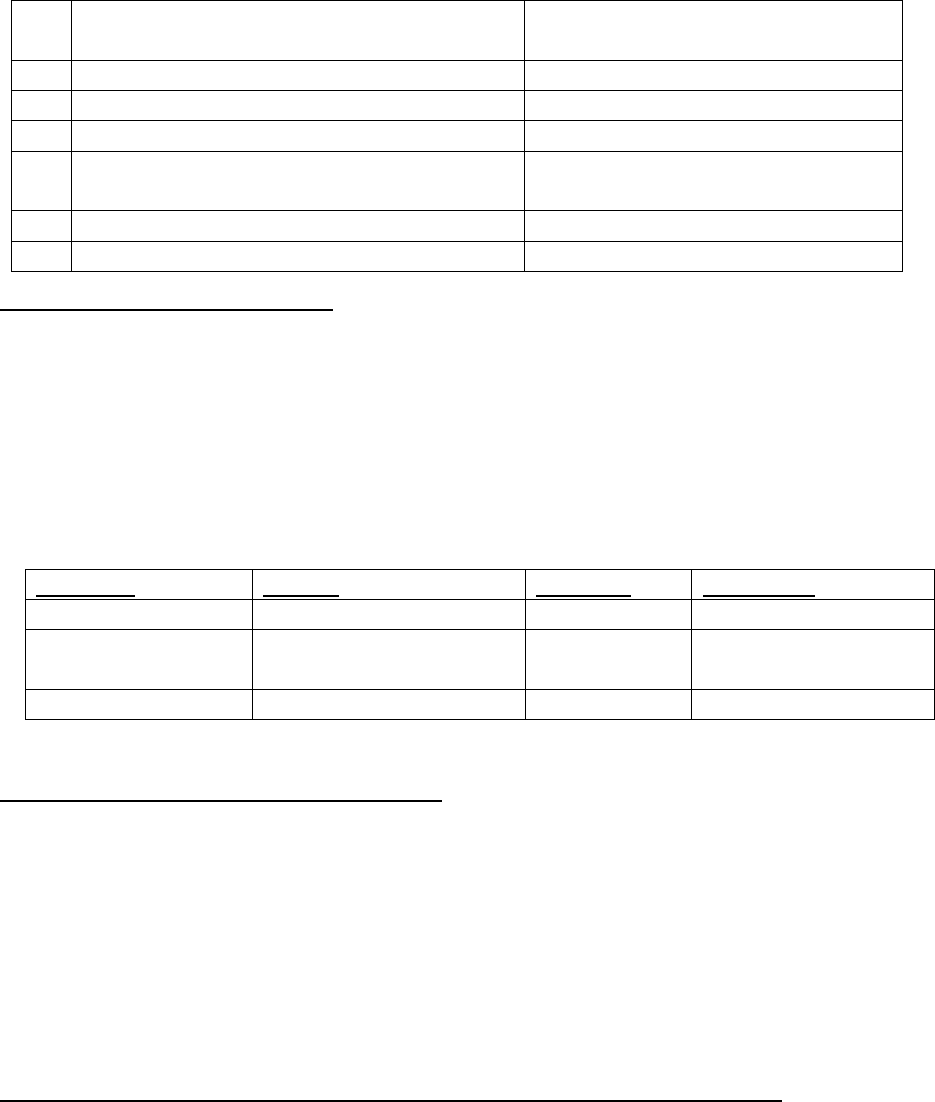
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
On line hearing on 25.03.2022
14.
Representation at the hearing
m) For the Complainant:
Himself.
n) For the insurer:
Mr. Mangesh Inamdar, Dr Minal
Vinoth.
15.
Complaint how disposed:
Allowed.
16.
Date of Award:
13/04/2022
Contentions of the Complainant:-
• The complainant had taken health insurance (Family floater) with Respondent Insurer The
Cholamandalam MS Gen Ins Co Ltd for self for Sum Insured Rs 5,00,000/-. He lodged claim of self-
hospitalization in three hospitals as per the chart given below. The total expenditure on
hospitalization was of Rs.3000/-+38700/-+121259/-.
• The RI repudiated the claim stating that the treatment given during the hospitalization period
doesn’t warrant inpatient admission.
HOSPITALISATION PERIOD:
HOSPITAL
PERIOD
AMOUNT
DIAGNOSIS
Paras Hospital
12.08.2020 to 13.08.2020
Rs.3000/-
Day care
7 orange Hospital
13.08.2020 to 14.08.2020
Rs.38700/-
Covid 19 for medical
management
Jeevan Jyoti Hospital
14.08.2021 to 21.08.2021
Rs.121259/-
Viral Pneumonia
• The complainant is requesting forum to intervene for settlement of full claim amount,
Contentions of the Respondent Insurer (RI):-
In claim repudiation letter dt. 16.10.2020, RI have stated that,
On perusal of the claim documents, it is observed that the treatment given during the
hospitalization period doesn’t warrant inpatient admission and can be treated in outpatient
department. No indemnity is available or payable which is outside the scope of policy coverage
part B section 1, which reads as “If the insured is diagnosed with an illness or suffers accidental
bodily injury which necessitates his hospitalization and the insurer will reimburse the insured
persons consequent hospitalization expenses”. In the absence of any illness necessitating the
hospitalization as specified in this coverage, the claim is inadmissible.
Result of personal hearing with both the parties (Observations & Conclusions):
An online hearing was held on 25/03/2022, attended by both the parties.
It was averred by complainant that though he was detected Covid -ve, he was diagnosed with
Pneumonia, and was treated for the same. He was admitted to Hospital as per doctor’s advice
and afterwards he was shifted from Paras Hospital to 7 Orange hospital and again to Jeevan Jyoti
Hospital. RI contended that they have not received treatment papers, vitals and medication
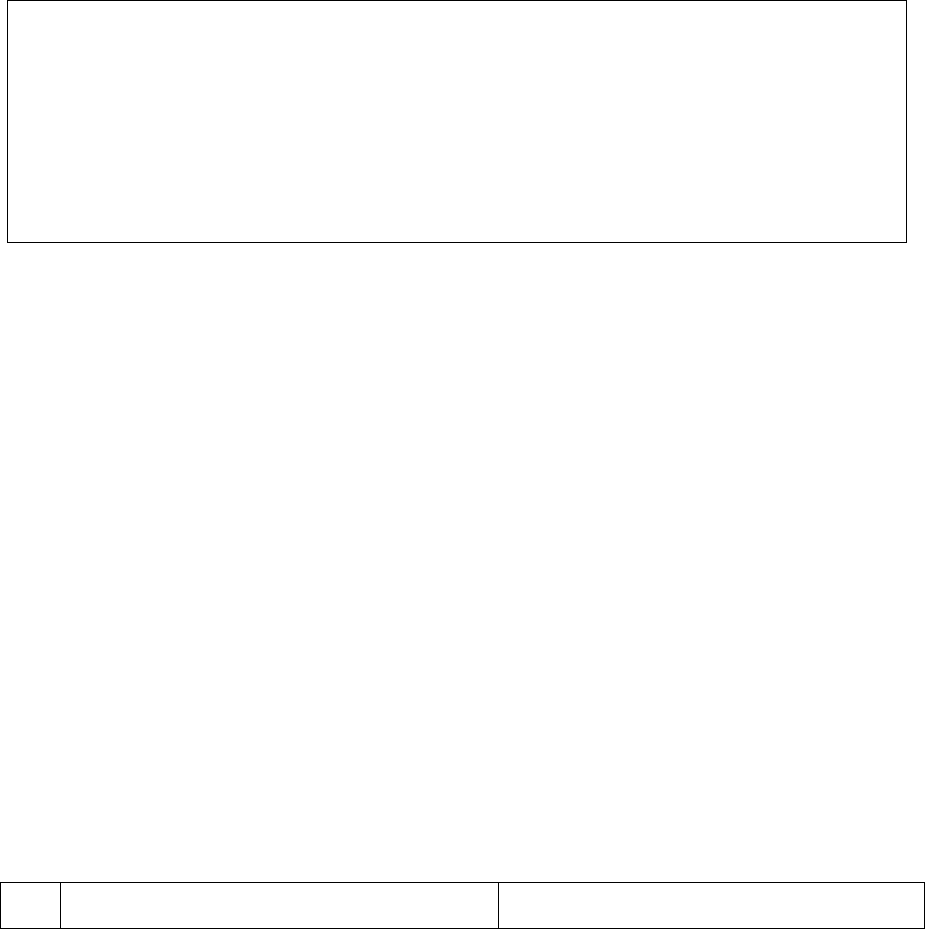
chart, ICP pertaining to hospitalization. Hence, based on discharge card, they have rejected the
claim as hospitalization did not seem necessary. The complainant reiterated that he has
submitted all hospitalization papers along with Covid report to Dr. Bhagyashree and other
officers of Cholamandalam.
In view of the contentions of the complainant of having submitted all the claim papers,
complainant is advised to resend the email/the correspondence to RI, through which he had
forwarded the papers for processing of the claim.
Forum found the claim is admissible.
Award follows;
AWARD
Under the facts and circumstances, RI is directed to settle the claim after compulsory
deductions as per terms & conditions of the policy towards full and final settlement of
the complaint.
The award is to be settled within one month from the date of receipt of this award failing
which it will attract interest at the prevailing bank rate plus 2% extra from the date of
rejection of the claim till the date of payment of this award.
The attention of the Complainant and the insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award
and intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurers.
Dated: on 13
th
day of April 2022, at Pune
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, PUNE
(STATE OF MAHARASHTRA EXCEPT MUMBAI METRO)
UNDER SECTION 16/17 OF THE INSURANCE OMBUDSMAN RULES-2017
OMBUDSMAN– VINAY SAH
CASE OF MR. VISHAL RAI V/S THE NEW INDIA ASSUARANCE CO. LTD
COMPLAINT NO: PUN-H-049-2021-0582
Award No IO/PUN/A/HI/ /2022-23
1.
Name & Address of the Complainant:
Mr. Vishal Rai, Thane
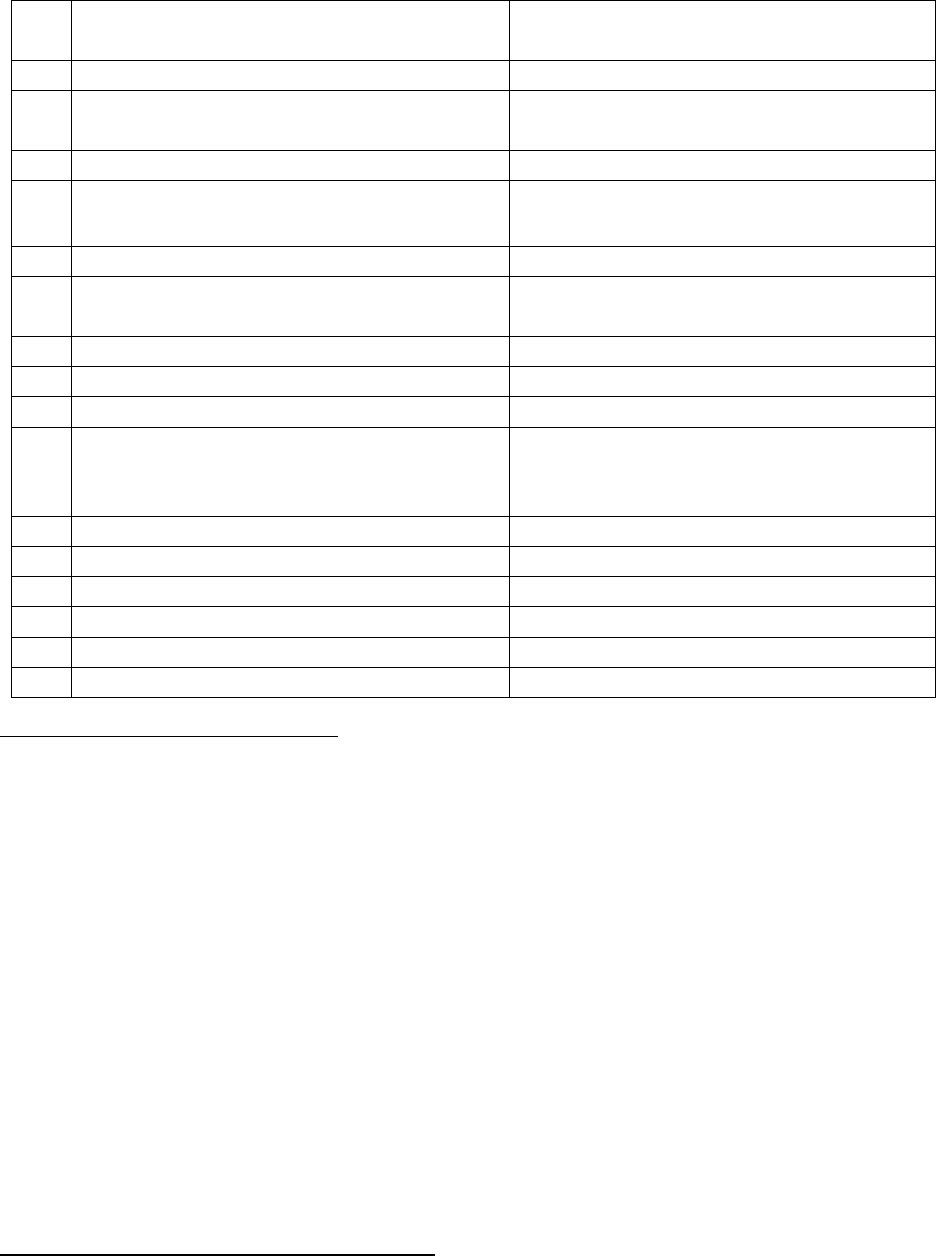
2.
Policy No:
Type of Policy:
11XXXX0011
Group Medical Insurance Policy
3.
Policy period:
01.05.2019 to 30.04.2020
4.
Sum Insured:
Rs. 50,000/-(for maternity - Child birth,
Normal Delivery
5.
Date of inception of first policy:
No policy Document available
6.
Name & Age of the Insured:
Name of the Policyholder:
Mrs. Priya Jaiswal, 26 years
Mr. Vishal Rai
7.
Name of the Insurer:
The New India Assurance Co. Ltd.,
8.
Reason for repudiation/Partial Settlement:
Partial Payment – Sum Insured-
Exhausted
9.
Date of receipt of the Complaint:
20.03.2021
10.
Nature of complaint:
Settlement of balance claim amount
11.
Amount of Claim:
Rs. 30,121/-
12.
Insurance Ombudsman Rule (IOR)2017
under which the Complaint was
registered:
Rule 13 1 (b)
13.
Date of hearing/Place:
On line hearing on 25.03.2022
14.
Representation at the hearing
o) For the Complainant:
Himself
p) For the insurer:
Mrs. Meenu Bhatia
15.
Complaint how disposed:
Allowed
16.
Date of Award
13.04.2022
Contentions of the Complainant: -
The Complainant is corporate policy holder & husband of the insured/patient Mrs. Priya Jaiswal,
who is covered under the insurance policy issued by the Respondent Insurer (hereinafter referred
to as RI). On 22.08.2019, the insured was admitted for full term pregnancy delivery. When the
claim of Rs. 50,000/- was raised with RI, only part payment of Rs. 19,879/- was paid, as the
Complainant was already paid the claim amount of Rs. 30,121/- (Maximum sum insured for
maternity Rs. 50,000/-) during insured’s earlier hospitalization for Urinary Tract Infection in May
2019.
The complainant got clarity from the doctor and as confirmed by them, there is no co-relation
between the UTI and pregnancy. The patient was admitted in the hospital both the times due to
different reasons and hence the claim raised for UTI in June 2019 should not be considered under
maternity limit. The Complainant has attached a doctor’s certificate dated 18.09.2019 justifying
his contention.
The Complainant has requested the forum to instruct the insurance company to pay the
remaining amount of Rs. 30,121/-
Contentions of the Respondent Insurer (RI):-
The TPA of RI replied to the Complainant vide their email dated 18.09.2019 that the previous
hospitalization during May, 2019 is for UTI. The reply is – As UTI is a common during pregnancy,
that’s because the growing fetus can put pressure on the bladder & urinary tract. The larger
urinary tract, along with increased bladder volume & decreases bladder tone, all cause the
urine to become more still in the urethra. Due to which common urinary infection occurs.”
The RI considered the maximum Maternity limit of Rs. 50,000/- is applicable for UTI.
Result of Online hearing of both the parties:-
During the online hearing on 25.03.2022, both the parties reiterated their respective stand.
Regarding partial non-payment, RI averred that in May 2019 the insured was admitted for UTI
which was due to pregnancy for which they have settled the claim of Rs 30,121/-. Now, they have
settled the remaining balance of Rs 19879/-towards maternity.
It is to be noted that, firstly, UTI is not caused by pregnancy alone. It is an infection which anybody
can contract. Secondly, ‘Maternity’ is an extra benefit given under the policy besides the cover
for other ailments. Hence, UTI even if was due to pregnancy, it has to be covered in regular course
and should not be merged in maternity benefits; because, maternity benefit is earmarked for
child birth alone. It is wrong to include any related ailment into it and deplete its limit.
Award follows,
AWARD
Under the facts and circumstances, RI is directed to settle the claim by paying the remaining
amount of Rs 30,121/- towards full and final settlement of this claim.
The award is to be settled within one month from the date of receipt of this award failing
which it will attract interest at the prevailing bank rate plus 2% extra from the date of
rejection of the claim till the date of payment of this award.
The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules 2017:
17(6) The Insurer shall comply with the award within thirty days of the receipt of the award and
intimate compliance of the same to the Ombudsman.
17(8) The award of Insurance Ombudsman shall be binding on the Insurers.
Dated: at Pune on 13
th
April 2022
VINAY SAH
INSURANCE OMBUDSMAN, PUNE
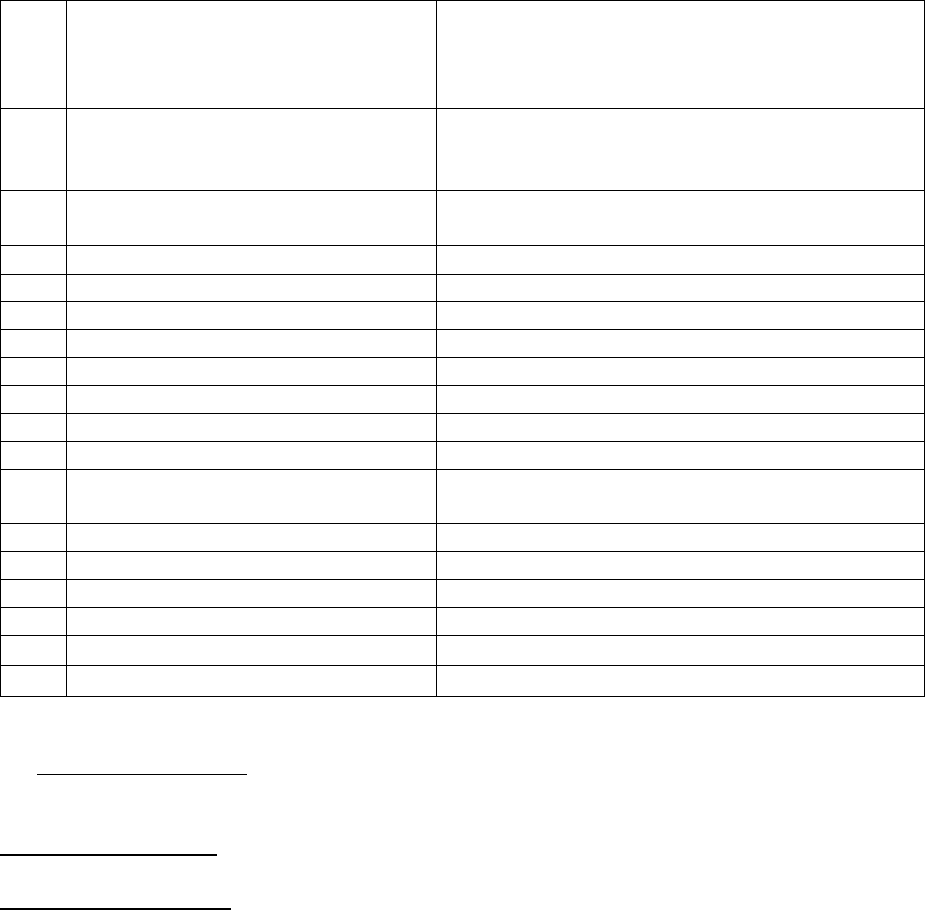
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. MADAN SINGH CHAUHAN V/S UNITED INDIA INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-051-2122-0627
AWARD NO:
1.
Name & Address of the Complainant
Mr. Madan Singh Chauhan
Indian Bank
133, Indira Udyan Marg, Ward No.-9
Vikas Nagar
2.
Policy No:
Type of Policy
Duration of policy/Policy period
5001002819P111085789
Group Health Insurance Policy
01-10-2019 to 30-09-2020
3.
Name of the insured
Name of the policyholder
Ms. Shavi Chauhan
Indian Banks Association, A/c Allahabad Bank
4.
Name of the insurer
United India Insurance Co. Ltd.
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the Complaint
24-02-2022
8.
Nature of complaint
Non-settlement of claim
9.
Amount of Claim
Rs. 1,47,977/-
10.
Amount and date of Partial Settlement
NIL
11.
Amount of relief sought
Rs. 1,47,977/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27-04-2022
14.
Representation at the hearing
a. For the Complainant
Mr. Madan Singh Chauhan
b. For the insurer
Ms. Pamela Pinto
15.
Complaint how disposed
Award
16.
Date of Award/ Order
28-04-2022
17) Brief Facts of the Case: This complaint is filed by Mr. Madan Singh Chauhan against United India
Insurance Co. Ltd. for non-settlement of his claim under his policy.
18) Cause of Complaint:
Complainant’s argument: Claimant is a member of Group Health Insurance Policy of Indian Banks
Association, A/c- Allahabad Bank, issued by United India Insurance Co. Ltd. for the period- 01-10-2019 to
30-09-2020.
● He submitted a claim on 09-09-2020 and replied queries on 14-10-2020.
● After several calls and e mails, TPA informed that the claim has been processed on 08-09-2021 and
sent a mail as “arranging to refer to the insurer for reopening.
● On 28-12-2021, he received a mail from TPA as ‘the claim has been processed and they have
referred the claim to insurer for approval of reopening.
● On 14-01-2021, the same e mail was received once again but the claim is long pending about 17
months.
Insurers’ argument: The insurance company submitted their SCN dated- wherein they submitted their
reply as under: -
● They had issued a Group Mediclaim Policy to Indian Banks Association -Allahabad Bank covering
their employees Along with their dependent members.
● Sh. Madan Singh Chauhan along with dependent members are included in the said policy for sum
insured of Rs. 4,00,000/-
● They have reviewed the claim and found that certain documents (Original Investigation Report, HPE
Report and Original Doctor’s Prescriptions) were pending to be submitted by the insured,
● Hence, the claim was closed under clause-505- Submission of claim documents.
● However, they have now received the query documents in due course and are in the process of
settling the claim to the tune of Rs. 1,44,010/-.
● The deduction of Rs. 5,685/- is towards non-medical expenses.
19) Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint letter
b) Policy document
c) Discharge Summary
d) SCN
21) Observations & Conclusion: -
Both the parties attended the online hearing on 27-04-2022.and reiterated their submissions.
The complainant stated that after submission of his claim as well as meeting all the queries, the claim is
long pending for about 17 months.
However, vide their e mail dated- 26-04-2022, the insurance company informed the office of Bima Lokpal
that the claim has been settled for Rs. 1,44,010/- only and the amount has been credited to Allahabad
Bank Welfare Fund Account in Indian Bank being a Group Policy who will in turn transfer the claim amount
to the claimant
It is observed that the inadvertent delay on the part of the insurer in settling the claim amounts to severe
deficiency in service. The insurance company is directed to pay interest also to the claimant as specified
under Protection of Policy Holder’s interest subject to the terms and conditions of the policy.
AWARD
The insurance company is directed to pay the interest to the claimant to be calculated from 28-
12-2021, i.e., the date when the claimant received a mail from TPA as ‘the claim has been
processed and they have referred the claim to insurer for approval of reopening, as specified
under Protection of Policyholders Interest, subject to the terms and conditions of the policy.

22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award
within thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 28.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. ASHWANI KUMAR V/S THE NEW INDIA ASSSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-049-2122-0579
AWARD NO:
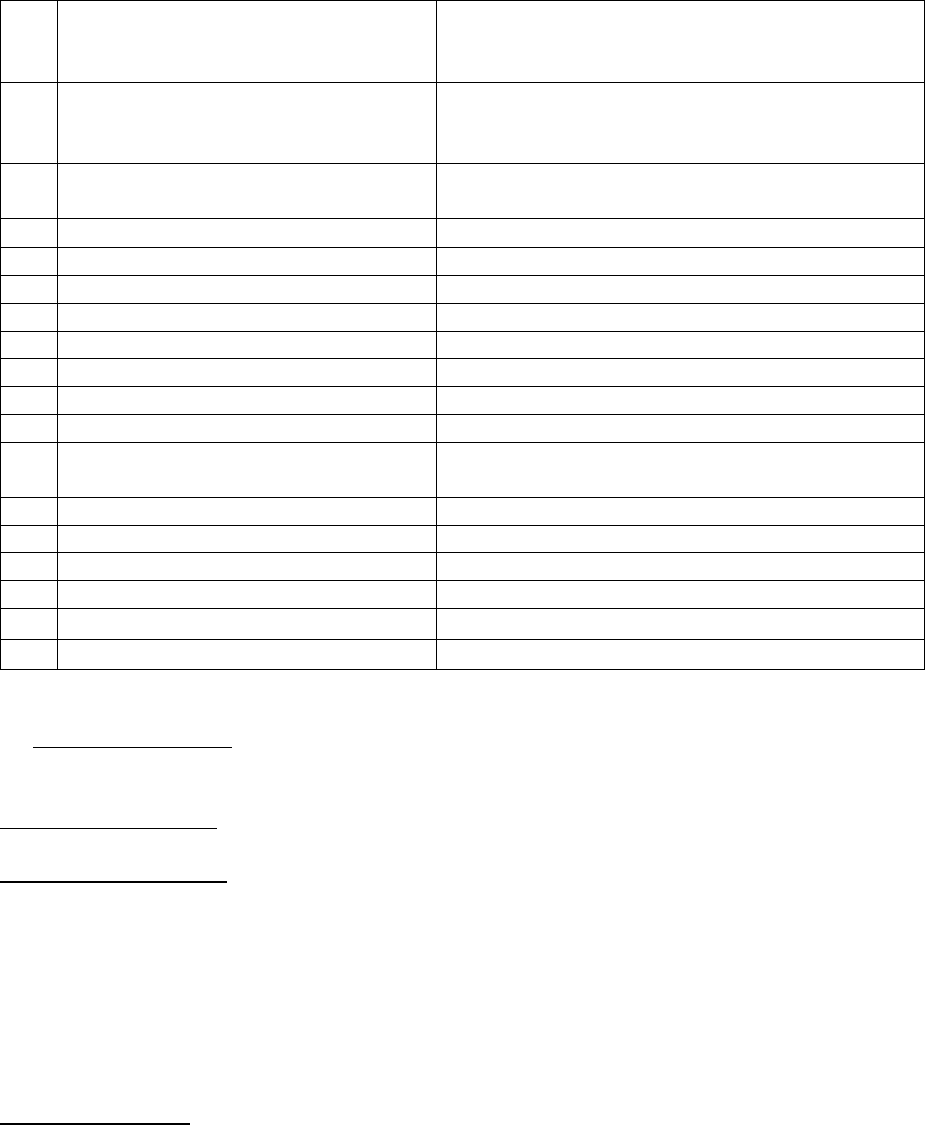
1.
Name & Address of the Complainant
Mr. Ashwani Kumar
69, Mohall Tuharam,
Pilibhit, UP-262001
2.
Policy No:
Type of Policy
Duration of policy/Policy period
120300341704000000010
Health (Group Insurance)
-
3.
Name of the insured
Name of the policyholder
Mr. Ashwani Kumar
LIC of India
4.
Name of the insurer
The New India Assurance Co. Ltd.
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the Complaint
03-02-2022
8.
Nature of complaint
Non-settlement of claim
9.
Amount of Claim
Rs. 2,70,286/-
10.
Amount and date of Partial Settlement
NA
11.
Amount of relief sought
Rs. 2,70,286/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27-04-2022
14.
Representation at the hearing
a. For the Complainant
Mr. Ashwani Kumar
b. For the insurer
Mr. Ankit Raghuvanshi
15.
Complaint how disposed
Award
16.
Date of Award/Order
28.04.2022
17) Brief Facts of the Case: This complaint is filed by Mr. Ashwani Kumar against The New India Assurance
Co. Ltd. for rejection of his claim under the policy.
18) Cause of Complaint:
Complainant’s argument: Claimant is a member of Group Health Insurance Policy of LIC of India which
was taken by them from The New India Assurance Co. Ltd.
● Claimant met with an accident in June, 2019. He submitted all his claim related documents in
original after recovery from the injuries, to the Life insurance company/s Pilibhit Branch.
● The claim is still pending and has not been settled by the LIC. It is being lingered on, on one pretext
or the other.
● The claim has neither been rejected nor paid.
Insurers’ argument: The insurance company submitted their SCN dated- 11-04-2022 wherein they
submitted their reply as under: -
● Insured 73 years/male was admitted in Indian Spinal Injuries Centre, New Delhi from 29
th
Jun,2020
to 4
th
Aug., 2020 for head injury, post head injury, decompression surgery, vp shunt for
cranioplasty.
● Reimbursement claim for Rs. 2,70,286/- towards the expenses incurred for the aforesaid
hospitalization was submitted, Claim was received and processed under claim No.-101513473.
● On scrutinizing the documents, it was found that few documents were required to process the
claim.
● Hence, on 3
rd
Oct., 2020, correspondence was sent to the insured and the following documents
were requested to be submitted, in order to process the claim: -
1. Original cancelled cheque with pre-printed name of proposer/ policyholder/employee for
transferring amount cancelled cheque.
2. Attested copy of documents. All documents attested copies from concerned TPA.
3. Settlement advice letter for main claim processed by other TPA/ company-provide
settlement letter from TPA where claim was partially settled.
4. Pre numbered paid receipt for the amount collected from the patient on 04-08-2020 for Rs.
510000- Receipt for balance payment amounts.
● Two reminders were sent to the complainant by the insurers.
● Since, according to policy terms and conditions:
The insured person shall submit to TPA all original bills, receipts and other documents upon which
a claim is based and shall also give the TPA/ Company such additional information and assistance as
the TPA/ Company may require.
● Finally, after 3 reminders, on 22 Nov., 2020, denial letter was sent to the claimant.
● However, later on 21 Jan, 2021 & 17 April, 2021, they received the additional documents i.e.,
another TPA, Family Health Plan Insurance Plan Insurance TPA had settled for Rs. 6 Lakh and
payment receipts of Rs. 5 lakh 10 thousand.
● Hence, they have instructed to process the claim based on the available documents.
19) Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint letter
b)
f) SCN
21) Observations & Conclusion: -
Both the parties attended the online hearing on 27-04-2022.and reiterated their submissions.
The complainant stated that he met with an accident in June, 2019. He submitted all his claim related
documents in original after recovery from the injuries, to the Life insurance company/s (employer) Pilibhit
Branch but the claim is still pending and has not been settled by the insurance company.
Insurer defended their decision on the grounds that on scrutinizing the documents, it was found that few
documents were required to process the claim. Hence, on 3
rd
Oct., 2020, correspondence was sent to the
insured and the few documents were requested to be submitted, in order to process the claim. Finally,
after 3 reminders, on 22 Nov., 2020, denial letter was sent to the claimant.
However, later on 21 Jan, 2021 & 17 April, 2021, they received the additional documents from another
TPA, Family Health Plan Insurance Plan Insurance who had settled for Rs. 6 Lakh and payment receipts of
Rs. 5 lakh 10 thousand. The insurance company is now processing the claim based on the available
documents.
It is observed that the claim has been badly delayed and handled with insensitivity. They had received
the additional documents from another TPA on 21-01-2021 & 17-04-2021 but even then, no steps were
taken to settle the claim after receipt of those documents. And now, as stated by the insurers, they are
going to settle the claim on the basis of available documents which should have been done long back.
Insurance company is directed to settle the claim within 10 days with interest to be calculated from 17th
April, 2021 (i.e., date of receipt of documents), as specified under Protection of Policyholders Interest,
subject to the terms of the policy.
AWARD
The insurance company is directed to settle the claim within 10 days with interest to be calculated
from 17th April, 2021 i.e., the date of 17-04-2021 (i.e., date of receipt of documents), as specified
under Protection of Policyholders Interest, subject to the terms and conditions of the policy.
22.If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award
within thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 28.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. VINOD SINGHAL V/S UNTED INDIA INSURANCE CO. LTD.
COMPLAINT REF: NO: NOI-H-051-2122-0593
AWARD NO:
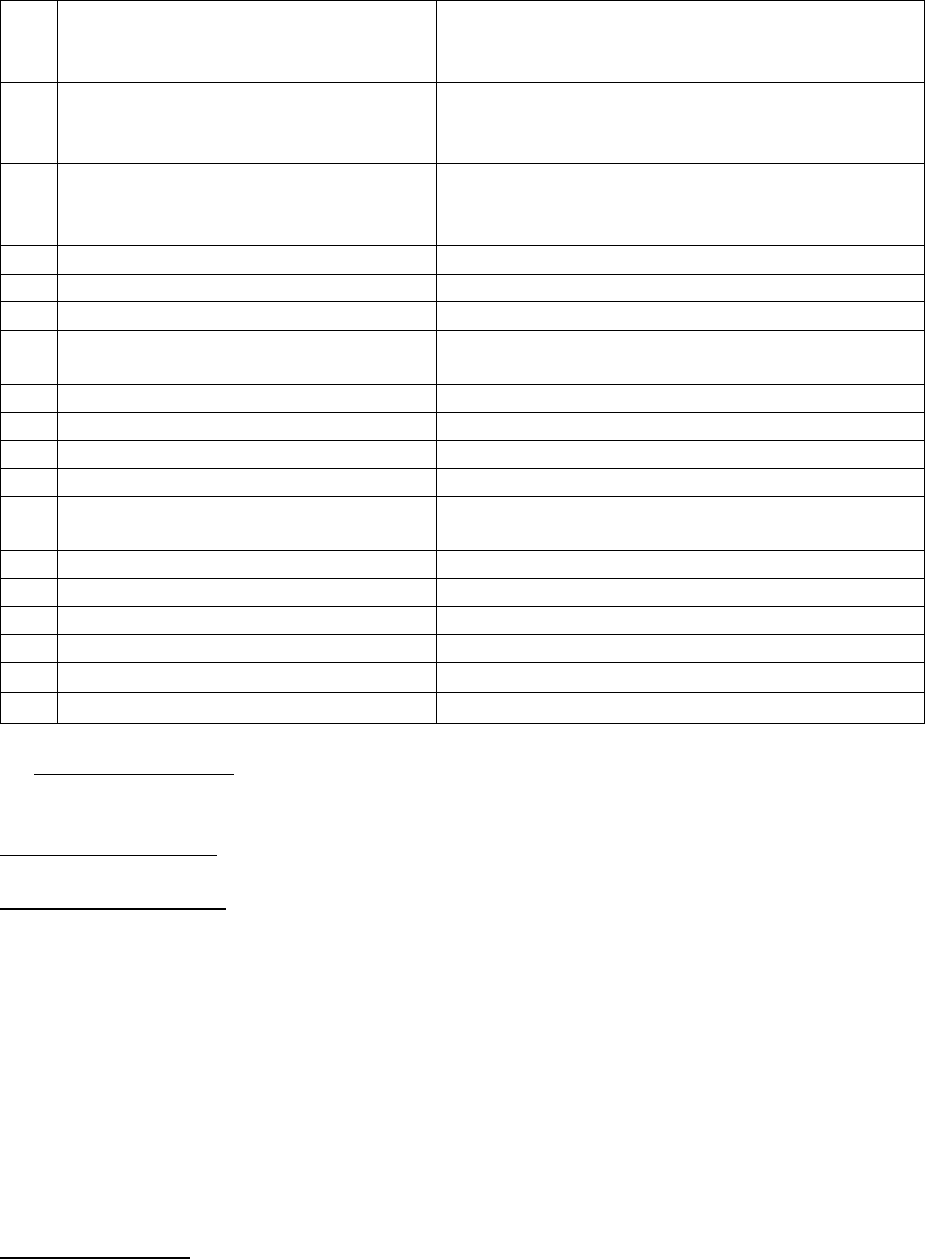
1.
Name & Address of the Complainant
MR. Vinod Singhal
89, HIG, Abhay Khand-I
Indirapuram (UP)- 201014
2.
Policy No:
Type of Policy
Duration of policy/Policy period
0504002820P102561452
Health (UBI Group Health Policy)
09-06-2020 to 08-06-2021
3.
Name of the insured
Name of the policyholder
Mr. Vinod Singhal
Mr. Vinod Singhal
4.
Name of the insurer
United India Insurance Co. Ltd.
5.
Date of Repudiation
NA
6.
Reason for repudiation
NA
7.
Date of receipt of the Complaint
09-02-2022
8.
Nature of complaint
Partial settlement of claim
9.
Amount of Claim
Rs. 4,79,904/-
10.
Amount and date of Partial Settlement
Rs. 15,000/-
11.
Amount of relief sought
Rs. 4,64,904/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27-04-2022/ NOIDA
14.
Representation at the hearing
a. For the Complainant
Mr. Ashish Gupta (Claimant’s son in law)
b. For the insurer
Ms. Rajni Ahuja & Ms. Hemlatha Arunachalam
15.
Complaint how disposed
Award
16 .
Date of Award/ Order
27-04-2022
17) Brief Facts of the Case: This complaint is filed by Mr. Vinod Singhal against United India Insurance Co.
Ltd. for partial settlement of his claim under the policy.
18) Cause of Complaint:
Complainant’s argument: Claimant is a member of Group Health Insurance Policy of Union bank of India
which was taken by them from United India Insurance Co. Ltd.
● Claimant contracted with Covid 19 in April, 2021 and unfortunately did not find hospital at that time
due to unavailability of beds.
● At that time people were on roads with their oxygen cylinders due to lack of hospital beds. Thus, he
had to setup medical facilities at home like many other patients.
● He filed his claim for Rs. 4,79,904/- with the insurer along with all original bills and required
documents but the insurer processed only Rs. 15,000/- citing the reason that under home care
treatment, only this much amount is possible.
● He told the insurer that treatment at home had to be opted by him by chance and not by choice but
they have denied processing the claim.
Insurers’ argument: The insurance company submitted their SCN dated- 23-02-2022 wherein they
submitted their reply as under: -

● As per AB Arogyadaan Insurance Policy condition No.5.29 Domiciliary Treatment is not covered.
● As per AB Arogyadaan Insurance Policy Condition No.4.2. Note 1, Procedures/treatments usually
done in out-patient department are not payable under the policy even if converted as an inpatient
in the hospital for more than24 hours or carried out in Day Care Centres
● However, during this pandemic situation, taking into consideration the evolving industry practice
and the regulatory advises, the following guidelines were issued by insurer’s HO has vide circular
dated 17.07.2020 to cover Home Care Treatment for Covid-19 Patients as detailed hereunder
● Home Care Treatment means Treatment availed by the Insured Person at home for Covid-19 on
positive diagnosis of Covid-19 in a government authorized diagnostic Centre, which in normal
course would require care and treatment at a hospital but is actually taken at home maximum up
to 14 days per incident provided that:
i. The Medical Practitioner advises the Insured Person to undergo treatment at home
ii. There is a continuous active line of treatment with monitoring of the health status by a
medical practitioner for each day through the duration of the home care treatment
iii. Daily monitoring chart including records of treatment administered duly signed by the
treating doctor is maintained.
iv. Insured shall be permitted to avail the services as prescribed by the Medical
Practitioner. Cashless facility shall be offered under home care expenses if the treatment
is through a network provider.
v. In case the insured intends to avail the services of non-network provider claim shall be
subject to re-imbursement, a prior approval from the Insurer / TPA needs to be taken
before availing such services.
● b. In this benefit, the following shall be covered if prescribed by the treating Medical Practitioner
and is related to treatment of COVID:
i. Diagnostic tests undergone at home or at diagnostics centre
ii. Medicines prescribed in writing
iii. Consultation charges of the medical practitioner
iv. Nursing charges related to medical staff
v. Medical procedures limited to parenteral administration of medicines
vi. Cost of Pulse Oximeter, Oxygen cylinder and Nebulizer
c. The benefit under this clause is limited to Rs. 15,000 per incident.
d. Where, the policy already has ‘Domiciliary Hospitalization’ cover, the Insured may be
given a choice to refer a claim under the said Domiciliary Hospitalization cover of the
policy or as per the above provision.
e. The claim intimation clause should be adhered to.
● Hence, they submitted that their stand in settlement of the claim is in order. As per their circular
their TPA has settled the claim for an amount of Rs.15000/-
19) Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint letter
b) Policy document

c) Circular on non-medical expenditure related to Covid & Non Covid treatments
d) SCN
21) Observations & Conclusion: -
Both the parties attended the online hearing on 27-04-2022.and reiterated their submissions.
The complainant stated that he contacted Covid 19 in April, 2021, and unfortunately did not find hospital
at that time due to unavailability of beds. He filed his claim for Rs. 4,79,904/- with the insurer along with
all original bills and required documents but the insurer processed only Rs. 15,000/- citing the reason that
under home care treatment, only this much amount is possible.
Insurer defended their decision on the grounds that as per AB Arogyadaan Insurance Policy condition
No.5.29 Domiciliary Treatment is not covered. Moreover, as per AB Arogyadaan Insurance Policy
Condition No.4.2. Note 1, Procedures/treatments usually done in out-patient department are not payable
under the policy even if converted as an inpatient in the hospital for more than24 hours or carried out in
Day Care Centres. However, during this pandemic situation, taking into consideration the evolving
industry practice and the regulatory advises, followed by the guidelines issued by the Company’s HO vide
circular dated 17.07.2020 to cover Home Care Treatment for Covid-19, according to which the benefit
under the clause-C is limited to Rs. 15,000 per incident. Hence, their stand in settlement of the claim is in
order
It is observed that the AB Arogyadaan policy does not cover Domiciliary Hospitalization expenses at all in
any circumstances vide policy clause number-5.29 under the heading Permanent Exclusions. However, an
amount of Rs. 15,000/- was paid to the claimant only because of insurance company’s circular dated-17-
07-2020, according to which under the heading- Home Care Treatment,3 (c), The benefit under this clause
is limited to Rs. 15,000/- per incident.
Insurer’s action is justified as per policy conditions and does not warrant any interference. Complaint is
dismissed.
22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
Place: Noida. C.S. PRASAD
Dated: 28.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTRAKHAND
UNDER INSURANCE OMBUDSMAN RULE 2017
OMBUDSMAN: SH. C.S. PRASAD
CASE OF SH.DESHRAJ ANAND V/S NATIONAL INSURANCE CO. LTD.
COMPLAINT REF. NO.: NOI-H-048-2122-0616
AWARD NO:
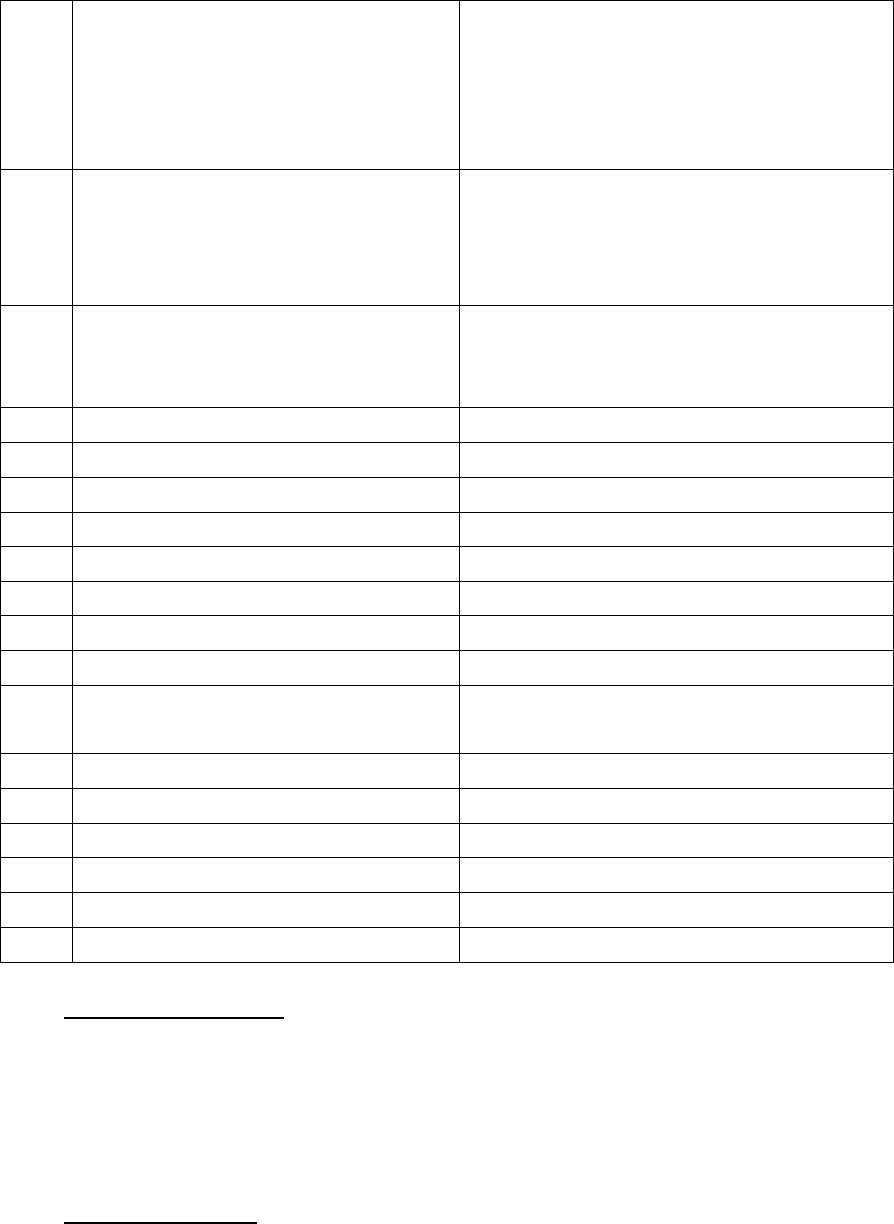
1.
Name & Address of the Complainant
Sh. Deshraj Anand
R/O 9 Rahul Vihar,
Govardhan Park,
West Dayal Bagh, Agra,
Uttar Pradesh – 282005.
2.
Policy No:
Type of Policy
Policy period
251100/50/21/10000230
Group Mediclaim Tailormade with
Floater Policy
01.11.2021 to 31.10.2022
3.
Name of the patient
Name of the policyholder
Name of Insured
Ms. Prakash Kumari, Spouse
Sh. Deshraj Anand
Indian Bank Retirees
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
--
6.
Reason for repudiation
--
7.
Date of receipt of the Complaint
22.02.2022
8.
Nature of complaint
Group Mediclaim
9.
Amount of Claim
Rs.32,396/-
10.
Date of Partial Settlement
Rs.20,980/- on 27.01.2022
11.
Amount of relief sought
Nothing mentioned in Annex. VI A
12.
Complaint registered under
Insurance Ombudsman Rule 2017
13 (1)b
13.
Date of hearing/place
20.04.2022 / NOIDA
14.
Representation at the hearing
a) For the Complainant
Sh. Deshraj Anand
b) For the insurer
Mr. R Bhatia, Manager, MCRO
15
Complaint how disposed
Award
16
Date of Award/Order
25.04.2022
17. Brief Facts of the Case:- The Complainant Sh. Deshraj Anand had taken Group Mediclaim
Tailormade with Floater Policy No. 251100/50/21/10000230 which was issued to the
Retired Employees of the Indian Bank for the period from 01.11.2021 to 31.10.2022. The
claim of the Complainant’s wife, Ms. Prakash Kumari was partially rejected by the
Insurance Company. Aggrieved, he requested the Insurer including its GRO to consider
the settlement of the claim but failed to get any relief. Thereafter, he has preferred a
complaint to this office for resolution of his grievance.
18. Cause of Complaint:-
a) Complainant’s argument:- Sh. Deshraj Anand, the Complainant stated in his complaint
that he had submitted the reimbursement claim of Rs.32,396/- which was settled by the
Insurance Company for Rs.20,980/- after deduction of Rs.11,416/- which is unjustified.
b) Insurers’ argument:- The Insurance Company stated in their SCN detailed the status of
claims of the above insured as under:
CLAIM NO. HH172271088, UNDER IBA POLICY 2021-22, PATIENT: PRAKASH KUMARI :
The claim wass related to the patient Ms. Prakash Kumari, aged 64 covered as spouse
of Sh. Deshraj Anand (retired employee of Indian Bank, Emp. Id 412984) in IBA policy.
● The patient was admitted for Right Eye Cataract in Netra Jyoti Kendra
(AGRA) on 26/12/2021 and discharged on 26/12/2021.
● They had received the reimbursement request of Rs.32,396/- for the above
mentioned treatment and accordingly they had registered the claim vide
CCN HH172271088.
● They had reviewed the claim based on the submitted documents and accordingly the
claim was settled for Rs.20,980/- and paid on 27/01/2022 vide UTR NO
KKBK220274832248 after making following deductions.
✔ Rs.695.00 on Bill No SR=490 dated 30/12/2021 (Medicines by Shop) - NO DOCTOR
ADVICE ENCLOSED.
✔ Rs.221.00 on Bill No SR=159 dated 24/12/2021 (Medicines by Shop) - NO DOCTOR
ADVICE ENCLOSED.
✔ Rs.10,500.00 on Bill No SR=674 dated 26/12/2021 (Medical Equipment) -
MAXIMUM AMOUNT PAYABLE AS PER REASONABLE & CUSTOMAR CLAUSE.
N.B:- They had taken into consideration of following hospital cataract rates in same region
for settlement of the case on an average basis:-
✔ Choudhary Eye Centre and Laser Vision-Rs.17000/-
✔ Fortis Vasant Kunj –Rs.19000/-
✔ Max healthcare – Rs.24000/-
19) Reason for Registration of Complaint: - Deduction in Mediclaim
20) The following documents were placed for perusal.
a) Customer complaint
b) Policy Copy
c) Annexure VI A
d) SCN
21) Observations and Conclusion :-
Both the parties appeared for personal hearing through video call and reiterated their
submissions. Sh. Deshraj Anand, the Complainant reiterated that he had submitted the
reimbursement claim of Rs.32,396/- which was settled by the Insurance Company for
Rs.20,980/- after deduction of Rs.11,416/- which is unjustified.
The Insurance Company reiterated that they had received the reimbursement request of
Rs.32,396/- for the treatment of Right Eye Cataract in Netra Jyoti Kendra. They had reviewed
the claim based on the submitted documents, and accordingly, the claim was settled for
Rs.20,980/- after deduction of Rs.11,416/-. Rs.695.00 and Rs.221.00 for medicines were
deducted because the insured did not provide any advice of the doctor. Rs.10,500.00 was
deducted on the basis of clause of reasonable and customary charges.
During the couse of hearing, it was asked to the Insurer that whether the treating hospital in
this case is PPN or not. The Insurer requested to check the same from their TPA. Therefore,
2 hours time was given to them to check the PPN status of the said hospital. But, the
Insurance Company did not revert till 21.04.2022.
On going through the documents exhibited and the oral submissions made during the
hearing, it was observed that deduction of Rs.10,500.00 was because of the REASONABLE
AND CUSTOMARY CHARGES. Rest of the deduction of Rs.695.00 and Rs.221.00 were due to
non submission of required documents. The Insurance Company could not provide the
confirmation regarding the PPN status of the above hospital. It is not the case of the
insurance company that the complainant did not pay the full amount to the hospital, nor are
they contending that the policy does not cover the expenses incurred by the insured.
Deduction based on R&C charges is quite unfair to the insured especially when there is no
dispute about his having paid the full amount to the hospital. Hence, it is directed to the
Insurance Company to pay the deducted amount of Rs.10,500.00 to the Complainant.
AWARD
Taking into account the facts and documents submitted and the oral submissions
made by both the parties during the course of hearing, it is directed to the
Insurance Company to pay the deducted amount of Rs.10,500.00 to the
Complainant.
The complaint is disposed off accordingly.
22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to
approach any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rules, 2017:

a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with
the award within thirty days of the receipt of the award and intimate compliance of the same
to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 25.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN –SH. C.S. PRASAD
CASE OF SH. AYUSH RASTOGI V/S NATIONAL INSURANCE CO.
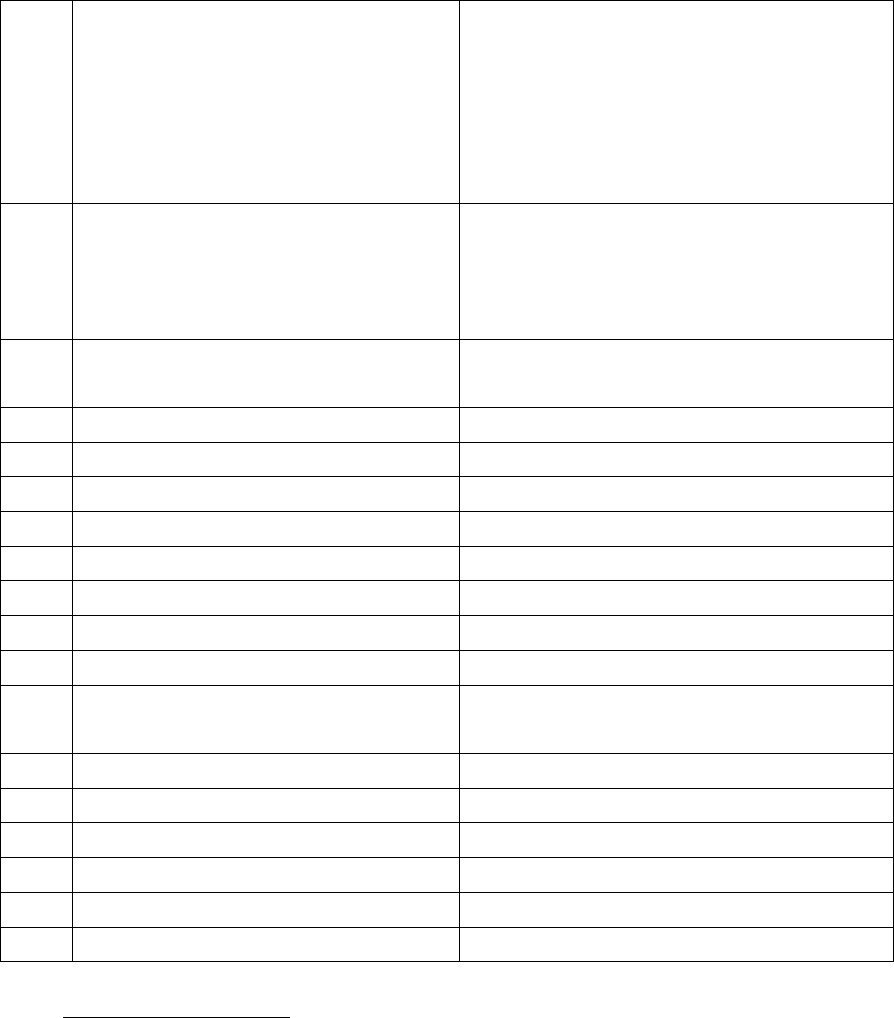
COMPLAINT REF. NO. : NOI-H-048-2122-0609
AWARD NO:
1.
Name & Address of the Complainant
Sh. Ayush Rastogi
E-1604, Saviour Green Arch,
Techzone-4, GH-10 A,
Amrapali Dream Valley,
Greater Noida,
Uttar Pradesh 201306.
2.
Policy No:
Type of Policy
Policy period
25110050****000403
Group Mediclaim Tailormade Policy
Bank of Baroda - Retirees
01.11.2020 to 31.10.2021
3.
Name of the insured
Name of the policyholder
Late Sh. Rajeev Kumar Rastogi
Bank of Baroda - Retirees
4.
Name of the insurer
National Insurance Co.
5.
Date of Repudiation
--
6.
Reason for repudiation
--
7.
Date of receipt of the Complaint
14.02.2022
8.
Nature of complaint
Group Mediclaim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Nothing mentioned in Annex VI A
12.
Complaint registered under
Rule of IOB rules,2017
13 (1) (b)
13.
Date of hearing/place
20.04.2022 /NOIDA
14.
Representation at the hearing
a) For the Complainant
Sh. Ayush Rastogi
b) For the insurer
Mr. R Bhatia, Manager, MCRO
15
Complaint how disposed
Award
16
Date of Award/Order
25.04.2022
17. Brief Facts of the Case : Late Sh. Rajeev Kumar Rastogi, the complainant’s father had taken
Group Mediclaim Tailor made Policy No.25110050****000403 commencing from
01.11.2020 to 31.10.2021, which was issued to Bank of Baroda - Retirees. The Insurance
Company had not paid the claim of the complainant’s father. Aggrieved, he requested the
insurer including its GRO to settle his claim but failed to get any relief. Thereafter, he has
preferred a complaint to this office for resolution of his grievance.
18. Cause of Complaint:
a) Complainant’s argument: The complainant Sh. Ayush Rastogi stated in his complaint that
his father Late Sh. Rajeev Kumar Rastogi,a Retired Bank of Baroda employee who died on
18th May 2021. His medical Insurance was from National Insurance (corporate Insurance)
for which they had claimed the hospital expenses and awaiting for a response from the
insurance company for the past more than 3 months. They have submitted all the hospital
related documents on 23rd of October, 2021.
b) Insurers’ argument: The Insurance Company in their SCN confirmed that the claim details
as under:
Policy Holder : BANK OF BARODA_IBA
Policy No : 251100502010000403_Without Domiciliary
Policy Period : 01/11/2020 To 31/10/2021
Primary Beneficiary : Rajeev Kumar Rastogi
Beneficiary : Rajeev Kumar Rastogi (Self)
Sum Insured : Rs.4,00,000 /-
Insurer : National Insurance Co. Ltd.
Claim type : Reimbursement
MAID : 5030899812
Claim No : 26283717
Claim Amount : Rs. 584134/-
The claim was presented for hospitalization of late Mr Rajeev Rastogi for the treatment of
COVID 19 for the period from 04/05/2021 to 18/05/2021 at Surya Multispeciality Hospital
And Trauma Centre, Meerut. The total expenses was Rs.5,84,134/- and partial claim
settled by Star Health Insurance for Rs.3 lakhs. Remaining Rs.2,84,134/- was claimed
under IBA policy.
However, on physical verification at the Surya Multispeciality and trauma centre, the
hospital, during the 1st Visit mentioned that the hospital authority was out of station,
hence, they revisited the hospital, but the hospital mentioned the same. Hence, they
traced the treating doctor Dr. A Sharma at his dispensary and he confirmed in writing that
the patient was not treated by him and also Dr. Nishant Wadhera confirmed that he has
not seen any Covid patient.
● Treating doctor letter confirms that this patient was not seen by him but discharge
summary has same doctor seal & sign and also Star health insurance seal & sign. The
treating doctor letter is presented for reference.
● The Dr. A Sharma’s registration number also tallies on the discharge summary and the
letter provided by the doctor, there is a possibility that the hospital is involved too in this
case.
Hence, the claim is repudiated under clause 6.4 of the policy.
19) Reason for Registration of Complaint:- Mediclaim rejected
20) The following documents were placed for perusal:-
a) Complaint copy
b) Policy copy
c) SCN
d) Annexure VI A
21. Observations & Conclusion :-
Both the parties appeared for personal hearing through video call and reiterated their
submissions. The complainant Sh. Ayush Rastogi reiterated that his father was diagnosed as
COVID and hospitalized for the period from 04.05.2021 to 18.05.2021 at Surya
Multispeciality Hospital, Meerut. Later, he died on 18th May 2021. But the Insurance
Company did not pay his claim.
The Insurance Company clarified that The total expenses was Rs.5,84,134/- and partial claim
settled by Star Health Insurance for Rs.3 lakhs. Remaining Rs.2,84,134/- was claimed under
their IBA policy. During their investigation, the treating doctor Dr. A Sharma confirmed in
writing that the patient was not treated by him and also Dr. Nishant Wadhera confirmed
that he had not seen any Covid patient. Therefore, the claim was rejected.
During the course of hearing, it was directed to the Insurer to reinvestigate the claim and
provide us their final decision. The Insurer confirmed vide their mail dated 21.04.2022 that
after reviewing the claim, the admissible claim amount comes to Rs.2,67,663/-.
Ongoing through the documents exhibited and the oral submissions made by both the
parties, it is observed that at the time of hospitalization of the Insured, there was very poor
condition in all the hospitals due to the pandemic. Due to the overburden on the doctors, it
was not easy for any doctor to provide the record of his each patient. Therefore, it was
directed to the Insurer to review the claim. The Company is ready to pay rest of the amount
of Rs.2,67,663/- to the complainant. Hence, it is directed to the Insurer to pay the claim to
the complainant as offered by them.
AWARD
Taking into account the facts and the submissions made by both the parties during the
course of hearing, it is directed to the Insurer to pay the claim to the complainant as
offered by them to our office.
The complaint is disposed off accordingly.

22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to
approach any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with
the award within thirty days of the receipt of the award and intimate compliance of the same to
the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 25.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN –SH. C.S. PRASAD
CASE OF SH. KULVANT JAIN V/S. CARE HEALTH INSURANCE. CO.
COMPLAINT REF. NO. : NOI-H-037-2122-0615
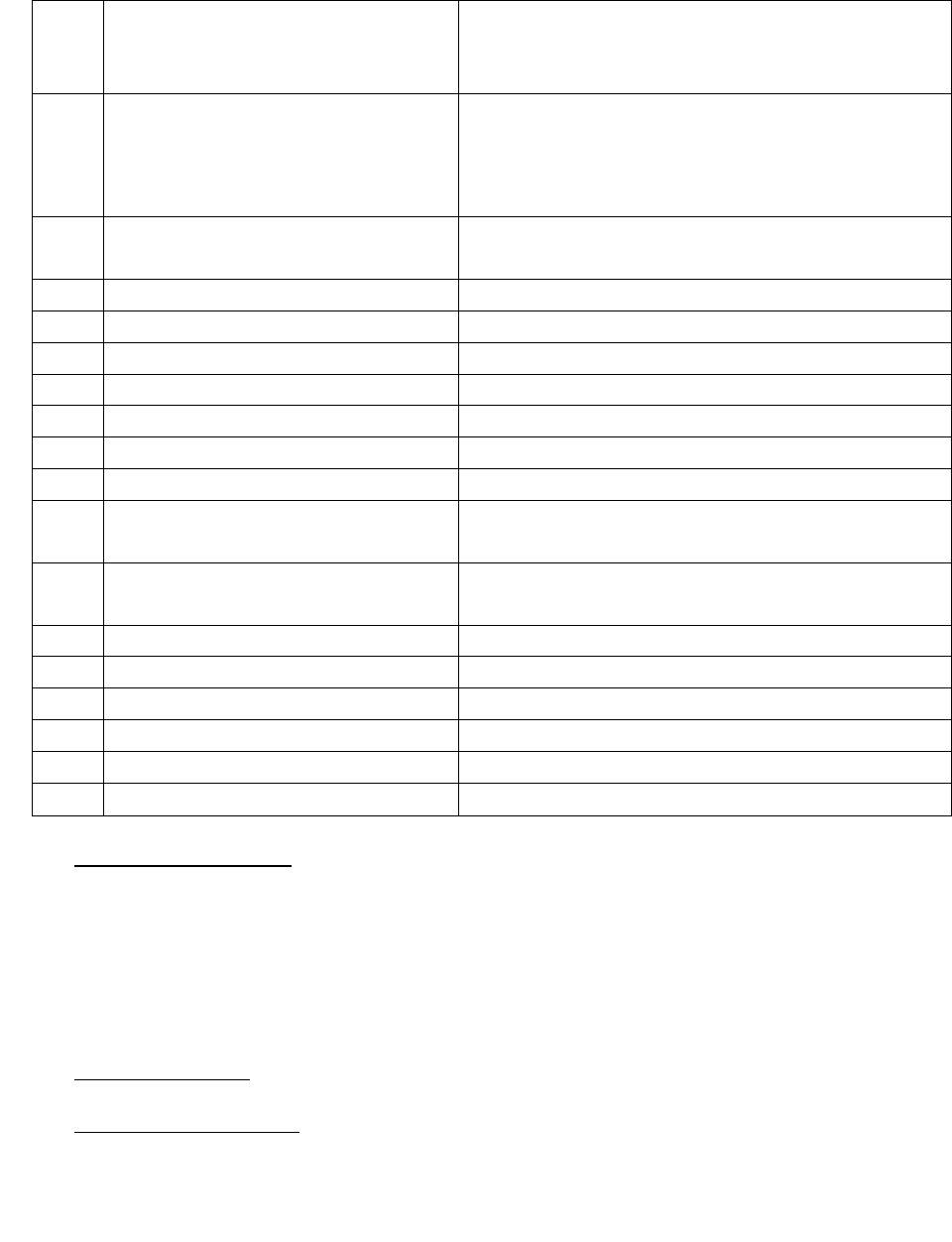
AWARD NO:
1.
Name & Address of the Complainant
Sh. Kulvant Jain
F-34, Sector-39, Noida,
Uttar Pradesh - 201301.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Sum Insured
1741**64
Group Care (PNB) Policy
26.05.2021 to 25.05.2022
Rs.10,00,000/-
3.
Name of the insured
Name of the policyholder
Sh. Kulvant Jain
Punjab National Bank
4.
Name of the insurer
Care Health Insurance Co.
5.
Date of Repudiation
08.11.2021
6.
Reason for repudiation
Non disclosure of material facts / PED
7.
Date of receipt of the Complaint
22.02.2022
8.
Nature of complaint
Group Mediclaim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.15,37,584/- restricted to S.I. of Rs.10,00,000/- +
Rs.51,000/- for legal fee as per Annex VI A
12.
Complaint registered under
Rule of IOB rules,2017
13 (1) (b)
13.
Date of hearing/place
20.04.2022 /NOIDA
14.
Representation at the hearing
a) For the Complainant
Sh. Kunal Jain, son of the complainant
b) For the insurer
Dr. Samiksha, Manager (Claims)
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
20.04.2022
17. Brief Facts of the Case : Sh. Kulvant Jain, the complainant had taken Group Care (PNB) Policy
No.11561922 which was issued to the Punjab National Bank and the complainant was covered
under Certificate No.1741**64 commencing from 26.05.2021 to 25.05.2022 was issued for a S.I.
of Rs.10,00,000/-. The Insurance Company rejected his claim on the basis of non disclosure of
material facts/PED. Aggrieved, he requested the insurer including its GRO to reconsider the claim
but failed to get any relief. Thereafter, he has preferred a complaint to this office for resolution
of his grievance.
18. Cause of Complaint:
a) Complainant’s argument : The complainant Sh. Kulvant Jain stated in his complaint that he has
been continuously covered in the Mediclaim policy under New India Assurance Co. Ltd. Since 2004
or so. In the year 2020-21, he migrated to Care Insurance Policy for the period from 26.05.2020
to 25.05.2021 and further renewed on 26.05.2021.
He had a major fall at home on 12.07.2021, which severely affected his memory and led to
slowness of activity and difficulty in speaking. He got admitted on 18.07.2021 at Apollo Hospital
with acute severe abdominal pain and gastritis. The Apollo Hospital has clearly mentioned in its
Discharge Summary that he had a recent head trauma due to fall. He got discharged on
20.07.2021.
He was again admitted on 08.09.2021 in Fortis Hospital for further management. The hospital
has recorded an incidental finding of Left MCA Bifurcation aneurysm and Right Parafalcine
meningioma. He underwent Left Fronto-parietal mini craniotomy procedure and got discharged
on 11.09.2021. The hospital bill was Rs.8,35,345/- which was totally denied by the Care Health
Insurance.
After 3 days of discharge, he had a seizure and again on 19.09.2021, he had a fall in the bathroom
and further he again got admitted on 21.09.2021 to 30.09.2021. On 22.09.2021, a procedure of
re exploration + endoscopy assisted subdural haematoma evacuation under MOAC was done and
finally, he got discharged on 30.09.2021 and the bill amount was Rs.6,39,037/-.
He submitted his pre and post claim of Rs.58,202/- on 01.10.2021, which was also denied by the
Care Health Insurance.
As per Doctor letter dated 09.09.2021, there was incidental finding of Left MCA bifurcation
aneurism and right Parafalcine Meningioma in 2008, and both were asymptomatic. So no drugs
were taken by him in last 13 years which is duly certified by the doctor. The water accumulation
in the brain was due to fall at home and not because of any pre-existing condition. But, the
Insurer rejected his claim of account of non-disclosure.
b) Insurers’ argument: The Company in their SCN stated that
1. The Company had issued a Health Insurance Policy through Punjab National Bank (Group Care)
vide Policy No.11561922 wherein the Insurance coverage was provided to the Complainant Mr.
Kulvant Jain and his wife- Mrs. Deepa Jain(hereinafter called as ‘Insured’) for a sum insured of
Rs.10,00,000/- with subject to the Policy terms and conditions. The said Policy was issued on 26
th
May 2020 till 25
th
May, 2021. The policy was lastly renewed on 26
th
May 2021 till 25
th
May 2022.
The policy documents were duly delivered to the policyholder’s addresses and no dispute
regarding the policies were raised by the complainant / Policy holder during the free-look period
as per the policy term and conditions.
2. During the continuation of the policy, the Complainant approached the Respondent Company on
28
th
October, 2021 with a Reimbursement Claim (Claim no.91963269) for the hospitalization
expenses incurred on the treatment of Complainant Mr.Kulvant Jain from 21
st
September 2021
to 30
th
September 2021 for recurrent left acute on chronic subdural hematoma.
3. During the internal investigation to check the veracity of the claims, it was observed in admission
history of the Fortis Hospital that the complainant had pre-existing ailment i.e. MENINGIOMA
AND MCA ANEURYSM in the year 2008 and the time of policy inception in the year 2020 same
was not disclosed to the respondent company.

4. Therefore the said reimbursement claim was rejected vide Denial Letter Dated 8
th
November
2021 as per Policy Terms and Conditions under Clause 5.2-Disclosure to Information Norm. The
relevant clause is reproduced herein below for your reference:
5.2 Disclosure to Information Norm
“The policy shall be void and all premium paid thereon shall be forfeited to the Company in the
event of misrepresentation, mis-description or non-disclosure of any material fact by the
policyholder”
5. The complainant in accordance to the tenets of insurance law was duty bound to disclose all the
material facts with respect to medical history. The complainant had the opportunity to declare
the true state of health to the respondent company in the proposal form duly filled by the
complainant but the same was not disclosed by the complainant for the reasons best known to
him. The proposer/complainant was asked the following questions in the proposal form:
● Has anyone been diagnosed/ hospitalized or is currently under investigation for cancer/
diabetes/ stroke/ heart disease/ kidney disease/ liver disease/ hypertension (blood pressure)
The answer was marked “YES” and it was further stated by the insured that he is a diabetes
patient from last two years
● Has the insured member ever got hospitalized due to any reason apart from common cough/
cold/ fever or ever undergone an surgery?
The answer was marked “NO” by the insured himself.
● Does the insured member use any recreational drugs or consume more than 5 cigarettes and/
or 4 units of alcohol per day?
The answer was marked “NO” by the insured himself.
In reference to the above mentioned facts it was observed by the respondent company that the
insured was having history of MENINGIOMA AND MCA ANEURYSM which was not disclosed
during the inception of the policy with the respondent company was classified as “Non-disclosure
of material facts”. It is pertinent to mention that even when the insured had the opportunity to
disclose the material fact however he chose to disclose it partially by stating about diabetes only.
6. It is pertinent to mention that MENINGIOMA AND MCA ANEURYSM are dropped risk as per the
underwriting guidelines of the Product-Group Care. If insured would have disclosed
MENINGIOMA AND MCA ANEURYSM at the time of proposal then the respondent company would
have rejected the proposal out rightly and would have not issued the policy.
7. It is humbly submitted that insured filed a grievance with the respondent company wherein it was
stated to the complainant on the basis of the clarification provide by the complainant maintains
its decision on claim rejection.
8. That in light of the above, it is reiterated that the Reimbursement Claims of the Complainant was
duly repudiated by the Respondent Company as per the Policy Terms and Conditions and there is
no deficiency in service on the part of the Respondent Company.
9. That In the Export Credit Guarantee Corp of India Ltd. Versus M/s Garg Sons International
pronounced by the SUPREME COURT OF INDIA that the“The insured cannot claim anything more
than what is covered by the insurance policy. “…the terms of the contract have to be construed
strictly, without altering the nature of the contract as the same may affect the interests of the
parties adversely.” The clauses of an insurance policy have to be read as they are…
Consequently, the terms of the insurance policy, that fix the responsibility of the Insurance
Company must also be read strictly. The contract must be read as a whole and every attempt
should be made to harmonize the terms thereof, keeping in mind that the rule of contra
proferentem does not apply in case of commercial contract, for the reason that a clause in a
commercial contract is bilateral and has mutually been agreed upon. (Vide : Oriental Insurance
Co. Ltd. v. Sony Cheriyan AIR 1999 SC 3252; Polymat India P. Ltd. v. National Insurance Co. Ltd.,
AIR 2005 SC 286; M/s. Sumitomo Heavy Industries Ltd. v. Oil & Natural Gas Company, AIR 2010
SC 3400; and RashtriyaIspat Nigam Ltd. v. M/s. Dewan Chand Ram Saran AIR 2012 SC 2829).”
Hence it is humbly submitted that all averments to the contrary in the complaint are denied, and
hence it is prayed that the Hon’ble Ombudsman may kindly be pleased to accept this self-
contained note and the complaint may be dismissed.
19) Reason for Registration of Complaint:- Rejection of Mediclaim
20) The following documents were placed for perusal:-
a) Policy Copy
b) Annexure VI A
c) SCN
d) Complaint copy
21) Observations and Conclusion :-
Both the parties appeared for personal hearing through video call and reiterated their submissions.
Sh. Kunal Jain, son of the complainant attended the hearing on behalf of the complainant and
reiterated that his father’s hospitalization was a case of neuro complication arising out of the fall at
home on 12.07.2021 which was rejected by the Company on the ground of non disclosure of material
facts/PED. As per Doctor letter dated 09.09.2021, there was incidental finding of Left MCA
bifurcation aneurism and right Parasaggital Meningioma in 2008, and both were asymptomatic. So
no drugs were taken by him in last 13 years which is duly certified by the doctor. The water
accumulation in the brain was due to fall at home and not because of any pre-existing condition. But,
the Insurer rejected his claim of account of non-disclosure.
The Insurance Company clarified that the repudiation of the claim was not an arbitrary decision but
based on the investigation to check the veracity of the claims. It was observed in admission history
of the Fortis Hospital that the complainant was diagnosed with MENINGIOMA AND MCA ANEURYSM
in the year 2008 and the time of policy inception in the year 2020, the same was not disclosed to the
respondent company. If insured would have disclosed MENINGIOMA AND MCA ANEURYSM at the
time of proposal then the respondent company would have rejected the proposal out rightly and
would have not issued the policy.
I have examined the documents exhibited and the oral submissions made by both the parties. It is
observed that the Insurance Company repudiated the claim on the basis of MENINGIOMA AND MCA
ANEURYSM as PED since 2008 which is the main reason of the present hospitalization of the Insured.
The Insurance Company has submitted their doctor Dr. Khush Preet Singh’ letter dated 16.03.2022
wherein he has clearly stated that MENINGIOMA AND MCA ANEURYSM were dropped risk as per the
underwriting guidelines of the Product-Group Care. If the insured had disclosed MENINGIOMA AND

MCA ANEURYSM at the time of proposal, then the respondent company would have rejected the
proposal out rightly and would have not issued the policy.
The Insured has also submitted the treating doctor’s letter dated 09.09.2021, there was incidental
finding of Left MCA bifurcation aneurism and right Parasaggital Meningioma in 2008, and both were
asymptomatic. The certificate cannot be taken as an indisputable proof because it does not contain
the stamp of the Doctor, and also, there is no mention of doctor’s MCI Registration number. we
cannot examine the doctor for evidence on record. The Insurer’s action of repudiating the claim in
the light of the opinion given to them by the independent doctor cannot be termed unjustified and
arbitrary. Moreover, in view of the conflicting opinions, it will be difficult to reach any conclusion
unless both the professionals are subjected to examination in chief and cross examination. Such
examination is beyond scope of this forum. The complainant may approach any suitable forum where
justice can be ensured after examination of both the medical examiners. The complaint is dismissed.
22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
Place: Noida. C.S. PRASAD
Dated: 20.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
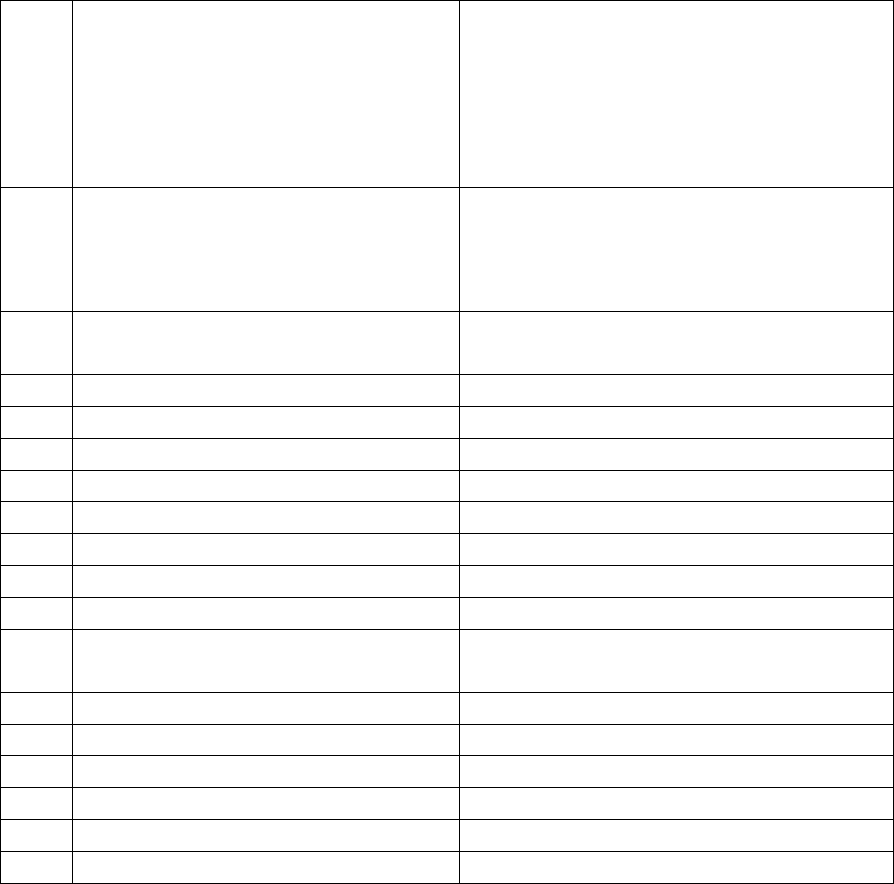
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF SH. PUSHKAR SINGH BADWAL V/S NATIONAL INSURANCE CO. LTD.
COMPLAIN REF. NO.: NOI-H-048-2122-0676
AWARD NO:
1.
Name & Address of the Complainant
Sh. Pushkar Singh Badwal
C/O S/O Jaman Singh Badwal
AH 102, 1
st
Floor, Raj Empire,
Rajnagar Extension,
Morti, Ghaziabad,
Uttar Pradesh-201003.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
25110050**10000252
Group Mediclaim Tailor Policy
(Punjab National Bank Employees)
01.10.2020 to 30.09.2021
3.
Name of the Insured
Name of the policyholder
Sh. Pushkar Singh Badwal
Sh. Pushkar Singh Badwal
4.
Name of the insurer
National Insurance Company Limited
5.
Date of Repudiation
--
6.
Reason for repudiation
--
7.
Date of receipt of the Complaint
10.01.2022
8.
Nature of complaint
Group Mediclaim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.54,197.33 as per Annex VI A
12.
Complaint registered under
IOB rules, 2017
13 (1)(b)
13.
Date of hearing/place
20.04.2022 / NOIDA
14.
Representation at the hearing
a) For the Complainant
Sh. Pushkar Singh Badwal
b) For the insurer
Mr. R Bhatia, Manager, MCRO
15.
Complaint how disposed
Award
16.
Date of Award/Order
20.04.2022
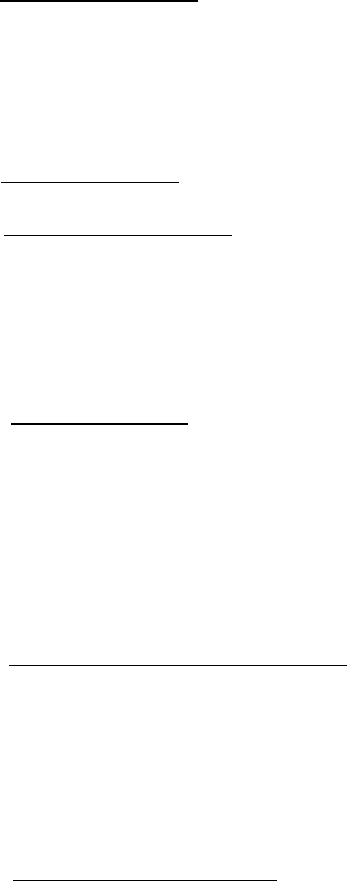
17. Brief Facts of the Case:- Sh. Pushkar Singh Badwal, the Complainant had taken Group Mediclaim Tailor
Policy (Punjab National Bank Employees) No. 25110050**10000252 for the period from 01.10.2020
to 30.09.2021. The Group Mediclaim Policy was issued to Punjab National Bank Employees covering
their Employees. The reimbursement of bills was partially settled by the Insurance Company.
Aggrieved, he requested the Insurer including its GRO to reconsider the claim but failed to get any
relief. Thereafter, he has preferred a complaint to this office for resolution of his grievance.
18. Cause of Complaint:-
a) Complainant’s argument:- Sh. Pushkar Singh Badwal, the Complainant stated in his complaint that
the partial payment made by the Insurer wherein the total bill amount was Rs.71,914/-, out of which
he had to pay an amount of Rs.38,480/-. After having a telephonic conversation, the representative
told him to claim the amount after the surgery. Upon claiming the amount which included
consultation fee + pharmacy + investigation fee and treatment, the total bill amount was of
Rs.54,197.33.
b) Insurers’ argument:- The Insurance Company stated in their SCN that the claim of Mr. Pushkar
Badwal under Punjab National Bank staff mediclaim policy 2020-21. The insured have taken
treatment at Centre for Sight, New Delhi on 13
th
August 2021 for Left eye (Cortical age-related
cataract) and they have authorized cashless for same. The insured ailment disease diagnosis
was CATRACT WITH PDRWITH DME and the procedure underwent is LE EYE MICS WITH
INTRAVITREAL INJECTION which means two procedures. As we have paid for cataract procedure
charges of Rs. 34,000/-, further amount of Rs. 42,897/- is also payable including for pre-post
hospitalization expenses.
19) Reason for Registration of Complaint: - Partial settlement of Mediclaim
20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN
21. Observations & Conclusion :-
Both the parties appeared for personal hearing through video call and reiterated their submissions.
The complainant Sh. Pushkar Singh Badwal reiterated that the total bill amount was Rs.71,914/-, out
of which the Company had deducted the amount of Rs.54,197.33.
The Insurance Company reiterated that they have paid for cataract procedure charges of Rs.34,000/-
to the complainant, and further amount of Rs. 42,897/- is also payable including for pre-post
hospitalization expenses.
Ongoing through the documents exhibited and the oral submissions made by both the parties, it is
observed that the Company is ready to pay rest of the amount of Rs. 42,897/- to the complainant.
Hence, it is directed to the Insurer to pay the claim to the complainant as offered by them during the
course of hearing.
AWARD
Taking into account the facts and the submissions made by both the parties during
the course of hearing, it is directed to the Insurer to pay the claim to the complainant
as offered by them during the course of hearing.
The complaint is disposed off accordingly.
22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with the award
within thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 20.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN –SH. C.S. PRASAD
CASE OF SH. SANKET KACHROO V/S. CARE HEALTH INSURANCE. CO.
COMPLAINT REF. NO. : NOI-H-037-2122-0578
AWARD NO:
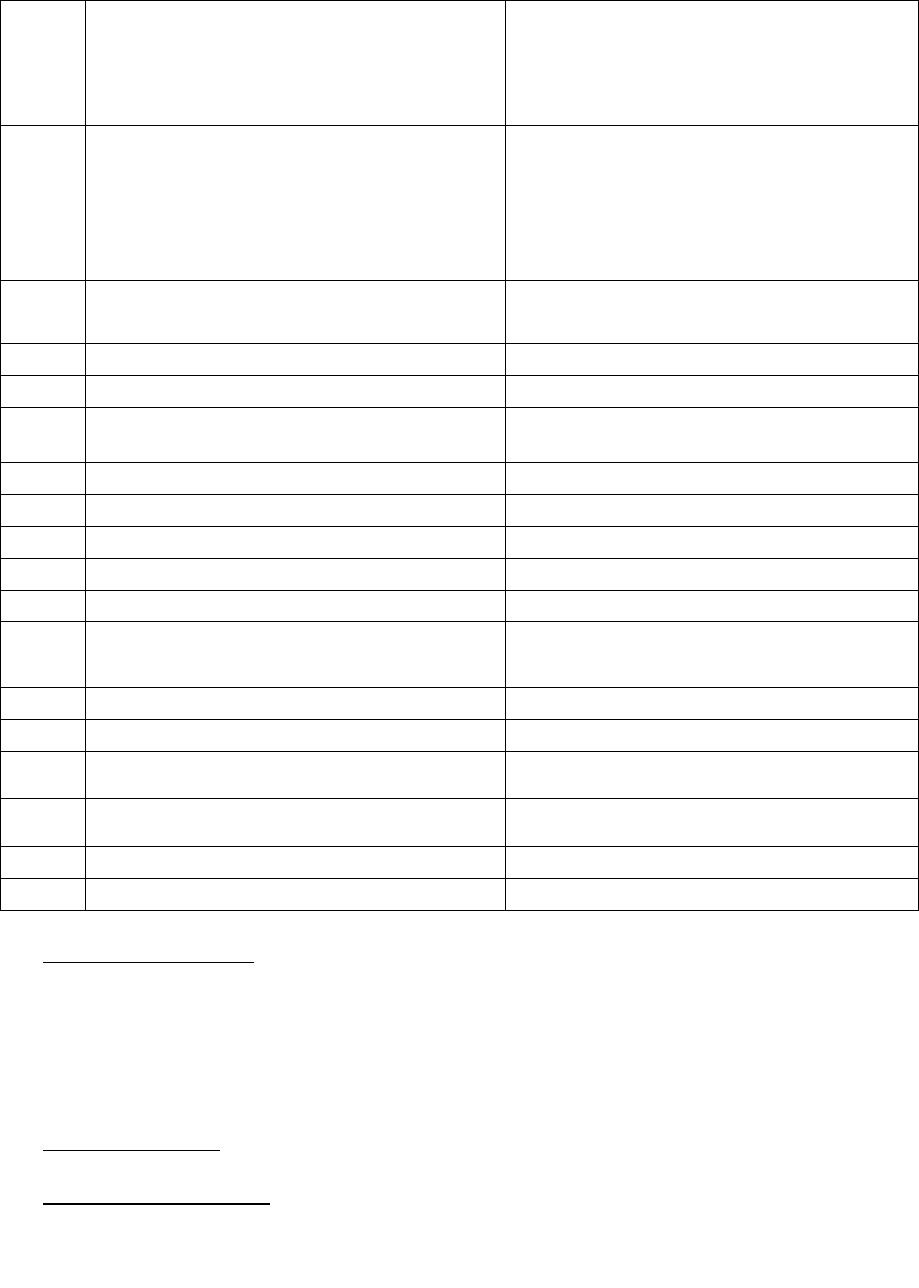
1.
Name & Address of the Complainant
Sh. Sanket Kachroo
E-1805, Ajnara, Genxx,
Crossing Republic, Ghaziabad,
Uttar Pradesh-201016.
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Sum Insured
19189418
Group Care 360* (PNB Platinum) Policy
09.12.2021 to 08.12.2022
Rs.10,00,000/-
3.
Name of the insured
Name of the policyholder
Late Sh. Tej Kishan Kachroo
Punjab National Bank
4.
Name of the insurer
Care Health Insurance Co.
5.
Date of Repudiation
08.09.2021
6.
Reason for repudiation
Rejected due to 3 years waiting period
7.
Date of receipt of the Complaint
01.02.2022
8.
Nature of complaint
Group Mediclaim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.2,78,888/- as per Annex VI A
12.
Complaint registered under
Rule of IOB rules,2017
13 (1) (b)
13.
Date of hearing/place
11.04.2022 /NOIDA
14.
Representation at the hearing
a) For the Complainant
Sh. Sanket Kachroo
b) For the insurer
Dr. Samiksha, Manager (Claims)
15
Complaint how disposed
Dismissed
16
Date of Award/Order
20.04.2022
17. Brief Facts of the Case : The father of the Complainant Sh. Sanket Kachroo had taken Group Care
360* (PNB Platinum) Policy No. 19189418 commencing from 09.12.2021 to 08.12.2022 was
issued for a S.I. of Rs.10,00,000/- which was issued to Punjab National Bank. The Insurance
Company rejected his father Late Sh. Tej Kishan Kachroo’s claim. Aggrieved, he requested the
insurer including its GRO to reconsider the claim but failed to get any relief. Thereafter, he has
preferred a complaint to this office for resolution of his grievance.
18. Cause of Complaint:
a) Complainant’s argument : The complainant Sh. Sanket Kachroo stated in his complaint that his
father’s hospitalization was a case of management of Transient loss of consciousness (TLoC) as a
result of an epileptic seizure and an uncomplicated faint occurred to him on 07.09.2021 in the
society park. Generally, Seizure is the major symptom of a ruptured brain aneurysm as it results
from a sudden burst of excess electrical activity in the brain. He has experienced a blackout due
to a drop in blood pressure and untimely the amount of oxygenated blood to the brain due to the
sudden onset of fainting due to the seizure.
He was rushed to the nearest Columbia Hospital and finally shifted to the Apollo Hospital from
08.09.2021 to 12.09.2021. The Apollo has diagnosed the case of Subarachnoid Hemorrhage a
medical emergency from building blood vessels that burst in the brain (aneurysm). The Cranial
CT Scan (Brain Scan) diagnostic test revealed the case of aneurysm rupture. The treating Dr.
Pranav Kumar has also confirmed that he has SAH. It is not because of Hypertension. But, the
Insurance Company has denied the claim as they had arbitrarily related the cause of death as
Hypertension which has 36 months waiting period under the policy.
b) Insurers’ argument: The Insurance Company stated in their SCN that a Health Insurance Policy
namely “Group Care 360° (PNB-Platinum)” bearing Group Policy No. 17499225 with Certificate of
Insurance No. 19189418 from 09-12-2020 till 08-12-2021 was issued to Sh. Tej Kishan Kachroo
(hereinafter referred to as the “Insured”) wherein insurance coverage was provided to the Insured
and his spouse Ms. Basanti Kachroo for a sum insured up to Rs. 10,00,000/ subject to policy terms
and conditions. Thereafter, the policy was again renewed from 09-12-2021 till 08-12-2022. Both
the Insured persons had disclosed pre-existing disease of Hypertension at the time of taking the
policy.
1. The Respondent Company received a cashless request (80571225) for the hospitalization of the
Insured at Indraprastha Apollo Hospital on 07-09-2021 and was provisionally diagnosed with
Aneurysm/Subarachnoid Hemorrhage (SAH).
It is pertinent to mention that “Hypertension is directly related to Aneurysm /Subarachnoid
Haemorrhage as it is one of the most important risk factors for SAH. That High blood pressure
(Hypertension) can cause thin-walled arteries to rupture, releasing blood into the brain tissue and
higher levels of blood pressure are linearly and positively associated with higher risks of Aneurysm
/SAH.”
As it is further pertinent to mention that as per Benefit 18 mentioned in the policy certificate there
is a 36 month waiting period from the date of policy inception for any treatment related to pre-
existing diseases.
Therefore, the case was rejected vide letter dated 08-09-2021 on the basis of 3 year Waiting Period
is applicable for pre-existing diseases and its related complications (HTN related complication).
2. Thereafter, the Respondent Company received a reimbursement claim (91920912) for the
hospitalization of the Insured at Indraprastha Apollo Hospital from 08-09-2021 till his date of death
i.e. 12-09-2021 due to Aneurysm/Subarachnoid Hemorrhage.
The reimbursement claim was also rejected on the basis of observation made during the cashless
request vide letter dated 16-10-2021 on the basis of 3 Year Waiting Period is applicable for pre-
existing diseases and its related complications (HTN related complication).
3. The Respondent Company also took an Expert Opinion to substantiate the fact that the present
ailment of the Insured is attributed to pre-existing disease of Hypertension and current ailment of
Aneurysm/Subarachnoid Hemorrhage (SAH). In this aspect as per the Expert Opinion appended by
Dr. C. H. Asrani, given “There is an established and well accepted direct cause effect correlation
between hypertension and subarachnoid hemorrhage.”.
4. The Respondent Company also received grievance from the Complainant regarding the rejection of
the claim. The same was replied via email dated 28-01-2022.
5. The Complainant is contending in the Complaint that the repudiation of claim by the Respondent
Company is not justified and there is deficiency in service on the part of the Respondent Company.
The Respondent Company however, humbly denies the above stated averments.
6. In the Export Credit Guarantee Corp. of India Ltd. Versus M/s Garg Sons International pronounced
by the Supreme Court of India that
“11. The insured cannot claim anything more than what is covered by the insurance policy. “…the
terms of the contract have to be construed strictly, without altering the nature of the contract as the
same may affect the interests of the parties adversely.” The clauses of an insurance policy have to
be read as they are… Consequently, the terms of the insurance policy, that fix the responsibility of
the Insurance Company must also be read strictly. The contract must be read as a whole and every
attempt should be made to harmonize the terms thereof, keeping in mind that the rule of contra
proferentem does not apply in case of commercial contract, for the reason that a clause in a
commercial contract is bilateral and has mutually been agreed upon. (Vide : Oriental Insurance Co.
Ltd. v. Sony Cheriyan AIR 1999 SC 3252; Polymat India P. Ltd. v. National Insurance Co. Ltd., AIR 2005
SC 286; M/s. Sumitomo Heavy Industries Ltd. v. Oil & Natural Gas Company, AIR 2010 SC 3400; and
RashtriyaIspat Nigam Ltd. v. M/s. Dewan Chand Ram Saran AIR 2012 SC 2829).”
In the New India Assurance Company Ltd. vs. Rekha Malhotra pronounced by National
Commission 2016(4) C.P.R. 455:
“In the matter at hand, the insured was issued medical cover with a condition that any claim related
to pre-existing ailments of diabetes and hypertension will not be paid for two years from the
inception of the policy. The National Commission while reversing the order of the State Commission
said that since admittedly the claim under the policy was preferred within a period of two years and
as a matter of fact within two months of obtaining the same, it was squarely covered under the
Exclusion Clause of the waiting period.”
Thus, in light of the above stated contentions and averments it is submitted that the claim of the
Insured has been rightly repudiated by the Respondent Company in strict adherence to the Policy
Terms and Conditions and as such there is no deficiency in service on the part of the Respondent
Company.
19) Reason for Registration of Complaint:- Rejection of Mediclaim
20) The following documents were placed for perusal:-
a) Policy Copy
b) Annexure VI A
c) SCN
d) Complaint copy
21) Observations and Conclusion :-

Both the parties appeared for personal hearing and reiterated their submissions. Sh. Sanket Kachroo
reiterated that his father’s hospitalization was a case of Subarachnoid Hemorrhage a medical
emergency from building blood vessels that burst in the brain (aneurysm). The treating Dr. Pranav
Kumar has also confirmed that he has SAH. It is not because of Hypertension. But the Insurance
Company has denied the claim as they had arbitrarily related the cause of death as Hypertension
which has 36 months waiting period under the policy.
The Insurance Company clarified that the repudiation of the claim was not an arbitrary decision but
based on the report of Dr. C.H. Asrani which has clearly established that the Hypertension has direct
cause effect relationship with SAH. Since, Hypertension and its related complications are excluded
for 36 months under the policy conditions, the claim was repudiated within the framework of the
policy.
I have examined the documents exhibited and the oral submissions made by both the parties. It is
observed that the Insurance Company repudiated the claim on the basis of opinion by a professional
doctor on the basis of documents shown to him. The complainant has submitted the treating doctor’s
opinion to the contrary. In light of conflicting professional opinions, the Insurance Company was
asked to consider the case once again. The Insurer has submitted their reply vide mail dated
12.04.2022 informing their inability to review their decision in view of the fact that treating doctor’s
opinion was submitted to the Insurer post rejection of the claim and is an afterthought. As there are
conflicting professional opinions on record, it will be difficult to reach to any conclusion unless both
the professionals are subjected to examination and cross examination. Such examination is beyond
scope of this forum. The complainant may approach any suitable forum where justice can be ensured
after examination of both the medical examiners. The complaint is dismissed.
22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
Place: Noida. C.S. PRASAD
Dated: 20.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES, 2017
OMBUDSMAN – SH. C.S. PRASAD
CASE OF MS. PRABHA SINGH V/S. BAJAJ ALLIANZ GENERAL INS. CO. LTD.
COMPLAINT REF. NO. : NOI-H- 005-2122-0600
AWARD NO:
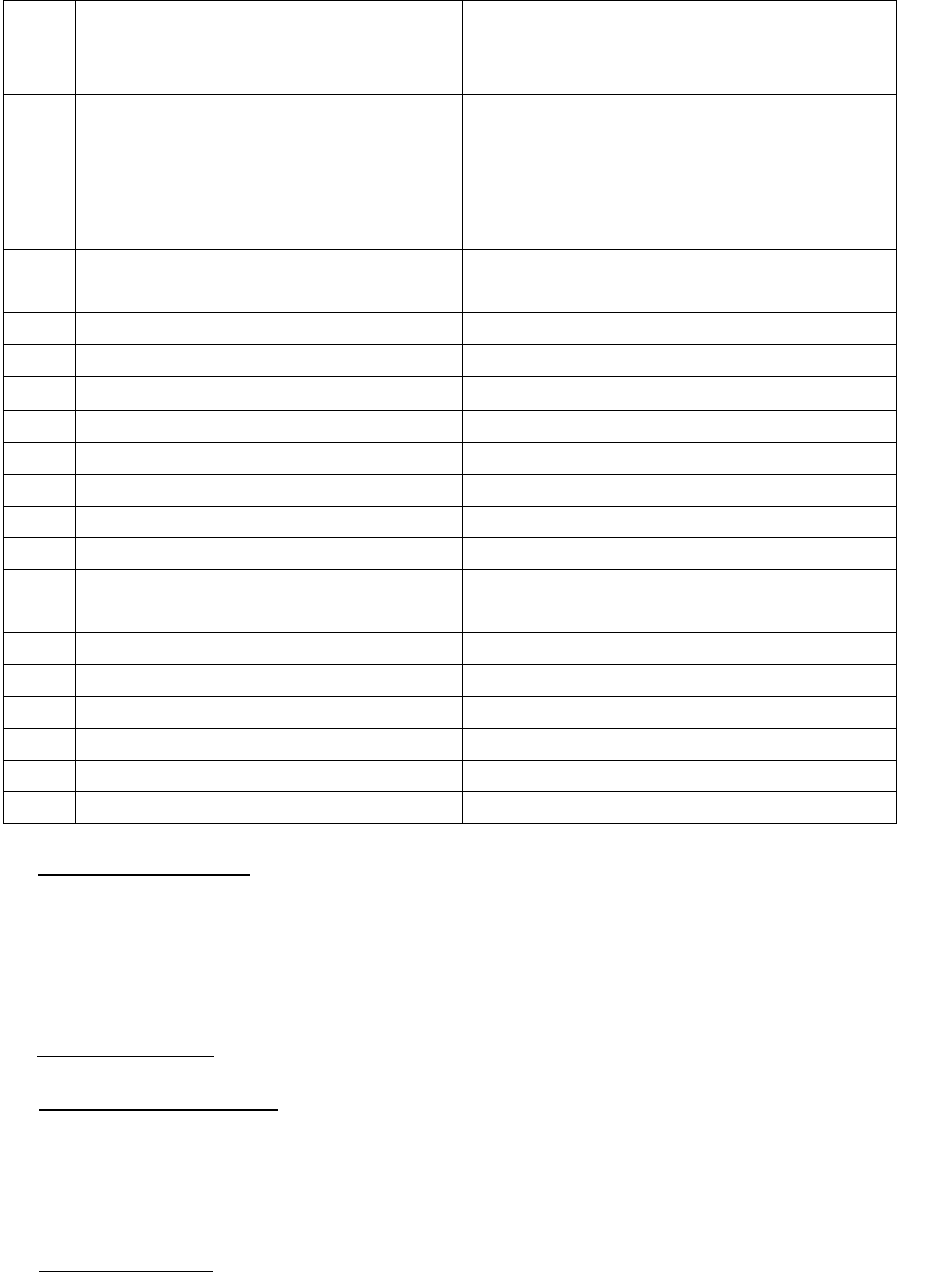
1.
Name & Address of the Complainant
Ms. Prabha Singh
C-39, Kamla Nagar, Agra,
Uttar Pradesh-282005.
2.
Policy No:
Type of Policy
Policy period
Sum Insured
OG-21-1108-****-00000528
Mediclaim Insurance Policy
(Canara Bank Group Policy)
23.09.2020 to 22.09.2021
Rs.10,00,000/-
3.
Name of the Patient
Name of the policyholder
Late Sh. Gopi Chand Manwani
Late Sh. Gopi Chand Manwani
4.
Name of the insurer
Bajaj Allianz General Ins. Co. Ltd.
5.
Date of Repudiation
--
6.
Reason for repudiation
--
7.
Date of receipt of the Complaint
07.02.2022
8.
Nature of complaint
Group Mediclaim
9.
Amount of Claim
N.A.
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs.2,32,256/- as per Annex VI A
12.
Complaint registered under
Rule no: of IOB rules, 2017
13 (1)(b)
13.
Date of hearing/place
11.04.2022 / NOIDA
14.
Representation at the hearing
a) For the Complainant
Ms. Prabha Singh
b) For the insurer
Sh. Shyama Charan Vats, Legal
15
Complaint how disposed
Award
16
Date of Award/Order
18.04.2022
17) Brief Facts of the Case : Late Sh. Gopi Chand Manwani, the brother of the complainant had taken a
Mediclaim Insurance Policy (Canara Bank Group Policy) No. OG-21-1108-****-00000528 for the
period from 23.09.2020 to 22.09.2021 for the Sum Insured of Rs.10,00,000/-. The Claim of the
Complainant’s husband was not settled by the Insurance Company. Aggrieved, she requested the
insurer including its GRO to reconsider the claim but failed to get any relief. Thereafter, she has
preferred a complaint to this office for resolution of her grievance.
18) Cause of Complaint:
a) Complainant’s argument : The Complainant Ms. Prabha Singh stated in her complaint that she had
submitted all original pre and post hospitalization documents to the Insurer for reimbursement. The
policy was issued in the name of Late Sh. Gopi Chand Manwani. He had passed away on 01.02.2021.
The policy was of Rs.10,00,000/- and exhausted during hospitalization period but according to policy
wordings sum assured will be doubled in case of SARCOMA.
b) Insurers’ argument: The Insurance Company stated in their SCN that
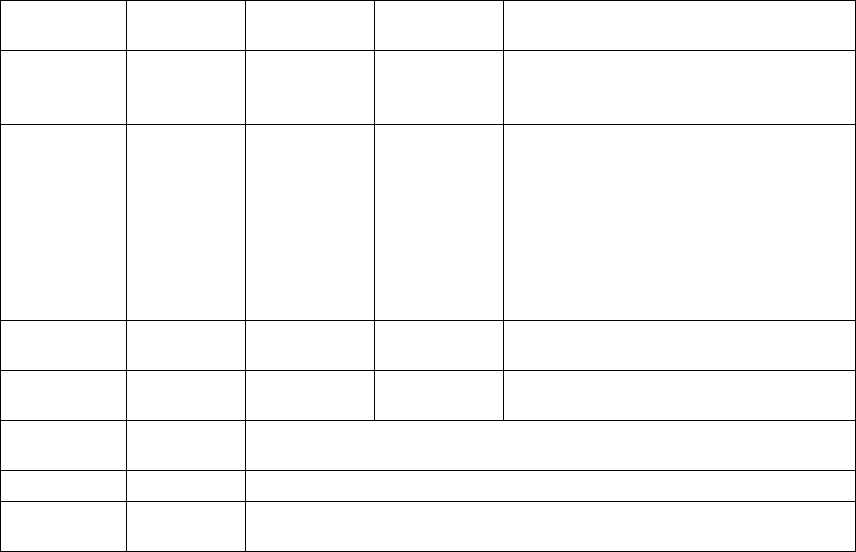
1. It is submitted that the claim of the complainant with respect to the hospitalization expenses of the
insured was denied by the Opposite Party on reasonable grounds and that too after following the
due procedure. The Complainant was duly intimated about the company’s inference of claim as put
forth by him, but he chose to remain silent on the same.
2. As soon as the claim for the treatment of “Recurrent Ca Left Lower Alveolus with Lung and Bone
Meta” by the complainant was intimated to the opposite parties, they scrutinized the documents
and found that the claim of the insured is payable. The claim was considered and an amount of
Rs.53,552/- was paid as the sum insured of the complainant had exhausted and some of the expenses
incurred on the treatment were for non-medical, which were excluded under the policy. The details
of the payment under the terms and conditions of the policy has been reproduced herein below for
the reference of the Hon’ble Ombudsman:
Particular
Bill Amt.
Disallowed
Amt.
Approved
Amt.
Deduction details
Non-
Medical
Charges
300
300
00
Medical Evaluation For Tpa-50, Medical
HistoryAssessment-250
Pharmacy
Charges
1,27,665
856
1,26,809
Nitrile Gloves - Powder Free
FingertipTextured-16,Iv Cannula Safety-
365,Iv Infusion Set Intrafix-
322,Transparent Iv
DressingCannulaFixator - (Rel.Iderm -IV)
7X9Cm 1 X
100 Pcs - Gujarat Healthcare (Batch :Doe
:-153
Doctor
Charges
12,500
0
12,500
NA
Pathology
Charges
10,200
0
10,200
NA
Other
deduction
92,507
Basic sum insured exhausted (details mentioned
below)
Claims paid
9,46,448
Amount paid under different claims mentioned below
Payment
done
53,552
(10,00,000 – 9,46,448)
It will be important to mention here that the insured/complainant has also claimed for several other
claims under the policy and the said claim amount has been paid under the policy due to which the
total sum insured of Rs.10,00,000/- has exhausted under the policy. The details of all the claims
amounts paid under the present policy has been mentioned below for reference:
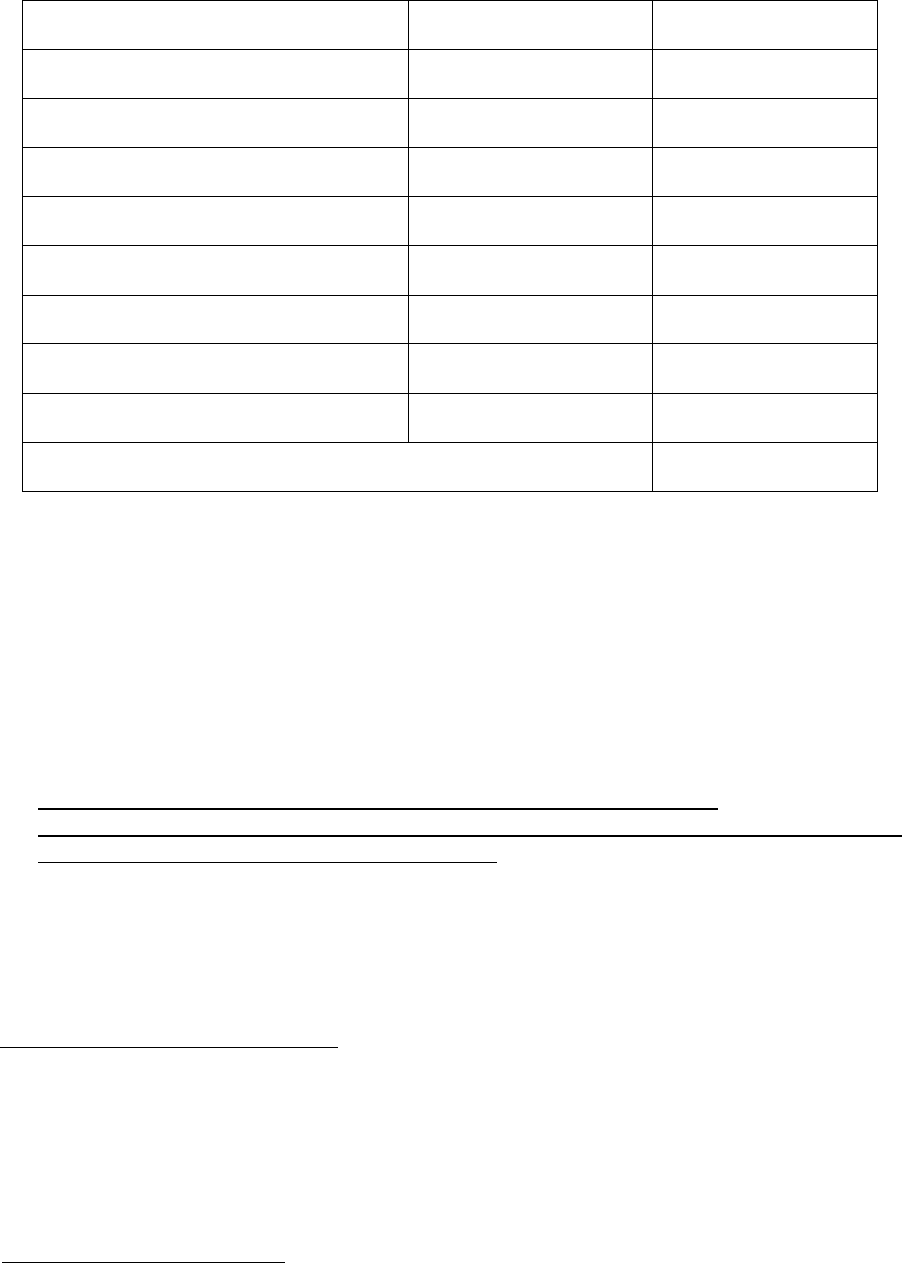
Claim number
Bill date
Amount paid (Rs.)
OC-21-1002-6021-00008831
28-Sep-2020
1,17,044
OC-21-1002-6021-00009321
12-Oct-2020
1,15,391
OC-21-1002-6021-00010251
24-Oct-2020
99,463
OC-21-1002-6021-00010264
23-Oct-2020
95,563
OC-21-1002-6021-00010332
02-Nov-2020
2,77,484
OC-21-1002-6021-00011592
16-Nov-2020
1,68,138
OC-21-1002-6021-00011883
23-Nov-2020
40,354
OC-21-1002-6021-00012104
25-Nov-2020
33,011
Total amount paid in the policy
9,46,448
As the claim amount has been paid by the opposite party to the insured/complainant there is no
cause of action left for the complainant to agitate here and thus, the case is liable to be dismissed.
3. It is mentioned that as per the terms and conditions of the policy, the sum insured is doubled only if
the disease i.e. cancer falls under the specific severity as prescribed under the terms and conditions
of the policy. As the severity of cancer which is measured with the TNM {tumor (T), nodes (N), and
metastases (M)} TNM classification or mitotic count from treating doctor, which was never provided
by the complainant for review. The relevant clause of the terms and conditions of the policy is
mentioned herein below for reference of the Hon’ble Ombudsman:
“10. Double Sum Insured for Cancer of specified severity (Indemnity based)
We will increase the Sum Insured for an insured person by 100% if he is diagnosed as suffering
from cancer of specified severity under this Policy”
4. The claim of the complainant has been duly and rightly considered and paid as per the terms and
conditions of the policy and the details of the same have been mentioned above and also explained
in the approval letter attached herewith. As the cause of action for filing the present complaint does
not exist the complaint is liable to be dismissed on this sole ground.
19) Reason for Registration of Complaint:- Partial settlement of Mediclaim.
20) The following documents were placed for perusal.
a) Annexure VI A
b) Complaint copy
c) Policy Copy
d) SCN
21) Observations and Conclusion :-
Both the parties appeared for personal hearing. The Complainant, Ms. Prabha Singh reiterated that
she had submitted all original pre and post hospitalization documents to the Insurer for
reimbursement. The policy was issued in the name of her brother Late Sh. Gopi Chand Manwani. He
had passed away on 01.02.2021. The policy was of Rs.10,00,000/- and exhausted during
hospitalization period but according to policy wordings sum assured will be doubled in case of
SARCOMA.
The Insurance Company informed that the insured/complainant had claimed for several other claims
under the policy and the said claim amount had been paid under the policy due to which the total
sum insured of Rs.10,00,000/- was exhausted under the policy. As per the terms and conditions of
the policy, the sum insured is doubled only if the disease i.e. cancer falls under the specific severity as
prescribed under the terms and conditions of the policy. As the severity of cancer which is measured
with the TNM {tumor (T), nodes (N), and metastases (M)} TNM classification or mitotic count from
treating doctor, which was never provided by the complainant for review.
I have examined the documents exhibited and the oral submissions made by both the parties. It is
observed in the present case that as per the terms and conditions of the policy, the sum insured is
doubled only if the disease i.e. cancer falls under the specific severity as prescribed under the terms
and conditions of the policy. During the course of hearing, the insurer submitted that they were
willing to settle the claim Hence, it is directed to the Insurer to pay the admissible claim to the
complainant.
AWARD
Taking into account the facts and circumstances of the case and the submissions made by both
the parties during the course of hearing, it is directed to the Insurer to pay the admissible claim
to the complainant.
The complaint is treated as disposed off accordingly.
22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with the award
within thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 18.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
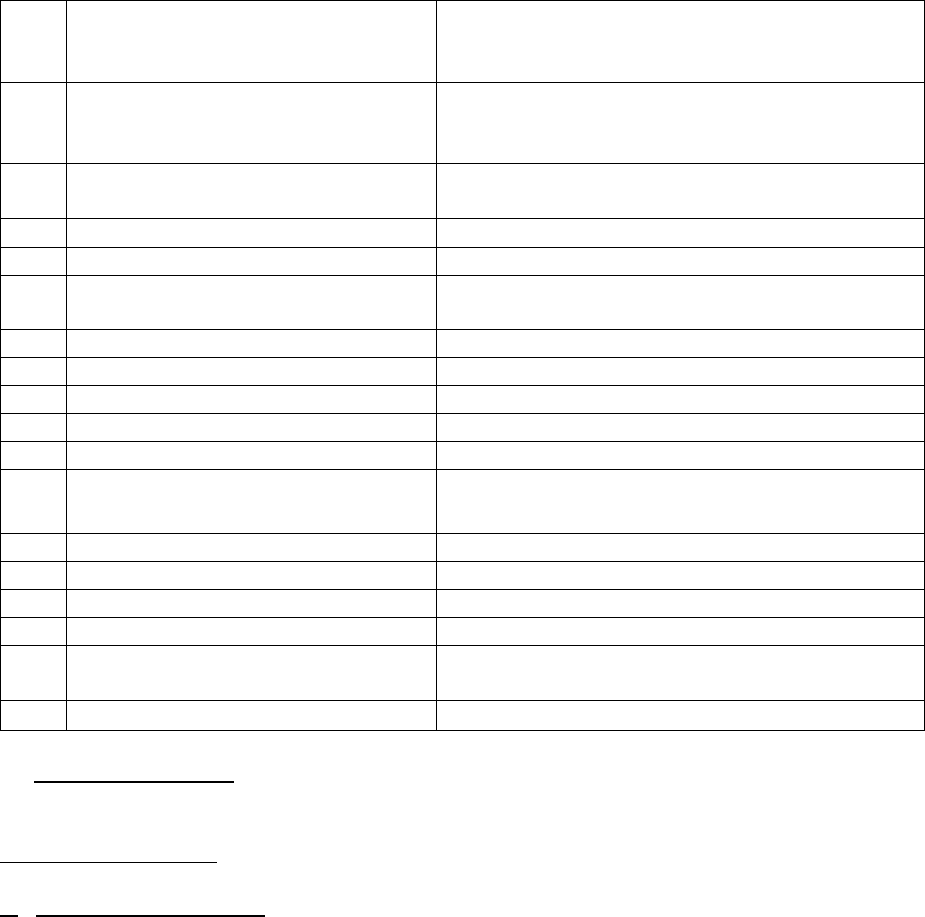
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. AND UTTARAKHAND
UNDER INSURANCE OMBUDSMAN RULES 2017
OMBUDSMAN – SHRI C.S. PRASAD
CASE OF MR. SANJEEVE JAIN V/S THE ORIENTAL INS. CO. LTD.
COMPLAINT REF: NO: NOI-H-050-2122-0589
AWARD NO:
1.
Name & Address of the Complainant
Mr. Sanjeeve Jain
35/20, North Civil Lines
Sadar Bazar, Muzaffar Nagar (UP)
2.
Policy No:
Type of Policy
Duration of policy/Policy period
253900/48/2021/3680
Health -PNB Oriental Mediclaim Policy-2017 (Group)
06-01-2021 to 05-01-2022
3.
Name of the insured
Name of the policyholder
Mr. Sanjeeve Jain
Smt. Kaushal Jain
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
25-08-2021
6.
Reason for repudiation
Treating hospital was suspicious and due to 24 hrs.
clause
7.
Date of receipt of the Complaint
08-02-2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 1,98,451/-
10.
Amount and date of Partial Settlement
NAC
11.
Amount of relief sought
Rs. 1,98,451/-
12.
Complaint registered under
IOB rules
13 (1) (b)
13.
Date of hearing/place
27-04-2022/ NODA
14.
Representation at the hearing
a. For the Complainant
Mr. Sanjeeve Jain
b. For the insurer
Mr. Harsh Kumar & Dr. Sheena
15.
Complaint how disposed
Award
16.
Date of Award/Order
28-04-2022
17) Brief Facts of the Case: This complaint is filed by Mr. Sanjeeve Jain against The Oriental Insurance Co.
Ltd. for repudiation of his mother’s (Smt. Kaushal Jain) claim, under the policy.
18) Cause of Complaint:
a) Complainant’s argument: Claimant’s mother was a holder of PNB Oriental Mediclaim Policy-2017
(Group Health).
● Claimant’s mother suffered from Covid-19 and due to that, she expired on 08-05-2021.
● Initially, she was taken to a Covid hospital but because of severe shortage of beds in the hospital,
she was advised domiciliary treatment.
● She received domiciliary treatment under a doctor from 19-04-2021 till her death.
● All claim related documents were submitted to the insurance company in original for settlement
of the case.
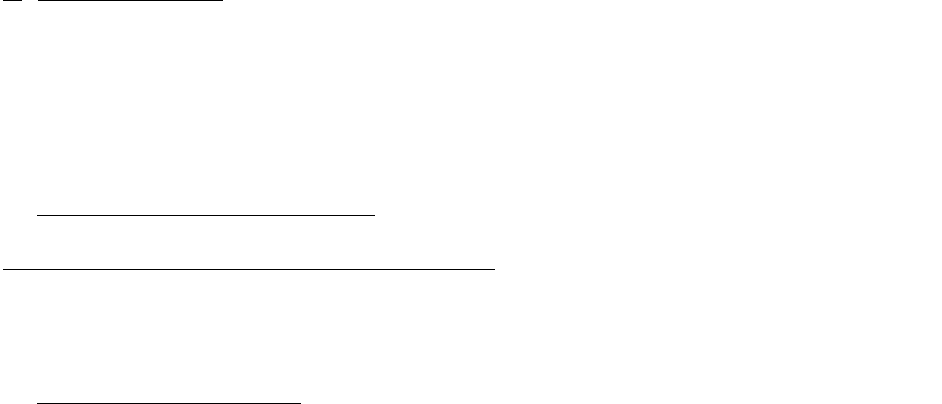
● Insurance company repudiated the claim since the treating hospital was suspicious and 24 hours
criteria for admission was not fulfilled.
b) Insurers’ argument: The insurance company submitted their SCN dated- 20-04-2022 wherein they
submitted their reply as under: -
● The patient was hospitalized for COVID-19 Viral infection, however neither the claim is
admissible for hospitalization as 24 hours were not completed, nor it falls under domiciliary
treatment as patient was hospitalized for the same.
19) Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules 2017.
20) The following documents were placed for perusal.
a) Complaint letter
b) Policy document
c) SCN
21) Observations & Conclusion: -
Both the parties attended the online hearing on 27-04-2022.and reiterated their submissions.
The complainant stated that his mother suffered from Covid-19 and due to that, she expired on 08-05-
2021.Initially, she was taken to a Covid hospital but because of severe shortage of beds in the hospital,
she was advised domiciliary treatment. Hence, she received domiciliary treatment under a doctor from
19-04-2021 till her death. Although all claim related documents were submitted to the insurance
company originally for settlement of the case, the Insurance company repudiated the claim since the
treating hospital was suspicious and 24 hours criteria for admission was not fulfilled.
Insurer defended their decision on the grounds that the claim is not admissible for hospitalization as 24
hours were not completed. Moreover, it does not fall under domiciliary treatment since the patient was
hospitalized for the same.
It is observed that the patient was discharged from the hospital only as per the advice of treating physician
in the hospital and was discharged before 24 hours due to severe shortage of beds in the hospital. Since,
the patient was advised to take further treatment at home by the hospital after finding her condition
stable on low flow of oxygen support through mask only, she had no other option but to take the
treatment at home only under the supervision of a medical practitioner. It is noted from the policy that if
the patient had taken treatment at home‘ on account of non-availability of room in a hospital’, then the
claim can be considered under Domiciliary treatment. However, as per Policy Condition No.- 2: Coverage;
B- Domiciliary Hospitalization Benefit is restricted to 10% of sum Insured subject to maximum Rs. 25,000/-
during the policy period. Hence, the claim needs to be settled as per policy terms and conditions.
The insurance company is directed to settle the claim as per terms and conditions of the policy.
AWARD
Taking into consideration the oral and written submissions made by both the parties, insurance
company is directed to settle the claim as per terms & conditions of the policy.
22.If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to approach
any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules,2017, the insurer shall comply with the award
within thirty days of the receipt of the award and intimate compliance of the same to the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 28.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
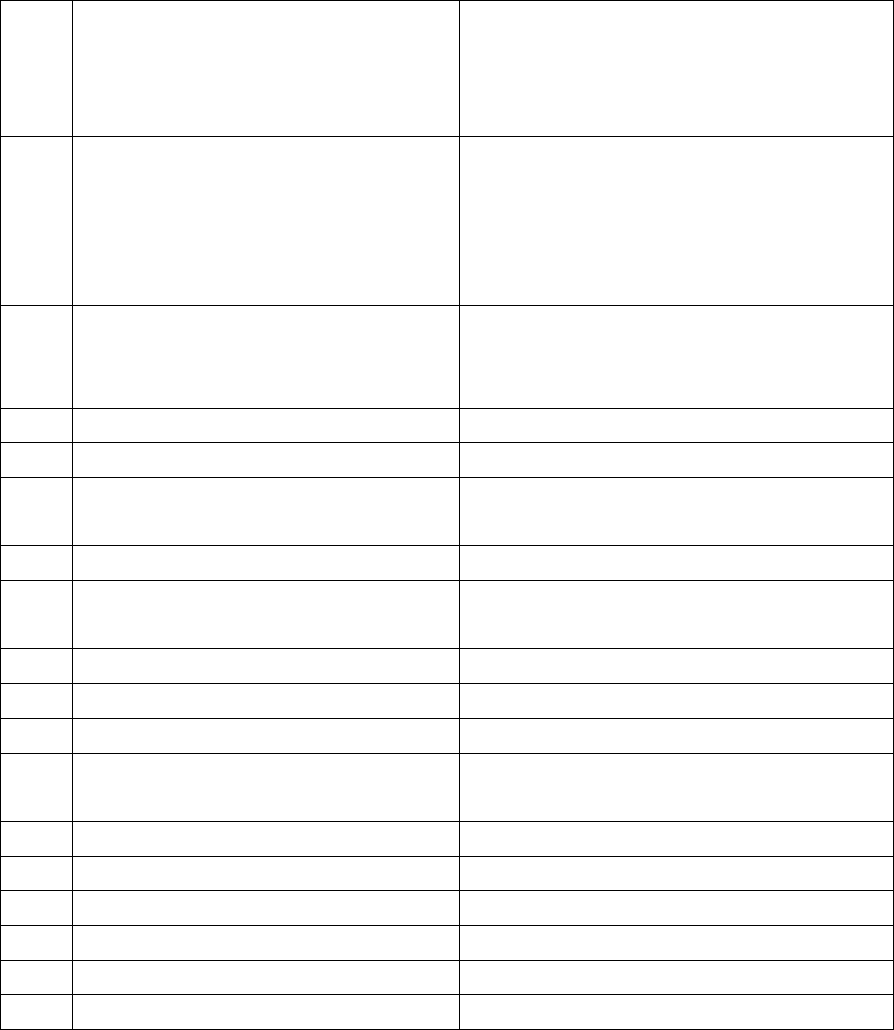
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF WESTERN U.P. & UTTRAKHAND
UNDER INSURANCE OMBUDSMAN RULE 2017
OMBUDSMAN : SH. C.S. PRASAD
CASE OF SH. SURESH CHANDRA V/S. NATIONAL INSURANCE CO. LTD.
COMPLAINT REF. NO.: NOI-G-048-2122-0602
AWARD NO:
1.
Name & Address of the Complainant
Sh. Suresh Chandra
S/O Sh. B.N. Agrawal,
713, Indira Nagar, Dehradun,
Uttarakhand-248006.
2.
Policy No:
Type of Policy
Policy period
Sum Insured
251100/50/20/10000379
Group Mediclaim Tailormade Policy
(Without Domiciliary)
01.11.2020 to 31.10.2021
Rs.4,00,000/-
3.
Name of the patient
Name of the policyholder
Name of the insured
Sh. Suresh Chandra
Sh. Suresh Chandra
Canara Bank Retirees
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
27.01.2022
6.
Reason for repudiation/Partial
Settlement
Treatment is not covered as per policy
terms and conditions.
7.
Date of receipt of the Complaint
14.02.2022
8.
Nature of complaint
Rejection of Medi-claim By Insurance
Company
9.
Amount of Claim
N.A.
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
Rs.78,924/- as per Annex. VI A
12.
Complaint registered under
Insurance Ombudsman Rule 2017
13 (1)b
13.
Date of hearing/place
11.04.2022 / NOIDA
14.
Representation at the hearing
a) For the Complainant
Sh. Suresh Chandra
b) For the insurer
Mr. R Bhatia, Manager, MCRO
15
Complaint how disposed
Award
16
Date of Award/Order
18.04.2022
17. Brief Facts of the Case:- Sh. Suresh Chandra, the Complainant had taken Group Mediclaim
Tailormade Policy No. 251100/50/20/10000379 for the period from 01.11.2020 to 31.10.2021
for Sum Insured of Rs.4,00,000/-. The Group Policy was issued in the name of Canara Bank
Retirees. The Insured was an employee of Canara Bank. The Complainant lodged the claim for
reimbursement of bills of Rs.78,924/- which was rejected by the Insurance Company.
Aggrieved, he requested the Insurer including its GRO to reconsider the claim but failed to get
any relief. Thereafter, he has preferred a complaint to this office for resolution of his
grievance.
18. Cause of Complaint:-
a) Complainant’s argument:- Sh. Suresh Chandra, the Complainant stated that the Insurance
Company informed him through mail on 31.12.2021 that his claim amount is approved by
MD India TPA but later informed rejection through mail on 27.01.2022.
b) Insurers’ argument:- The Insurance Company stated in their SCN that
Policy No. : - 251100/50/20/10000379
Claim No. : - MDI6698117
Patient Name : - Sh. Suresh Chandra
Name of Hospital : - Saaol Health Consultancy Services - NEW DELHI
Date of Admission : - 10-Oct-2021
Date of Discharge : - 10-Oct-2021
Diagnosis : - [Conservative] Cad/ EECP
Sum Insured : - Rs.4,00,000/-
Claim Amount : - Rs.78,924/-
The Patient was admitted to Saaol Health Consultancy Services - NEW DELHI on dated 10-
Oct-2021 and treated for EECP, and after treatment, discharged from hospital on 10-Oct-
2021.
After discharge from the hospital, the insured had submitted claim documents with amount
of Rs.78924 /-. After review the claim documents, said claim is repudiated as per the Policy
terms and conditions.
A 70 yrs old patient diagnosed with Coronary Artery Disease. During hospitalization, the
patient was treated with EECP. As per policy terms and condition, EECP is not listed as day
care procedure. Hence, the claim has been repudiated
CRS Clause: 2.10: As per claim documents procedure is done on day care basis and as per
policy terms and conditions, the procedure is not covered under day care treatment, hence,
claim is not payable.
19) Reason for Registration of Complaint: - Rejection of Mediclaim

20) The following documents were placed for perusal.
a) Customer complaint
b) Annexure vi and vi (a)
c) Reply of Insurance Company
d) SCN
21) Observations and Conclusion :-
Both the parties appeared for personal hearing through video call and reiterated their
submissions. Sh. Suresh Chandra, the Complainant reiterated that he is a heart patient. His
claim has been wrongly rejected by the Insurance Company. The Insurance Company stated
that the Hospital does not satisfy the definition of hospital as per terms and conditions of
the policy.
The complainant clarified that the patient was treated with EECP. As per policy terms and
condition, EECP is not listed as day care procedure.
I have examined the documents exhibited as evidence and oral submissions made by both
the parties. At the outset, it is observed that the Insurance Company has concurred with the
opinion of the TPA and confirmed that the claim has been rightly repudiated. Both the TPA
and the Insurer seem to have taken a very narrow and technical view of the case with the
intention to repudiate the claim. There is no dispute about the fact that the complainant
was admitted and treated in Saaol Heart Centre for his heart ailments. It is evident from the
documents submitted that Saaol Heart Centre is a well established institution run by well
known medical practitioners nursing staff and is engaged in providing treatment to the
patients. It is also not irrelevant to observe from the TPA’s mail that the hospital is having
less than 15 beds in-patients.
The second ground of rejection is that complainant was managed by EECP in OPD which is
not covered under the policy. It is pertinent to mention that Saaol Heart Centre is a well
known institution run by qualified doctors including Dr. Bimal Chhajer who is known for
applying unconventional and unorthodox methods to treat heart ailments.
The orders passed by other Ombudsmen (Chandigarh, Delhi and Jaipur) in respect of similarly
placed patients who underwent similar treatment at Saaol Heart Centre have been perused.
They have awarded relief to the above complainants whose claims were also repudiated by
the Insurance Companies. It is also mentioned that the policy taken by the instant
complainant does not say anything about not entertaining the cost of treatment taken in
such hospitals like Saaol Heart Centre. Following the judicial discipline, I feel that the ends of
justice will be met if the complainant’s claim is settled by the Insurance Company.
AWARD
Taking into account the facts and circumstances of the case and the submissions
made by both the parties during the course of hearing, the Insurance Company is
directed to settle the claim and pay the admissible amount to the complainant as
per terms and conditions of the policy.
The complaint is treated as disposed off accordingly.
22. If the decision of the Forum is not acceptable to the Complainant, he/she is at liberty to
approach any other Forum/Court as per laws of the land against the respondent Insurer.
23. The attention of the Complainant and the Insurer is hereby invited to the following
provisions of Insurance Ombudsman Rules, 2017:
a) According to Rule 17(6) of Insurance Ombudsman Rules, 2017, the insurer shall comply with
the award within thirty days of the receipt of the award and intimate compliance of the same to
the Ombudsman.
Place: Noida. C.S. PRASAD
Dated: 18.04.2022 INSURANCE OMBUDSMAN
(WESTERN U.P. & UTTARAKHAND)
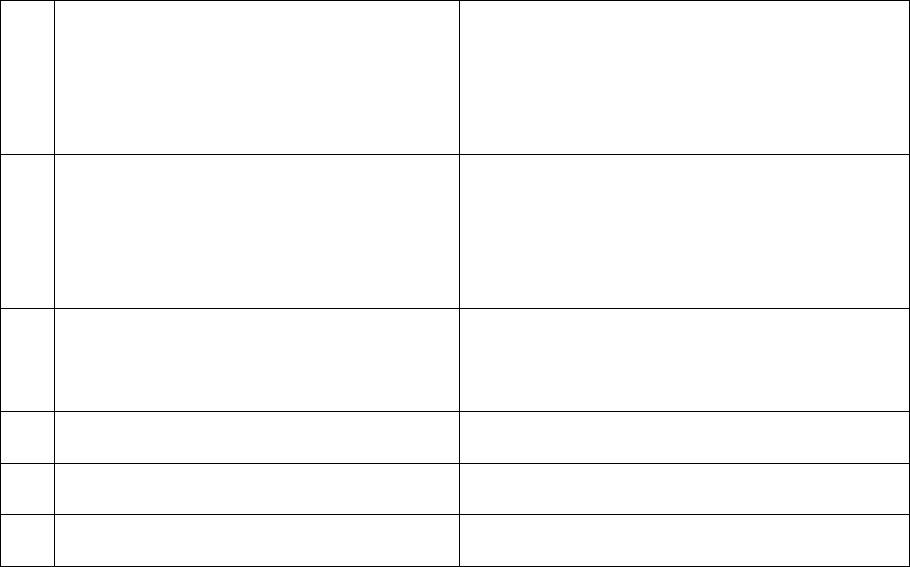
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Atul Jerath
Case of Reshma Devi V/S ICICI Lombard General Insurance Co. Ltd.
Complaint Ref. NO: CHD-H-020-2122-0958
1.
Name & Address of the Complainant
Smt. Reshma Devi
House No.- 17019, Agarwal Colony, 40ft Road,
Bathinda, Punjab- 151001
2.
Policy No:
Type of Policy
Duration of policy/Policy period
4016/13**84216/03/000
Group Health(Floater)
04.10.2020 to 03.10.2021
3.
Name of the insured
Name of the policyholder
Smt. Reshma Devi
BSE Limited
4.
Name of the insurer
ICICI Lombard General Insurance Co. Ltd.
5.
Date of Repudiation
15.09.2021
6.
Reason for repudiation
Misrepresentation
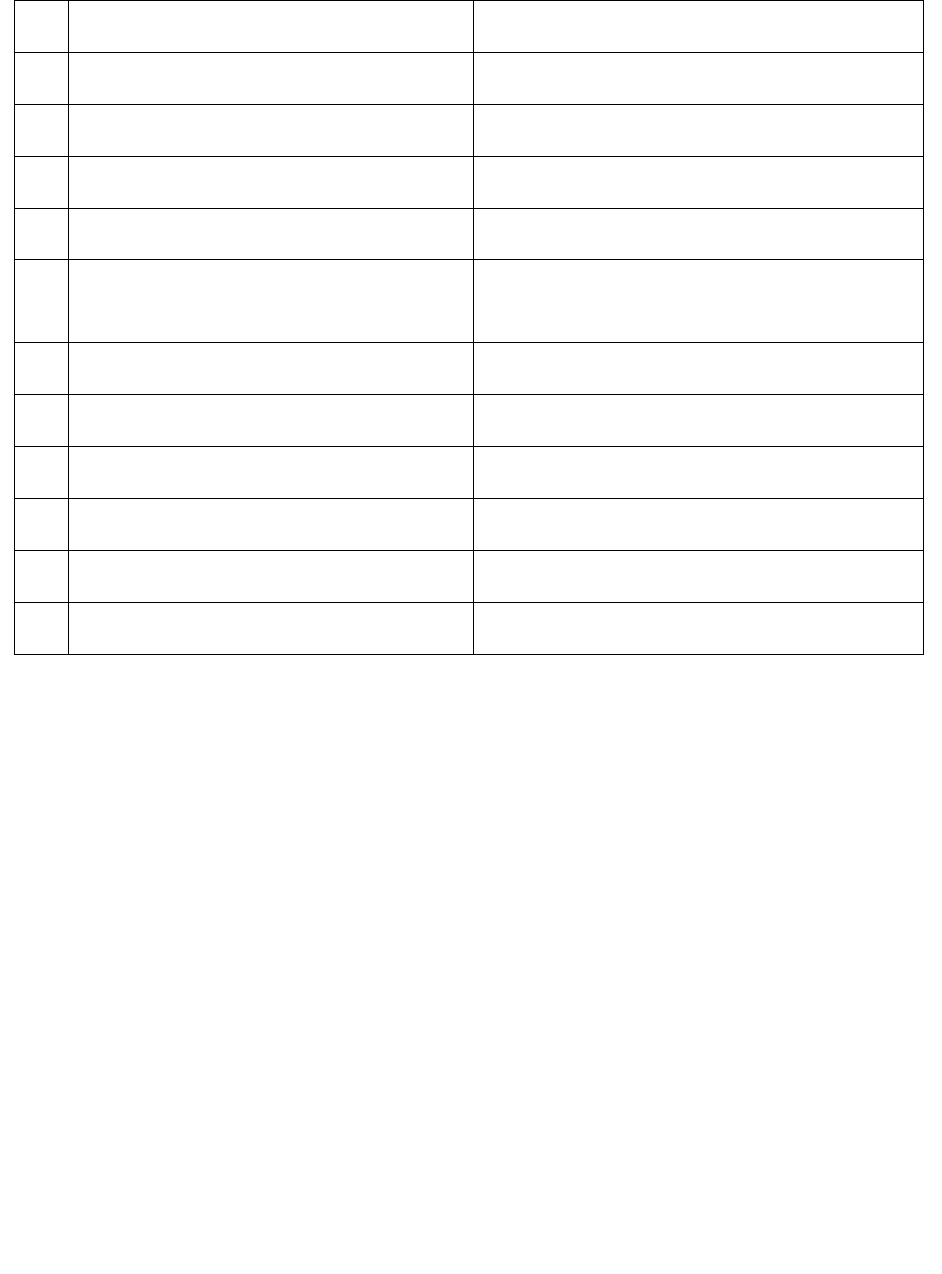
7.
Date of receipt of the Complaint
11-02-2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Not provided
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Not provided
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation
of claims by an insurer
13.
Date of hearing/place
08.04.2022/Online hearing
14.
Representation at the hearing
For the Complainant
Mrs. Reshma Devi, Mr.Deen Dayal
For the insurer
Mr.Karan Bagdai
15
Complaint how disposed
Recommendation under rule 16
16
Date of Award/Order
08.04.2022
17. Brief Facts of the Case: Smt. Reshma Devi (hereinafter, the complainant) has filed this complaint
against ICICI Lombard General Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect denial of
claim.
18. Cause of Complaint:
a) Complainant’s argument: Her Son who is working in BSE, Delhi had purchased a Medi-claim
Policy from ICICI Lombard Mumbai and the policy is continuing for about 20 years and also paid
extra premium on account of their age of 66 yrs and 72 yrs(husband), senior citizens. On 14-07-
2021, she suddenly fell ill and started vomiting with yellow water, chest pain. After waiting for
some time at home my situation deteriorated and her husband took her to MALWA HOSPITAL, ,
Bathinda under Dr. RUPINDER SINGH (M.D, D.M) who admitted me to the hospital and
administered injections to stop the vomiting and also advised me to get the further checks
related to heart as her body was cold and she was having chest pain. As the hospital was not
having heart specialists and facilities available the doctor advised to go to the nearby Pulse

Hospital to meet Dr. Sharad Gupta (DM, Cardio). Dr Sharad Gupta charged her Rs 800 as
Emergency Patient Fees duly computerized receipt given already. The Doctor checked and
investigated various tests like Blood Test, ECG, ECHO, LIVER FUNCTION etc. The Computerized
Bills and Receipts are attached during the original claim submission.
In the tests, serious blood infection with heavy increase of TLC, DLC and White Cells found at
alarming levels. The Doctor treated and supervised injections accordingly. Afterwards, they
returned to MALWA Hospital and again after the treatment The doctor advised them to go for
ULTRASOUND SCAN. The Ultra Sound Scan was done by Dr. Rumana. After Ultra Sound Scan Dr.
Rupinder Singh checked the reports and found Blockage in Intestines. The Doctor started the
treatment for Acute Gastroenteritis and at the hospital administered I/V Antibiotics, I/V PPI & I/V
antiemetic for the whole night and next day the doctor advised them to go for CT Scan. CT Scan
was done and after checking CT Scan Report the doctor accordingly treated and administered IV
Antibiotics and other medicines as deemed suitable by the doctor. All the medicine bills, Test
Reports and Payment Receipts are computerized except Malwa Hospital Admission and
Discharge bill duly printed, signed and stamped by the doctor.
She remained Hospitalized for 36 hours. All the reports of Lab Tests, ECG, ECHO, Ultra Sound
Scan, CT scan have been submitted along with the claim papers to ICICI Lombard. She has only
the copies with her. Being senior citizens they forgot to get the discharge summary from the
hospital and the same could not be given during the claim. The discharge summary is taken from
the hospital and the copy is attached for your kind perusal.
ICICI Lombard representative visited Malwa Hospital and verified facts related to our claim. The
representative even called us and afterwards the representative said the issue related to
blockage is true and verified. ICICI Lombard even arranged a video call with us and the only
objection raised was related to non-computerized Malwa Hospital Bills. As per the representative
on video call, all other documents were in order. The Malwa Hospital does not have a system to
provide computerized bills. But the printed bill on Malwa Hospital letterhead signed and stamped
by the doctor and payment received on the printed numbered receipt is given by the hospital.
They submitted the claim to ICICI Lombard and ICICI Lombard out rightly rejected their Claim.
They are residing in Bathinda and their son who is employed stays in Delhi away from them. All
original bills and claim related documents are already given to ICICI Lombard along with the
claim.
b) Insurer’s Argument: Company has reviewed grienveance of complainant and has decided to process
the claim for Rs. 21280/- as per terms and conditions of the policy towards the full ad final settlement of
the claim.
19. Reason for Registration of Complaint: Incorrect denial of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called for online hearing. Both parties were present and recall their arguments as noted in Para 18
above. Company informed that they have taken clarification from treating doctor. After same, insurance
company offered to pay Rs.21280/- as per policy terms and conditions towards final settlement of above
said case. Complainant accepted the offer of the insurance company. Accordingly, an agreement by way
of conciliation has arrived at between the insurer and complainant, which I consider as fair and reasonable
for both the parties.
In the light of the amicable settlement of complaint between the Parties, the complaint is disposed- off
with a direction that the company shall comply with the agreement and shall send a compliance report to
this office within 30 days after the receipt of award copy for information and record.
Award
The complaint is resolved in terms of agreement of conciliation arrived at between the complainant
and insurers as stated above. Accordingly, both the parties should implement this agreement within
30 days.
( Atul Jerath )
Insurance Ombudsman
April 08, 2022
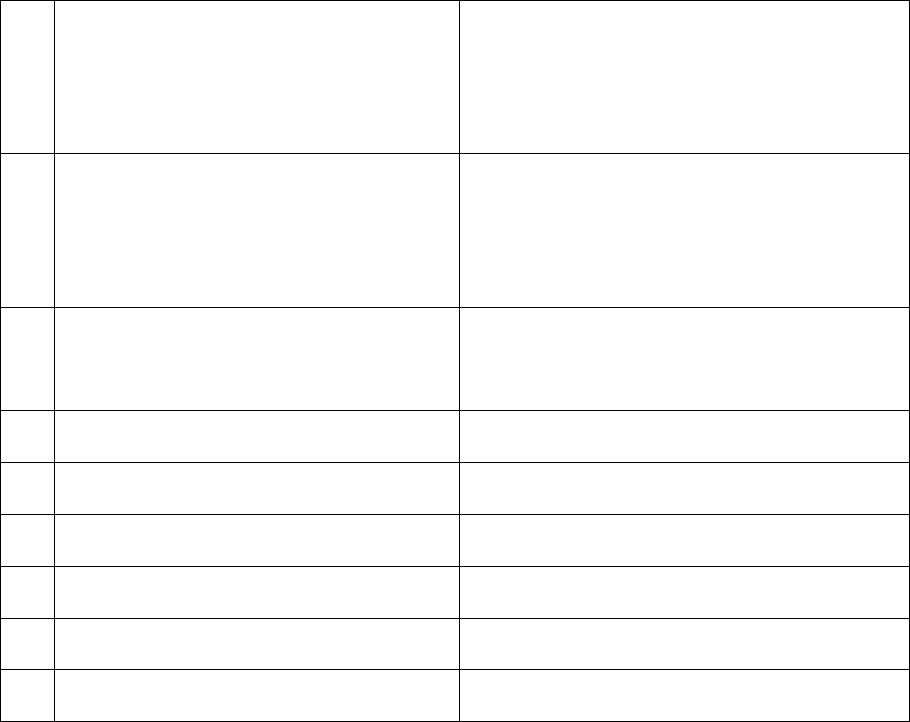
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Atul Jerath
Case of Param Jit Grover V/S The Oriental Insurance Co. Ltd.
Complaint Ref. NO: CHD-H-050-2122-0935
1.
Name & Address of the Complainant
Shri Param Jit Grover
# 1157, Sector-7, Karnal, Haryana-132001
Mobile No.- 9873411570
2.
Policy No:
Type of Policy
Duration of policy/Policy period
261301/48/2021/1361
PNB Oriental Mediclaim Group Policy
29-01-2021 to 28-01-2022
3.
Name of the insured
Name of the policyholder
Param Jit Grover & Meenu Grover
Param Jit Grover
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
25.02.2022
6.
Reason for repudiation
No active treatment
7.
Date of receipt of the Complaint
07-02-2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.54590/-
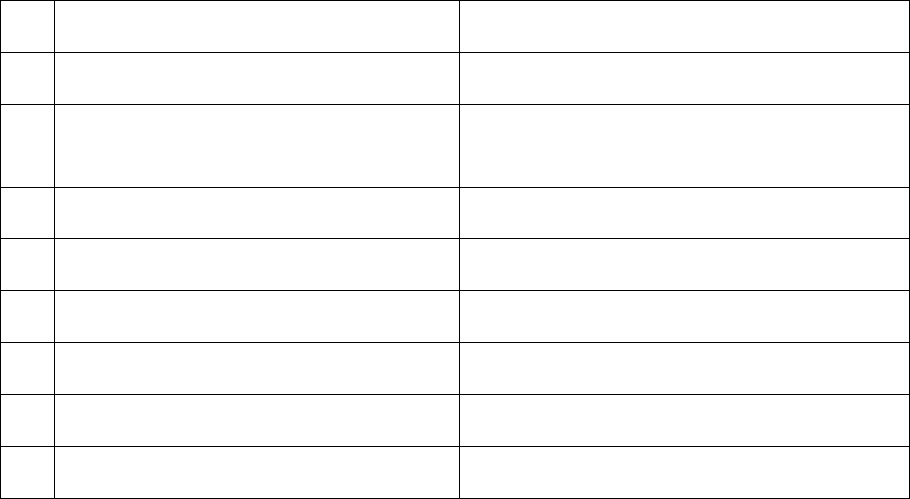
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs.54590/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation
of claims by an insurer
13.
Date of hearing/place
08.04.2022/Online hearing
14.
Representation at the hearing
For the Complainant
Mr.Param Jit Grover
For the insurer
Mr.Kapil Khapra
15
Complaint how disposed
Award under rule 17
16
Date of Award/Order
20.04.2022
17. Brief Facts of the Case: Shri Param Jit Grover (hereinafter, the complainant) has filed this complaint
against The Oriental Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect denial of claim of his
wife.
18. Cause of Complaint:
a) Complainant’s argument: The claim case was submitted to M/s Raksha Health Insurance TPA Ltd.,
Chandigarh on 02.08.2021 for reimbursement of Rs. 54590/- as hospitalization expenses incurred for
the treatment of Meenu Grover at Apollo Credle Hospital, Delhi where cashless facility was not
available. The said claim was denied by TPA vide letter dt. 05.10.2021 with the reasons as per policy
clause no. 4.9 read as ‘Expense incurred at Hospital or Nursing Home primarily for
evaluation/diagnostic purposes which is not followed by active treatment for the ailment during
hospitalized period’. He submitted appeal against this on 11.10.2021 for reconsideration of above said
claim with valid reasons, but no response received from company or TPA. He requested for payment
of claim.
b) Insurer’s Argument: As per SCN of the company, on scrutiny of the claim documents, they observe
that the claim is not admissible in view of the following:
- Mrs. Meenu Grover, w/o Sh.Paramjit Grover was admitted and this was a case of Post Menopausal
bleed for which hysteroscopy was done which is a OPD basis diagnostic procedure. As per policy
conditions hospitalization merely meant for standalone diagnositic procedures without any active
treatment stands as an exclusion under clause 4.9.
- Also the claim was repudiated due to patient was admitted in hospital for less then 24 hours. As per
policy clause 3.18, minimum 24 hours admission/hospitalization is required.(Definition – 3.18).
- Also, this treatment doesn’t falls under specified day care procedures/treatments (Definition – 3.14).
19. Reason for Registration of Complaint: Incorrect denial of health claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called for online hearing. Both parties were present and recall their arguments as noted in Para 18
above. Complainant informed that her wife had bleeding from uterus, admitted in hospital and tests were
also performed to check cancer. Moreover, treatment remains continued even after hospitalization. But
insurance company denied the hospitalization claim of Rs. 54590/-. Representative of insurance company
argued that there was no active line of treatment as such claim was denied under clause 4.9. Moreover it
was an OPD basis procedure and policy condition of 24 hours hospitalization was not fulfilled.
As per repudiation letter, said claim is repudiated on the basis of policy clause no. 4.9, which relates to
expenses incurred at hospital primarily for evaluation/diagnostic purpose which is not followed by active
treatment for the ailment during the hospitalized period. As per discharge summary of patient Mrs.
Meenu Grover, diagnosis was postmenopausal bleed and procedure performed is hysteroscopy under
general anesthesia. As such plea of insurance company that there was no active line of treatment is not
hold good.
As per discharge summary patient admitted at 12.44 on 15.07.2021 and discharged at 10.36 on
16.07.2021 which is just less than 24 hrs. But, Insurance Company has nowhere taken this stand in
repudiation letter, and can’t take fresh plea after registration of complaint.
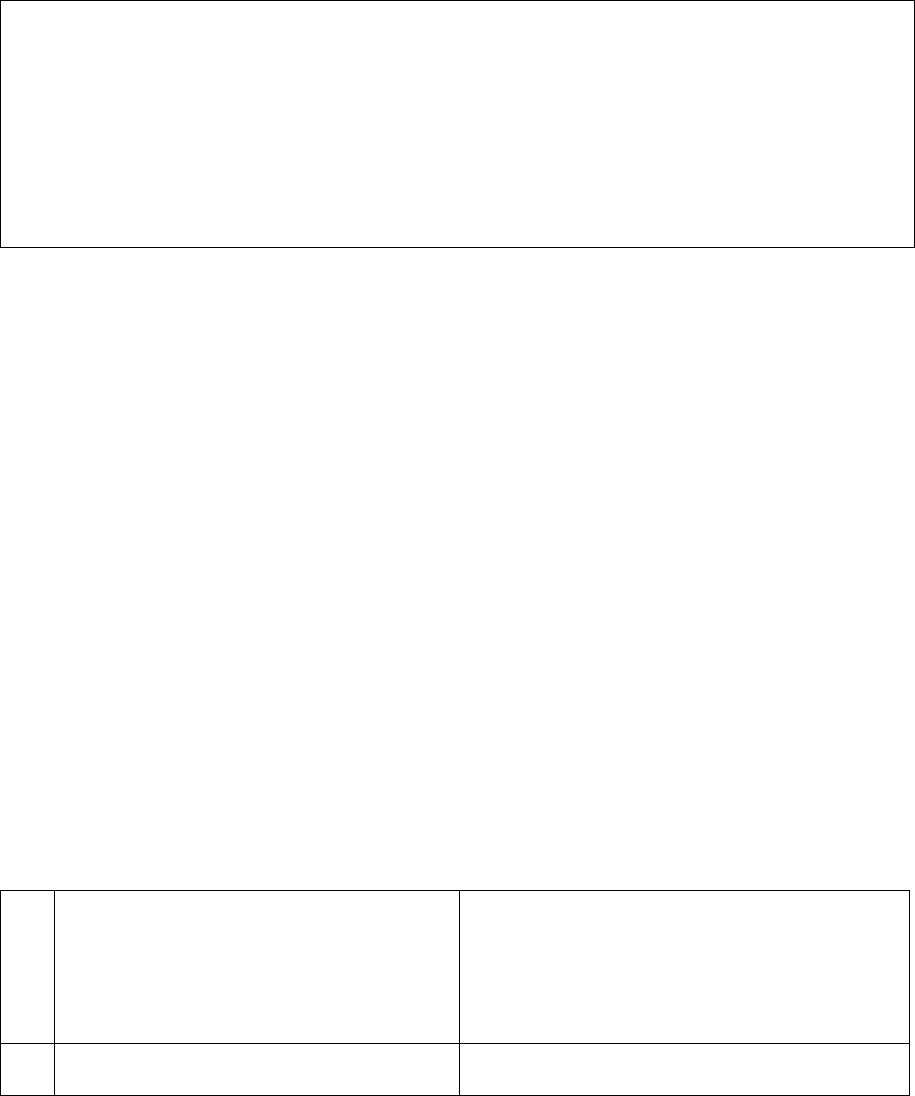
In view of above facts and above discussion, decision of insurance company in above said claim to
repudiate the claim is not correct. Accordingly they are directed to pay admissible claim in above said
case, as per terms and conditions of the policy, within 30 days of award.
Award
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of online hearing, the company is directed to pay admissible claim as per
terms and conditions of policy within 30 days of receipt of award as per section 17(6) of Ombudsman
Rules, 2017.
(Atul Jerath)
Insurance Ombudsman
April 20, 2022
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Atul Jerath
Case of Vipul Sud V/S The Oriental Insurance Co. Ltd.
Complaint Ref. NO: CHD-H-050-2122-0936
1.
Name & Address of the Complainant
Shri Vipul Sud
# 3341, Sector-50-B, Bankers Enclave,
Chandigarh-160047
2.
Policy No:
23**00/48/2022/620
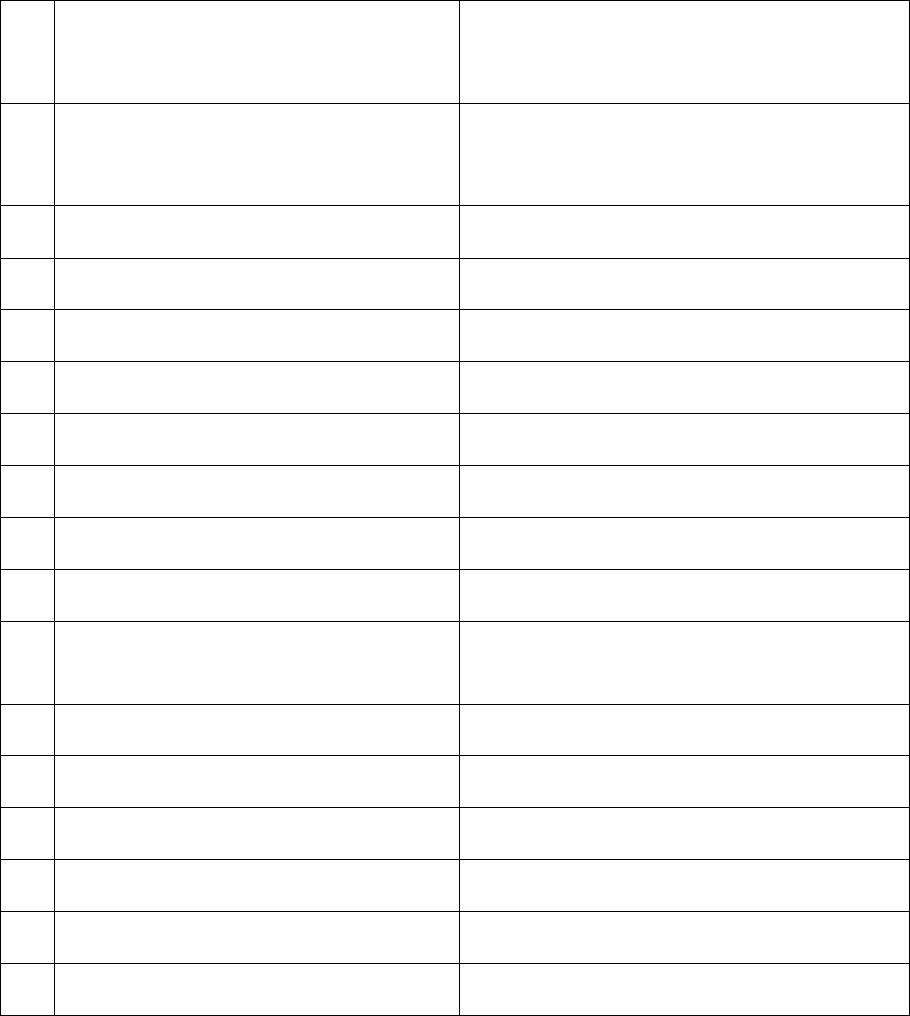
Type of Policy
Duration of policy/Policy period
Oriental Ins. Bank Saathi Group Policy
26-10-2021 To 25-10-2022
3.
Name of the insured
Name of the policyholder
Vipul Sud/Shweta Sood
Vipul Sud
4.
Name of the insurer
The Oriental Insurance Co. Ltd.
5.
Date of Repudiation
25.11.2021
6.
Reason for repudiation
Under clause 2.13
7.
Date of receipt of the Complaint
07-02-2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs.62239/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Not specified
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation
of claims by an insurer
13.
Date of hearing/place
08.04.2022/Online hearing
14.
Representation at the hearing
For the Complainant
Mr.Vipul Sud
For the insurer
Ms.Arvinder Kaur
15
Complaint how disposed
Award under rule 17
16
Date of Award/Order
19.04.2022
17. Brief Facts of the Case: Shri Vipul Sud (hereinafter, the complainant) has filed this complaint against
The Oriental Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect denial of health claim of her
wife.
18. Cause of Complaint:
a) Complainant’s argument: The claim for Rs.62239/- was submitted on 11
th
Nov., 2021 with formal
intimation before the submission of claim. All the original documents, bills, receipts and reports were
submitted to the company office at Medi Assist TPA, but the claim was repudiated by company vide letter
received on 25.11.2021.Company mentioned reason for declining the claim under Paragraph : 3 as
maternity expenses. Whereas this medical termination was lawful as per the admission and discharge
summary of Dr.Bedi of Bedi Nursing Home, Chandigarh, who is well recognized gynecologist. Secondly,
the pregnancy termination has no limitation in number as far it is lawful termination as per company’s
own terms and conditions under section 2:13, specifying the lawful termination has lifetime cover for the
spouse of insured person. He requested for reimbursement of the claim.
b) Insurer’s Argument: Insured is covered under Mediclaim policy since 26.10.2016 with sum insured of
Rs. 5,00,000/-. As per complaint received from insured, his spouse Ms.Shweta Sood was admitted to Bedi
Hospital on 26
th
Oct. 2021 with complaint of missed abortion and severe Anemia and the present Gravida
G3,P2,L2 and was treated with a surgical procedure of Dilation and Curettage. On scrutinizing the
submitted claim documents, it is observed that the patient Shweta Sood, 43 yrs old female was admitted
with incomplete abortion, severe anemia, underwent D & c. The lodged claim was considered for
repudiation as per clause no. 2.13(ii) since the insured is already having two living children, so the claimant
is not eligible for this benefit.
19. Reason for Registration of Complaint: Incorrect denial of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called for online hearing. Both parties were present and recall their arguments as noted in Para 18
above. Complainant underlined that termination of pregnancy was accidental and they were not willing
for same, as such it should be treated as differently. Further termination is not defined under the policy
and even for two pregnancies, it can be for n numbers. Company has categorized it under maternity for
their convenience only. Actually there was first illness, blood infused and reason of termination may be
due to some illness, accident or some internal problem etc.
Insurance company through SCN informed that since the insured is already having two living children, so
the claimant is not eligible for maternity benefit as per clause 2.12(ii). During hearing, Insurance Company
stated that as complainant has sum insured of Rs. 5 lac, she is not eligible for Maternity expenses. They
also pointed out that termination of pregnancy happened due to tablet Norethisterone taken twice by
patient on 15.10.21 and 16.10.21 as confirmed in Bedi Hospital’s prescription slip dt.22.10.2022.
As per repudiation letter dt. 25.11.2021, issued by insurance company, it is a case pertaining to 43 yrs old
diagnosed with incomplete abortion. The claim is inadmissible as maternity not covered in the policy.
Claim denied under terms and conditions of section 2.13 of policy.
According to discharge summary of patient Mrs. Shweta, 43 yrs P2L2A1 female presented with incomplete
abortion with severe anemia with heavy bleeding. There is H/O intake of Tab Norethisterone twice on
15.10.2021 and 16.10.2021. As policy clause 2.13 related to maternity expenses the company shall pay
the medical expenses incurred as an in-patient for a delivery or lawful medical termination of pregnancy
during the policy period limited to two deliveries or terminations or either during the lifetime of the
insured person. This cover is available for SI slabs equal to or greater than INR 10 Lacs and available only
to the insured or his spouse, provided that
i. Plan has been continuously in force for a period of minimum 24 months in respect of both the
insured and his/her spouse.
ii. Those insured persons who have already having two or more living children will not be eligible
for this benefit.
iii. Liability of the Company limited to 2.5% of the Sum Insured.
Since sum insured of relevant policy is Rs. 500000/-, as such insured is not eligible for maternity expenses
coverage as per policy condition. Moreover, as per above mentioned clause, as insured already have two
children; she is not eligible for this benefit.
In view of these facts, and above discussion, insurance company has rightly repudiated the above said
claim as per policy terms and conditions and their decision does not require any interference. Accordingly,
the complaint shall deserve to be rejected.
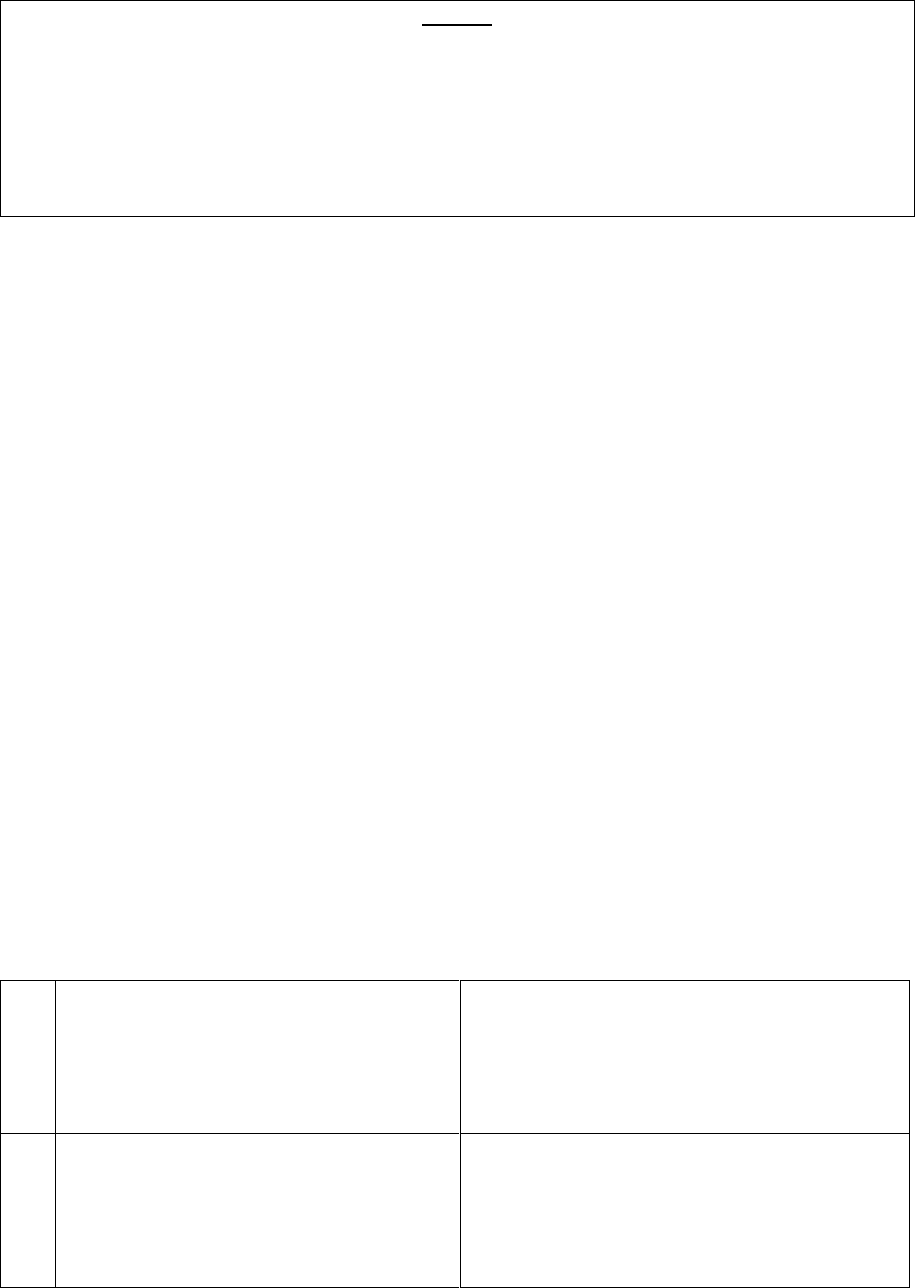
AWARD
Taking into account the facts & circumstances of the case, documents submitted and the submissions
made by both the parties during the course of online hearing, the said complaint is hereby dismissed
on merits and no relief is granted.
( Atul Jerath )
Insurance Ombudsman
April 19, 2022
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shir Atul Jerath
Case of Kamal Kumar V/S The United India Insurance Co. Ltd.
Complaint Ref. NO: CHD-H-051-2122-0967
1.
Name & Address of the Complainant
Shri Kamal Kumar
H.No 8-9, Vashisht Nagar, Ambala Cantt,
Ambala,Haryana
2.
Policy No:
Type of Policy
Duration of policy/Policy period
5001002819P111085979
Group Mediclaim Policy
01.10.2019 to 30.09.2020
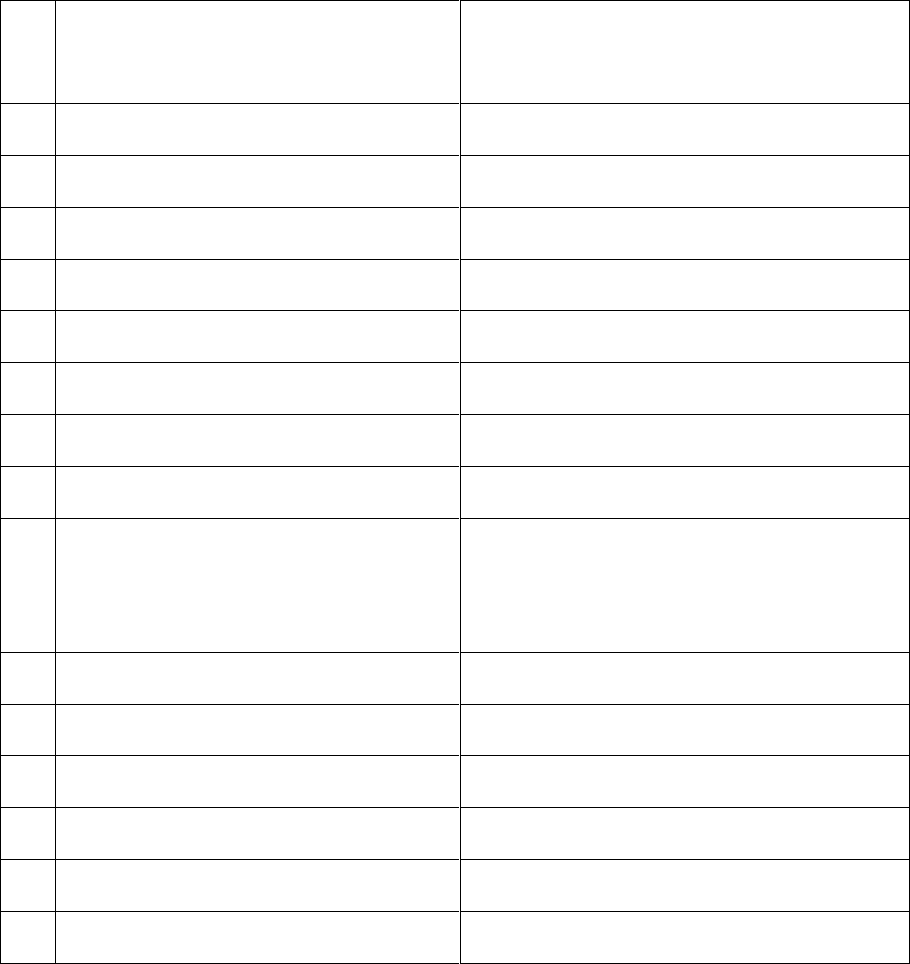
3.
Name of the insured
Name of the policyholder
Kamal Nain Kumar
IBA- Bank of Baroda
4.
Name of the insurer
The United India Insurance Co. Ltd.
5.
Date of Repudiation
02.02.2021
6.
Reason for repudiation
Delay in submission of documents
7.
Date of receipt of the Complaint
15.02.2022
8.
Nature of complaint
Incorrect denial of claim
9.
Amount of Claim
10.
Date of Partial Settlement
N.A
11.
Amount of relief sought
Rs.309000/-
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claims by an insurer
13.
Date of hearing/place
12.04.2022/ online hearing
14.
Representation at the hearing
For the Complainant
Shri Kamal Kumar , the complainant
For the insurer
Ms. Pamela Pinto Dy. Manager
15
Complaint how disposed
Recommendations under rule 16
016
Date of Award/Order
12.04.2022
17. Brief Facts of the Case: Shri Ravi Kumar Jain (hereinafter, the complainant) has filed this complaint
against The United India Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect denial of claim.
18. Cause of Complaint:
a) Complainant’s argument: He was hospitalized at lifeline Medicare Hospitals for his Covid treatment
from 22.09.2021 to 29.09.2021. On the day of discharge, the complainant got the news of sad demise of
his father and had to rush to support his family. After getting things back to normal he applied for
reimbursement after 1.5 months due to family reasons. The Mediassist TPA has rejected the claim on
the administrative basis of the late submission of a claim and returned papers. In-spite of the facts the
genuine reasons beyond the control of a human being his employer has accepted the request and
agreed to the condoning of the delay in submission of the papers and waiving the condition of the
policy. Please note that IRDA circular no.IRDA/HLTH/MISC/CIR/216/09/11 which states that the insurers’
decision to reject a claim shall be based on sound logic and valid grounds. “Rejection of claims on purely
technical grounds in a mechanical fashion will result in policy holders losing confidence in the insurance
industry, giving rise to excessive litigation. It is also advised that the insurers must not repudiate such
claims unless and until the reasons of delay are specifically ascertained, recorded and the insurers
should satisfy themselves that the delayed claims would have otherwise been rejected even if reported
in time”. In his case, it would be the responsibility of the TPA to place before the insurance company for
condonation of late in submission of claim documents. The complainant sought the intervention of this
forum for payment of his claim.
b) Insurer’s Argument: We have issued a Group Mediclaim Policy to the Indian Bank Association- Bank
of Baroda covering their employees along with their dependent members for the period from
01.10.2019 to 30.09.2020. Shri Kamal Kumar along with dependent members are included in the above
mentioned policy for sum insured of Rs.400000/-. The complainant has submitted a claim for
hospitalization period of 22.09.2020 to 29.09.2020 in December 2020 which is way beyond the cutoff
date for submission i.e 15.11.2020. We attach herewith the instructions issued to the HRM of Banks
dated 09.10.2020 regarding the cut off dates. Claim has been rejected as per terms and conditions
(Clause 5- Document Submissions time frame) of the policy.
19. Reason for Registration of Complaint: Incorrect denial of claim
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion): Case called for hearing.
Both parties are present and recall their arguments as noted in Para 18 above.
During the online hearing, it was enquired from the insurance company whether in the view of the facts
emerging they would like to re-look at the claim and arrive at an agreement. The representative of the
insurer offered to settle the claim as per terms and conditions of the policy subject to submission of
required documents. The same was agreed upon by the complainant during online hearing.
Accordingly, an agreement by way of conciliation was arrived at between the insurer and complainant,
which I consider as fair and reasonable for both the parties.
In the light of the amicable settlement of complaint between the Parties, the complaint is disposed- off
with a direction that the complainant shall file required documents with the insurer within 15 days from
the receipt of award’s copy. The company shall comply with the agreement and shall send a compliance
report to this office within 30 days after the receipt of award copy for information and record.
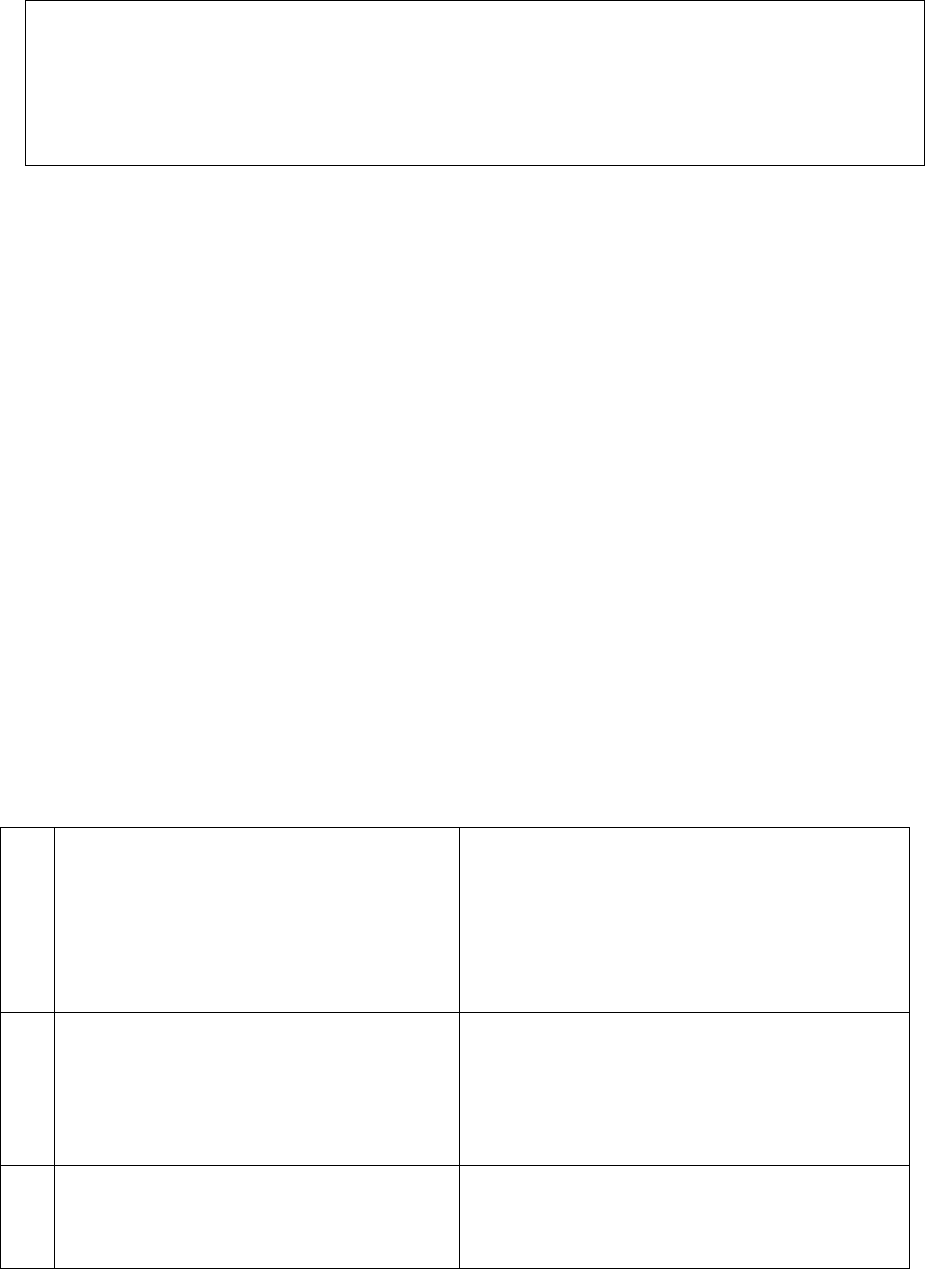
Award
The complaint is resolved in terms of agreement of conciliation arrived at between the complainant
and insurers as stated above. Accordingly, both the parties should implement this agreement within
30 days.
(Atul Jerath )
Insurance Ombudsman
12
th
April, 2022
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shir Atul Jerath
Case of Sangeeta Devi V/S Liberty General Insurance Co. Ltd.
Complaint Ref. NO: CHD-H-028-2122-0965
1.
Name & Address of the Complainant
Smt. Sangeeta Devi
H. No.- B-33-1488/2A, New Ashok Nagar-A,
Shelu Boot House, Saleh Tabri, Ludhiana
Punjab-141008
2.
Policy No:
Type of Policy
Duration of policy/Policy period
4217-400202-19-7000002-00-000
Liberty Secure Future Connect Group Policy
02.04.2019 to 01.04.2024
3.
Name of the insured
Name of the policyholder
Akhilesh Kumar
Aditya Birla Finance Limited
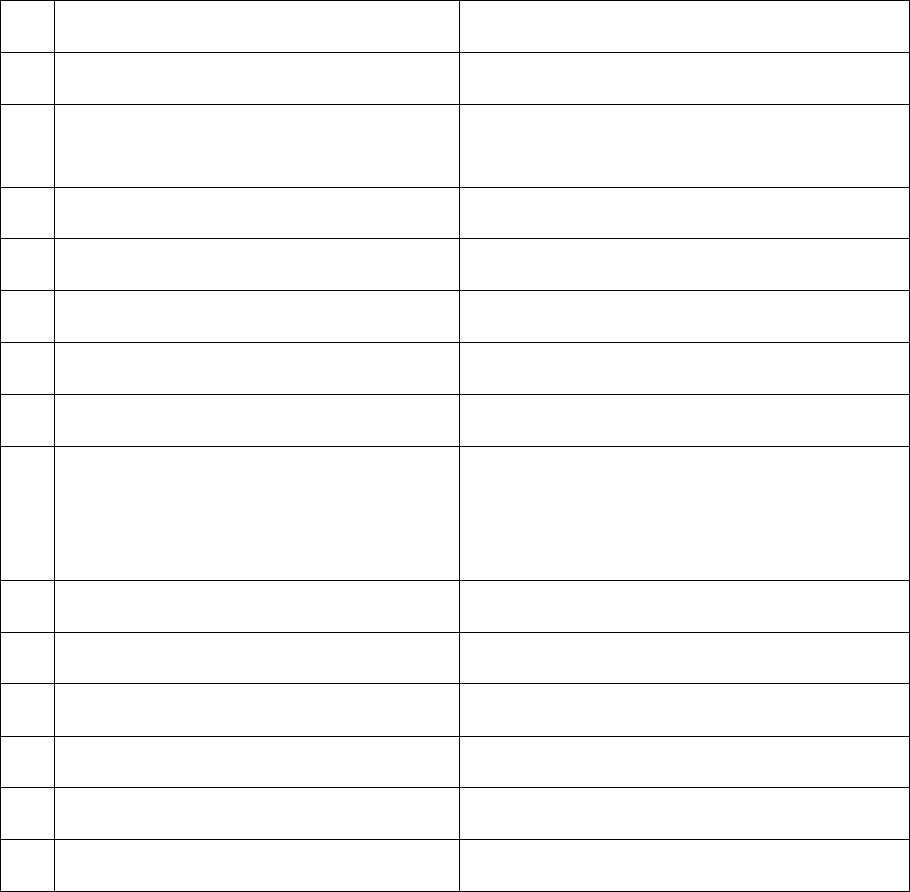
4.
Name of the insurer
Liberty General Insurance Limited
5.
Date of Repudiation
22.06.2021
6.
Reason for repudiation
Claim not payable as only listed critical illnesses
covered under the policy
7.
Date of receipt of the Complaint
09-02-2022
8.
Nature of complaint
Incorrect denial of claim
9.
Amount of Claim
10.
Date of Partial Settlement
N.A
11.
Amount of relief sought
Rs.10,00,000/-
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claims by an insurer
13.
Date of hearing/place
12.04.2022/ online hearing
14.
Representation at the hearing
For the Complainant
Shri Ravi Kumar (Brother)
For the insurer
Ms. Apeksha Sawant, AVP
15
Complaint how disposed
Award under rule 17
16
Date of Award/Order
19.04.2022
17. Brief Facts of the Case: Smt. Sangeeta Devi (hereinafter, the complainant) has filed this complaint
against Liberty General Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect denial of claim.
18. Cause of Complaint:
a) Complainant’s argument: Her husband Late Shri Akhilesh Kumar took a loan from Aditya Birla finance
company on sept. 2020. The finance company insured his loan through liberty General Insurance
Company. He died on 22.05.2021 due to Covid-19 complications. As a nominee, the complainant filed
claim against the insurance company. But the insurance company refused the claim on the ground that
the policy did not cover the covid-19. The complainant has sought the intervention of this forum for
payment of claim.
b) Insurer’s Argument: That, this Respondent Liberty General Insurance Ltd. issued Liberty secure
future connect group policy to Aditya Birla Housing Finance Limited bearing Master Policy No. 4217-
400202-19-7000002-00-000 for the period from 02.04.2019 to 01.04.2024. A certificate of insurance
bearing number 42173008716 was issued to Mr. Akhilesh Kumar valid for the period 12.10.2020 to
11.10.2023. The policy is issued to beneficiaries who have obtained loan against property from the
Master policy holder i.e. Aditya Birla Housing Finance Limited. The policy was issued through the
Brokers, Aditya Birla Insurance Brokers Limited. The Policy granted the following basic benefits:
a. Critical Illness
b. Personal Accident
c. 30 days survival period
The Policy covers defined critical illness, medical event or surgical procedure as specifically mentioned
below whose signs or symptoms first commence more than 90 days after the commencement of cover
or accidental death or Permanent Total disability as detailed under the Part II Section II of the Policy
up to the Sum Insured of Rs. 10,00,000/- mentioned in the Policy schedule.
Part 2: BENEFITS UNDER THE POLICY 1.1 SECTION I: CRITICAL ILLNESS
The policy covers the following specified critical illnesses:
• Cancer of Specified Severity
• End Stage Renal Failure
• Benign Brain Tumor
• Parkinson’s Disease
• End Stage Liver Failure
• Alzheimer’s Disease
• Motor Neuron Diseased with Permanent Symptoms
• Multiple Sclerosis with persisting symptoms
• Muscular Dystrophy
• Systematic Lupus Erythematous with Lupus Nephritis
• Medullary Cystic Disease
• Major Organ/Bone Marrow Transplant
• Open Heart Replacement or Repair of Heart Valves
• Open Chest CABG
• Surgery of Aorta
• Pneumonectomy
• Stroke resulting in Permanent Symptoms
• Permanent Paralysis of Limbs
• Myocardial Infarction First Heart Attack of Specified Severity
• Coma of Specified Severity
• Third Degree Burns
• Deafness
• Loss of Speech
• Primary (Idiopathic) Pulmonary Hypertension
Admissibility of the claim under the Policy is governed by the terms of the insurance contract. That,
claim was reported under the Critical Illness benefit of the Policy by the complainant for death of the
insured person on 20.05.2021 due to B/L Pneumonia, Septicemia, Type 1 Resp Failure. From the
documents submitted by the complainant, it was observed that the deceased Mr. Akhilesh Kumar was
admitted on 11
th
May 2021 at Mohandai Oswal Hospital and diagnosed for Post COVID recovered, B/L
Pneumonia, Septicemia, Type 1 Resp Failure. That the ailment that caused the death of the Insured
was not a specified critical illness covered by the Policy, therefore the claim was accordingly denied as
per terms of the Policy for lack of coverage under the Policy. The Respondent Insurer submits that the
Policy provides coverage for specific named illness under the Critical Illness section. There is no
ambiguity in the Policy terms in so far as the coverage or definition of critical illness is concerned. It is
well settled principle that once the coverage is limited to specified & listed illness as in this case, no
benefit can be granted if the Insured person suffers any other illness irrespective of its severity.
Unfortunately, the benefit of cover is not available to the complainant and this Respondent Insurer is
constrained by the Policy terms & benefits. It is well settled that the terms of the Policy are binding
on both the parties and accordingly a decision on the claim was conveyed to the Complainant. The
complainant submitted a representation against repudiation. However, as no new facts were brought
on record which warranted reconsideration in the matter, a response reiterating the same decision
was sent to the complainant copy of which is produced by the complainant on record already hence
not filed again.
19. Reason for Registration of Complaint: Incorrect denial of claim
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion): Case called for hearing,
both the parties are present and recall their arguments as noted in Para 18 above.
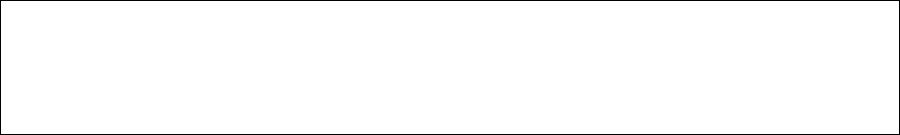
The complainant stated that Insurance Company wrongly rejected the claim of her husband who expired
due to lungs failure and pneumonia. They further submitted that they had received only three page policy
without any details with regard to coverage under the critical illness.
The representative of the insurance company submitted that the deceased Shri Akhilesh Kumar death was
due to B/L Pneumonia, Septicaemia, and Type 1 Resp. failure. The ailment that caused the death of insured
was not a specified critical illness covered by the policy. Therefore the claim was denied as per term and
conditions of the policy for lack of coverage under the policy.
The complainant during hearing had also stated that they have received a claim under the critical illness
from other insurance company. Therefore, the complainant was advised to share/submit the details of
the said claim. But the complainant did not submit any detail of claim received from other insurer. The
insurers as per direction of this forum provided the dispatch details for insurance documents sent to the
insured vide their mail dated 14.04.2022.
As per death summary, the patient Mr. Akhilesh Kumar was diagnosed for post covid recovered, B/L
Pneumonitis, Septicemia, Type 1 Res. Failure. As per policy terms and conditions said ailment are not
covered under major medical illness section of policy. The policy provides coverage only for the specific
named illness. The plea of complainant during hearing about non-receipt of complete coverage details
under the policy is not tenable as it is clearly mentioned in the certificate of insurance issued to the insured
that customer can visit their website and down load the policy wording.
In view of the observations made in Para 18b above and various documents submitted by the insurer,
claim repudiation by the insurer is justified as per policy terms and conditions. Therefore, the claim denial
decision of the insurer does not warrant any interference. The complainant is dismissed being devoid of
merits and no relief is granted.
Award
Considering the facts & circumstances of the case and the submissions made by both the parties
during the course of hearing, the complaint is hereby dismissed being devoid of merits.
(Atul Jerath)
Insurance Ombudsman
19
th
April 2022
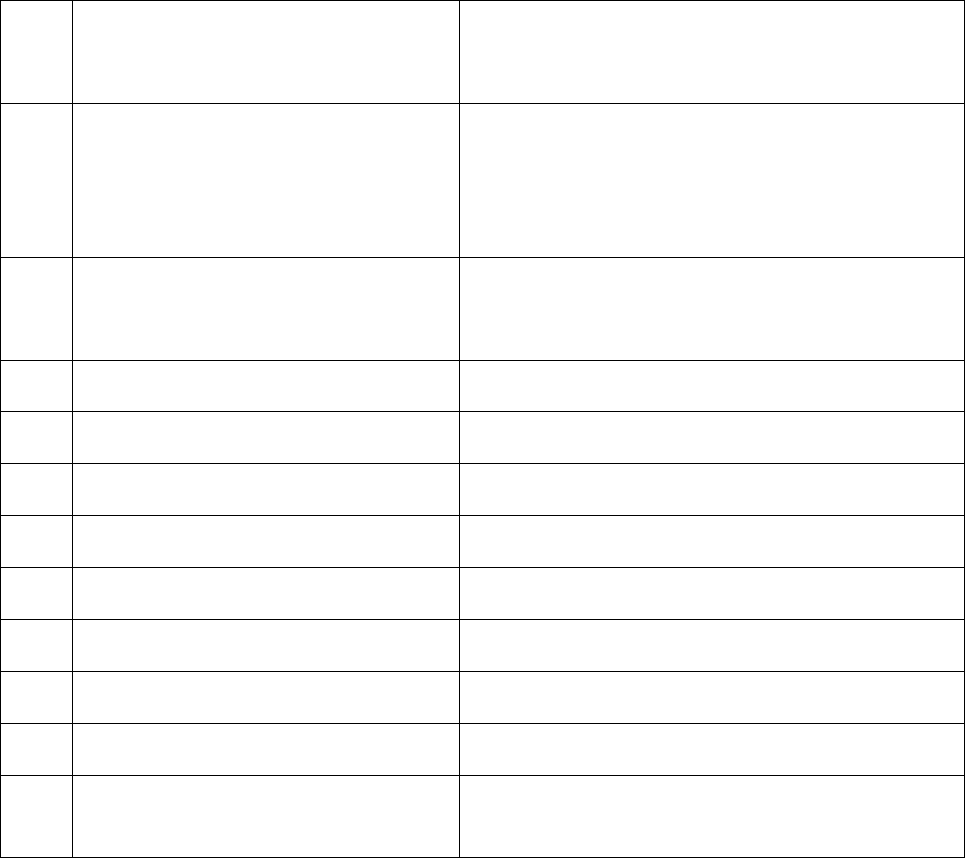
PROCEEDINGS OF THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of The Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Atul Jerath
Case of Surendra Singh v/s Universal Sompo General Insurance Co.
Ltd. Complain
t Ref. No: CHD-H-052-2122-0947
1.
Name & Address of the Complainant
Shri Surendra Singh
328/5, Ladhout Road, Basant Vihar, Rohtak
2.
Policy No:
Type of Policy
Duration of policy/Policy period
2840/60958891/01/000
Karnataka Bank Group Policy (SI-Rs 3.00 Lacs)
20-01-2021 to 19-01-2022
3.
Name of the insured
Name of the policyholder
Poonam
Surendra Singh
4.
Name of the insurer
Universal Sompo General Insurance Co. Ltd
5.
Date of Repudiation
24-12-2020
6.
Reason for repudiation
Disease falls under 36 months waiting period.
7.
Date of receipt of the Complaint
10-02-2022
8.
Nature of complaint
Deduction of claim
9.
Amount of Claim
Rs 9,57,591/-
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs 9,57,591/-
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of
claim by an insurer
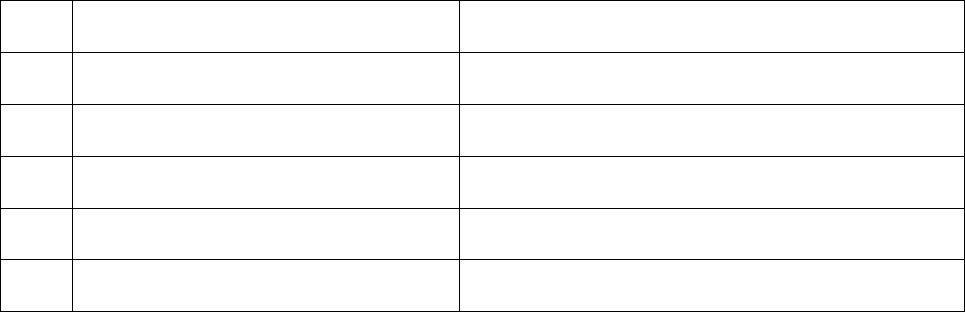
13.
Date of hearing/place
13-04-2022/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Surendra Singh, Complainant
For the insurer
Shri Gaurav Sharma
15.
Complaint how disposed
Award under Rule 17
16.
Date of Award/Order
26-04-2022
17. Brief Facts of the Case: Shri Surendra Singh (hereinafter, the Complainant), has filed this complaint
against Universal Sompo General Insurance Co. Ltd (hereinafter, the Insurers) for undue repudiation of
his wife health claim.
18. Cause of Complaint:
a) Complainant’s argument: On 10-02-2022, Shri Surendra Singh had filed a complaint for rejection of
hospitalization claim of his wife Poonam on false ground of the claim waiting period is of 36 months for
pre-existing disease. His was running the health policy of HDFC since 2012 and was ported to universal
Sompo in 2019. The policy was issued by the Karnataka Bank, but his wife was struggling with breathing
problem and leg pain. After some tests doctors advised the surgery for heart valves and her leg as blood
clot was there in her leg. His wife got hospitalized for Mitral Valve Replacement Mitral Valve
Replacement expenses incurred at Artemis Medicare for the period 27/09/21 to 19/10/21. However,
when he applied for the reimbursement company rejected the claim waiting period is there of 36
months for pre-existing disease.
Consequent to the exhaustion of basic sum insured he has preferred the claim under the Super policy of
the company having SI of 10 Lakh with the threshold limit of Rs.3 lakh. The claims team of the company
arbitrarily denied the claim and applied the dual role in the rejection of the claim that he has not disclosed
the earlier hospitalization at Mann Hospital during the year 2017. The representative of the Karnataka
Bank insisted on porting the policy with continuity of cover. Accordingly, he has disclosed the previous
policy of the HDFC Ergo from 2012 and taken the policy of universal Sompo General Insurance Company.
He denies the allegation of non-disclosure as the company has accepted both the policies and one claim
settled for Rs.3,00,000/- the same illness by Complete Health care Insurance Policy under policy
no.2825/60686675/00/00 . The claims team should not apply different rules for disclosure on policy-to-
policy basis. Moreover, the current hospitalization has no links with the earlier nature of hospitalization
and the main claim has been accepted and approved by the company. The MVR also does not come under
the pre-existing clause of the policy and the policy is in the second year of renewal. He requested this
forum to kindly settle his insurance claim.
b) Insurers’ argument: In the SCN (Self- Contained Note), insurance company stated that the
Insured availed facility of health insurance Policy from the respondent from 31/01/2021 to
30/01/2022. Insurance company stated that, Ms. Poonam Surendra Singh (wife of the
complainant) was diagnosed with ailment of Dyspnea and was admitted to Artemis Medicare
Service Ltd from 27-09-2021 to 19-10-2021. The cashless claim was generated bearing No.
271323, for the claimed amount. The said claim for cashless facility came to be denied on
19/10/2021 for the reason- Admissibility of the claim cannot be ascertained on the basis of
available documents / information. Detailed investigation is required to conclude the liability
hence cashless request is being rejected. However, denial of authorization for cashless access
does not imply denial of the treatment and does not in any way prevent the insured from seeking
necessary medical attention or hospitalization. Please note that the denial of pre-authorization
request shall not be construed to mean that you cannot claim for reimbursement under the terms
and conditions of the Policy.
Thereafter, again the said claim was generated for reimbursement, claimed amount was of Rs.
8,66,438.00 /-. An amount of Rs. 3,00,000.00 was approved /- and an amount of Rs. 2,48,400.00/-
was paid to insured person and an amount of Rs. 5,66438.00/- was not paid to the complainant
as it is not payable as per the terms and conditions of the insurance company. It includes charges
of - Medicines & Consumables Charges, Miscellaneous Charges, Investigation Charges-
Professional Fees Charges, Room & Nursing Charges all charges were not paid as per the terms
and conditions of the respondent company’s policy for the reason “Sum Insured Exhausted”.
Therefore, the claim of the complainant stands partly repudiated. The same is separately
mentioned in Column “amount not paid”, of the “Claim Settlement Letter” Dated 23/12/2021
are the charges which are not payable as per the terms and conditions of the respondent
company. Therefore, they humbly stated that the claim has been rightly paid as per the policy
terms & conditions.
19. Reason for Registration of Complaint: - Repudiation of claim.
20. The following documents were placed for perusal.
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called, both parties are present and recall their arguments as noted in Para 18 above.
Complainant stated that insurance company has repudiated his wife’s hospitalization claim on flimsy
ground of PED. His base policy from insurance company since 2012 and he has fulfilled all the conditions
of policy. The denial of claim based on Pre-existing disease and waiting period is also not correct as his
policy is in continuation and he had taken the top-up policy from same insurance company. He requested
for payment of his claim.
During online hearing, the company was advised to explore the possibility of review of the claim to arrive
at an agreement. Insurance Company reiterated their stand of SCN and stated that their repudiation
decision is in order.
On examination of various documents available in file including the copy of complaint, SCN filed by
insurance company, submissions made by both the parties at the time of online hearing and it is seen that
the complainant’s wife claim for has been partly denied by insurance company vide letter dated 06-01-
2022. The denial has been done mainly due to reasons “Non-disclosure of information and Pre-existing
Disease which was not disclosed in proposal form by complainant when he purchased Super Care health
Policy which was a Top-up policy for the first time. Insurance company denial was done because from the
scrutiny of documents “it is revealed out that the insured admitted on 15/8/2017 at Mann Hospital for
management of acute hypertension, acute vertigo, pneumonitis right lung. The insured did not disclosed
to us the detailed past medical history in the proposal form on policy inception date vide policy no
2840/60958891/01/000.”
Complainant stressed that his case doesn’t falls under waiting period as he was having policy of HDFC Ergo
from 2012 and there is no question of PED since policy was ported to Universal Sompo. Above version of
complainant doesn’t hold ground since complainant had two mediclaim policies- Base policy (Complete
Health Care Policy, which was taken in 2012 from HDFC Ergo and got ported to Universal) and another
was fresh top-up policy (Super Healthcare Insurance) purchased by complainant which incepted on 20-
01-2020. Further, there is no condition under the regular Mediclaim policy (Base Policy) or Top-up policy
wherein relaxation in respect of PED is given during filling up of proposal form. Both policies are
independent from each other. As such complainant can’t take a shelter of base policy to justify his stand
of Pre-existing disease under the cover of portability or continuation of his base policy since 2012 during
filling up of proposal form for Top-up policy.
On perusal of the same as well as policy conditions it is evident that the repudiation made by the insurer
is in line with the policy terms, clauses and conditions. Accordingly, the claim has been repudiated
correctly by the insurer and does not warrant any intervention at our end. The complaint is rejected being
devoid of merits.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of hearing, the claim has been repudiated correctly by the insurer and
does not warrant any intervention at our end.
The complaint is rejected being devoid of merits.
(Atul Jerath)
Insurance Ombudsman
April 26, 2022
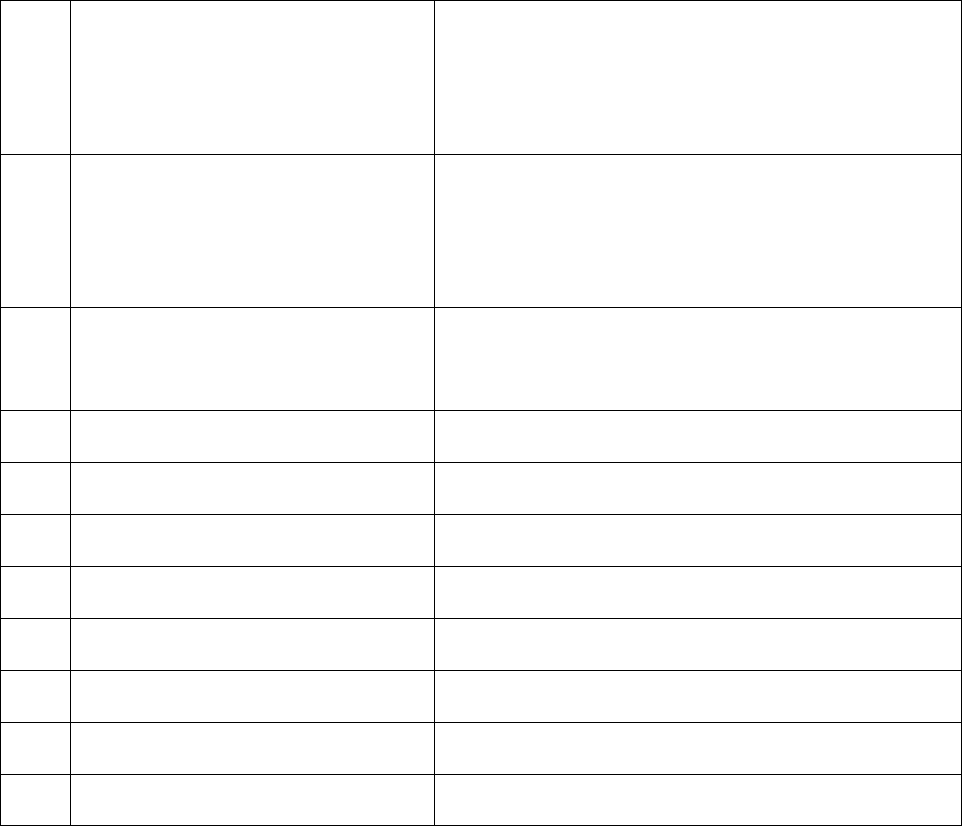
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman- Shri Atul Jerath
Case of Mukesh Kumar v/s Star Health and Allied Insurance Co.
Ltd. Complain
t Ref no: CHD-H-044-2122-0978
1.
Name & Address of the Complainant
Shri Mukesh Kumar
Kotak Mahindra Bank Ltd. SCO-120,
Brass Market, Ground Floor, Rewari-123401
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/170000/01/2021/073XXX
Group Insurance Policy, SI – Rs 4.00 Lacs
31-03-2021 to 30-03-2022
3.
Name of the insured
Name of the policyholder
Mukesh Kumar
Kotak Mahindra Bank Limited
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
16-10-2021
6.
Reason for repudiation
Treatment taken in excluded provider Hospital
7.
Date of receipt of the Complaint
18-02-2022
8.
Nature of complaint
Repudiation of claim.
9.
Amount of Claim
Rs 43,000/- approximately
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs 43,000/- approximately
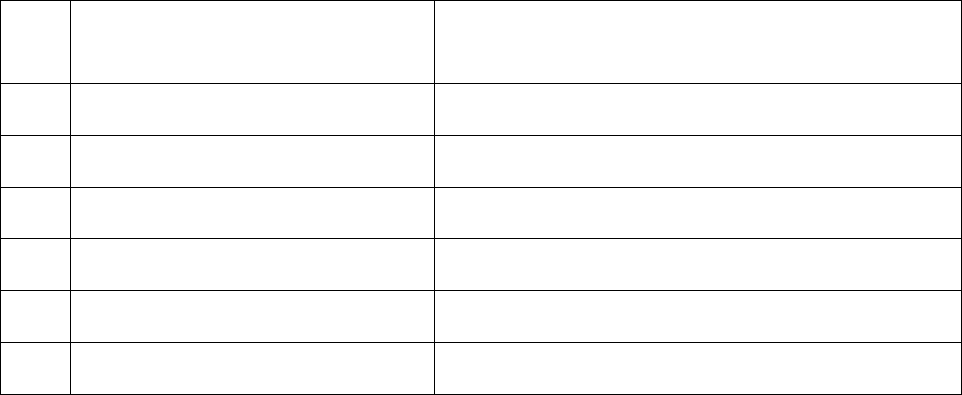
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of claims
by an insurer
13.
Date of hearing/place
13-04-2022/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Mukesh Kumar, Complainant
For the insurer
Smt Mamta Gupta, Senior Manager (Claims)
15
Complaint how disposed
Award under rule 17
16
Date of Award/Order
26-04-2022
17. Brief Facts of the Case: Shri Mukesh Kumar (hereinafter, the Complainant) has filed this complaint
against Star Health and Allied Insurance Co. Ltd (hereinafter, the Insurers), for repudiating his health claim.
18. Cause of Complaint:
a) Complainant’s argument: On 18-02-2022, Shri Mukesh Kumar filed a complaint stated that he
was admitted in Surendra hospital –Rewari from 13-08-2021 to 18-08-2021 due to typhoid fever. He
completed all claim related queries. But his claim was repudiated on the ground that hospital is an
excluded provider. He stated that insurance company should have repudiated his claim in one go rather
than asking for query. Further, at the time of emergency everybody tries to get treatment rather than
asking for excluded provider. Inspite of representation to grievance nothing fruitful came out. He
requested this forum for intervention and requested for payment his medical claim.
b) Insurers’ argument: In the SCN insurance company stated that the complainant Mr.Mukesh
Kumar along with his Family is covered in the Star Group Health through Zonal Office –Mumbai, issued
to Kotak Mahindra Bank Limited for the floater Sum Insured of Rs. 4,00,000/- vide Policy no-
P/170000/01/2021/073945 for the period of 31.03.2021 to 30.03.2022. The Insured, Mr. Mukesh Kumar,
33 years 1 months / Male was admitted on 13/08/2021 at Surendra hospital –Rewari and discharged on
17/08/2021. As per Discharge Summary, the insured was diagnosed for Typhoid Fever. The Insured
submitted claim documents for reimbursement of medical expenses. On scrutiny of documents, it is
observed that the Insured patient has taken treatment in the Surendra hospital –Rewari which is an
excluded provided hospital. The hospital is designated as Excluded hospital on 13.8.2020. From the above
finding, it was noted that the insured patient has taken treatment in the excluded provided hospital which
is not payable as per Excluded Providers - Code Excl 11. As per Excluded Providers - Code Excl 11, the
Company is not liable to make any payment in respect of expenses incurred towards treatment in any
hospital or by any Medical Practitioner or any other provider specifically excluded by the Insurer and
disclosed in its website / notified to the policyholders is not admissible. However, in case of life
threatening situations or following an accident, expenses up to the stage of stabilization are payable but
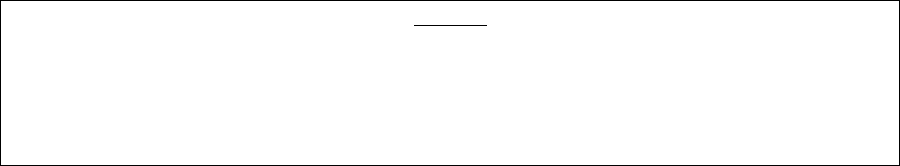
not the complete claim. Hence, the claim was repudiated and communicated to the insured vide letter
dated 16/10/2021. They requested for dismissal of complaint.
19. Reason for Registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called for hearing, both the parties are present and recall their arguments as noted in Para 18 above.
Complainant stated that due to emergency he got admitted in Surendra hospital –Rewari. The denial of
claim by insurance company is not in order. He requested for payment of his claim.
During online hearing, the company was advised to explore the possibility of review of the claim to arrive
at an agreement. Insurance Company reiterated their stand of SCN and stated that their repudiation
decision is in order.
On examination of various documents available in file including the copy of complaint, SCN filed by
insurance company, submissions made by both the parties at the time of online hearing, and it is seen
that the complainant hospitalization claim for Typhoid Fever has been denied by insurance company vide
letter dated 16-10-2021. The denial has been done mainly due to reasons as per Excluded Providers - Code
Excl 11 which states that “Excluded Providers - Code Excl 11 of the above policy, the expenses incurred
towards treatment in any hospital or by any Medical Practitioner or any other provider specifically
excluded by the insurer and disclosed in its website / notified to the policyholders are not admissible.”
On perusal of the same as well as policy conditions it is evident that the repudiation made by the insurer
is in line with the policy terms, clauses and conditions. Accordingly, the claim has been repudiated
correctly by the insurer and does not warrant any intervention at our end. The complaint is rejected being
devoid of merits.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of hearing, the claim has been repudiated correctly by the insurer and
does not warrant any intervention at our end. The complaint is rejected being devoid of merits.
(Atul Jerath)
Insurance Ombudsman
April 26, 2022
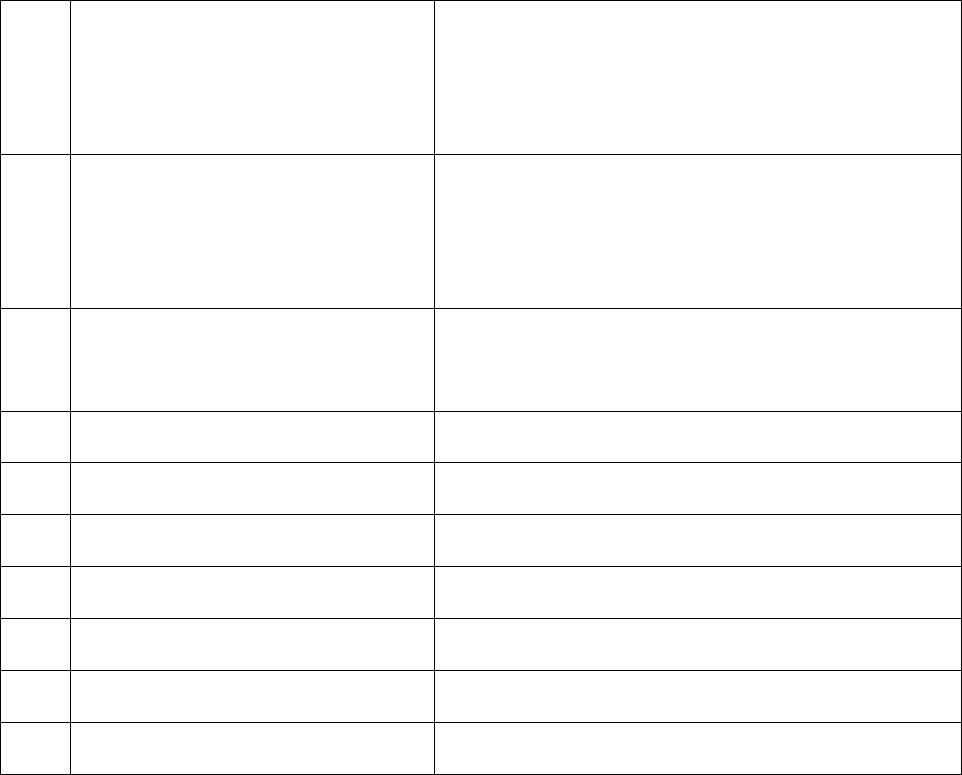
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman- Shri Atul Jerath
Case of Apoorva Kumar Gupta v/s Star Health and Allied Insurance Co.
Ltd. Complain
t Ref no: CHD-H-044-2122-0987
1.
Name & Address of the Complainant
Shri Apoorva Kumar Gupta
Spinning Department, GBTL Limited
Bhiwani-127021
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/211128/01/2021/003104
Group Policy – SI – Rs 3.00 Lacs
31/03/2021 to 30/03/2022
3.
Name of the insured
Name of the policyholder
Apoorva Kumar Gupta
GBTL Limited
4.
Name of the insurer
Star Health and Allied Insurance Co. Ltd.
5.
Date of Repudiation
08-07-2021
6.
Reason for repudiation
Misrepresentation of facts
7.
Date of receipt of the Complaint
22-02-2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs 2,42,074/- (As per SCN).
10.
Date of Partial Settlement
Not applicable
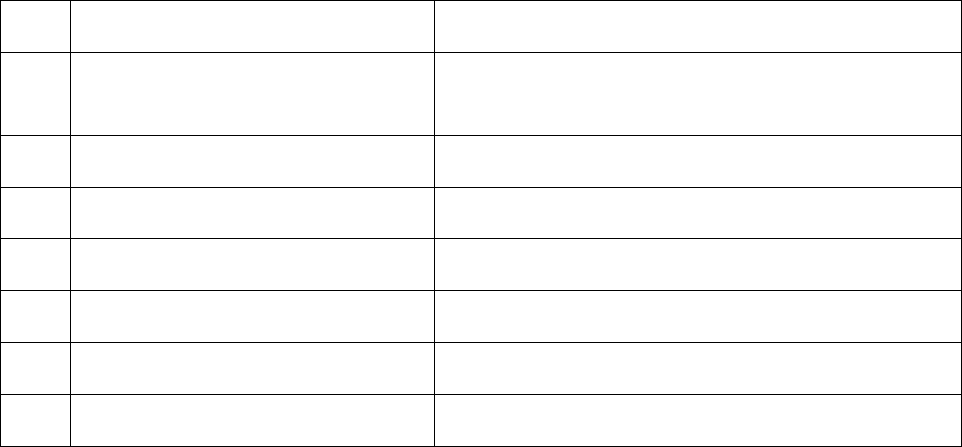
11.
Amount of relief sought
Rs 2,42,074/- (As per SCN).
12.
Complaint registered under Rule no:
Insurance Ombudsman Rules, 2017
Rule 13 (1)(b) – any partial or total repudiation of claims
by an insurer
13.
Date of hearing/place
13-04-2022/ Online hearing
14.
Representation at the hearing
For the Complainant
Shri Apoorva Kumar Gupta, Complainant
For the insurer
Smt Mamta Gupta, Senior Manager (Claims)
15
Complaint how disposed
Recommendation under Rule 16
16
Date of Award/Order
13-04-2022
17. Brief Facts of the Case: Shri Apoorva Kumar Gupta (hereinafter, the Complainant) has filed this
complaint against Star Health and Allied Insurance Co. Ltd (hereinafter, the Insurers), for repudiating his
wife’s covid reimbursement claim.
18. Cause of Complaint:
a) Complainant’s argument: On 22-02-2022, Shri Apoorva Kumar Gupta filed a complaint that their company
took Star Health Group Mediclaim Policy first time in April 2021. At that time Star Health Team provided
a list of panel hospital and claim Form Part-A & B but not provided the excluded hospitals list. So, they
were not aware about the same. When they came to know about the exclusion of SMSG hospital from
Star Health local branch manager, Mr Vijay Sharma on 26 June 2021, they immediately informed all our
employees not to take medical treatment in excluded hospitals.
In communication insurance company mentioned that the team Insured was duly informed about the
exclusion during the admission in the Hospital but as per insured, no-one told him about the exclusion.
Star Health executive collected patient and hospital details from us and provided a claim reference
number for further processing. If the hospital was in excluded list than why insurance company registered
this case and provided claim reference number to the Insured. He also objected on rejection reason
because previously this case was rejected saying that "Patient was not admitted in the hospital" which
was not correct and now they are saying that this case is rejected because the said hospital was in
excluded list. He did compliance of all claim related formalities. He requested for claim payment on
priority.
b) Insurers’ argument: In the SCN insurance company stated that the Insured Mr. Apoorva Kumar
Gupta along with his Family (Mr. Ashok Kumar Gupta –father, Ms. Madhuri Gupta- Spouse, Ms.Manju
Gupta – Mother, Ms. Akshadha Gupta-dependent Daughter) are covered in the Star Group Health
Insurance - Revised through Branch Office – Bhiwani, issued to M/s GBTL LIMITED for the floater Sum
Insured of Rs. 3,00,000/- vide policy no. P/211128/01/2021/003104 for the period of 31.03.2021 to
30.03.2022. The Insured has reported the claim in Group Mediclaim Insurance Policy. As per Claim form,
the Insured claimed an amount of Rs. 2,42,074/- during reimbursement of medical expenses. The Insured,
Madhuri Gupta 40 years / Female, was admitted on 18/05/2021 in SMSG Multi-specialty Hospital-Bhiwani
and discharged on 27.05.2021. As per Discharge Summary, he was diagnosed with COVID 19. The Insured
has submitted claim documents for reimbursement of medical expenses. On scrutiny of the claim
documents and Investigation Report, it is observed that the date of discharge as per discharge summary
and claim form submitted to us by the Insured is 26-05-2021, however, as per Hospital Final Bill and ICP
date of discharge mentioned is 27-05-2021 even all pharmacy bills submitted are of 27-05-2021. The vital
chart, and medication chart are prepared upto dated 27-05-2021. In Final bill (hospital Bill) submitted is
Rs 1,53,600/- but duplicate bill provided to our investigator on 18.11.2021 during his visit is of Rs
1,22,000/. In duplicate bill catheterization charges in Qty shown is 01, where as in hospital bill submitted
is in Qty written is 02. DOA and DOD are mentioned on the discharge summary submitted them, but on
copy of discharge summary no dates of DOA and DOD is mentioned this means there are 02 discharge
summaries for the claim Purpose. In nursing admission assessment form (ICP age 07/23) the temp shown
is 98.8 0F means normal, SPO2 level shown is 95% but in reason for coming to hospital written is fever,
cough and SOB (ICP page 07/23) same way shown in Vital chart of 18 & 19.05.2021 (16/23). There is no
document with treating Dr/ another Dr stamp. No OPD slip or emergency certificate of admission date.
ICPs are written in stereotyped handwriting. Thus, there is discrepancy in the records which amounts to
misrepresentation of facts. From the above finding, it is noted that there is discrepancy regarding the
hospitalization which amounts to misrepresentation of facts, the same is not payable. As per terms and
Conditions of the policy. Hence, the claim was repudiated and communicated to the Insured vide letter
dated 08/07/2021. They requested for dismissal of complaint.
19. Reason for Registration of Complaint: Repudiation of claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion):
Case called, both parties are present and recall their arguments as noted in Para 18 above.
Complainant stated that his wife claim filed under the policy has been repudiated on flimsy ground by
Insurance Company Limited. He requested for payment of his wife covid 19 reimbursement claim. During
online hearing, the company was advised to explore the possibility of review of the claim to arrive at an
agreement. Insurance Company reiterated their stand of SCN and stressed on discrepancies in IPD papers
and maintenance of hospital records.
On examination of various documents available in file including the copy of complaint, SCN filed by
insurance company, submissions made by both the parties at the time of online hearing, it is seen that in
the instant complaint, insurance company primarily repudiated the complainant’s wife hospitalization
expenses claim on account of discrepancies noted in the medical records of hospital.
In the instant case, the complainant was admitted as per advice of the treating doctor in which
complainant has no role. Further, insurance company can’t put whole onus on the complainant for
discrepancies noted in the medical record. On the other hand, it is duty of complainant also to satisfy the
query of insurance company in order to facilitate them for making decision on merit of the documents
before them.
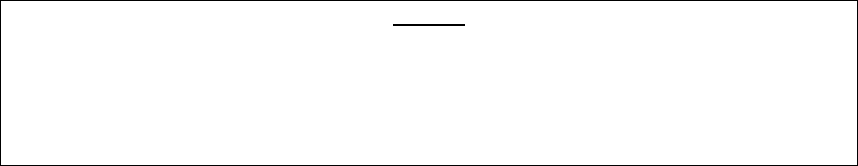
As such to meet end of Justice, it is directed to have a joint meeting of complainant and insurance
company with the hospital doctor to clarify the issues raised by insurer. During online hearing complainant
agreed to arrange a meeting with hospital authorities within seven days and insurer consented to the
same. Post the meeting, if satisfied with the clarification by the treating doctor, insurer agreed to settle
the claim as per policy terms and condition within 30 days.
Accordingly, an agreement by way of conciliation was arrived at between the insurer and complainant,
which I consider as fair and reasonable for both the parties.
AWARD
The complaint is resolved in terms of agreement of conciliation arrived at between the
complainant and insurers as stated above. Accordingly, both the parties should implement this
agreement within 30 days.
(Atul Jerath)
Insurance Ombudsman
April 13, 2022
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Atul Jerath
Case of Ms Madhuri Garg V/S National Insurance Company Ltd.
Complaint Ref. NO: CHD-H-048-2122-0913
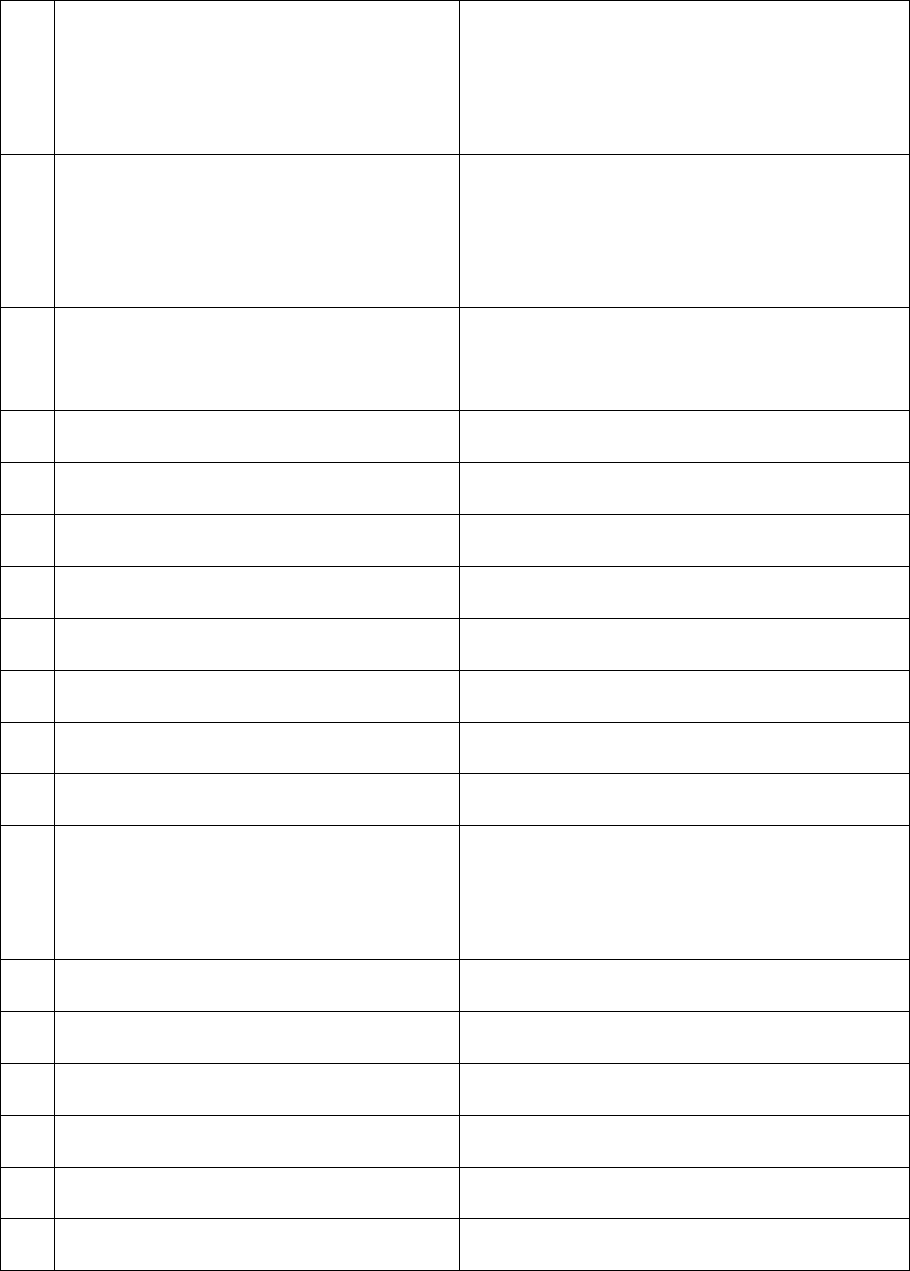
1.
Name & Address of the Complainant
Ms Madhuri Garg
Central Bank of India
Pinjore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
251100502010000260
IBA-Central Bank of India
01.10.2020 to 30.09.2021
3.
Name of the insured
Name of the policyholder
Central Bank of India
Madhuri Garg
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
No repudiation
6.
Reason for repudiation
Non submission of papers
7.
Date of receipt of the Complaint
31.01.2022
8.
Nature of complaint
Non settlement of health claim
9.
Amount of Claim
Rs. 2,03,350/-
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs. 2,03,350/-
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claims by an insurer
13.
Date of hearing/place
21.04.2022 Online hearing, Chandigarh
14.
Representation at the hearing
For the Complainant
Ms Madhuri Garg
For the insurer
Sh Ranjan Bhatia
15
Complaint how disposed
Recommendation under Rule 16
16
Date of Award/Order
22.04.2022
17. Brief Facts of the Case: Ms Madhuri Garg (hereinafter, the complainant) has filed this complaint
against National Insurance Co. Ltd. (hereinafter, the insurers) alleging incorrect denial of his wife's covid
19 claim.
18. Cause of Complaint: Non settlement of health claim.
a) Complainant’s argument: On dated 31.01.2022, Mrs Madhuri Garg has stated that she is a employee
of Central Bank of India. She had lodged health claim of her husband Sh Parminder Walia at HITPA
TPA under policy no.251100502010000260 on 21.06.2021. But his claim is still pending.
She has further stated that she lodged claim for the hospitalization claim of her husband on 21.06.2021
for Rs. 2,03,350/-. She submitted all the claim documents as required by customer care. On dated
23.09.2021, customer care officer told on telephone that there are some queries in the claim documents
as per their letter dated 16.08.2021 wherein they called for hard copy of all the documents. But she
never received that letter before that. She was never asked for original papers by any executive. She
sent the same in the last week of October 2021. The customer care executive confirmed the receipt of
papers on 21.11.2021. In the month of December she was raised another query. After that she lodged
complaint with grievance department who again raised another query which was different from the
previous one which she got in the month of January through speed post.
She was told that his husband's claim was closed due to non submission of reply of three notices whereas
she received only one notice in the first week of January 2022.
b) Insurer’s Argument: As per SCN, Sh Parminder Singh Walia admitted as a case of Covid 19
positive, Viral pneumonitis, Type 1 Respiratory Failure from 16.05.2021 to 25.05.2021. Claim
was submitted for Rs. 2,03,350/-. Since, the Company did not receive complete reply to the
queries, the claim was closed on 31.12.2021. Hence, the insured lodged complaint with the
ombudsman.
The claim was revisited. The following documents were required to process the claim:
1. Original bill against the bill dated 20.05.2021,21.05.2021 and 22.05.2021(submitted one
are in duplicate)
2. Original numbered payment receipt of RS. 50000/- against th final bill from hospital. The
Insurance Company has receipt for RS. 51,050/-Provide remaining.
3. Duly filled and signed KYC Form along with following documents(Ration card/DL/Aadhar
Card/Vote card/Passport/Any other government authorized identity proof of the
proposer carrying name, photograph and address.
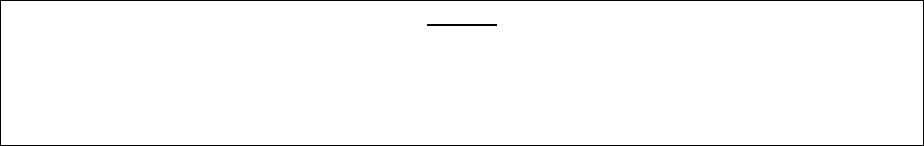
19. Reason for Registration of Complaint: Non settlement of 4 health claims.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion): Case called for hearing. Both
parties are present and recall their arguments as noted in Para 18 above
During online hearing the complainant has informed that she had lodged the claim of hospitalization on
21.06.2022. She submitted all the claim papers but till date her claim was not settled. The representative of
insurance company has stated that the claim was closed due to non submission of original claim papers after
three reminders.
It was enquired from the insurance company whether in the view of the facts emerging, they would like to re-
look at the issue with regard to settle the claim. The representative of the insurer agreed to review the
settlement subject to submission of orignal claim papers and as per terms and conditions of the policy.
Accordingly, an agreement by way of conciliation was arrived at between the insurer and complainant, which
I consider as fair and reasonable for both the parties. The complainant is directed to submit the original claim
papers to the Insurance Company within 7 days.
In the light of the amicable settlement of complaint between the parties, the complaint is disposed- off with a
direction to the company shall comply with the agreement and shall send a compliance report to this office
within 30 days after the receipt of papers from the complainants for information and record.
AWARD
The complaint is resolved in terms of agreement of conciliation arrived at between the complaint and
insures as stated above. Accordingly, both the parties should implement this agreement within 30
days.
(Atul Jerath)
Insurance Ombudsman
Dated: 22.04.2022
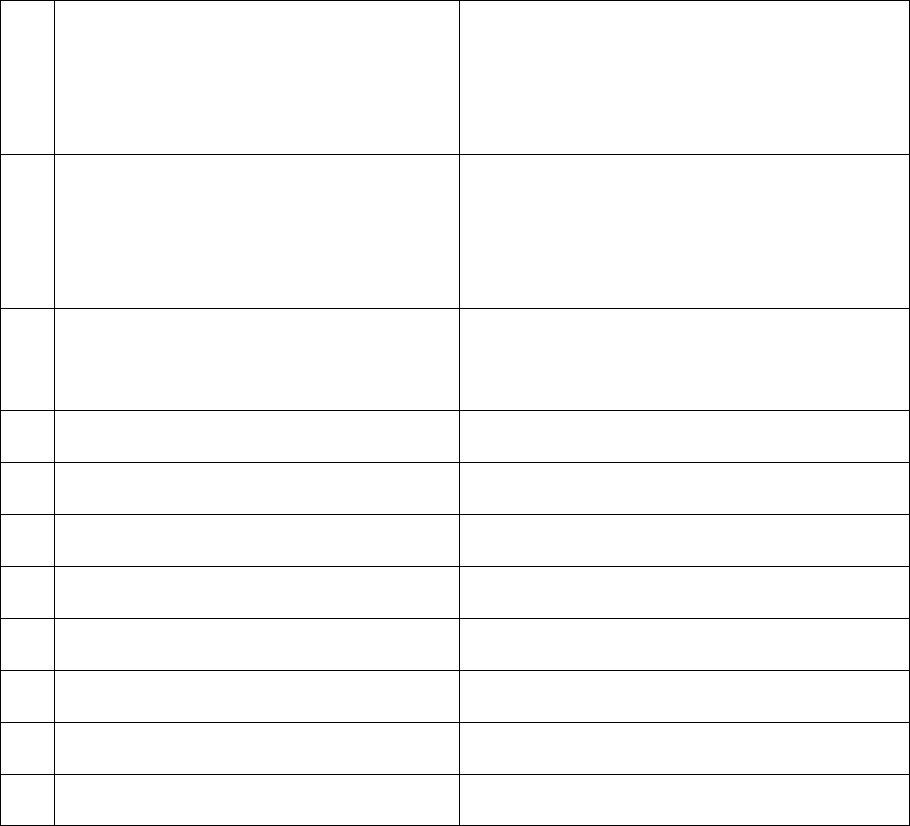
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, CHANDIGARH
(Under Rule 13 r/w 16/17 of the Insurance Ombudsman Rules, 2017)
Insurance Ombudsman: Shri Atul Jerath
Case of Kiran Singhal V/S National Insurance Co. Ltd.
Complaint Ref. No: CHD-H-048-2122-0962
1.
Name & Address of the Complainant
Mrs Kiran Singhal
H No. 5516, 38 West
Chandigarh
2.
Policy No:
Type of Policy
Duration of policy/Policy period
251100502010000345
IBA UCO Bank
29.10.2020 to 28.10.2021
3.
Name of the insured
Name of the policyholder
UCO Bank
Sh B P Singhal
4.
Name of the insurer
National Insurance Company Ltd.
5.
Date of Repudiation
No repudiation
6.
Reason for repudiation
Non Settlement of health claim
7.
Date of receipt of the Complaint
08.02.2022
8.
Nature of complaint
NA
9.
Amount of Claim
4 Lacs
10.
Date of Partial Settlement
NA
11.
Amount of relief sought
Rs 4 lacs
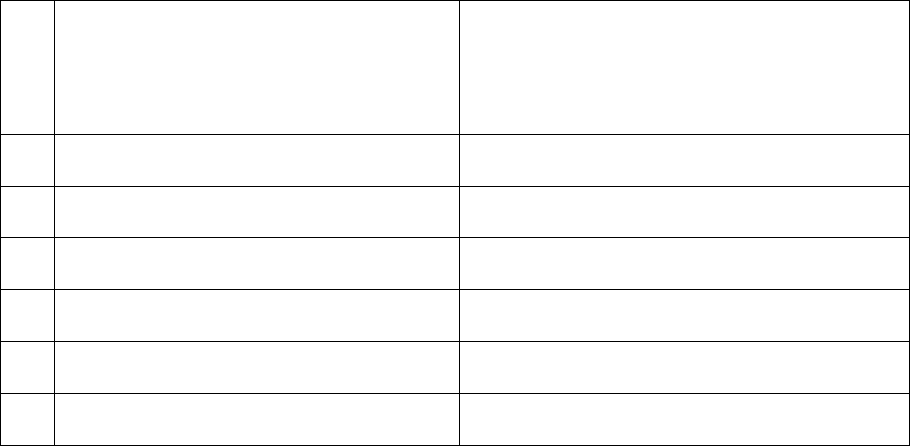
12.
Complaint registered under
Rule no: Insurance Ombudsman Rules,
2017
Rule 13 (1)(b) – any partial or total repudiation
of claims by an insurer
13.
Date of hearing/place
21.04.2022
14.
Representation at the hearing
For the Complainant
Mrs Kiran Singhal
For the insurer
Sh Ranjan Bhatia
15
Complaint how disposed
Recommendation under Rule 16
16
Date of Award/Order
22.04.2022
17. Brief Facts of the Case:
(hereinafter, the complainant) has filed this complaint against Aditya Birla Health Insurance Co. Ltd.
(hereinafter, the insurers)
18. Cause of Complaint: Non settlement of health claim
a) Complainant’s argument : On 14.02.2022, Mrs Kiran Singhal has stated in her complaint that her
husband Sh B P Singhal suffered from Covid 19 and was admitted in Santokh Nursing Home, Sector 38,
Chandigarh on 15.05.2021. He was shifted to PGIMER on 18.05.2021 as his condition was worsended.
He was put on ventilator on 20.05.2021 and expired on 11.07.2021.
She had submitted all the original documents to the company in September 2021. She had paid Rs.
88,417/- to Santokh Nursing Home and Rs. 65,261/- to PGIMER.
But the Insurance Company keep on raising serveral queries one after another. She replied all the
queries from time to time after visiting the above hospitals a number of times. The
Insurance Company is demanding original Discharge Summary of Santokh Nursing Home. She requested
the hospital many times, but the hospital did not provide the same, instead they issued Discharge
Certificate which was attested and verified by the hospital but the word dulpicate was written on the
Discharge Certificate. The original Discharge Certificte might have been retained by the PGI on
18.05.2021.
But the Insurance Company is repeatedly asking for the same documents as below:
1. Provide Covid Report:
Reply: She has already submited in the claim paers of Santokh Nursing Home.
2. Provide Original Final Bill cum receipt for Hospitalizatin from 18.05.2021 to 11.07.2021 with
supporting documents or provide details regarding the payment of Rs 5000/- on 11.07.2021.
Reply: His husband remained on ventilator from 20.05.2021 tol 11.07.2021. Rs. 5000/- were ICU
Charges taken by PGIMER from 18.05.2021 till 11.07.2021. Treatment given and whatever tests
were conducted on him, they were on daily and hours to hour basis and all medicines were being
brought by us everyday a number of times. Details of all the medicine bills and Investigation test slips
were duly signed by PGI Doctors were submitted by her while lodging the claim.
3. Provide all original reports against investigation duly claimed.
Reply: Her husband remained in ICU and on ventilator and during that period serveral tests were
conducted on him. Docotrs check the reports on their computers, so these test reports were not
provided by them to her. All tests, slips, money reeipts were deposited with the insurance company
duly signed by the PGIMER doctors.
She further stated that PGI is a renewed Govt hospital and the test slips issued by PGI should be valid for
the purpose of claim. She has requested the Forum to intervene and provide justice.
Insurer’s Argument: As per SCN, the Insurance Company has stated that the patient Sh B P
Singhal admitted in Santokh Nursing Home on 15.05.2021 and discharged on 18.05.2021. They
received reimburement claim for Rs. 88417/-. On Scrutiny of claim , some claim objections were
raised which were partially replied by Mrs Kiran Singhal. The claim is lying pending for the want
of documents as below:
1. Provide Covid Report
2. Provide Original Final Bill cum receipt for Hospitalizatin from 18.05.2021 to 11.07.2021
with supporting documents or provide details regarding the payment of Rs 5000/- on 11.07.2021.
3. Provide all original reports against investigation duly claimed.
After that they received the reimbursement bill of RS 65,263/- of PGI which is also pending for the want
of requisite documents against the main bill.
19. Reason for Registration of Complaint: Non settlement of health claim.
20. The following documents were placed for perusal:
a) Complaint to the Company b) Copy of Policy Document
c) Annexure VI-A d) Reply of the Insurance Company
21. Result of Personal hearing with both parties (Observations & Conclusion): Case called for hearing. Both
parties are present and recall their arguments as noted in Para 18 above.
During online hearing, the complaint stated that her husband was contacted with Covid
19 and was admitted in Santokh Nursing Home. He was referred to PGIMER on 18.05.2021 wherein he expired
on 11.07.2021. She had submitted all the claim papers but in spite of sending all the documents, the Insurance
Company is asking for submission of papers again and again. The representative of the Insurance Company
stated that the claim was closed due to non submission of claim papers.
During the online hearing, it was enquired from the insurance company whether in the view of the facts
emerging; they would like to re-look at the issue with regard to settle the claim. The representative of the
insurer agreed to review the settlement subject to submission of claim papers and as per terms and conditions
of the policy.
Accordingly, an agreement by way of conciliation was arrived at between the insurer and complainant, which
I consider as fair and reasonable for both the parties.
In the light of the amicable settlement of complaint between the parties, the complaint is disposed- off with a
direction to the complainant to end the required papers or forwarding letter along with courier receipt
confirming that all the required papers are already submitted. The company shall comply with the agreement
and shall send a compliance report to this office within 30 days after the receipt of papers from the
complainants for information and record.
AWARD
The complaint is resolved in terms of agreement of conciliation arrived at between the complaint and
insures as stated above. Accordingly, both the parties should implement this agreement within 30
days.
(Atul Jerath)
Insurance Ombudsman
Dated: 22.04.2022
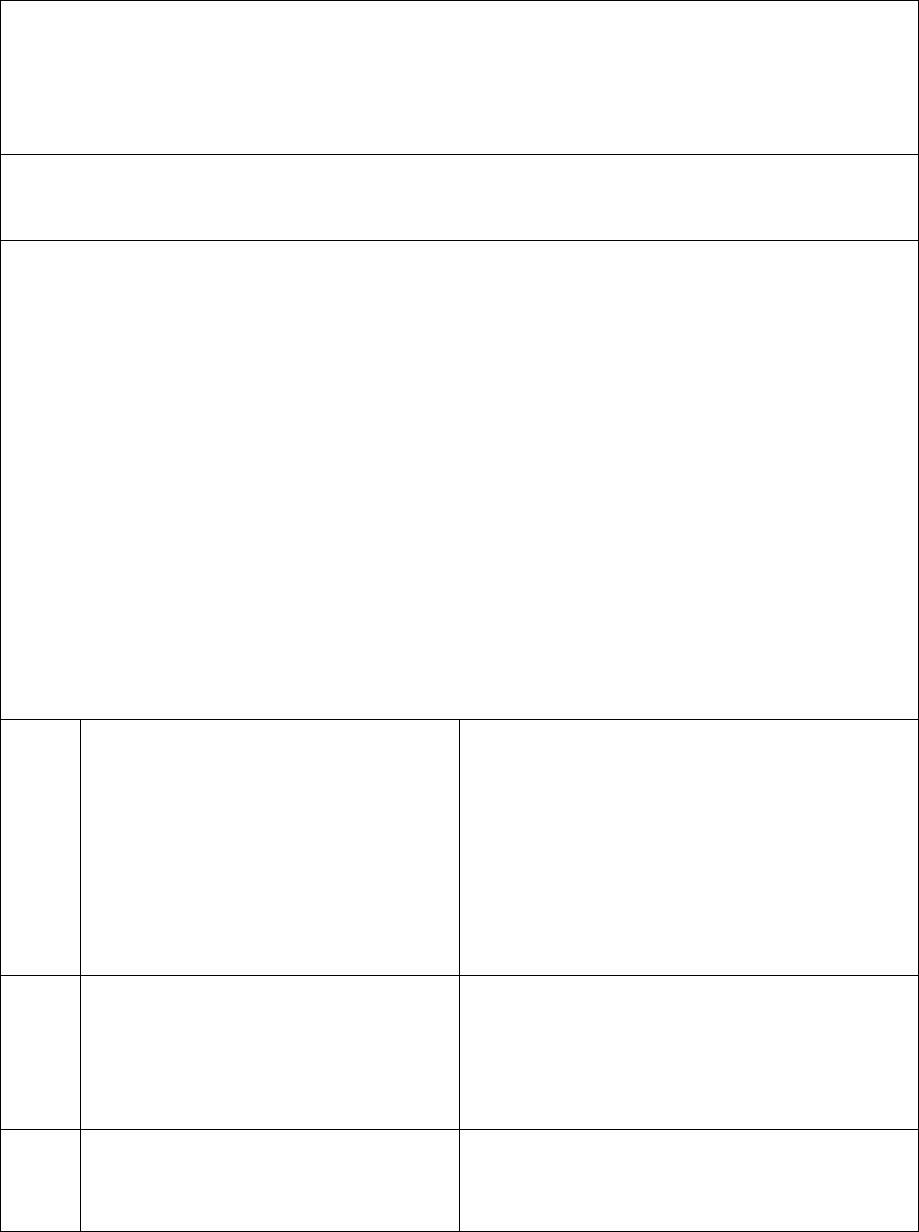
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Shri. N SANKARAN
Ombudsman
Case between: Mr. SRINIVAS MAJETI………………Complainant
Vs
M/s The National Insurance Co. Ltd………Respondent
Complaint Ref. No. I.O.(HYD).H .048.2223.0017
Award No.: I.O.(HYD)/A/HI/ 0002/2022-23
1.
Name & address of the complainant
Mr. Majeti Srinivas Staff 645772
Union Bank of India
Telagayapalem, Kakumanu Mandal,
Guntur District,
Andhra Pradesh- 522 112
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
25xxxxxxxxxxxx0250
Group insurance policy
01.10.2020 to 30.09.2021
3.
Name of the insured
Name of the Policyholder
Mr. Majeti Srinivas
M/s The Union Bank of India Ltd.
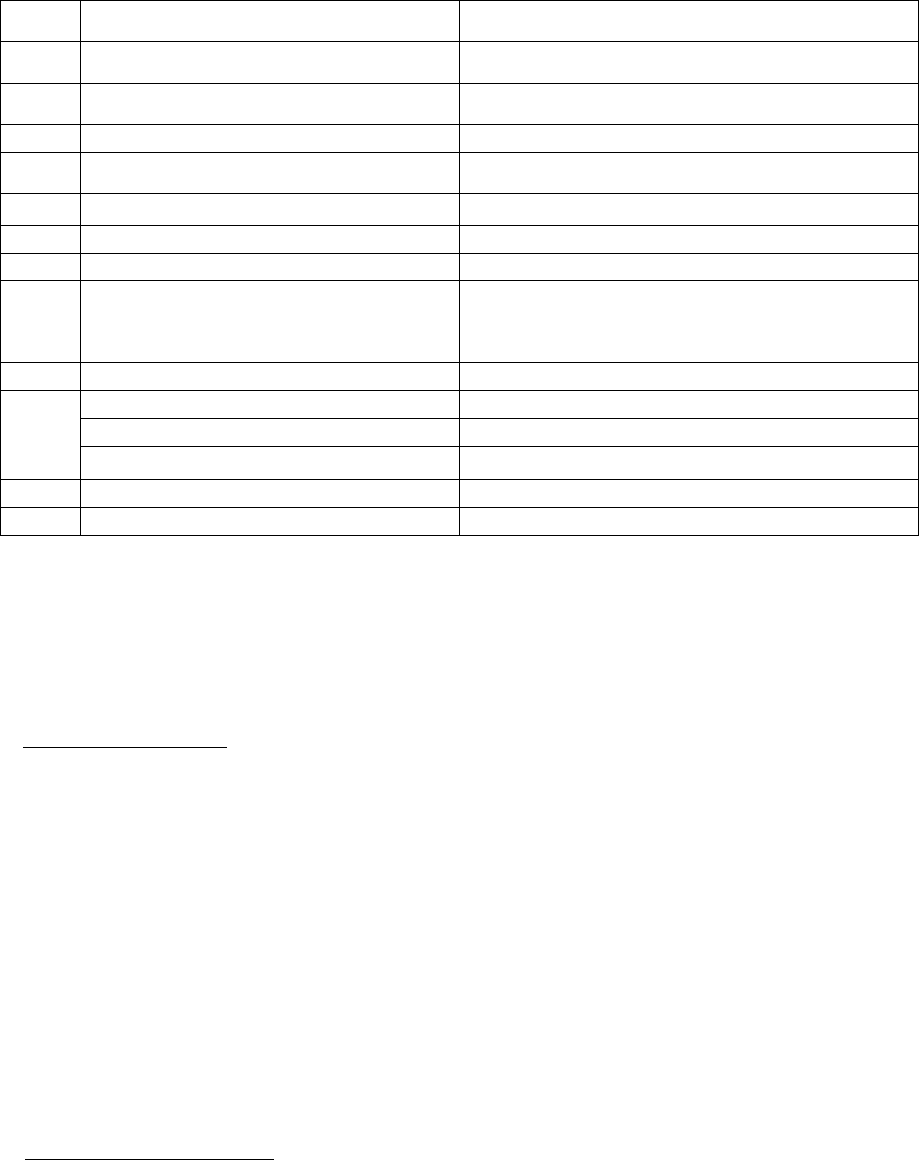
4.
Name of the insurer
M/s The National Insurance Co. Ltd.
5.
Date of Repudiation
24.08.2021
6.
Reason for repudiation
Deficiency in submission of documents
7.
Date of receipt of the Complaint
22.11.2021
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 96,822/-
10.
Date of Partial Settlement
-------
11.
Amount of Relief sought
Rs. 96,822/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation
of claims by the Life insurer, General Insurer or
the Health insurer
13.
Date of hearing/place
20.04.2022, online hearing Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr. Ranjan Bhatia, Manager
15.
Complaint how disposed
Allowed
16.
Date of Order/Award
21.04.2022
17) Brief Facts of the Case:
The complainant by virtue of being an employee of M/s The Union Bank of India was covered under the
group medical insurance policy that was issued by the respondent company. He was admitted in Sri
Kamakshi Care Hospital, Chirala where he underwent treatment for Covid-19 between 22.04.2021 and
29.04.2021 to undergo treatment for her diagnosed illness. Since her hospitalization claim was denied by
the respondent under the medical insurance policy, the complainant had approached this Forum to seek
justice.
18) Cause of Complaint: Repudiation of claim made against the medical Insurance policy.
a) Complainant’s Submissions:
In his letter addressed to this Forum, the complainant had stated that all the necessary documents for his
reimbursement claim were submitted to the TPA of respondent company through his employer.
Subsequently, a letter dated 24.08.2021 by the TPA was received, mentioning that the indoor case papers
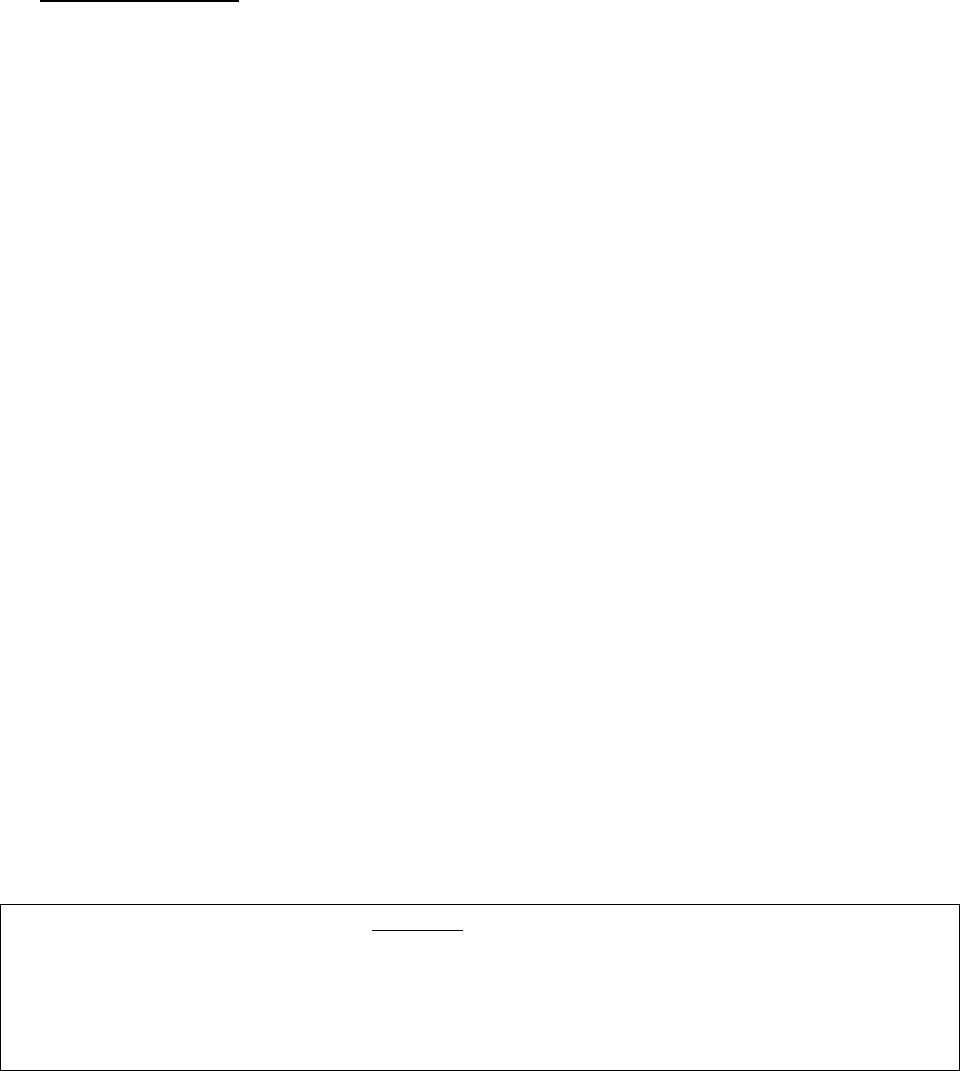
and RT-PCR test report were required to be furnished to process the claim. The complainant stated that
the indoor case records were already submitted to the TPA on 15.08.2021 along with Covid-19 test reports
dated 17.04.2021 and 22.04.2021. However, the claim was rejected giving no specific reason. Thereafter
he had represented the matter to the respondent’s Grievance department on 05.10.2021. As there was
no reply from the respondent, the complainant had to approach this Forum for speedy justice.
b) Insurer’s Submissions:
No SCN has been submitted. However, vide their email dated 13.04.2021, insurer has conveyed that as
per the policy terms and conditions, they are agreeable to settle the claim for an amount of Rs.96,822/-
as full and final.
19) Reason for Registration of Complaint:
The insurer rejected the claim preferred by the complainant. As the complaint falls under Rule 13.1(b) of
Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a. Policy copy along with terms and conditions
b. Discharge summary with final bill
d. Rejection letter
e. Correspondence with insurer
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum both parties attended the online hearing
The complainant reiterated the facts mentioned in his complaint. He stated that he had approached the
insurer for reimbursement of his medical expenses for an amount Rs.96,822/-. However, he informed
that after approaching the Forum, he has been offered full settlement of the claim, for which has agreed.
The respondent insurer submitted that after receipt of the complaint from the forum they have revisited
and reviewed the claim of the complainant. They have informed vide their mail dated 13-04-2022 of
their proposal for settlement of Rs.96,822/- in full and final settlement of the claim.
The forum asked the complainant whether he was agreeable to the amount offered by the insurance
company towards settlement of his claim. The Complainant stated that he is agreeable and is willing to
accept the offer of settlement made by the insurer. As the complainant has expressed his consent for the
above settlement, the forum directs the respondent insurer to admit and settle the claim immediately as
agreed upon mutually by both the parties.
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the parties
during the course of the hearing, the insurer is directed to settle the claim immediately as agreed upon
mutually by both the parties.
In result, the complaint is Allowed.
22) The attention of the Insurer is hereby invited to the following provisions of Insurance Ombudsman
Rules, 2017:
a) According to Rule 17(6), the insurer shall comply with the award within 30 days of the receipt of the
award and intimate compliance to the same to the Ombudsman.
b) According to Rule 17(7), the complainant shall be entitled to such interest at a rate per annum as
specified in the regulations, framed under the Insurance Regulatory & Development Authority of India
Act from the date the claim ought to have been settled under the Regulations till the date of payment
of the amount awarded by the Ombudsman.
c) According to Rule 17 (8), the award of Insurance Ombudsman shall be binding on the Insurers.
Dated at Hyderabad on the 21
st
day of April, 2022.
( N. SANKARAN )
INSURANCE OMBUDSMAN FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
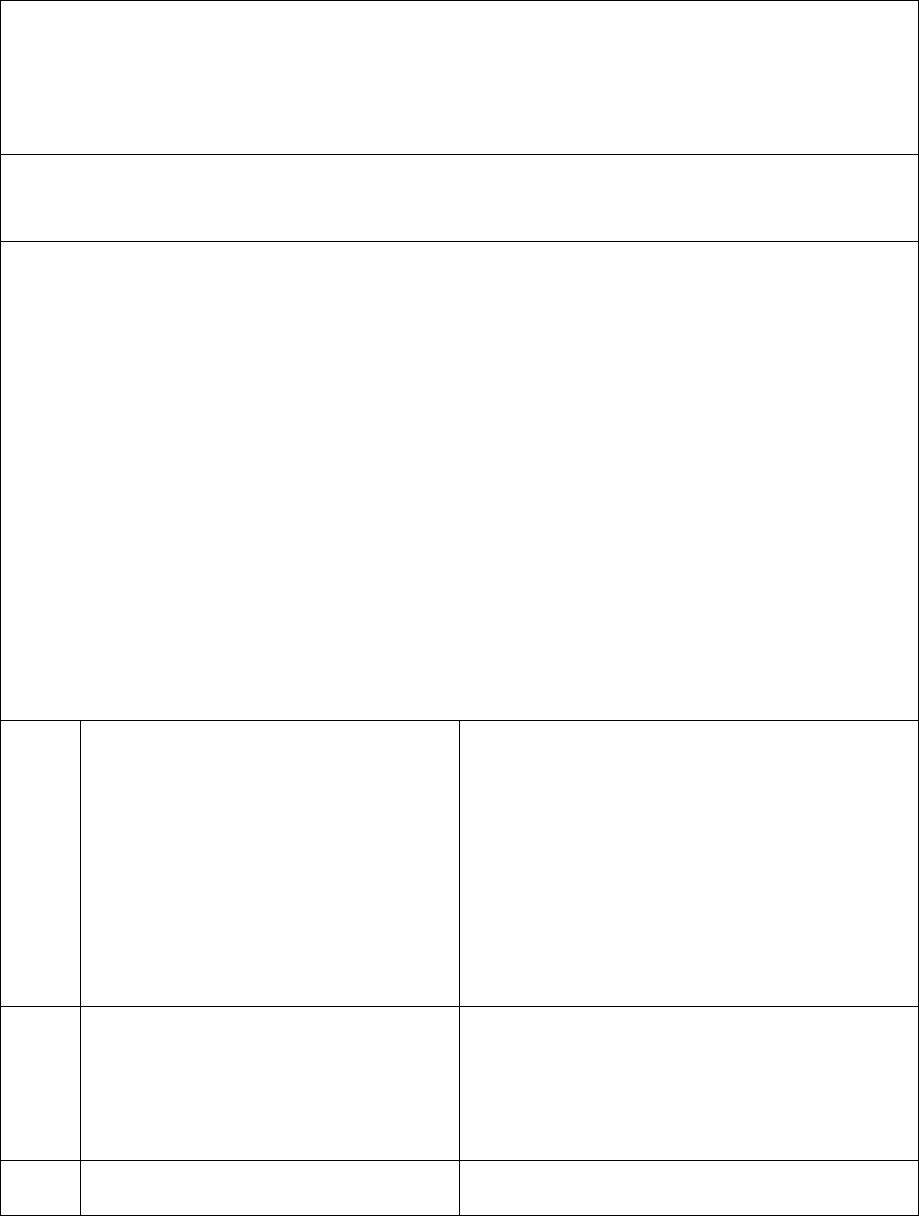
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATES OF A.P., TELANGANA & YANAM
(Under Rule 16(1)/17 of The Insurance Ombudsman Rules, 2017)
Shri. N SANKARAN
Ombudsman
Case between: Mr. B VIJAY KUMAR………………Complainant
Vs
M/s ICICI Lombard General Insurance Co. Ltd………Respondent
Complaint Ref. No. I.O.(HYD).H .020.2223.0049
Award No.: I.O.(HYD)/A/HI/ 0007 /2022-23
1.
Name & address of the complainant
Mr. B Vijay Kumar
Heritage Foods Limited VJA,
Besides IOB bank, Amaravati Arcade,
Door #11-511, Penamaluru Centre, Poranki
Village,Penamaluru Mandal, Vijayawada,
Andhra Pradesh- 521 137 .
2.
Policy No./Collection No.
Type of Policy
Duration of Policy/Policy period
40XX X XXXXX7929 00 000
Group Health (Floater) Insurance policy
21.04.2021 to 20.04.2022
3.
Name of the insured
Name of the Policyholder
Mr. B Vijay Kumar
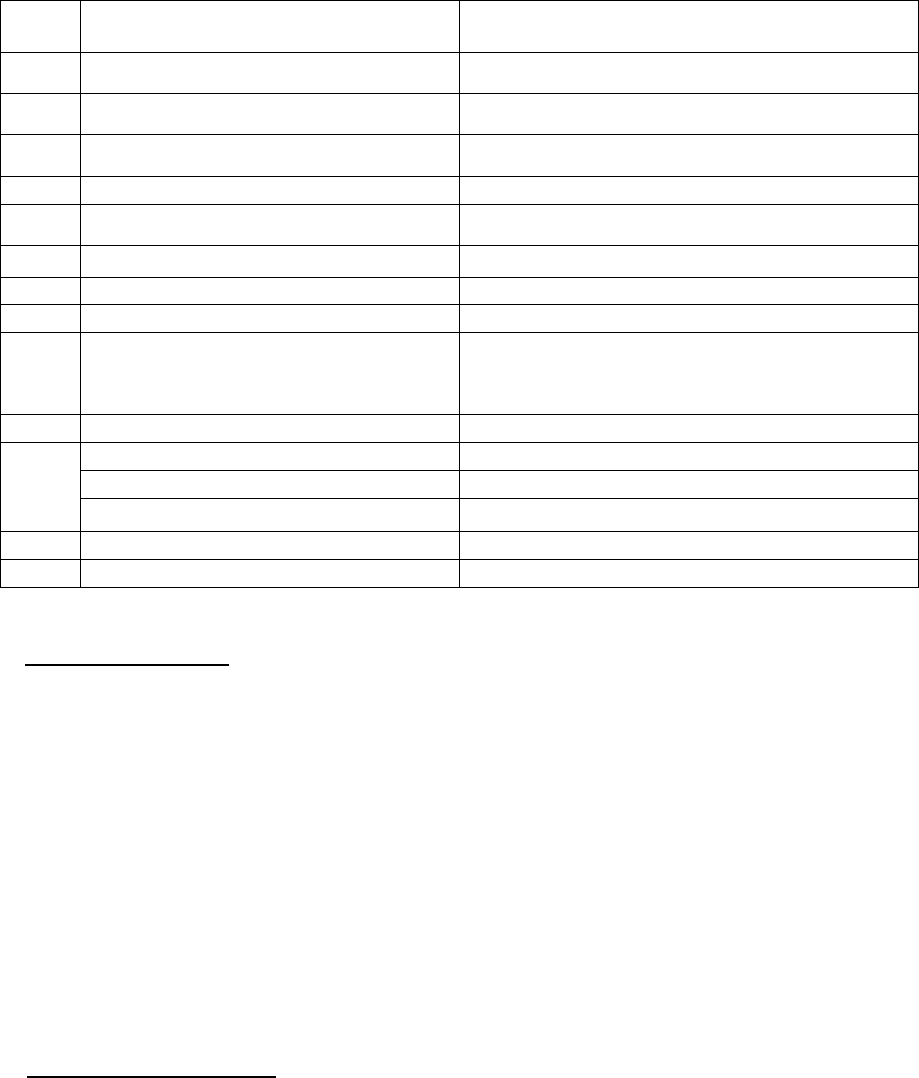
17) Brief Facts of the Case:
The complainant was covered under the Group medical insurance cover issued by the respondent
company in the name of M/s Heritage Foods Limited. He was hospitalized in Shiva Hospitals, Guntur with
Broncho pneumonitis/ Covid Pneumonia between 14.05.2021 and 20.05.2021 where he was stated to
have been treated with IV antibiotics, steroid and put on oxygen support. Since his hospitalization claim
was denied by respondent under the group medical insurance policy, the complainant had approached
this Forum to seek justice.
18) Cause of Complaint: Repudiation of claim made against the Group medical Insurance policy.
a) Complainant’s Submissions:
In his letter addressed to this Forum, the complainant had submitted that he visited Arun Kidney Centre
as he had symptoms of Covid. He was advised to undergo CT scan. As the test report revealed mild acute
presence of Covid, he got tested at a government authorized centre and was directed to Covid care centre.
Since he could not withstand the cough and cold, he got admitted in Shiva Hospital where he was treated
and discharged on 20.05.2021. Subsequently, he had filed a claim for Rs. 295,747/- with the respondent
company which was rejected without citing any reason for the same. He had contacted the customer care
center of respondent company to ascertain the cause for rejection of his claim. He received a reply from
M/s Heritage Foods Limited
4.
Name of the insurer
M/s ICICI Lombard General Insurance Co. Ltd.
5.
Date of Repudiation
23.09.2021
6.
Reason for repudiation
Misrepresentation of material facts
7.
Date of receipt of the Complaint
23.02.2022
8.
Nature of complaint
Claim pertaining to medical insurance policy
9.
Amount of Claim
Rs. 2,95,747/-
10.
Date of Partial Settlement
------
11.
Amount of Relief sought
Rs. 2,95,747/-
12.
Complaint registered under
Rule No.13.1 (b) of Ins. Ombudsman
Rules, 2017
Rule 13.1 (b) – any partial or total repudiation
of claims by the Life insurer, General Insurer or
the Health insurer
13.
Date of hearing/place
25.04.2022, online Hyderabad
14.
Representation at the hearing
a) For the complainant
Self
b) For the insurer
Mr.Karan Bagdai, Manager, Legal
15.
Complaint how disposed
Disposed
16.
Date of Order/Award
28.04.2022

the respondent company on 17.01.2022 that his claim was rejected on account of incorrect statements
and representation by him. He was asked by the enquiry team to give his response to which he informed
them that he got admitted in the hospital because he had kidney infection.
b) Insurer’s Submissions:
Self contained note was submitted by the respondent. They had issued a Group Health Insurance policy
to Heritage Foods Limited covering their employees. They received a reimbursement claim from the
Mr.B.Vijay Kumar for hospitalization at Shiva Hospital, Guntur on 14.05.2021 and diagnosed with Covid
Pneumonia. The complainant made a claim for Rs.295747/-. During investigation of the claim, they
observed from the written statement made by the insured confirming he had paid Rs.2,30,000/- for
hospital bills, Rs.51647/- as Pharmacy bills and Rs.14100/- as Lab bills and all of which were paid by cash.
On verification with the hospital, they found that he had incurred an amount of Rs.285747/- and had
requested the hospital to hike an amount of Rs.10,000/-. The hospital authority vide their letter dated
23.08.2021 had confirmed that they have not provided any break up of pharmacy and lab bills and on the
request of the complainant, the hospital had exaggerated the bill by Rs.10,000/-.
As the Company observed a fraudulent activity, the policy was treated as null and void and the claim of
the complainant was not entertained as per clause Part III of the Policy: Standard terms and conditions
applicable to group benefits 1. Incontestability and Duty of Disclosure :”The policy shall be null and void
and no benefit shall be payable in the event of untrue or incorrect statements, misrepresentation,
misdescription or on non-disclosure in any material particular in the proposal form, personal statement,
declaration and connected documents, or any material information having been withheld, or a claim being
fraudulent or any fraudulent means or devices being used by the Insured or any one acting on his behalf
to obtain any benefit under this policy”. Clause 8. Fraud: “If any claim made by the insured person, is in
any respect fraudulent, or if any false statement, or declaration is made or used in support thereof, or if
any fraudulent means or devices are used by the insured person or anyone acting on his/her behalf to
obtain any benefit under this policy, all benefits under this policy shall be forfeited. Any amount already
paid against claims which are found fraudulent later under this policy shall be repaid by all person(s)
named in the policy schedule, who shall be jointly and severally liable for such repayment.” Therefore the
claim of the complainant was rejected by the Company and the same was communicated vide rejection
letter dated September 03, 2021. It is therefore submitted that the claim is not payable and the Hon'ble
Ombudsman may be pleased to absolve us of the liability.
19)The claim preferred by the complainant was denied by the insurer. As the complaint falls under Rule
13 (b) of Insurance Ombudsman Rules, 2017, it was registered.
20) The following copies of documents were placed for perusal:
a) Policy with terms and conditions
b) Rejection mail
c) Correspondence with insurer
d) Self contained note with enclosures.
21) Result of the personal hearing with both the parties:
Pursuant to the notices given by this Forum both the parties attended online hearing at
Hyderabad.
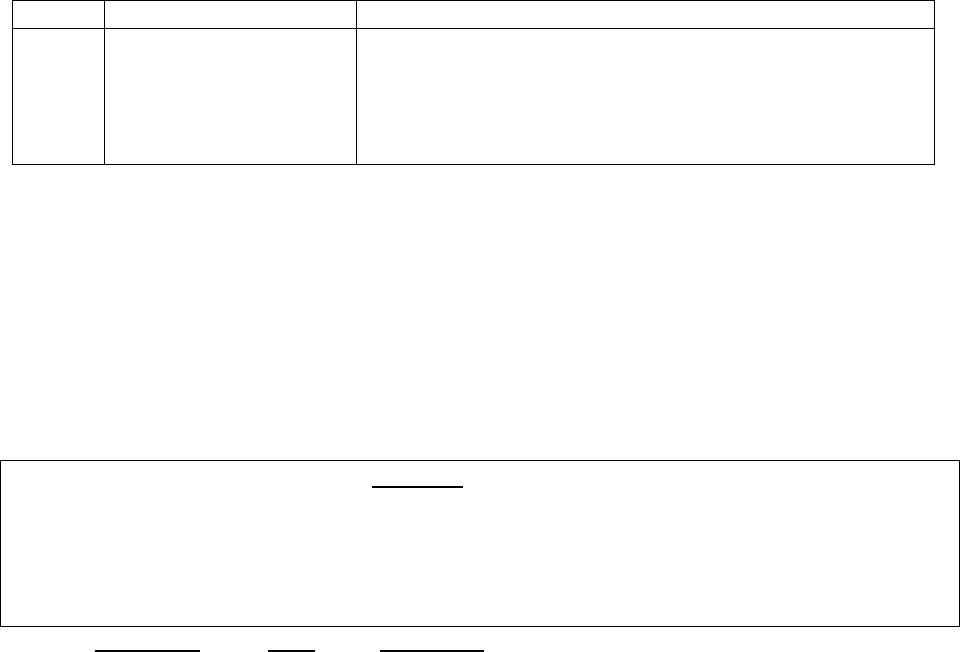
The complainant submitted that he was admitted in Shiva Hospital, Guntur from 14.05.2021 to
20.05.2021 and was diagnosed Covid positive. His claim towards hospitalization expenses was rejected by
the insurance company without giving him any reason. He had intimated the claim to his employer M/s
Heritage Foods Limited who had taken the Group Policy.
The respondent insurer submitted that on investigation of the claim they found that the insured
had hiked the hospitalization bill by Rs.10,000/-. He had paid an amount of Rs.2,85,747/- whereas he had
submitted a reimbursement claim for Rs.2,95,747/-. Since this act on the part of the insured amounted to
Fraud, as per policy conditions Part 3 Clause 1 & 8 the claim was rejected and letter dated 03.09.2021 was
sent to the insured as under:
Sr.No
Reason
Description
1
Fraudulent Claims
1. As per GHI guidelines part 3 schedule exclusion clause
1 & 8 in the event of untrue or incorrect statements,
misrepresentation, misdescription in any material and
connected documents are not payable hence the claim
rejected.
The insured submitted that he had approached the respondent insurer for providing him the
original information to reject his claim and he had not received the response from the insurer. The Forum
observes that the rejection letter dated 03.09.2021 by the insurer mentions reason as ‘fraudulent claims’
and does not mention the specific documents based on which the decision was arrived at. From the
documents on record the Forum observes that the respondent insurer had not communicated the specific
documents for rejection and sought the insured’s response on the same. To this effect, there is non
observance of the principle of natural justice by the insurer. Considering the above aspect, the Forum
directs the respondent insurer to review the case and provide adequate opportunity to the insured to
support his claim and decide thereafter.
A W A R D
Taking into account the facts & circumstances of the case and the submissions made by both the parties
during the course of hearing and the documents submitted, the Forum directs the respondent insurer to
review the case and provide adequate opportunity to the insured to support his claim and decide
thereafter.
Dated at Hyderabad on the 28th day of April 2022.
(N.SANKARAN)
INSURANCE OMBUDSMAN
FOR THE STATES OF A.P.,
TELANGANA AND YANAM CITY
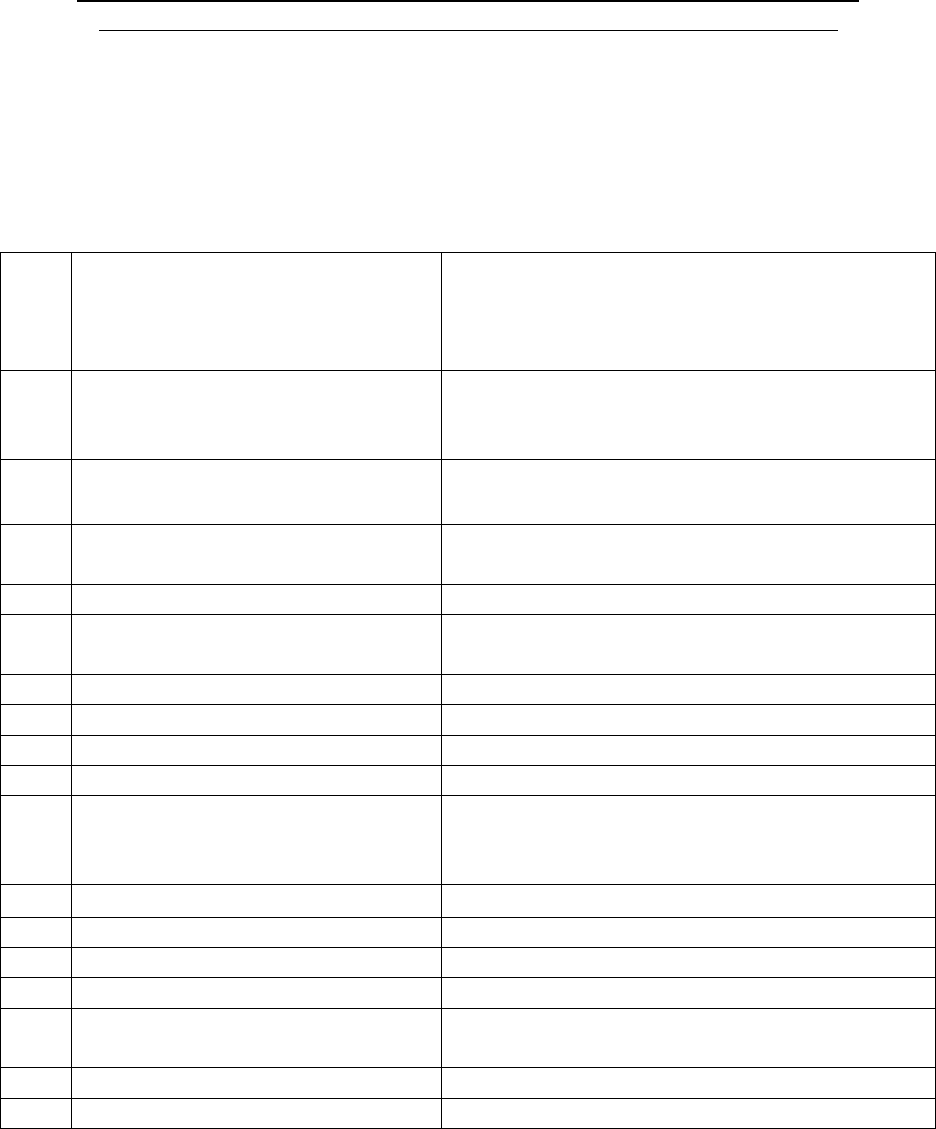
PROCEEDINGS BEFORE - THE INSURANCE OMBUDSMAN, STATE OF M.P. & C.G.
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULE 2017)
OMBUDSMAN – RAVINDRA MOHAN SINGH
Ms. Priyanshi Jain ….……….……………………………………………………..….. Complainant
V/s
Star Health & Allied Insurance Co. Ltd. ….…………………………………………Respondent
COMPLAINT NO: BHP-H-044-2122-0658 ORDER NO: IO/BHP/A/HI/0002 /2022-2023
• Ms. Priyanshi Jain (Complainant) has filed a complaint against Star Health & Allied
Insurance Co. Ltd. (Respondent) alleging repudiation of claim.
1.
Name & Address of the
Complainant
Ms. Priyanshi Jain
Plot No. 1, Rear Portion 408,
Vijay Nagar
Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
P/2xxxxx/xx/xxxx/xx9132
Star Group Health Insurance Plan
01.09.2020 to 31.08.2021
3.
Name of the insured
Name of the policyholder
Mr. Vijay Jain
Globalization HR Solutions India Pvt. Ld.
4.
Name of the insurer
Star Health Insurance and Allied Insurance Co.
Ltd
5.
Date of Repudiation/ Rejection
24.05.2021
6.
Reason for Repudiation/
Rejection
Treatment taken on OPD basis.
7.
Date of receipt of the Complaint
10.01.2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 64,317/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs. 64,317/ + Rs. 10,000/ for mental
harassment
12.
Complaint registered under Rule
Rule No. 13(1)(d) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
2022 at OIO Bhopal878/-
14.
Representation at the hearing
q) For the Complainant
Ms. Priyanshi Jain, over GoTo Meet App
r) For the insurer
Ms. Sonam Saxena, Manager over GoTo Meet
App
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
06.04.2022
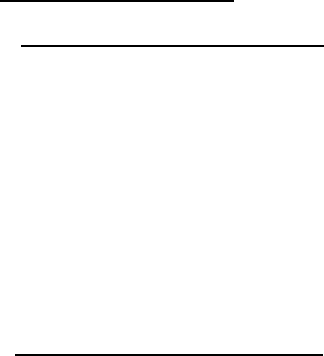
• Brief facts of the Case –
• Contention of the complainant - The complainant has stated that the claim was rejected
for taking treatment on OPD basis but her father was hospitalized at Gohil Sampurn
Hospital, Shajapur for emergency treatment from 15.04.2021 to 21.04.2021 for B/L Viral
Pneumonitis. HRCT was done on 15.04.2021and 50% involvement was there and CT score
was 12/25. As per Doctor, HRCT report was abnormal and hospitalization was done for 6
days. But the Company has not taken any action on her representation sent on 28.07.2021
and has approached this forum for redressal of grievance.
• Contention of the respondent –The respondent has stated that Ms. Priyansh Jai had
availed Star Group Health Insurance Policy covering SELF (Ms. PRIYANSHI JAIN), MOTHER
(Ms. ARCHANA JAIN) and Father (Mr. VIJAY JAIN) for a floater sum insured of Rs.
10,00,000/- vide Policy No. P/201115/01/2021/009132 for the period 01.09.2020 to
31.08.2021 and the same was renewed as Policy No. P/201115/01/2021/009132 for the
period from 01.09.2021 to 31.08.2022.The Insured, Mr. VIJAY JAIN, aged 60 years / Male,
has taken treatment for Viral Pneumonitis on 14.04.2020 at Vyas Hospital & Research
Centre and again taken treatment for Post Viral Pneumonitis on 21.04.2021 at Gohil
Sampurn hospital – Shajapur. Subsequently, the insured submitted documents for
reimbursement of medical expenses. Based on the submitted documents, it was observed
that the insured patient has taken treatment as an outpatient and not as an in-patient in
the hospital. As per terms and conditions of the above policy, the policy provides coverage
for hospitalization expenses for treatment taken as an inpatient only. Hence, the claim
was repudiated and the same was communicated to the insured vide letter dated
24.05.2021. It is submitted that, on receipt of the Notice from the Hon’ble Ombudsman,
the claim was once again reviewed by our Medical Panel and considering to settle the
claim as per terms and conditions for Rs. 14,003/-.We would seek the Honorable
Ombudsman to mediate on our behalf and absolve us from the complaint made.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.

• I have heard both the parties at length and perused papers filed on behalf of the
complainant as well as the Insurance Company.
• Observation and Conclusion – During the hearing the complainant submitted that her
father’s claim was rejected for taking treatment on OPD basis whilst her father was
hospitalized at Gohil Sampurn Hospital, Shajapur for emergency treatment from
15.04.2021 to 21.04.2021 for B/L Viral Pneumonitis. HRCT test was done on 15.04.2021
and there was 50% involvement with CT Score of 12/25. As per doctor HRCT was normal
and her father was hospitalized for 6 days. A representation was made to the respondent
company on 28.07.2021 but respondent had not taken any action therefore the
complainant has appealed to this forum for settlement of the claim.
During their turn the respondent admitted having issued the policy no.
P/2xxxxx/xx/xxxx/xx9132 covering Ms. Priyanshi Jain, Mrs. Archana Jain and Mr. Vijay Jain
for a floater SI of Rs.10 lacs period 01.09.2021 to 31.08.2022. The respondent has further
submitted that Mr. Vijay Jain has taken treatment for viral Pneumonitis at Vyas Hospital
and Research Centre and again treatment of post viral Pneumonitis on 21.04.2021 at Gohil
Sampurn Hospital, Shajapur. Respondent further submitted that on examining the
documents it was found that the treatment has taken as out patient and hence not covered
in the policy hence therefore the claim was rejected.
I have heard both the parties and examined the documents available in the file. It is being
put on record that the SCN from respondent’s side was delayed inordinately and therefore,
the hearing was scheduled without the SCN. On fixing of the date of hearing at the last
moment we have received a calculation sheet of the claim without any proper note or
narration. The respondent has failed to submit a reply even after approximately 3 months
from receipt of complaint in spite of rigorous follow-up from this office. The SCN has been
incorporated as a special case with the caution to respondent that respondent should take
a cognizance of this and taken appropriate measures to ensure that this does reoccur again.
It is beyond any doubt that patient was hospitalized as there is discharge summery in the
file and the contention of the respondent that the patient took treatment as outdoor
patient seem ridiculous and speaks volume about the casual approach taken in this claim
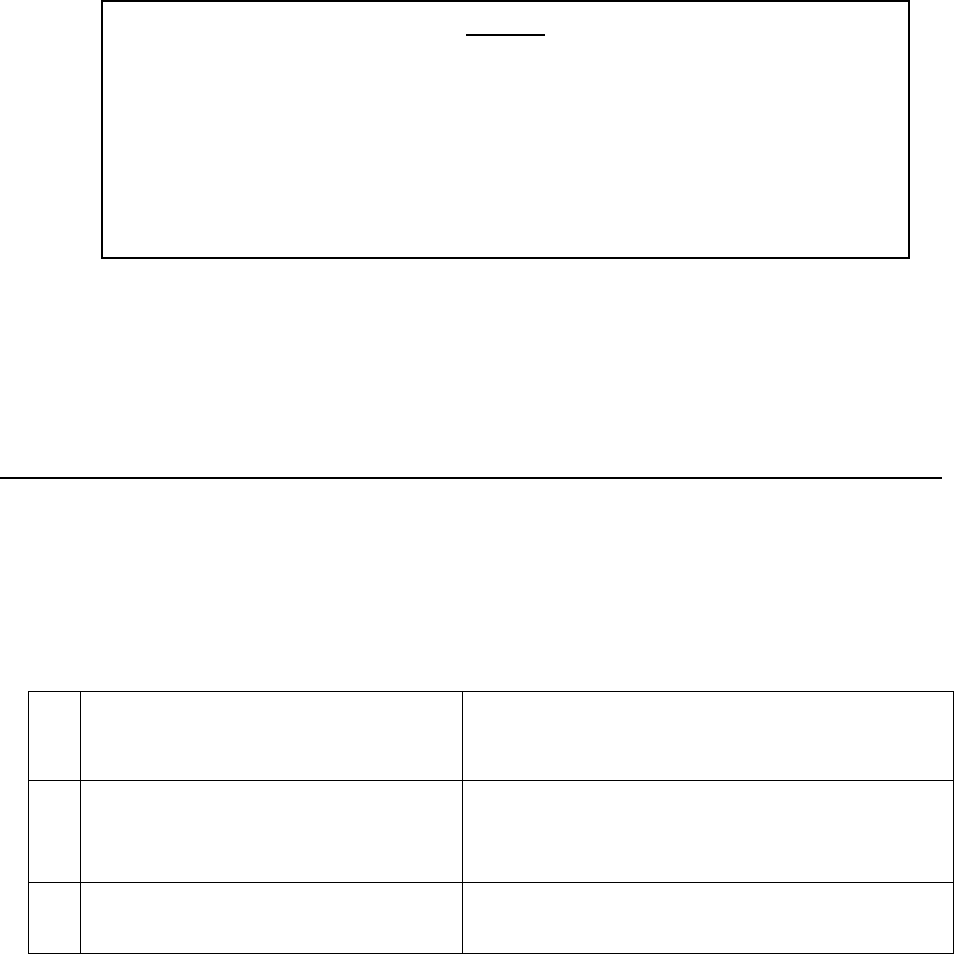
by not even going properly through the placed documents. The calculation sheet which has
been sent to this office does not taken room rent etc. in their calculation. The complainant
has represented for payment of Rs.64307/- as the claim amount which is correct. The
respondent failed to examine the papers and kept papers pending over since a year from
hospitalization. Such an unresponsive action speaks volumes about customer care and
customer service. The complaint is being allowed for Rs.64307/-.
•
• Let copies of the order be given to both the parties. Compliance shall be intimated to this
forum.
Place : Bhopal (RAVINDRA MOHAN SINGH)
Date: 06.04.2022 INSURANCE OMBUDSMAN
Mr. Jai Prakash Kori ..…………..……..……………...……………..……………….…………………...…Complainant
V/s
Reliance General Insurance Co. Ltd…………...……………….…….……...………….………….....Respondent
COMPLAINT NO: BHP-H-035-2122-0732 ORDER NO: /BHP/A/HI/0035 /2022-23
1.
Name & Address of the Complainant
Mr. Jai Prakash Kori
204/A, Hemasha Apts, South Civil Lines,
Jabalpur
2.
Policy No:
Type of Policy
Duration of policy/Policy period
Pol- 92029xxxxxx0000441-866292xxxxx000023
RGI-BOI Swasthya Bima
19.05.2021 to 18.05.2022
3.
Name of the insured
Name of the policyholder
Mr. Jai Prakash Kori
As above
AWARD
The complaint filed by Ms.Priyanshi Jain is allowed with directions to the
respondent company to settle the claim for Rs.64,307/- (Rupees Sixty four
thousand three hundred seven only) within 30 days from the date of receipt of
this Award.
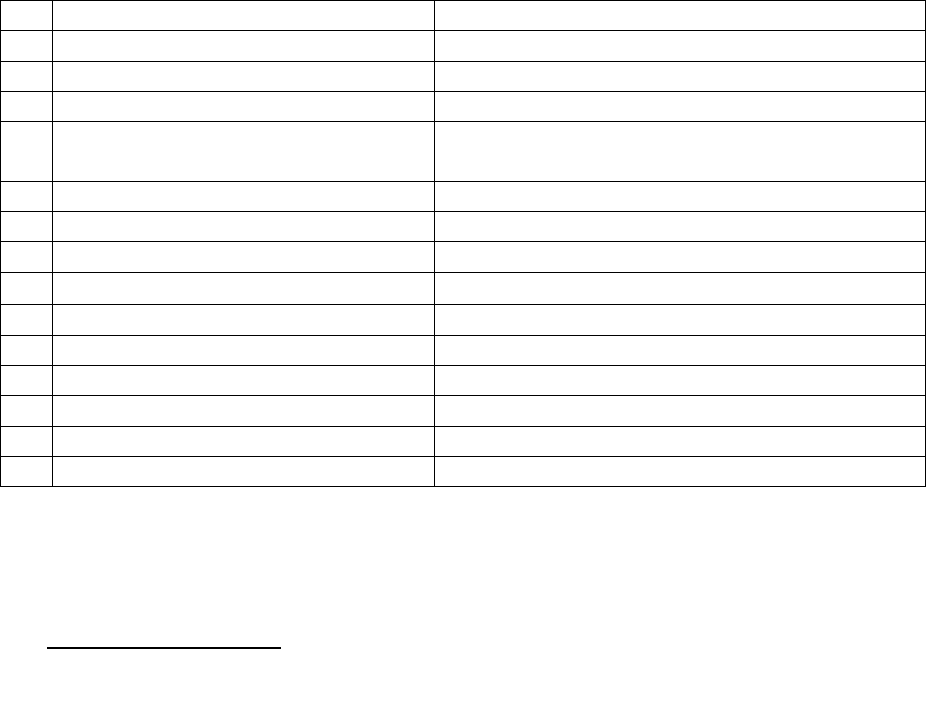
• Mr. Jai Prakash Kori filed a complaint against Reliance General Insurance Co. Ltd.
(Respondent) alleging not providing the Policy and continuity benefit to his son.
• Brief facts of the Case –
• Contention of the Complainant: -
The Complainant has states that he had issued a health insurance policy in the year 2013
named ‘Bank of India National Swasthya Bima Yojna’ in which Bank of India stood as agent
between the National Insurance Co. and he extended to cover for his family. He had
declared about the pre existing disease of his son i.e. Inflammatory Bowel Disease he was
/ is suffering from the year 2011. He was made aware by the National Insurance Co. about
a 3 years lock in period, namely my son would not be eligible for insurance benefits up to
3 years from the date of policy activated in respect of the pre- existing disease as
declared. Later, in the year 2018-19, the collaboration between the BOI & NIC came to
an end and Reliance General Insurance Co. came forward and took over the National
Swasthya Bima Yojna’ taken by BOI under existing terms & conditions and responsibility
for continuing the policy without any break thereon. He submitted further that he him-
self, his spouse and son (total three) persons were covered under the said cashless health
insurance policy against single yearly premium. His son’s health insurance was covered
4.
Name of the insurer
Reliance General Insurance Co. Ltd.
5.
Date of Repudiation/ Rejection
-
6.
Reason for Repudiation/ Rejection
-
7.
Date of receipt of the Complaint
12.01.2022
8.
Nature of complaint
Removal of Son’s name from the Policy &
discontinued the coverage / continuity benefit
9.
Amount of Claim
-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
-
12.
Complaint registered under Rule
Rule No. 13(1)(b) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
07.04.2022 At Bhopal
14.
Representation at the hearing
a) For the Complainant
Mr. Jaiprakash Kori, over Go To Meet App
b) For the insurer
Mrs. Ira Jain, Manager over GoTo Meet App
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
08.04.2022
under RGI health insurance policy till 2019- 20 but when policy was renewed for the year
2020-21 the name of my son was astonishingly removed from the policy on grounds of
age bar since attaining the age of 30 years. It is emphatically submitted at this juncture
that when I sought for the 2 clarification on the point of age bar the RGI answered that
though the name of my son continued to appear in the policy papers of National Insurance
Co. and Reliance General Insurance until 2019-20 but in fact and in effect, my son had
become ineligible for the health insurance after attaining the age of 25 years. Such
information sustained deep mental shock to me, assuming that what would have
happened if his son's hospitalization would have been necessitated during the past 5
years? He stated further that, in the above ‘peculiar’ facts and circumstances, he had to
go for a separate health insurance policy cover for his son as RGI offered him
telephonically through the authorized agent one shri Vivek Kharya, Jabalpur. In the above
context a sum of yearly premium for Rs.5546/- was paid online by him on date 14.05.2021
which got astonishingly refunded on date 27.05.2021 without assigning any valid or
adequate reason this or that. On this happening when I sought clarifications and/ or any
acceptable reason from the RGI authorized agent shri Vivek Kharya he was rudely
answered that accepting or declining the insurance proposal is a matter of sole right of
the underwriter. But the considerable merit and the substantial point of fact of his
complaint is that as to how the pre existing disease that of already declared at the
beginning of the policy in 2013 can be made a ground for declining and/ or discontinuance
of the policy by RGI that of ran without any objection for past 8 years particularly when
the declared disease (i.e. Ileac Inflammatory Bowel Disease does not find place in the list
of pre-existing diseases which may lead to disqualifying proposals for health insurance
cover and furthermore overall for the unchallengeable will of interest/ desperation
shown by the RGI for taking over the National Insurance Co. Policy and the ‘Bank of India
National Swasthya Bima Yojna’ was taken over under ‘as it is Terms & Conditions’?.
Complainant has prayed to command the RGI Co. to continue my son’s health insurance
policy without any break and inapplicability of 3 years lock in period meant for the new
policies.
• Contention of respondent-
The respondent in their SCN have stated the Policy vide No. 84629212451000023 has
been issued on 19.05.2021 for 18.05.2022 in the name the complainant and his wife . The
said policy has been issued by renewing his earlier policy bearing No.
846292028451000006 (issued for 19.05.2020 to 18.05.2021) which has been issued on
the basis of proposal form submitted by him. In the said proposal from the complainant
himself have categorically filed his name and his wife’s name. No Complaint was received
from the Complainant for the policy 846292028451000006 issued for 2020-21 as renewal.
The Complainant has also thereafter renewed the policy and 846292128451000023
issued for 2021-22. Hence the Complainant was aware about the beneficiaries uninsured
under the policy and satisfied with the issued policy. It is imperative to mention here that
the policy in question has been issued only upon the name of the complainant and his
wife based upon his own declaration in the proposal form. The complainant has submitted
his and his wife’s name only. Respondent stated further that there is no complaint from
Complainant for the policy 846292028451000006. Hence the present complaint is not
maintainable and deserves to be dismissed
• The Complainant has filed complaint letter, Annex. VIA and correspondence with
Respondent while respondent have filed SCN with enclosures.
• I have heard both parties at length and perused paper filed on behalf of the complainant
as well as the Insurance Company
• Observation and Conclusion : During the hearing the complainant submitted that he
purchased a health insurance policy in the year 2013 named Bank of India, National
Swastha Bima Yojna in which Bank of India stood as an agent between Bank of India and
National Insurance Co. The complainant further submitted that he had declared about
the pre-existing disease of his son i.e. Inflammatory Bowel disease which he was suffering
from year 2011. He was made aware by National Insurance Co. about 3-year lock-in period
meaning thereby that his son would not be eligible for insurance benefit upto 3 year from
the date of policy activated in respect of the pre existing disease as declared. Later in the
year 2018-19 National Insurance was replaced by Reliance General Insurance Co. and took
over the National Swashya Bima Yojna under existing terms and condition and with
continuation of the policy. The complainant further submitted that he himself, spouse
and son were covered under the said cash-less Health Insurance Policy. His son’s health
insurance was covered under RGI till 2019-20 but when the policy was renewed the name
of my son was astonishingly removed in year 2020-21 on the ground of age barred
because of attaining of 30 years. The respondent company clarified that beyond the age
of 25 years such policy can not be given and infact his son had become ineligible for the
health insurance attaining the age of 25 year. So, he had to go in for a separate health
insurance policy for his son which RGI advised him telephonically accordingly a yearly
premium of Rs.5546/- paid online by him on date 14.05.2021 which got refunded on
27.05.2021 without assigning any valid reason. When he sought clarification from the RGI
authorized agent rudely answered that accepting or declining the insurance proposal is
sole right of the underwriter. But the substantial point of fact is that as to how the pre
existing disease that of already declared at the beginning of the policy in 2013 can be
made a ground for declining and / or discontinuance of the policy by RGI that ran without
any objection for past 8 years particularly when the declared disease (i.e. lleac
Inflammatory Bowel Disease )does not find place in the list of pre-existing diseases which
may lead to disqualifying proposals for health insurance cover.
The respondent in his turn argued that they have issued the policy from 2021-22 for
complainant and his wife. The said policy has been issued by renewing his earlier policy
for 2020-21 on the basis of proposal form submitted by him. In the said proposal form the
complainant himself have categorically filed his name and his wife’s name. No complaint
was received from the complainant for the policy of issued for 2020-21 as renewal.
Whereas the complainant was aware about the beneficiaries uninsured under the policy.
So, complaint is not maintainable. The respondent sought some time to get resolved the
issue pertaining to policy issuance for his son with continuity basis without 3 years locking
/ waiting clause. Considering the request, the hearing was re- scheduled.
The complaint was rescheduled and heard on 08.04.2022. The complainant has prayed
to direct the RGI Co. to continue his son’s health insurance policy coverage without any
break and inapplicability of 3 years lock in period through a new policy by charging
premium as per normal tariff. The respondent came with the offer to issue the policy for
his family in the name of his wife and include to his son proving continuity as per last
renewal.
I have heard both the parties and viewed the documents made available by both the
parties. It is observed that in the policy there is no condition of age bar for son to exclude
from coverage after attending the age of 25 years. If so, then how the coverage was
granted till the age of 30 years. The policy for his son was discontinued inappropriately.
Hence the complaint is allowed with the direction to respondent to issue health insurance
cover for his son providing continuity benefit without any locking /waiting clause charging
normal and applicable tariff.
•
• Let copies of the order be given to both the parties. Compliance shall be intimated to this
forum.
Place : Bhopal (RAVINDRA MOHAN SINGH)
Date: 08.04.2022 INSURANCE OMBUDSMAN
Mrs. Vimla Tiwari ………….....……………………………………………………..….. Complainant
V/s
Care Health Ins Co. Ltd. … ………. ………….. ….………….……………………Respondent
COMPLAINT NO: BHP-H-037- 2122-0834 ORDER NO: IO/BHP/R/HI/0019 /2022-2023
AWARD
The complaint filed by Mr Jaiprakash Kori is allowed with directions to
the respondent company to issue health insurance cover for his son
providing continuity benefit without any locking /waiting clause charging
normal and applicable tariff within 30 days from the receipt of this order.
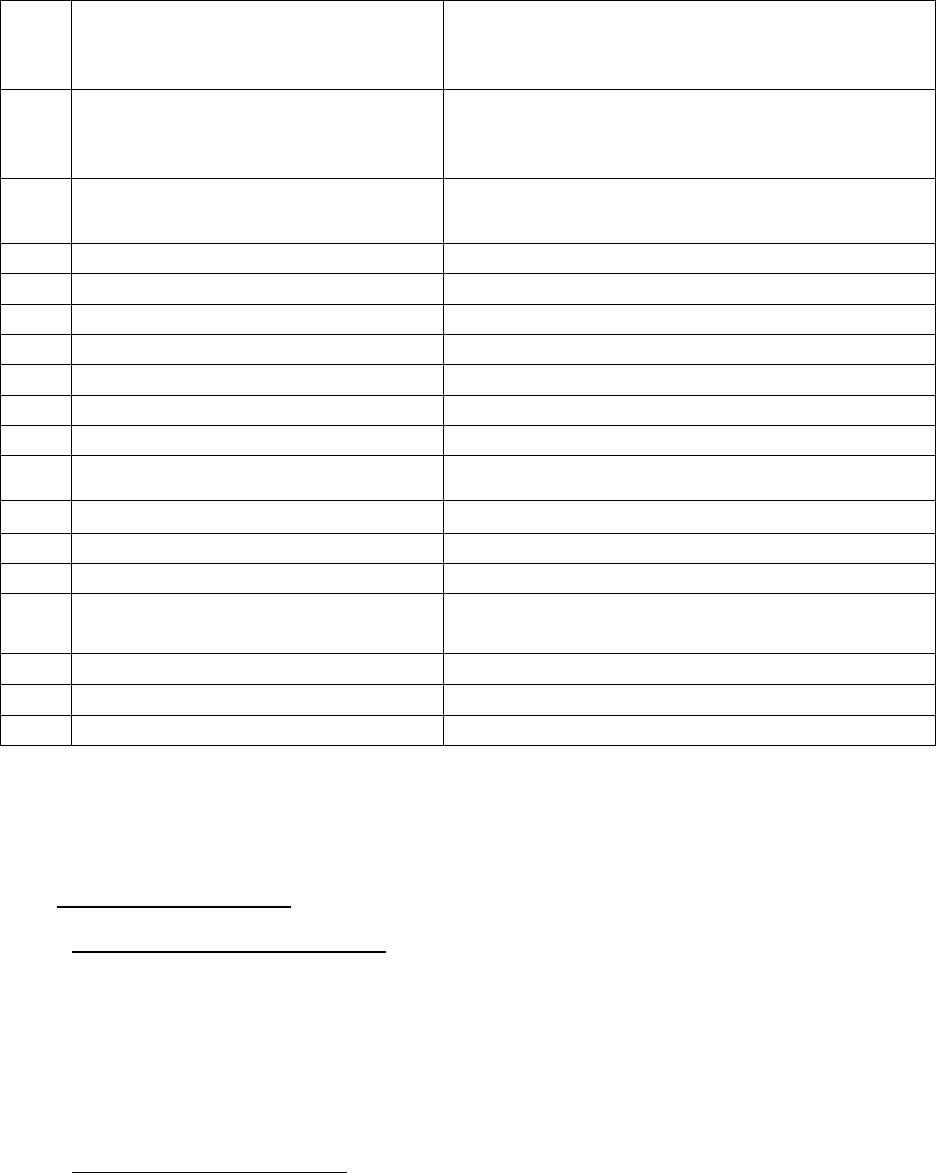
• Mrs. Vimla Tiwari Complainant) has filed a complaint against Care Health Ins Co. Ltd
(Respondent) alleging partial settlement of claim
• Brief facts of the Case –
• Contention of the complainant - The complainant has stated that she took treatment
from Aradhana Hospital from 22.03.2021 to 11.04.2021. The amount of bill was Rs.
4,80,724/-. But the Company paid only Rs. 2,31,584/- and deducted an amount of Rs
2,49,140/- and made him to pay Rs. 87,452/- to the hospital. The company did not give
any justification for the less payment.
• Contention of the respondent - The respondent in their SCN have stated that they are ready to
settle the claim for Rs. 87,452/- towards full and final settlement as per policy terms and
conditions., subject to submission of required documents: a. NEFT b. KYC of proposer c. Payment
1.
Name & Address of the
Complainant
Mrs. Vimla Tiwari
EWS 45 A Sector,
Rajeev Nagar, Bhopal
2.
Policy No:
Type of Policy
Duration of policy/Policy period
17XXX9225
Group Care 360 PNB
28.11.2020 to 27.11.2021
3.
Name of the insured
Name of the policyholder
Mrs. Vimla Tiwari
PNB
4.
Name of the insurer
Care Health Ins Co. Ltd
5.
Date of Repudiation/ Rejection
-
6.
Reason for Repudiation/ Rejection
-
7.
Date of receipt of the Complaint
11.02.2022
8.
Nature of complaint
Partial settlement of claim
9.
Amount of Claim
Rs. 4,80,724/-
10.
Date of Partial Settlement
11.
Amount of relief sought
Rs. 87,452/-
12.
Complaint registered under Rule
Rule No. 13(1)(d) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
18.04.2022 at OIO Bhopal
14.
Representation at the hearing
c) For the Complainant
Mr. Suryakant Tiwari, Son of complainant over
GoTo app
d) For the insurer
Dr. Samiksha, Manager over GoTo Meet App
15.
Complaint how disposed
Recommendation
16.
Date of Award/Order
18.04.2022
of receipts of Rs. 87,452/- The Sum Insured of the referred group policy issued to the complainant
is Rs. 7, 00,000/- and the policy period is 28.11.2020 to 27.11.2021
• The complainant has filed complaint letter, Annex. VI A and correspondence with respondent,
while respondent have filed SCN with enclosures.
• I have heard both the parties at length and perused papers filed on behalf of the complainant
as well as the Insurance Company.
• Observation and Conclusion –
During the hearing the complainant submitted that she took treatment from Aradhana
Hospital, from 22.03.2021 to 24.03.2021 the claim amount was Rs.480784/-. But the
respondent company paid only 231584/- and deducted an amount of Rs.249140/-. The
complainant further submitted that he had to pay Rs.87452/- to the hospital. He has
appealed to this forum for payment of Rs.87452/-.
During their turn the respondent submitted that they are ready to settle the claim for
Rs.87452/- subject to submission of required documents (i) NEFT details (ii)Payment receipts
of Rs.87452/-. The forum directed the complainant to send the above documents by mail to
the respondent company by 4 PM. The documents were sent by the complainant and duly
received by the respondent company which they have confirmed by mail dated 18.04.2022
at 04.12 PM.
Hence the complaint was resolved mutually between both parties.
•
AWARD
The matter within parties has been resolved mutually, hence the respondent is directed
to pay Rs.87452/- (Rs. Eighty seven thousand four hundred fifty two only) within 15 days
on receipt of the order.
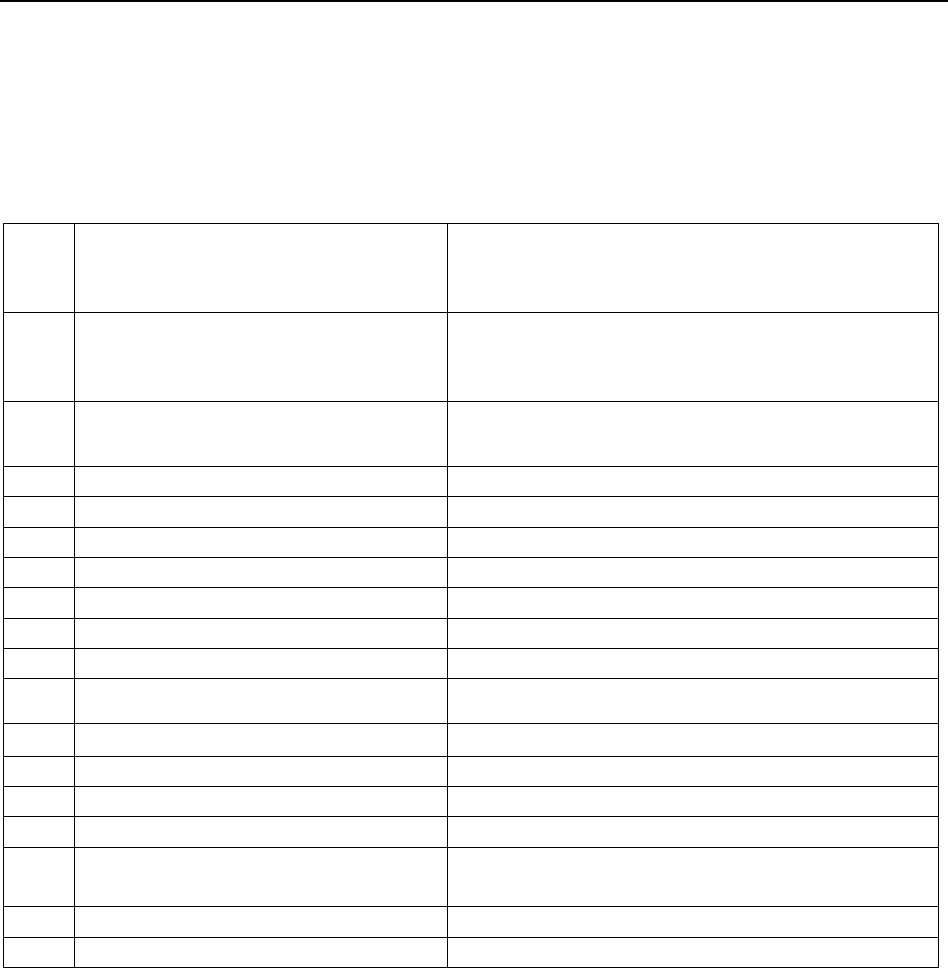
• Let copies of the order be given to both the parties. Compliance shall be intimated to this
forum.
Place : Bhopal (RAVINDRA MOHAN SINGH)
Date: 18.04.2022 INSURANCE OMBUDSMAN
Mr. Kailash Chandra Sen ……….……………………………………………………..….. Complainant
V/s
SBI General Ins. Co. Ltd. ………………………. ….…………………………………………Respondent
COMPLAINT NO: BHP-H-040-2122-0806 ORDER NO: IO/BHP/A/HI/0051 /2022-2023
• Mr. Kailash Chandra Sen (Complainant) has filed a complaint against SBI General Ins. Co.
Ltd. (Respondent) alleging repudiation of claim.
1.
Name & Address of the
Complainant
Mr. Kailash Chandra Sen
14, Ahilyapaltan
Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
00xxxxxxxx7393
Group Health Ins. Policy
13.02.2020 to 12.02.2021
3.
Name of the insured
Name of the policyholder
Mrs. Manjula Sen
Mr. Kailash Chandra Sen
4.
Name of the insurer
SBI General Ins. Co. Ltd.
5.
Date of Repudiation/ Rejection
29.03.2021
6.
Reason for Repudiation/ Rejection
Pre Existing Disease
7.
Date of receipt of the Complaint
04.02.2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 2,83,837/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs. 2,83,837/-
12.
Complaint registered under Rule
Rule No. 13(1)(d) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
27.04.2022 at OIO Bhopal
14.
Representation at the hearing
e) For the Complainant
Mr Kailash Chandra Sen over GoTo Meet App
f) For the insurer
Ms Chynika Modie, Manager over GoTo Meet
App
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
29.04.2022

• Brief facts of the Case –
• Contention of the complainant - The complainant has stated that he is working in the
District Court , Indore and he did not apply for reimbursement of medical expenses in
his Dept. He was issued a policy (No. 00xxxxxxxxxx7393) dated 12.02.2019 by the then
Branch Manger of SBI, Indore, Shri Alok Sharma and no medical tests were done on him
nor on his wife. The premium for the year 2020 was paid through his S.B account and his
wife Smt. Manjula Sen was admitted In Geetanjali Hospital, Indore on 23.11.2020.
Thereafter was shifted to Medicare Hospital , Indore on 24.11.2020 and got discharged
on 07.12.2020. He was told to pay Rs. 2,83,837 later on when medical bill was submitted
it was said that the payment will be made to him. All the bills were submitted to the
Insurance Co. and the Company was verbally informed. But his claim was rejected. After
few months his papers returned to him. The complainant has approached this forum for
redressal of grievance.
• Contention of the respondent - The respondent in their SCN have stated that the at the
outset Company disputes and denies every averment and allegations made in the
Complaint save and except the matters of record and facts specifically mentioned herein.
Further, The Hon’ble Ombudsman may be pleased to allow the Company , the right to file
additional submissions and documents should the same be warranted at a later stage, in
the interest of Justice.That the present Complaint has been made with a foremost prayer
to reconsider and settle the repudiated claim bearing IP-2524805/200620086819-01 of
the Complainant. It is submitted that the claim of the Complainant has already been
investigated by SBI General and as per their findings, based on submitted documents vis-
a-vis policy terms and conditions, the said claim was closed as inadmissible on exclusion
clause-1 mentioned under policy. That the same is explained and substantiated
herewith.A Group Health Insurance Policy bearing no. 00xxxxxxxxxx7393-01 was issued
by SBI General in the name of Complainant/Insured i.e. “Mr. Kailash Chandra Sen” wherein
his wife was also insured i.e. “Ms. Manjula Sen”. The said policy was effective from
13.02.2020 to 12.02.2021, subject to its terms and conditions and any claim is admissible
in adherence to the terms and conditions Ms. Manjula Sen was hospitalized in “Medicare
Hospital & Research Centre, Indore” from 24.11.2020 to 07.12.2020 for the treatment of
Left Thalamic Bleed in known case of diabetes mellitus and hypertension for which she
underwent medical management. After going through the Hospital papers and
scrutinising all circumstances regarding the subject claim, the TPA observed discrepancy
in the submitted claim documents. Therefore, the Company appointed an Independent
Investigator viz., “Mediprobe Consultancy Services Pvt. Ltd.” (“Investigator”) to investigate
the facts of the case, collect additional documents and submit Final Investigation report
to the Company. That after going through submitted documents on record as well as
scrutinising all the relevant circumstances, the subject claim was assessed conclusively.
Accordingly, based on TPA’s final assessment and Final Investigation Report vis-a-vis policy
terms and conditions, SBI General observed the following:Patient Ms. Manjula Sen, 53
years female was admitted in said Hospital for complaints of giddiness, hemiplegia with
giddiness. She was diagnosed as a case of left thalamic bleed in known case of diabetes
mellitus and hypertension.Initially patient was admitted in Geetanjali Hospital from
23.11.2020 to 24.11.2020 then admitted in Medicare Hospital from 24.11.2020 to
07.12.2020. Patient denied to have any past history of diabetes mellitus and hypertension.
Treating doctor i.e. Dr. Deepak Kularkarni, has confirmed that diabetes and blood pressure
are the risk factors of left thalamic bleed, but he does not know the exact duration of
same. As per IPD papers dated 24.11. 2020, patient was seen by Dr. Mukesh Khapra in
Geetanjali Hospital. That Dr. Mukesh Khapra has confirmed that patient is known case of
diabetes mellitus and hypertension, was on and off treatment for the same since 3 years.
Diabetes mellitus and hypertension are risk factors for left thalamic bleed, and the same
is proved by analysing effects of diabetes and hypertension on thalamic hemorrhage,
providing co-morbidities of the disease, clinical examination of the procedures and
conclusion in regards to evidence-based practices. In view of the documents on record
and Investigation Report, it was evident that it was observed that insured was admitted
in hospital on 24.11.2020 and the first policy inception date is 13.02.2019. As per doctor’s
letter diabetes mellitus and hypertension are risk factors for Left Thalamic Bleed and the
Insured has diabetes mellitus and hypertension since 3 years, which makes it pre-existing
in nature and current ailment is complication of the same. That as per terms of the policy
the expenses arising out of above ailment is not payable as pre-existing illness is not
covered under the policy exclusion clause-1. That Diabetes mellitus and hypertension are
risk factors for left thalamic bleed, and the same is proved by analysing effects of diabetes
and hypertension on thalamic hemorrhage, providing co-morbidities of the disease,
clinical examination of the procedures and conclusion in regards to evidence-based
practices. The copy of Review Article on ‘The Effects of Diabetes Type II in Hypertensive
Thalamic Hemorrhage’ and ‘Clinical properties of regional thalamic hemorrhages’ are
annexed That in view of the aforesaid facts and findings, vis-à-vis policy terms and
conditions, the expenses arising out of above ailment were observed as untenable in view
of the misrepresentation of facts. Hence, in the given premises, relevant conditions of the
subject policy is reproduced hereunder for ready reference and convenience of the Ld.
Ombudsman:
“Pre-existing Disease means any condition, ailment, injury or disease:a) That is/are
diagnosed by a physician within 48 months prior to the effective date of the policy issued
by the insurer or its reinstatement b) For which medical advice or treatment was
recommended by, or received from, a physician within 48 months prior to the effective date
of the policy issued by the insurer or its reinstatement. EXCLUSIONS: -That Accordingly as
per policy exclusion clause no 1 – Pre-existing Diseases Exclusion: Benefits will not be
available for any condition, ailment or injury or related condition(s) for which Insured has
been diagnosed, received medical treatment, had signs and / or symptoms, prior to
inception of Insured first Policy, until 48 consecutive months have elapsed, after the date
of inception of the first Policy with the insurer. This Exclusion shall cease to apply if Insured
Person has maintained this Health Insurance Policy with Insurer for a continuous period of
a full 4 years, Without break from the date of Insured’s first group Health Insurance Policy
with Insurer….” Furthermore, Insured while contracting for the said Health Insurance policy,
deliberately failed to disclose that she had any ailment/illness in 2019 while filling the
Proposal Form. It is pertinent to mention that the Insured deliberately withheld the said
information, inspite of the fact that the Proposal Form had specific and individual

checkboxes for past history and ailments of the proposer. That aforesaid misrepresentation
and concealment of material facts, led to the violation of declaration in Proposal Form
submitted for issuance of inception policy. Accordingly, based on misrepresentation of facts
and policy exclusion clause-1 the said claim falls beyond purview of policy coverage and
hence was appropriately repudiated by SBI General. The communication regarding the said
decision was sent to the Insured through our claim declination letter dated 30.01.2021.
Further, the Company has not received any representation from the Complainant referring
its grievances to GRC (Grievance Redressal Committee). It is pertinent to submit that
Policyholders who have Complaints against insurers are required to first approach the
Complaints/Grievance Redressal Cell of the company. Further, if they do not receive a
response from the insurer within a reasonable period of time or are dissatisfied with the
response of the company, they may approach the Ld. Ombudsman. However, Insured has
not exhausted its alternative remedy and has wrongly approached the Ld. Ombudsman. It
is thus submitted that Complainant’s right to file an Ombudsman Complaint has not accrued
In the light of the aforesaid facts, it is submitted that the claim of the insured/complainant
has been denied in accordance with the terms and conditions of the said Policy, absolving
the company from any and all claims, demands and liabilities arising out of or related to the
said claim. Hence, we humbly submit that there is no error on part of the SBI General which
calls for the interference of the Ld. Ombudsman and the present complaint is liable to be
dismissed on account of being misconceived and without merit.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties over GoTo Meet App at length and perused papers filed on
behalf of the complainant as well as the Insurance Company.
• Observation and Conclusion – During hearing the complainant submitted that he is
working in the District Court Indore and he had taken a policy No.00xxxxxxxxxx7393 for the
period 13.02.2020 to 12.02.2021 from Branch Manager of SBI Indore Shri Alok Sharma. He
further submitted that no medical tests were done for him or his wife. His wife Smt Manjula
Sen was admitted in Geetanjali Hospital, Indore on 23.11.2020. Thereafter was shifted to
Medi Care Hospital, Indore on 24.11.2020 and discharged on 07.12.2020. He paid
Rs.2,83,837/- to the Hospital. All the bills were submitted to the respondent company but
his claim was rejected. The complainant has appealed to this forum for settlement of claim.
On their turn the respondents admitted having issued the above policy and having received
the claim of Mrs Manjula Sen. She was admitted in Medicare Hospital and Research Centre,
Indore from 24.11.2020 to 07.12.2020 for the treatment of Left Thalamic Bleed and is a
k/c/o of Diabetes Mellitus and Hypertension for which she underwent medical
management. On scrutiny of the claim documents the concerned TPA found some
discrepancy and appointed an independent investigator Medico Consultancy Services Pvt
Ltd to investigate the facts of the case. The respondent further submitted that Mrs Manjula
Sen was admitted in the Hospital for complaints of giddiness, hemiplegia with giddiness.
She was diagnosed as a case of left thalamic bleed. Patient denied to have any past history
of Diabetes and Hypertension. The respondent further submitted that on examining the
IPD papers dated 24.11.2020 patient was seen by Mr Mukesh Khapra in Geetanjali Hospital,
Indore and he has confirmed that patient is k/c/o/ of Diabetes and Hypertension and was
on and off treated for the same since three years. Thus DM and HTN are pre existing in
nature and on the basis of this respondent company repudiated the claim. The respondent
further argued that DM and HTN are risk factors for left thalamic bleed and the same is
proved by analysing effects of these two diseases on thalamic hemorrhage, provide co-
morbidity of the disease, clinical examination of the procedure and conclusion with regard
to evidence based practices. The respondents further submitted that ‘Pre-existing Disease
means any condition, ailment, injury or disease : a) That is/are diagnosed by a physician
within 48 months prior to the effective date of the policy issued by the insurer or its
reinstatement b) For which medical advice or treatment was recommended by, or received
from, a physician within 48 months prior to the effective date of the policy issued by the
insurer or its reinstatement. EXCLUSIONS: -That Accordingly as per policy exclusion clause
no 1 – Pre-existing Diseases Exclusion: Benefits will not be available for any condition,
ailment or injury or related condition(s) for which Insured has been diagnosed, received
medical treatment, had signs and / or symptoms, prior to inception of Insured first Policy,
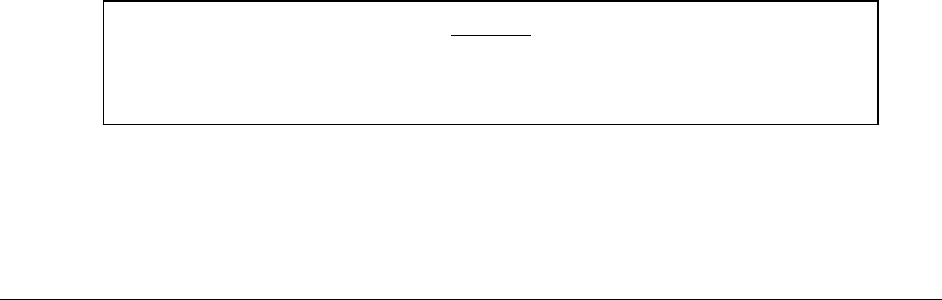
until 48 consecutive months have elapsed, after the date of inception of the first Policy with
the insurer. This Exclusion shall cease to apply if Insured Person has maintained this Health
Insurance Policy with Insurer for a continuous period of a full 4 years, Without break from
the date of Insured’s first group Health Insurance Policy with Insurer”.
The respondent put forth their argument that the insured has deliberately with held the
information of DM and HTN which they should have declared at the time of proposal and
accordingly the claim was repudiated for misrepresentation of facts as per policy exclusion
Clause NO.1 and the same was communicated to the complainant on 30.01.2021.
I have heard both the parties and examined the documents carefully. It is clearly
established from Dr Mukesh Khapra’s report that the patient was suffering from Diabetes
Mellitus and Hypertension for the last three years. The pre existing clause of the policy
defines very clearly that any disease i.e. diagnosed within 48 months is not covered under
the policy. Since the complainant had not declared these ailments at the time of inception
of the policy, therefore it leads to deliberate mis representation and justifies respondents
action of repudiating the claim. Therefore the complaint is liable to be dismissed.
•
• Let copies of the order be given to both the parties.
Place : Bhopal (RAVINDRA MOHAN SINGH)
Date: 29.04.2022 INSURANCE OMBUDSMAN
OMBUDSMAN – RAVINDRA MOHAN SINGH
Mr. Ravishankar Kewalramani ..…………………………………………..….. Complainant
V/s
Care Health Ins. Co. Ltd. ………….………….….………….……………………Respondent
AWARD
The complaint filed by Mr Kailash Chandra Sen stands dismissed herewith.
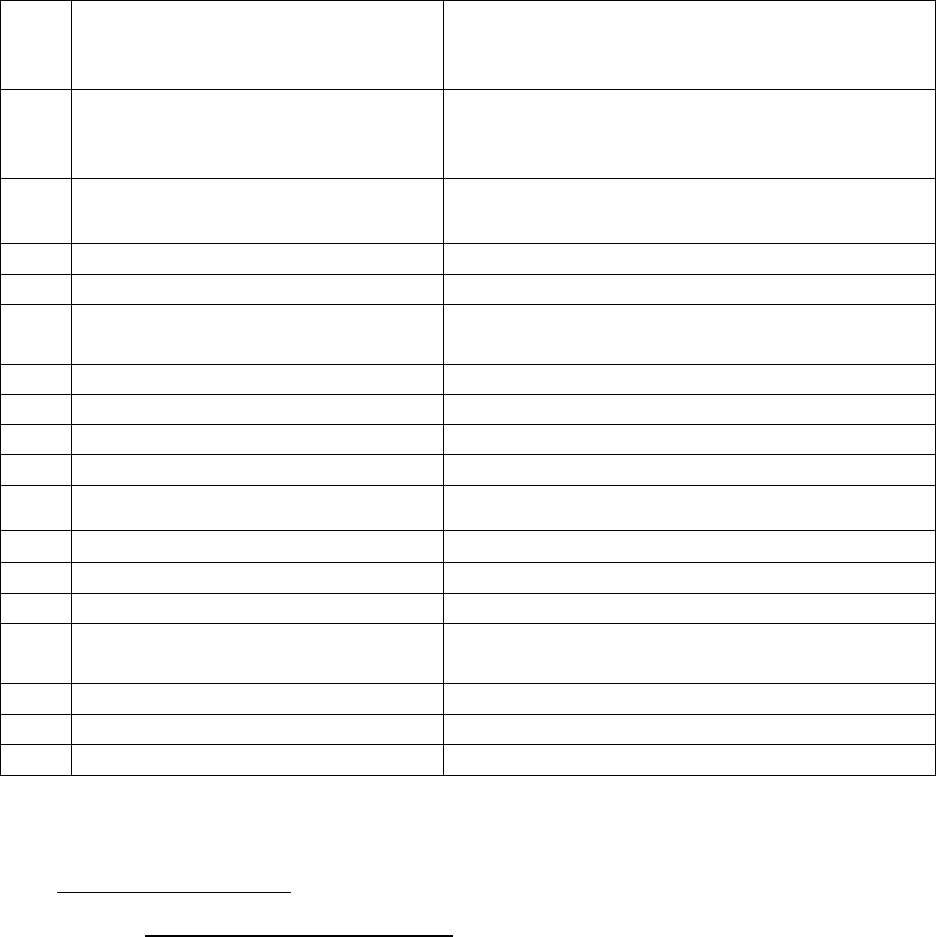
COMPLAINT NO: BHP-H-037- 2122-0833 ORDER NO: IO/BHP/A/HI/0044 /2022-2023
• Mr. Ravishankar Kewalramani Complainant) has filed a complaint against Care Health Ins
Co. Ltd (Respondent) alleging repudiation of claim.
• Brief facts of the Case –
a) Contention of the complainant - The complainant has stated that he with family
members were covered by National Insurance Co. for about 5 years initially and then
transferred to The New India group mediclaim policy in 2019 and thereafter ported through
Punjab National Bank to Care Heath Insurance “ Group care 360 degree PNB Platinum” from
20.03.2021 with zero waiting period for all Pre existing disease (PED) as per PNB product
offering. He has not taken any claim since beginning from any insurance Company. While
processing his application as Health & Lifestyle Information he was asked “Has anyone
1.
Name & Address of the
Complainant
Mr. Ravishankar Kewalramani
Block No. 6, Jeripatka
Nagpur
2.
Policy No:
Type of Policy
Duration of policy/Policy period
17xxx9225
Group Care 360 degree PNB Platinum
20.03.2021 to 19.03.2022
3.
Name of the insured
Name of the policyholder
Mr. Ravishankar Kewalramani
Mr. Ravishankar Kewalramani
4.
Name of the insurer
Care Health Ins Co. Ltd
5.
Date of Repudiation/ Rejection
24.08.2021
6.
Reason for Repudiation/ Rejection
Misrepresentation, Misdescription or Non
disclosure of material facts
7.
Date of receipt of the Complaint
11.02.2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
Rs. 2,17,564/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs. 2,17,564/-
12.
Complaint registered under Rule
Rule No. 13(1)(d) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
27.04.2022 at OIO Bhopal
14.
Representation at the hearing
g) For the Complainant
Mr Ravishankar Kewalramani over GoTo Meet
App
h) For the insurer
Dr Samiksha Saxena over GoTo Meet App
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
28.04.2022

been diagnosed, hospitalized or is currently under investigation for cancer , diabetes,
stroke, heart disease, kidney disease , liver disease, hypertension(BP) to which replied
promptly “No” to employee of Care Ins. before the Manager of PNB. But the Company on
24.08.2021 has rejected his claim stating : Non disclosure of Obesity High BMI at the time
of policy inception. Non disclosure of pre existing illness if there has been a
misrepresentation, Mis description or Non disclosure of any material particulars the Co.
shall have no liability to make payment of any claims.
b) Contention of the respondent - The respondent in their SCN have stated that the
Company denies all the averments and allegation filled by the complainant in the complaint
and all the other communication and documents filed by the complainant. That the
Complainant purchased a Health Insurance Policy namely “PUNJAB NATIONAL BANK- Group
Care 360°(PNB-Platinum)” bearing Group Policy No. 17499225 and Certificate of Insurance
No. 30734542 from the Respondent Company wherein insurance coverage was provided to
Complainant Mr. Ravishankar C Kewalramani Complainant’s spouse Mrs. Simran R
Kewalramani, complainant’s son Mr. Jay R Kewalramani and Complainant’s daughter Ms.
Bhavika R Kewalramani for a sum insured upto Rs. 4,00,000/- covering the period from
20.03.2021 to 19.03.2022 subject to Policy Terms and Conditions. The policy was ported
from New India Assurance Co. Ltd. wherein the date of first enrollment was
20.03.2019.That during the continuation of the policy, the Complainant herein approached
the Respondent Company for Reimbursement Claim for his hospitalization at M/s Mohak
Hi-Tech Speciality Hospital from 21-07-2021 to 25-07-2021 for his diagnosis of Morbid
Obesity, Hypothyroidism, Recently Diagnosed T2DM and underwent operation of LAP.
Sleeve Gastrostomy done under general anesthesia. Upon care full examination of the claim
documents made available to the Respondent Company, the following observations were
made: That as per the Discharge Summary of M/s Mohak Hi-Tech Specialty Hospital dated
25-07-2021, it is mentioned that the insured was admitted to Hospital with weight Gain
which is leading to Morbid Obesity. It is pertinent to mention that insured weight at the
time of admission was 123.55 K.G. and BMI was 43.2kg/m2.That as per the Medical
Prescription of M/s Mohak Hi-Tech Specialty Hospital dated 14-07-2021, it is mentioned
that the insured was having a complaint of morbid obesity and was advice to undergo
Bariatric surgery. It also mentioned that weight of insured was 123.55 kg. In reference to
above mentioned facts, it was observed that the Insured was suffering from Obesity High
BMI prior to the inception of the policy which was not disclosed to the Respondent
Company. Accordingly this was classified as “Non-disclosure of Material Facts.” That
subsequently, the Reimbursement Claim was rejected vide Rejection Letter dated
24.08.2021 due to “Non-Disclosure of Material Facts/Pre-Existing Ailments at Time of
Proposal”. That subsequently in accordance to the aforesaid facts and observations, the
claim of the insured was rejected on the grounds of “Non-disclosure of Obesity High BMI
Prior to the Inception of Policy” in accordance to clause 7.1 of the policy terms and
conditions. The relevant clause is reproduced herein as under: 7.1. Disclosure to
Information Norms The Policy shall be void and all premium paid thereon shall be forfeited
to the Company in the event of misrepresentation, mis-description or non-disclosure of any
material fact by the policy holder. Note: “Material Facts” for the purpose of this clause
policy shall mean all relevant information sought by the Company in the proposal form and
other connected documents to enable it to take informed decision in the context of
underwriting the risk. In continuation to the above clause the Company may also adjust the
scope of cover and / or the premium paid or payable, accordingly. That the Insured herein,
in accordance to the tenets of the Insurance Law was duty bound to disclose all the material
facts with respect to his medical history. The insured had the opportunity to declare the
true state of health to the Respondent Company in the Proposal form. However, the same
was not disclosed by the Complainant for reasons best known to him. That in the Proposal
Form, under the heading “Details of the Person to be insured (including Applicant), it is
mentioned by the insured himself that his weight at the time of inception of policy was 75
kg. It is further stated that as per the Insurance Regulatory and Development Authority of
India (IRDAI) (Protection of policy Holder’s Interest) Regulations, 2017 under Clause 19(4)
enumerating the “General Principal” casts an absolute duty to disclose all material facts to
the Insurer in order to assess the risk as per its capacity. “The policyholder shall furnish all
information that is sought from him by the insurer either directly or through the distribution

channels which the insurer considers as having a bearing on the risk to enable the insurer
to assess properly the risk covered under a proposal for insurance.” It is humbly submitted
that High BMI is considered to be a dropped risk as per the underwriting guidelines for the
product-“Punjab National Bank- Group Care 360°(PNB-Platinum)” . If insured member
would have disclosed he have high BMI, then respondent company would have not issued
the policy only.That In the Export Credit Guarantee Corp of India Ltd. Versus M/s Garg Sons
International pronounced by the SUPREME COURT OF INDIA that the “The insured cannot
claim anything more than what is covered by the insurance policy.“…the terms of the
contract have to be construed strictly, without altering the nature of the contract as the
same may affect the interests of the parties adversely Hence it is humbly submitted that all
averments to the contrary in the complaint are denied, and hence it is prayed that the
Hon’ble Ombudsman may kindly be pleased to accept this self-contained note and the
complaint may be dismissed.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties over GoTo Meet App at length and perused papers filed on
behalf of the complainant as well as the Insurance Company.
• Observation and Conclusion – During hearing the complainant submitted that he with his
family members were covered by National Insurance Co. for about five years initially and
then transferred to the New India Group Mediclaim policy in 2019 and thereafter ported
through Punjab National Bank to Care Health Insurance under ‘Group Care 360 Degree PNB
Platinum’ from 20.03.2021 with zero waiting period for all pre existing disease as per PNB
Product offering. His claim has been rejected by the Company for non disclosure of obesity,
high BMI at the time of policy inception. The complainant further said that while processing
his application for health and lifestyle information he was asked ‘Has anyone been
diagnosed, hospitalized or is currently under investigation for cancer , diabetes, stroke,
heart disease, kidney disease , liver disease, hypertension(BP) to which replied promptly
“No” to employee of Care Ins. before the Manager of PNB. Complainant has appealed to
this forum for settlement of his claim.
During their turn the respondent admitted of having issued policy No. 17xx9225 Group Care
360 Degree PNB Platinum for the period 20.03.2021 to 19.03.2022. They also admitted
that this was ported from New India Group Mediclaim policy in 2019 and the date of first
enrolment was 20.03.2019. The complainant has preferred a reimbursement claim for his
hospitalization at Mohak High Tech Specialty Hospital from 21.07.2021 to 25.07.2021 for
his diagnosis of morbid obesity, Hypothyrodism recently diagnosed T2DM and underwent
operation of LAP Sleep gastrostomy done under general anesthesia. The respondent
company further submitted that on careful examination of the documents of Mohak High
Tech Specialty Hospital it is mentioned that insured was admitted to Hospital with weight
gain leading to morbid obesity. The respondent company further put forth their argument
that at the time of admission the complainant’s weight was 123.55 kg and BMI was 43.2.
As per the medical prescription of Mohak High Tech Speciality Hospital dated 14.07.2021
the insured was having a complaint of morbid obesity and was advised to undergo Bariatric
surgery. Therefore it is clear that insured was suffering from obesity and high BMI prior to
the inception of the policy which was not disclosed to the insurance company. This amounts
to non disclosure of material fact and on these ground the claim was rejected. The
respondent company further argued that in the proposal form under the details of person
to be insured (including applicant) it is mentioned by the insured himself that at the time
of inception of policy his weight was 75 kg. The respondent further said that high BMI is
considered to be a dropped risk as per the underwriting guidelines of the product ‘Punjab
National Bank Group Care 360 Degree PNB Platinum’.
I have heard both the parties and carefully examined the documents on record. It is very
clear from the proposal form of the respondent company that weight declared by the
complainant was 75 kg on inception of the policy i.e. 20.03.2021. But during the time of
admission i.e. on 21.07.2021 the weight is indicated to be 123.55 kg and BMI as 43.2. It is
really difficult that over a period of four months weight of somebody increases from 75 kg
to 123.55 kg. This clearly tantamounts to non disclosure of material fact. The respondent
company’s action of repudiation is correct. Therefore the complaint is liable to be
dismissed.
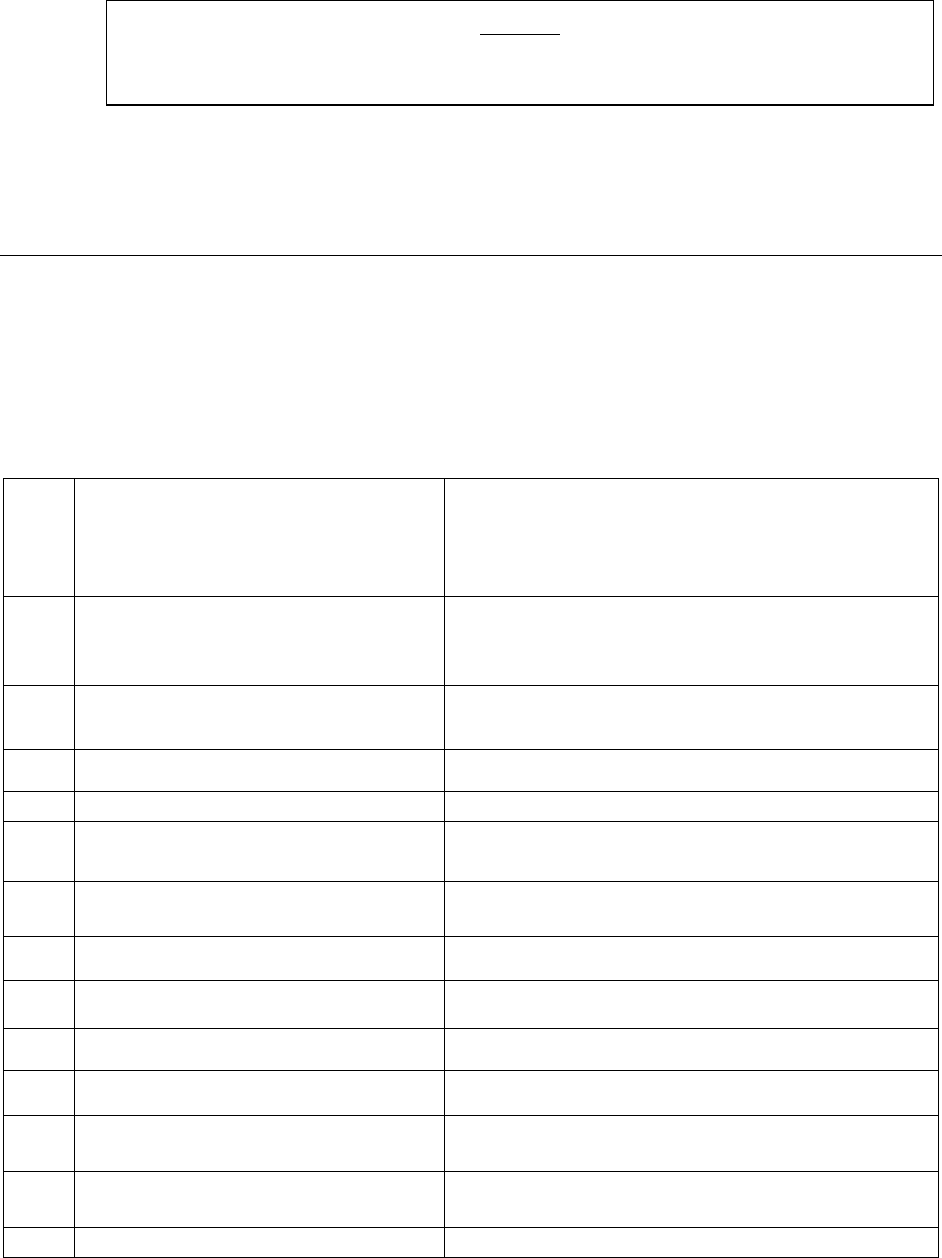
•
• Let copies of the order be given to both the parties.
Place : Bhopal (RAVINDRA MOHAN SINGH)
Date: 27.04.2022 INSURANCE OMBUDSMAN
Mr. Yatish Kumar Thakur .…….……………………………………………………..….. Complainant
V/s
National Insurance Co. Ltd. ……. ………. ………….. ….………….……………………Respondent
COMPLAINT NO: BHP-H-048-2122-0803 ORDER NO: IO/BHP/A/HI/0045 /2022-2023
1.
Name & Address of the
Complainant
Mr. Yatish Kumar Thakur
Punjab National Bank Kartar Sharm Bhawan
Mandi Gate ke Pass, Pandri
Raipur
2.
Policy No:
Type of Policy
Duration of policy/Policy period
25xxxxxxxxxxxxxxxxxx0252
Group Mediclaim Tailor Made Policy
01.10.2020 to 30.09.2021
3.
Name of the insured
Name of the policyholder
Mr. Yatish Kumar Thakur
Mr. Yatish Kumar Thakur
4.
Name of the insurer
National Insurance Co. Ltd.
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/
Rejection
--
7.
Date of receipt of the Complaint
04.02.2022
8.
Nature of complaint
Partial settlement of claim
9.
Amount of Claim
Rs.2,62,335/-(Rs. 156160 + Rs. 106175)
10.
Date of Partial Settlement
26.04.2021
11.
Amount of relief sought
Rs. 5,00,000/- + Claim amount
12.
Complaint registered under Rule
Rule No. 13(1)(d) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
28.04.2022 at OIO Bhopal
14.
Representation at the hearing
AWARD
The complaint filed by Mr Ravishankar Kewalramani stands dismissed herewith.
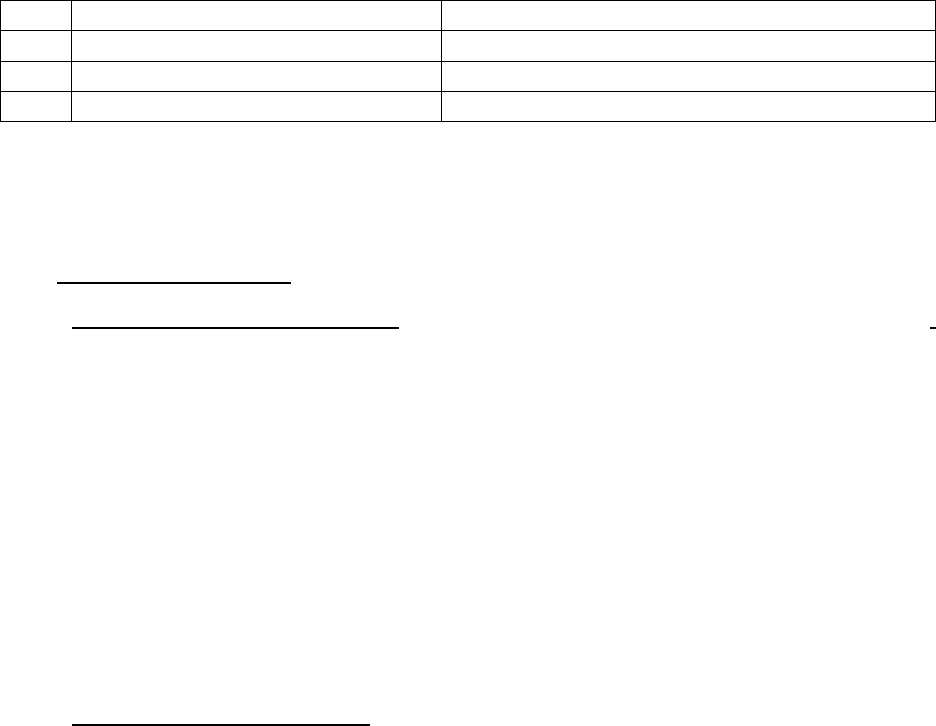
• Mr. Yatish Kumar Thakur Complainant) has filed a complaint against National Insurance
Co. Ltd (Respondent) alleging partial settlement of claim.
• Brief facts of the Case –
• Contention of the complainant - The complainant has stated that the claim no.
5823212227222, claim amount Rs. 156160/- is pending with Raksha TPA, Raipur, since
20.03.2021. On 13.09.2021 the documents were submitted through mail to local office.
The claim with regard to Retinopathy is paid but the basic claim is not paid. In the claim
no. 58232021741597, out of the claim amount of Rs. 106175/- only Rs. 50,000/- is paid
but amount of Rs. 56,175/- is deducted. It is clearly mentioned in the policy that in such
cases maternity benefit has to be paid. The complainant states that due to the mental
harassment and financial loss an amount of Rs. 5 lakh (other than the claim amount be
paid to him).
• Contention of the respondent - The respondent has stated that the claim of Mr. Yatish
Kumar Thakur pertains to treatment taken by spouse Mrs. Vibha Rajput under Punjab
National Bank staff mediclaim policy 2020-21. The insured have taken treatment for
Maternity at Mata Luxmi Nursing Home, Raipur from 09.02.2021 to 18.02.2021. We have
reviewed the claim no. 58232021741597 in which it has been observed that patient was
hospitalized from DOA- 09.02.0221 to 18.02.2021 for Normal delivery and Rs. 50,000/-
was sanctioned as per capping mentioned in policy terms and condition no. 3.5 (maternity
expenses benefit extension). Hence claim settlement is in order and as per terms and
condition. For patient admission from 15.01.2021 to the claim No.09.02.2021 for
maternity complications, we have already paid Rs. 1,01,025/- in claim
no. 58232122004375.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
i) For the Complainant
Mr Yatish Kumar Thakur over GoTo Meet App
j) For the insurer
Ms Sunita Batham over GoTO Meet App
15.
Complaint how disposed
Dismissed
16.
Date of Award/Order
28.04.2022

• I have heard both the parties over GoTo Meet App at length and perused papers filed on
behalf of the complainant as well as the Insurance Company.
• Observation and Conclusion – During hearing the complainant submitted that in the claim
No. 5823212227222 claim amount of Rs.1,56,160/- is pending with Raksha TPA, Raipur. On
13.09.2021 the documents were submitted through mail to local office but it is pending till
date. The complainant submitted that in the claim No.58232021741597, out of claim
amount of Rs.1,06,175/- only Rs.50,000/- is paid and an amount of Rs.56,175/- is deducted.
Complainant further argued that it is clearly mentioned in the policy that in such cases
maternity benefit has to be paid. He has appealed to this forum for settlement of grievance
and due to mental harassment and financial loss an amount of Rs.5 lacs other than the
claim amount should be paid to him.
During their turn the respondent admitted to having issued the above policy and the claim
pertaining to treatment taken by spouse Mrs Vibha Rajput under Punjab National Bank staff
Mediclaim policy. The insured has taken treatment for maternity at Mata Luxmi Nursing
Home Raipur from 09.02.2021 to 18.02.2021. The respondent further submitted that they
have reviewed the claim No. 58232021741597 in which they have paid Rs.50,000/- as per
capping mentioned in policy terms and condition No.3.5. Respondent further submitted
that for another claim in which the patient was admitted from 15.01.2021 to 09.02.2021
for maternity complications the claim has been settled for 1,01,025/-. The claim number
for this has been mentioned as 58232122004375 by the respondent company.
I have heard both the parties and carefully examined the documents on record. For Claim
No.58232021741597 as per the claim settlement sheet of respondent company the
payable amount is Rs.50,000/- is correct and justified. For claim No.58232122004375
(complainant’s mentioned claim No.58232122272229) the net payable amount of
1,01,025/- paid by the company as per the claim processing sheet is as per the terms and
conditions of the policy. The complaint is therefore liable to be dismissed.
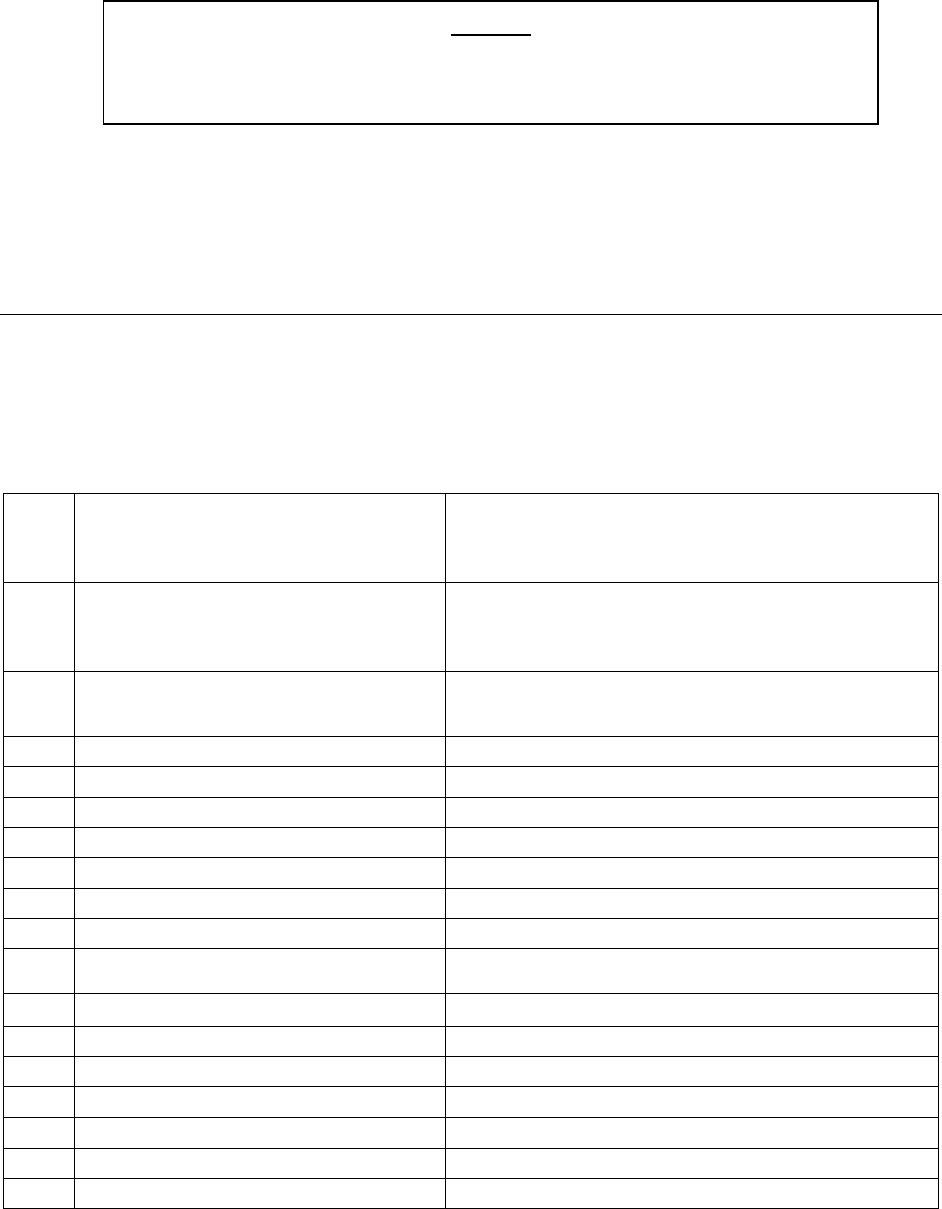
•
• Let copies of the order be given to both the parties.
Place : Bhopal (RAVINDRA MOHAN SINGH)
Date: 28.04.2022 INSURANCE OMBUDSMAN
Mr. Vaibhav Pandey….……….……………………………………………………..….. Complainant
V/s
TATA AIG General Ins. Co. Ltd. …………….….…………………………………………Respondent
COMPLAINT NO: BHP-H-046-2122-0822ORDER NO: IO/BHP/A/HI/ 0050/2022-2023
1.
Name & Address of the
Complainant
Mr. Vaibhav Pandey
42, Anudeshak Nagar,
Indore
2.
Policy No:
Type of Policy
Duration of policy/Policy period
02xxxxxxx/xxxxxx5048
Group Medicare
29.3.2021 to 28.03.2022
3.
Name of the insured
Name of the policyholder
Mr. Satish Chandra Pandey
Mr. Satish Chandra Pandey
4.
Name of the insurer
TATA AIG General Ins. Co. Ltd
5.
Date of Repudiation/ Rejection
07.09.2021
6.
Reason for Repudiation/ Rejection
Non-disclosure of material facts
7.
Date of receipt of the Complaint
11.02.2022
8.
Nature of complaint
Repudiation of claim
9.
Amount of Claim
--
10.
Date of Partial Settlement
--
11.
Amount of relief sought
Rs. 3,48,564/-
12.
Complaint registered under Rule
Rule No. 13(1)(d)Ins. Ombudsman Rule 2017
13.
Date of hearing/place
28.04.2022 at OIO Bhopal
14.
Representation at the hearing
k) For the Complainant
Mr Vaibhav Pandey over GoTo Meet App
l) For the insurer
Mr Dhiraj Mhatre over GoTo Meet App
15.
Complaint how disposed
Allowed
16.
Date of Award/Order
29.04.2022
AWARD
The complaint filed by Mr Yatish Kumar Thakur stands dismissed herewith.

• Mr. Vaibhav Pandey Complainant) has filed a complaint against TATA AIG General Ins.
Co. Ltd(Respondent)alleging repudiation of claim.
• Brief facts of the Case –
a) Contention of the complainant - The complainant has stated that he has lodged
the claim under TATA AIG General Insurance Co. Ltd.As per received repudiation letter from
TATA AIG general insurance Co. Ltd. He is not satisfied by the reason of repudiation. He
had taken the policy through CANARA BANK, MR-10 Branch, Indore. His father Late Shree
Satish Chandra Pandey has been admitted in SHALBY Hospital, Janjeerwala Square, Indore
on 17.05.2021 and he has passed away on 28.05.2021. He has been admitted for COVID-19
and treatment given to him for COVID-19. Father opted the policy through CANARA bank
since inception on 29.03.2016. This health policy has been taken through CANARA Bank tie-
up. His father had renewed his policy continuously from date of inception as given below
under the head policy details. 29.03.2016 to 28.03.2017-:
120100/12001/2016/A005425/PE00196553-: Apollo Munich health Ins. Co. Ltd.-: SUM
INSURED-: 500000. 29.03.2017 to 28.03.2018-: 12/xxxxxxxxxxxxxxxxx3/015-: Apollo
Munich health Ins. Co. Ltd. -: SUM Insured -: 500000. 29.03.2018 to 28.03.2019-:
12xxxxxxxxxxxxxxxxx1/396-: Apollo Munich health Ins. Co. Ltd. Sum Insured-:
500000.29.03.2019 to 28.03.2020-: 12xxxxxxxxxxx6/837-: Apollo Munich health Ins. Co.
Ltd. SUM Insured -: 500000. 29.03.2020 to 28.03.2021-: 12xxxxxxxxxxxxx8/031-: HDFC
ERGO Health insurance Ltd. 29..3.2021 to 28.03.2022-: 02xxxxxxx/xxxxx5048-: TATA AIG
general insurance Co.Ltd. SUM insured -: 500000. Reason of repudiation of TATA AIG
general insurance Co. Ltd.-: They have repudiated the claim under clause “NON-
DISCLOSURE FOR CKD”. Representation Reason -:Here we would like to confirm you that
the claim has been reported after five years waiting period of policy and as per policy
terms & condition all Pre-Existing diseases are payable after 3 years waiting period and
our policy is in force over & above three years i.e. Claim reported after five years waiting
period. Hence there was no applicability of DISCLOSURE or NON-DISCLOSURE. He has
not hid the facts since inception of the policy i.e., 2016, March, 29. Policy is in force without
break in renewal and the premium has been debited directly from the account of my father

as shifting of policy or choice of any company is not at all our end. This is a bank insurance
health policy and even we have not intimated at the time of renewal of the policy
automatically they are debiting the amount from our account & renewing the health policy
every year without failed. Sir now TATA AIG is intently repudiating the claim of my
father, as they want to take the advantage of the circumstances of the people and our
country, as they know that my father has been suffering for COVID-19 and at the time of
his treatment condition of entire country was very pathetic. TATA AIG Insurance company
is not paying our claim since long time. We were continuously taking follow ups with them
but till date neither they settled my claim nor cooperating to us. Finally, we have decided
to take the help from respective Ombudsman department. I humbly request you to please
look at the matter on high priority as he has already lost my father from COVID-19 and
even troubling from financial issues. He has spent Rs. 348564/-. This amount is of
submitted claim and also, he has already spent over & above 4 lac rupees for his treatment.
Sir, request you to kindly instruct to the TATA AIG team to immediately settle & pay claim
without delay. Almost 7 months have been passed away and entire family is suffering from
financial crisis. TATA AIG is not settling to claim and even behavior is also very much harsh
hence approaching to this office.
b) Contention of the respondent - The respondent in their SCN have stated that the
insured Mr.Satish Chandra Pandey had obtained the Group Medicare Policy SI – 5 L bearing
number 0238452957 [Certificate No – 00035048] on 29.03.2021 along with the terms and
conditions mentioned there under. Section 4 : General Conditions ; reads as under :7. Mis-
representation, or non-disclosure of material facts : We will not be liable to pay under the
policy if any Misrepresentation or non-disclosure of material facts noted at the time of
claim or otherwise, whether by You or any Insured Person or anyone acting on behalf of
You or an Insured Person & Policy shall be void ab-initio without any premium refund. The
insured Mr.Satish Chandra Pandey was admitted in Shalby Hospital, Indore for the period
17.05.2021 to 28.05.2021. It was observed that the insured was diagnosed with “Covid 19
Positive
Infection”.
FHPL TPA Claim Number – 2021060400182
Tata AIG Claim No –
0821979381A.
Estimated Hospitalization Cost – INR 348564/-We had denied claim vide
letter dated 07.09.2021
under“NonDisclosure”clause.
It is submitted that as per various
treatment records, insured was found suffering with following ailments prior to our policy
inception. In the OPD case paper of Dr.NareshPahwa [Consultant Nephrologist]
dated05.11.2019 below history found ;Diabetes since 1995, HTN & thyroid since 15 years
. In 2014 S. Creatinine 2 mg/dl &Hb 6 gm . On 17.10.2019 S. Creatinine 2 mg /dl. On
13.09.2018, Serum Creatinine – 3.56 mg/dlIn various case papers of Dr.NareshPahwa of
2019 & 2020 below drugs found ;
ThyroxThyroxine Failing Thyroid
Zoryl 1 mg Glimepride to control blood sugar
Ativan Lorazepam Sedative
NephtorTorsemide Failing Kidney
Prolomet XLMetoprolol High Blood Pressure
In Enrollment Form , this is an application for insurance & will form the basis of policy
certificate that we may issue. Every information, this application seeks is important &
mandatory. Please read all questions & answer them carefully. You must provide
complete & correct information. Incomplete/incorrect/partially correct information
may lead to cancellation of proposal & policy certificate even if it is issued. Based on
declarations made by insured during policy inception, we had issued the policy. The policy
copy & policy wording was sent to insured via Courier [POD/Dispatch number –
DN5588415 - 845156]It is submitted that insured has not disclosed to us about above
mentioned history to us while taking policy from us in March 2021. The medical history if
any is material information to us for issuance of a health policy which was not declared to
us while taking policy from us. Had this information been made available to us, we would
not have issued the policy at all. We would like to submit as under: the declaration of
Failing Kidney & Thyroid, Diabetes, High Blood Pressure prior to the policy is material to us
for accepting coverage under the Medicare policy. The claim has been denied due to
material non-disclosure in the proposal form. Had customer declared about above diseases
to us, we would not have issued policy in first place. Hence, we were unable to consider his
claim. We had given ample opportunity to insured to disclose all significant past history.

Also we had mentioned implications of “Not declaring health condition” in the Enrollment
form also. Claim was therefore repudiated strictly in accordance with the terms &
conditions of the Policy.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
• I have heard both the parties over GoTo Meet App at length and perused papers filed on
behalf of the complainant as well as the Insurance Company.
• Observation and Conclusion - During hearing the complainant submitted that his father
late Shri Satish Chandra Pandey had opted for the present policy through Canara Bank
since inception on 29.03.2016. His father had renewed his policy continuously - 29.03.2016
to 28.03.2017-: 120100/12001/2016/A005425/PE00196553-: Apollo Munich health Ins. Co.
Ltd.-: SUM INSURED-: 500000. 29.03.2017 to 28.03.2018-: 12/xxxxxxxxxxxxxxxxx3/015-:
Apollo Munich health Ins. Co. Ltd. -: SUM Insured -: 500000. 29.03.2018 to 28.03.2019-:
12xxxxxxxxxxxxxxxxx1/396-: Apollo Munich health Ins. Co. Ltd. Sum Insured-:
500000.29.03.2019 to 28.03.2020-: 12xxxxxxxxxxx6/837-: Apollo Munich health Ins. Co.
Ltd. SUM Insured -: 500000. 29.03.2020 to 28.03.2021-: 12xxxxxxxxxxxxx8/031-: HDFC
ERGO Health insurance Ltd. 29.03.2021 to 28.03.2022-: 02xxxxxxx/xxxxx5048-: TATA AIG
general insurance Co.Ltd. SUM insured -: 500000. The complainant further submitted that
his father late Shri Satish Chandra Pandey was admitted in Shalby Hospital, Janjeervala
Square, Indore on 17.05.2021 and he passed away on 28.05.2021. The respondent
company repudiated the claim under the clause non disclosure for CKD. The complainant
put forth the argument that the claim has been reported after five years waiting period of
the policy and as per the present policy terms and conditions all pre existing diseases are
payable after three years waiting period. Therefore this clause does not apply in their case.
The complainant further maintained that no facts are hidden by them since inception of
the policy i.e. 2016. This is a Bank Insurance Health Policy and it is renewed ever year
automatically by the Bank by debiting the amount from their account. The complainant
submitted that he has spent Rs.3,48,564/- and has requested this forum to settle the claim.
During their turn the respondent company admitted having issued the above policy and
also of receiving the claim from the complainant. They further submitted that Mr Satish
Chandra Pandey was admitted in Shalby Hospital for the period 17.05.2021 to 28.05.2021
and was diagnosed with Covid 19 positive infection. The claim has been repudiated on
07.09.2021 on non disclosure clause. The respondent company further submitted that as
per OPD case paper of Dr Naresh Pahwa dated 05.11.2019 the medical history of the
patient is as follows - Diabetes since 1995, HTN & thyroid since 15 years. In 2014 S.
Creatinine 2 mg/dl &Hb 6 gm. On 17.10.2019 S. Creatinine 2 mg/dl. On 13.09.2018, Serum
Creatinine – 3.56 mg/dlIn. The respondent further submitted that in enrolment form there
is an application for insurance and every information is important and mandatory. They
further said that medical history is very important and should have been declared during
the time of taking the policy and having known about this they would not have accepted
the insurance proposal.
I have heard both the parties and carefully examined the documents on record. It is clearly
established that the complainant’s father had been insured since 29.03.2016 till date. The
policy has been ported to TATA AIG From the previous insurers without any break. The
enrolment form of the respondent company has been very closely examined and it does
not have a column for mentioning anything about the medical history of the patient.
Besides, since the policy has been in existence since 2016 and has been ported therefore
at this stage to dispute about what should have been declared at the inception of this
particular policy carries no meaning and the clause of PED or non disclosure does not apply.
In view of foregoing, the complaint is liable to be allowed.
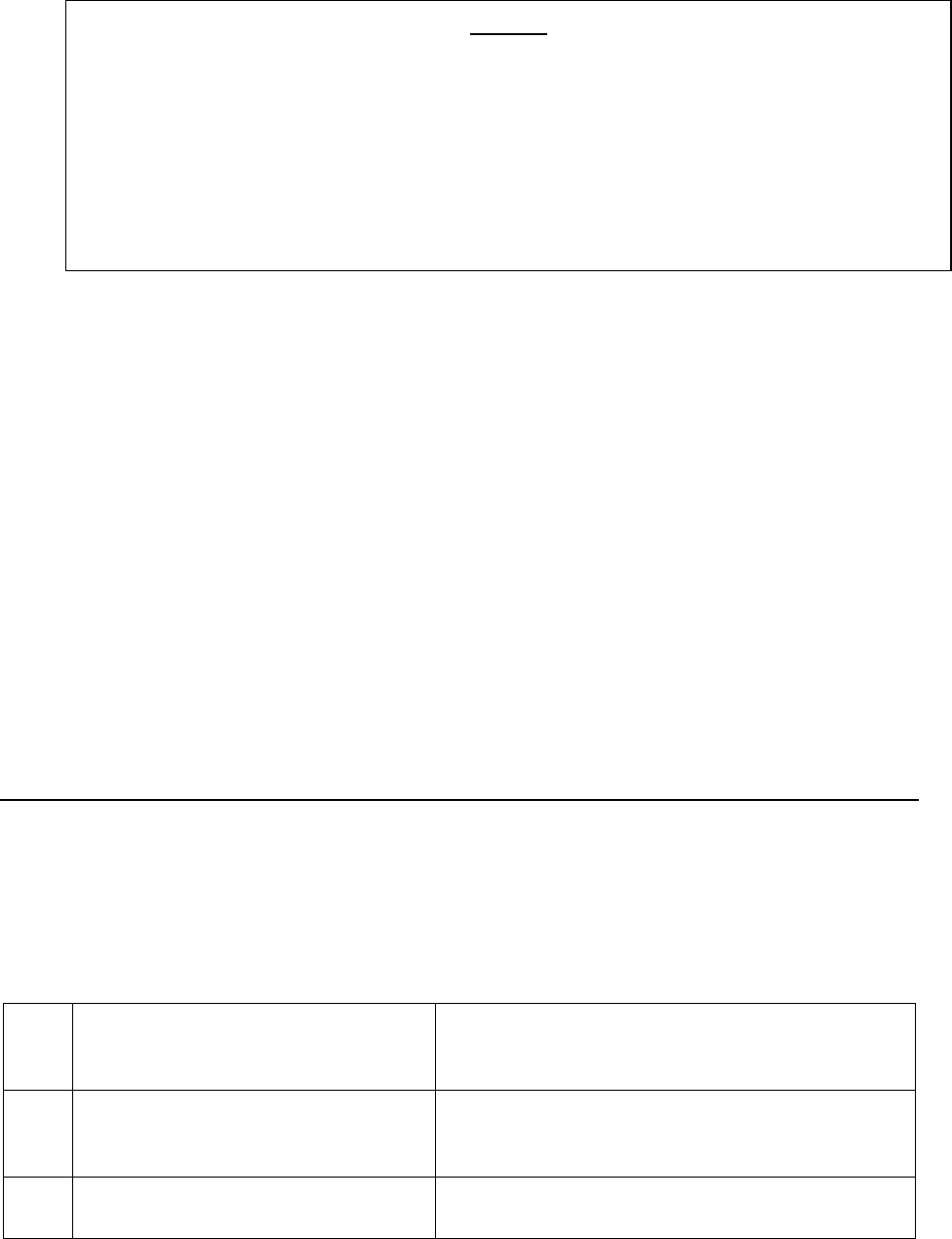
•
• Let copies of the order be given to both the parties. Compliance shall be intimated to this
forum.
Place: Bhopal (RAVINDRA MOHAN SINGH)
Date: 29.04.2022 INSURANCE OMBUDSMAN
Mr. Ramesh Kumar Sihote ……….…………………………………………….….. Complainant
V/s
Oriental Insurance Co. Ltd. ………. ………….. ….………….……………………Respondent
COMPLAINT NO: BHP-H-050-2122-0829 ORDER NO: IO/BHP/A/HI/ 0048 /2022-2023
1.
Name & Address of the
Complainant
Mr. Ramesh Kumar Sihote
Kasturba Nagar, Jarhabhata
Bilaspur
2.
Policy No:
Type of Policy
Duration of policy/Policy period
193391/48/2021/511
PNB –OREINTAL Mediclaim Policy 2017
02.01.2021 to 01.01.2022
3.
Name of the insured
Name of the policyholder
Mrs. Saroj Sihote
Mr. Ramesh Kumar Sihote
AWARD
The complaint filed by Mr. Vaibhav Pandey is allowed with directions to the respondent
company to settle the claim and pay Rs.3.48,564/- (Rs. Three Lacs Forty Eight Thousans
Five Hundred Sixty Four only) to the complainant with interest @ 2% over bank rate from
the date of receipt of claim to the date of payment within 30 days from the receipt of this
order.
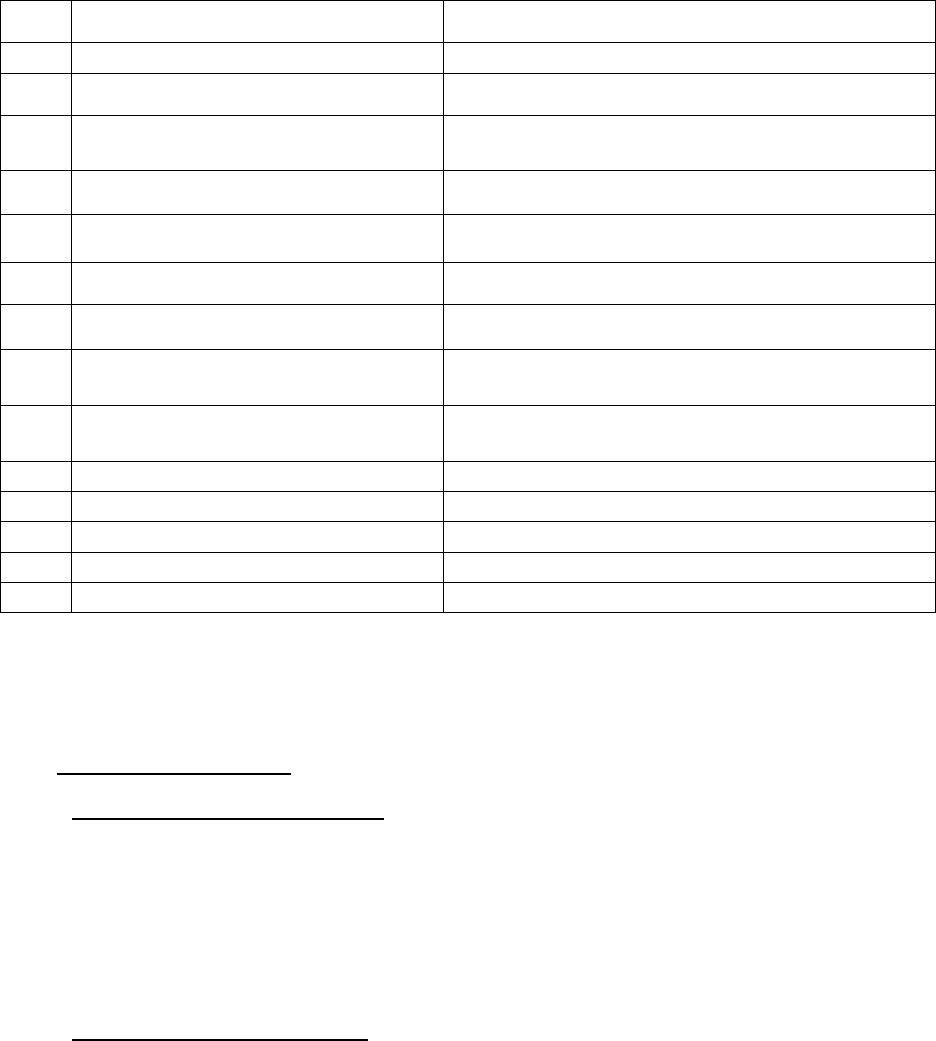
• Mr. Ramesh Kumar Sihote (Complainant) has filed a complaint against Oriental Insurance
Co. Ltd (Respondent) alleging non settlement of claim.
• Brief facts of the Case –
• Contention of the complainant - The complainant has stated that he had bought the
aforementioned policy from the respondent Company. His wife Mrs. Saroj Sihote was
admitted in Cure and Care Hospital, Bilaspur from 18.04.2021 to 26.04.2021. He had
submitted the documents in the Company’s office on 03.06.2021 , but the claim is not
paid till date.
• Contention of the respondent - The respondent in their SCN have stated that out of the
claim amount/ bill of Rs. 3,39,191/- an amount of Rs. 2,40,553/- is paid by the Company
under the heads of Pharmacy & Medicine Charges, Consultant Charges, Misc. Charges,
Investigation & Lab Charges.
• The complainant has filed complaint letter, Annex. VI A and correspondence with
respondent, while respondent have filed SCN with enclosures.
4.
Name of the insurer
Oriental Insurance Co. Ltd.
5.
Date of Repudiation/ Rejection
--
6.
Reason for Repudiation/ Rejection
--
7.
Date of receipt of the Complaint
11.02.2022
8.
Nature of complaint
Non settlement of claim
9.
Amount of Claim
Rs. 339191/-
10.
Date of Partial Settlement
--
11.
Amount of relief sought
--
12.
Complaint registered under Rule
Rule No. 13(1)(d) Ins. Ombudsman Rule 2017
13.
Date of hearing/place
29.04.2022 at OIO Bhopal
14.
Representation at the hearing
m) For the Complainant
--
n) For the insurer
--
15.
Complaint how disposed
Settled before hearing
16.
Date of Award/Order
29.04.2022
• Observation and Conclusion - The complainant vide letter dated 28.04.2022 has informed
that he has received payment from the respondent company on 02.03.2022 and therefore
he has requested to close the complaint. The complaint is hereby closed as it is mutually
settled between the two parties before hearing.
•
• Let copies of the order be given to both the parties.
Place: Bhopal (RAVINDRA MOHAN SINGH)
Date: 29.04.2022 INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, Kolkata
(States of West Bengal, Sikkim and Union Territories of Andaman & Nicobar Islands)
(UNDERRULENO.16/17OFTHEINSURANCEOMBUDSMANRULES,2017)
Ombudsman Name: SHRI P.K.RATH
CASE OF COMPLAINANT– SHRI RABIN KUMAR NAG
VS
RESPONDENT: NATIONAL INSURANCE COMPANY LIMITED
COMPLAINT REF: NO: KOL-H-048-2122-0919
AWARD NO:IO/KOL/A/HI/0027/2022-2023
1.
Name &Address of the Complainant
Shri Rabin Kumar Nag
Swiss Abode, Flat No.3A
66, Russa Road (East), 1
st
Lane
Tollygunge, Kolkata – 700 033.
AWARD
The complaint filed by Mr. Ramesh Sihote is closed as it has been mutually settled between
the two parties before hearing.
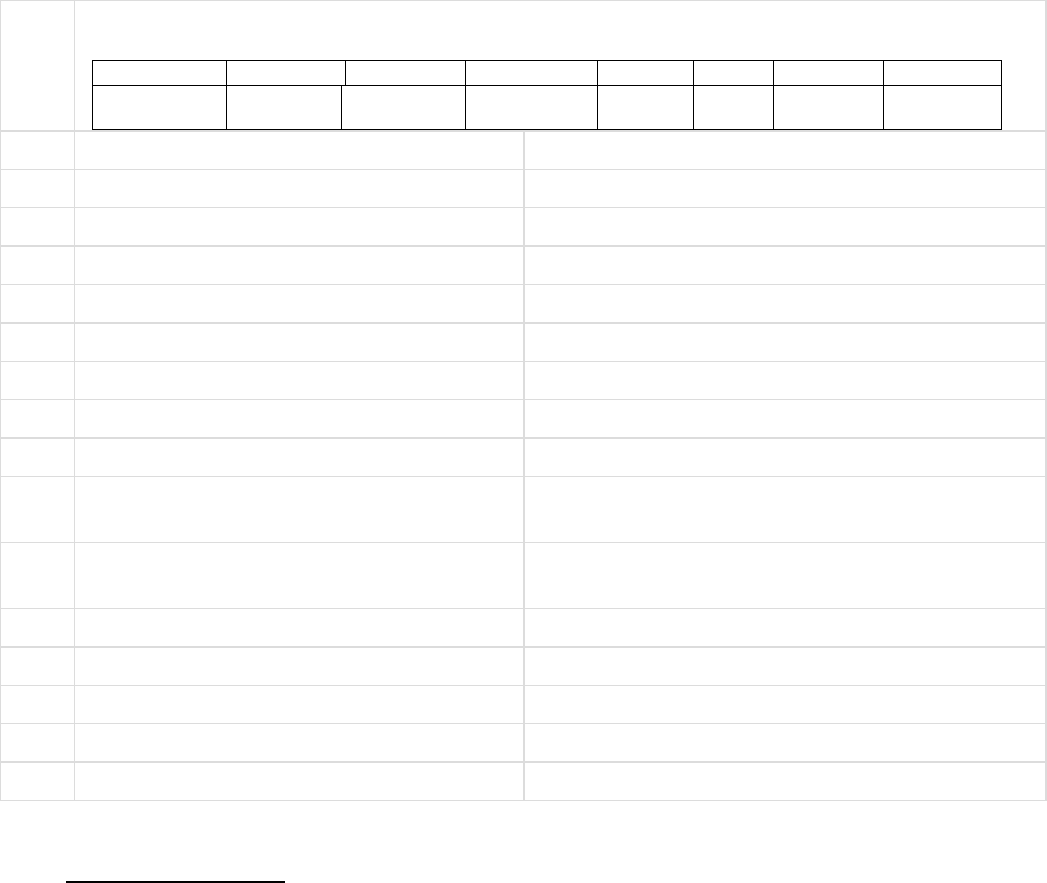
2.
Type Of Policy: Life / Health / General
Policy Details:
Policy Number
Sum Assured
From Date
To Date
DOC
Premium
Policy Term
Paying Term
251100XXXX
XXXX0269
40000001-
01-11-2021
31-10-2022
One year
3.
Name of insured
Mrs. Dulali Nag
4.
Name of the insurer
National Insurance Company Limited
5.
Date of Repudiation
6.
Reason for Repudiation
7.
Date of receipt of the Complaint
17-Jan-2022
8.
Nature of Complaint
Partial settlement of claim
9.
Amount of Claim
16,611.00
10.
Date of Partial Settlement
11.
Amount of relief sought
16,611.00
12.
Complaint registered under Insurance
Ombudsman
Rules 2017
Rule 13(1)(b) – any partial or total repudiation of
claim by the insurer
13.
Date of hearing
Place of hearing
25-Apr-2022
14.
Representation at the hearing
a)For the Complainant
Shri Rabin Kumar Nag
b)For the Insurer
Shri Ranjan Kumar Bhatia
15.
Complaint how disposed
16.
Date of Award
28-Apr-2022
17. Brief Facts of the Case:
The complainant is a retired employee of Bank of India and covered himself and his wife, Mrs. Dulali Nag
under Group Mediclaim Policy with National Insurance Company. Mrs. Dulali Nag was admitted in the
hospital on 02-12-2021 for Cataract Surgery and discharged on the same day. The total hospital bill was
for Rs.35,000/- and the Insurance Company approved cashless claim for Rs.26,000/-. After discharge from
the hospital, the insured lodged reimbursement claim for Rs.20,563/- but the Insurance Company
settled the claim for Rs.4,152/-.
The Insurance Company has stated in their self-contained note that the insured, Mrs. Dulali Nag was
admitted in the hospital for cataract surgery and availed cashless facility for Rs.26,000/- against the total
hospital of Rs.35,000/-. After discharge from the hospital, the insured lodged reimbursement claim for
Rs.20,563/- and the Insurance Company settled the claim for Rs.4,152/-. The deduction details are as
follows :
Rs.9,000.00 as per PPN guidelines (Total hospital bill Rs.35,000/-)
Rs.6,157.00 beyond date
Rs.200.00 Administrative charged
Rs.315.00 Eye Pad
Rs.140.00 Service Charge
Rs.399.00 Medicines – not payable
18. Contention of the complainant: The complainant has stated in the hearing that the insured, Mrs.
Dulali Nag, wife of Shri Rabin Kumar Nag was admitted in the hospital for cataract surgery and after
discharge from the hospital, the insured lodged claim for reimbursement of treatment expenses but the
Insurance Company settled the claim partially. The Insurance Company also settled the pre and post
claim partially.
19. Contention of the Respondent:
The representative of the Insurance Company has stated in the hearing that the insured was admitted in
the hospital for Cataract surgery and the Insurance Company approved cashless claim for Rs.26,000/- as
per PPN agreement. In regard to pre and post claim, the Insurance Company settled the same as per
Policy terms and conditions.
Observation and conclusions: The complainant has attended the hearing physically at this office premises
whereas the representative of the Insurance Company has attended the hearing online. The complainant
has stated what he already stated in his written complaint submitted to this office. The representative
of the Insurance Company has stated that the claim has been settled as per PPN agreement as well as
policy terms and conditions.
It is found from the submitted documents as well as submissions made by the parties that the Insurance
Company settled the claim as per PPN Agreement as well as Policy terms and conditions.
AWARD
Taking into account the facts and circumstances of the case and submissions made by both the parties
during the course of hearing and after going through the documents on record, it is observed that the
insured was admitted in the hospital for cataract surgery and availed cashless claim. After discharge
from the hospital, the insured lodged reimbursement claim but the Insurance Company settled the claim
partially. It is found from the submitted documents as well as submissions made by the parties that the
basis of settlement of the claim by the Insurance Company is as per PPN Agreement as well as Policy
terms and conditions. Thus, the Insurance Company is not liable to make any payment to the insured
further. Hence, the complaint is dismissed without any relief to the complainant.
If the decision is not acceptable to the complainant, she/he is at liberty to approach any other
Forum/Court as per Law of the Land against the Respondent Insurer.
Dated at Kolkata on 28
th
day of April, 2022 P K RATH
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF RAJASTHAN
UNDER THE INSURANCE OMBUDSMAN RULES, 2017(as amended till date)
OMBUDSMAN – SHRI RAJIV DUTT SHARMA
CASE OF AJAY MEENA V/S THE NATIONAL INSURANCE CO.LTD
COMPLAINT REF: NO JPR-H-048-2223-0040
AWARD No. IO/JPR/H/A/2223/000
1.
Name & Address of the Complainant
Shri Ajay Meena,
80/414, Patel Marg, Mansarover, Jaipur
2.
Policy No:
Type of Policy
Commencement of the Risk /Policy
period Sum Insured
25110050xxxx000250
Group Health Insurance Policy (Union Bank
employees)
01.10.2020 to 30.09.2021
Rs. 4.00 Lacs
3.
Name of the insured
Name of the policyholder
Shri Ajay Meena
Shri Ajay Meena
4.
Name of the insurer
The National Insurance Company Ltd
5.
Date of Repudiation
Partially Settled on 18.12.2021
6.
Reason for repudiation
Partial settlement of covid claim
7.
Date of receipt of the Complaint
30.03.2022
8.
Nature of complaint
Partial settlement of covidclaim
9.
Amount of Claim
Rs.257259
10.
Date of Partial Settlement
Rs.144846
11.
Amount of relief sought
Rs.42000
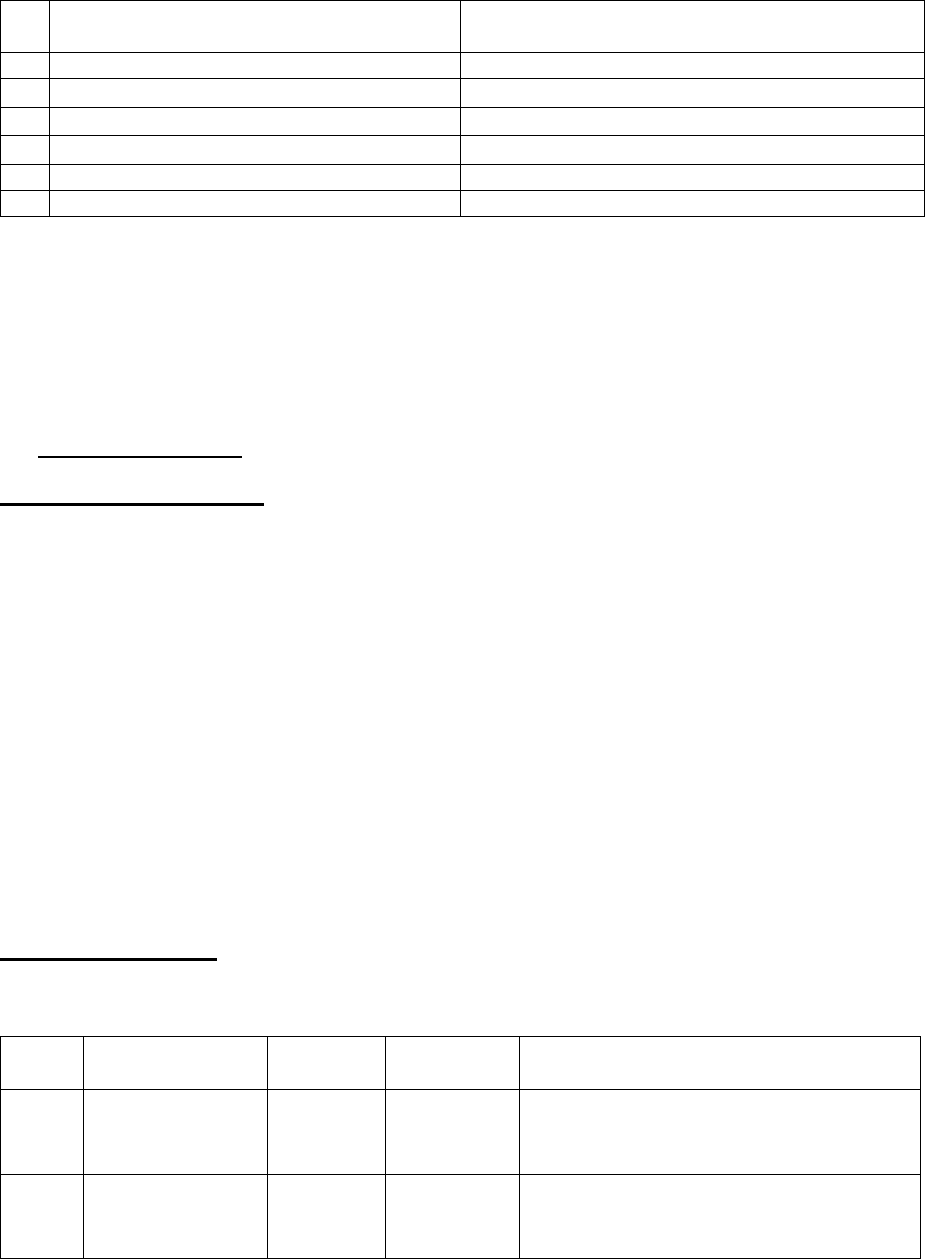
12.
Complaint registered under
Rule no: of IOB rules
13(1) (b)
13.
Date of hearing/place
27.04.2022/ Through GoToMeeting
14.
Representation at the hearing
. For the Complainant
Shri Ajay Meena
b. For the insurer
Shri Ranjan Bhatia, Manager
15
Complaint how disposed
Award
16
Date of Award/Order
27.04.2022
17). Brief fact of the case : Shri Ajay Meena(herein after referred to as the complainant) had filed
a complaint against the decision of The National Insurance Company Ltd (herein after referred to
as respondent Insurance Company) alleging partial settlement of mediclaim under Group Health
Insurance policy no.25110050xxxx000250.
18) Cause of Complaint:
Complainant’s argument: The complainant stated that he had insured under group health
insurance policy for from Respondent insurance company with risk coverage from 01.10.2020 to
30.09.2021 insuring self and family taken by his employer (Union Bank). The complaint himself
suffered from covid and remained hospitalized in Santokaba Durlabhji Memorial Hospital, Jaipur
from 24.05.2021 to 04.06.2021. After discharged from the hospital the hospitalisation
reimbursement claim for Rs. 257259 was submitted by him to the insurance company under claim
no. 251100502196454038 on 24.06.2021. Out of which the insurance company settled the claim
for Rs. 144846 and balance of Rs. 12413were disallowed towards excess room rent charges and
some other grounds. The complainant represented his case for settlement to the GRO of insurance
company on 31.12.2021 and 10.02.2022. But the insurance company maintained its decision to his
representation. Being aggrieved complainant approached this forum for redressal of his grievance.
Insurer’s argument:- The Insurance Company in its SCN dated 21.04.2022 submitted that the
following deductions have been made from the claimed amount as per details :-
S.no.
Main Head
Amount
Deduction
Reason for deduction
1
Room Rent ICU
63700
28700
Excess room charges not payable as per
policy terms and conditions
2
Room Rent
Private Room
60000
35000
Excess room charges not payable as per
policy terms and conditions
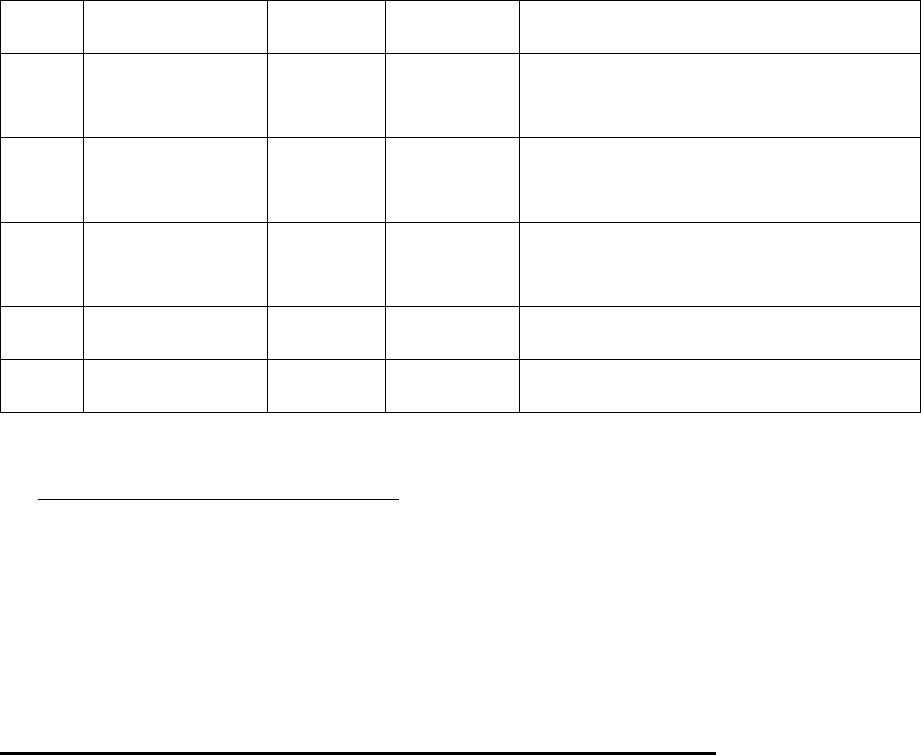
3
Consumables
5040
5040
As detailed brake up not available.
4
Pathology
reports
23580
23580
As reports not signed by MD
Pathologist
5
Para Medical
care
18000
18000
No Proper detail with supporting
document not enclosed
6
Miscellaneous
charges
893
893
Not payable as per policy terms and
conditions
7
Consultation fee
1200
1200
Consultation note not provided
Total
122149
122149
The respondent, therefore, settled the claim as per the terms and conditions of the policy
19) Reason for Registration of Complaint: Partial settlement of mediclaim under health insurance
policy.
20) The following documents were placed for perusal.
a. Complaint letter
b. Copies of documents submitted by the complainant
c. Form VI A duly signed by the complainant.
d. SCN and a form VIIA duly signed by the Insurance Company
21) Result of hearing with both parties (Observations and Conclusion) :- Heard both the sides,
the complainant and the Insurance Company through video conferencing. The complainant submitted that
his claim particularly related to the ICU room rent and Pathology report charges were not settled by the
insurance company correctly. His ICU room entitlement was Rs. 7500 as per policy conditions and
deduction owing to pathology reports not signed by the Doctor was not informed by the insurance company,
otherwise he would have complied and removed this discrepancy. The Insurance company reiterated their
submission made in the SCN and also submitted that the case was reviewed again and agreed to settle the
difference of ICU room charges of Rs. 2500 for 7 days = 17500 (i.e. Rs. 7500-5000 (paid earlier) and
Rs.23580 for pathology reports charge.
On perusal of the documents exhibited and oral submissions made during the course of Video
Conferencing, it is observed that the insurance company is ready to settle the balance amount of
claim of Rs. 17500 towards ICU charges and Rs. 23580 towards Pathology reports (total 41080);
hence the complaint is hereby disposed off.
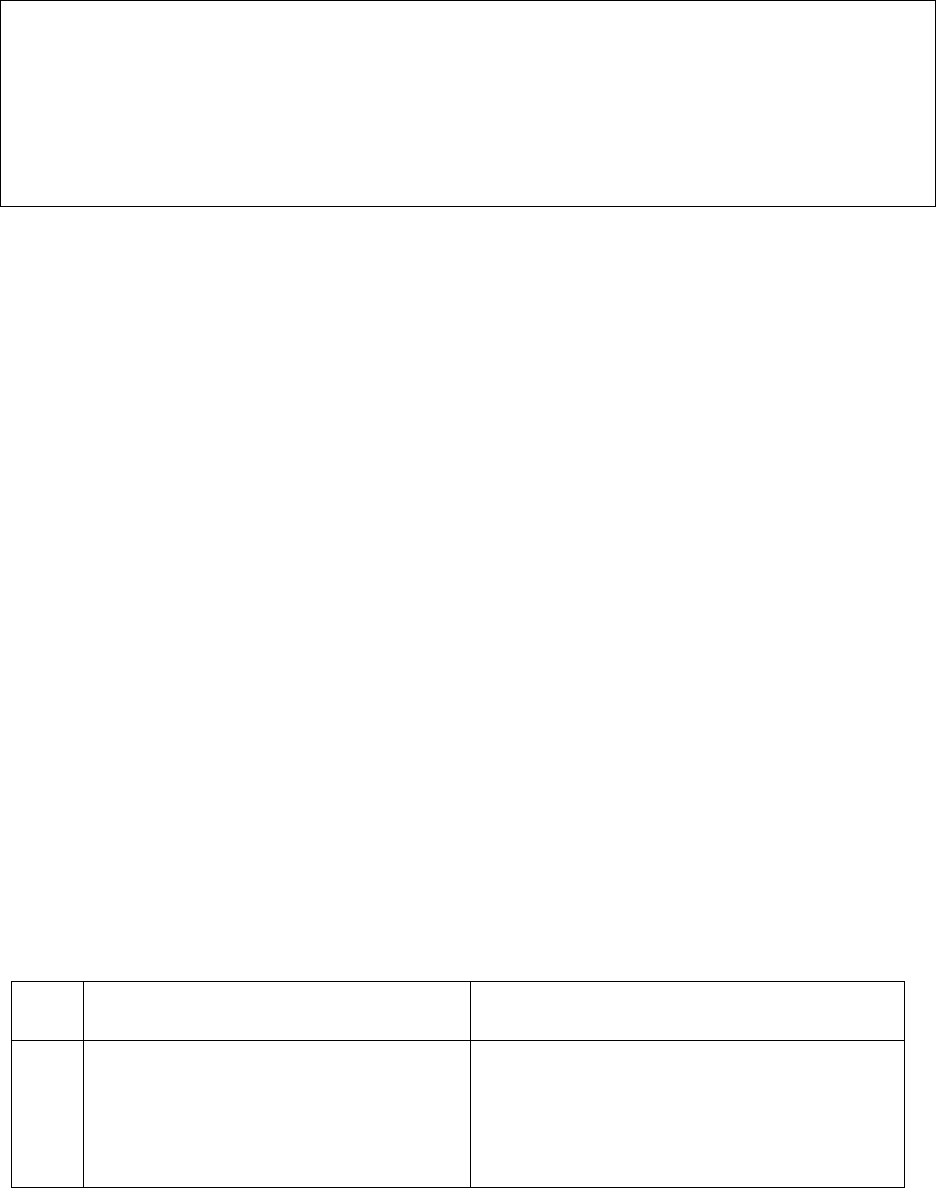
Award
Taking into account the facts and circumstances of the case and submissions made by both
the parties during the course of hearing, the Insurance Company is directed to settle the
claim of Rs. 41080 to the complainant as agreed.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions of
Insurance Ombudsman Rules, 2017 (as amended till date):
a)
According to Rule 17(5) of Insurance Ombudsman Rules, 2017
(as amended till date)
, a copy of the
award shall be sent to the complainant and the insurer named in the complaint.
b)
As per Rule 17(6) of Insurance Ombudsman Rules, 2017
(as amended till date)
, the insurer shall
comply with the award within 30 days of the receipt of the award and intimate compliance of the same to
the Ombudsman.
Place: Jaipur RAJIV DUTT SHARMA
Dated: 27.04.2022 (INSURANCE OMBUDSMAN)
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF RAJASTHAN
UNDER THE INSURANCE OMBUDSMAN RULES, 2017(as amended till date)
OMBUDSMAN – SHRI RAJIV DUTT SHARMA
CASE OF SMT. NUPUR SAREEN V/S UNITED INDIA INSURANCE CO.LTD
COMPLAINT REF: NO JPR-H-051-2223-0046
AWARD No. IO/JPR/H/A/2223/000
1.
Name & Address of the Complainant
Smt. Nupur Sareen,
S-14, Shopping Centre, Tilak Nagar, Jaipur
2.
Policy No:
Type of Policy
Commencement of the Risk
Sum Insured
1622012021xxxx00001023028
Group Health Insurance (Maha Bank
Swasthya Yogna Policy)
20.11.21 to 19.11.22
Rs.500000/-
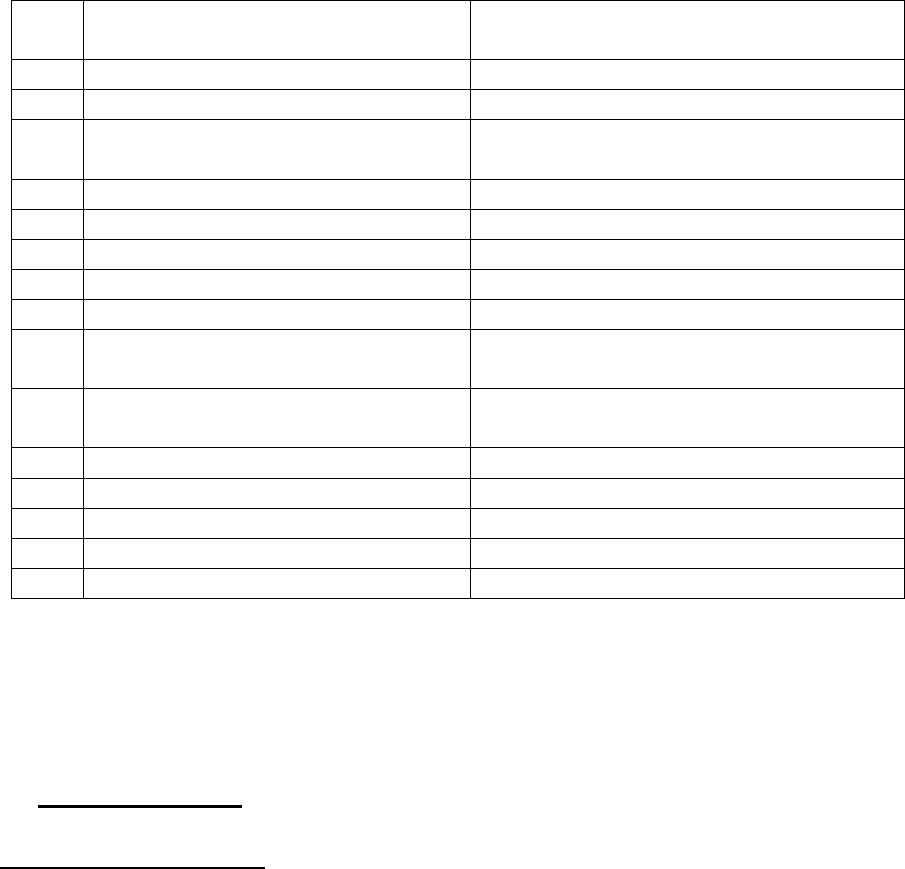
3.
Name of the insured
Name of the policyholder
Smt.Nupur Sareen
Smt.Nupur Sareen
4.
Name of the insurer
United India Insurance Company Ltd
5.
Date of Repudiation
05.03.2022
6.
Reason for repudiation
Falls under exclusion-treatment not listed in
day care procedure as per cl. No.3.2
7.
Date of receipt of the Complaint
04.04.2022
8.
Nature of complaint
Full Repudiation of mediclaim
9.
Amount of Claim
Rs 159880/-
10.
Date of Partial Settlement
N.A.
11.
Amount of relief sought
Rs.159880/-
12.
Complaint registered under
Rule no: of IOB rules
13(1) (b)
13.
Date of hearing/place
27.04.2022 / Video Conferencing through
GoToMeeting
14.
Representation at the hearing
a) For the Complainant
Shri Girish Sareen, Husband
b) For the insurer
Mrs. Nayana Makaji, Dy. Manager
15
Complaint how disposed
Award
16
Date of Award/Order
27.04.2022
17). Brief fact of the case :Smt. Nupur Sareen (herein after referred to as the complainant)
had filed a complaint against the decision of United India Insurance Company Ltd (herein
after referred to as respondent Insurance Company) alleging repudiation of mediclaim
under Health Insurance policy no.1622012021xxxx00001023028.
18) Cause of Complaint:
Complainant’s argument:The complainant stated that she had taken health insurance mediclaim
policy from Respondent insurance company with risk commencement date from 20.11.2021 to
19.11.2022 for Sum Insured of Rs. 5,00,000 covering self and family member. The complainant’s
herself was diagnosed with Bone Metastatic Breast Cancer(stage IV) in December 2021.
Subsequent to her treatment, on the advice of treating doctor, she was admitted to BMCHRC,
Jaipur to monitor the effect of cancer drug being administered for treating her Bone Metastatic
Breast Cancer on 17.02.2022and discharged on next day. Where she was administered of
Zoledronic acid, which was used in treatment of Stage IV breast cancer with Bone Mets and for
supportive care after administration of dose of Palbace and letrozone under observation. The
Mediclaim for reimbursement of the treatment taken were submitted by the Complainant to the
Insurance Company for Rs. 159880 including pre and post hospitalisaton expenseson 28.02.2022,

which was repudiated by Insurance Company on 05.03.2022on the ground that there was not any
anti-cancer drug for CA breast and Inj. Zolendric Acid was not payable as per policy condition
clause no.3.18. The complainant approached GRO on 27.03.2022 for reconsidering the Mediclaim.
But the Insurance Company reiterated its decision to his representation on the ground that patient
was hospitalized with diagnosis for supportive therapy with IV Zoledronic Acid, which was given
standalone therapy. It was neither Chemo/Immunotherapy/ Hormonal/Monoclonal Antibody nor
targeted therapy. But it was just a supportive therapy in cancer treatment. Infusion of IV Zoledronic
Acid could be done on OPD basis and it was not required 24 hours hospitalization. Hence, as per
clause 3.2 – Procedures/treatment usually done in OPD basis are not payable under policy even if
converted as an inpatient in the hospital for more than 24 hours, hence he did not get any relief
from the Insurance Company. Being aggrieved complainant approached this forum for redressal
of his grievance.
It was further submitted by the Complainant that earlier claims of the same treatment/medicine
taken in the hospital as Day care and hospitalization have been paid by the Insurance Company in
compliance of the Award passed by the Valsad District Consumer Commission, Gurjat in Dipali
Firozbhai Vasava Vs United India Insurance Company Ltd, CC no. 192/2019 dated 24.11.2020
and Manmohan Nanda Vs United India Insurance Company an Anr. Civil Appeal no. 8386/2015
in reference to her claim. The Insurance company had failed to appreciate that only a treating
doctor and not the insurance company can decide the line of the treatment given to the patient for
a disease / ailment which is not only life threatening but also painful. The hospitalization of the
patient was carried out only on the medical advice of the treating doctor for her treatment.
Insurer’s argument:- The Insurance Company in its SCN dated 11.03.2022 submitted that
Insured was admitted with the diagnosis of CA breast cancer and during hospitalization Injection
Zoledronic Acid was administered. The claim was repudiated as per policy clause no. 3.15 – Day
care treatment means the medical treatment and of surgical procedure which is (i) undertaken under
general or local anesthesia in the hospital/day care centre in less than 24 hours because of
technological and (ii) which would have otherwise required a hospitalization of more than 24
hours. Treatment normally taken on an out-patient basis is not included in the scope of this
definition. As the same procedure is day care procedure and not included under procedure list
provided as per terms and conditions. In support of its contention, the insurance company

submitted the opinion by Chief Medical Officer, TPA, Mumbai. As per his opinion the captioned
claim is medially admissible subject to compliance of other relevant T/C of the policy. However,
the claim recommended for repudiation because I/V/O Zoledronic Acid and not necessitating 24
hours hospitalization, not a day care procedure as per latest list circulated by IC. Neither the drug
is Chemo/Immunotherapy/Hormonal/Monoclonal Antibody nor Targeted therapy. Therefore, the
Respondent had repudiated the claim in accordance with the terms and condition of the policy.
19) Reason for Registration of Complaint: Total repudiation of mediclaim under health
insurance policy.
20) The following documents were placed for perusal.
a) Complaint letter
b) Copies of documents submitted by the complainant
c) Form VI A duly signed by the complainant.
d) SCN and a form VIIA duly signed by the Insurance Company
21)Result of hearing with both parties (Observations and Conclusion) :- :- I heard both the
sides, the complainant (represented by her husband) and the Insurance Company through
Video conferencing. The complainant submitted that he was not paid claim of hospitalizations
for chemotherapy by the Insurance Company. The complainant submitted that insurance
company settled the claim on clause no. 3.18, 3.2, which were totally irrelevant conditions to
the claim. Finally, the reply received from the GRO that the hospitalization was not required
for this treatment. It was also added by the complainant that the hospitalization was made on
the advice of the treating doctor and there was active line of treatment, hence the claim was
justified. In support of his contention, the complainant quoted the decision which has been
narrated in his application to this forum. The Insurance Company reiterated the contents
submitted in the SCN and further added that the drug administered was not the chemotherapy
and also not listed in the Day care procedure list, as as per the policy conditions day care
procedure only parent or oral chemotherapy was covered.
On perusal of the documents exhibited and oral submission made during the course of Video
Conferencing, I find that as per the discharge ticket, the patient was admitted for administration
of Zoledronic acid, which is used in treatment of Stage IV Breast cancer with bone mets and
for supportive care after administration dose of palbace and letrozole. The drug administered
and used for treatment of cancer spread in bones and supportive care for infusion of injection
under close observation, which was necessary keeping in view the condition of the patient. It
is the treating doctor to decide treatment as per the condition of patient, hence active line of
treatment can not be questioned. The patient underwent for this therapy as last left option for
her treatment on the advice of the treating doctor. Keeping all the aspects in view, I find that
all the claim is payable.
Accordingly, an Award is passed with a direction to the Insurance Company to pay the
claim to the insured, as admissible.
22. The attention of the Complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rules, 2017(as amended till date):
a) According to Rule 17(5) of Insurance Ombudsman Rules, 2017(as amended till date), a copy
of the award shall be sent to the complainant and the insurer named in the complaint.
b) As per Rule 17(6) of Insurance Ombudsman Rules, 2017(as amended till date), the insurer shall
comply with the award within 30 days of the receipt of the award and intimate compliance of
the same to the Ombudsman.
Place: Jaipur RAJIV DUTT SHARMA
Dated: 27.04.2022 INSURANCE OMBUDSMAN
AWARD
Taking into account the facts and circumstances of the case and the submissions made by
both the parties during the course of hearing, the Insurance Company is directed to pay
the claim to the insured, as admissible.
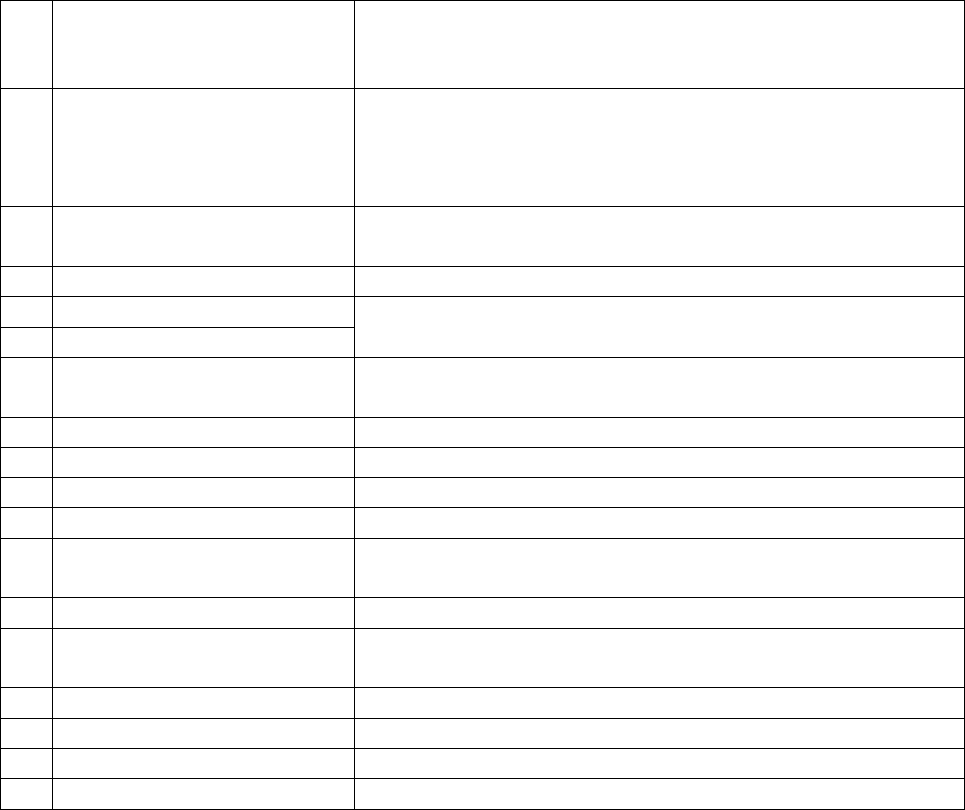
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mrs. Jhuma Sinha vs. Unite India Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-051-2122-0329
AWARD NO: IO/BHU/A/HI/ /2022-23
1.
Name & Address of the
Complainant
Mrs. Jhuma Sinha.
Plot No. 1194/27D, Sector-6 CDA,
Po: Abhinab Bidanasi, Cuttack-753014. Mob-93xxxxxx00
2
Policy No:
Type of Policy
Duration of policy/Policy
period
03xxxxxxxxxxxxxxxxxx39 (SIV Rs.1,00,000/-) Group Health
Insurance Policy, 16/03/2019 to 15/03/2020
Date of admission 24/02/2020 D.O.D 26/02/2020
3.
Name of the insured
Name of the policyholder
Mrs. Jhuma Sinha
Mrs. Jhuma Sinha
4.
Name of the insurer
United India Insurance Insurance Co. ltd
5.
Date of Repudiation
Not repudiated, partially settled.
Not applicable
6.
Reason for repudiation
7.
Dt of receipt of the
Complaint
27/01/2022
8.
Nature of complaint
Requested to advice the Insurer to settle the balance amount
9.
Amount of Claim
Rs.39,600/-/-
10.
Date of Partial Settlement
22/08/2020
11.
Amount of relief sought
Rs.39,600/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
25/04/2022, Bhubaneswar
14.
Representation at the
hearing
a) For the Complainant
Self through VC
b) For the insurer
Mr. P K rout in person
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017
16
Date of Award/Order
25/04/2022
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mrs Jhuma Sinha was
covered under policy No. 03xxxxxxxxxxxxxxxx39 for the period from 16/03/2019 to 15/03/2020
having sum insured of Rs.1,00,000/-. She was admitted in Rotary Club of Cuttack Eye Hospital &
Research Institute on 24/02/2020 with diagnosis of RE PSEUDOPHAKIA and LE NS GR II + VH and
discharged on 26/02/2020. Then she lodged a claim for Rs. 39,600/- which was settled by the
insurer for Rs.13,594/. Being aggrieved with the partial settlement the complainant, made an
appeal before this forum for redressal.
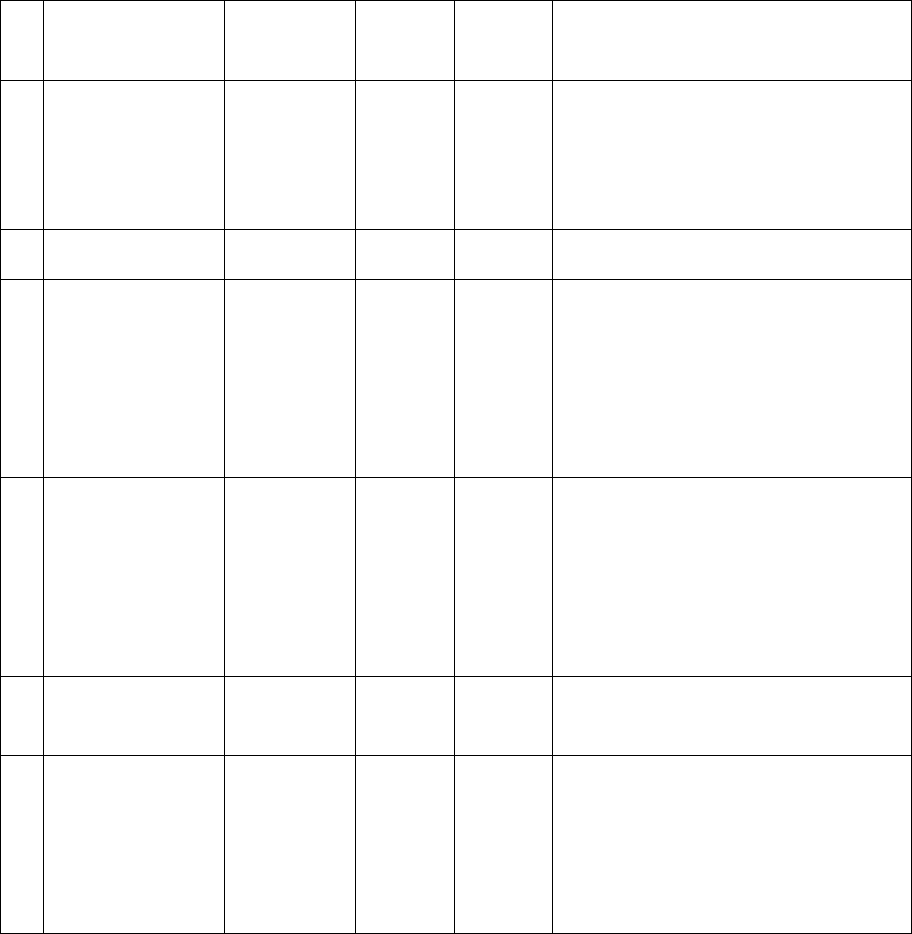
b. The insurer in their self-contained note confirmed issuance of the above policy and stated
that, the Insured Mrs Jhuma Sinha went for Left Eye Cataract Surgery and got herself admitted in
J.P.M Rotary Club of Cuttack Eye Hospital & Research Centre for the period 24/02/2020 to
26/02/2020. (It may please be noted that this is the 2nd claim as earlier (a year before) also she
got her Right Eye treated for cataract under previous policy in the same Hospital and her period
of stay was 28/01/2019 to 30/01/2019). Total bill amount raised by the Hospital for her
treatment during the period 24/02/2020 to 26/02/2020 is Rs 39,600/- against maximum capping
of Rs 25,000 (as capping for cataract is also limited to 25% of the Sum Insured of Rs.1.00 lakh as
per condition no- 1.2.1) On this, TPA made the payment of Rs 13,594, the bifurcations of which
are as follows:
l.
Bill for
Bill
Amount
Payable
amount
Non
payable
Reason for deduction
1.
Room Rent and
Nursing
6000+2700
2700
6000
Excess of Room Rent Rs.6000
2
Pathology
450
450
0
3
OT Charges
4000
920
3080
Proportionate deduction due to
higher room rent occupancy
Rs.3080
4
Anaesthetise
charges
1500
345
1155
Proportionate deduction due to
higher room rent occupancy
Rs.1155
5
Consultation
visit
150
150
0
6
Procedure
charges
500
115
385
Proportionate deduction due to
higher room rent occupancy
Rs.385
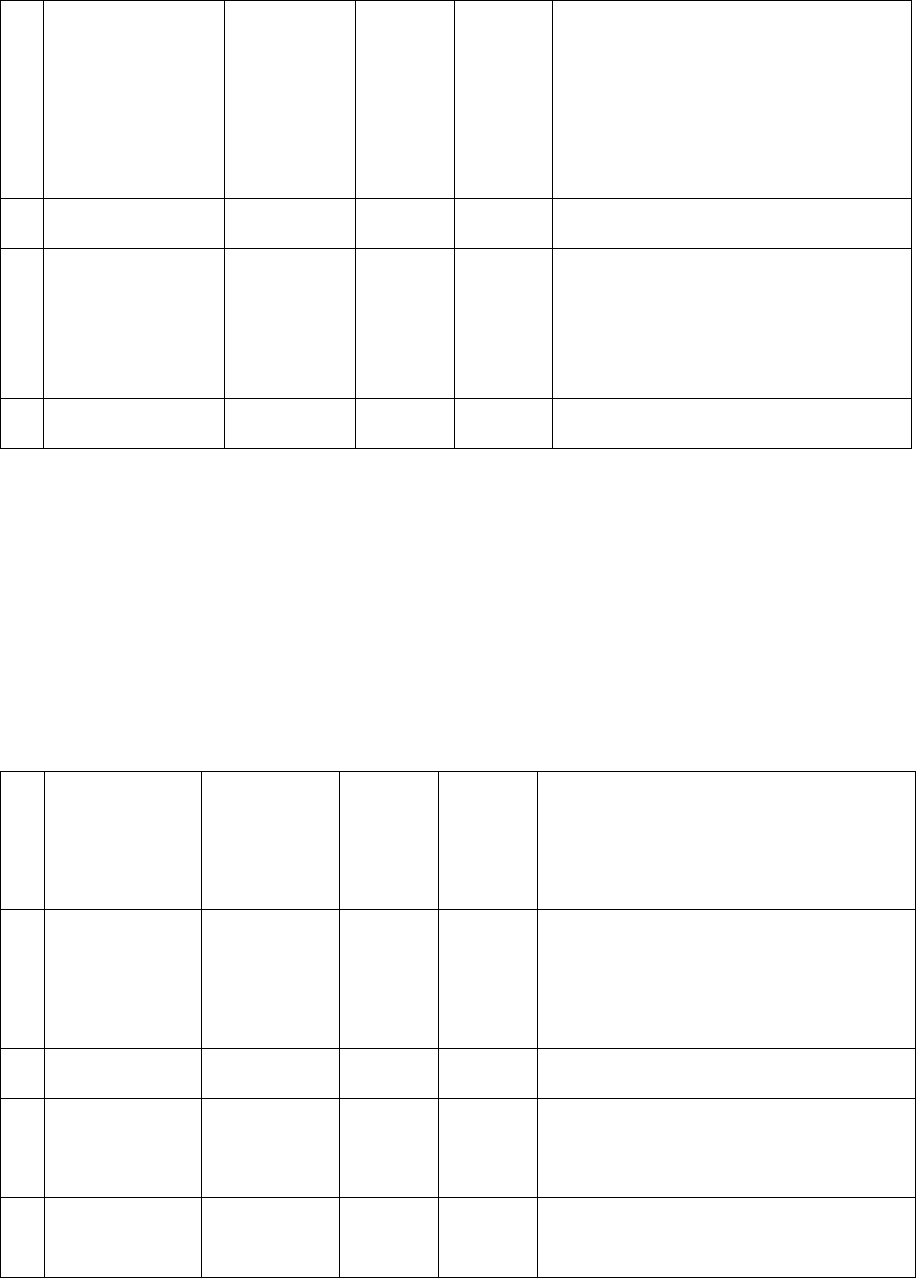
7
Surgeon charges
10500
2414
8086
Proportionate deduction due to
higher room rent occupancy
Rs.8086
8
Implant/stent
6500
6500
0
9
OT
Consumables
7300
0
7300
OT. consumable details not
submitted,
Total
39600
13594
26006
The insured is aggrieved for less settlement of the claim. The concerned office paid the claim on
the line as recommended by TPA. As mentioned above the claim was paid for Rs.13594/ against
claimed amount of Rs.39600/-, because the insured has opted for a higher room rent category.
Hence the claim was reduced proportionately to match the sum insured of Rs. 1,00,000, as per
which Room Rent and Nursing should be within Rs. 1000/ (i.e. 1% of Rs.1 Lakh), but the insured
has opted for a room rent of Rs 2900/-. Hence deduction was made according proportionately.
However again on review of the all the documents available, the concerned office informed that
a supplementary compensation of Rs. Rs 4712 / can further be offered to her as per the following
calculations.
Sl.
Bill for
Bill Amount
Payable
amount
(Earlier
paid)
Extra
payable
Reason for deduction
1.
Room Rent
and Nursing
6000+2700
3000
(2700)
300
Room Rent and Nuring fall under
same head which is limited to
maximum of 1% of Sum Insured i.e,
Rs 1000 per day in this case.
2
Pathology
450
450
0
Pre hospitalisation charges
3
OT Charges
4000
1379
(920)
459
Proportionate deduction due to
higher room rent occupancy
4
Anaesthetise
charges
1500
517
172
Proportionate deduction due to
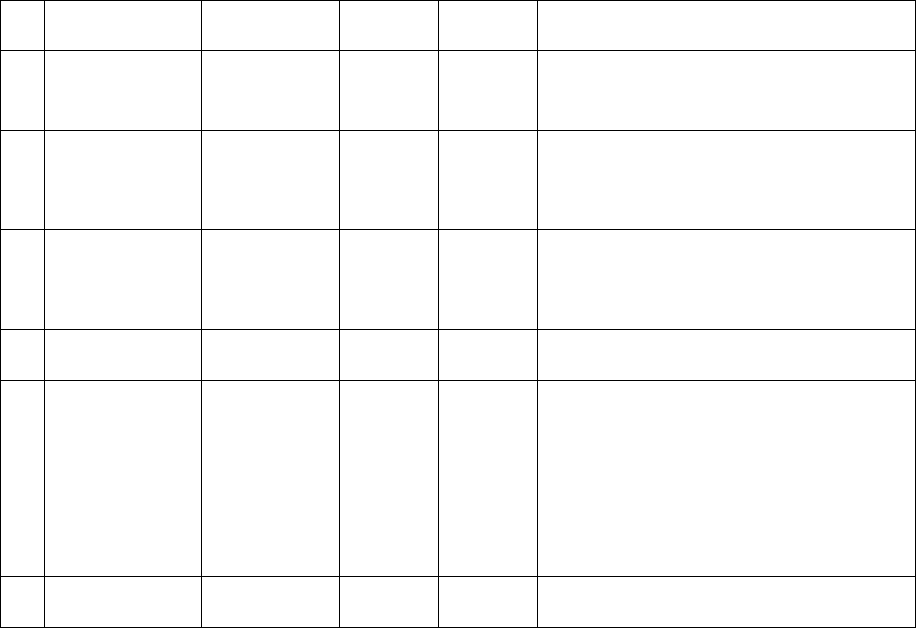
(345)
higher room rent occupancy
5
Consultation
visit
150
150
0
Pre- hospitalisation charges
6
Procedure
charges
500
172
(115)
57
Proportionate deduction due to
higher room rent occupancy
7
Surgeon
charges
10500
3621
(2414)
1207
Proportionate deduction due to
higher room rent occupancy
8
Implant/stent
6500
6500
0
Full amount honoured
9
OT
Consumables
7300
2517
(00)
2517
OT Consumables details were not
shared by the Hospital to TPA even
after several reminders hence TPA
has not honored that,However we
can still allow it as per Proportionate
%
Total
39600
18306
4712
Accordingly, the concerned office has informed that they are already in the process of making a
further payment of Rs.4712/-. to the insured. In view of the above they requested this forum to
kindly peruse the above sympathetically and dismiss the above complaint by giving them a just
order, as the claims was dealt by honouring the terms, condition, and exclusion of the policy,
18. a. Complainant’s Argument. She has submitted bill for Rs.39,600/. But insurer settled the
claim for Rs.13,594/- which is not justified.
b. Insurer’s Argument: Insured opted higher room rent so they proportionately reduced the
charges.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of medical report and bills
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard both the
parties. The complainant stated that the insurer has wrongly deducted the amounts and offered
Rs.13594/- against claim amount of Rs.39600/-, which is not acceptable. The insurer stated that
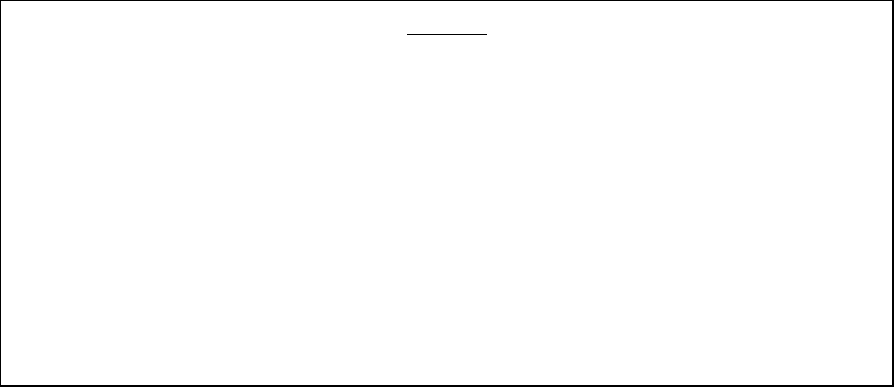
the benefit under cataract is limited to Rs.25,000/- under the policy and the complainant has
availed higher category room rent, accordingly he is eligible for proportionate payment for all
other expenses under policy terms and conditions. The insurer added that they had earlier
offered Rs.13594/- and now they have recalculated and have come out with a new offer at
Rs.18307/-.
22. The attention of the complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rule,2017:
a. According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall comply
with the award within 30 days of the receipt of the award and shall intimate the
compliance of the same to the Ombudsman.
b. As per Rule 17(8) of the said rules, the award of Insurance Ombudsman shall be binding
on the Insurers.
Dated at Bhubaneswar on the 25th day of April 2022 INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
AWARD
Taking into account the facts and circumstances of the case and submissions made by
both the parties during the course of hearing, the forum observes that revising the claim
amounts after a complaint is lodged not only causes problems for the claimants but also
tarnishes their own image. The Forum observes that even after review of the claim by
the insurer, the claim is not properly assessed. The complainant is eligible for more than
Rs.25,000/- even after allowing proportionate deductions due to higher room rent
category, but since the maximum capping under the policy is limited to Rs.25,000/-, the
insurer is directed to pay the complainant Rs.25,000/- (Rupees twenty-five thousand
only) towards full and final settlement of the claim under this complaint.
Accordingly, the complaint is allowed.
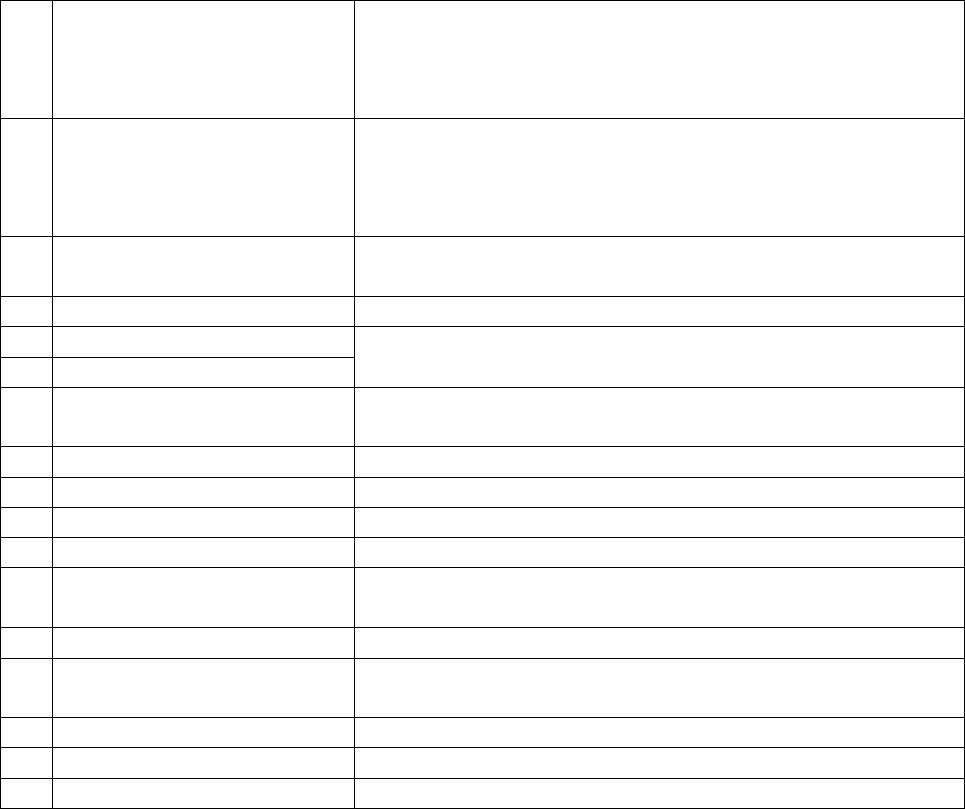
PROCEEDINGS BEFORE
THE INSURANCE OMBUDSMAN, STATE OF ODISHA, BHUBANESWAR
(UNDER RULE NO: 16(1)/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
OMBUDSMAN – Shri Suresh Chandra Panda
CASE OF Mr. Sadananda Swain Vrs. Tata AIG General Insurance Co. Ltd
COMPLAINT REF: NO: BHU-H-047-2122-0275
AWARD NO: IO/BHU/A/HI/ /2021-22
1.
Name & Address of the
Complainant
Mr. Sadananda Swain
4699/27 Adimata Colony, Near Sainika School,
PO; Mancheswar Railway, Bhubaneswar-751017
Mob-9437141167
2
Policy No:
Type of Policy
Duration of policy/Policy
period
02838452957 00904428 (SIV Rs.5,00,000/-) Group Medicare
16/08/2020 to 15/08/2021 (Inception 16/08/2020)
Date of admission 31/07/2021 D.O.D 02/08/2021
3.
Name of the insured
Name of the policyholder
Mr. Sadananda Swain
Mr. Sadananda Swain
4.
Name of the insurer
Tata AIG General Insurance Co. Ltd
5.
Date of Repudiation
28/10/2021
Non-disclosure of pre-existing disease.
6.
Reason for repudiation
7.
Dt of receipt of the
Complaint
07/01/2022
8.
Nature of complaint
Requested to advice the Insurer to settle the claim
9.
Amount of Claim
Rs.55,243/-
10.
Date of Partial Settlement
Not applicable
11.
Amount of relief sought
Rs.55,243/-
12.
Complaint registered under
Rule no: of IO rules
13(1)b
13.
Date of hearing/place
17/03/2022, Bhubaneswar
14.
Representation at the
hearing
a) For the Complainant
Self through phone
b) For the insurer
Not appeared
15
Complaint how disposed
U/R 17 of the Insurance Ombudsman Rules, 2017

16
Date of Award/Order
17/03/2022 and 28.04.2022
17. a. Brief Facts of the Case/Cause of Complaint: - The Complainant Mr. Sadananda Swain
was covered under policy No. 02838452957 00904428 for the period from 16/08/2020 to
15/08/2021 having sum insured Rs.5,00,000/-. He was hospitalised in Utkal Hospital,
Bhubaneswar from 31/07/2021 to 02/08/2021 with complaints of Intermittent fever and cough
for 2 days f/b loose stool, 2 episodes COVID-19 Positive with Dengue Fever, Hypertension.
Thereafter he lodged a claim for reimbursement of hospitalisation expenses which was
repudiated by the Insurer on the ground non-disclosure of pre-existing disease. Being aggrieved
with the repudiation the complainant made an appeal before this forum for redressal.
b. The insurer in their self-contained note confirmed issuance of the above policy and stated
that the complainant Mr. Sadananda Swain was admitted in Utkal Hospital, Bhubaneswar for the
period from 31/07/2021 to 02/08/2021. It was observed that the complainant was diagnosed
with “Covid-19 Positive with Dengue Fever, Hypertension.” He lodged a claim for reimbursement
of hospitalisation expenses of Rs.55,243/-. They rejected the claim vide their letter dated 28
th
Ocotober,2021 under “Non-Disclosure Clause”.
It is submitted that in various treatment records, below ailments found which are prior to their
policy inception.
Hypertension (High Blood Pressure) – 2006
Gall Bladder Surgery (Cholecystectomy) – 2009
Prolapsed Intervertebral Disc – 2017
Plantar fasciitis -2013
Epicondylitis Elbow joint-2013
Gross Prostatomegaly -2019
Bilateral Kidney Cysts -2019
Hernia Surgery – 2019
The complainant has not disclosed the above-mentioned history to them while taking the policy
in August,2020. The above medical history is material information for issuance of a health policy.
Had this information been made available to them, they would not have issued the policy at all.
Condition Mis-Representation, or non-disclosure of material fact “We will not be liable to pay
under the policy if any Misrepresentation or non-disclosure of material facts noted at the time
of claim or otherwise, whether by you or any Insured person or anyone acting on behalf of you
or an Insured person & policy shall be void ab-initio without any premium refund.”
They annexed copy of proposal form and a self-declaration form submitted by the complainant
at the time of proposing the policy. They also annexed copy of previous treatment records.
18. a. Complainant’s Argument; The above diseases were cured before proposing the policy. So,
it was needless to mention in the application.
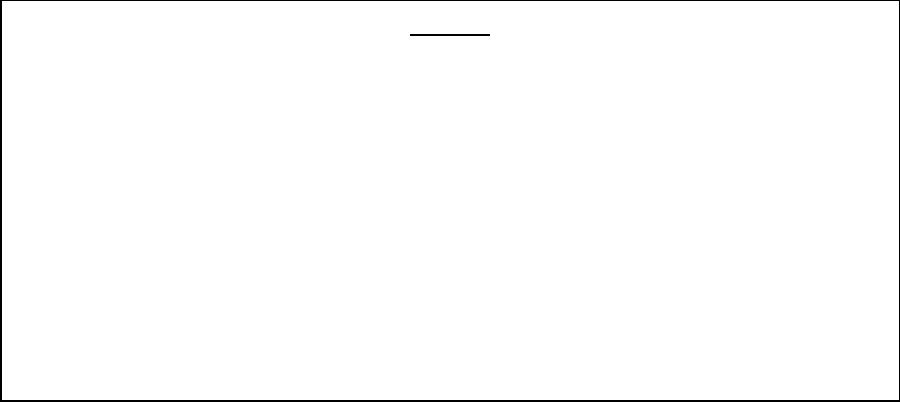
b. Insurer’s Argument: The claim was repudiated strictly in accordance with the terms &
conditions of the policy. The complainant is devoid of any merits and should be dismissed.
19. Reason for Registration of Complaint: Scope of the Insurance Ombudsman Rules, 2017
20. The following documents are placed in the file.
a. Policy copy and clauses
b. Photo copy of medical report
21. Result of hearing with both parties (Observations & Conclusion): - This Forum has
carefully gone through all the documents and papers relating the complaint and heard the
complainant in absence of the insurer. The complainant stated that he had taken the first policy
from Apollo Munich as the bank had earlier tied up with the said insurer. He had to port the policy
to the respondent insurer since the banker has changed the insurer. He suffered from Covid and
was treated, but the insurer declined the claim under pre-existing disease.
22. The attention of the complainant and the Insurer is hereby invited to the following provisions
of Insurance Ombudsman Rule,2017:
a. According to Rule 17(6) of Insurance Ombudsman Rules,2017, the Insurer shall comply
with the award within 30 days of the receipt of the award and shall intimate the
compliance of the same to the Ombudsman.
b. As per Rule 17(8) of the said rules, the award of Insurance Ombudsman shall be binding
on the Insurers.
AWARD
Taking into account the facts and circumstances of the case and submissions made by
the complainant during the course of hearing, the forum examined the facts stated by
the complainant and found to be correct that the policy has been in force since
16.08.2018. The forum also examined the medical documents submitted by both the
parties and failed to find any record of pre-existing disease. Moreover, Covid is a new
disease and has no bearing on the pre-existing disease. In view of the above, the insurer
is directed to pay the complainant Rs.52,481/- (Rupees fifty-two thousand four hundred
eighty-one only) after a reasonable deduction of 5% towards non-payable items, as full
and final settlement of the claim under this complaint.
Accordingly, the complaint is allowed.
Dated at Bhubaneswar on the 17th day of March, 2022 INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
Corrigendum: Date:
Further to Award dated 17th March, 2022 it is found that the insurer had also terminated the
policy, which was part of the main complaint but the point was missed out in the award.
Considering the facts of the matter, it is further examined and the found that the termination
of policy is not appropriate as the basis, on which the claim was rejected, was not correct.
Therefore, the insurer is directed to also revive and renew the policy of the complainant
allowing all renewal benefits.
Dated at Bhubaneswar on the 28
th
day of April, 2022 INSURANCE OMBUDSMAN
FOR THE STATE OF ODISHA
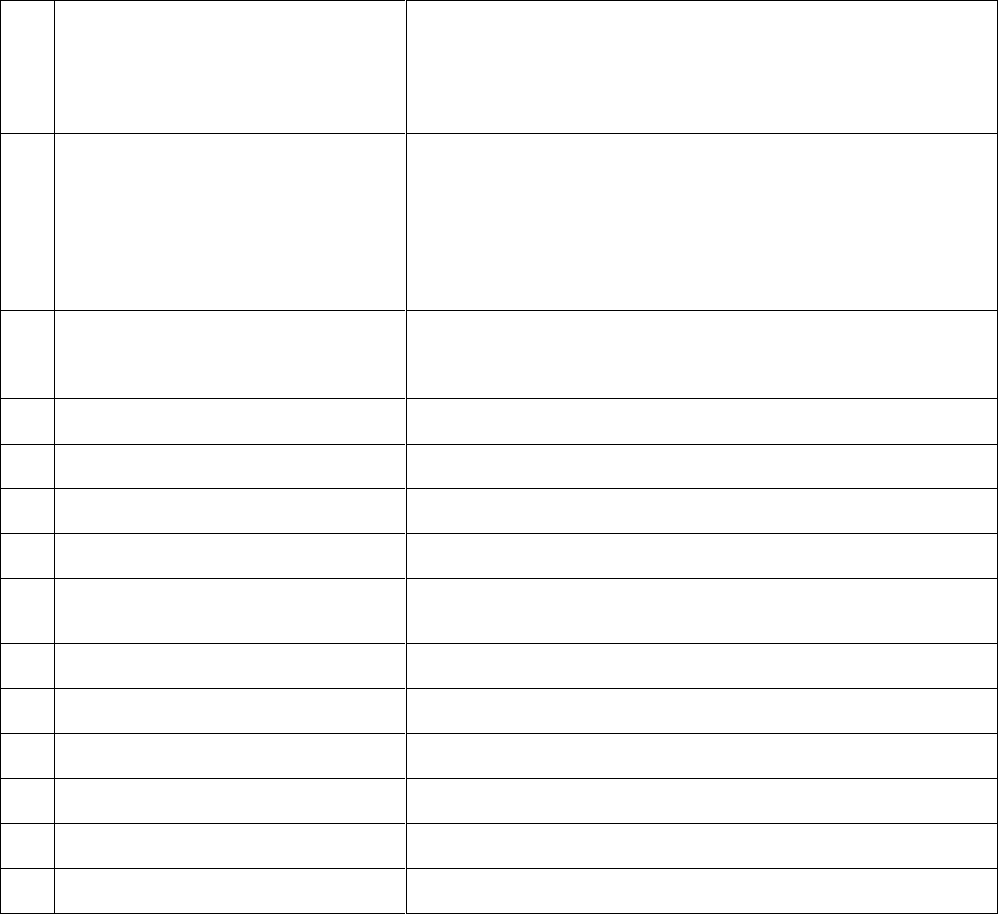
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN, AHMEDABAD
State of Gujarat and Union Territories of Dadra, Nagar Haveli and Daman & Diu
(Under Rule No: 16 / 17 of The Insurance Ombudsman Rules, 2017)
Case Mr. Laxman Gangaram Barot Vs. The National Insurance Company Ltd.
Complaint Ref. No. AHD-H-048-2122-3033
1
Name & Address of the
Complainant
Mr. Laxman Gangaram Barot
25, Hemang Park Society, NR. Boot Bhavani Bus Stop,
Vejalpur, Ahmedabad, Gujarat-380051
2
Policy No:
Type of Policy
Policy period
Sum Insured
251100502010000380
Union Bank Retiree Group Policy
01.11.2020 to 31.10.2021
Rs. 4,00,000/-
3
Name of the insured
Name of the policy holder
Mr. Laxman Gangaram Barot
Mr. Laxman Gangaram Barot
4
Name of the insurer
The National Insurance Company Ltd.
5
Dates of Hospitalization
10.09.2021 to 11.09.2021
6
Reason for Dispute
Partial Settlement of Claim
7
Date of receipt of complaint
05.01.2022
8
Reason for Partial Settlemetn
Reasonable and Customary
9
Date of Consent
25.02.2022
10
Date of receipt of SCN
Not received
11
Amount of claim
Rs. 58,655/-
12
Amount paid by Insurer
Rs. 34,155/-
13
Amount of relief sought
Rs. 24,500/-
14
Complaint registered under
Rule 13(1)(b) of the I.O. Rules 2017
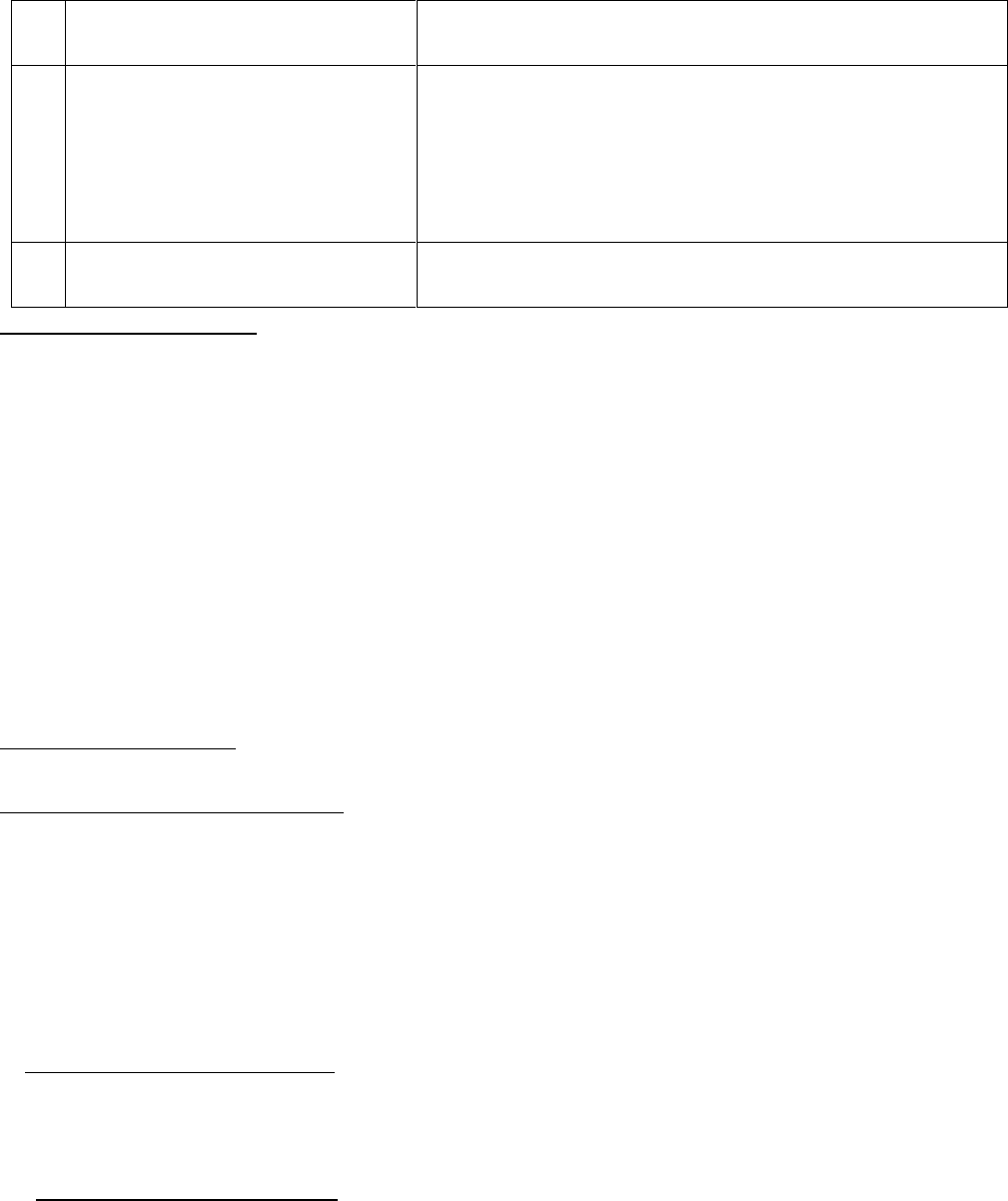
15
Date of video hearing
27.04.2022/ Video Hearing / Ahmedabad
16
Representation at the
hearing:
For the Complainant
For the Insurer
Mr. Laxman Gangaram Barot
Mr. Ranjan Bhatia
17
Date of Award/Order
28.04.2022
18. Brief facts of the case:
The Complainant was insured under Union Bank Retiree Group Policy issued by National
Insurance Company, Pol no. 25xxxxxxxxxxxx0380 for the period 01.11.2020 to 31.10.2021 for the
S.I. Rs. 4,00,000. He was admitted at Akshat Eye Hospital , Ahmedabad on 10.09.2021for Cataract
surgery of Left Eye and was discharge on 11.09.2021. He submitted the claim for Rs.58655/- to
the respondent insurer, which was partially settled for Rs. 34,155/- after deduction of Rs.24,500/-
stating reason :Reasonable & Customary charges. Aggrieved by the decision of the Insurance
Company the Complainant has approached this Forum for redressal of his grievance.
19. Cause of Complaint:
A. Arguments by the Complainant:
The Complainant stated that the deduction of Rs.24,500/- against his justified claim is arbitrary.
At the time of giving the claim intimation , no communication was made to him that the claim
would not be settled for more than Rs.34,155/- and there is no capping for Cataract Surgery. He
requested the Forum to help him to get his legitimate balance amount of the claim Rs.24,500/-.
B. Arguments by the Respondent:
The respondent Insurer has not submitted SCN and post Hearing Deposition.
21. Observations and Conclusion :
Based on the submissions made by both the parties and the documents put on record it is
observed that:
The complainant was covered under Union Bank Retiree Group Policy from National Insurance
Co. Ltd. He was admitted at Akshat Eye Hospital, Ahmedabad on 10.09.2021 and discharged on
11.09.2021 for Cataract surgery of Left Eye. His claim for the said treatment for Rs.58,655/- was
partially settled for Rs. 34,155/- after deduction of Rs.24,500/- stating reason reasonable &
customary charges.
A) “As per IRDAI circular on standardization in health insurance, reasonable and customary
charges means, the charges for services or supplies which are the standard charges for the
specific provider and consistent with the prevailing charges in the geographical area for identical
or similar service, taking into account the nature of the illness/injury”. It is to be noted that
Customary and reasonable expenses for any treatment/procedure will vary with the passage of
time and depends upon various factors like:
A) Qualification, Experience and expertise of the treating doctor.
B) Nature, seriousness and gravity of disease and condition of the patient.
C) Geographical location of the Health Services providers.
D) Availability of Medical and other infrastructure facilities in the Hospital.
E) Usage of advance medical technology.
In the absence of any capping for expenses payable for various procedures/treatments in the
policy, insured has the right of choice to opt for advance medical treatments available and claim
for the same under the policy.
The Customary and reasonable charges change with passage of the time and with improvement
of technologies and facilities. Since the cataract operation was primarily to improve the eye sight
and
restore it to its normalcy, the Surgeon charges, implant charges, anesthesia charges, Operation
Theatre charges, Pathology and pharmacy charges cannot be considered as unreasonable.
Respondent Insurer has not submitted SCN and Post hearing deposition. In view of the forgoing
facts, the decision of the respondent insurance company to deduct Rs.24,500/- invoking policy
condition – Reasonable and Customary charges from the total claim amount of Rs.58,655/- is
not
justified. Hence complaint is admitted.
21. The attention of the Complainant and the Insurer is hereby invited to the following provisions
of the Insurance Ombudsman Rules, 2017:
A) According to Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within thirty days of the receipt of the award and intimate compliance of the
same to the Ombudsman.
B) According to Rule 17(8) of Insurance Ombudsman Rules, 2017, the award of Insurance
Ombudsman shall be binding on the Insurers.
Dated at Ahmedabad on 28
th
day of April, 2022.
(KULDIP SINGH)
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,
State of Gujarat and Union Territories of Dadra, Nagar Haveli and Daman & Diu
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both the
parties during the course of hearing the Respondent is hereby directed to make payment of
Rs.24,500/- to the complainant subject to other terms and conditions of the Policy being full and
final settlement of the claim.
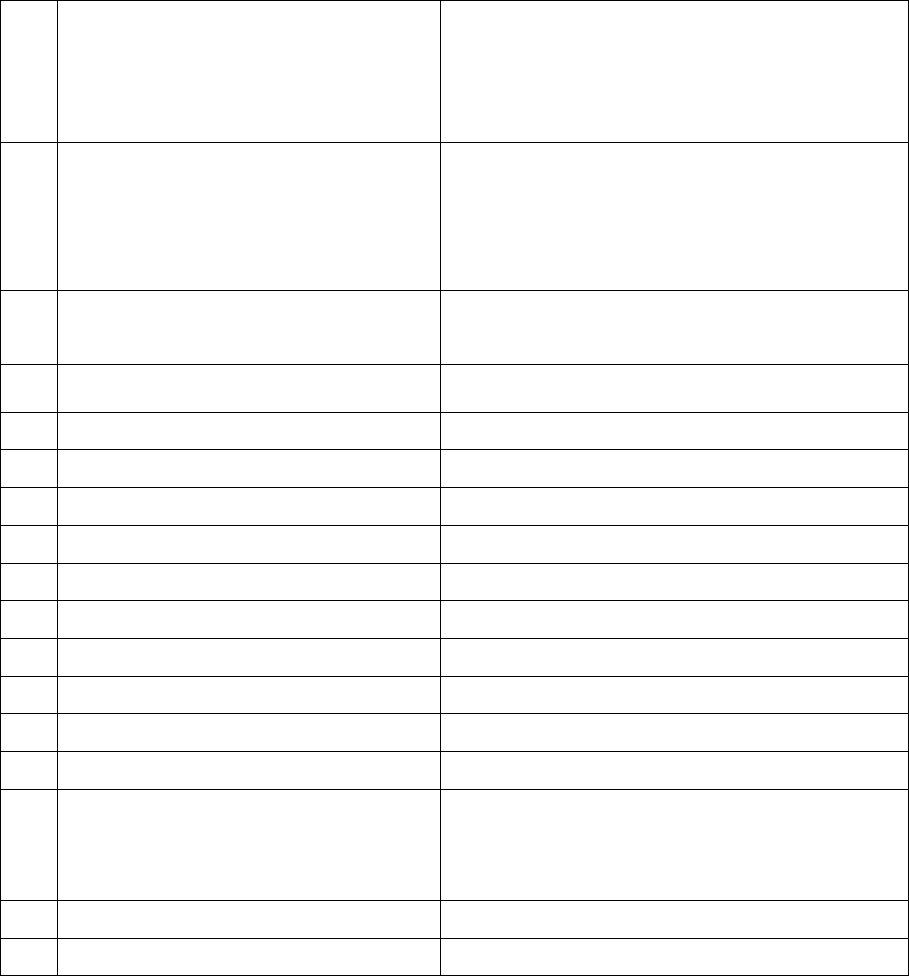
(UNDER RULE NO: 16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Case of Mr. Indravadan Ambalal Bhavsar V/S The Oriental Insurance Co. Ltd.
Complaint No.: AHD-H-050-2122-3059
1
Name & Address of the
Complainant
Mr. Indravadan Ambalal Bhavsar
E-502, Saubhagya Appartment, NR. Sola
Overbridge, S.G. Highway, Gulab Tower Road,
Thaltej, Ahmedabad, Gujarat
2
Policy No.
Type of Policy
Effective from
Sum Insured
144000/48/2021/4240
Oriental Royal Mediclaim Policy (PNB)
14.06.2020 to 13.06.2021
200000/-
3
Name of the Insured
Name of the Policy Holder
Mr. Indravadan Ambalal Bhavsar
Mr. Indravadan Ambalal Bhavsar
4
Name of the insurer
The Oriental Insurance Co. Ltd.
5
Period of Hospitalization
20.04.2021 to 25.04.2021
6
Reason of partial settlement
As per terms and conditions of the policy.
7
Date of receipt of complaint
24.11.2021
8
Nature of complaint
Partial settlement of the claim
9
Amount of claim
92681/-
10
Claim Amount Settled
30195/-
11
Amount of relief sought
62486/-
12
Complaint registered under Rule No.
Section 13 (1) (b) of I.O. Rules,2017
13
Date of receipt of VI-A / SCN
02.03.2022 /22.04.2022
14
Date of hearing/place
27.04.2022– Video Hearing
15
Representation at the hearing:
For the Complainant
For the Insurer
Mr. Indravadan Ambalal Bhavsar
Mr. Praveen Antal
16
Complainant how disposed
Award
17
Date of Award/Order
27.04.2022

18.Brief History:
The Complainant was covered under PNB Royal Mediclaim Policy with the period of 14.06.2020
to 13.06.2021 with a Sum Insured for Rs 200000/- issued by the Oriental Ins. Co. Ltd. He was
hospitalized at Ananta Multispecialty Hospital, Ahmadabad during 20.04.2021 to 25.04.2021 and
treated for CoViD-19 positive pneumonia. The claim was lodged for Rs.92681/- and was settled
by the respondent insurance company for Rs.30195/- after deduction of Rs.62486/- as per terms
and conditions of the said policy. Furthermore, he also represented to the Company against the
partial settlement, but of no avail. Aggrieved by the same, the complainant approached this
forum.
19. Cause of Complaint:
(A) Complainant’s argument:
The complainant submitted that he was hospitalized at Ananta Multispecialty Hospital,
Ahmadabad during 20.04.2021 to 25.04.2021 and treated for CoViD-19 positive pneumonia. The
claim was lodged for Rs. 92681/- and was settled by the respondent insurance company for
Rs.30195/- after deduction of Rs.62486/- as per terms and conditions of the said policy. He has
urged the Forum to help him in getting the genuine claim.
(B) Insurer’s Argument:
The representative of the respondent submitted that as per claim documents submitted by the
complainant, the claim was settled as per terms and conditions of the said policy. She further
mentioned that as per coverage clause of the subject policy proportionate deduction have made
from the claim. In view of the same, he has prayed before the forum to dismiss the case without
any relief to the insured.
20. Result of hearing with both parties (Observation & Conclusion):
Based on the submission of both the parties and the materials made available to this Forum, the
following points have emerged which are pertinent to decide the case:-
1) The complainant was admitted in at Ananta Multispecialty Hospital, Ahmadabad during
20.04.2021 to 25.04.2021 and treated for CoViD-19 positive pneumonia.
2) The claim was lodged for Rs. Rs. 92681/- and was settled by the respondent insurance
company for Rs.30195/- after deduction of Rs.62486/- as per terms and conditions of the
said policy.
3) With a view to rationalize the treatment cost for Covid-19 patients; the Govt. of Gujarat
through Ahmedabad Municipal Corporation issued guidelines vide their circular dated
01.06.2020 & 11.12.2020 which is required to be followed by all hospitals providing CoViD
19 treatment.
4) Therefore, this forum shall evaluate the admissibility of the claim strictly in accordance
with the guidelines dated 01.06.2020 & 11.12.2020 issued by the Government of Gujarat
through Ahmedabad Municipal Corporation.
5) The patient was hospitalized in isolation Ward for 06 days, which is mentioned in the said
guidelines dated 01.06.2020 & 11.12.2020 issued by the Government of Gujarat through
Ahmedabad Municipal Corporation.
6) Hence, this forum would abide by the charges fixed for the same which are fixed towards
Isolation package charges, which include the charges for routine investigations and some
of the medicines except medicine Tocilizumab, special doctor visit fee, specialized lab test
and dialysis.
7) As per the guidelines dated 01.06.2020 issued by the Government of Gujarat through
Ahmedabad Municipal Corporation the complainant is eligible for room charges @
11300/- per day.

8) As per said guidelines the covid -19 hospitalized patient is entitled to receive special
Dr’s visit charges under two category 2000/- and 3500/- respectively. Proper
documentation required from the hospital for the same. The special doctor visit fees
are allowed @Rs.3500/- per visit, Maximum two times in a day for the specialist doctor
charges.
9) The specific name and qualification of doctor/s is/are necessary to be mentioned in the
Discharge Summary. Even though the team of doctor is managing the entire treatment,
the name of the in-charge/head of the team along with his professional qualification has
to be necessarily mentioned to enable the Insurance Company to validate that the
treatment has been given by the qualified and concerned doctor only.
10. It is observed that the claim has been settled by the respondent based on the terms and
conditions of Happy Family Floater Policy and settled the claim for Rs. 30195/-, which is not
justified in accordance with the issued guidelines, Govt. of Gujarat through Ahmedabad
Municipal Corporation vide their circular dated 01.06.2020 & 11.12.2020.
Therefore, this Forum directs to the insurance company to evaluate the admissibility of the
claim strictly in accordance with the guidelines dated 01.06.2020 & 11.12.2020 issued by the
Government of Gujarat through Ahmedabad Municipal Corporation and other terms and
conditions of the policy and pay the additional claim after deduction of Rs. 30195/- claim
amount already paid to the insured.
In view of the forgoing facts, The Complaint is admitted and disposed off accordingly.
AWARD
Taking into account the facts & circumstances of the case and the submissions made the
complaint is disposed off as per above direction.
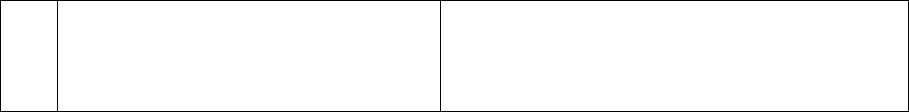
21. The attention of the Complainant and the Insurer is hereby invited to the following
provisions of the Insurance Ombudsman Rules, 2017:
C) According to Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall
comply with the award within thirty days of the receipt of the award and intimate
compliance of the same to the Ombudsman.
D) According to Rule 17(8) of Insurance Ombudsman Rules, 2017, the award of Insurance
Ombudsman shall be binding on the Insurers.
Dated at Ahmedabad on 27th day of April 2022
(KULDIP SINGH)
INSURANCE OMBUDSMAN
PROCEEDINGS BEFORE THE INSURANCE OMBUDSMAN,AHMEDABAD
State of Gujarat and Union Territories of Dadra, Nagar Haveli and Daman & Diu
(UNDER RULE NO: 16/17 OF THE INSURANCE OMBUDSMAN RULES, 2017)
Case of Mr. Sandeep Agrawal V/S CholaMandalam MS Gen. Ins. Co. Ltd.
Complaint No.: AHD-H-012-2122-3058
1
Name & Address of the
Complainant
Mr. Sandeep Agrawal
201, Prestige Tower, Daman Road,
Chala, Vapi, Gujarat-396195
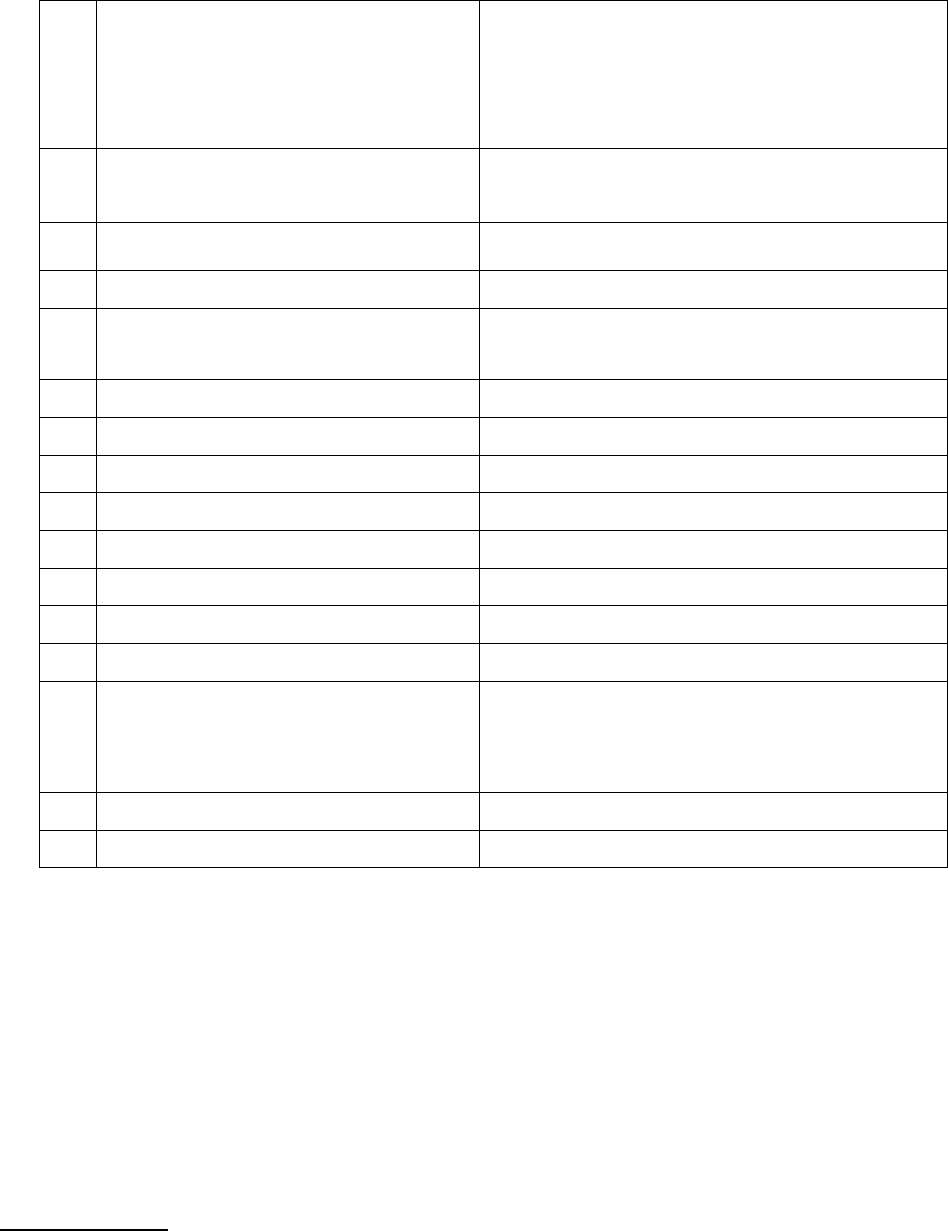
2
Policy No.
Type of Policy
Effective from
Sum Insured
2876/00083927/001/00
Group Health Insurance Policy
19.10.2020 to 18.10.2021
Rs. 7,50,000/-
3
Name of the Insured
Name of the Policy Holder
Mr. Sandeep Agrawal
Mr. Sandeep Agrawal
4
Name of the insurer
CholaMandalam MS Gen. Ins. Co. Ltd.
5
Period of Hospitalization
21.04.2021 to 02.05.2021
6
Reason of repudiation
Claim Repudiated as per terms and
conditions of the policy.
7
Date of receipt of complaint
29.10.2021
8
Nature of complaint
Repudiation of the claim
9
Amount of claim
2,00,588/-
10
Claim Amount Settled
N.A.
11
Amount of relief sought
2,00,588/-
12
Complaint registered under Rule No.
Section 13 (1) (b) of I.O. Rules,2017
13
Date of receipt of VI-A / SCN
03.03.2022/07.04.2022
14
Date of hearing/place
27.04.2022– Video Hearing
15
Representation at the hearing:
For the Complainant
For the Insurer
Mr. Sandeep Agrawal
Dr. Birva Shah
16
Complainant how disposed
Award
17
Date of Award/Order
29.04.2022
18. Brief History:

The Complainant and his family were covered under Group Health policy through PNB with S.I.
750000. The complainant was hospitalized in Arya Hospital, Vapi during 21.04.2021 to
02.05.2021 and treated for viral pneumonia. The claim was lodged for Rs. Rs.200588 /- which
was repudiated by the respondent insurer invoking policy condition no. 4.16 . Furthermore, he
also represented to the Company against the repudiation, but of no avail. Aggrieved by the
same, the complainant approached this forum.
19. Cause of Complaint:
(A) Complainant’s argument:
The complainant submitted that he was hospitalized in Arya Hospital, Vapi during 21.04.2021
to 02.05.2021 and treated for viral pneumonia. The claim was lodged for Rs. Rs.200588/-
which was repudiated by the respondent insurer invoking policy condition no. 4.16. He stated
that he has submitted the all necessary medical document with claim form & payment
receipts to the insurer which was repudiated by the insurer citing that the submitted
document are manipulated and fabricated without genuine hospitalization. He requested the
forum for the genuine claim to be paid to him.
(B) Insurer’s Argument:
The representative of the respondent submitted that as per claim documents submitted by
the complainant, the patient was found to be admitted for treatment of viral pneumonia. As
per investigation Reports and submitted medical documents, it is observed that the
submitted documents are manipulated and fabricated without genuine requirement of the
hospitalization hence the claim is not payable as per policy condition no. 4.16 of the policy.
The representative of the insurance company mentioned that the following are the points
owing to which it has been inferred that the claim is not genuine:
a) Day to day nursing note, progress note and treatment sheet not maintained by hospital.
b) As per insured’s statement dtd. 21.06.2021 he had partially paid hospital bill at the
time of discharge from the hospital.

In view of the same, she has prayed before the forum to dismiss the case without any relief to
the insured.
20. Result of hearing with both parties (Observation & Conclusion):
Based on the submission of both the parties and the materials made available to this Forum, the
following points have emerged which are pertinent to decide the case:-
1) The complainant was hospitalized at Arya Hospital, Vapi during 21.04.2021 to 02.05.2021
and treated for viral pneumonia. The claim was lodged for Rs. Rs.200588/- which was
repudiated by the respondent insurer invoking policy condition no. 4.16.
2) The complainant stated that he has submitted all required documents along with payment
receipt copy total for Rs. 140450/-to the insurance company.
3) The respondent insurer submitted copy of investigation report of Oracle Investigation
Agency, It is mentioned in the report that they have visited and verified treating doctor,
insured, diagnostic centre and pharmacy. The brief findings are as below:
i. Oracle Investigation Agency has confirmed the diagnosis and duration of
hospitalization and entire treatment was given by Dr.Vinit Gupta (MD) Investigator
also confirmed that total hospitalization cost around 140450/- paid to the hospital
through cash and cheque.
ii. Day to day nursing note, progress note and treatment sheet not maintained by
hospital.
iii. Considering the above mentioned findings in the investigation report and other
discrepancies observed, the respondent insurer had repudiated the claim invoking
clause no.4.16 of the policy vide repudiation letter dated 09.08.2021.
4) It is observed from the submitted repudiation letter that respondent insurer repudiated the
claim invoking clause no. 4.16 -: any travel or transportation costs or expenses, which is not
related to the reason of the repudiation mentioned in the repudiation letter as well as in SCN.
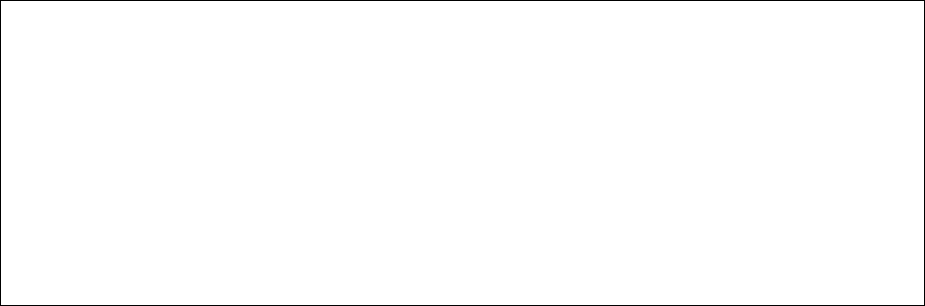
It seems that insurer has not reviewed the claim properly in accordance with the terms of
the subject policy.
5) The IR is not signed by the C.A. and name of the Investigator also not mentioned in the
submitted IR. The conclusive documentary evidence for proving the misrepresentation is
not submitted by the respondent insurer.
6) While analyzing the case with the submitted documents before this Forum, It is found that
the insured patient was hospitalized in Arya Hospital, Vapi during 21.04.2021 to 02.05.2021
and treated for viral pneumonia. The claim was lodged for Rs. Rs.200588/-(Rs.140450.00
Hospital main bill+ Rs.18630.00 Lab charges & pre &post exp.+ 35508.00 Pharmacy charges.)
7) The Forum observed that, the repudiation letter does not make any mention about the
nature and details of the misrepresentation /discrepancies observed by the company and
also the evidences relied upon to arrive at the decision to reject the claim. The company does
not seem to have written to the complainant seeking clarifications. Therefore the decision of
respondent to reject the claim is arbitrary, defective and legally not sustainable.
In view of the forgoing facts, the decision of the respondent insurance company to repudiate the
claim is not justified, hence the complaint stands admitted.
AWARD
Taking into account the facts & circumstances of the case and the submissions made by both
the parties during the course of hearing the Respondent is hereby directed to make payment
of admissible amount along with interest to the complainant, subject to available Sum
Insured and other applicable terms and conditions of the policy, in full and final settlement
of the claim.

21. The attention of the Complainant and the Insurer is hereby invited to the following
provisions of the Insurance Ombudsman Rules, 2017:
E) According to Rule 17(6) of Insurance Ombudsman Rules, 2017, the Insurer shall comply
with the award within thirty days of the receipt of the award and intimate compliance
of the same to the Ombudsman.
F) Rule 17(7)-
‘The complainant shall be entitled to such interest at a rate per annum as specified in the
regulations, framed under the Insurance Regulatory and Development Authority of India
Act, 1999, from the date the claim ought to have been settled under the regulations, till
the date of payment of the amount awarded by the Ombudsman.’
G) According to Rule 17(8) of Insurance Ombudsman Rules, 2017, the award of Insurance
Ombudsman shall be binding on the Insurers.
Dated at Ahmedabad on 29
th
day of April 2022.
(KULDIP SINGH)
INSURANCE OMBUDSMAN
